(Washington) – New data from the World Health Organization (WHO) shows that many governments around the world did not meet public healthcare spending benchmarks amid the Covid-19 pandemic, Human Rights Watch said today. The new information indicates possible violations of countries’ obligations to the human right to health.
WHO’s Global Health Expenditure Database, released in December 2023, shows that most governments did not spend more than 5 percent of Gross Domestic Product (GDP) or 15 percent of their national budget on health care through public means in 2021. These two benchmarks are common and important tools for assessing whether countries are on track to ensure universal health coverage, an international policy target grounded in the human right to the highest attainable standard of health. Despite a global surge in spending related to the Covid-19 pandemic, about 80 percent of the world’s population lived in countries that met neither spending benchmark.
“When governments neglect to invest in their healthcare systems, people and families end up shouldering the burden,” said Matt McConnell, economic justice and rights researcher at Human Rights Watch. “While more spending is not enough on its own to ensure universal access to high quality healthcare services, it can help shift this burden, which causes the most harm for people with the fewest resources.”
The Human Rights Watch analysis of healthcare spending in more than 190 countries around the world, available in a summary table at the end of this document, also found that:
- Despite a mass increase in healthcare spending across the globe in response to the pandemic, 38 governments spent less on health care in 2021, as a share of their GDP, than the year before it began.
- Despite governments’ commitments to reduce out-of-pocket expenditures, individuals and their households collectively paid the equivalent of about US$1.68 trillion for health care out of their own pockets in 2021, a figure comparable to the annual GDP of Australia or the Republic of Korea.
- At the height of the pandemic, out-of-pocket payments covered the costs of more than 20 percent of health care in 119 countries. Only high-income countries averaged less than 20 percent in 2021 (17 percent), while upper-middle (29.9 percent), lower-middle (34.6 percent), and low-income (39.1 percent) countries averaged far more.
- In 47 countries in 2021, individuals and their households collectively paid more out-of-pocket for health care than their governments spent on it.
- Twenty years after agreeing to the Abuja Declaration and committing to spend at least 15 percent of their national budgets on health care, only 2 of the African Union’s 55 member countries met this target in 2021: Cabo Verde (15.75 percent) and South Africa (15.29 percent). On the whole, countries in the African Union spent an average of 7.35 percent of their national budgets on health care that year.
- Eighty-three governments paid more per person to service their external public and publicly guaranteed debts in 2021 than on health care.
The International Covenant on Economic, Social and Cultural Rights requires countries to dedicate the maximum available resources toward the progressive realization of economic, social, and cultural rights, which includes ensuring universal access to quality healthcare services. They should also avoid, unless fully justified, any backward steps, including through budget cuts.
The next few months will provide multiple opportunities for governments to do more than just renew their rhetorical commitments to the realization of the right to health, including at the 77th World Health Assembly in May, at the United Nations Summit of the Future in September, and at the fourth International Conference on Financing for Development in 2025.
Governments should, among other things, set spending benchmarks such as the equivalent of at least 5 percent of GDP or 15 percent of general government expenditures on health care through domestically generated public funds, or an amount that otherwise ensures the maximum available resources for the realization of rights, including the right to health.
Many governments could increase their revenues to fund health care by levying progressive taxes, stemming tax abuses, and tackling public corruption. Wealthier creditor governments should also deliver on their commitments to international assistance and cooperation by ensuring that public debt repayments do not hinder debtor governments’ ability to adequately fund health care.
The coming months also provide an opportunity to address the impact of debt payments on the ability of governments to fund human rights obligations. At the 2024 spring meetings of the World Bank Group and International Monetary Fund, creditor governments and institutions should commit to conducting assessments of such impacts and to considering debt restructuring or relief where appropriate to ensure that debtor governments can adequately protect rights, including health.
“The pandemic showed the vulnerability of healthcare systems around the world to external shocks,” McConnell said. “But it also exposed just how many of these systems were already failing people. Governments need to put their money where their mouth is and commit to financing more resilient, more sustainable, and more rights-realizing healthcare systems for all.”
Health Budgets Under International Human Rights Law
International human rights law includes obligations to respect, protect, and fulfill economic, social, and cultural rights, which includes the right to health.
Governments have the duty to make constant progress toward realizing these rights, and to do the best within their capacities (an obligation to use “the maximum of their available resources”) to reach the highest possible standards of these rights. Retrogressive measures, which can include a decrease in funding for realization of a right, are presumptively a violation of this obligation unless fully justified, such as in some cases of natural catastrophe or financial crisis.
The ultimate measure of progress is the impact of spending on people’s health. For example, the United States spent about 9.6 percent of its GDP on health care through public means in 2021, about 2.56 percentage points above the average among countries in the Organization for Economic Co-operation and Development (OECD). But the impact of this spending on healthcare outcomes was low when compared with other OECD countries, with the US having the lowest life expectancy at birth, the highest death rates for avoidable or treatable conditions, among the highest suicide rates, and among the worst maternal mortality within the OECD in 2021.
There are many reasons why the US healthcare system is expensive, complicated, and does not work for the vast majority of people in the US. But as recent Human Rights Watch research has illustrated, its expensive, largely market-based healthcare system and failure to appropriately regulate pharmaceutical companies and private healthcare serviceproviders produces immense disparities of access and quality that disproportionately affect people with lower incomes and people with medical conditions.
Funding is a key indicator of a government’s priorities, though how much a government spends on health care also does not necessarily capture all its efforts, or lack thereof, to realize the right to health. This includes other indicators, such as laws and policies that effectively address structural or other discrimination, or efforts to improve the social determinants of health with better food, water, housing, and education. Additionally, the reliability and accuracy of official records and other government data, upon which the WHO’s estimates largely depend, can differ, particularly among countries that are less transparent and publicly accountable.
Comparing Public Healthcare Spending to International Benchmarks
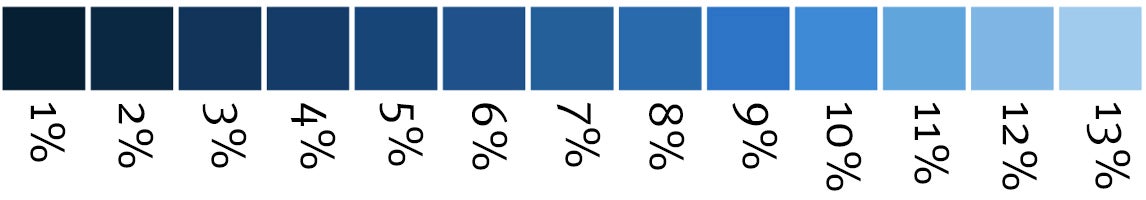
Two of the most common and useful ways of assessing governments’ healthcare spending are by comparing public healthcare expenditures to either (1) the size of the country’s economic output (that is, Gross Domestic Product or “GDP”); and (2) to the size of a country’s total national budget.
Status of Global Public Healthcare Spending, 2021
|
Benchmark |
Global Median |
Global Average |
Countries & Est. Pop. Above (#/%) |
Countries & Est. Pop. Below (#/%) |
|
5% of GDP |
3.54% |
4.08% |
63 Countries; or about 1.4 billion people (18% of world pop.) |
126 Countries; or about 6.3 billion people (82% of world pop.) |
|
15% of National Budget |
10.53% |
11.22% |
47 Countries; or about 1.4 billion people (18% of world pop.) |
142 Countries; or about 6.3 billion people (82% of world pop.) |
Benchmark 1: Percentage of GDP Needed to Fulfill Universal Coverage
The WHO has estimated that providing universal health coverage, a goal distinct from but grounded in the human right to universally accessible health care, will generally require governments to spend the equivalent of at least 5 to 6 percent of their GDP on health care. It has used a 5-percent-of-GDP figure as an indicator to monitor health spending for several decades.
Numerous other assessments of the cost for achieving universal health coverage and related healthcare goals have similarly coalesced around this range. For example, a 2017 review of health economics literature conducted by academics at the University of Cape Town and Harvard University found that:
- Government spending of about 6 percent of GDP reduces the incidence of financial catastrophe and impoverishment from out-of-pocket payments to negligible levels, in-line with WHO guidelines;
- Government spending on health of more than 5 percent of GDP will achieve the very conservative coverage target of 90 percent, set by the WHO’s Commission on Macroeconomics and Health, for 2 fundamental healthcare access and utilization indicators (that is, deliveries performed by a skilled birth attendant and child immunization).
Many of these healthcare goals correspond with several targets and indicators for Sustainable Development Goal (SDG) No. 3, one of the 17 SDGs adopted by all UN Member States in 2015 as part of a global plan to drive economic prosperity and social well-being. When Human Rights Watch compared the WHO healthcare expenditure data with the WHO’s UHC Service Coverage Index, which measures countries’ progress toward SDG 3.8.1 (i.e. “Coverage of essential health services”), there was a moderate-to-strong, positive correlation between public healthcare spending as a percentage of GDP and coverage for essential healthcare services. In general, the more a country spends on health care through public means, the greater share of its population has access to essential healthcare goods and services.
In 2021, however, the last year for which global data is available, the global median public healthcare expenditure was only 3.54 percent of GDP, well below that benchmark. Only 63 of 189 governments spent the equivalent of more than 5 percent of their GDP on health care in 2021. This means that, despite being at the height of the Covid-19 pandemic, 126 countries – governing about 82 percent of the world’s population, or 6.3 billion people – spent less than 5 percent of their GDP on health care through public means in 2021.
Public Healthcare Spending (GGHE-D) as Percent GDP, 2021
About half the countries that met this 5-percent-of-GDP indicator were members of the OECD, a group of high-income countries. Together, these countries, which have some of the most developed health systems, spent an average of about 7.04 percent of GDP on health care from public sources in 2021, roughly double the global median at the height of the pandemic.
High-income countries were not the only ones that heavily invested in health care. Some of the countries that spent the most on health care through public means in 2021, as a share of GDP, were smaller island nations. Cuba, for example, reported spending the equivalent of 12.63 percent of GDP on health care in 2021.
While no low-income countries met this benchmark, six lower-middle income countries did: Kiribati (11.12 percent), Timor-Leste (7.26 percent), El Salvador (6.40 percent), Nicaragua (6.14 percent), Bolivia (5.88 percent), and Samoa (5.12 percent).
Benchmark 2: 15 Percent of National Budget
On average, a country’s national budget equates to about one-third of its GDP. If a country’s budget-to-GDP ratio is around this global average, 15 percent of its national budget will also be about 5 percent of GDP, the level of public investment discussed above that generally corresponds to better healthcare access and outcomes.
Only 47 countries spent more than 15 percent of their national budgets on health care in 2021, with the average around 11.22 percent. That means that 142 countries with about 6.3 billion people – or 82 percent of the total world’s population – did not reach that threshold.
However, if a government does not raise sufficient revenues to meet the global average budget-to-GDP ratio, it can spend 15 percent of its national budget on health care and still fall short of 5 percent of GDP. Comparing these two benchmarks can help identify countries that are demonstrating a commitment to funding health care through their national budgets but may have room to improve by increasing their revenues.
Only 10 Countries Spent More than 15 Percent of their National Budget on Health Care in 2021, But Not 5 Percent of GDP
|
Country |
Public Healthcare Spending (%GDP) |
Public Healthcare Spending (% National Budget) |
Size of National Budget (%GDP) |
|
Iran (Islamic Republic of) |
3.19% |
26.11% |
12.21% |
|
Singapore |
3.51% |
20.81% |
No Data |
|
Paraguay |
4.47% |
18.01% |
24.80% |
|
Dominican Republic |
3.29% |
17.74% |
18.54% |
|
Guatemala |
2.33% |
17.41% |
13.53% |
|
Peru |
3.99% |
16.94% |
23.56% |
|
Lebanon |
2.90% |
16.70% |
9.13% |
|
Cabo Verde |
4.71% |
15.75% |
30.61% |
|
Antigua and Barbuda |
3.93% |
15.54% |
24.01% |
|
South Africa |
4.99% |
15.29% |
32.59% |
These differences are most stark among countries in the African Union (AU), which made an explicit commitment to meet this 15-percent-of-budget benchmark in the 2001 Abuja Declaration. Twenty years later, only 2 of the AU’s 55 member countries spent more than 15 percent of their national budgets on health care: Cabo Verde (15.75 percent) and South Africa (15.29 percent). However, both fell short of meeting the 5 percent of GDP benchmark, although just barely, in the case of South Africa.
Public Healthcare Spending as Percent of General Government Expenditure in Africa, 2021
Twenty Years after the Abuja Declaration, Only Two Countries Met Spending Commitments.
While some other AU countries were not far off – notably Botswana (14.62 percent), São Tomé and Príncipe (13.14 percent), Tunisia (12.40 percent), and Eswatini (12.30 percent) – most countries in Africa were far from meeting this goal.
On the whole, countries in the AU spent an average of 7.35 percent of their national budgets on health care in 2021. Since 2000, the year before Abuja, the average allocation of public funds for health care in Africa has grown by only about 0.31 percentage points, or about one-third the global average over this period.
Retrogression in Public Healthcare Spending
The 20 years leading up to the Covid-19 pandemic were a period of growth in public healthcare spending. In 2000, the average country spent the equivalent of only 2.9 percent of GDP on health care through public means. By 2019, this had grown to 3.59 percent.
However, this growth in public healthcare spending was not equally distributed. The average for high-income countries crossed over the 5 percent of GDP threshold around 2008 and has stayed above this benchmark ever since. Public healthcare spending in low-income countries, meanwhile, essentially stagnated, only slightly growing at a rate about one-sixth the global average.
A Widening Gap:Low-Income Countries’ Public Healthcare SpendingThese disparities and trends in healthcare spending are even clearer when using per-person data adjusted for purchasing power, that is, the amount of goods and services that this money can actually pay for. When data from different countries is equalized to adjust for differences in purchasing power, that metric is often referred to as purchasing power parity (PPP). Using this approach, the average high-income country’s public healthcare spending per person has been worth more than double what is spent by the average country globally since 2000. Only upper-middle-income countries gained much ground over this period, with their income-group average rising to about one-half of the global average by 2021. Low-income countries, meanwhile, went from spending about 3.7 percent of the global average in 2000 to just 2.2 percent in 2021, a roughly 40 percent decline from already-low levels. |
Between 2019 and 2020, public healthcare spending surged by about 0.51 percent of GDP, reflecting the exceptional circumstances of the pandemic. Much of this spending was allocated toward important but costly reactive needs like vaccines and personal protective equipment. But preliminary data from 2022 suggests that this pandemic-related increase in public healthcare spending was largely temporary.
Despite increased healthcare spending across the globe by 2021, 38 governments actually spent less on health care as a share of their GDP, than in the year before the pandemic began.
Economic decreases can hide real-term declines in public healthcare spending, for example, if spending as a percentage of GDP stays the same while a country’s GDP shrinks, hospitals and clinics can receive less funding while government spending appears to remain unchanged. At least six countries had net positive increases in their public healthcare spending as a share of GDP between 2019 and 2021 but decreased their per capita spending when measured in inflation-adjusted US dollars.
Inflation can also hide declines in real-term spending. For example, without adjusting for inflation, Lebanon had a roughly 23 percent decline in its per person public health spending between 2019 and 2021, falling from about 594,388 Lebanese pounds to 519,687. But when adjusted for inflation to constant 2021 values, this is actually a 78 percent real-term decline.
Overall, without adjusting for inflation, 24 governments spent less on health care per person in 2021 than they did in 2019. But when these expenditures are adjusted for inflation, this rises to 41 governments.
Going back further, without adjusting for inflation, only two governments spent less on health care per person in 2021 than they did in 2000: Benin (- 41 percent) and Vanuatu (-16 percent). But when adjusted for inflation into 2021 values, 16 countries reduced their per-person spending, with Madagascar, Benin, and Lebanon all experiencing roughly 62 percent declines.
Sixteen Countries Spent Less on Health Care Per Person in 2021 Than They Did in 2000
|
Country |
2000 Per Capita Public Healthcare Spending (2021 National Currency) |
2021 Per Capita Public Healthcare Spending (2021 National Currency) |
Change (% Difference) |
|
Madagascar |
37,718 |
14,211 |
−62 |
|
Benin |
6,308 |
2,399 |
−62 |
|
Lebanon |
1,364,243 |
519,687 |
−62 |
|
Eritrea |
181 |
81 |
−55 |
|
Vanuatu |
8,681 |
4,017 |
−54 |
|
Haiti |
1,342 |
631 |
−53 |
|
Central African Republic |
5,964 |
3,319 |
−44 |
|
Tuvalu |
1,221 |
724 |
−41 |
|
Chad |
5,447 |
3,417 |
−37 |
|
Sudan |
3,880 |
2,484 |
−36 |
|
Jordan |
116 |
76 |
−35 |
|
Solomon Islands |
736 |
596 |
−19 |
|
Papua New Guinea |
132 |
108 |
−18 |
|
Brunei Darussalam |
1,038 |
869 |
−16 |
|
Cameroon |
4,866 |
4,482 |
−8 |
|
Marshall Islands |
333 |
325 |
−2 |
World Health Organization, Global Health Expenditure Database (Domestic General Government Health Expenditure (GGHE-D), in current NCU per capita); inflation-adjusted to 2021 values using World Health Organization, Global Health Expenditure Database (Gross domestic product - Price index (2021=100).
While these spending changes before and during the pandemic may reflect differences in the healthcare needs of these countries’ populations, they may also reflect changing policy and practice that furthered or hindered the realization of the right to health.
Under the International Covenant on Economic, Social and Cultural Rights, any deliberately retrogressive policies, which can be reflected in decreasing funding allocated to health care, is presumptively a violation of the right to health unless it is fully justified.
Ultimately, what might fully justify such deliberately retrogressive measures is a matter of debate. But the Committee on Economic, Social and Cultural Rights has made clear that the bar is quite high, as even the existence of an armed conflict alone is not sufficient to justify such measures.
The African Commission on Human and Peoples’ Rights General Comment No. 7, providing authoritative normative guidance for interpreting and implementing African state obligations under the African Charter on Human and Peoples’ Rights in the context of private provision of social services, articulates (para. 29) a clearer standard of what states must demonstrate to carry out deliberately retrogressive measures. Stating that such measures must (i) be temporary, (ii) pursue a legitimate aim, (iii) be necessary, (iv) be proportionate, (v) be nondiscriminatory, (vi) involve the full and effective participation of affected groups, and (vii) protect the core content of economic, social and cultural rights at all times.
The Impact of Insufficient Public Healthcare Spending on Out-Of-Pocket Costs
One way to estimate the impact of healthcare spending on people’s right to health is to look at how much people spend on health care from their personal income or savings: their out-of-pocket expenses. When governments don’t fund health care, individuals and households are left to shoulder the burden.
In 2021, households in 47 countries collectively paid more out-of-pocket for health care than their governments spent on it. In Nigeria, the largest economy in Africa in nominal GDP, households’ out-of-pocket health care costs were more than 4.7 times what the government spent. In India, the world’s fifth-largest economy, out-of-pocket costs were the majority of all health care spending that year.
These out-of-pocket expenses generally increase inequalities and create discriminatory barriers to health care based on income, widening gaps in quality of life and life expectancy. The cost of these user fees can also put other rights at risk, including public participation, housing, water, or education.
For example, the WHO’s 2010 World Health Report found that the incidence of financial catastrophe – that is, the proportion of people who spend more than 40 percent of their incomes after deducting expenses for food each year on out-of-pocket healthcare costs – only falls to “negligible levels” when out-of-pocket expenses constitute no more than 15 to 20 percent of a health systems’ total financing. But in 2021, at the height of the pandemic, out-of-pocket payments financed more than 20 percent of the healthcare system in 119 countries.
Only high-income countries averaged below this percent threshold (17.0 percent), while upper-middle (29.9 percent), lower-middle (34.6 percent), and low-income (39.1 percent) countries averaged far higher.
But there is an easy way to bring down healthcare systems’ reliance on out-of-pocket fees. Globally, there is a moderate, negative correlation between public healthcare spending and the share of healthcare costs paid by individuals and households. But this relationship is strongest among low-income countries, where increasing public spending appears to have a much stronger effect on lowering healthcare systems’ reliance on user fees.
Funding for Public Healthcare Expenditures
Many countries may find it difficult to garner the financial resources needed to shift their healthcare systems away from regressive user fees and toward a system grounded in universal access through public healthcare expenditures.
This is often especially true during financial crises. But increasing public spending during economic downturns (that is, “counter-cyclical spending”) has a “clear and well-documented effect on economic growth” and can prevent and manage crises, equalize opportunities, and maximize the realization of human rights, as outlined in guiding principlesadopted by the UN Human Rights Council in 2018, which were drafted by the UN independent expert on the effects of foreign debt.
However, whether a country can adopt such policies and adequately fund programs to mitigate the human rights effects of economic downturns may be influenced by many factors. Whether facing an acute crisis or not, governments can increase needed revenues by addressing external public debt, levying progressive taxes and stemming tax abuses, tackling public corruption, and securing external support from donor countries. Some of these require or will be more effective with international assistance and cooperation.
Public indebtedness appears to be a major impediment to governments’ investment in health care. According to the World Bank’s International Debt Statistics database, in 2021, 83 countries paid more per capita to service their external public and publicly guaranteed debts than on public healthcare expenditures. Benin, for example, paid nearly 26 times as much on foreign debts than on health care in 2021. Belize, which had the largest per capita debt servicing payment in 2021, spent more than 14 times as much on its foreign debt as health care on a per capita basis.
Another important consideration is a country’s revenue raising policies, particularly taxes. A 2016 report from the International Monetary Fund (IMF) suggests that tax revenues above 15 percent of GDP are key to reducing inequality. The World Bank has similarly used this 15 percent tax-to-GDP ratio to measure how much more money governments could raise to spend on social services.
Another reference point may be the average tax-to-GDP ratio among OECD countries, which was about 20 percent in 2021. Some nations with robust social welfare systems may even double these World Bank and IMF benchmarks, such as Denmark, which had a tax-to-GDP ratio of about 35 percent in 2021.
As it may be expected, when Human Rights Watch compared IMF tax-to-GDP data with the WHO’s healthcare spending data, there was a moderate, positive correlation between a country’s tax-to-GDP ratio and its public healthcare spending as a percent of their GDP. In short, states with a larger tax base relative to GDP generally spend more on health care, with low-income states showing the strongest relationship (Pearson Coefficient +0.74).
The IMF has only published 2021 tax-to-GDP ratio data for 107 countries. Of these, 34 countries spent less than the equivalent of 5 percent of their GDP on public healthcare spending and had tax-to-GDP ratios below the World Bank and IMF recommended 15 percent. This suggests that some of these countries may be able to improve funding for healthcare services.
Another way governments could increase their health funding is through addressing abuse of tax systems, both within and outside of their borders. For example, a 2023 report from the Tax Justice Network estimated that countries around the world are losing about US$480 billion each year to tax abuse: both illicit and licit means by which companies and people avoid and evade contributing to public coffers. The Tax Justice Network found that this lost revenue amounts to the equivalent of 9 percent of their collective public health budgets. But for lower-income countries, it amounts to the equivalent of 49 percent of their collective public health budgets. Shoring up tax enforcement can raise considerable public funds that can be allocated, among other priorities, to health care.
Data from 2021 suggests that many countries also relied on assistance from wealthier nations to support their healthcare systems. In 32 countries, donor governments and financial institutions paid for more than 25 percent of all healthcare spending.
Between 2020 and 2021, per capita healthcare spending from donors increased by about 60 percent. This equates to the second-largest increase in the past 20 years after 2003 to 2004.
Research from The Brookings Institution in 2022 found that, while official development assistance rose significantly during the pandemic, donor funds appeared to have been reallocated away from spending essential to health care to increase funds for pandemic preparedness and response.
Public corruption is another tremendous drain on the ability of many governments to fund health care. While estimates vary, it is clear that governments need to address it.
Moving Forward
The new data helps show that many healthcare systems around the world are not meeting international healthcare spending benchmarks that are helpful indicators of whether they are realizing the right to health.
It costs money to create and sustain robust public healthcare systems and to adequately regulate private providers to ensure their public service obligations to society are in line with human rights. But even amid a deadly pandemic, many governments’ policy and budgeting decisions resulted in healthcare financing models that indicate backward movement, inconsistent with their international human rights law obligations.
Funding alone is not enough. Cases like the United States show that an inefficient and expensive healthcare system may not deliver on the right to health despite significant public spending. Spending, however, is a necessary condition for delivering on the right to health.
The next months will provide an opportunity for all governments to renew their commitments to the realization of the right to health. Governments will convene to measure their progress towards the Sustainable Development Goals in April at the UN Economic and Social Council Forum on Financing for Development and in September for an ambitiously titled Summit of the Future. This builds on the UN High-Level Meeting on Universal Coverage that occurred in September 2023, where the representatives of nations all around the world reaffirmed their commitments to “scal[ing] up efforts to ensure nationally-appropriate spending targets for quality investments in public health.”
To realign their domestic financing and healthcare spending with their right to health obligations, states should:
- Set a goal to spend through domestically-generated public funds the equivalent of at least 5 percent of GDP or 15 percent of general government expenditures on health care, or an amount that otherwise ensures the dedication of the maximum available resources for the realization of rights, including the right to health.
- Avoid reductions in funding for health care, unless under exceptional circumstances publicly justified, as outlined by the UN Committee on Economic, Social and Cultural Rights.
- Creditor governments and institutions should assess the impact of debt payments on the ability of governments to meet their human rights obligations and consider debt restructuring or relief where appropriate to ensure governments can adequately protect rights.
- Seek to increase public revenues for allocation to public health care through progressive taxes and changes to policy and enforcement to reduce tax abuses.
- Take steps to prevent and combat public corruption and strengthen international cooperation to realize human rights, in line with the 2021 Political Declaration adopted during the Special Session of the United Nations General Assembly Against Corruption.
Correction: The summary data table originally included at the end of this report omitted relevant years from certain headers as well as data on countries’ inflation-adjusted public healthcare spending per capita. These and a few minor data entry errors in a column summarizing countries’ percent change in gross domestic product per capita between 2019 and 2021 have since been corrected.