(Amsterdam) – The Afghan government is failing to provide sufficient psychosocial, or mental health, support to Afghans who have experienced traumatic events, Human Rights Watch said today.
More than half the Afghan population, including many survivors of conflict-related violence, struggle with depression, anxiety, and post-traumatic stress, but fewer than 10 percent receive adequate psychosocial support from the state, according to government documents. The Afghan government and international donors should expand mental health services and outreach campaigns.
“Decades of violence have left many Afghans experiencing deep psychological wounds, as well as physical ones,” said Jonathan Pedneault, conflict and crisis researcher at Human Rights Watch. “There is an urgent need for expanded psychosocial services to support Afghans exposed to violence, suicide bombings, and airstrikes, and prevent the long-term effects that can be debilitating to survivors, families, and entire communities.”
With large parts of the country facing armed conflict, a weak health system, and a lack of professional health and social workers, mental health services are largely failing to meet the population’s needs. People in rural areas, about 75 percent of the population, are particularly affected. Discriminatory social norms create extra barriers for women and girls.
Forty-one years of war have had a devastating impact on the mental health of millions of Afghans. A 2018 European Union survey found that 85 percent of the Afghan population had experienced or witnessed at least one traumatic event, and averaged four. Half of those surveyed had experienced psychological distress, with one in five Afghans “impaired in his or her role because of mental health problems.”
The government spends only US$7 per capita on health services annually, far below the $30 to $40 that the United Nations Commission on Macroeconomics and Health considered appropriate in 2001. The Public Health Ministry says only about 26 cents of that is spent on mental health. While the mental health budget has increased since 2006, it remains below the $3 to $4 per capita the World Health Organization (WHO) has determined is an appropriate investment for mental health systems in low-income countries such as Afghanistan.
The lack of services, as well as a distrust in public health care and corruption, lead people to pay about three-quarters of their health cost, despite government efforts to provide universal free health care. While adequate investment in mental health is important, the funds need to be spent appropriately, respecting human rights standards, Human Rights Watch said.
The Afghan government has an obligation under international human rights law to move toward the highest attainable standard of health, including mental health, to the maximum of its available resources and on the basis of informed consent. All parties to the conflict, including the Taliban insurgents, are responsible in the areas they control for the availability, accessibility, acceptability, and quality of health care, and to facilitate humanitarian aid.
In 2004, the government made mental health a high health priority and included it in the Basic Package of Health Services (BPHS), which outlined what every Afghan should be able to get within an hour’s walking distance of their home. While government services have fallen short, permanent and mobile clinics run by nongovernmental organizations for displaced people sometimes offer psychosocial services.
In April 2019, Human Rights Watch interviewed 21 Afghans – 14 men and 7 women – in Kabul, Kandahar, and Herat who had experienced psychological distress after direct exposure to conflict-related violence, such as suicide attacks, aerial bombardment, ground fighting, and casualties from unexploded munitions. More than half said they had received little or no psychological support from public health services. Nearly half said they did not know about existing mental health resources.
Human Rights Watch also interviewed 11 doctors and public health specialists who regularly encounter survivors of conflict-related violence, and eight aid workers who provide mental health care and fund programs.
The Human Rights Watch findings, while based on a small number of interviews, are consistent with recent reports and studies on Afghanistan’s mental health system.
Several people interviewed said they believed the lack of early mental health support exacerbated their psychological distress, which included flashbacks, depression, suicidal thoughts, and inflicting violence on family members. In some cases, they lost income or their jobs.
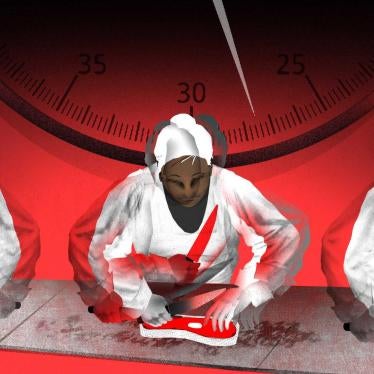
“Ahmad S.,” 23, was offered no psychological counseling after a suicide bombing attack that killed at least 20 people. “It was time to leave the office, about 4 p.m.,” he said about the attack near the Supreme Court in Kabul. “The suicide bomber passed by me and stepped on my shoe, so I took a tissue to clean it and then the explosion happened. I saw dead bodies all around me and parts of bodies.”
Ahmad was treated for injuries at the military hospital, but “Nobody came to ask about my mind,” he said. “They only treated my body.” Two years later, Ahmad sought help but the trauma remains. “I still have flashbacks, all night I can’t sleep,” he said. “I get angry easily, [especially] when people make noise. But I was keeping that anger inside, and I was very sad. I don’t know what kind of treatment should be provided but there should be people asking about our needs.”
In a September 30 email to Human Rights Watch, the Afghan public health minister, Dr. Feroz Ferrozuddin, confirmed that his ministry is aware of the inadequacies of mental health services and that “further policy and financial investment is required given the extent and scope of the challenge to ensure we can effectively address it.”
To begin addressing the shortfalls, the government should increase the scope and reach of its public awareness campaigns to raise mental health literacy and reduce stigma. It should instruct health workers to provide referrals to mental health services, with special attention to women and children. And it should consider less expensive ways to provide basic services, such as remote counseling through mobile phones, focusing intervention on specific communities, self-help training, and peer support groups, as well as incentives to increase the number of counselors in rural areas. All of this should be done from a person-driven approach that does not rely on involuntary treatment or hospitalization.
“This should not be about handing out pills but about getting people the support they need,” said Pedneault.
Afghanistan’s international donors should increase support for government efforts that strengthen the mental health system, particularly those focused on women and children. They should also help improve training for health workers and psychosocial counselors.
“Donor countries should continue to assist the government in prioritizing local psychosocial intervention and increase the availability of mental health services to survivors of conflict-related violence, country-wide,” Pedneault said. “Not doing so will exacerbate suffering from the war and carry many social costs.”
Lack of Mental Health Support
One-third of the 21 survivors of conflict-related violence Human Rights Watch interviewed said they received medical care at clinics or hospitals shortly afterward. All were treated for their physical injuries and described to medical staff how they were injured, but none were referred to mental health counselors or services, or were told such services existed. In part, this was due to the limited referral systems between components of Afghan’s health system. All survivors interviewed are identified with pseudonyms to protect their privacy.
“Armin B.,” a 38-year-old merchant from Kabul, described his reaction when his 13-year-old son was killed in a suicide attack on a Shia Muslim gathering in March 2018 and he recognized a piece of his son’s jacket at the bomb site: “I fell to the ground, I couldn’t control myself. My body was shaking, and I was trying to put Allah in my heart and accept what had happened.” As for mental health services, he said: “I am not aware about [these] services offered by the government. It would be necessary, but I don’t think they exist at all.”
More than a year later, Armin said he still struggled with the impact of his son’s death: “I get angry when my other children do something and then I regret it an hour later.”
“We should follow up with survivors [of traumatic violence], go to their homes and follow them over months,” said Dr. Shafi Azim, a psychiatrist working at the public Kabul Mental Health Hospital. “But the budget and resources do not allow for this.”
Health literacy – the capacity to obtain, process, and understand basic health information – remains low in Afghanistan and awareness of mental health conditions and services is even more limited. A third of those interviewed who experienced trauma-related distress had not considered seeking help because they did not know such services existed.
“Sayyid A.,” a 28-year-old law graduate from Kabul, said his education and work prospects were deeply affected after experiencing depression when his younger brother died in a bomb blast on the road to Maidan, just outside Kabul, five years ago.
“I was 23 and finishing my law studies [when he died],” Sayyid said. “It was difficult for the whole family. I was top in my class, but it changed my grades a lot.” While he remembers having an easy time connecting to people before the tragedy, he says he now finds it difficult to relate to life. “Back then, I was very enthusiastic. But now I don’t want to be in parties or places where there is laughter and happy people. Whenever I [do], I suddenly remember that I lost my brother and that there was so much sadness and crying.”
While Sayyid recognizes that he has been struggling with his brother’s tragic death, he didn’t try to seek help. “It didn’t cross my mind that I could share those thoughts with someone,” he said.
The lack of mental health literacy and the stigma and incomprehension that come along with it highlight the need for health authorities to reach out to victims of conflict-related violence and their relatives and increase public awareness campaigns about mental health and available services. The government’s 2019-2023 National Mental Health Strategy says, “the weakest aspect of the current mental health programme is the lack of sustained public mental health education to increase awareness and acceptance of mental health care.” Doing this would require improving the referral systems and their dissemination among all health personnel.
Health professionals should also be better trained to identify mental health conditions and to refer patients to community-based programs, social services, and psychosocial counselors.
“Siddiqui J.,” a 62-year-old man from Bamiyan, survived a suicide bombing during Ashura celebrations at Kabul’s Abu Fazl mosque in 2011. He lost a hand during the attack and received medical treatment. But when he looked for support to deal with the psychological impact, the doctors provided sleeping medication that he said did not help.
Siddiqui said that shortly after the attack, he began to experience psychological distress. “When I try to sleep, war memories come to my mind and my body starts shaking. Everything gets dark and I lose consciousness. I feel hot in the body and pressure on my shoulders, so I get out of bed and then fall unconscious,” he said.
Siddiqui finally sought help from a doctor six years later. “He only prescribed me a medication and said that I am OK,” he said. Since his condition did not improve, Siddiqui went to see another doctor six months ago. “I went for my body and said I can’t sleep and the doctor prescribed me medicine to sleep,” he said. “When the doctor asked why I can’t sleep, I told them what had happened, and I got a tablet and syrup. He referred me to a ‘brain doctor’ but [he] only prescribed me medicine to sleep.”
The scarcity of community-based support, social services, and mental health counseling and the lack of broader mental health promotion and literacy campaigns can exert a high cost on individuals, families, and society.
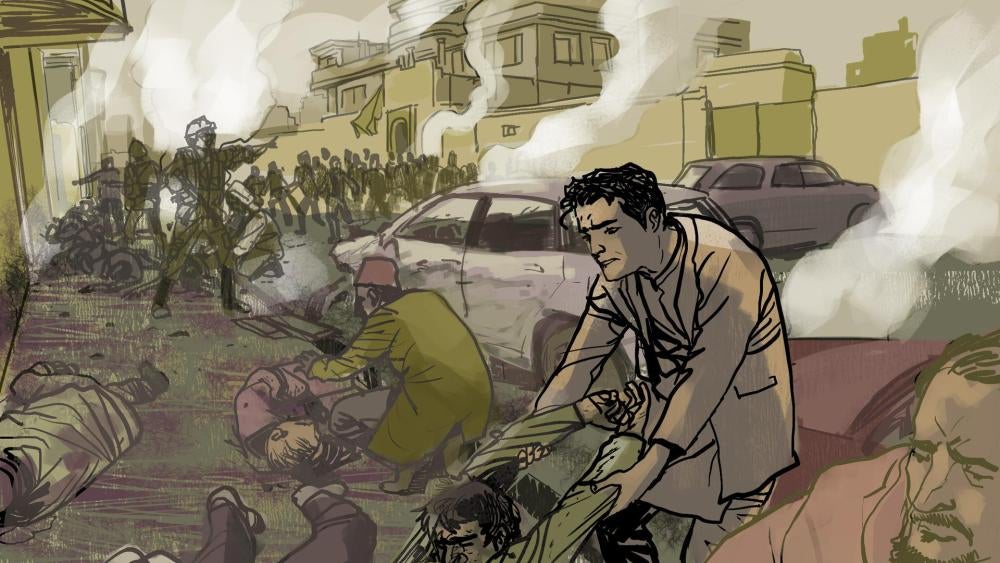
“Farzaneh G.,” 26, said that her life completely changed after her husband, Arash, survived two insurgent attacks in the Dasht-e Barchi neighborhood of Kabul. When he was treated at a hospital, no one asked him about his mental well-being. Shortly thereafter, he began to experience emotional distress and subject his family to outbursts of anger. “In the past, life was good,” Farzaneh said. “Not anymore. I was two months pregnant [when the second attack happened]. When I saw the injured body of my husband, I got shocked and lost the baby two days later.”
Adding to Farzaneh’s despair is her husband’s current psychological state. “Sometimes I feel bad, but I am forcing myself to manage the house and the children since my husband is sick,” she said. “When I get angry or sad or feel pressured, I don’t enter the house because I don’t want him to feel bad. Sometimes, I hit my babies and get in a corner of the room. I cannot breathe, I feel like I am suffocating and just start to cry loudly. If I don’t, it feels like I can’t speak.”
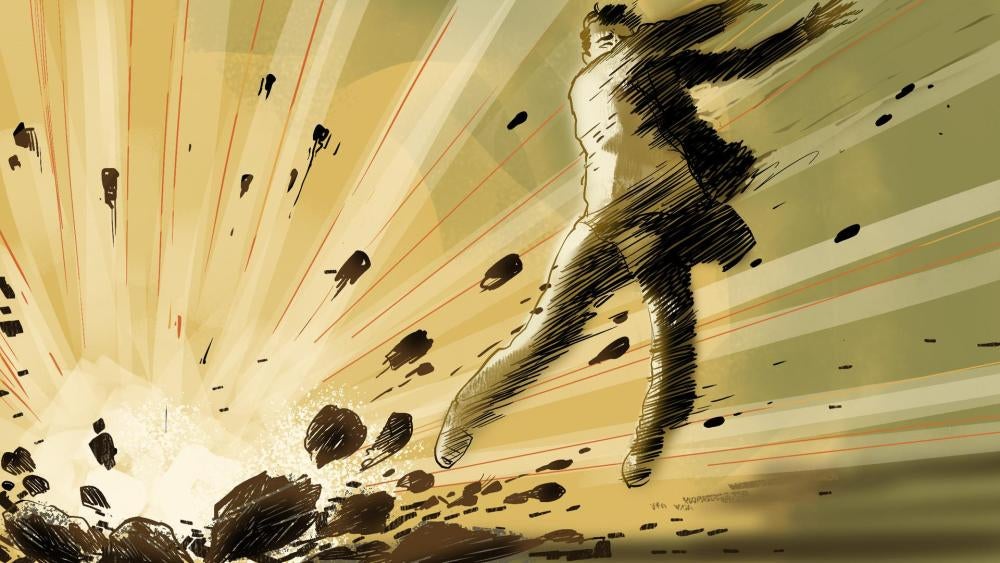
“Amiri K.,” an 18-year-old witness to the August 26, 2017 attack on Imam Zaman mosque and a survivor of the March 7, 2019 attack during a commemoration for an ethnic Hazara leader, Abdul Ali Mazari, killed in 1995 by the Taliban, explained how his experiences affected his life.
The young man, a gymnast, said he saw bodies without feet or a head and streets full of blood when he passed by the Imam Zamam mosque on his way back from training.
Amiri was then shot in the arm during the 2019 Mazari attack and hospitalized at the emergency surgical center for war victims. “Right after the incident, I took a tablet prescribed by the doctors to relax the body and the mind every night for two weeks,” he said, adding that the medication failed to improve his mental health. He said that over less than a month, between March and April 2019, he experienced three “shocks:”
When I get shocked, I remember all that happened and then everything becomes black and I lose consciousness. It usually happens when people talk about the war; the memories just return, and I cannot control it. If I don’t go unconscious by the time they have changed subject, [the memories] just continue. And in Afghanistan, most people talk about the war.
Amiri feels he has little hope for the future. “Misfortunes continue in Afghanistan, and people just continue to suffer in silence,” he said, adding that he has stopped going to school and abandoned gymnastics out of fear of further attacks.
Accounts of people who are receiving mental health services show how a trained psychosocial counselor’s attention can help to alleviate a person’s trauma and mitigate the long-term effects on mental health.
“Mahvash N.,” in her twenties, got psychosocial counseling, but only years after she began experiencing symptoms. As fighting between Afghan government forces and the Taliban intensified in her home province of Faryab after 2013, the United States carried out more airstrikes in the province, some of which hit near Mahvash’s home.
“Planes came and targeted areas outside the village,” she said. “We could hear the bomb and see the lights.” Whenever there was fighting, Mahvash and her children would cower in their house. “We would hide in the rooms and be by the side of a wall.…[T]he children were scared, but not crying, not saying anything. We were afraid to sleep for many nights after that.”
Mahvash’s oldest son, Naqibullah, died during fighting near her house. “The child was scared, and he ran and fell in the well,” she said. Ever since, Mahvash said, she experiences flashbacks: “When I remember this, there is too much burden on my heart. When I see boys the same age [as my son], I get too stressed. If my other children cry, I get angry with them and whatever I have at hand I throw at them.”
In 2018, Mahvash and her surviving children fled the violence and a drought in Faryab for Herat. She joined tens of thousands of internally displaced people living in a camp outside the city.
At the camp, she has been receiving some limited psychological counseling from HealthNet TPO, an international organization contracted by the Public Health Ministry to provide mobile health services. “With the counseling, it helps,” she said. “Now, when I have flashbacks, I go out and consult my heart to remember that everyone passes away.”
Exposure to Violence, Trauma
Afghanistan has been at war since April 1978. The extraordinary level of violence experienced and witnessed by tens of millions of Afghans over three generations has inflicted deep traumatic wounds. Conflict-related trauma can persist and worsen unless those affected have access to psychosocial support.
A World Health Organization review published in June 2019 that examined 129 studies of “mental disorders” in conflict-affected populations found that nearly one-quarter of these populations experienced depression, anxiety, post-traumatic stress, bipolar condition, and schizophrenia. The study, which included Afghanistan, highlighted the “humanitarian imperative to reduce suffering [and] implement scalable mental health interventions to address this burden.”
Conditions in Afghanistan are extreme, and the prevalence of psychosocial and mental health conditions may be higher as a result. Just how many Afghans are affected is difficult to assess, but a 2002 US Centers for Disease Control and Prevention survey in 50 districts with 699 Afghans without disabilities and 100 Afghans with disabilities found that 62 percent had experienced four or more traumatic events over the prior 10 years, including exposure to attacks, loss of relatives, and lack of water and food.
The study found that 68 percent of people without disabilities and 72 percent of people with disabilities reported symptoms of depression. 72 percent of people without disabilities and 85 percent of people with disabilities reported symptoms of anxiety. The prevalence of symptoms of post-traumatic stress was 42 percent in both groups.
A 2005 consultation by the Afghan Independent Human Rights Commission of abuses since the Soviet invasion gives a similar sense of the problem’s proportions:
The atrocities that were committed in Afghanistan are of an enormous scale, and the sense of victimization among the people we spoke to is widespread and profound. Almost everyone had been touched by violence in some way. When we asked 4,151 respondents as part of the survey whether they had been personally affected by violations during the conflict, 69 percent identified themselves or their immediate families as direct victims of a serious human rights violation during the 23-year period.
Another 2005 study found that 67 percent of Afghans reported experiencing the devastating effects of trauma or other psychosocial conditions from the ongoing conflict, with the unemployed, older people, and widowed women particularly affected.
A 2011 report published by the World Bank estimated that half of the Afghan population age 15 or older has experienced depression, anxiety, or post-traumatic stress.
In 2018, Human Rights Watch documented the enduring harm to families and communities from ongoing violence, insecurity, and economic hardship, including serious emotional and psychological trauma, and urged the government and donors to provide them support.
Barriers to Services
Afghans who experience mental health and psychosocial conditions face a variety of hurdles to obtain services. The 2019-2023 National Mental Health Strategy says that fewer than 10 percent of the population are getting the services that are available.
Whether people seek help is influenced by an array of individual, cultural, and structural factors, ranging from poor health literacy to poverty, social exclusion, stigma, gender discrimination, and the ongoing conflict.
Women and girls face notable difficulties since their freedom of movement is often disproportionately affected by insecurity. Gender inequality and discriminatory social norms also create major barriers for women and girls. Their access to health services is often determined by male members of their household and may be conditioned on the availability of segregated services with female staff and segregated infrastructure, such as separate gates and waiting areas.
While a number of international and national groups are providing psychosocial services designed specifically for women and survivors of gender-based violence, the Public Health Ministry has a long way to go in ensuring equal access for women.
According to Public Health Ministry data, as of 2016, only 40 percent of health professionals (doctors, nurses, midwives) were female, 63 percent of them midwives. Because an estimated 87 percent of Afghan women and girls experience some form of abuse in their lifetimes, their mental health needs may be related to or compounded by abuse from the same men who determine whether they can seek services.
Human resources available for mental health programming are also limited. Across Afghanistan, only one psychosocial counselor is available for every 46,000 people, according to Afghanistan’s National Strategy for Mental Health for 2019-2023. Their ability to conduct successful therapy is affected by their lack of experience and limited training.
The WHO says the country has roughly only one psychiatrist for every 435,000 people and one psychologist for every 333,000 people. Only 200 beds are available in public mental health facilities, or one for every 172,500 Afghans.
As a result, few Afghans who describe experiencing the psychological impact of the conflict will seek professional mental health services. A 2018 EU-commissioned nationwide mental health survey found that 88 percent of the total respondents, half of whom had experienced psychosocial distress, never sought mental health assistance. Of the 12 percent who sought assistance, 47 percent said they consulted a doctor, 36 percent went to see community health workers, and 17 consulted an imam (prayer leader in a mosque).
There is heavy reliance on community health workers or volunteer community members, usually a married couple trained to provide limited health services at the community level, especially in areas where doctors are not nearby. The 2019-2023 Mental Health Strategy states that fewer than half of them are trained to provide psychological first aid. Similarly, religious figures are often ill-equipped to appropriately assist people experiencing psychosocial distress and sometimes contribute to disseminating stigmatizing beliefs, such as the notion that people with mental health conditions are possessed by evil spirits.
Six of the people interviewed came from rural areas and had been displaced to urban centers as a result of the conflict or environmental disasters. Most described struggling to get services in their home areas because of the insecurity, absence of nearby health facilities, and the costs, including travel expenses, medication, or private doctor fees. The government has abolished service fees, but the Public Health Ministry estimates in its 2016-2020 National Health Strategy that up to 74 percent of health expenditure consists of out-of-pocket expenses and that the delivery of health services is made worse by “persistent corruption.”
The Afghan mental health system remains largely hospital-based and struggles to meet the demand, particularly outside of urban centers. WHO estimates that to meet the health-related UN Sustainable Development Goals in low-income countries such as Afghanistan, a minimum of 23 health professionals – doctors, midwives, nurses – are needed per 10,000 habitants. But, according to 2016 Public Health Ministry figures, there were only 4.98 professional health workers per 10,000 habitants, with WHO figures showing that the number of physicians is as low as 0.6 per 10,000 habitants in rural areas, in comparison to 7.2 in urban ones.
“Firouzeh G.,” who was married at 15 and is now 20, was 17 when her husband departed their home province of Badghis for Iran, leaving her to care for their two children in a war zone. “He left for work,” she said. “He didn’t tell me anything, about how long he would go. He said, ‘I’m leaving and if I’m not captured, I’ll be back.’ My heart sank.”
Shortly before her husband left, fighting had increased in her district, which has experienced intense fighting between the Taliban and US-backed Afghan forces since 2016. Firouzeh said that Taliban fighters began to pressure wealthier villagers to support them and executed those who refused. “Once, we also witnessed an airstrike near the village,” she said. “It was a heavy strike and it was very close. It killed animals and there were body parts everywhere.”
Eventually, Firouzeh learned that her husband had been jailed in Iran and would not return. “That night, all night, I was just going in and out of the house,” she said. “I couldn’t control myself. I woke up in the morning and I would be in distress.” Firouzeh said there were no doctors in her area. “There were no doctors close because of the fighting, so [the community] brought me garlic and ice to feel better.” But the garlic and ice did not help. “When I would think about him, I would become impatient, my heart was heavy, and I became unconscious,” she said. “It happened once a day, at least. Sometimes up to five times.”
Firouzeh fled with her children to an internally displaced persons camp near Herat, where she receives psychosocial counseling from volunteers for HealthNet TPO.
International Legal Standards
Afghanistan is a party to the International Covenant on Economic, Social and Cultural Rights, which in article 12 obligates governments to recognize “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health,” and requires governments to ensure that health care – including mental health services – based on informed consent and to make them progressively more available, accessible, acceptable, and of good quality.
Non-state armed groups such as the Taliban that exert effective control over areas of the country are not legally bound by the covenant but should respect the right to the highest attainable standard of health.
Afghanistan is also a party to the Convention on the Rights of Persons with Disabilities and its Optional Protocol. The convention states that governments should provide health services “as close as possible to people’s own communities, including in rural areas,” and provide for “early identification and intervention as appropriate, and services designed to minimize and prevent further disabilities.” It also states that governments should take “all necessary measures to ensure the protection and safety of persons with disabilities in situations of risk, including situations of armed conflict [and] humanitarian emergencies.”
Under international humanitarian law, or the laws of war, applicable to the conflict in Afghanistan, all parties to the conflict must use their best efforts to provide protection and care for the wounded and sick, which extends to mental well-being. The Second Additional Protocol to the Geneva Conventions of 1977 states that all wounded and sick people “shall receive, to the fullest extent practicable and with the least possible delay, the medical care and attention required by their condition” from the parties to the conflict. This includes “civilians, who, because of trauma, disease or other physical or mental disorder or disability, are in need of medical assistance.” Parties are also obligated to facilitate aid organizations to provide for the civilian population’s protection and care.
As a growing body of military and civilian studies demonstrates the pervasive psychological impacts of sustained exposure to conflict, medical attention to victims of conflict-related violence should include attention to their short and long-term psychological well-being.
The voices and needs of people with disabilities, including people with mental health conditions, have largely been absent from many countries’ peace and security agendas. On June 29, 2019, the United Nations Security Council adopted Resolution 2475, meant to protect people with disabilities in conflict, urging governments “to enable [their] meaningful participation and representation…in humanitarian action, conflict prevention, resolution, reconciliation, reconstruction and peacebuilding.”
Recommendations
The government of Afghanistan, with assistance from international donors, should expand and promote mental health services and psychosocial support for people who have experienced traumatic events related to the conflict. The following recommendations offer ways for the Afghan government and donors to provide timely and ongoing psychosocial support to survivors of attacks and other conflict-related trauma.
The Afghan Ministry of Public Health should:
Seek to increase the number of psychosocial counselors and trained health workers (community health workers, nurses, midwives, doctors), especially women, who can educate their communities and patients about mental health, perform psychological first aid, provide limited forms of psychosocial counseling, and ensure proper referral to mental health professionals (psychologists, psychiatrists, neurologists) if requested by the patient or as appropriate. Training should be offered in rural areas and those recruited should have adequate working conditions and other incentives to promote retention.
Establish monitorable and robust referral systems so that emergency, women’s, and other health departments can request and obtain appropriate mental health support for patients.
Set sufficient standards in the attribution of health service delivery contracts to aid agencies and other organizations to ensure that they deliver appropriate, timely, and culturally sensitive and consent-based mental health services.
Instruct health care providers and existing mental health professionals to offer available government-funded psychological first aid to survivors of conflict-related events free of cost.
Design and provide mental health services specifically targeted to help women and girls.
Take all necessary measures to ensure the availability and continuity of mental health services in areas controlled by the Taliban.
Increase outreach to the public about mental health and available services, such as through radio, television, and community events. Efforts should focus on groups who are less likely to access mental health services, including women and girls, and rural populations.
Investigate corrupt practices, such as charging patients at public hospitals for free services, both within the Public Health Ministry and by other health providers that hinder access to mental health services.
Consider raising with mullahs and other religious figures, in coordination with the Religious Affairs Ministry, the importance of referrals to appropriate services and support.
International donors to Afghanistan should:
Provide technical assistance to the Public Health Ministry to ensure more efficient appropriation of resources to help address budgetary under-investment in mental health services. These efforts should address the disparities in mental health services between rural and urban areas through less expensive community-based psychosocial services, such as increasing psychosocial first aid by community health workers and midwives and the expanded use of mobile clinics.
Assist the Public Health Ministry to provide remote mental health education and confidential psychosocial counseling by phone, possibly by strengthening and expanding services by the free “6464 Family Support Hotline.”
Support government efforts to develop mental health services that target underserved women and girls.
Support Public Health Ministry efforts to increase the number and professionalism of psychosocial counselors and trained health workers (community health workers, nurses, midwives, doctors) who can educate their communities and clients about mental health, perform psychological first aid, provide basic psychosocial counseling, and provide referrals as appropriate to mental health professionals (psychologists, psychiatrists, neurologists). The ministry should give priority to developing and retaining trained staff in rural and conflict-affected areas through better working conditions and job incentives.
Parties to the conflict should:
Cease all intentional attacks on civilians, attacks that do not or cannot discriminate between civilians and combatants, and attacks that are likely to cause disproportionate civilian harm.
Protect the right to health to all civilians living in areas under control, facilitate humanitarian access to populations in need, including for the provision of mental health support, and cease all attacks on medical infrastructure and personnel.






![In a separate interview, Arash’s wife, “Mozhdah,” 26, said the attacks changed her life completely: “In the past, life was good,” she said. “Not anymore. I was pregnant for two months [when the second attack happened].](/sites/default/files/styles/image_gallery/public/multimedia_images_2019/201910eme_afghanistan_mentalhealth_illustration7.jpg?itok=GerVV5qq)