Summary
This woman shouted for ‘Kevin’ to come to the desk. I shrunk in my seat, hoping she would see the note on the chart about my gender change. But she just kept yelling for Kevin. I finally had to get up and cross the room in a walk of shame. Will I ever go back there? No way.
– Connie, 31, Miami, Florida
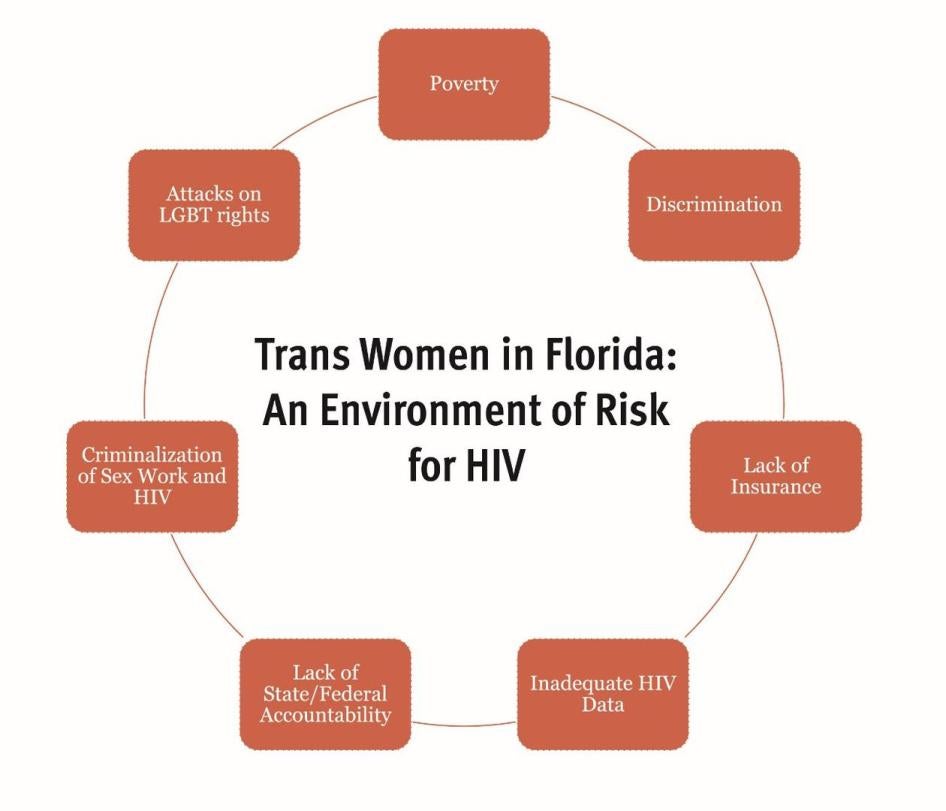
Connie is HIV-positive, one of many transgender women in Florida facing the challenge of finding health care that is safe, gender-affirming, and affordable. The 1.4 million transgender and gender-non-conforming people in the United States generally face multiple barriers, from family rejection to non-acceptance and abuse at school, and pervasive discrimination in employment, housing, and health care. Social and economic marginalization as a result of these factors lead to higher rates of suicide, poverty, violence, and incarceration, particularly for trans people of color. This is a severe and compound environment of risk for HIV that demands a robust response – one that the state of Florida, and the federal government, are failing to deliver.
Nationally, rates of HIV are declining as treatment becomes more effective and, if administered regularly, can eliminate the potential for transmission of the virus. Rates of HIV among transgender men appear to be low, though more study is needed. But among transgender women, rates of new HIV infection have remained at crisis levels for more than a decade. One of four trans women, and more than half of African-American trans women are living with HIV, rates that are far higher than the overall prevalence of HIV in the US of less than one percent. Transgender women are testing positive for HIV at rates higher than cisgender men or women, and racial disparities are stark: HIV prevalence is more than three times higher among African-American transgender women than their white or Latina counterparts.
Since 2010, the National HIV/AIDS Strategy has recognized trans women as a “key” population whose needs must be addressed. Trans people frequently experience disrespect, harassment, and denial of care in health care settings, and many avoid seeking health care as a result. HIV policymakers know what to do: ample evidence indicates that to be effective, health care services for trans individuals must be affordable, gender-affirming, and should be integrated with transition-related care. This is particularly important for HIV care. If forced to choose, trans women will frequently prioritize Hormone Replacement Therapy (HRT) over HIV care, making it essential to combine these services in a “one-stop shop.”
Numerous pilot programs across the country have demonstrated that providing integrated HIV care that engages and respects trans women is feasible and successful in reducing HIV risk and improving health outcomes. But this investigation of HIV prevention and care for trans women in south Florida found that trans women are navigating a difficult landscape that state and federal authorities have not done nearly enough to address. Services are fragmented, integrated care is limited, and cost and lack of insurance leave medical and mental health care out of reach. To the extent that such services exist, they are more a result of community demand and local advocacy efforts rather than federal or state policy, which contain no targeted requirements or standards to ensure that trans women are receiving the services they need.
The problem is not money. As a state with one of the country’s highest rates of HIV infection, Florida receives hundreds of millions of dollars from the Ryan White program, the federal government’s primary vehicle for funding HIV prevention and treatment services. The state HIV budget has increased more than 15 percent in the last three years. Nationwide and in Florida, more than half of people living with HIV receive care through a Ryan White funded program. Ryan White services are important for transgender women – when they stay in treatment in Ryan White programs, their health outcomes are significantly better than when they do not.
Despite a wide network of public and private providers in the metropolitan areas of Miami and Fort Lauderdale, only a handful of HIV clinics are consistently identified as providing what is recognized best practice, and to some experts, the standard of care, for transgender women. State HIV officials told Human Rights Watch that all Ryan White funded clinics “welcome” trans patients, but there was no systemic monitoring of the issue to determine whether this is the case, and evidence from the ground suggests otherwise. In fact, Human Rights Watch found that many transgender women experienced disrespect, harassment, and denial of services in health care settings, and that such experiences often result in avoidance of health care altogether.
The Ryan White program covers medications for patients under the AIDS Drug Assistance Program (ADAP). The federal government sets core criteria, but states can also cover medications for needs and conditions related to HIV, such as mental health and hepatitis C medications. In 21 states, ADAP covers hormone replacement medications for the purpose of gender transition – an important part of ensuring that HIV care meets the health needs of transgender women. Florida is not one of these states, and federal policy does not require it to do so.
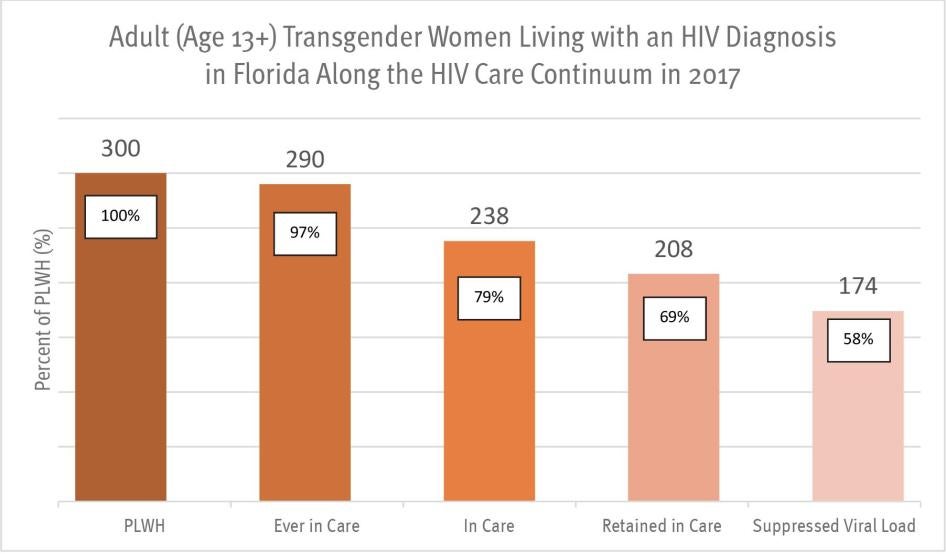
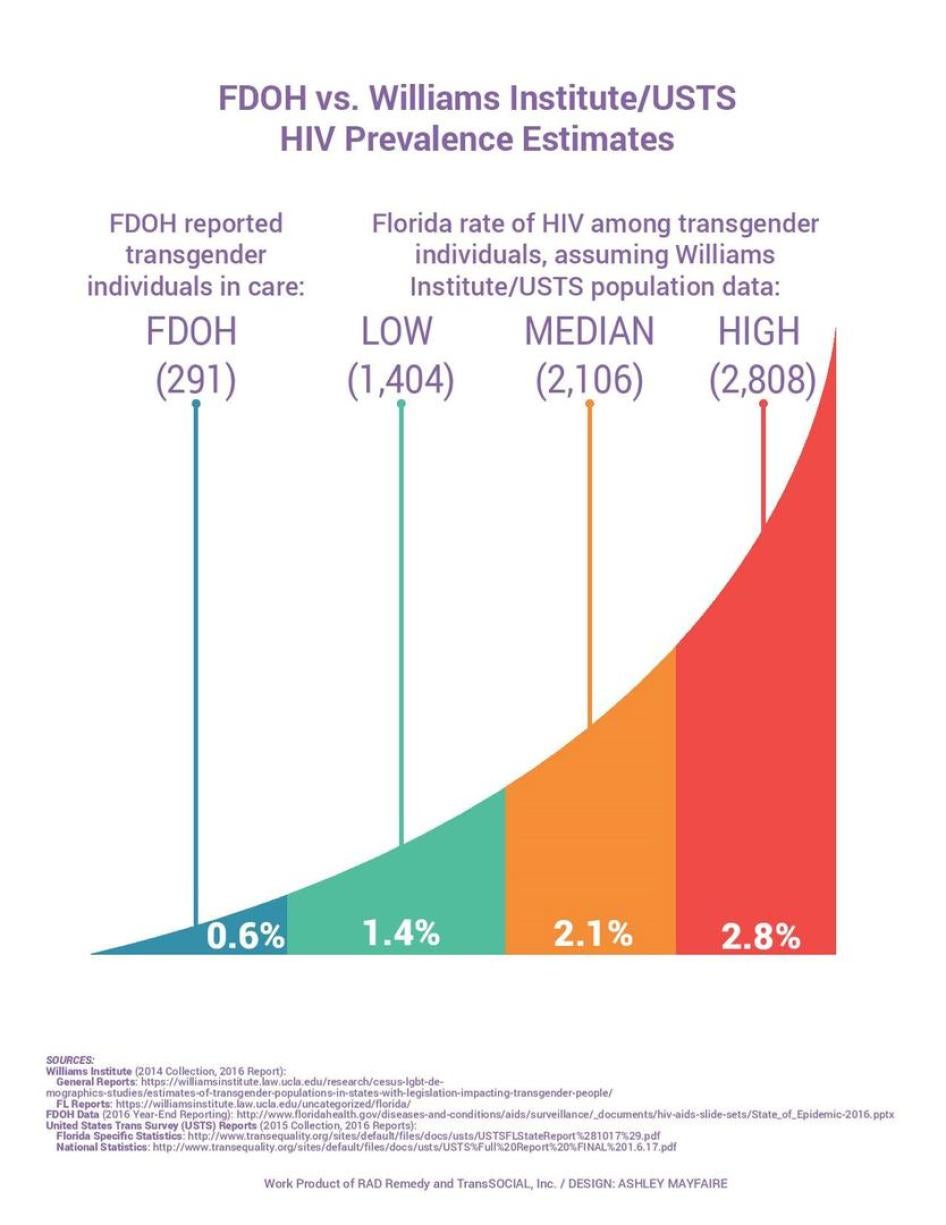
Underlying this lack of targeted government policy is the lack of accurate information about HIV risk and infection among trans women in Florida. The failure to collect accurate or complete HIV data among trans people is an ongoing problem. Decades into the epidemic, neither the state nor the federal government know how many trans women are living with HIV. Most states, including Florida, have only partially implemented federal recommendations for how to improve data collection for HIV among trans populations, and though Florida’s data on trans women is improving, they remain incomplete. Estimates developed from other experts indicate that the number of transgender people living with HIV in Florida may be five to ten times higher than reported by the state.
Given that government response is driven by data, the undercounting of HIV prevalence means trans women are left out of many federal and state programs intended to monitor or improve HIV services. Often perceived by policymakers as a population too small to help, conditions for trans women on the ground remain unknown, unchanged, or inadequate. Over thirty years into the epidemic, the stark reality is that trans women are at an extremely high risk of HIV, but as a distinct population remain largely invisible to the federal and state HIV surveillance and monitoring systems that guide government response.
For this report, Human Rights Watch investigated access to health care, including HIV prevention and treatment, for women of trans experience in south Florida. We administered 125 survey questionnaires among trans women in Miami-Dade and Broward counties, two counties with the highest rates of new HIV infections in the country. These questionnaires, and the more than 100 interviews with trans women, their advocates, and HIV service providers indicated that many trans women in south Florida, particularly women of color, experience high HIV risk as a result of multiple factors, with poverty and lack of health insurance standing out as primary vulnerabilities. More than 63 percent of survey participants reported income of less than $10,000 per year, more than half were unemployed, and one of three were in “unstable” housing situations. This data is consistent with national surveys showing that many trans people live in extreme poverty and are three times more likely to be unemployed than those in the general population.
Nearly half of survey participants – 45 percent – had no health insurance. This alarming reality is tied to Florida’s refusal to expand its Medicaid program under the Affordable Care Act, a decision that has left hundreds of thousands of low income and working Floridians without access to health insurance. It is a decision that has a severe impact on transgender women, who are among the most impoverished residents of the state. Medicaid expansion could dramatically improve access to health care for trans individuals, many of whom would be included in its coverage of adults without dependents. Access to Medicaid could increase options for trans women as they attempt to locate gender-affirming health care in their community, providing vital access to HIV prevention and treatment.
Nationally, one of five trans women has been incarcerated, with African-American trans women three times more likely to face arrest than their white counterparts. Many trans women often turn to sex work in order to survive, leaving them vulnerable to police abuse and criminal charges that can begin, and perpetuate, a cycle of unemployment and lack of income. In the Human Rights Watch survey, more than half of respondents said they had been arrested at least once. Involvement in the criminal justice system increases HIV risk – even short jail stays have been shown to have negative health outcomes. Jails and prisons are also dangerous places for trans women, who report alarming rates of sexual assault in detention.
As trans women in Florida and throughout the US are struggling to access HIV prevention and care, the Trump administration has pressed forward with policies that will erode key LGBT rights protections and erect new barriers to their enjoyment of the right to health. The right to health does not guarantee to everyone a right to be healthy. Rather, its realization requires governments to implement policies that promote access to health care without discrimination, with particular attention to those facing the most barriers to care – low income persons, women, minorities, people with disabilities, and others.
Since Inauguration Day 2017, President Trump has moved in the opposite direction with a policy agenda that has sought repeal of the Affordable Care Act, restrictions on Medicaid access, and the rollback of regulations that protect LGBT Americans from discrimination. The rights of trans people are specifically threatened, with attempts to ban trans soldiers from the military, eliminate protections in federal law and policy that protect trans people from discrimination in employment and health care on the basis of gender identity, and weaken protections for transgender federal prisoners. For trans women, who face pervasive discrimination in employment and health care settings, the rollback of existing protections could have a particularly devastating impact.
In this increasingly hostile environment, trans women are in greater danger than ever and in greater need of federal and state support. For health officials, few questions remain about what to do to reduce HIV infection among trans women. But without commitment by both federal and state policymakers to take these steps and remain accountable for doing so, the lives and health of trans women will remain at risk, and the crisis will continue.
Recommendations
To the President of the United States:
- Re-establish federal leadership addressing the HIV epidemic in the United States, including appointment of a director and staff for the Office of National HIV/AIDS Strategy and making appointments to the President’s Advisory Council on HIV/AIDS comprised of public health experts, community leaders, and representatives of groups most heavily impacted by HIV, including trans women.
- Withdraw the executive order issued October 12, 2017 that permits unregulated health insurance plans inconsistent with the requirements of the Affordable Care Act.
- Withdraw the executive order issued May 4, 2017 instructing the Department of Health and Human Services to amend regulations for conscience-based objections to preventive care provisions of the Affordable Care Act.
To the Department of Health and Human Services:
- Protect and support expansion of the Medicaid program to ensure access to health care for low income people. Withdraw support for state waiver provisions that would reduce access to health services.
- Either defend the interpretation of section 1557 of the Affordable Care Act to protect against discrimination on the basis of gender identity, or introduce new legislation codifying those same protections.
- To the Health Resources and Services Administration (HRSA):
- Implement policy regulations and guidance to states ensuring the protection of LGBT individuals from discrimination in insurance coverage. This includes the revision of Medicaid regulations to address denials on the basis of perceived gender incongruity.
- Establish policies, monitoring, and evaluation procedures to promote gender-affirming care, including hormone replacement therapy, in all sites receiving Ryan White program funds, and support coverage of hormone replacement therapy in the AIDS Drug Assistance Program.
To the Centers for Disease Control and Prevention:
- Conduct a systematic review of implementation of the CDC Guidance for Working with Transgender HIV Data to ensure that states are taking effective steps to implement the Guidance and improve HIV data collection for trans communities.
- Identify states in need of technical assistance and prioritize provision of services accordingly.
- Report on steps taken and progress toward development of a national “indicator” for data collection on HIV among transgender communities as set forth in the National HIV/AIDS Strategy Update for 2020.
To the US Bureau of Prisons:
- Withdraw revisions to the Bureau of Prisons Transgender Offender Manual that weaken protections for transgender prisoners.
- Ensure that all regulations comply with Prison Rape Elimination Act requirements in order to reduce sexual assault in detention.
To the Congress of the United States:
- Stop attempts to repeal or further dismantle the Affordable Care Act without an adequate replacement.
- Support expansion of the Medicaid program to ensure access to health care for low income people.
- Pass legislation protecting LGBT persons from discrimination in health care, employment, and public accommodation.
- To the Senate: ratify the International Covenant on Economic, Social, and Cultural Rights.
To the State of Florida:
- To the Governor of the State of Florida:
- Expand Medicaid under the Affordable Care Act to ensure access to health care for low income people including adults living in poverty with no dependents, and to reduce poverty in the state.
- To the Florida State Legislature:
- Repeal HIV-specific criminalization laws.
- Support criminal justice reform including alternatives to incarceration and decriminalization of consensual, adult sex work.
- To the Department of Health:
- Issue a public report on progress to date and timelines for implementation of CDC Guidance for Working with Transgender HIV Data.
- Establish policies, procedures, and monitoring systems to ensure that gender-affirming care is integrated with HIV care and services in all health care settings, including all sites receiving Ryan White funds.
- Participate in the federal ECHO program to evaluate and improve the quality of HIV services for transgender people.
- Ensure coverage for hormone replacement therapy in the AIDS Drug Assistance Program in all geographic areas and increase awareness of its availability.
- To the Office of Health Care Administration:
- Develop explicit policy ensuring Medicaid coverage for transgender health care.
Methodology
This report is based on research conducted between June 2017 and June 2018 in the south Florida counties of Miami-Dade and Broward. Human Rights Watch utilized a mixed-method approach that combined quantitative survey and qualitative interviews and legal and policy analysis. The research focuses on access to health care, including HIV prevention, for individuals who self-identified as women of trans experience – a term that was intended to reflect a variety of experiences and expressions – and that was left to the individual to define.
In addition to basic demographic information, the questions emphasized access to health care, including HIV care, access to HIV prevention, and interaction with the criminal justice system. Human Rights Watch identified respondents primarily through organizations providing social services to transgender people in the two counties and through the personal networks of peer interviewers. This approach produced a diverse group of respondents but should not be considered a representative sample of trans individuals in these counties, as survey participants were likely to be connected to health and HIV services.
For the quantitative component of the research, Human Rights Watch trained 15 peer interviewers in the administration of a survey, human rights documentation, and research ethics, including the importance of informed consent and confidentiality. Peer interviewers were diverse in age, gender identification, and ethnicity and were selected on the recommendation of, and in some cases were themselves representatives of, organizations providing services for transgender people in Miami-Dade and Broward counties. Of 125 questionnaires, 81 were administered by peer interviewers and 44 were administered directly by Human Rights Watch.
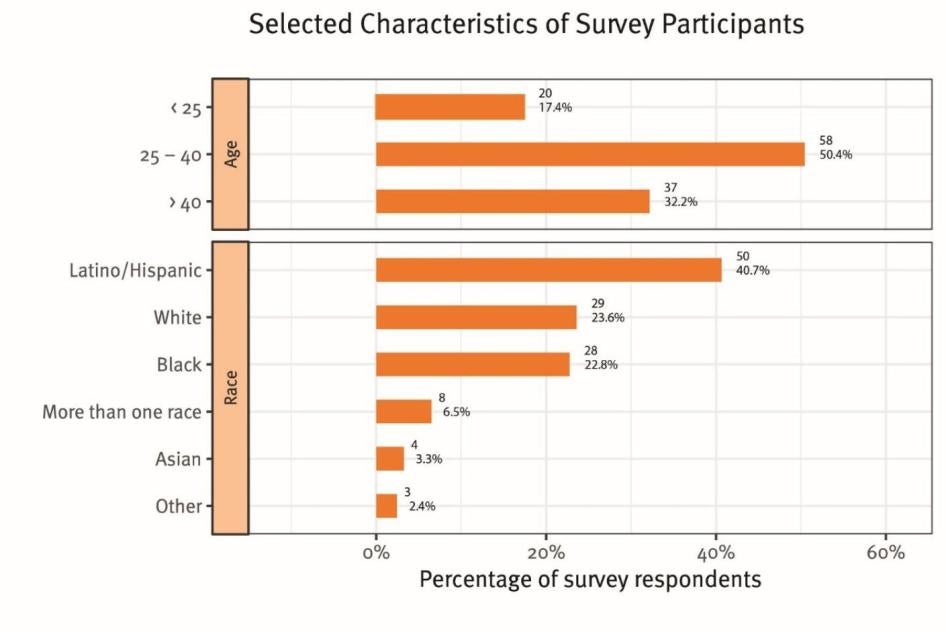
Survey participants were all Florida residents in Miami-Dade or Broward Counties who self-identified as women of trans experience; the survey tool made no inquiry into the definition of that term. The responses to the survey’s demographic options showed that 41 percent identified as Latina/Hispanic, 24 percent as White/Caucasian, 23 percent as Black/African-American, 4 percent as Asian and 7 percent as other or as “more than one race;” ages reported ranged between 19 and 70 (see Graph I).[1]
Peer interviewers were paid a nominal stipend for their training time and administration of the survey. Gift cards were provided to interviewees to reimburse them for travel and related expenses.
All participants were informed of the purpose of the survey, its voluntary nature, and the ways in which the information would be used. All participants provided oral consent to be interviewed and consent was noted on each survey form. Participants were assured Human Rights Watch would not publish their names; all names of survey participants reported are pseudonyms. Survey results were tabulated and analyzed by Human Rights Watch.
Human Rights Watch also interviewed more than 100 advocates, health care providers, public defenders, sheriff and jail officials, members of state HIV planning councils, federal health and criminal justice officials, and national experts on transgender health. The Florida Department of Health HIV/AIDS Section responded to written questions in writing and responded on behalf of Miami-Dade and Broward County departments of health; Broward County Department of Health officials also met with Human Rights Watch in person. Documents were obtained from the Florida Department of Health, Broward County Department of Health, Broward County Sheriff’s Office, and Hollywood, Florida Police Department. All documents cited are publicly available or on file with Human Rights Watch. Pseudonyms are used for anyone not interviewed in their official capacity to protect privacy and confidentiality.
Background
Discrimination, Abuse, and Health Risks Among Transgender People
In the United States, an estimated 1.4 million people (0.6 percent of the population) identify as transgender. Transgender or “trans” is an umbrella term intended to be inclusive of the full range of nuance and diversity of gender expression and identity among those who may not identify with the sex they were assigned at birth.[2] Trans women were assigned male sex at birth but identify as women; trans men were assigned female sex at birth but identify as men.
Trans and gender-non-conforming people tend to face barriers in multiple aspects of life, from family rejection to non-acceptance and abuse at school, and pervasive discrimination in employment, housing and health care. Social and economic marginalization as a result of these factors are linked to higher rates of suicide, poverty, and incarceration, particularly for trans people of color. According to a survey conducted in 2015 by the National Center for Transgender Equality (NCTE), trans people were more than twice as likely as the US population as a whole to live in poverty and three times as likely to be unemployed.[3] A staggering 40 percent of respondents had attempted suicide, compared to 1.6 percent in the US population.[4] Violence was a fact of everyday life, with nearly half reporting having been sexually assaulted at one point and one in ten reporting sexual assault within the last year.[5]
In the national survey, African-American and Latino/a trans respondents fared worse than their white counterparts nearly across the board, reporting lower income, less access to health care and health insurance, as well as higher rates of homelessness, employment discrimination, and incarceration.[6] Trans people of color were more likely than white trans people to report abuse by the police as well as victimization while in jail or prison.[7] This is consistent with data collected under the federal Prison Rape Elimination Act indicating that African-American and Latina trans women report sexual assault in detention at higher rates than white women.[8] Violence and hate crimes against trans people have increased in recent years, though accurate data is hindered by lack of reporting and misinformation regarding the gender identity of victims.[9] FBI data show that reported hate crimes against trans people increased by 44 percent between 2015 and 2016.[10] At least 21 trans individuals, mostly women of color, have been killed in 2018, five of them in Florida.[11]
Barriers to Health Care and Services
Trans people in the US face both socio-economic barriers and discrimination in access to health care and services. Trans people are less likely than the general population to have health insurance and more likely to rely on publicly funded insurance than private or employer-provided coverage.[12] The 2015 US Transgender Survey indicated that one of three trans people had needed to see a doctor in the last year but could not afford to do so.[13] Trans people face outright denial of services as well as harassment in health care settings. A 2017 national survey by the Center for American Progress found that one in three trans respondents said that they had been turned away by a medical provider on the basis of their gender identity; one in five reported being subject to harsh or abusive language in a health care setting; and one in three reported unwanted physical or sexual contact by a medical provider.[14] A common response to these conditions is avoidance of health care altogether – one national survey found that one in four trans people stopped seeking health care as a result of bad experiences in health care settings.[15]
Health Care for Transgender People
As do all people, transgender individuals have diverse physical and mental health concerns, some that are related to their trans experience and some that are not. Standards of care for medical and mental health providers to treat transgender patients have evolved significantly in the last decade. The World Professional Association for Transgender Health (WPATH) takes care to distinguish gender non-conformity from the clinical diagnosis of gender dysphoria.[16] According to WPATH and the American Psychiatric Association, there is nothing inherently pathological about gender non-conformity; gender dysphoria is a mental health condition in which one is experiencing clinically significant distress or social/occupational impairment as a result of gender non-conformity.[17] This diagnosis remains controversial as it is perceived as stigmatizing and pathologizes distress which, in the view of many, originates largely from societal prejudice and discrimination.[18] However, the diagnosis remains relevant as a basis for medical and surgical interventions for transgender and gender non-conforming people who wish to pursue them, and in many cases, as a prerequisite for insurance coverage for these treatments.[19]
One principle that is widely accepted is that effective health care for trans people should be respectful, safe, and culturally appropriate – a large number of health experts, provider organizations, and transgender advocates have published detailed guidelines on how to provide “gender-affirming” services in health care settings.[20] Recommendations for best practices not only include clinical standards for care but emphasize the importance of respectful and knowledgeable staff interaction with patients – use of gender-affirming pronouns, avoiding assumptions about gender identity or expression, recognizing that a patient’s official identity documents may not match their gender expression, and other considerations.[21] Underpinning these practices is a recognition of the evidence that failure to implement gender-affirming services will result in avoidance of health care for transgender patients. As stated by the University of California at San Francisco Center for Excellence in Transgender Health Care (CETH), “Providing a safe, welcoming, and culturally appropriate clinic environment is essential to ensure that transgender people not only seek care but return for follow up.”[22]
An example of the importance of gender-affirming policies in health settings is provided by Connie, a 31-year-old trans woman living in Miami, Florida. Connie’s driver’s license does not yet reflect her transition to female, so in her first visit to a local health clinic she asked them to note her current name and gender identity on the chart. However, on her second visit she was in the waiting room with other patients, and she heard her birth name called out loudly to summon her to the reception desk. Connie recalled:
This woman shouted for ‘Kevin’ to come to the desk. I shrunk in my seat, hoping she would see the note on the chart about my gender change. But she just kept yelling for Kevin. I finally had to get up and cross the room in a walk of shame. Will I ever go back there? No way.[23]
Transgender Women and HIV
Data are scarce and incomplete but alarming — both globally and domestically, trans women are heavily burdened by the HIV epidemic. According to the World Health Organization (WHO), existing studies show that nearly one of five transgender women around the world are living with HIV – this is a prevalence rate of 19 percent, compared to a rate of 0.8 percent in the general global adult population.[24] Globally, transgender women are 49 times more likely to acquire HIV during their lifetime than the general population of reproductive age.[25] HIV prevalence among trans men appears to be much lower, but data remain limited and more research is needed (see text box). WHO and UNAIDS, the leading international agencies charged with addressing the HIV epidemic worldwide, have designated transgender women as a “key population” along with men who have sex with men, prisoners, people who inject drugs, and sex workers. Because HIV among people within these groups (and their intimate partners) account for 40-50 percent of the global HIV epidemic, WHO and UNAIDS have declared that “without addressing the needs of key populations, a sustainable response to HIV will not be achieved.”[26]
In the United States, the National HIV/AIDS Strategy also designates transgender women as a “high-risk” and “key” population as studies indicate an HIV prevalence ranging from 22 percent to as high as 56 percent among transgender women of color.[27] This is grossly disproportionate to the overall prevalence of HIV in the US, which is under one percent.[28] In a recent survey of nine million HIV tests nationwide, transgender women had the highest percentage of positive results of any gender category.[29] Racial disparities are stark: HIV prevalence is more than three times higher among African-American transgender women than their white or Latina counterparts.[30]
HIV in the United States
More than 1.1 million people in the US are living with HIV, and one in seven are unaware of their infection.[31] Over the past decade, the number of people living with HIV has increased as treatment has become more effective. For the first time in the history of the epidemic, the number of new infections has begun to decrease overall, but still remains high among specific populations.[32]
In recent years, treatment has become the cornerstone of both HIV prevention and care. Public health and HIV experts have increasingly emphasized the importance of early and universal access to anti-retroviral medication not only to improve individual outcomes, but to reduce the risk of transmission to others. The approach characterized as “Treatment as Prevention” has gained traction globally and in the US as research confirms that sufficient suppression of the virus through anti-retroviral therapy can effectively eliminate the risk of transmission from one person to another and in communities as a whole.[33] Key to the success of this approach is the ability of the person to become aware of their status and to sustain a lifetime course of anti-retroviral medication that must be taken on a daily basis.[34]
Increased access to treatment has reduced new infections nationwide, but rates of infection remain high among certain groups, including gay, bisexual, or other men who have sex with men; African-American men and women; Latino men and women; people who inject drugs; youth 13-24 years old; people in the southern United States; and transgender women.[35]
Race and Poverty
Many factors combine to place trans women, and particularly women of color, at high risk of HIV. In the United States, HIV has become a disease of social, economic, and racial exclusion. Trans women are disproportionately impacted by many of these forces of marginalization, facing what has been characterized by HIV experts as “multiple, concurrent HIV risks and underlying vulnerabilities.”[36]
In the US HIV epidemic, racial disparities are extreme, with African-Americans comprising 12 percent of the US population, but 44 percent of new HIV infections. Though new infections have decreased among Americans overall, they continue to increase among African-Americans.[37] Indeed, African-Americans comprise the highest percentage of people living with HIV, people becoming newly infected, and people living with AIDS.[38]
African-American people in the US are more likely to be poor than white people, and poverty is one of the primary drivers of the HIV epidemic.[39] In contrast to sub-Saharan Africa’s HIV epidemic affecting the entire population, HIV in the United States is concentrated in impoverished urban areas and small towns, with the highest concentration of people living with HIV and new HIV infections occurring in the US South.[40] In some impoverished areas of the US, HIV prevalence has been found to be higher than in many African countries where the HIV epidemic is severe.[41]
As noted above, many transgender people live in poverty – the 2015 US Transgender Survey indicated that nearly one in three had an income of less than $10,000 per year, with 55 percent living on less than $25,000 per year.[42] In their 2015 report, “Paying an Unfair Price: Financial Penalties for Being Transgender in America,” the Center for American Progress found that discrimination in school, employment, housing and health care, as well as an inability to obtain gender-affirming identity documentation, combined to force many transgender people into poverty and into underground economies such as sex work for daily survival.[43]
Sex Work and Incarceration
People who exchange sex for money or life necessities are at increased risk for HIV, a risk that impacts some trans women who engage in sex work. This risk results from not only a higher number of sexual partners but, in many cases, from environmental factors such as poverty, homelessness, and substance use – all factors that have been independently associated with HIV risk and poor health outcomes.[44] In addition, Human Rights Watch and others have documented increased HIV risk to sex workers from the harmful consequences of criminalization: police harassment, arrest, and incarceration have been found to be associated with higher HIV risk, less access to medical care, and impaired ability to manage HIV medications.[45] A criminal history after conviction on prostitution charges creates a significant barrier to employment that perpetuates poverty and the necessity of sex work in order to meet one’s basic needs.
Trans women experience high rates of incarceration, with one in five trans women reporting having been in jail or prison.[46] The rate of incarceration for African-American trans women is three times as high as it is for white trans women – some studies indicate that half of African-American trans women report a history of incarceration.[47] Incarceration creates numerous barriers to HIV prevention and care – condoms are not available in the majority of prisons and jails in the United States; access to HIV medications and treatment is often inadequate or in many jails, non-existent; and linkage to medical care upon re-entry is uneven at best.[48]
In addition to incarceration itself as an HIV risk factor, transgender women experience alarming rates of sexual assault in prison. According to federal Prison Rape Elimination Act data for 2015, more than one-third of incarcerated trans women reported assault by other prisoners or staff.[49] African-American and Latina trans women are more likely to be victims of assault in jail or prison than their white counterparts.[50] Most HIV-positive prisoners were HIV-positive prior to their incarceration. However, a lack of HIV prevention measures and failure to provide safe environments for trans prisoners – such as the widespread practice of placing trans women in male prison facilities — increases HIV risk in correctional settings.[51]
Mental Health Issues and HIV
Trans people report experiencing high rates of mental health conditions including anxiety, depression, and substance use disorders. Many report anxiety, depression, and trauma resulting from societal factors – including stigma, discrimination, harassment, violence, and other mistreatment based on their gender non-conformity.[52] While cautioning against assuming that all mental health issues are related to gender identity, transgender health experts have identified distress and trauma from familial and societal non-acceptance as key to understanding and treating trans individuals.[53] Many transgender people seek mental health services to help them cope with the effects of prolonged concealment of their gender identity and harms resulting from attempts to express this identity in hostile environments.[54]
Mental health issues have been correlated with increased risk of HIV and poorer outcomes once infected. Depression, anxiety, low self-esteem, sexual abuse, post-traumatic stress disorder, and substance use disorders all have been associated with higher risk of acquiring and transmitting HIV in men who have sex with men, youth, people who use drugs, and transgender women.[55] People living with HIV experience higher rates of anxiety, depression, and substance use disorders than people without HIV, with trans women reporting higher rates of anxiety and depression, and reporting lower quality of life, than other groups living with HIV.[56]
Anxiety, depression and other mental health issues reduce one’s ability to adhere to a daily regimen of anti-retroviral medications, a key determinant of maintaining one’s health and wellbeing while living with HIV. For this reason, access to mental health services is considered an integral component of HIV care.[57]
|
Transgender Men and Barriers to Health Care Trans men face many of the same barriers to health care as trans women: a shortage of gender-affirming health settings, lack of knowledgeable providers, and denials of insurance coverage for basic health services – pap smears, mammograms and other services – that are perceived as “gender incongruent.” Trans men are significantly more likely to live in poverty and to lack health insurance than cis-gender men.[58] Research on health issues for trans men, including HIV research, remains extremely limited. The prevalence of HIV among trans men appears to be significantly lower than that among trans women – ranging from one to three percent in most studies – but still higher than in the general US population.[59] Many trans men have sex with cis-gender men who identify as gay or bisexual, placing them at increased risk of HIV infection.[60] Engaging in sex work and the use of alcohol or drugs also increase HIV risk. However, HIV testing among trans men remains low.[61] For trans men, sex with cis-gender men can be a complex issue, especially for those who are navigating the gay and bisexual community for the first time. Diego Herrera is a staff member working on transgender programs at Sunserve, a non-profit organization serving the LGBT community in Broward County. He told Human Rights Watch that many trans men are secretive about engaging in sex with cis-gender men, making HIV screening and referrals to prevention or treatment services difficult. Lots of trans men are having sex with men, but they do not feel comfortable being open about it. The community is not that supportive of it. Some fear homophobia, and for others it contradicts the ‘masculine’ identity that they are working to develop. There are guys that I know that have a lot of sexual partners, some for money – they need PrEP and HIV testing but won’t do it.[62] In addition, many trans men having sex with men report preferring to get health services in settings that focus on men who have sex with men, but often feel excluded or unwelcome in these environments. This may contribute to lower HIV testing rates and lower access to condoms, lubricant, and other methods of HIV prevention among trans men than among cis-gender men.[63] To date, HIV risk among trans men has not been accurately assessed or prioritized by federal or state HIV policymakers. Inadequate data as well as barriers to health care, including lack of access to affordable, gender-affirming care and HIV prevention services jeopardize the health of trans men. |
Barriers to Access to Medical and Mental Health Care
Trans people generally face formidable barriers in accessing gender-affirming health care. For many trans women with HIV, medical and mental health services remain out of reach. A national survey published in 2016 by the Transgender Law Center’s Positively Trans Project examined the health needs and concerns of trans people living with HIV. The majority (84 percent) of respondents were women, and 41 percent of respondents had a history of incarceration in prison, jail, or immigration detention. Forty-three percent reported income of less than $12,000 per year.[64] The methodology of the survey skewed toward respondents who were likely to be connected with some type of health care rather than those who might be more isolated. Even so, 41 percent of respondents had not seen a doctor for six or more months following their HIV diagnosis.
The primary reason given for not seeing a doctor after their diagnosis was a previous or anticipated discrimination by a health care provider. Cost was also cited as a major factor in failing to access care. African-American and Latino/a respondents reported lower income and were less likely to have health insurance than white respondents. When asked to list their number one health concern, the top concern identified by more than 60 percent of respondents was a need for “gender-affirming and non-discriminatory health care.” The next-highest concerns were hormone therapy and mental health care, including trauma recovery. HIV care was fifth on the list of concerns.[65]
For trans women with HIV, the first priority in addressing their needs is to ensure access to health care that provides them with fundamental respect and dignity. In 2017, a nationwide group of HIV-positive transgender leaders convened by AIDS United issued recommendations for best practices in health care. These leaders stated, “Due to the disproportionate impact of HIV on transgender and gender expansive communities, it is critical that clinics and support services are welcoming, inclusive and competent in serving this population.”[66]
For trans people, services that support them in transition or maintenance of their gender identity are not optional aspects of health care – they are fundamental to affirming individual identity and meeting established standards of transgender health care. The World Professional Association for Transgender Health (WPATH), for example, includes as its core principles:
· Exhibit respect for patients with non-conforming gender identities
· Provide care that affirms patients’ gender identities and reduces gender dysphoria, when present
· Become knowledgeable about the health care needs of gender non-conforming people
· Match the treatment to the specific needs of patients, particularly their gender expression and their need for relief from gender dysphoria
· Seek patients’ informed consent before providing treatment[67]
Trans women frequently prioritize hormone replacement therapy over other health concerns.[68] For this reason, access to hormone therapy is of the utmost importance for trans women living with HIV.[69] Public health and HIV experts, experts in transgender HIV care and, most importantly, trans women living with HIV identify access to transition care, including HRT, as fundamental to effective HIV care for trans women. The Center for Excellence in Transgender Health recommends “bundling” HIV care with HRT and other health services sought by trans women.[70] The AIDS United statement emphasizes the importance of a “one-stop shop” where trans people can receive HIV care as well as comprehensive transgender-focused health services.[71] The WHO states that for transgender women living with HIV, “transition care was perceived as vital pre-requisite for subsequent health care” and recommends that governments prioritize gender-affirming care in developing their plans for addressing HIV in this key population.[72]
The availability of hormone replacement therapy is an essential component of the standard of care for transgender people, and HRT plays an important role in HIV prevention and treatment. As CETH states, “HIV and its treatment are not contraindications to hormone therapy. In fact, providing hormone therapy in the context of HIV care may improve engagement in and retention in care as well as decrease viral load and increase adherence.”[73] Hormone therapy reduces anxiety and depression, factors known to increase HIV risk as well as to interfere with adherence to HIV medications.[74] The National Association of State and Territorial AIDS Directors stated, “Medication adherence among transgender people is heavily dependent on the availability of gender-affirming health services and continued hormone therapy.”[75]
Evidence suggests that in addition to reducing anxiety and depression, access to HRT can be an important factor in reducing HIV-related risk behaviors for trans women. Transition therapy has been found to increase quality of life for trans people including improved employment prospects that may reduce the necessity to engage in sex work.[76] Moreover, for trans women, sex with men can provide gender validation.[77] Numerous studies among trans women indicate that HIV-related risk behaviors – including unprotected sex and sex work – are often related to what has been characterized as an “unmet need for gender affirmation.”[78] Some trans women describe taking risks to have sex with men in order to confirm femininity and affirm their identity as women. Women also describe the relief obtained by access to HRT and other gender-affirming services, either under medical supervision or from street hormones for those who could not access health care.[79] For trans individuals, ensuring access to hormone replacement therapy is an indispensable element of the standard of care for both HIV prevention and treatment.
Federal Policies Contribute to HIV Risk for Transgender Women
Throughout the course of the HIV epidemic, federal agencies have been slow to respond to issues of HIV among transgender people. In 2010 the first US National HIV/AIDS Strategy announced its vision:
The United States will become a place where new HIV infections are rare and when they do occur, every person regardless of age, race/ethnicity, sexual orientation, gender identity or socio-economic circumstance, will have unfettered access to high-quality, life-extending care, free from stigma and discrimination.[80]
The Strategy established three primary goals: 1) reducing new HIV infections; 2) increasing access to care and optimizing health outcomes for people living with HIV; and 3) reducing health-related disparities. In 2015, the Office of National HIV/AIDS Policy released the National HIV/AIDS Strategy Updated to 2020, a document that reaffirms the vision of the original strategy and summarizes progress made toward the three goals using a group of 17 “indicators” for measurement of whether specific targets had been reached.[81] Overall, most people who stay in medical care are achieving viral suppression, but the failure to effectively link people to care after diagnosis and retain them in care for treatment adherence are recognized as key problem areas that are having a severe impact on continued high rates of HIV infection among certain groups. As a consequence, the Update identifies linkage to, and retention in, medical care as top priorities for agencies involved in the nation’s HIV response.[82]
The Strategy identified HIV among transgender women as a serious concern and acknowledged the problem of inadequate access to gender-affirming health care:
Transgender individuals are particularly challenged in finding providers who respect them and with whom they can have honest discussions about hormone use and other practices, and this results in lower satisfaction with their care providers, less trust and poorer health outcomes.[83]
Stating that “historically, efforts targeting this specific population have been minimal,” the 2010 Strategy identified transgender women, particularly women of color, as a “high-risk” population and urged that Congress and relevant federal agencies fund and implement targeted programs for prevention, treatment and support services.[84]
In this context, the needs of transgender women are addressed in numerous provisions of the Update, including a continuing recognition that the dearth of “culturally competent” care for transgender individuals that results in poor health outcomes and a call to establish a new “indicator” for improved data collection of HIV among the transgender population.[85]
But the reality is that despite ample, even overwhelming, evidence of the need to implement culturally competent care and how to do so effectively, implementation of these intentions on the ground is incomplete, fragmented and not incorporated into policy requirements, monitoring, or evaluation.
Some concrete steps were taken under the Obama administration to address trans health care and the alarming risk of HIV infection for trans women. Medicaid expansion was offered to states with the federal government footing most of the bill. The anti-discrimination protections in the Affordable Care Act were interpreted by the Department of Health and Human Services to include discrimination based on gender identity. The CDC issued technical guidance to states to improve their HIV data collection for trans populations and federally funded initiatives such as the Ryan White program, the nation’s largest source of funding for HIV care and services, began to utilize a two-step gender identification process for its clients.[86] But implementation was incomplete, new HIV infections among trans women continued to rise, and the Trump administration is taking numerous steps to undo progress in increasing access to health care.
For example, Medicaid coverage, essential to access to health care generally as well as to HIV prevention, is being undermined by the Trump administration and Congress in a variety of ways. Government respect for transgender rights, including the right to health, is moving in the wrong direction. The burdens faced by transgender women in nearly every aspect of life are occurring in an environment of federal policy that not only remains insufficiently protective of LGBT people’s rights but has also seen the rollback of many recent gains.
LGBT people are protected by a patchwork of laws and regulations that vary in scope and geography. There are no federal laws that explicitly protect persons from discrimination on the basis of either sexual orientation or gender identity. However, under the Obama administration, federal agencies issued a series of rules and regulations based on sexual orientation and gender identity to decrease discrimination in federally funded programs. The departments of Education, Justice, Housing and Urban Development, and Health and Human Services, among others, issued guidance or regulations clarifying that discrimination based on sexual orientation and/or gender identity is impermissible under federal law.[87]
Since 2017, the Trump administration has reversed many of those positions, withdrawing anti-discrimination protections and opposing inclusive interpretations of federal anti-discrimination laws in court.[88] Most recently, the administration has enacted two rules that significantly weaken anti-discrimination protections in federally funded health care activities and programs. These actions are likely to exacerbate health disparities for a population that is already significantly at risk. The first is proposed changes to the protections offered to LGBT people under the Affordable Care Act. Section 1557 prohibits discrimination in health care based on race, color, national origin, sex, age, or disability. In 2016, the Department of Health and Human Services issued a rule clarifying that discrimination based on “sex” includes discrimination based on gender identity and pregnancy status.[89]
The rule would have ensured that transgender people could not be denied care or coverage – including for transition-related services – because of their gender identity. However, shortly after the rule was introduced, eight states and religiously affiliated health care providers challenged it in court, and a federal judge in Texas enjoined it from taking effect.[90] Reversing the Obama administration’s decision to defend this interpretation in court, the Trump administration has indicated that it no longer considers section 1557 to protect against discrimination based on gender identity or pregnancy status.[91] Though the text of section 1557 has not changed, the administration’s re-interpretation of the rule has left transgender people without legal protection and signaled that federal agencies will no longer advance trans-inclusive interpretations of provisions prohibiting discrimination on the basis of sex. In October 2018, the New York Times reported that the administration is considering narrowing the definition of “sex” to male and female for all federal agencies, a move that could eliminate protection against discrimination for transgender and intersex people in employment, education, health care and other areas of life.[92]
The Department of Health and Human Services issued a proposed rule that would give sweeping discretion to providers to discriminate against LGBT people on the grounds of moral and religious belief.[93] The regulation would broaden existing protections for religious objectors by codifying vague, open-ended definitions that would invite discrimination against LGBT people, women and others.[94] In the absence of any provisions that would mitigate harm, these redefinitions risk greatly exacerbating discrimination and barriers to access women and LGBT people already experience. Other actions by the Trump administration include attempts to bar transgender persons from military service and weakening protections for transgender prisoners in the federal Bureau of Prisons. Passage of laws in numerous states that invite discrimination against LGBT persons in health care, adoption, and public accommodations combine with federal action to create a hostile environment that jeopardizes the health of transgender women.[95]
JoAnne Keatley, Director Emeritus of the UCSF Center for Excellence in Transgender Health, is concerned that any momentum for trans women with HIV that did exist will be lost as the Trump administration creates, what she calls, an environment that is “hostile to LGBT rights, but particularly hostile to transgender people.”[96]
In June 2018, the Trump administration released a report on the National HIV/AIDS Strategy indicating that on several key fronts progress had been made and reaffirming the commitment to end the nation’s HIV epidemic.[97] But, as noted by leading HIV advocacy organizations, the administration report did not acknowledge the major policy shifts that threaten continued progress, from attacks on Medicaid to the failure to appoint a director for the Office of National HIV/AIDS Strategy or members to the President’s Advisory Council in HIV/AIDS (PACHA). As noted in an AIDS United press release, “HIV policy does not occur in a vacuum.”[98] Cecilia Chung is a trans woman, national HIV policy advocate, and former member of PACHA. Chung told Human Rights Watch, “Without health care, and without respect for trans people’s rights, we will never end the HIV epidemic in this country.[99]
The federal response has produced some visibility for HIV risk among trans women as well as a patchwork of initiatives and grants. But the crucial issue of whether HIV care is integrated with trans health care and provided in a gender-affirming setting has not been translated into federal policy.
This policy void is most problematic in relation to the Ryan White HIV/AIDS program, a statutory program that since 1996 has provided the majority of national funding for medical care, medication and support services for people living with HIV.[100] Administered by HRSA and implemented by the states, Ryan White is a safety net program – eligibility for Ryan White programs, including the AIDS Drug Assistance Program (ADAP) that helps pay for medications, is based on income and availability of health insurance. Ryan White patients must have an HIV diagnosis and income of less than 400 percent of the federal poverty level.[101] Ryan White is intended to be the provider of last resort – the program is available for those who have no insurance, but it can also supplement services that are left uncovered by insurance and, in the case of medications, help pay some premium costs and co-pays to ensure access to HIV medications.[102] Care and services offered through Ryan White funded programs are critical to the US HIV response: an estimated 52 percent of people living with HIV — 550,462 people in 2016 — utilize Ryan White. Ryan White patients have significantly better health outcomes, as these services have proven to be vital to their health; 85 percent of Ryan White patients have achieved viral suppression compared to 49 percent nationwide.[103]
The purpose of the Ryan White program is to ensure care for those who have no other options, and in states like Florida with limited access to Medicaid, the program is of lifesaving importance for trans women living with HIV. According to HRSA’s annual Ryan White report for 2016, there are 7,166 transgender clients in Ryan White programs nationwide, 355 of whom reside in Florida. Most are trans women (93 percent) and African-American (54 percent). An overwhelming majority live in extreme poverty: 78 percent live at or below the federal poverty level, earning less than $12,000 per year.[104] Though lower than for Ryan White clients overall, viral suppression rates for transgender clients are high (79 percent), much higher than the national average of viral suppression of 49 percent, illustrating the importance of the Ryan White program to transgender women living with HIV. Ryan White-funded clinics clearly help trans women once they enter and stay in the program – but as with other key groups impacted by the US HIV epidemic, there are troubling gaps in engagement and retention in care.
The necessity of gender-affirming care to engage and keep trans women in HIV care is well established, as is the feasibility of implementing this approach. In 2012, HRSA began funding a Special Project of National Significance (SPNS) project called the Transgender Women of Color Initiative (TWOC). TWOC was a demonstration project for improving HIV care at nine sites – both health facilities and community organizations. One of the primary elements of this project was the integration of trans-related health care, including HRT, with HIV care at several of the sites. None of the TWOC sites was in Florida, but for more than five years this project has demonstrated how a focus on providing gender-affirming care — from putting posters with images of trans people on the wall in a clinic to helping with documentation to ensuring availability of HRT — can improve HIV outcomes for trans women of color, and full results are expected to be published in fall of 2018.[105]
The quality of HIV care for trans individuals is included in one federal demonstration project, but participation by states and clinical providers is optional. HRSA is funding a project to offer technical assistance to state health departments and Ryan White-funded health care providers to improve the quality of HIV care to high-risk populations. The project, called the ECHO project, commenced in July 2018, and is designed to respond to requests for assistance from clinics whose data indicate health disparities for any of four groups, including transgender people. Transgender HIV experts will be available to consult on ways to increase trans engagement and retention in care. But whether entities will reach out for assistance with trans clients remains to be seen. According to one administrator for the HRSA ECHO program, response from providers is uncertain:
We are not sure that trans issues will be addressed. It is a time commitment to participate – ten hours of training a month, data reports monthly, consultant involvement – this is a lot of time for a very small population.[106]
Another HRSA-funded project commencing in 2018 will support 26 clinics around the US to implement evidence-based approaches to HIV care for high risk populations, including transgender people. Yet no policies or standards require federally funded HIV care to be provided in a gender-affirming setting and there is no systematic monitoring or evaluation of this issue by the federal government.
JoAnne Keatley has published extensively on the importance of integration of care and provided technical assistance for the TWOC project. According to Keatley, “Even before the TWOC project, we had the evidence we need – we know what to do to improve HIV outcomes for trans women. We have been working for decades to incorporate these findings into federal policy.”[107]
In the absence of federal standards or guidance, integration of HIV care with trans health care remains aspirational, limited, and incomplete in many states such as Florida. As discussed in detail below, Florida HIV officials provide funding to clinics that promote and offer gender-affirming care, but information from the ground indicates that they are also funding sites that do not. The AIDS Drug Assistance Program (ADAP) provides HIV medications to those without health insurance, but in many states, including Florida, medications necessary for gender transition care are missing. Although millions of federal dollars are being administered, states implement Ryan White funding without policy guidance or compliance standards from the federal government for ensuring that gender-affirming care is implemented. According to Florida Department of Health HIV program officials:
After a thorough search we could find no HRSA or Ryan White regulations that addressed gender-affirming care for transgender women living with HIV.[108]
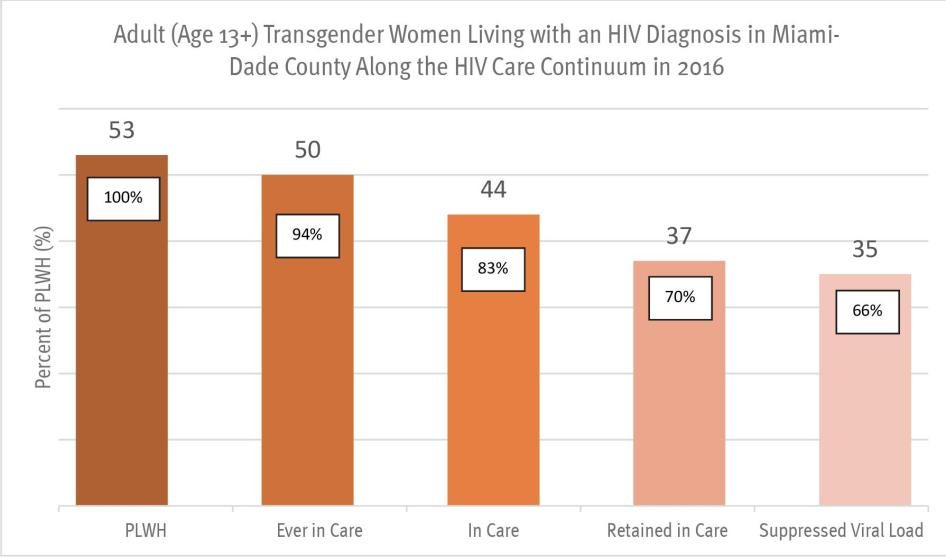
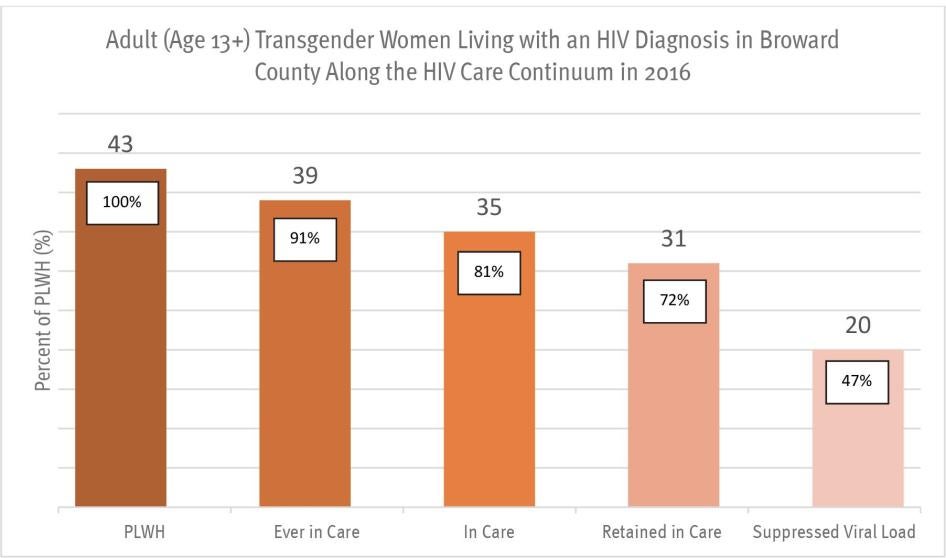
HIV in Florida
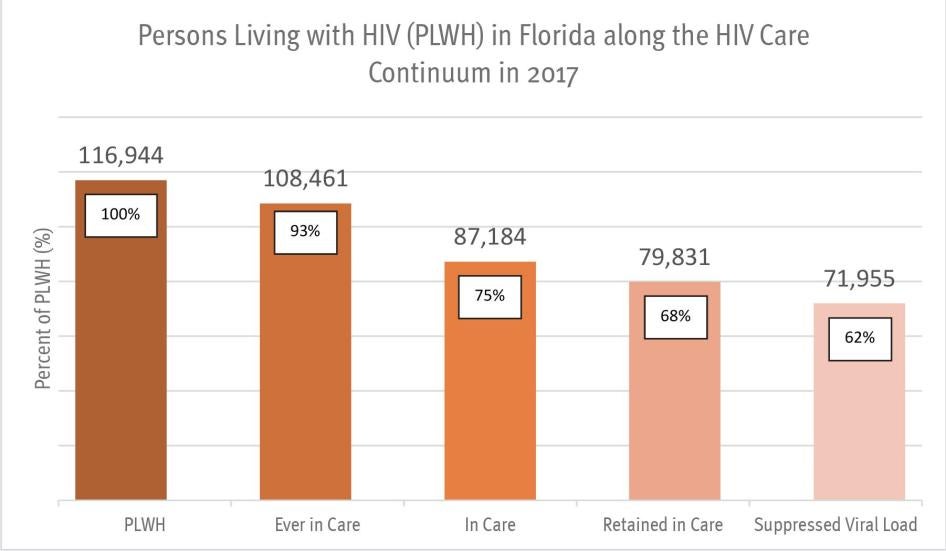
The state of Florida, along with the rest of the US south, lies at the center of the nation’s HIV epidemic. With more than 116,000 people known to be living with HIV, Florida accounts for 11 percent of HIV cases in the US.[109] Florida has the nation’s third highest rate of new HIV infections, and the epidemic is concentrated in urban areas of the state. The cities of Miami, Fort Lauderdale and West Palm Beach accounted for 47 percent of the state’s new HIV infections in 2016.[110] The rates of HIV infection in Miami-Dade and Broward counties are the highest in the nation. In 2017, the metropolitan areas that included Miami-Dade and Broward counties ranked first and second in the US in the rate of new HIV infections.[111]
Racial disparities are stark. In Florida, one in every 151 adults is known to be living with HIV; one in 295 whites, one in 49 African-Americans and one in 155 Hispanics.[112] African-Americans are 15 percent of the state’s population, but account for 42 percent of adult HIV infection cases and 50 percent of adult AIDS diagnoses. Hispanic people comprise 24 percent of Florida’s adult population but represent 31 percent of HIV infection cases and 24 percent of AIDS cases.[113] The rate of HIV infection in Florida is five times higher for Black men than white men, and 12 times higher for Black women than white.[114]
Florida surveillance data indicate that male-to-male sexual contact is the primary mode of transmission for both those living with HIV and new infections, followed by heterosexual contact and injection drug use.[115] As discussed in detail below, this data does not accurately reflect either cases or transmission modes among the transgender population.
State Response to HIV
In the US, the federal government is the primary source of funding for state HIV response, and the severity of the epidemic in Florida has resulted in what the statewide HIV Prevention and Care Plan calls “one of the nation’s most comprehensive programs for HIV/AIDS surveillance, education, prevention, counseling, testing, care, and treatment.”[116] In fiscal year 2017-2018, Florida’s HIV budget totaled nearly $300 million, mostly from federal sources. This budget has increased in the last three years by 15.6 percent. [117]
In Florida, lack of other insurance options has resulted in a significant reliance on Ryan White. One in five people in Florida is uninsured, the third-highest percentage in the nation.[118] More than half of people living with HIV in the state rely on care and services from the Ryan White Program.[119] Florida has a very restrictive Medicaid program and many people cannot afford to purchase private insurance, do not receive it from their employer, or are not eligible for federally subsidized insurance premiums under the Affordable Care Act. An estimated 384,000 people fall into this “coverage gap” in the state.[120] In Florida, the majority of Ryan White clients are African-American men, have incomes under 100 percent of the federal poverty level (less than $13,860 per year for an individual), and have no insurance.[121]
Florida’s extensive public HIV program has produced mixed results. Significant improvement has occurred over the last decade: Between 2008 and 2017, there was an 18 percent decline in HIV cases diagnosed, a 51 percent decline in AIDS cases diagnosed, and a 47 percent decline in HIV-related deaths.[122] Some recent trends are promising. Between 2014 and 2016, more Floridians with HIV entered medical care, remained in care, and became virally suppressed.[123] In the state ADAP program, 9 of 10 clients have achieved viral suppression.[124]
However, new infections have increased since 2013. Rates of new infection are highest among men who have sex with men (a category that erroneously includes many trans women), particularly young men of color.[125] The number of patients who fail to remain in treatment for HIV is concerning; of persons diagnosed with HIV, 92 percent are linked to care, but only 66 percent remain in care and 60 percent become virally suppressed.[126] Despite improvement in some areas, Florida is still struggling to bring its HIV epidemic under control.[127] In 2018, state HIV officials reported that many of the targets set in the previous year – including reducing new HIV infections, reducing new infections among African-American and Hispanic people, and reducing rates of infection among Hispanics – had not been met.[128]
Florida faces many challenges in effectively managing HIV. With 20 million people, it is the fourth most populous state in the US, a vast geographical area both urban and rural. Floridians are multi-ethnic (17 percent African-American and 24 percent Hispanic or Latino, according to 2017 census estimates) and there is a considerable transient population comprised of migrant workers as well as seasonal and part-time residents.[129] Its fiscal policy is conservative, with a constitution that prohibits state income taxes – the last tax increase occurred in 1988 and increased the sales tax by one percent.[130] Under Republican Governor Rick Scott, health and education budgets have experienced deep cuts.[131] In 2017, public health funding in Florida as a percentage of the budget ranked 40th in the nation; effective health care policy, comprised of factors such as percent uninsured, health spending, and vaccination coverage, ranked 46th among 50 states.[132]
In 2018, the legislature failed to pass a bill that would have permitted syringe exchange programs to operate statewide, leaving Miami-Dade as the only county with a syringe exchange program. Rejection by conservative legislators of proven public health and harm reduction approaches to injection drug use are problematic as the state, and the US, faces an unprecedented epidemic of drug overdose and increasing rates of HIV, hepatitis C, and other illnesses from injection drug use.[133]
The policy most detrimental to Florida’s ability to manage its HIV epidemic is the state’s failure to expand its Medicaid program. Under the Affordable Care Act, states have the option to expand eligibility guidelines for their Medicaid programs with payment largely covered by the federal government.[134] Florida is one of 18 states that have rejected this option despite Florida’s very restrictive Medicaid eligibility guidelines for its state program. Florida limits Medicaid eligibility both categorically (one must be disabled, parents of dependent children, a pregnant woman, or in need of long-term care) and income (for example, parents and caretakers’ income cannot be higher than 29 percent of the federal poverty level, or more than $7,380 per year).[135]
Medicaid expansion has benefited people living with HIV, primarily by ensuring coverage for a core group of comprehensive medical services without exclusion for pre-existing conditions.[136] In Medicaid expansion states, Medicaid coverage for people living with HIV rose 11 percent, with the most significant gains in coverage experienced by people with the lowest incomes and people of color.[137] Medicaid expansion has the potential to significantly mitigate HIV risk as well; expansion has been shown not only to increase access to comprehensive health services but to reduce poverty, a primary driver of HIV risk in the US.[138] Because Medicaid expansion regulations incorporate the anti-discrimination provisions of the Affordable Care Act, expansion is particularly important for LGBT people and other groups experiencing discrimination in health care.[139]
Broader eligibility under Medicaid expansion extends not only to working people with higher incomes, but to adults without dependent children. For Floridians, and for many trans women, this is a key factor as the Florida Medicaid program is limited to adults with dependent children, pregnant women or people with disabilities. In Florida, 87 percent of people who fall into the health insurance “coverage gap” as a result of failure to expand Medicaid are adults without dependent children, and 47 percent are people of color.[140]
Findings
For this report, Human Rights Watch administered 125 questionnaires to women of trans experience in Miami-Dade and Broward counties, gathering demographic information as well as information related to access to health care, including HIV prevention and treatment. The surveys and additional interviews with trans women, their advocates, HIV providers, and others indicated that many trans women in south Florida, particularly Latina and African-American women, live in an environment of high HIV risk as a result of multiple factors, with poverty and lack of health insurance standing out as primary vulnerabilities. Lack of income was associated with high rates of participation in sex work and with high rates of involvement with the criminal justice system – factors that increase HIV risk. These findings are consistent with other surveys of trans women in Florida, such as the one conducted by the 2015 US Transgender Survey, showing high rates of poverty and criminal justice involvement for trans women, particularly women of color.[141]
This severe and compound environment of risk for HIV demands a robust response from both state and federal government. There is ample evidence of how to provide effective health care, including HIV care, for trans women. But in south Florida, trans women face a fragmented landscape for health care that fails to ensure that effective, integrated HIV care is available at a cost that transgender women can afford. With no explicit or coordinated policies to ensure systematic monitoring and evaluation of HIV prevention or care for trans women, accountability is lacking. Policy development is hindered by lack of accurate or complete data regarding HIV among transgender women, a continuing problem that perpetuates a cycle of perceiving this at-risk population as “too small to help” at both the state and federal levels. Criminalization of sex work and HIV promote unemployment, poverty, and stigma that make access to health services more difficult. Few questions remain about what needs to be done, but without commitment by policymakers to do it, trans women will continue to experience grossly disproportionate disparities in access to health and HIV prevention and care.
Trans Women Face Barriers to Health Care in Florida
Trans women in Miami-Dade and Broward counties face multiple challenges that impact access to health care. As part of the research for this report, Human Rights Watch conducted a survey of 125 trans women with the assistance of local organizations and trans health advocates. The results below indicate severe socio-economic deprivation and a fragile existence for the majority of trans women interviewed.
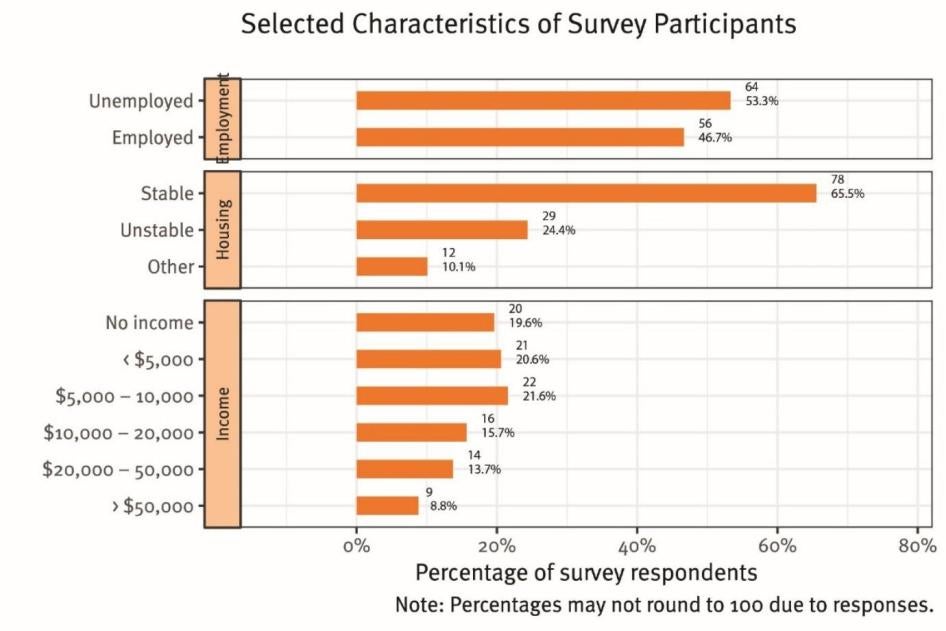
The survey results reveal many trans women experience extreme poverty, with 63 percent of participants reporting income of less than $10,000 per year (20 percent of survey participants had no income; 21 percent reported income under $5,000 per year; 22 percent reported income between $5000 and $10,000 per year). More than half (53 percent) were unemployed. One third reported that their housing situation was “unstable” or “other” than stable (see Graph II).
These were not the most marginalized trans women living in areas with scarce resources. The survey was distributed through organizations providing services to trans women and participants were more likely to be connected to health care than in a more randomized sample. Also, the surveys were distributed in two major metropolitan areas with extensive health and HIV care infrastructure. Yet the results below indicate significant gaps in coverage and access to health insurance or care (see Graph III).
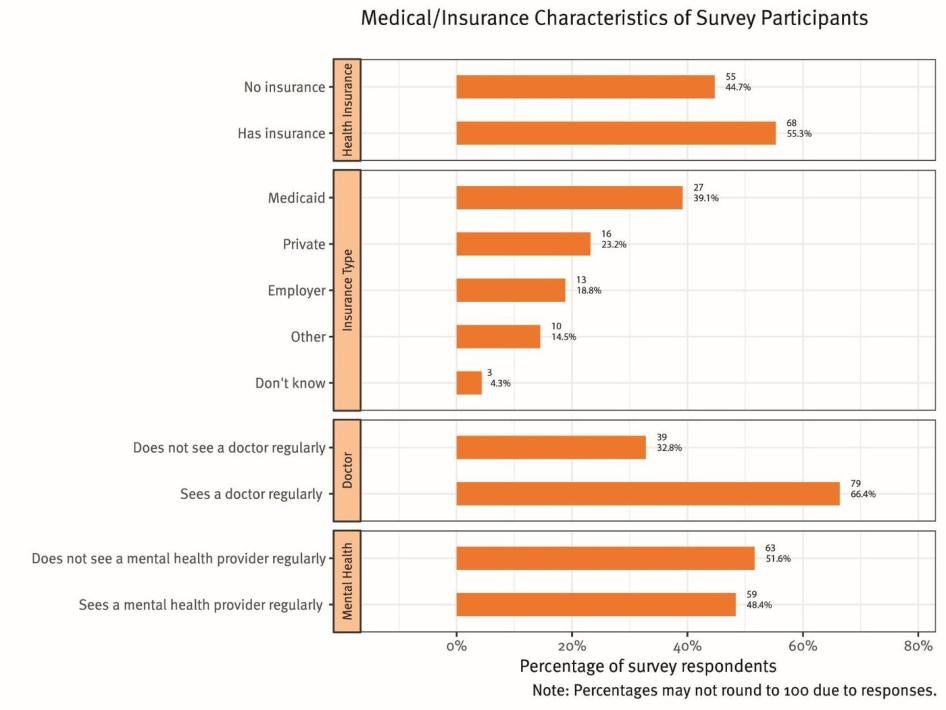
Of trans women surveyed, 45 percent had no health insurance. Of those that had health insurance, 39 percent had Medicaid and 23 percent reported having private insurance. Sixty-six percent see a doctor regularly (defined as twice a year or more) and 48 percent see a mental health provider regularly. Of those who did not see a doctor regularly, 38 percent said they could not afford it.
In detailed survey responses, many women described bad experiences with medical providers and their struggles to access gender-affirming care:
“Every time you walk into the doctor’s office, you become a science experiment.” – Ellen, age 44.[142]
“When I transitioned, my doctor wouldn’t see me after that. I couldn’t get in to see them. I had an infection and they wouldn’t call in the antibiotics. It was an ordeal. It was scary. I just felt bad about how they treated me.” Susan, age 22.[143]
“I used to go to Jackson hospital, but I haven’t been there in over a year. They are terrible. Not knowledgeable about trans health. They misgendered me. I don’t feel comfortable or trust them.” – Barbie, age 65.[144]
Many described cost and lack of insurance as the key factor in lack of health care:
“I made $450 a month and was working for ten years. Was denied Obamacare. Very hard to find insurance in Florida.” – Valerie, age 50.[145]
“I have diabetes. Hormones and diabetes medications cost $500 a month, I can’t afford that.” – Diana, age 54.[146]
Knowledge of where to get an HIV test was high, with 91 percent reporting that they knew where they could get tested. Nearly one quarter (23 percent) of survey participants reported that they were HIV-positive. To place this result in context, many surveys were distributed through agencies that provide referrals for HIV-related services. More than one in three (35 percent) trans women living with HIV had no health insurance. However, 88 percent of women living with HIV reported seeing a doctor regularly, and most were taking HIV medications (92 percent). With 77 percent of women living with HIV reporting that they had achieved an undetectable viral load, these results indicate the importance of the Ryan White safety net in states such as Florida, where many are without insurance and Medicaid has not been expanded.
Many of the women, including those living with HIV, described a difficult process for finding care that centered around safety and trust concerns.
Misty Eyez is a trans woman who works as an educator, trainer and case manager for trans women at Sunserve, an NGO in Broward County. Eyez described the fear of going to the doctor:
Many trans women are not comfortable leaving their house during the day. Therefore, going to the doctor can be an ordeal. For many reasons, some feel they have to put themselves totally together with the dress, the wig, the makeup in order to go out of the house, and then will they be safe in public, on the street, or on the bus? And how will they be treated when they get there? It is very lonely and isolating.[147]
Lack of Gender-Affirming Care Impedes HIV Response
For trans women, including those living with HIV, gender-affirming health care is not optional. Not all trans women want hormone replacement therapy (HRT), but for many it is central to their wellbeing and their number one health care priority. As Morgan Mayfaire, a trans man and co-director of TransSOCIAL, an advocacy organization for trans people living with HIV in Broward and Miami-Dade counties, told Human Rights Watch: “In this community, HRT is all. You will walk through a moat full of alligators to get your hormones.”[148]
This is true even for women living with HIV, which is one reason that HIV and trans health experts consider integration of HRT and HIV care to be critically important. The WHO, the Center for Excellence in Transgender Health at the University of California at San Francisco, the Fenway Institute, and others clearly identify integration of HRT and HIV care to be a best practice for HIV care for trans individuals.[149] The trans leaders convened by AIDS United emphasized the importance of a “one-stop shop” providing HRT and HIV treatment:
Due to financial hardship, housing instability, trauma due to a very real fear of violence in their lives, and distrust of medical personnel, trans people often fall out of care. If trans people are to successfully engage in and remain retained in care, clinical settings must design care that accounts for this reality. [As a best practice] Providers should consider establishing trans medical homes that address all health needs in a “one-stop shop” to retain and engage people in a consistent level of preventive and primary care.[150]
According to Dr. Madeline Deutsch, an expert in transgender health at the University of California at San Francisco, integration of HRT with HIV treatment should be considered not only a best practice, but the standard of care for trans people living with HIV:
Hormone therapy can increase engagement in care and increase adherence to anti-retroviral medication. It may not yet be considered a standard of care, but it should be. Not providing hormone therapy with HIV care is akin to providing HIV care in a Latina neighborhood without any Spanish speakers available.[151]
In south Florida, finding health care in a gender-affirming environment is difficult, and for trans people living with HIV the options are limited. Human Rights Watch interviewed trans women and their advocates, Ryan White providers, public health officials, and organizations in each county whose primary mission includes directing trans people either recently diagnosed with, or living with, HIV to appropriate medical services. These latter resources, many of which are small non-profit agencies, make it their priority to stay abreast of which clinics offer gender-affirming care, including HRT, to trans HIV patients so they can make effective referrals for care. It is a fluid situation that often depends on the presence of an individual trans-friendly or trans doctor, case manager, or another key employee. Based upon these sources, three to five clinics in each county were consistently identified as providing gender-affirming integrated HIV care to transgender people.
HIV care is widely available in Miami-Dade and Broward counties. An extensive, federally funded network of private, public and community-based providers offer prevention, medical care, case management and support services. The Health Resources Services Administration (HRSA) administers the Ryan White program funding in the US. HRSA designates priority funding for primary medical services under Part A of the program to metropolitan areas throughout the country. Due to the severity of their local HIV epidemics, Broward and Miami-Dade counties are two of six Florida metropolitan areas that receive Ryan White funds for primary medical services under Part A of the Ryan White program. In fiscal year 2017-18, Miami received more than $26 million in Part A funding for treatment and care and Fort Lauderdale received more than $15 million. This does not include separate funding received by both counties for Part B services which include the AIDS Drug Assistance Program (ADAP) for HIV-related medications.[152]
In Broward County, there are 13 providers of primary medical care for HIV that are entirely or partially funded by Ryan White. In Miami-Dade County, there are 24 providers of primary medical care for HIV entirely or partially funded by Ryan White. These range in type from private non-profit organizations such as the AIDS Healthcare Foundation to the University of Miami Comprehensive AIDS Program at the Miller School of Medicine. In both counties, clinics are available in all regions of the county, though most services are concentrated in the cities of Fort Lauderdale and Miami.[153]
However, finding gender-affirming health services is a challenge. Arianna Lint is a Latina trans woman and director of Arianna’s Center, a non-profit organization whose mission is to provide support services, outreach, and advocacy for Latina trans women in both Miami-Dade and Broward counties. Arianna is a woman living with HIV and, as part of the national Positively Trans initiative sponsored by the Transgender Law Center, about one third of Arianna’s 350 clients are HIV-positive trans women. Arianna explains that in south Florida, finding a clinic where Spanish language services are available is not a problem, but HRT availability is limited, making referrals difficult for many of her clients.
For the girls who are HIV-positive I help them in every way – I counsel them about HIV, I get them connected to medical care that they can afford, and I help them stay on their HIV medications. I know which clinics in the area are trans-friendly, and they can either start or get onto hormones if they want them. Unfortunately, there are very few clinics that provide both hormones and HIV care, but I know which ones they are, so that is where I send women when they call me for help.[154]
As co-director of TransSOCIAL, a non-profit organization that provides a wide array of support, Morgan Mayfaire refers hundreds of trans people to services in both Broward and Miami-Dade counties each year. TransSOCIAL also provides cultural competence trainings to businesses, health centers, and HIV providers in an effort to expand safe and affirming resources for the trans community. Mayfaire is also a member of the state HIV Comprehensive Planning Network (FCPN), and he told Human Rights Watch:
There is a severe lack of HIV providers who are willing to prescribe hormones or offer a trans-friendly environment. We refer to a handful of clinics and that covers both Miami-Dade and Broward counties. It’s a big problem because there are many more HIV providers than HRT providers, but most HIV providers do not want to prescribe hormones, or people have had bad experiences going to that location. We spend a lot of time working on trying to make HRT and ART available in the same place.[155]
Dr. Sheryl Zayas is the Medical Director of Care Resource Community Health Center in Fort Lauderdale, a full-service health center that is partially funded by Ryan White to provide HIV care in the community. Dr. Zayas estimates that between 10 and 15 percent of her several hundred patients are trans women, many of them HIV-positive. Dr. Zayas describes Care Resource as a gender-affirming environment, an opinion that was confirmed by trans survey participants and those who refer trans patients for HIV care. At Care Resource Fort Lauderdale, services are offered on a sliding scale for income, staff are trained regularly on trans-sensitive issues, low thresholds are set for documentation and it need not be conforming to one’s gender identity, and a trans woman is employed in an outreach program to inform trans women about HIV services at the clinic. Dr. Zayas told Human Rights Watch that she considers offering hormone replacement therapy to be “essential” to keeping people in care:
This is a community under stress. Homelessness, lack of jobs, lots of having to do sex work to survive. All of my trans clients don’t want hormones, but most do, and I have a better chance to keep them in health care if I can prescribe it.[156]
However, not all of the Care Resource locations offer this level of service to trans patients. At one clinic, for example, Dr. Zayas said, “We have one provider who treats HIV patients but doesn’t want to do HRT. I don’t know why. It might be for religious reasons.”[157]
Dr. Zayas believes training of medical professionals can go a long way toward reducing reluctance to provide hormone therapy. She is not an endocrinologist, but finds it sufficient to follow the WPATH guidelines for transgender primary care and the standards for hormone treatment established by the Endocrine Society Clinical Guidelines. She participates in medical training symposia that address transgender health issues and clinical practice.
Dr. Maureen Greenwood’s practice at the AIDS Healthcare Foundation clinic in Oakland Park, Broward County, focuses on HIV. Dr. Greenwood has approximately 200 transgender patients. Dr. Greenwood, a Doctor of Nursing Practice, said she follows the WPATH guidelines for transgender clinical care and consults their staff endocrinologist in more complex cases, but that that situation is rare. Dr. Greenwood also stated that training for medical practitioners in transgender health issues is essential to increasing the availability of services.[158]
Some medical providers may not be aware that standards and best practices for transgender health have evolved, moving away from specialist care for hormone therapy and eliminating the need for a mental health referral to initiate hormone replacement therapy. Historically, a mental health provider had to approve an individual for HRT before a primary care physician could prescribe the medication. Though this approach is still accepted by WPATH as valid, an “informed consent” model is now widely implemented that lowers the threshold and focuses on the elements of informed consent that are ethically required for administration of all other medications: an individual’s understanding of the risks, benefits and consequences of taking, and of not taking, gender-affirming medications. This model is endorsed by WPATH, CETH, and other experts as appropriate for medical providers to implement on their own.[159] Under current standards, doctors, nurse practitioners, physicians’ assistants, and other providers qualified to assess and diagnose gender dysphoria and assess informed consent can prescribe hormone replacement therapy for gender transition. As stated in an article by Dr. Madeline Deutsch of CETH:
Prescribing gender-affirming hormones is well within the scope of a range of medical providers… Most medications used in gender-affirming hormone therapy are commonly used substances with which most prescribers are already familiar due to their use in the management of menopause, contraception, hirsutism, male pattern baldness, prostatism, or abnormal uterine bleeding.[160]
Florida State Response
The Florida state HIV Plan for 2017-21 identifies transgender people, particularly women of color, as a “high priority” population, and the state has taken a variety of steps to address HIV among transgender women. Between 2013 and 2017, statewide programs provided HIV testing for more than 2,500 transgender individuals, identifying 85 trans persons as living with HIV. Since 2012, $8 million in federally funded HIV grants have been distributed to community-based organizations statewide for prevention activities focused on all priority populations, including transgender women. Because prevention efforts now include ensuring that people living with HIV are in treatment, these programs offer traditional prevention activities such as education and condoms as well as linkage to treatment services for people living with HIV. During 2016 and 2017, prevention services were provided to more than 1,000 transgender women in the state through these programs.[161]
In Broward and Miami-Dade counties, federal and state funds support at least seven agencies that provide HIV prevention and supportive activities and events for transgender communities.[162] Since 2016, the state has used federal and state funds to conduct eight trainings to improve LGBT cultural competency for both DOH staff and community providers in various cities in Florida, including two in Miami. To the credit of state HIV officials, HRW survey results show that most trans women participants living with HIV were receiving HIV care. This result likely reflects the methodology of the survey, which was administered largely through organizations that provide services to trans women, including referrals to HIV treatment and support.
Retention in Ryan White care, however, is a significant issue in Florida, and the state has very incomplete information regarding how many trans women living with HIV are actually in care, why they are not receiving care, or why they fail to remain in care. The problem is not a fiscal one; federal funding for HIV care has remained stable, and unlike many other states in the Deep South, state funding also contributes to HIV prevention, care, and support services.[163] The Department of Health told Human Rights Watch that there is no shortage of funds for transgender related services.[164] Rather, the problem is a policy void. There is no mention of gender-affirming HIV care in the State HIV Plan and there is no systematic approach – no policy, no guidelines, no monitoring, no evaluation – of whether the multiple medical care providers in Miami-Dade and Broward counties are providing gender-affirming care or making hormone replacement therapy available.
State HIV officials told Human Rights Watch:
The Ryan White program does not specifically fund transgender-specific services. However, both Part A and Part B programs fund agencies that provide transgender-friendly services... Several clinics in Broward County provide gender-affirming care… There are a few in Miami-Dade as well.[165]
According to state HIV officials, “transgender individuals are always welcome at any Ryan-White supported medical provider.”[166] But in reality, there are no mechanisms in place to ensure that that is true, and evidence from the ground suggests otherwise. Multiple survey participants described bad experiences at local Ryan White clinics, and trans health advocates described their unwillingness to refer clients to most of the Ryan White clinics in Miami-Dade and Broward counties. Arianna Lint stated:
Most of the Ryan White clinics I would not refer [clients] to – women tell me about rude staff and doctors who won’t give hormones or don’t understand their bodies. Many bad stories. One clinic told me ‘transgenders are not a priority.’[167]
Morgan Mayfaire told Human Rights Watch, “We recently called a Ryan White clinic in Fort Lauderdale to ask if they offer gender-affirming care. They hung up on us. [168] Ashley Mayfaire of TransSocial said, “Another Ryan White clinic we called recently told us they don’t have a doctor at that location that treats trans patients.”[169]
Joey Wynn is Community Relations Director at Empower-U, a federally qualified health center in north Miami. Empower-U is one of the few clinics in Miami that provide gender-affirming care, including hormone replacement therapy, to transgender clients with HIV. According to Wynn, “We serve many transgender clients with HIV and we use Ryan White funds to partially support our HIV services. But state involvement in the quality of care for our trans clients is minimal – it is not something they are following closely.”[170]
Three to five clinics offering HIV and HRT services meets the needs of some trans women in Miami and Fort Lauderdale. But the fact that these represent a fraction of the federally and state funded HIV clinics is cause for concern. Consistent with principles of non-discrimination, all Ryan White clinics should accept trans patients.[171] Moreover, more trans-competent providers are needed. Many trans women not connected to referral services may not find these clinics or may face transportation and other barriers to accessing care at these locations. When service is disrupted, as is not uncommon when doctors leave or stop taking new patients, delays and waiting lists can leave women without care. Ashley Mayfaire stated, “Just in the last few months we have had doctors leave two of our clinics that we most often refer people to – we are not sure if or when these will be replaced.”[172] Pressure on these few locations is increased by the shortage of gender-affirming health care services elsewhere in the state, which brings trans people from throughout Florida to Miami-Dade and Broward counties for care.[173] “We get calls all the time from all over the state – these clinics are a ‘mecca’ for trans people who can’t find care where they live.”[174]
According to state HIV officials, much of the problem is a failure of federal Ryan White policy to prioritize transgender care:
It has been difficult to fund services for the trans community, because many of the services that are needed are not allowable (e.g. surgery) under the Ryan White legislation. Some areas of the state have included HRT (hormone replacement therapy) in their formularies. But other body transformation services (implants, lip enhancements, etc.) cannot be supported by Ryan White funds. Serving the transgender community has been a challenge in many areas and is one of the top issues identified for training and technical assistance for providers throughout the state. This is an issue that the patient care program continues to struggle with, and continuously works to improve on.[175]
State officials are correct in pointing to deficiencies in Ryan White coverage for transgender health issues, as discussed in detail below. But gender-affirming care comprises more than funding for surgeries. Many of its components – staff awareness of trans issues, knowledgeable providers, trans employees and involvement, and other factors that create a safe space – could, and should, be a focus of state HIV policy, planning, and evaluation. As they noted, provider training is of the utmost importance, but eight trainings statewide in 2.5 years does not signal a commitment to ensuring that all trans women are “welcome” at Ryan White facilities and services.
State leadership could also make a huge difference to trans women living with HIV by ensuring that hormone replacement therapy is available through the Ryan White ADAP program.
Cost and Lack of Insurance Coverage for Hormone Replacement Therapy (HRT)
In the insurance-based health care system in the United States, lack of insurance coverage is a major barrier to accessing care. As reflected in the Human Rights Watch survey, many trans people lack insurance altogether. For those who do have insurance, the issue of coverage for transgender people’s health care is complex and characterized by harmful gaps in coverage. Claims for care are often denied by both private and public insurers, whether for services and medications related to gender affirmation or for primary care such as pap smears, prostate tests, and other procedures not related to transgender identity.[176] Providers bill for services using codes for diagnosis and procedure, and claims denial or delay often originates due to perceived gender incongruity between gender and diagnosis or procedure codes.
For example, pap smears for a patient whose gender is reported as male in the medical record may be automatically denied by the insurer or sent back for clarification.[177] To address chronic denials of care on the basis of gender, legal protections have been established in recent years at the federal level for transgender patients. Most important of these is section 1557 of the Affordable Care Act that prohibits discrimination in both federally funded and private insurance coverage based on factors that include “sex,” a category interpreted by the Obama administration to include gender identity.[178] Federal regulations for the Medicare program also explicitly address the issue of gender incongruity denials and provide a special billing code intended to prevent the practice and an appeal process if a claim is erroneously denied.[179] Enforcement and implementation of these protections, however, was incomplete and discrimination in coverage remained widespread, a situation expected to worsen under the Trump administration’s plan to abandon gender identity entirely as a protected category under 1557.
In contrast to Medicare, no such protections exist for the Medicaid program, a gap that significantly impacts many trans people living with HIV. Federal Medicaid regulations are silent when it comes to transgender health issues and coverage, leaving coverage determinations for transgender patients to the states and to a “case-by-case basis.”[180] Although 18 states and the District of Colombia specifically prohibit discrimination against transgender patients in their Medicaid plans, Florida is not one of them – state Medicaid regulations are silent on the issue. There is no explicit state Medicaid policy that excludes or includes trans health care. This leaves coverage of transition-related care, from HRT to body transformation surgeries, to be decided by the state Medicaid office on a case by case basis. This lack of policy guidance creates inconsistencies and confusion among both patients and providers regarding coding, billing, and coverage. Advocates have pressed state Medicaid officials and the state Insurance Commissioner for policy guidance but to date have not been successful.[181]
Even when a trans woman finds a doctor to prescribe hormone replacement therapy, cost can be a significant barrier.[182] In the Human Rights Watch survey, 45 percent of those without a doctor identified cost as a barrier to health care and many commented on their inability to afford HRT. As one survey participant commented, “I have no access to hormones, insurance doesn’t cover them.”[183] Another said, “I am taking pills (hormones) informally – I can’t afford them from the doctor and they aren’t covered by insurance.”[184] Indeed, many trans women turn to the street for hormones due to cost barriers, a practice that carries health risks including lack of dosage monitoring, unknown substances, and the possibility of shared needles for injected hormones.[185]
In their survey responses, some trans women expressed despair about the obstacles faced in obtaining hormone therapy:
I am afraid because cost is so high; all the girls say it is so expensive. When am I going to be able to see my real self? To be my real self? Very fearful that I will never be able to be my real self because I can’t afford it.[186]
Trans patients whose doctors will prescribe hormones often struggle to pay for them. In addition to medication cost, hormone levels must be regularly monitored, and the lab work can cost as much as $250.[187] Even at clinics where hormones were prescribed for trans patients and services were offered on a sliding scale to those who had no insurance, providers described issues with cost for hormone treatment.
Amethyst St. John, director of Behavioral Health at the Empower-U clinic in Miami, said that 90 percent of their transgender patients have the goal of starting hormone replacement therapy. However, according to St. John, lack of insurance coverage for the treatment forces out-of-pocket payments, which few patients can afford. “Without the proper finances in place, or an insurance plan that will adequately cover the cost of this therapy, clients are stalled for months or years waiting to begin hormones.”[188]
Dr. Michelle Powell at the AIDS Healthcare Foundation clinic at Mercy Hospital in Miami-Dade County stated, “I will prescribe hormones, but cost is a problem. Medicaid only covers hormones for cisgender people. Ryan White doesn’t cover it.”[189]
Dr. Maureen Greenwood at the AIDS Healthcare Foundation in the Oakland Park clinic in Broward County said that some hormones are covered by Medicaid and other insurance providers for cisgender patients. “But the same claim will be denied for trans patients, and most of my patients pay for their hormones out of pocket as a result. Once insurance companies find out it is for a transgender person, they won’t cover it.”[190]
For trans women living with HIV, access to HRT through the Ryan White program would address a primary health care need as well as improve HIV outcomes for a population at high risk. However, the Ryan White program fails to ensure coverage for hormone replacement therapy medications under its AIDS Drug Assistance Program (ADAP). The program, funded under Part B of the Ryan White legislation, is a lifeline for the more than 200,000 Ryan White clients nationwide, including 20,000 in Florida, whose medications are covered by ADAP, either directly or through assistance with insurance premiums or medication costs. Importantly, ADAP covers more than just anti-retroviral medications for people living with HIV. ADAP regulations establish minimum criteria that require state formularies to 1) include at least one medication from each class of anti-retroviral medication, 2) be FDA-approved, 3) be consistent with HHS Adult HIV/AIDS Treatment Guidelines, and 4) be available on an equitable basis to all ADAP clients within the jurisdiction.[191]
Consistent with this criteria, ADAP formularies in all 50 states cover some number of medications in addition to anti-retroviral medications, including drugs for co-occurring infections, anxiety and depression, hepatitis C, and other conditions for patients living with HIV. As stated by the National Association of State and Territorial AIDS Directors (NASTAD), an organization that issues a major annual analysis and evaluation of ADAP programs nationwide, “ADAP’s inclusion of treatment medications for co-occurring needs demonstrates a commitment to addressing the full physical and mental health of the clients they serve.”[192]
Ryan White program data indicates that approximately 1 percent of ADAP clients are identified as transgender, yet coverage of hormone replacement therapy for trans patients is limited.[193] In an issue brief addressing ADAP policies regarding transgender patients, NASTAD highlighted the importance of adding gender-affirming hormone medications to state ADAP formularies:
Medication adherence among transgender people is heavily dependent on the availability of gender-affirming health services and continued hormone therapy. Although the extent to which members of the transgender community may avail themselves of various gender-affirming health services changes by the individual’s experience, it is integral for ADAPs to assess plans to include coverage of care and treatment for the needs of transgender people.[194]
According to NASTAD, 29 states provide some hormone medications on their formulary, but only 21 states designate those medications for use in gender transitioning, an important distinction in several respects. Florida has a state drug formulary and formularies that apply in its Part A jurisdictions (for urban areas with high HIV prevalence, including Miami-Dade and Broward counties). The state and the Part A formularies list some hormone medications, but many of the medications used for gender transition are missing.[195] None of the formularies indicate that these medications are designated for gender transition treatment rather than to address wasting, weight loss, and other conditions in cisgender people resulting from HIV or AIDS. This is an omission that limits awareness on the part of patients and providers that these medications could be covered by ADAP and results in unnecessary denials from insurance companies.[196]
When asked about the failure to include HRT on ADAP formularies, federal officials referred Human Rights Watch to the state ADAP program.[197] The federal regulations do leave to the states discretion to add medications for co-occurring needs – but as NASTAD noted in its brief, HRSA has taken steps to encourage states to add certain medications such as hepatitis C treatment medications, and should do the same for hormone replacement therapies.[198] State officials also disclaimed responsibility, stating that they do not have jurisdiction over Ryan White Part A medication formularies as these formularies are administered by local county government.[199] This is another area where state leadership could establish a clear policy that would improve coverage and awareness of a vital component of HIV care for trans women in Florida.
Trans Women Face Barriers to Key HIV Prevention Medication
Pre-exposure prophylaxis (PrEP) is a combination of two medicines (tenofovir and emtricitabine) in one pill that, if taken every day, has demonstrated significant results in HIV prevention for people who are HIV-negative. This key biomedical intervention has been shown to reduce the risk of getting HIV from sex by as much as 90 percent. If combined with other prevention methods such as condoms, the risk of acquiring HIV can be even lower.[200] Federal agencies tasked with reducing new HIV infections have made increased awareness of and access to PrEP a top priority. The CDC, HRSA, SAMHSA, and other agencies have called for a 500 percent increase in access to PrEP by 2020. A framework document outlines a broad array of federal initiatives intended to raise awareness, provide technical assistance and training for medical personnel and fund community-based and public health departments to provide PrEP to groups at high risk of HIV.[201]
Trans women are one of the groups at highest risk for HIV in the US. Yet attention to transgender people in both research and distribution of PrEP has been limited and taken a back seat to a focus on men who have sex with men (MSM). The first clinical trial of PrEP, published in 2010, included both MSM and trans women and was the only study with confirmed enrollment of trans women; other clinical trials for MSM are open to trans women but enrollment levels are unclear.[202] Overall, the study showed 44 percent decrease in risk of HIV acquisition, but no decrease among trans women.[203] The failure of the first PrEP study to show a decrease in risk for trans women has been attributed primarily to lack of adherence to the daily medication regimen; negative interaction of PrEP with hormone medications was not observed but requires further study.[204]
Federally funded projects that distribute PrEP through community organizations and public health entities also show very low participation of trans women.[205] The first CDC guidelines for prescription of PrEP by medical providers, issued in 2014, did not mention transgender women at all; the updated guidelines, issued in 2017, note lack of research into efficacy of PrEP for trans women but recommend that they be included in consideration for PrEP as a group at high risk of HIV from sexual transmission.[206] In 2015, CDC published a report finding that PrEP would be an indicated prevention for 1.2 million people at high risk for HIV, but this report addressed only MSM, cisgender heterosexual women and people who inject drugs, failing to make any mention of transgender people.[207]
PrEP has tremendous potential to make a difference in lowering new HIV infections for trans women. In a 2016 study in San Francisco, knowledge of PrEP was low but once introduced to it, interest among trans women was strong.[208] But trans health experts emphasize that PrEP implementation guidelines must consider and address trans women’s unique barriers and facilitators to uptake and adherence. On the ground, integration of PrEP distribution with gender-affirming health care is fundamental to successful uptake of PrEP among trans women. One trans health expert put it bluntly:
Gender-affirming providers and clinic environments are essential components of any sexual health programme that aims to serve trans women, as they will largely avoid settings that may result in stigmatizing encounters and threats to their identities.[209]
Race is another barrier to PrEP access and represents another burden for trans women of color seeking to access PrEP.
Federal efforts to increase access to PrEP have been incomplete and problematic even for the groups it prioritizes, with evidence of wide racial disparities in coverage for MSM, heterosexual women and people who inject drugs. According to the CDC, of the estimated 1.2 million people who are in need of PrEP, 69 percent are people of color; 44 percent are Black and 25 percent, Hispanic. However, only one percent of Black people who need it are on PrEP, creating what CDC has called “an urgent” need to increase PrEP coverage for this population, noting that most Black people who are in need of PrEP, but not taking it, live in the US South.[210]
HRW survey results in south Florida indicate that awareness of PrEP was high among participants – 82 percent of survey participants indicated that they were familiar with PrEP. But few women were taking PrEP: of those who were HIV-negative, only ten percent were on PrEP, with 62 percent of participants indicating they “didn’t need it” and 19 percent (nearly one of four) stating they “did not know enough about it” to take it. Other reasons given for not taking PrEP included cost issues, too much stigma, and mistrust, with one woman stating, “I don’t want to be part of an experiment.”[211] Need for PrEP, however, was demonstrated; of survey participants who were HIV negative and not taking PrEP, 38 percent said they have exchanged sex for money, drugs, or life necessities in the last year.
In 2016, Florida began a campaign to increase access to PrEP as part of a plan to reduce new HIV infections. The State Surgeon General issued a mandate that by the end of 2018, PrEP should be available at no cost in each of the 67 county health departments. As part of this campaign the state made efforts to increase education and infrastructure to distribute PrEP, compiled a resource guide and directory for sites that offer PrEP statewide, made PrEP available through the central pharmacy system that serves state Medicaid and Medicare patients, and launched targeted social media campaigns aimed at increasing PrEP awareness among minority populations.[212] A series of intensive PrEP training courses were presented in partnership with the University of California at San Francisco (UCSF) and other organizations throughout 2018 with the goal of reaching every county health department as well as providers and interested community organizations in that area.[213] According to Dr. Jonathan Fuchs of USCF, Florida’s effort to make PrEP available in all county health departments is broader and more ambitious than in any other state, and the commitment from Florida Department of Health has been exemplary. Fuchs described the training curriculum as including substantive components on the experience of transgender women and the issues they may face in relation to PrEP.[214]
The campaign, supported primarily with state funds, has already achieved significant results. As of May 2018, 37 of 67 county health departments, including Miami-Dade and Broward counties, were implementing a PrEP distribution program. Between July 2017 and April 2018, the number of PrEP clients served by county health departments has increased from 18 to 632.[215]
The state provided no data on how many trans women were enrolled in these programs, however. Both Miami-Dade and Broward county health departments have created PrEP programs as part of this statewide campaign, but transgender participation in both of these programs remains low.[216] In Miami-Dade County, Dr. Susanne Doblecki-Lewis is one of the medical advisors to the county PrEP program. Dr. Doblecki-Lewis said that the PrEP clinic at the department of health does not have many trans women clients. She attributed this to many factors, including the cost of PrEP and mistrust of a health department setting. “Health departments may not provide the most comfortable environment for trans women.”[217]
The Miami-Dade program has made efforts to increase the participation of trans women, specifically by engaging a local and trusted community organization that provides a variety of services to trans women to encourage referrals to the county program. According to state HIV officials, the involvement of Survivor’s Pathway, which is located near to the department of health PrEP clinic, has increased trans women’s engagement, though no data was provided regarding trans participation in the program.[218]
In Broward County, the department of health PrEP program hired Regina Gerbier, a trans woman, to act as Coordinator of Transgender Programs for the HIV Prevention unit. According to Ross, trans women’s participation in the PrEP program remains low, again as a result of numerous factors including reluctance to engage with a county health department, low knowledge of PrEP, lack of “readiness” for PrEP and cost barriers. According to Gerbier:
PrEP is not a pill, it is a program. It requires someone to see a doctor every three months to get labwork. This is a commitment, and it is expensive if you don’t have insurance.[219]
Cost is a major barrier to PrEP roll out nationwide, as a one month course of PrEP can cost up to $2000 per month for the uninsured.[220] The Ryan White and ADAP programs do not cover it as they serve people already living with HIV. Primary sources of funding for the medication are limited to donations from the manufacturer and as in the case of Florida, states themselves. Gilead Pharmaceuticals, the manufacturer of Truvada, will subsidize PrEP coverage for six months for those who meet low income requirements, but one must re-apply every six months. “Even for trans women who do want to take PrEP, paying for it is still a problem. I spend a lot of my time trying to help women find a place they can get it paid for,” said Gerbier.[221]
Insurance coverage, including Medicaid, has been found to significantly increase PrEP participation and adherence.[222] Medicaid covers PrEP, but in states like Florida that have not expanded Medicaid, access remains limited for low income people. Dr. Doblecki-Lewis has conducted numerous clinical trials involving PrEP accessibility and found lack of insurance coverage in Florida contributes to lower PrEP adherence compared to that in other locations. Dr. Doblecki-Lewis stated, “In Florida, Medicaid expansion would make a huge difference to PrEP access-given their socio-economic status, it would be very important for trans women.”[223] For trans women, availability of Medicaid would alleviate some of the cost concerns as well as provide options for finding PrEP outside of county health departments, sites where they may not feel safe or comfortable.
In Broward County, PrEP availability for trans women has begun to improve, according to Misty Eyez who provides many referrals for trans women to HIV prevention and care services through Sunserve. In the spring and summer of 2018, two health clinics began to offer PrEP to people without insurance, and most importantly, they also offer hormone replacement therapy at no or low cost to PrEP patients who are transitioning. Eyez stated, “This is the model that works for trans women. If they can get their hormones at the same time, they are much more likely to go. However, some of these clinics already have waiting lists, creating long waits for an appointment.[224]
In June 2018, Broward County Health Department took steps to address cost issues by establishing a PrEP partnership with the AIDS Healthcare Foundation (AHF) in Fort Lauderdale. AHF will provide patients with an immediate supply of PrEP medication as well as cover the cost for doctor visits and labwork. The ability of Broward County to refer clients to a no-cost clinic has significantly increased participation in the PrEP program – between June and August 2018 more than 300 patients enrolled in the program, more than during the entire previous year before the no-cost option became available. Participation by trans women, however, remains low – only a handful of these new AHF patients are trans women.[225] AHF does not provide hormone replacement therapy as part of the PrEP program, and Gerbier heard feedback that some trans women had bad experiences there in the past. Gerbier hopes to address these issues in the coming months, including by launching a social media campaign to make sure than trans women know about the new program and provide reassurance that it is trans-friendly.[226]
|
Latina Trans Women and HIV Latina trans women share many of the social determinants of health with Black trans women that place both groups at higher risk for HIV than their white counterparts, including higher rates of poverty, lack of insurance, pervasive intersectional discrimination, unemployment and involvement in the criminal justice system.[227] However, Latina trans women often face unique circumstances that impact access to health care and increase HIV risk. Chief among these are language barriers, lack of awareness of social services and, for undocumented immigrants, avoidance of health care services due to fear of deportation.[228] Each of these factors impact HIV risk for Latina trans women in Florida, a highly diverse state where three-quarters of immigrants originate from Mexico, Central America and the Caribbean.[229] HIV disparities are significant among Latinx people; despite comprising 18 percent of the US population, Latinx people represent one quarter of those living with HIV.[230] New HIV infections continue to increase among young Latino men who have sex with men, a category that often incorrectly includes trans women. Latinx people are more likely to delay HIV testing, to receive an AIDS-related diagnosis once tested, and to die within one year of HIV diagnosis than non-Latinx African-Americans or white populations.[231] In the Human Rights Watch survey, Latina trans women comprised 41 percent of participants. Survey results indicated that Latina trans women surveyed were more likely to be HIV-positive than non-Latina respondents, but if HIV-negative, were more likely to be on PrEP. They were insured at the same rate—45 percent—as non-Latina participants, but were more likely to be unemployed, more likely to have engaged in sex work, and more likely to have been arrested. Francesco Duberli is Executive Director of Survivors’ Pathway in Miami, an organization providing social, psychological, legal and other support services to the LGBT and Latinx communities. According to Duberli, “Trans Latina women are under many pressures and for most of them HIV is not their primary concern even though they are at risk. Immigration issues, poverty, domestic violence, and human trafficking are all common stressors for our clients.”[232] Survivors’ Pathway in Miami-Dade County and Arianna’s Center in Broward County work closely with the Florida Department of Health to provide HIV testing and linkage to PrEP, programs that are helping to address HIV risk in the Latinx trans community and should be expanded. |
Lack of Data Impedes Government Response
For trans women living with HIV, the legal and policy environment is worsening, but has long been characterized by government neglect. The clearest example of this is the failure for decades of federal and state governments to collect accurate data related to HIV infection among the transgender population. Accurate data collection on HIV among specific populations is vitally important to developing effective government funding and support for prevention, treatment and services related to HIV. As stated by one evaluator of the federal HIV data collection system, this information is used for “allocation of funding, program evaluation, and as a driver for public health action.”[233]
Since 1981, the federal Centers for Disease Control (CDC) has collected data on a multitude of aspects of the HIV epidemic including incidence (new infections occurring), prevalence (how many people are living with HIV), modes of transmission, deaths from AIDS and other categories. There are numerous sources for this information: the National HIV Surveillance System (NHSS) is the primary source, supplemented by other programs such as the Medical Monitoring Project (funded in approximately 30 states to collect data on people living with HIV who are in care) and the Behavioral HIV Surveillance System that gathers information on specific populations at risk for HIV such as people who inject drugs and men having sex with men.[234]
All states and territories require HIV diagnoses to be reported to the local health departments and this information is then provided to the state.[235] States receive HIV-related information from a variety of sources – clinical reports, lab tests, death certificates, and other documents. This information is transferred into a standardized database called eHARS (electronic HIV/AIDS reporting system), available to all states for the purpose of reporting this information to the CDC.[236]
For many decades, transgender people were invisible to the national and local HIV surveillance system; to the extent that data was collected for transgender women, they were incorrectly grouped into the category of “men who have sex with men.” It was not until 2009 that states had the option to submit “current gender identity” as well as “male” and “female” into eHARS. In 2011, the CDC reporting forms used to transfer information into eHARS were revised and eHARS fields were updated to reflect current gender identity as well as sex assigned at birth. In 2012, the CDC issued its first guidance document to states regarding this two-step process for more accurate collection of data regarding transgender persons and this guidance was updated in 2015.[237] The guidance emphasized the importance of utilizing numerous sources for identification of transgender people among those reported to be living with HIV; for example, state surveillance staff should attempt to flag discrepancies between the sex assigned at birth on a birth certificate and the information recorded on the standardized reporting form in order to make an accurate input of gender identity into eHARS.[238]
However, state implementation of these optional guidelines varies widely; 26 states provide no publicly available surveillance data relating to HIV among transgender people. Numbers that do exist are likely to be grossly underestimated. A 2015 analysis of national surveillance HIV data for transgender persons during the years 2009-2014 found that, “Diagnosed HIV among transgender populations may be vastly underestimated or misclassified due to data collection challenges for jurisdictions, including correctly identifying current gender identity from documentation in medical records and other data sources.”[239]
The absence of data related to HIV among transgender people is a nationwide problem, not limited to the state of Florida. The CDC has stated that, “Because there is no reliable system for collecting and sharing sex and gender identity information in health records, our nation currently lacks reliable HIV surveillance data for transgender populations.”[240] Largely ignored as an issue for decades, the National HIV/AIDS Strategy Updated for 2020 acknowledges that transgender HIV data is so scarce that the federal government has no way to systematically evaluate the collection process or the data itself, and recommends that such an “indicator” be developed.[241] Collecting data and developing such an indicator are essential first steps, but without more urgent and coordinated attention from federal policymakers it is a goal that will remain out of reach, leaving transgender women at a huge disadvantage in funding, programming and support for HIV prevention and care.[242]
Incomplete Data Collection in Florida
A key factor hindering Florida from implementing an effective HIV policy for trans women is lack of accurate and complete data. Without knowing how many trans women are living with HIV, where they are located and to what extent current programs are effectively serving trans women and identifying unmet need, Florida trans women will continue to navigate a fragmented and inadequate health care system for both HIV prevention and treatment.
Florida officials have emphasized that accurate data and surveillance information is key to the state’s HIV response:
The Department of Health, Bureau of Communicable Diseases, HIV/AIDS Section collects, analyzes and disseminates surveillance data on HIV infection. These surveillance data are one of the primary sources of information on HIV and AIDS in Florida. For instance, HIV and AIDS surveillance data are used by the Department’s public health partners in local health departments, federal agencies, non-profit organizations, academic institutions, and the general public to help focus prevention efforts, plan services, allocate resources, and monitor trends in HIV infection.[243]
According to the Williams Institute, an estimated 100,000 transgender people reside in the state of Florida, largely located in Broward, Miami-Dade, Orange, Pinellas and Hillsborough counties. The Williams Institute estimate indicates that 50 percent of trans people in Florida are white; 26 percent are Hispanic or Latino; 19 percent are Black, non-Hispanic and four percent fall into other racial or ethnic categories.[244] Yet transgender people are largely invisible in Florida state HIV surveillance data. In the most recent report publicly available, “The State of the HIV Epidemic in Florida 2017,” genders are limited to “male” and “female” for every component of the epidemic that is addressed in the report.[245]
The 2017 surveillance data does include one slide referencing transgender persons and HIV (see Table I) [246]:
According to this slide, there were 310 transgender people living with HIV in the state of Florida in 2017. The text at the bottom acknowledges the limitations of the information presented, both in gender identification and modes of transmission. State HIV officials told Human Rights Watch that their data on HIV among transgender persons is likely to be underestimated.[247] Also, this number is significantly lower than that shown in the Ryan White program report issued by HRSA showing 355 transgender clients enrolled in the Florida Ryan White program in 2016.[248]
The state data sets can only be as accurate as the information relied upon. As noted above, the CDC’s primary form for reporting HIV cases, the Adult Case Reporting Form (ACRF) has included a two-step gender identification question since 2013. But according to state officials, most information received is from providers and laboratories who may not provide accurate information on current gender identity.[249]
The state does monthly reviews of data in the eHARS system to identify discrepancies in gender reporting such as birth certificates that do not match the gender in medical records. But if medical providers, HIV testing and counseling sites, and other sources do not report accurately, gaps in eHARS will remain. Also, the state does not yet match the eHARS data with that from other databases such as the Ryan White system that uses a two-step gender process for patients, or ADAP records, other state electronic health records and other sources. According to state officials, these cross-database matches are planned but the timeline is unclear.[250]
In the meantime, the state’s information regarding HIV among trans people is incomplete and not reliable. For example, the state’s transgender data slide fails to accurately record how people acquired HIV. For 87 percent of male to female transgender individuals, the mode of exposure listed is “men having sex with men,” and the slide indicates that mode of exposure is categorized by sex assigned at birth. In order to distinguish modes of exposure for trans women from men who have sex with men, the CDC Guidance document for working with transgender data states that “transmission categories correspond to a person’s sex assigned at birth and therefore may not accurately describe the mode of transmission for a transgender person with diagnosed HIV infection.” The Guidance recommends that states consider using alternative categories such as “sexual transmission” instead of “male to male sexual contact” or “heterosexual contact.”[251] Ryan White providers are utilizing this category; the 2016 Ryan White report indicates “sexual contact” as the mode of transmission for 97 percent of transgender Ryan White clients in Florida, but the state has not yet matched its eHARS database to the Ryan White data to capture this information.[252]
Perhaps most important is state surveillance data indicating health outcomes for trans people with HIV. Nationally and statewide, public health decisions are made based upon HIV surveillance data known as the “continuum of care” — a chart that shows how many people diagnosed with HIV are in medical care, stay in medical care, and become virally suppressed. Continuum of care data are typically shown in the aggregate as well as broken down by race, gender, age and mode of transmission. The most recent continuum of care for the state of Florida shows that statewide, 93 percent of people diagnosed with HIV were in care at one time, 68 percent have been retained in care, and 62 percent are virally suppressed (see Graph IV).[253] In 2016, of people living with HIV who are out of care, 73 percent were identified as male, and 27 percent as female; 40 percent were Black, 26 percent were White, and 23 percent were Hispanic.[254]
Continuum of care data for trans women is important as they are a population that is likely to be lost to follow up. Given their difficulty in accessing health care, their frequent failure to return to care after a bad health care experience, and lower rates of adherence to HIV medications than other groups, trans women are at high risk of falling out of HIV care and not achieving viral suppression.[255] Outcomes are likely to be particularly poor for African-American trans women; in Florida, African-Americans are less likely than either whites or Hispanics to be linked to care, to stay in care, and to achieve viral suppression.[256] Lack of accurate transgender data hinders the state’s ability to address these issues among trans women of color.
In 2017, the state reported that of the 300 transgender women living with HIV in the state of Florida, 79 percent were in care at one time, 69 percent were retained in care and 58 percent had achieved viral suppression or an “undetectable” viral load.[257] In 2016, the most recent data available show that in Miami-Dade County, there are 53 trans women identified as living with HIV; 70 percent are said to be in care, and 66 percent have achieved viral suppression. In Broward County, 43 trans women are identified as living with HIV; 72 percent are retained in care however, viral suppression is only 47% (see Graphs V[258], VI[259], VII[260]).
Given the limitations on data collection for trans individuals in Florida, the numbers of trans women living with HIV are likely to be significantly underestimated. This data shows that high numbers of trans women are initially engaging in care, but significantly fewer women remaining in treatment and achieving viral suppression. This reflects the larger problem of retention in care that is occurring at the state and national levels for people living with HIV. However, Florida may be missing opportunities to obtain valuable information to supplement their surveillance data to learn more about why trans women may be lost to care.
For example, Florida has a specific program dedicated to identifying people who have been diagnosed with HIV but fallen out of care. The “Data to Care” Program is a federally funded initiative for states to use multiple data sources to identify, contact and support persons with an HIV diagnosis who are not in care. In 2017, 20 percent of people identified in Florida through this program were connected to medical care. The state tracked the percentage of males and females in the program and showed that those most likely to drop out of care are Black men, but there is no data on transgender clients.[261] State HIV officials told Human Rights Watch that any transgender persons identified as out of care or never linked to care would be “added automatically to our Data To Care lists for linkage/ re-engagement” and that “as we work to improve and automate the D2C process, we constantly evaluate priority populations including Transgender persons who need linkage/re-engagement services.”[262] Yet the state provided no information about how many transgender people had been identified as out of care as part of the Data To Care program or the results of any evaluations conducted.
Another missed opportunity occurred in a retention in care study in Miami. In 2017, the Miami-Dade County Department of Health, concerned about high rates of people dropping out of Ryan White programs, undertook a study to examine retention issues. However, according to the state, “a separate retention analysis for transgender clients was not undertaken due to too few clients being represented in the sample. Analysis found lower retention rates among Blacks/African-Americans.”[263] Despite evidence indicating that trans women of color are at high risk of dropping out of care, trans individuals were excluded from this study. This illustrates the circular and problematic “too small to be included” argument that impedes many efforts to address a grossly disproportionate HIV burden among a population whose numbers are acknowledged to be underestimated.
In Broward County, the Department of Health called the lack of information on HIV among the county’s trans population “horrible – we have very few pieces of the puzzle,” and explained that lack of data leads to lack of targeted programs, a vicious cycle that impedes their ability to address the needs of a vulnerable population.[264] Broward County officials said they had conducted trainings for two-step gender identification for HIV testing and care providers funded by Ryan White or by the state or county health departments, but those not funded were considered to be out of their control.[265] They expressed a strong desire to improve the situation, describing plans to partner with Florida International University to conduct community-led research into how to improve HIV data collection in an effective, culturally competent manner.[266]
Trans and HIV advocates in Florida frustrated with the lack of progress on data collection at the federal and state levels are taking steps to address it. Jen Laws, a health policy consultant and member of the state HIV Comprehensive Planning Network (FCPN) told Human Rights Watch, “We are tired of excuses, and the data the state is presenting is obviously flawed and incomplete. But the lives of trans people are at stake.”[267] Laws and other trans advocates are moving ahead on their own – at a statewide planning meeting in April 2018 several trans members of FCHN presented data estimating more accurate numbers for trans people living with HIV in the state of Florida. This data was developed using a synthesis of available information on national and state estimates of transgender population, the national transgender survey, Florida population-level data on race and ethnicity, and epidemiological and HIV surveillance data from the state of Florida. Based upon these sources, Laws estimates that between 1,404 and 2,808 transgender people are living with HIV in Florida, five to ten times more than the 291 reported by the state of Florida Department of Health (see Graph VIII).[268]
The Florida Department of Health has expressed concern about the accuracy of these much higher estimates; the complete text of their response to these estimates is included in this report as Appendix A. Health officials and advocates agree, however, that current data attempts to quantify HIV among transgender people in Florida are incomplete, likely to be inaccurate and need to be improved.
HIV data collection is challenging, requiring synthesis of information received from hundreds, and in states as large as Florida, thousands, of independent and varied sources. Reporting systems are not uniform, and the state is taking some steps to address it. But the stark reality is that for a group known to be one of the most heavily burdened with HIV, neither the federal government nor the state of Florida has accurate, complete data on how many trans people have HIV, how they got it, how many are in medical care for it, and the effectiveness of such treatment. Thirty-plus years into the epidemic, lack of information continues to jeopardize the health, and lives, of a group known to be at high risk of HIV.
Criminal Justice Involvement Increases HIV Risk
Trans women experience high rates of incarceration, with one in five trans women reporting having been in jail or prison.[269] The rate of incarceration for African-American trans women is three times higher than for white trans women – some studies indicate that half of African-American trans women report a history of incarceration.[270] This experience was reflected in the surveys conducted by Human Rights Watch; 40 percent of trans women surveyed reported having been arrested at least once. Seven women reported being arrested five to ten times, and one woman reported more than 20 arrests. Nearly half (49 percent) of survey respondents said they had exchanged sex for money, drugs, or life necessities in the last year. Of these, 38 percent said they had been arrested for sex work. The survey indicated racial disparities, with white women reporting higher income, significantly less engagement in sex work and fewer arrests than their African-American or Latina counterparts.
The evidence continues to increase that involvement in the criminal justice system at every stage carries negative health consequences, particularly for LGBT individuals. Even short jail stays have been linked to negative health outcomes. Harassment and abuse at arrest and during pre-trial detention, lack of access to medical care while incarcerated, and the impact of a criminal record on employment and housing stability contribute to health disparities for members of minority and LGBT communities.[271] Incarceration also has been found to increase poverty, a major barrier to access to health care for trans women.[272]
Human Rights Watch has documented police harassment of trans women and profiling them as sex workers in major US cities, as well as police harassment for carrying condoms, which can be considered evidence to support prostitution charges.[273] In the Human Rights Watch survey conducted for this report, one third of those engaging in sex work reported harassment by police for carrying condoms and 43 percent reported harassment by police for other reasons. One woman described a recent experience in Miami when she was attempting to take an Uber and the police surrounded her, examined her purse, and said she was “prostituting.” They called her a “puta” and said they would arrest her if they saw here around there again.[274]
Violence from clients increases HIV risk for sex workers, but fear of the police often leaves them without assistance. Of the women who exchanged sex for money, drugs or life necessities, half had been threatened or assaulted by clients, but only 15 percent called the police. One woman reported having been drugged and raped by a client in Miami, but never went to the hospital or called the police, saying she “did not feel safe” and expected to be harassed.[275]
Incarceration creates numerous barriers to HIV prevention and care – condoms are not available in the majority of prisons and jails in the United States; as Human Rights Watch has documented, access to HIV medications and treatment is often inadequate or in many jails, non-existent and linkage to medical care upon re-entry is uneven at best.[276]
In addition to incarceration itself as an HIV risk factor, transgender women experience alarming rates of sexual assault in prison. According to federal data for 2015, more than one-third of trans women reported assault by other prisoners or staff.[277] African-American and Latina trans women are more likely to be victims of assault in jail or prison than their white counterparts.[278] Most prisoners were HIV-positive prior to their incarceration. However, lack of HIV prevention measures and failure to provide safe environments for trans prisoners – such as the widespread practice of placing trans women in male prison facilities – increases HIV risk in correctional settings.[279] Of the women surveyed by Human Rights Watch who had been jailed in Florida in the last year, 10 of 15 reported having been placed in a male facility; 6 of 10 reported abuse from jail staff and five reported abuse from other prisoners.
The Prison Rape Elimination Act (PREA) is a federal law, passed in 2003, that established standards for US prisons and jails for protection of prisoners from assault while incarcerated.[280] In 2012, the Department of Justice issued detailed guidelines for determining a gender-appropriate and safe housing assignment for trans and gender non-conforming prisoners, but these guidelines are non-binding and not implemented in many of the nation’s prisons and jails.[281] The Trump administration has changed those guidelines to weaken consideration of gender identity in making housing determinations, an act challenged by advocates as undermining the purpose of the PREA legislation itself.[282] Both Miami-Dade and Broward County Jails have adopted PREA-mandated procedures for placement of trans prisoners, but survey responses and interviews with trans women indicate that concerns about safety remain. One woman wrote about her experience in two Miami jail facilities, “When I was arrested, they put me alone. Even times I was placed alone I was still harassed by inmates and staff.[283]
In Broward County Jail, most LGBT prisoners are placed in a separate “pod” where meals, activities, and recreation occur without encountering the general population. According to jail officials, the jail is organized into “pods” for all prisoners and there are no restrictions or limitations that result from placement in the what they call the “fragile” pod.[284] One trans woman, however, told Human Rights Watch that her experience in Broward County Jail in February and March of 2018 was “a nightmare.” According to Savannah Cash, it began at intake when they would not recognize her California drivers’ license that indicated her full and legal transition to female. Because they had booked her years before into the jail as a man, they insisted on calling her by her “dead name” the entire 40-plus days she was there.
In the “fragile” pod, Cash says she was harassed by staff and other prisoners, placed in solitary confinement – a punitive method with potentially harmful consequences for mental and physical health – as a result of conflicts with one staff member who threatened her.[285] According to Cash the staff member called her “sir” continually and said to her ‘who do you think you are, you are a fucking man.’ Cash also experienced delays in receiving her previously prescribed hormone replacement therapy for much of the time she was incarcerated.[286] Her attorney told Human Rights Watch that during a legal visit, he observed staff “cat-calling her and wolf whistling” while she walked to meet him in the visitation room.[287] Since release, Cash is working with her lawyer on possible legal action and Broward Sheriff’s Office said they were unable to comment on the case.[288]
An arrest history or criminal record also carries negative consequences for trans women’s employment prospects. For a community experiencing pervasive discrimination and with many living in extreme poverty, this can be devastating. There are no federal laws explicitly protecting LGBT people from employment discrimination, and the Trump administration has generally been unwilling to read such protections into existing laws. In 2017, the Department of Justice adopted the position that Title VII’s prohibition on sex discrimination does not include sexual orientation or gender identity.[289]
Florida has no state legislation explicitly protecting against employment discrimination on the basis of sexual orientation or gender identity. The National Transgender Discrimination Survey indicated “alarming” rates of employment discrimination in Florida, where 81 percent of respondents reported having experienced harassment or mistreatment on a job, 46 percent reported not being hired, and 36 percent reported losing a job due to their trans status.[290] A 2017 report by the Williams Institute at UCLA School of Law found pervasive stigma and discrimination against LGBT individuals in Florida including employment discrimination.[291] Both Broward County and the City of Miami have local ordinances prohibiting discrimination on the basis of sexual orientation and gender identity.[292] However, many trans women told Human Rights Watch of their experiences with employment discrimination in south Florida. One woman lost her job at a Broward County academic institution within days of announcing her gender transition. Another woman was demoted at a computer company in Broward County and isolated from her work colleagues: “Imagine 1,000 people in a cafeteria and no one will sit by you,” she said. “Employment discrimination is trauma.”[293] Another said, “I am looking for a job but hear ‘the position has been filled.’ Also, they ask on the application ‘have you ever been known by any other name.’”[294]
In this difficult employment environment, a criminal record can be the end of job prospects altogether and it begins, and perpetuates, a cycle of engaging in sex work for many trans women in order to survive. Participants in the Human Rights Watch survey who had been arrested had lower incomes than those who had not. In Florida, prostitution is prohibited under a range of both misdemeanor and felony charges addressing solicitation as well as human trafficking.[295] Florida also imposes enhanced penalties for engaging in prostitution while knowingly HIV-positive.[296] Public health and HIV experts have found these and other laws criminalizing HIV exposure as unnecessary, stigmatizing and counterproductive in that they may discourage HIV testing and disclosure.[297]
Many of these laws, including those in the state of Florida, require no actual transmission of HIV, fail to account for current medical treatment that can eliminate any potential for transmission, and have been shown to be disproportionately enforced against people of color and sex workers.[298] Arianna Lint works with many trans women who engage in sex work and told Human Rights Watch, “The girls are aware of the laws about HIV and prostitution – they don’t want to get tested, and they don’t even want to get medications sometimes because they are afraid of felony charges.”[299]
In Florida, a criminal record also makes obtaining gender-affirming documentation from the state more difficult. For trans people, state-issued documentation that reflects their gender identity is fundamental to overcoming the obstacles they face in almost every area of life. A drivers’ license that shows a different gender than they are presenting can trigger negative encounters, keep one from getting a job, and lead to violence. In the national survey, one of three trans people reported experiencing physical or sexual assault, being asked to leave, or being denied benefits after showing a non-conforming identity card.[300]
In Florida, the law permitting name changes requires both a background check with fingerprints and disclosure of any conviction that has resulted in a suspension of civil rights.[301] Neither provision automatically disqualifies someone with a criminal record, but the statute grants wide discretion to the judge in case of a criminal record and trans women and their advocates described how having arrests or convictions for misdemeanors resulted in denials of name changes. Alisha Hurwood is an attorney at Broward County Legal Aid who assists trans people with changing their names and gender markers on state and federal documentation. “It is not a ground for automatic disqualification, but it makes it more complicated and gives judges an easy method to deny name change despite no reasonable grounds for denial.”[302] The background check and fingerprinting also costs $65 and obtaining certified dispositions of past criminal cases can cost hundreds of dollars. Clients who are represented by counsel can get assistance in applying for indigent petitions to waive these fees, but many trans women do not have lawyers or advocates to assist them. As the first crucial step in obtaining a drivers’ license and social security card with a marker that matches their gender identity, these can be daunting barriers in the gender transition process.
HIV officials both state and federal acknowledge sex work as a factor contributing to HIV risk for trans women. Inclusion of trans women in PrEP rollout efforts are based largely on recognition of high rates of engagement in sex work. But there is little reference in HIV planning or strategy documents to the role of the criminal justice system in increasing HIV risk for any of the populations that are at highest risk both for incarceration and for HIV – people of color, youth, LGBT persons, and people who use drugs. To the extent that criminal justice issues are addressed, they largely focus on ensuring linkage to HIV care at re-entry from jail or prison.[303] But this limited approach neglects the increased risk of HIV and other negative health outcomes that result from entering jail or prison in the first place.
Criminalization of adult, consensual sexual relations is incompatible with human rights protection for personal liberty and autonomy.[304] Human Rights Watch takes the position that this also holds true with regard to the commercial exchange of sexual services. In addition, Human Rights Watch has extensively documented the harmful consequences of criminalization, both globally and in the US.[305] Human Rights Watch also opposes criminal laws such as the Federal Online Sex Trafficking Act of 2018 that conflate human trafficking – a serious violation of human rights – with adult, consensual sexual relations.[306] Failure to make this critical distinction interferes with the right of sex workers to work safely and to advocate for their rights. Decriminalization of adult, consensual sex work, as well as repeal of criminal laws that enhance penalties for HIV exposure, would be important steps toward reducing the many HIV risks for trans women that result from incarceration. There is ample evidence to support public health arguments for criminal justice reform, both nationally and in the state of Florida.[307] In addition, support for Medicaid expansion, a program shown to reduce poverty, could improve economic conditions for trans women and reduce engagement in sex work as a necessity.
Human Rights Standards
For transgender women, socio-economic conditions combine with harmful or inadequate federal and state policies that undermine their human rights and contribute to an environment in which their risk of HIV infection is higher than among any other group. With a particularly devastating impact on African-American and Latina women, this is a public health crisis that federal and state governments are obligated under international law to address.
Right to Health
All people have the right to health, a principle established by numerous international instruments including the Universal Declaration of Human Rights (UDHR).[308] The UDHR, endorsed by all members of the United Nations, including the United States, and considered to be broadly reflective of customary international law, protects the right to health as part of the right to a “standard of living adequate for the health and well-being of one’s self and one’s family.”[309] The International Covenant for Economic, Cultural and Social Rights (ICESCR) establishes that medical care, necessary social services and housing are integral components of human dignity.[310] The ICESCR treaty has been ratified by 166 countries but not by the United States. The United States has signed, but not ratified, the ICESCR.[311]
In addition, the right to health is inseparable from provisions on the right to life and the right to be free from discrimination, protections included in the International Covenant on Civil and Political Rights (ICCPR), a treaty the United States has signed and ratified.[312] Article 26 of the ICCPR states, “All persons are equal before the law and are entitled without any discrimination to the equal protection of the law. In this respect, the law shall prohibit any discrimination and guarantee to all persons equal and effective protection against discrimination on any ground such as race, colour, sex, language, religion, political, or other opinion, national or social origin, property, birth or other status.”[313] Authoritative treaty bodies as well as UN special rapporteurs and other international legal experts interpreting this provision have determined that it prohibits discrimination on the basis of sexual orientation and gender identity.[314]
The right to health does not guarantee to everyone the right to be healthy. Rather, it obligates governments to enact policies that promote the availability and affordability of basic health care services, without discrimination against those most likely to face obstacles to access – the poor, minorities, LGBT persons, women, prisoners, people with disabilities, and others.[315] The Trump administration has promoted policies that would have the opposite impact, attempting to repeal and undermine the Affordable Care Act without an adequate replacement, reducing the reach of Medicaid programs and turning away from interpretations of existing federal laws and regulations that would protect LGBT individuals from discrimination. As of October 2018, the Trump administration was moving ahead with plans to expand the grounds for religious and moral objections to providing health care services.[316] Without adequate provisions to ensure protection against discrimination, these and other Administration moves are likely to worsen pervasive and well documented discrimination against LGBT people in access to health services.
A key component of promoting affordability and availability of health services for transgender people is ensuring access to transition-related care. Under the Yogyakarta Principles, a set of non-binding standards endorsed by international legal experts from 25 countries that apply existing international human rights law to sexual orientation and gender identity, states are obligated to protect LGBT persons from discrimination in health care settings. This obligation includes “ensuring that gender-affirming health care is provided by the public health system or, if not so provided, ensuring that such services are covered under private and public insurance schemes.”[317]
Right to Be Free from Racial Discrimination
The federal, state and local governments in the United States are obligated to address all forms of racial discrimination, including the stark disparities that characterize the domestic HIV epidemic. This duty is fundamental to upholding international human rights law, including the ICCPR and the International Convention on the Elimination of All Forms of Racial Discrimination (CERD).[318] CERD, to which the United States is a party, requires governments, when circumstances warrant, to take “special and concrete measures” to ensure the development and protection of racial groups “for the purpose of guaranteeing them the full enjoyment of human rights and fundamental freedoms.”[319]
CERD obligates governments to address not only intentional racial discrimination but laws, policies and practices that result in disparate racial impact.[320] The UN Committee on Racial Discrimination, the international expert body responsible for interpreting the ICERD, has expressed its concern that the United States lacks appropriate mechanisms for implementation of the treaty at the state level.[321]
Right to an Adequate Standard of Living
The Universal Declaration of Human Rights states:
Everyone has the right to a standard of living adequate for the health and well-being of one’s self and one’s family, including food, clothing, housing and medical care and necessary social services, and the right to security in the case of unemployment, sickness, disability, widowhood, old age or other lack of livelihood due to circumstances beyond his control.[322]
Disproportionately, trans women struggle to secure access to many of these basic necessities. Living in extreme poverty keeps many trans women on the margins of society and vulnerable to violence, stigma and discrimination. Circumstances beyond their control – including numerous federal and state policies – contribute to this condition, including lack of legal protection against discrimination in employment, health care and public accommodation. Health care policies that reduce access to care for low income people and criminal laws that make it more difficult to find a job expose trans women to the harms of arrest and incarceration and reduce their ability to seek HIV prevention and care.
The state of Florida’s continued rejection of expanded Medicaid coverage is a key policy decision that helps to entrench these grim realities. In his report on the United States, the UN Special Rapporteur on Extreme Poverty and Human Rights documented the “shocking” extent of extreme poverty in the US and criticized federal and state health care policy to undermine and restrict the Affordable Care Act. [323]
Acknowledgements
This report was researched and written by Megan McLemore, senior health researcher at Human Rights Watch.
It was reviewed and edited by Diederik Lohman, Health and Human Rights Division director; Brian Root, senior qualitative analyst; Jasmine Tyler, US Program Advocacy Director; Amanda Klasing, Women’s Rights Division senior researcher; Ryan Thoreson, LGBT Program researcher; Chris Albin-Lackey, senior legal advisor; and Babatunde Olegboji, deputy program director.
Delphine Starr and Cara Schulte, program associates; and Fitzroy Hepkins, administrative manager, provided production assistance.
Freddy Gonzales and Jen Laws provided consulting services and Professor Jill McCracken of the University of South Florida advised on the survey instrument.
We thank the many individuals and community organizations who shared their expertise with us, helped us to identify research participants, and facilitated interviews, including Arianna Lint, Aryah Lester, Morgan and Ashley Mayfaire, Joey Wynn, Camille Lewis, Misty Eyez and Francesco Duberli, and Herb Sosa; Alisha Hurwood of Legal Aid Service of Broward County; Silvana Erbstein of AIDS Health Care Foundation; Cecilia Chung of the Transgender Law Center and Shannon Wyss of AIDS United who read and commented on a draft of this report.
We are especially grateful to the many courageous transgender women who shared their stories and participated in the survey for this report.