Summary
I thought I was going to die, not from the cancer, but from the pain.
— Marianna Hernandez, 58-year-old woman with liver and abdominal cancer, Guatemala City, December 2014
They are punishing the patient…. Life is difficult. Having cancer is even more difficult. Why do they have to make things harder?
—Dr. Eva Duarte, palliative care physician, Guatemala City, December 2014
Each year, an estimated 28,500 Guatemalans experience advanced, chronic illnesses, such as cancer; heart, lung, or renal disease; and HIV/AIDS. Many thousands of them will suffer significant pain related to their illness.
This pain can generally be treated well with inexpensive medications and eased with palliative care: a health service that includes treatment of pain but focuses on improving the overall quality of life of people with life-limiting illnesses.
However, a Human Rights Watch analysis has found that Guatemala’s lack of effort to ensure access to palliative care, regulatory barriers, and needlessly restrictive and complex regulations on controlled substances condemn many patients with pain to needless suffering, with devastating consequences for them and their families.
The 79 individuals interviewed—including 37 people with cancer or their relatives, and 38 health care workers—described extreme pain and other symptoms; struggles coping with a dim prognosis; visits to multiple doctors unable to adequately treat pain; and often lengthy travel on crowded buses to reach hospitals that offer pain treatment.
Gabriel Morales, for example, endured a journey for more than seven hours every 10 to 15 days on public buses to get pain medications for abdominal cancer in Guatemala City. He said:
I would wake up at 1 a.m., walk about half a kilometer, and catch the 2:30 a.m. bus. I would get to the boundary of Guatemala City around 8 a.m., where I would take a second bus to the center of the city.
Opioid analgesics, such as morphine, are essential for treating moderate to severe pain that cancer and other diseases cause. Yet because they are derived from the poppy plant—the source of opium—they are considered to be controlled substances. National and international law requires that countries strike a balance between ensuring that people with legitimate medical need can access opioids and preventing their misuse.
However, our review of Guatemala’s drug control system and interviews with health care workers reveal a system almost myopically concerned with controlling these medicines with little consideration for patients. Among our findings:
- Only four public or government-supported hospitals offer palliative care: all are in Guatemala City, although nearly 80 percent of the population lives elsewhere;
- Only 50 to 60 out of around 14,000 doctors in Guatemala have special prescription pads needed to prescribe morphine, all of whom work in Guatemala City;
- Only three pharmacies in the country, all in Guatemala City, consistently carry opioid analgesics.
Patients who ultimately manage to find a physician to treat their pain are the lucky ones: many more die under excruciating circumstances with no access to such treatment. Indeed, at least 5,500 Guatemalans with cancer and HIV/AIDS suffer annually due to barriers accessing low-cost opioid medications. With life expectancy and the percentage of the population over 65 both projected to rise, the burden of chronic illness looks likely to only grow. According to World Health Organization (WHO) data, an estimated 57 percent of all deaths in 2015 in Guatemala were due to non-communicable diseases.
“I mourn for all the patients I can’t see,” one doctor who provides palliative care said. “There are so many people who don’t have access to a doctor who can prescribe opioids or even someone to refer them to a doctor who can.”[1]
Restrictive Regulations
The 1961 Single Convention on Narcotic Drugs, the international treaty that forms the basis for the global response to drugs, states that the medical use of opiates continues to be “indispensable for the relief of pain and suffering” and that “adequate provision must be made to ensure the availability of narcotic drugs for such purposes.”
WHO includes morphine and several other opioid analgesics in its Model List of Essential Medicines, a roster of the minimum essential medications that should be available to all persons who need them.
As noted, countries are obligated to regulate the use of these medicines. The 1961 Single Convention sets out four basic requirements that national regulatory systems must fulfill:
- Only licensed individuals may handle and dispense these medications;
- The medications may only be transferred between authorized institutions or persons;
- Dispensing may only happen based on a medical prescription;
- Relevant records must be kept for at least two years.
The convention allows countries to impose further requirements if they feel these are needed, but, as WHO states, countries must take care that any additional requirements do not unnecessarily impede medical access.
Guatemala’s drug regulations are needlessly restrictive, inconsistent with both WHO and International Narcotics Control Board (INCB) recommendations and out of line with regulations in other countries in the region.
One internal medicine physician said: “I get mad at the system. I know what to do and how to do it, but they [the regulations] tie my hands….” Some health care workers told us that they knowingly violate regulations to help patients, risking disciplinary and criminal sanctions. For example, one physician said: “For us, there’s no choice [but to circumvent the regulations]. We’re in front of the patients. What else can we do but help?”
A number of hospitals have taken the unusual step of providing medicines for outpatients from their internal pharmacies, recognizing they will not have access to them if they do not.
Obstacles
The system also creates multiple, often insurmountable obstacles for physicians, pharmacists, and patients, including the requirement that:
- A physician use a special prescription pad that is needlessly difficult to obtain;
- Physicians must write a second prescription form for many patients;
- Patients must obtain a stamp to validate the prescription before a pharmacy can dispense the medications.
“None of the doctors outside Guatemala City have special prescription forms,” a palliative care physician in Guatemala City said. “It’s a lot of work to get it. They would have to come to Guatemala City and would lose a full day of work.” Referring to the requirement to validate prescriptions, a pharmacist said: “The patients are literally dying and in pain. I can’t send them to the [validation office] on a bus. I feel responsible to continue [dispensing] to them.”
These regulatory barriers mean that the use of opioid analgesics in Guatemala is very low: the amount of morphine used per year would be sufficient to treat some 3,000 (35 percent) patients with terminal cancer or AIDS per year if used exclusively to treat them. In reality, morphine is also used for acute pain in trauma cases, post-surgery, and other situations.
Failure to Reform
Palliative care physicians have repeatedly brought these challenges to the attention of the Guatemalan government. WHO, INCB, and other United Nations bodies have also repeatedly called on countries to remove regulatory barriers to the use of opioid analgesics. Most recently, in April 2016, the UN General Assembly Special Session on the World Drug Problem called on countries to consider reviewing “unduly restrictive” regulations and impediments “to ensure access to controlled substances for medical and scientific purposes, including for the relief of pain and suffering….”
WHO has urged countries to ensure that palliative care is integrated into all health care levels; to implement health and health financing policies to promote it; to ensure that health professionals are adequately trained; and to ensure the availability of palliative care medicines, such as opioid analgesics.
However, successive administrations in Guatemala have failed to carry out reforms needed to improve access of patients with life-limiting illnesses to opioid analgesics.
Although the Ministry of Health formally created a palliative care commission in December 2011, Guatemala still does not have a policy or strategy to develop palliative care and ensure it is available outside Guatemala City. The country’s only public medical school does not teach palliative care and pain management as part of its undergraduate curriculum; only one of the three private medical schools does.
Moreover, physicians specializing in oncology, internal medicine, and other areas of medicine that frequently care for patients with life-limiting illnesses do not receive any academic or clinical training in palliative care. Physicians specializing in anesthesiology have a two-month rotation in palliative care.
***
International human rights law requires the Guatemalan government to ensure that patients with life-limiting illnesses have adequate access to pain treatment and palliative care. Its failure to do so violates the right to the highest attainable standard of health and may violate the obligation to protect people from cruel, inhuman, and degrading treatment.
The government of Guatemala faces many complex health care challenges due to resource problems, inadequate infrastructure, shortages of medicines, and weak public health care services. Ensuring adequate access to palliative care for all Guatemalans who need it will be no easy feat. But the government has a real opportunity to make a significant difference in the lives of thousands of people by taking a number of low-cost, straight-forward steps to remove barriers to the provision of palliative care. A number of key steps, such as increasing the number of forms per prescription pad, can be taken immediately without any regulatory reform and would significantly improve access to palliative care for patients. Other changes would require regulatory reform.
In April 2016, at the UN General Assembly Special Session on the World Drug Problem, Guatemala’s President Jimmy Morales strongly emphasized the importance of ensuring that the health and well-being of humankind becomes the cornerstone of global drug control efforts.
Human Rights Watch believes that as part of its efforts to place health at the center of the domestic response to controlled substances, the Guatemalan government should reform its drug regulations and health policies to ensure patients who suffer from severe pain due to various life-limiting illnesses have adequate access to opioid analgesics and palliative care.
Key Recommendations
To the Government of Guatemala:
- Reform drug control regulations. Drug control regulations are needlessly restrictive; deter doctors and pharmacists from prescribing and dispensing opioids; and lead to unnecessary suffering for thousands of Guatemalans. Some of these issues can be addressed immediately and without regulatory changes; others require regulatory reform. The government can immediately increase the number of prescription forms per pad and allow physicians to have two prescription pads at once. It should amend its regulations to remove the dictamen requirement and abolish or at least modify authorization procedures. The Ministry of Health should hold an inclusive meeting of relevant stakeholders to inform them of these regulatory reforms.
- Ensure immediate-release oral morphine becomes available in every departmento of Guatemala. Ensure that there is at least one pharmacy in each departmento that stocks immediate-release oral morphine. Where no private pharmacies stock oral morphine, ensure that a hospital pharmacy dispenses oral morphine to outpatients.
- Develop a mandatory undergraduate curriculum in palliative care and mandatory clinical training in palliative care for doctors of certain postgraduate programs. San Carlos University, the largest and only public medical school in Guatemala, should develop a mandatory undergraduate curriculum in palliative care to ensure basic training in the discipline. Doctors of certain postgraduate programs who frequently treat patients with chronic illnesses—including oncology, pediatrics, and internal medicine—should be required to undertake rotations in palliative care units.
- Take steps to create pain and palliative care units in key departmentos. Identify key facilities countrywide to develop pain treatment and palliative care units. These could act as regional hubs for palliative care and expand palliative care services beyond Guatemala City. The facilities would allow for clinical rotations in palliative care, expanding the number of physicians trained in this health service.
Methodology
This report is based on research conducted between December 2014 and August 2015, including visits to Guatemala in December 2014 and July and August 2015. Field investigation was conducted primarily in Guatemala City. Additional research was conducted in Quetzaltenango. We also conducted extensive desk research regarding palliative care treatment availability in various other parts of the country.
Over a cumulative total of three weeks in Guatemala, a Human Rights Watch researcher conducted 79 interviews with a wide variety of stakeholders, including 37 people with cancer or their relatives; 38 health care workers, including oncologists, anesthesiologists, palliative care doctors, and pharmacists; and representatives of the Department of Regulation and Control of Pharmaceutical Products and Related Products.
Interviews with patients and their relatives were conducted at a variety of hospitals. They were conducted in private whenever possible. Interviews were semi-structured and covered a range of topics related to pain treatment and palliative care. Before each interview, we informed interviewees of its purpose; of the kinds of issues that would be covered; and asked whether they wanted to participate. We informed them that they could discontinue the interview at any time or decline to answer any specific questions, without consequence. No incentives were offered or provided to persons interviewed.
The identities of all patients, relatives, and health care workers interviewed have been disguised to protect their privacy, except when they specifically agreed that their real name could be used.
Most interviews were conducted in Spanish with the assistance of an interpreter. Some interviews were done in English.
All documents cited in the report are either publicly available or on file with Human Rights Watch.
I. Background
Importance of Palliative Care and Pain Relief
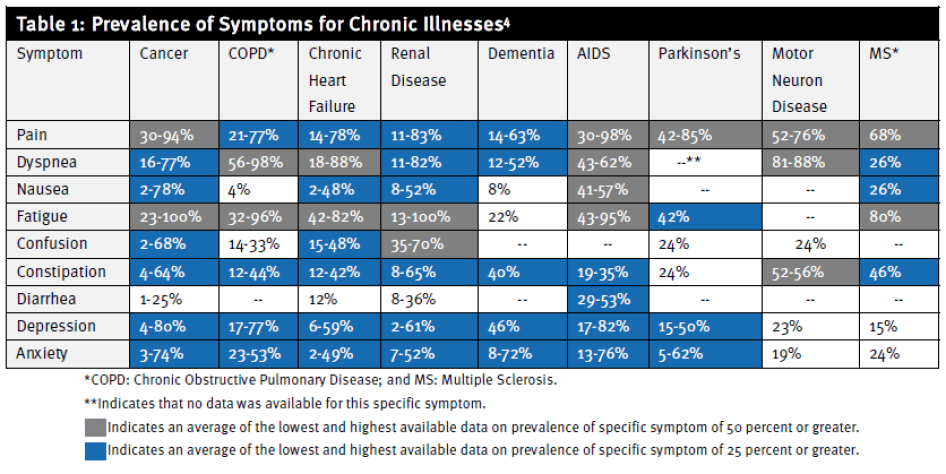
With life expectancy increasing worldwide, the prevalence of non-communicable diseases (NCDs) and chronic illnesses is rising rapidly.[2] NCDs—such as cancer, heart disease, diabetes, and respiratory illnesses—are by far the leading cause of mortality in the world.[3] They and other chronic illnesses are often accompanied by pain and other distressing symptoms, such as breathlessness, nausea, anxiety, and depression (see Table 1).[4]
This epidemiological shift is happening in Guatemala as well.[5] Indeed, according to WHO, in the last 25 years, mortality due to NCDs in the country increased by 61 percent, while mortality due to communicable diseases decreased by 63 percent during the same period.[6] Based on WHO’s global burden of disease data, NCDs accounted for around 57 percent of all deaths in Guatemala in 2015.[7] With life expectancy and the percentage of the population over 65 projected to increase, the burden of chronic illness is likely to grow.[8]
Palliative care, an emerging field of medicine, focuses on relieving these symptoms and ensuring that people with life-limiting illnesses and their loved-ones can enjoy the best possible quality of life throughout the course of their disease up until their last moments.
An important aspect of palliative care is addressing chronic, severe pain. Persistent pain profoundly impacts life quality and can have physical, psychological, and social consequences. These include: less mobility and consequent loss of strength; a compromised immune system; and interference with a person’s ability to eat, concentrate, sleep, or interact with others.[9] The physical effect of chronic pain and the psychological strain it causes can even influence the course of disease: as WHO notes in its cancer control guidelines, “pain can kill.”[10] Social consequences include the inability to work; to care for oneself, children, or family members; to participate in social activities; and to find closure at the end of life.[11]
According to WHO, “Most, if not all, pain due to cancer could be relieved if we implemented existing medical knowledge and treatments” (original emphasis).[12] The mainstay medication for treating moderate to severe cancer pain is morphine, an inexpensive opioid made of poppy plant extract. Morphine is a controlled medication; its manufacture and distribution is strictly regulated internationally and nationally.
Medical experts have recognized the importance of opioid pain relievers for decades. The 1961 Single Convention on Narcotic Drugs, the international treaty that governs the use of narcotic drugs, explicitly states that “the medical use of narcotic drugs continues to be indispensable for the relief of pain and suffering,” and WHO has recognized that strong opioids, such as morphine, are “absolutely necessary.”[13]
While pain is often a key symptom in people with life-limiting illnesses, palliative care is broader than just relief of physical pain. For example, many people with chronic illness experience shortness of breath—or dyspnea—a distressing symptom that makes the patient feel they can never get enough air.[14] The physical and psychological effects of dyspnea can cause depression, anxiety, and insomnia.[15] The psychological effects of dyspnea are particularly pronounced, as even mild alterations in breathing patterns may be “cognitively and emotionally interpreted as serious threats to health and life….”[16]
Treatment protocols, such as breathing techniques, oxygen, and relaxation, have been shown to provide significant relief for some patients with dyspnea.[17] Increasingly, morphine has also been recommended to reduce the symptoms of dyspnea.[18]
People with life-limiting illness and their relatives also frequently confront profound psychosocial and spiritual questions as they face life-threatening, incurable, and often debilitating illness. Anxiety and depression are common symptoms.[19] Palliative care interventions like psychosocial counseling and spiritual support have been shown to considerably diminish the incidence and severity of such symptoms and to improve the quality of life of patients and their families.[20]
WHO has urged countries, including those with limited resources, to make palliative care services available. WHO recommends that countries prioritize implementing palliative care services in medical institutions that deal with large numbers of patients requiring palliative care and in the community where it can be provided at low cost to people with limited access to medical facilities.[21]
WHO has observed that these measures cost very little but can have a significant effect.[22] Indeed, as many countries face difficulty accommodating the increased demand for NCD services, some studies have found that offering palliative care leads to overall cost savings for health systems by reducing the pressure on medical systems.[23]
Despite the importance of this essential health care service, access to palliative care has lagged behind the development of other health services due to well-documented barriers in the areas of health care policy, health care education, and medication availability.[24] Indeed, a joint report by the WHO and the Worldwide Hospice Palliative Care Alliance states that 98 countries have no known palliative care services.[25] As Human Rights Watch has found, the gap between the need for pain treatment and palliative care and its availability is the result of a vicious cycle of under-treatment: because these health interventions are not priorities for governments, health care workers do not receive appropriate training, which leads to under-treatment and low demand for the service.[26]
According to the International Narcotics Control Board (INCB), the body charged with monitoring the 1961 Single Convention on Narcotic Drugs, “[a]pproximately 5.5 billion people, or three quarters of the world’s population … have inadequate access to treatment for moderate to severe pain….”[27]
Due to limited access to essential medications, WHO estimates that tens of millions of people around the world, including around 5.5 million end-stage cancer patients and 1 million people with AIDS, suffer from moderate to severe pain each year without treatment.[28]
II.Experience of People Needing Pain Treatment
In Guatemala, the voice of the patient is not heard. They are not organized. They can’t express their needs to the government…. [So the government] does not see the problem. If they spent one week here with us, it would change their minds.
— Dr. Victor Samayoa, chief palliative care physician at the Cancer Institute of Guatemala, Guatemala City, July 2015[29]
An estimated 11,000 Guatemalans die each year from cancer and HIV.[30] Almost 8,500 of them are likely to develop moderate to severe pain that may require treatment with opioid analgesics.[31] In total, some 28,500 Guatemalans—including around 1,500 children—require palliative care each year.[32]
Yet, only four public or government-supported hospitals—the Cancer Institute of Guatemala (Instituto de Cancerología, INCAN Hospital); the National Pediatric Oncology Center (Unidad Nacional de Oncología Pediátrica); the Specialty Social Security Hospital (Hospital de Especialidades del Instituto Guatemalteco de Seguridad Social); and Roosevelt Hospital—currently offer palliative care, mostly the result of initiatives of individual staff members.[33]
All of these hospitals are located in Guatemala City, while 80 percent of the population lives outside the capital.[34] Moreover, three of the hospitals only attend to cancer patients (the two cancer hospitals and the social security hospital), and one of these three only treats children. An estimated 61 percent of people in need of palliative care have a chronic illness other than cancer.[35] Guatemala has two private palliative care providers, a not-for-profit hospice and a private hospital, each in Guatemala City. A few private physicians also offer palliative care and offer limited services outside the capital.
A common narrative emerged among the 37 patients and their families we interviewed: extreme pain and other symptoms; struggles coping with a dim prognosis; visits to multiple doctors who cannot adequately treat their pain; and often lengthy travel on crowded buses to reach a hospital that offers pain treatment.
Suffering Due to Untreated Pain
Emmanuel Garcia was diagnosed with a brain tumor in 2012 when he was a 17-year-old high school student in Guatemala City. His mother took him to a hospital for diagnostic tests after he developed severe headaches, nausea, vomiting, and temporary loss of vision. After his diagnosis, Garcia underwent surgery at General Hospital San Juan de Dios, a tertiary care public hospital in Guatemala City.
Despite the surgery, Garcia continued to experience severe pain, forcing him to drop out of school a few months before he was expected to graduate. His mother broke down in tears when interviewed by Human Rights Watch: “The pain was so intense [at some points] that he would grab his hair screaming and run through the streets calling for help.”[36]
Despite Garcia’s pain, the doctors did not prescribe him strong pain medicines. Indeed, his mother felt that the doctors paid little attention to his symptoms once they decided that curative measures were not feasible. Eventually, his mother learned of a not-for-profit hospice outside Guatemala City, Hospice Estuardo Mini, and took her son there in September 2014. At the hospice, she said that staff put him on morphine and oxycodone and “controlled his pain instantaneously.”[37] He passed away there about five months later.
Gabriel Morales was 60 years old when he felt a sudden pain in his abdomen while lifting a heavy object at work. The pain did not subside, so he went to a hospital. He was diagnosed with abdominal cancer and admitted for treatment. Over the next two and a half months, Morales’ pain went from bad to worse to the point where his relatives thought his death was imminent. He said:
The pain was very high…. I received injections of [an anti-inflammatory pain medicine] that … would relieve the pain for a few hours, but it would come back. It was very difficult…. My family started mourning me when they saw the pain I was in.[38]
Mariel Torres, a 58-year-old women with a facial tumor, said:
I started having symptoms about four months ago…. My only symptom was pain on the left side of my face. The pain was [the worst I could have imagined]. I cried so much with the pain. I couldn’t sleep. I couldn’t eat. I couldn’t talk.[39]
Delayed Access to Palliative Care
Sometimes patients consult with other doctors before they come. They only prescribe them ibuprofen or other low-grade pain medications…. So many of the patients [rate their] pain as 10 out of 10 [on a scale from 0 to 10] when they arrive. So many times they are taking two to three times the [maximum] dose of low-grade pain killers. It’s very difficult.
—Palliative care physician, Guatemala City, December 2014[40]
Many people interviewed described significant delays accessing pain treatment and palliative care. As it is available in only a few hospitals in Guatemala, many of them, including Gabriel Morales and Mariel Torres, initially sought care at hospitals around the country that did not properly assess or treat their symptoms. They described severe suffering and intense anguish as doctors struggled to address their urgent health needs.
Catalina Gutierrez, a 40-year-old baker from Guatemala City, first developed symptoms in early 2014. Tests at a public hospital revealed colon cancer. Gutierrez underwent two surgeries followed by rounds of chemotherapy, but by April 2014 she developed intense pain. Her doctors prescribed her a non-opioid pain medications, but she told Human Rights Watch they were insufficient to control her pain:
This relieved the pain, but a very short time later it would come back…. Since I began the second surgery, from this point until now, I’ve been suffering from pain.… I couldn’t stand the pain. I couldn’t sleep anymore.[41]
Gutierrez was eventually referred to Guatemala’s cancer institute where physicians put her on an opioid analgesic that helped bring her pain under control.
Elena Garcia, a 61-year-old women with ovarian cancer, also spent months in pain before receiving proper care. Her daughter told Human Rights Watch:
It started with pain on her side…. My mom couldn’t sleep…. Every time she tried to walk, she felt like there were needles sticking into her foot…. The first time we went to a public hospital near our house … the only thing they gave her was [ibuprofen] and set another meeting for two months later to re-check the pain.[42]
Fifteen days later, when the pain would not subside, Garcia and her daughter traveled to Guatemala’s cancer institute where she was assessed for pain and treated. Garcia’s daughter said: “Some days are better, some days are worse, but the pain has been relieved a lot.” [43]
Long Distances to Palliative Care Providers
I take about four buses to get here. I wake up at 4 a.m. to get here for a morning appointment. It’s very difficult. I manage an internet café, and I must close all day to come here. I have a two-and-a-half-year-old child that I must leave. I come twice a month, but, since the medication is increasing, I sometimes come three to four times a month.
—Luciana Garcia, daughter of patient with ovarian cancer, December 16, 2014[44]
Since all hospitals that offer palliative care are in Guatemala City, many patients must travel long distances to access it, frequently on public transport. The cost and inconvenience of such travel may be unavoidable for curative care, as primary and many secondary care facilities do not have the specialists, diagnostic equipment, and laboratory capacity to properly manage patients with complex illnesses. This is not true, however, for palliative care, which does not involve complex interventions for most and can be easily and cheaply provided at lower levels of care, closer to patients’ homes.
For many people with advanced illness travel can be very difficult, if not impossible. They often end up having to choose between three unenviable options:
- Enduring hardships of traveling, even in a fragile condition, to receive optimal care;
- Sending relatives—often their only caregivers—to get medications. In such cases, they do not see the physician themselves, compromising the ability of the palliative care team to provide proper care; or
- Staying home and getting no care at all.
The cost of travel is a second dilemma. Patients and their families have often already incurred extensive costs, frequently accumulating considerable debt, paying for diagnostic tests and curative care. Even when palliative care services and medications are offered free of charge, travel often drives them deeper into poverty.
Various people whom Human Rights Watch interviewed described the hardships of having to travel long distances to get access to palliative care. Morales, the man with abdominal cancer described above, said he faced enormous difficulty traveling to Guatemala City on public transport to receive pain medications:
Before being an in-patient at the cancer institute, I would come every 10 to 15 days for a consult. I would take two buses. I would wake up at 1 a.m., walk about half a kilometer, and catch the 2:30 a.m. bus. I would get to the boundary of Guatemala City around 8 a.m., where I would take a second bus to the center of the city.
Since it was difficult for me to walk, it would take me 45 minutes to get from the second bus stop to the hospital. And then it was the same process to get back. It was very uncomfortable to travel because of all the pain. The last time I came, the incision from an operation bled while I was traveling. Because of this, I wasn’t able to go home, and I spent the night at a homeless shelter.[45]
Antonia Castillo, a 68-year-old woman with abdominal cancer, described similar difficulties:
Right now, I come every month to the cancer institute. Because I can’t take the pain on the bus, my son must drive to where I live and then drive me back. Both the time and the money are very difficult. My son usually rests on Sundays from work. That day, he comes to my house and stays over. The next day we leave early for the hospital. We left around 5:30 a.m. to get here this morning.[46]
Because of the long distances traveled to access palliative care services, many patients miss appointments. This creates significant challenges for palliative care providers and may result in lower quality care for the patient. As one palliative care physician noted:
We frequently see patients from five to six hours away…. Because of the travel, they don’t come as often as they should. It makes it difficult to properly manage patients and see what secondary effects the medications are causing.[47]
|
Public Transportation in Guatemala For many low-income Guatemalans, the only option to travel to and within Guatemala City is a fleet of low-cost, government-subsidized buses.[48] The brightly-painted, recycled American school buses crisscrossing through Guatemalan City traffic are hard to miss; notoriously difficult to navigate; dangerously overcrowded; poorly maintained; treacherously driven; and frequently the targets of armed robberies and gang violence.[49] Indeed, according the Guatemala’s human rights ombudsman, 418 people were killed and 434 injured using public transport in Guatemala in 2014.[50] Although riding these buses is a part of millions of Guatemalans’ daily commute, it poses a unique challenge to people with life-limiting illnesses who are forced to travel long distances to receive care. The mother of Raul Mendoza, a 16-year-old boy with kidney cancer, told Human Rights Watch that she and her son had to stop taking public transport because people on the crowded buses would press on his nephrostomy bag, which collects urine diverted from the kidneys. She said: [W]e used to take a bus to the hospital. We would leave around 4 a.m. and take three buses to get here around 7 a.m. After the surgery, they had to put a drainage tube in. Because the buses are so full, they would press on his bag. Now I have to take a taxi, which usually cost 150 Guatemala Quetzales (GTQ) (US$19) each way…. It’s very difficult. We have to save up to money for the trips.[51] |
Positive Effect of Palliative Care on Patients’ Lives
As noted above, palliative care providers can generally control symptoms from life-limiting illnesses well, often with basic medications and interventions. Morphine and other opioid analgesics are highly effective in relieving cancer pain. Several people told us how dramatically their quality of life had improved once they received access to proper treatment.
Marianna Hernandez, a 58-year-old women with metastatic cancer of the abdomen, described her symptoms before and after going to a palliative care unit:
The pain was very intense. On a scale from 1 to 10, it was an 11. I couldn’t sleep anymore, and I lost my appetite. The pain lasted for three months until I came here to the palliative care unit and they prescribed oxycodone. Now my pain is a three or a four. I can sleep well, I can go to the bathroom, and I can eat.[52]
Filipe Soto described his father’s transformation after receiving pain treatment as follows:
Before coming here, they couldn’t control his pain. The pain was too strong. It was a 10 [on a scale of 0 to 10]. He couldn’t sleep when the symptoms started. He could do a little work, but he couldn’t finish it. He always had to stop and lay down. Since [coming to the cancer institute], the pain has been managed well. It makes him feel comfortable.… We actually feel satisfied with how he’s being taken care of.[53]
When Human Rights Watch first met Blanca Coslo, a 24-year-old woman with cervical cancer with metastasis in her lungs, she was waiting to be seen by a palliative care physician at the National Cancer Institute in Guatemala City. She was in a lot of pain and was experiencing trouble breathing. “I was very agitated and had a lot of pain in my chest,” she said.[54] After the palliative care doctor gave her pain medicines, she visibly improved. In an interview with Human Rights Watch she commented: “After [the morphine] was administered, I felt better, more calm, thank God. The coughing, the agitation, and the pain got better.”[55]
Laura Marina Muares Guzman, a patient with thyroid cancer, described a similar experience:
It has been difficult because when the pain comes, it’s on this part [of my neck] here, and if I strain myself a little then I feel that my neck becomes stiff. But an hour or half hour after I’ve taken [oxycodone], I feel relieved, and the pain lessens and it goes away slowly. I take it [my medication] every six hours.[56]
III. Exploring Barriers to Palliative Care in Guatemala
I get mad at the system. I know what to do and how to do it, but they [the regulations] tie my hands. I get even more frustrated because when the patients are in the hospital, I can relieve their pain. But in two to three days, when the patient leaves the hospital, they will have nothing.
−Internal medicine physician at a public hospital three hours from Guatemala City, December 2014[57]
Barriers to Accessing Opioid Analgesics
WHO and INCB have repeatedly called on countries to ensure the adequate availability of opioid analgesics for patients who need them. To improve access, WHO recommends that countries adopt a “medicines policy” to ensure the “availability of essential medicines for the management of symptoms … and, in particular, opioid analgesics for relief of pain and respiratory distress.”[58]
International human rights standards to which Guatemala is a party have been interpreted as requiring that countries ensure the availability and accessibility of opioid analgesics included in the WHO Model List of Essential Medicines. The UN Committee on Economic, Social and Cultural Rights maintains that providing essential medicines as determined by WHO is a core obligation that cannot be limited by claims of limited resources.[59]
Because opioid analgesics are controlled substances, countries are obligated to regulate how they can be produced, distributed, prescribed, and dispensed. The 1961 Single Convention on Narcotic Drugs (1961 Convention), the international agreement that provides the framework for national drug control efforts, contains four basic requirements for national regulations of controlled medicines:
- Individuals dispensing the medication must be licensed, either by virtue of their professional license or through a special licensing procedure;
- Medications may only be transferred between authorized institutions or persons;
- Medications can only be dispensed to a patient upon a medical prescription; and
- Records on the movement of the medications are kept for no less than two years.[60]
The 1961 Convention specifically allows countries to put in place additional requirements, including a special prescription form for controlled medications. Countries, however, have a dual obligation with respects to these medicines: they must ensure their adequate availability for medical and scientific use while preventing their misuse and diversion.[61]
Countries should take care that any requirements beyond those specified in the 1961 Convention do not unnecessarily impede medical access.[62] As WHO notes:
[I]t is important to analyze the effects of any stricter rules…. If a rule provides a barrier for availability and accessibility, but does not contribute to the prevention of abuse … [it should be] eliminated or changed. In the case where a rule both contributes to prevention and constitutes a barrier for medical use…, alternative ways of providing the same level of prevention without posing a barrier to rational medical use should be explored.[63]
Guatemala’s Regulatory Framework
Data on the use of opioid analgesics show that a major gap in the treatment of moderate to severe pain in Guatemala. The INCB classifies Guatemala as having “very inadequate” opioid availability.[64]
The latest available data indicates that Guatemala consumes an annual amount of morphine sufficient to treat approximately 3,000 patients with terminal cancer or AIDS per year—around 35 percent of people with those illnesses who need it.[65] This estimate does not take into account the morphine needs of people with pain that is due to illnesses such as heart and lung disease or diabetes. Given that morphine is also used to treat pain caused by trauma and surgery, a considerable proportion of the morphine Guatemala consumes is not actually used in palliative care.
Human Rights Watch’s analysis of Guatemala’s drug control regulations and practices shows that they go far beyond the requirements of the 1961 Convention and create significant barriers to prescribing and dispensing opioids to outpatients. The most problematic aspects of the regulatory system are the requirements that:
- Doctors need a special prescription pad to prescribe an opioid analgesic. These contain just 25 scripts; can only be purchased at one location in the country, one pad at a time; and physicians must pay for them and produce a receipt from a specific bank showing payment. A new pad can only be issued once the previous one has been returned. The logistic burden these requirements create is a barrier to the use of these medicines.
- Patients who need an opioid analgesic for more than eight days—most patients with advanced life-limiting illness—require a second prescription form, referred to as a dictamen. The physician must provide additional details on this, including the amount of medication the patient needs on a daily, weekly, and monthly basis. This requirement is of no real use and impedes physicians’ ability to adjust dosage when a patient’s pain worsens, which is common. The dictamen also requires a special stamp—timbre medico—that physicians have to buy at the College of Surgeons and Medical Doctors in Guatemala City, another logistical barrier.
- Patients must usually get the Ministry of Health to authorize a prescription before a pharmacy can dispense medications. This can be done at only one location in the country, in Guatemala City, and in person. Theoretically, pharmacies outside Guatemala City have an exemption from this procedure, although none currently use it.
|
Guatemala’s Regulations on Opioid Analgesics Guatemala’s regulatory regime is complex, containing numerous rules and exceptions. These rules are outlined in the following regulatory documents:
|
Special Prescription Pads
None of the doctors outside Guatemala City have special prescription forms. It’s a lot of work to get it. They would have to come to Guatemala City and would lose a full day of work.
—Dr. Maria Elena Alcantara, private palliative care physician, Guatemala City, July 2015[66]
Under Guatemalan regulation, doctors must prescribe opioids on special prescription forms.[67] While the 1961 Convention specifically allows countries to require their use, WHO has noted that requiring special prescription forms increases the administrative burden for health care workers and drug control authorities.[68] It has stated that this problem is “compounded if forms are not readily available, or if health professionals need to pay for them.”[69] It recommends that countries “ensure that this system does not impede the availability and accessibility of controlled medicines.”[70]
In Guatemala, obtaining a special prescription pad is complex and time-consuming. First, prescription pads can only be obtained at a single office in the entire country: the office of the Department of Regulation and Control of Pharmaceutical Products and Related Products, located in Guatemala City (Department of Regulation). The doctor, or their representative, must come to the office in person. It is not possible to request or receive the prescription pad by mail or electronically.
Furthermore, doctors must pay for the prescription pads, which cannot be done at the office that issues them. Instead, physicians must make a payment—of GTQ30 (US$3.89)—at the Rural Development Bank into the Department of Regulation’s account, a requirement that adds additional time and expense to the process.[71] The physician, or their representative, must provide a deposit receipt as proof of payment. Finally, the physician must provide a sheet of paper with four signatures and four imprints of their professional seal, which is apparently used to verify the applicant’s identity.[72]
Compounding the burdensome nature of this process, special prescription pads contain only 25 scripts. Thus, physicians who see large numbers of palliative care patients have to go through this process frequently. In Guatemala City, some pharmaceutical companies and pharmacies help physicians with the logistical process, such as submitting paperwork and collecting the prescription pads.
Problematically, a physician can have only one special prescription pad at a time. Authorities may only issue a new booklet when all the scripts of the previous pad have been used and returned to it. As a result, physicians are left without prescriptions while arranging to get a new pad.
The prescription pad requirement is a major obstacle to patient access to opioid analgesics. According to the Department of Regulation, which is charged with issuing prescription pads, only 50 to 60 doctors out of 14,287 doctors in Guatemala have them.[73] No doctor living outside Guatemala City has a special prescription pad.[74] Similarly, few pharmacies carry opioid analgesics: Human Rights Watch could only identify three in Guatemala City. Given that no doctors have prescription privileges outside Guatemala City, it is likely that access to pharmacies that dispense opioids is even more limited in other departments.[75]
|
Morocco: Reducing Regulatory Barriers to Obtaining a Special Prescription Pad Moroccan law also requires that prescriptions for opioids are written on special prescription pads. However, unlike in Guatemala, the government has taken a number of key steps to minimize the burden on physicians of this requirement.[76] Physicians and hospital administrators can apply for the special prescription pad by mail rather than having to go in person. The Ministry of Health can issue two prescription pads at a time, each containing 50 scrips, which significantly reduces the risk of a physician being left without prescription forms during the application process.[77] Finally, physicians in public hospitals in Morocco do not have to pay for the special prescription forms. |
Dictamen: Additional Prescription Form
By regulation, certain prescriptions of opioid analgesics require an additional form: the so-called dictamen.[78] This form is mandated when opioid analgesics are prescribed for longer than eight days or when the patient is considered to be “habituated to the use of narcotic drugs.”[79] As palliative care patients often need opioid analgesics for more than eight days, the additional form is required frequently.
This requirement is highly unusual, especially given that Guatemala already requires a special prescription form. The dictamen, downloadable from the website of the Ministry of Health’s drug control office, requires the physician to provide information on the patient in addition to that which is required on the special prescription form, including the commercial name and presentation of the medication and its daily, weekly, and monthly dosage.
As pain levels often change rapidly in palliative care patients, the requirement to indicate dosage on a weekly and monthly basis makes little clinical or practical sense.[80] A physician told us it forces doctors to write fictional dosages on the dictamen in order to maintain flexibility to make adjustments as needed.[81]
A system that forces physicians to write prescriptions that do not correspond to the actual dosage needed for the patient is problematic, especially as it can lead to confusion among patients and their families regarding the instructed dosage. It may also lead to larger amounts of opioid analgesics left over in people’s homes after patients pass away.
The dictamen also requires a so-called timbre medico, a kind of postage stamp that is used to confirm that an official document, such as a death certificate, is issued by a physician. Physicians must buy the timbre medico at the College of Medical Doctors and Surgeons in Guatemala City or in one of the provinces where it has an office at a cost of GTQ5 (US$0.65) each.
The dictamen requirement creates extra work for physicians, which may further deter them from prescribing these medicines. Physicians and officials in Guatemala told Human Rights Watch that dictamenes are simply filed away and that they were not aware of any way in which they have been used to improve clinical practice or reduce the risk of misuse of opioid analgesics.
Government officials told Human Rights Watch that the dictamen was part of Guatemala’s regulations aimed at prevention abuse of opioid medications but could not explain exactly how the dictamen helped achieve that goal.[82] In its research on palliative care, which spans dozens of countries, Human Rights Watch has never encountered this kind of requirement.
Government Authorization of Prescriptions
The patients are literally dying and in pain. I can’t send them to the [Department of Regulation] on a bus. I feel responsible to continue [dispensing] to them.
— Pharmacist who dispenses opioid analgesics without validation of the prescription form, Guatemala City, December 2014[83]
Guatemala’s regulations also require that prescriptions for opioid medications receive government authorization from the Department of Regulation before they are dispensed.[84] In practice, this means that before purchasing medications from a private pharmacy in Guatemala City, patients, or their representatives, must have the prescription authorized in-person at an office of the department.[85] This can only be done at one office in the country. At this office, patients must present their prescription, which is then reviewed and authorized. The regulation provides no guidance or limitations as to when the department staff may decline to authorize a prescription.[86] Officials told us that there are no internal documents that instruct staff on criteria to authorize or reject prescriptions.[87]
For prescriptions not requiring a dictamen, patients’ prescriptions are simply stamped and signed.[88] If a dictamen is required, patients receive a card with a patient identification number.[89] This must be written on all subsequent prescriptions in order for them to be authorized.
This system creates an obstacle for patients and families, many of whom have already traveled for hours to visit a doctor. They must travel to the Department of Regulation’s office after receiving the prescription, a trip that frequently involves long rides on public transport. For patients who do not know Guatemala City, additional expense and time are not the only challenges. As one palliative care physician noted:
Many of the people who come here, they don’t know the area. They can’t navigate to the office and then back to the hospital. Sometimes they are afraid. They don’t know how to take the bus; they don’t have a car. Sometimes the patients can’t even speak Spanish [but only indigenous languages]. [90]
When authorization is refused, patients or family members have to obtain a new prescription from their physician and attempt to receive authorization again. Officials insisted to Human Rights Watch that they refuse authorizations infrequently and mostly due to clerical errors, such as forgetting to apply the professional stamp to a dictamen.[91]
Palliative care physicians, however, told Human Rights Watch that it is not uncommon for prescriptions to be rejected and that some are rejected because of the high dose or medication prescribed.[92] Officials insisted they do not second-guess doctors’ clinical decision.[93] Human Rights Watch was unable to determine how frequently authorization is refused as the government does not track refusals. We were also unable to review any rejected prescriptions to determine whether any were rejected based on clinical criteria.
Guatemala’s regulations contain an exception to the above rule: private pharmacies outside Guatemala City may fill prescriptions without government authorization and submit monthly reports to the Department of Regulation for approval in lieu of authorization of individual prescriptions.[94]In theory, this means patients who live outside the capital can avoid the authorization process. But officials told Human Rights Watch that no pharmacies outside Guatemala City stock opioid analgesics and that this exception has never been used.[95]
Analysis of the regulations shows that details of how this exception would work in practice are ill-defined. For example, it is not clear exactly what would happen if a prescription was rejected after it was dispensed. A Department of Regulation representative said the department would take disciplinary action against the pharmacy in such case.[96] Lacking clear guidance, pharmacies might be justifiably concerned about undertaking this responsibility: a pharmacist could face up to 20 years in prison for illegally supplying opioid analgesics.[97]
A new July 2015 instruction from the Ministry of Health’s Office of Food and Medicines further complicates the process. While in the past a representative of a patient—such as family member or pharmaceutical representative—could simply take the prescription form to the Ministry of Health to be authorized, prescriptions can now only be authorized if the individual has a letter that designates them as the patient’s representative. The letter must contain the full name of the patient, a copy of the ID card and its number. If the representative works for a pharmaceutical company, the letter must be printed on letterhead paper and stamped and signed by an authorized official.[98]
Guatemala’s authorization requirement is highly unusual and creates an enormous obstacle for patient access to opioid analgesics. In the vast majority of countries around the world, including Central American countries like Costa Rica, Mexico, and Panama, a doctor’s prescription for an opioid medication can generally be filled at the pharmacy without further authorization.[99]
Since records on prescribing and dispensing must be kept for at least two years, authorities already have the opportunity to inspect physicians’ prescribing practices and dispensing. Authorities are therefore already in a position to take corrective steps against physicians or pharmacists who are found to violate prescribing and dispensing rules.
|
Regulatory Reform in Mexico In June 2015, Mexico’s Ministry of Health launched an electronic platform that allows physicians to download special prescription forms online. The system was designed to reduce the regulatory burden of prescribing opioids.[100] Mexico’s regulation require physicians to obtain a special license, special prescription forms, and barcoded stickers in order to prescribe opioids. Prior to the launch, the process for obtaining barcoded stickers, which required physicians to travel to state capitals in person to collect them, was a major barrier to accessing opioids.[101] The new electronic system lets physicians can obtain their special license—as well as special prescription forms with barcoded stickers—from a secure website and print them from any computer. Pharmacists will keep electronic record books, which are expected to reduce the bureaucratic burden. Finally, prescriptions are canceled once a pharmacist scans them, preventing patients from re-using a prescription. The new system has a number of benefits:
|
Prescription Requirements for Hospitalized Patients
The above regulations only apply to outpatients. For patients who are hospitalized, hospital pharmacies can develop their own internal policies that guide prescribing and dispensing opioid analgesics.[103]
Physicians told Human Rights Watch that these internal policies can vary greatly from hospital to hospital, with some preventing and others facilitating use of these medications.
Examples of problematic internal procedures include the requirement that health care workers return empty ampoules of morphine to the pharmacy before they can get more (which can delay the initiation of treatment for patients in severe pain), or the requirement for multiple signatures on an internal prescription for opioid analgesics before the medication can be issued.[104]
These requirements go beyond what is required under international drug control treaties and may deter the proper medical use of opioid analgesics. Some hospital pharmacies also impose arbitrary limitations on the number of ampoules the hospital pharmacy will dispense for a hospitalized patient per day, regardless of their condition or need.[105]
While internal hospital pharmacies generally do not supply medications to patients who are not hospitalized, the internal regulations of four public or government-supported hospitals currently allow them to dispense opioid analgesics to outpatients, an arrangement that palliative care physicians at these hospital use extensively. This allows them to circumvent the above-mentioned prescribing and dispensing regulations for opioid analgesics, as the medications can be given to patients without a special prescription form, dictamen, or government authorization.[106]
For example, in 2014 Roosevelt Hospital’s pharmacy adapted its internal policies to permit the dispensing of oral opioids analgesics to out-patients. Prescriptions must be written on an internal controlled substance prescription pads, which is readily available to a select group of physicians whom the hospital approves to prescribe these medications.[107] With these prescriptions, patients can get their medications from the internal hospital pharmacy without needing a dictamen or government authorization.
The National Cancer Institute (NCI) uses a similar procedure. Dr. Victor Samayoa, head of the palliative care unit at the NCI, explained what a difference it makes for patients:
When I first came to NCI, it was a shock. In 10 minutes, the patient receives his medication. [If we had to follow the regulations] it would be chaos…. Most of the patients who come here live far away. I just had a patient who traveled nine hours to get here. It is not possible to adequately treat these patients if we had to follow the regulations.[108]
However, as providing outpatients with medications from hospital pharmacies is very unusual, most hospitals in Guatemala do not allow their internal pharmacies to dispense opioid analgesics for outpatients. These hospitals, including San Juan de Dios General Hospital, a major tertiary level hospital in Guatemala City, stick to the established practice that outpatients must purchase their medications from private pharmacies.[109]
|
Colombia: More Pharmacies Carry Oral Opioids A dearth of pharmacies stocking oral morphine is a major challenge in many countries. Administrative requirements, low demand, concerns about potential misuse or diversion, and the potential for scrutiny from law enforcement deter many pharmacy owners from stocking it. Several have actively tried to address this issue. In Colombia, for example, intensive engagement between the government, NGOs, and academics led to a revised regulation for regional medicines procurement in 2008. Under that regulation, all 32 Colombian states have to have at least one private or public pharmacy where opioids are guaranteed to be in stock at all times.[110] This commitment to opioid availability was solidified in article 8 of Colombia’s recently passed palliative care law.[111] Following these and other efforts to increase access to palliative care in Colombia, opioid consumption has increased dramatically. Between 2006 and 2012, the government reported a 270 percent rise in opioid consumption.[112] |
***
|
Should I Follow the Regulations? An Ethical Dilemma for Doctors and Pharmacists
Guatemala’s excessively restrictive opioid regulations create an acute ethical dilemma for some physicians who prescribe these medicines and for pharmacists: they cannot offer proper care to patients, as required by their professional oath, without stretching or breaking the law, exposing themselves to potential disciplinary or criminal penalties. We learned of a number of different ways in which physicians and pharmacists push the boundaries of the law to make sure their patients can get the pain treatment they need:[114]
Regulations that force health care workers to choose between providing proper care—fulfilling their ethical duty—and breaking the law are obviously problematic. No health care worker should have to risk jail time in order to prescribe essential medications. Moreover, the above-mentioned ways in which health care workers, pharmacists, and patients get around official requirements undermine the very purpose of the regulations: to establish a clear procedure for prescribing these medicines that prevents their diversion and misuse and allows the government to investigate such incidents. |
Legal Sanction for Violations of Prescribing Regulations
Guatemala’s regulations and criminal law provide for potentially harsh legal sanction for physicians and pharmacists who violate regulatory requirements. In fact, the country’s drug regulations are so complex that they make it difficult for even the most attentive doctor or pharmacist to be able to comply with them. Regulations frequently mention potential criminal penalties that may result from regulatory violations.
Violations of drug regulations would likely fall under articles 38 and 44 of Guatemala’s drug trafficking law, which states:
Article 38: Anyone who without lawful authorization acquires, disposes of in whatsoever manner, imports, exports, stores, transports, distributes, supplies, sells, retails or carries on any other activity connected with the trafficking in seeds, leaves, plants, flowers or substances or products classified as narcotic or psychotropic substances or drugs or precursors shall be punished by a term of imprisonment of between 12 and 20 years and a fine of between GTQ50,000 (roughly US$6,642) and GTQ1,000,000 (roughly $132,846). Anyone who provides the means, or who facilitates or permits the landing of aircraft used for illicit trafficking, shall be liable to the same punishment.
Article 44: Any physician who, in breach of the relevant laws or regulations, prescribes or supplies drugs that require a prescription when they are not indicated for treatment purposes shall be punished by a term of imprisonment of between three and five years, a fine of between GTQ200 (roughly $27) and GTQ10,000 (roughly $1328) and disqualification from carrying on his profession, which additional punishment may not exceed the duration of the custodial punishment.[116]
Violations of this article are punishable by three to five-year prison sentence.[117] The penalty for illegally supplying narcotic drugs is 12 to 20 years in prison and a GTQ50,000 to GTQ1,000,000 ($6,642 to $132,846) fine.[118]
Guatemala’s regulations may leave physicians and pharmacists potentially exposed to legal sanctions. For example, the regulations state:
Establishments that sell narcotic drugs … shall release these drugs only when the prescriptions forms are from the official prescription form book and authorized by the Department [of Regulation]. Otherwise, the release of these drugs will be regarded as illegally supplying narcotic drugs and will be penalized as such.[119]
This article suggests that filling prescriptions before government authorization—whether in Guatemala City or outside—could trigger drug trafficking charges.
The regulations also suggest that clinical decisions about the dosage or types of medications prescribed could lead to criminal punishment even in the absence of evidence that a physician deliberately wrote a prescription for an opioid analgesic to someone who did not have a medical need for one:
In the event that there is not sufficient scientific evidence for use and the dose used, the prescriber must answer to the Department [of Regulation], without prejudice to the penalties that may apply as a result of the crime or offense.[120]
While we did not identify any physicians who had faced investigations or punishment under this provision, WHO identifies fear of potential legal sanction as a key reason for the low consumption of opioid medications in some countries.[121] To combat this, it recommends that countries have clear regulations and proportional sanctions so that doctors do not fear punishments for unintended or technical violations of the law.[122]
Availability of Different Formulations of Opioid Analgesics
The WHO Model List of Essential Medicines contains a section on pain and palliative care that includes a total of 20 medications in three categories: non-opioids and non-steroidal anti-inflammatory medicines; opioid analgesics; and medicines for other common symptoms in palliative care patients.
The list includes morphine in five formulations—granules, injection, oral liquid, tablet (slow release), and tablet (immediate release)—often with multiple dosages at each formulation. WHO recommends that these medicines be available to all who need them in the formulations and dosages indicated on the list.[123]
The most basic form of morphine WHO recommends is instant release oral morphine in 10mg tablets. Yet, the only form of immediate release morphine available in Guatemala are 30mg capsules, a dosage that creates clinical challenges that would not arise if 10mg tablets were available, including:[124]
- Difficulty breaking capsules into smaller doses for patients requiring 5 mg or 10 mg;
- Physicians normally instruct patients to treat breakthrough pain—peaks in pain that are not adequately controlled with the normal dose prescribed—to take a small extra dose, which is difficult with 30 mg capsules.[125]
Moreover, health care workers are not supposed to prepare new formulations from morphine tablets, such as morphine syrup.[126] However, for patients who cannot swallow, that may be the only option to give them their medication.
WHO recommends that countries having multiple formulations and dosages of morphine available to physicians to give them flexibility to tailor their treatment. Oral liquid morphine, for example, is critical for patients who have trouble swallowing or have uncontrollable nausea, both common in palliative care patients. Oral solutions are also essential for many young children.
Guatemala has two medicines’ lists—one for Ministry of Health hospitals, one for social security hospitals—from which their facilities can choose to procure medications.[127] There are several important differences between these lists:
- Immediate release morphine—the most basic and lowest cost formulation— is not included on either list;
- Granules and oral liquid morphine, both important for patients who have trouble swallowing and for pediatric patients, are not included on the lists; and
- On the social security list, slow-release morphine and injectable morphine are exclusively available for hematology, oncology, intensive care, and emergencies. Yet, over 60 percent of people in need of pain treatment in Guatemala have a chronic illness other than cancer.[128]
In 2012, the National Commission on Palliative Care presented the Ministry of Health’s narcotics division with a proposal to modify regulation 16-2002, under which prescription forms would be pre-authorized so that patients would be able to fill them without having to validate them. However, the ministry never responded to the proposal.
Barriers to Developing Palliative Care
WHO and its decision-making body, the World Health Assembly (WHA), recommend that national health systems integrate palliative care. To achieve this, WHO recommends that governments formulate and implement a number of specific policies that it considers essential for expanding palliative care, in addition to a policy to ensure availability of palliative care medicines. These include:
- Health system policies to ensure palliative care is integrated into the structure and financing of national health care systems at all levels of care;
- Policies for strengthening and expanding human resources, including education and training of health care professionals to ensure adequate responses to palliative care needs, together with training volunteers and educating the public.[129]
WHO has noted that such measures, fundamental for developing palliative care, “cost very little but can have a significant effect.”[130] A WHA resolution on palliative care, a document that sets out the global consensus and policy goals, unanimously adopted by UN member states on May 23, 2014, closely mirrors these recommendations.[131]
Adherence to these recommendations is important to governments’ efforts to realize the right to health as guaranteed under international human rights law. The Committee on Economic, Social and Cultural Rights—the body that monitors and guides states’ efforts to realize and protect the right to health as articulated in the International Covenant on Economic, Social and Cultural Rights (ICESCR)—maintains that countries should adopt and implement a national public health strategy and plan of action and ensure access to essential medicines as defined by WHO.[132] It has identified providing appropriate training for health personnel as an obligation “of comparable priority.”[133] Human Rights Watch believes that failure to take steps in these areas results in violating the right to health.
Integrating Palliative Care into the Health Care System
According to WHO, national health system policies should promote the integration of palliative care into the structure of health care systems at all levels of care. In these policies, the emphasis should be on primary, community, and home-based care.[134]
Guatemala does not have a national palliative care strategy although it has incorporated palliative care into several key health policy documents (see below). While the non-communicable diseases (NCD) strategy for 2010-2015 does not mention palliative care, the government’s NCD treatment guide states: “palliative treatment is a most important parameter in the treatment of cancer and can be provided in health services of the first and second level.”[135] The national HIV/AIDS strategy allocates 1 percent of the HIV budget to palliative care.[136] A 2014 Ministry of Health guide on prevention and integral care for cervical cancer contains a chapter on palliative care.[137]
In December 16, 2011, the Ministry of Health issued an order to create a National Commission on Palliative Care to advise the national program on the prevention of non-communicable diseases and cancer on improving health care provision to patients with advanced cancer.
The commission was supposed to meet at least monthly to, among other things, promote the availability of opioid analgesics; develop public policies aimed at implementing palliative care services; develop epidemiological surveillance tools; and coordinate training activities for health care providers and families. However, the commission’s work was fraught with difficulties. After a few months, Ministry of Health officials stopped calling monthly meetings and the commission died.[138]
|
Panama: Integrating Palliative Care into the Health Care System Panamanian law grants patients a right to receive palliative care, requires that all hospitals have palliative care units, and places responsibility on primary health centers for providing palliative care to patients who require it over extended periods.[139] In 2011, Panama’s Health Ministry adopted a national palliative care strategy to help implement the law.[140] The philosophy behind the strategy is that patients should always receive care as close to home as possible. It sets out a model that links different levels of the health care system so that patients can move easily between them depending on their situation. A key role in this model is assigned to Panama’s regional hospitals, all of which must have multidisciplinary palliative care teams. These teams not only offer clinical care but are also responsible for training health care workers at the primary level of care; offering them ongoing support in patient care; and working with NGOs, churches and others, to develop community support for palliative care. The multidisciplinary teams are also the link between the different levels of care, facilitating referrals up and down the chain. Panama has made significant progress in implementing this strategy. Each of the country’s 10 provinces has a palliative care coordinator, more than half of the regions have active palliative care programs, and the number of patients receiving palliative care has risen steadily from 1,000 in 2010 to more than 2,600 in 2015. Even so, challenges remain, especially in remote regions, within the social security system, and in providing palliative care to children.[141] |
Palliative Care Education for Health Care Workers
Adequate training and education for health care workers are essential for providing palliative care.[142] Indeed, in many countries a lack of such training is the single greatest barrier to its provision.
The Committee on Economic, Social and Cultural Rights considers appropriate training of health care workers a matter of key importance in government efforts to ensure the right to health.[143] WHO recommends that “education about palliative care (including ethical aspects) is offered to students in undergraduate medical and nursing schools and to health care providers at all levels….”[144]
The May 2014 WHA resolution calls on countries to include palliative care as an “integral component of the ongoing education and training offered to care providers” and specifies that:
- All doctors should receive basic training and continuing education on palliative care;
- Health care workers who routinely work with patients with life-threatening illnesses should receive intermediate training; and
- Specialty training should be available for doctors who provide complex palliative care interventions.[145]
This layered approach to palliative care education is essential to integrating palliative care across all levels of the health care system, as the WHA resolution recommends. A health care system in which all health care workers have training in palliative care appropriate for their role allows patients to receive care as close to home as possible, sparing them arduous, expensive, and time-consuming trips to specialists. It also allows specialists to focus on the most complex cases while general practitioners can attend to routine ones, thus improving the efficiency of the system.[146]
Guatemala has four universities with medical schools.[147] Only one, Mariano Galvez University, has a mandatory undergraduate curriculum in palliative care.[148] San Carlos University, the country’s largest and only public medical school, does not have palliative care as part of its curriculum.[149] As a result, most physicians graduating from medical school in Guatemala have no or limited knowledge of palliative care and lack clinical exposure to this health service, greatly complicating efforts to integrate it into the health care system.
Similarly, most medical students and doctors are not exposed to palliative care during residencies and in the specialization phase of their training. With the exception of anesthesiologists, physicians in fields of medicine that frequently care for patients with life-limiting illnesses—such as oncology, internal medicine, and cardiology—do not receive any mandatory academic or clinical training in palliative care. Anesthesiology residents from San Juan de Dios Hospital, Roosevelt Hospital, and the Central Military Hospital all must take part in a one to two-month clinical rotation in palliative care at the Cancer Institute of Guatemala’s palliative care unit. Physicians doing their anesthesiology specialization in hospitals outside Guatemala City do not do a palliative care rotation.
In the absence of these rotations, many doctors in Guatemala begin their careers with very limited exposure to palliative care. As one physician who was taking part in a palliative care rotation noted:
[T]he program is essential. In my hospital we don’t use opioids to manage pain. We just use them during surgery [for anesthesia]. We don’t know what happens to patients afterwards. When you come here, you learn how to manage pain.[150]
Palliative care is also not a medical specialty in Guatemala, meaning young physicians who aspire to practice it must look outside the country for training. Between 2012 and 2014, San Carlos University offered the educational opportunity closest to a medical specialty in palliative care available in Guatemala: a post-graduate diploma. The program consisted of 350 hours of theoretical training in palliative care and graduated 70 students during the two years it was offered.[151] However, a new university administrator decided not to renew the program in 2015 because she did not consider it a priority.[152]
IV. Guatemala’s Obligation to Improve Pain Treatment
National Law
Guatemala’s constitution guarantees the right to health in article 93, declaring it a fundamental right afforded to all Guatemalans, without discrimination.[153] Article 94 elaborates:
The State will see to the health and the social assistance of all the inhabitants. It will develop, through its institutions, actions of prevention, promotion, recovery, [and] rehabilitation … in order to procure [for them] the most complete physical, mental, and social wellbeing.[154]
The constitution also explicitly recognizes a state responsibility to protect the “physical, mental, and moral health” of older people.[155]
Interpreting the right to health, Guatemala’s Constitutional Court stated:
[The right] implies that all persons have access to those services that allow for the maintenance or the restoration of physical … well-being [and] that the State must take adequate measures in order to … make the necessary services … to satisfy basic needs accessible to all persons. It also implies that adequate legislation be adopted so that the nation’s inhabitants are able to exercise this right.
The protection of the public health is meant to be undertaken through the direct and decisive action of the State.[156]
As part of the Guatemala Peace Agreement, which formally ended 36 years of internal armed conflict in 1996, the government promised to undertake a number of reforms aimed at ensuring the effective exercise of the right to health.[157] The agreement states:
[It is a responsibility] of the Ministry of Health … to formulate policies to provide the entire Guatemalan population with integrated health services…. The system would create the conditions for ensuring that the low-income population has effective access to quality health services…. The decentralized organization of the various levels of health care should ensure that health programmes and services are offered at the community, regional and national levels.
The Right to Health
The International Covenant on Economic Social and Cultural Rights (ICESCR), to which Guatemala acceded in 1988, specifies in article 12 that everyone has a right “to the enjoyment of the highest attainable standard of physical and mental health.”[158] The Committee on Economic, Social and Cultural Rights, the body charged with monitoring compliance with the ICESCR, maintains that states must make available in sufficient quantity “functioning public health and health-care facilities, goods and services, as well as programmes,” and that these services must be accessible.[159]
International law recognizes that the capacity of states to deliver quality health care services differs depending on the resources at their disposal. The right to health is considered a right of “progressive realization.” By becoming party to the international agreements, a state agrees “to take steps … to the maximum of its available resources” to achieve the full realization of the right to health.[160]
In other words, high-income countries will generally have to provide health care services at a higher level than those with more limited resources, because they have the capacity to do so. But all state parties to the ICESCR are expected to prioritize progress in this area and to take concrete steps toward the increased provision of services. Deliberate, retrogressive measures that erode enjoyment of the right to health are often a violation of the right to health—one that the state in question bears the burden of justifying.[161]
Notably, the United Nations Committee on Economic, Social and Cultural Rights maintains that there are certain core obligations intrinsic to the right to health that are so fundamental that all state parties to the ICESR must meet them immediately rather than progressively realizing them over time. While resource constraints may justify only partial fulfillment of some aspects of the right to health, the committee has observed vis-à-vis the core obligations that “a State party cannot, under any circumstances whatsoever, justify its non-compliance with the core obligations…, which are non-derogable.”[162] The committee has identified, among others, the following core obligations:
- To ensure the right of access to health facilities, goods and services on a non-discriminatory basis, especially for vulnerable or marginalized groups;
- To provide essential drugs, as from time to time defined under the WHO Action Programme on Essential Drugs;
- To ensure equitable distribution of all health facilities, goods and services; and
- To adopt and implement a national public health strategy and plan of action, based on epidemiological evidence, addressing the health concerns of the whole population.[163]
The committee lists the obligation to provide appropriate training to health personnel as an “obligation of comparable priority.”[164]
Palliative Care and the Right to Health
Given that palliative care is an essential part of health care, the right to health requires that countries take steps to the maximum of their available resources to ensure that it is available. Indeed, the Committee on Economic, Social and Cultural Rights has called for “attention and care for chronically and terminally ill persons, sparing them avoidable pain and enabling them to die with dignity.”[165] In Human Rights Watch’s view, the practical application of this principle requires that states:
- Refrain from enacting policies or undertaking actions that arbitrarily interfere with providing or developing palliative care; and
- Take reasonable steps to ensure the integration of palliative care into existing health services, both public and private, through regulatory and other powers, as well as funding streams.
No Interference with Palliative Care
The Committee on Economic, Social and Cultural Rights has stipulated that the right to health requires that states “refrain from interfering directly or indirectly with the enjoyment of the right to health.”[166] States may not deny or limit equal access for all persons, enforce discriminatory health policies, arbitrarily impede existing health services, or limit access to information about health.[167]
Applied to palliative care, this interpretation means that ICESCR state parties should not put in place medicine control regulations that arbitrarily impede the availability and accessibility of essential palliative care medications, such as morphine and other opioid analgesics.
Ensuring Integration of Palliative Care into Health Services
The ICESCR requires state parties to take the steps necessary for the “creation of conditions which would assure to all medical service and medical attention in the event of sickness.”[168] The Committee on Economic, Social and Cultural Rights maintains that people are entitled to a “system of health protection which provides equality of opportunity for people to enjoy the highest attainable level of health,” including patients with chronic or terminal illnesses.[169]
The committee has called for an integrated approach to the provision of different types of health services that includes elements of “preventive, curative and rehabilitative health treatment.”[170] It has also said that investments should not disproportionately favor expensive curative health services, which are often accessible only to a small, privileged fraction of the population, rather than primary and preventive health care benefiting a far larger part of the population.[171]
The same principle applies to palliative care services. Given the large percentage of cancer and other patients who require palliative care services, particularly in low and middle income countries, there is considerable urgency in developing palliative care services to these patients.
Pain Treatment Medication and the Right to Health
Countries should provide injectable and oral morphine since they are on the WHO List of Essential Medicines for adults and for children.[172] States should make sure these medicines are both available in adequate quantities, and physically and financially accessible to those who need them.
In order to ensure availability and accessibility, states should, among others things:
- Put in place regulations to ensure an effective procurement and distribution system and create a legal and regulatory framework that enables health care providers in both the public and private sector to obtain, prescribe, and dispense these medications. Any regulations that arbitrarily impede the procurement and dispensing of these medications may lead to a violation of the right to health;
- Adopt and implement a strategy and plan of action for the roll out of pain treatment and palliative care services. Such strategy and plan of action should identify obstacles to improved services as well as steps to eliminate them;
- Regularly measure progress in ensuring availability and accessibility of pain relief medications; and
- Ensure that, per the requirement of physical accessibility, these medications are “within safe physical reach for all sections of the population, especially vulnerable or marginalized groups.”[173] States must ensure that enough health care providers or pharmacies stock and dispense morphine and that an adequate number of health care workers are trained and authorized to prescribe these medications.
Although the right to health does not require that states offer medications for free, financial accessibility means that medications should be “affordable for all.” In the words of the committee:
Payment for health-care services … has to be based on the principle of equity, ensuing that these services, whether privately or publicly provided, are affordable to all, including socially disadvantaged groups. Equity demands that poorer households should not be disproportionately burdened with health expenses as compared to richer households.[174]
Pain Treatment and the Right to Be Free from Cruel, Inhuman, or Degrading Treatment
The right to be free from torture, cruel, inhuman, or degrading treatment or punishment is a fundamental human right that numerous international human rights instruments recognize.[175] The right also creates a positive obligation for states to protect persons in their jurisdiction from such treatment.[176]
This obligation has been interpreted to include protecting people from unnecessary pain related to a health condition. As Manfred Nowak, then-UN special rapporteur on torture, cruel, inhuman or degrading treatment or punishment wrote in a joint letter with the UN special rapporteur on the right to health to the Commission on Narcotic Drugs in December 2008:
Governments also have an obligation to take measures to protect people under their jurisdiction from inhuman and degrading treatment. Failure of governments to take reasonable measures to ensure accessibility of pain treatment, which leaves millions of people to suffer needlessly from severe and often prolonged pain, raises questions whether they have adequately discharged this obligation.[177]
In a report to the Human Rights Council, Nowak later specified that, in his expert opinion, “the de facto denial of access to pain relief, if it causes severe pain and suffering, constitutes cruel, inhuman or degrading treatment or punishment.”[178]
Even under this reading, not every case where a person suffers from severe pain but has no access to appropriate treatment would constitute cruel, inhuman, or degrading treatment or punishment. In a 2013 report to the Human Rights Council, UN Special Rapporteur on Torture Juan Mendez stated this will only be the case when the following conditions apply:
- The suffering is severe and meets the minimum threshold required under the prohibition against torture, cruel, inhuman, or degrading treatment or punishment;
- The state is, or should be, aware of the level and extent of the suffering;
- Treatment is available to remove or lessen the suffering but no appropriate treatment was offered; and
- The state has no reasonable justification for the lack of availability and accessibility of pain treatment.[179]
V.Full Recommendations
The government of Guatemala needs to take urgent steps to remove barriers to the availability and accessibility of opioid analgesics—and palliative care services more generally—for patients suffering from moderate to severe pain due to life-limiting illnesses. The government has an obligation to ensure that it citizens have access to affordable pain treatment services and medications.
Availability of Opioid Analgesics
Actions Not Requiring Regulatory Reform
The government can take a number of key steps without amending the country’s regulations on opioid analgesics. These steps should be taken without delay.
- At least double the number of scripts in the special prescription pad from 25 to 50. The limit of 25 scripts per prescription pad is not required by regulation. Moreover, the limit does not meaningfully reduce the risk of opioid misuse and increases the frequency that doctors must endure the time-consuming process of obtaining a new prescription pad.
- Allow doctors to obtain at least two special prescription pads at a time. The one prescription pad limit increases the frequency that doctors must obtain new pads and the likelihood they will be without a pad during the application process.
- Remove the requirement for the timbre medico from the dictamen. This requirement creates an unnecessary logistical burden for physicians to prescribe opioid analgesics.
- Abolish the July 31, 2015 requirement that representatives have a signed letter to authorize prescription forms. This newly introduced requirement complicates the ability of relatives or pharmaceutical companies to authorize prescription forms for opioid analgesics.
- Create internal, publicly available guidelines for authorizing prescriptions. These should outline the circumstances under which authorization will be denied and clarify that the Department of Regulation’s staff should not reject prescriptions due to dosage.
- Create and distribute publicly available guidelines for private pharmacies dispensing opioids in outside departments. As noted above, private pharmacies outside Guatemala City can submit monthly reports to the department for approval in lieu of having patients authorize each prescription individually. As of March 2017, no pharmacies were using this exception. The Department of Regulation should create guidelines on how this monthly authorization process will function and distribute them to pharmacies to ensure they are aware of this option and how to use it.
- Develop and implement a program to increase the number of physicians with prescription privileges. The government should develop outreach programs to ensure that multiple doctors in each hospital have a special prescription pad and training in pain management interventions.
- Ensure oral morphine is available in at least one pharmacy in every departmento. The government should ensure that at least one pharmacy in each departmento stocks oral morphine and utilizes the monthly authorization process. Where there are no private pharmacies stocking oral morphine, the government should ensure that a hospital pharmacy dispenses oral morphine to outpatients.
- Ensure that oral morphine is available at San Juan de Dios hospital’s pharmacy. San Juan de Dios is one of the largest hospitals in the country and attends to many patients with chronic illnesses who require pain treatment and palliative care.
- Include on the MSPAS and IGGS lists of medications all formulations and dosages of opioids on the WHO’s Model Lists of Essential Medications. Neither list should limit these medications to specific fields of medicine, such as oncology. Immediate-release morphine should be made available in smaller dosages.
Actions Requiring Regulatory Reform
- Reform the opioid control regulations. The opioid regulations are needlessly restrictive; deter doctors and pharmacists from prescribing and dispensing opioids; and lead to unnecessary suffering for thousands of Guatemalans. These problems cannot be adequately addressed within the current regulatory regime. The Ministry of Health should hold an inclusive meeting of relevant stakeholders to inform a regulatory reform process. This process should not just consider removing existing regulatory barriers, it should also develop regulations that promote opioid access.
- Allow doctors to apply for a new prescription pad by mail or electronically. The current in-person procedure created by regulation 16-2002 for obtaining a prescription pad deters doctors from prescribing and dispersing opioids, particularly rural doctors. The Department of Regulation should establish a procedure for doing these activities by mail or electronically.
- Remove the dictamen requirement from the Government Agreement and regulations 16-2002 and 17-2002. The addition of the dictamen does not meaningfully reduce the risk of opioid misuse. It also complicates the prescription process and increases the risk that prescriptions will be denied due to clerical errors.
- Abolish or at least modify the unusual and burdensome authorization procedure. It creates major barriers for patients who require opioid analgesics and has resulted in physicians and hospitals seeking shortcuts to avoid it, undermining its original purpose. If, in the short term, abolishing the procedure is not feasible, steps should be taken to reduce the regulatory burden. Options include:
- Modify regulation 17-2002 to allow for phone or electronic authorization. The Government Agreement only notes that opioid prescriptions “must first be authorized by the department before it is released.” A process could be created where pharmacies receive authorization by phone or electronically;
- Modify regulation 17-2002 to allow for pre-approved prescriptions. A process could be established whereby certain physicians are given prescriptions that are pre-approved by the department; and
- Modify the Government Agreement and regulation 17-2002 to allow pharmacies within Guatemala City to submit monthly reports to the Department of Regulation for approval in lieu of having patients authorize each prescription individually. This is already allowed for pharmacies outside Guatemala City.
- Reduce fear of legal sanction. The new regulations should be written clearly and accompanied by detailed guidelines to ensure that doctors and pharmacists acting with appropriate diligence do not fear accidental violations of the regulations.
Integrating Palliative Care into the Health Care System
- Create a pain treatment and palliative care strategy. The government should convene an inclusive meeting of relevant stakeholders to help it develop a national pain treatment and palliative care policy and strategy. The policy should address existing barriers to developing pain treatment and palliative care, including policy, regulatory, educational, and other obstacles. It should set clearly defined benchmarks and timelines for overcoming these barriers and introducing pain treatment palliative care in institutional and community settings. It should set up a system for periodically reviewing progress and adjustments of benchmarks.
- Work with key hospitals to provide pain treatment and palliative care. The government and health care system should identify key health facilities around the country to provide pain treatment and palliative care. They should train health care workers and ensure relevant medicines are available and accessible.
Integrating Palliative Care into Health Care Financing
- The Ministry of Health should review implementation of referral arrangements to INCAN Hospital. The government currently agrees to provide free care at INCAN Hospital for patients referred from public hospitals. However, referral practices are inconsistent and can take a month—too long for patients with life-limiting illnesses.
- Review MSPAS’ coverage of essential medications. MSPAS should be reformed with a view to ensuring that outpatient medication costs do not constitute an undue barrier to obtaining essential palliative care medications.
Education
- Develop a mandatory undergraduate curriculum in palliative care. The Ministry of Health in partnership with San Carlos University, Guatemala’s only public medical school, and private medical schools, should develop a mandatory undergraduate curriculum in palliative care to ensure that all medical students receive at least basic training in the discipline.
- Develop mandatory clinical training in palliative care. The Ministry of Health should develop a plan together with relevant hospitals to mandate rotations in palliative care units for doctors of certain postgraduate programs, including oncology, internal medicine, and anesthesiology to ensure clinical exposure to palliative care.
- Recognize palliative care as a medical specialty.The Ministry of Education in partnership with San Carlos University and private universities should begin developing a curriculum for palliative care to be a specialty, which is essential for its long-term development.
Acknowledgments
Research for this report was conducted by Matthew Simon, New York University School of Law fellow in the Health and Human Rights Division of Human Rights Watch, and Diederik Lohman, acting director of the Health and Human Rights Division. Matthew Simon wrote the report. The report was reviewed by Diederik Lohman; Chris Albin-Lackey, legal advisor; Daniel Wilkinson, managing director of the Americas Division, and Danielle Haas, senior editor in the Program Office.
Jennifer Pierre, senior associate, and Matthew Parsons, associate, in the Health and Human Rights Division; Stephanie Martinez and Teresa Kennedy, interns in the Health and Human Rights Division; and Alejandra Aguilar de Hernandez, mission-coordinator and translator, provided invaluable assistance. Translation into Spanish was provided by Gabriela Haymes. Production assistance was provided by Oliva Hunter, Rafael Jimenez, Jessie Graham, Pierre Bairin, Jenny Catherall, Fitzroy Hepkins, and José Martinez.
We are deeply grateful to the many palliative care patients in Guatemala who, despite being gravely ill, agreed to be interviewed for this report. Without them and their relatives, this manuscript would not have been possible. We are committed to using this report to try to make sure that others who develop life-threatening illness—and pain and other symptoms associated with it—will not have to endure the suffering many of these patients faced.
We are also greatly indebted to the many palliative care advocates, doctors, nurses, pharmacists, social workers, and volunteers in Guatemala and elsewhere who helped us conduct our research, understand our findings, and write this report. Their commitment to serving people at the most vulnerable time of their lives is both humbling and inspiring. We are particularly grateful for the assistance of Dr. Eva Duarte, Dr. Victor Samayoa, Dr. Maria Elena Alcantara, Dr. Silvia Rivas, Dr. Marisol Bustamante, and Dr. William Santizo whose advocacy and clinical work has improved the lives of thousands of Guatemalans.