Summary
Because of the pain I couldn’t sleep. I couldn’t talk to my friends. I wanted to crush my head against the wall and shake…. …. My pain tears me apart..
—Adil Akram, 29, who battled cancer in his leg for years, Rabat, October 1, 2014
In 2013, Zayan Ebrahim (pseudonym) was a college student and restaurant chef in a city about 250 kilometers from Rabat, Morocco’s capital, when he began experiencing pain. After two local physicians misdiagnosed and treated him for hemorrhoids, the pain became so intense that, in his words, it began to drive him “crazy.” “I’m not sleeping,” he said. “Even when I am very tired, I only sleep for one hour [at a time]. Then I wake up because of the pain.”
On the advice of a local pharmacist, he traveled to Rabat to seek further medical help. A doctor there discovered that he had colon cancer. Zayan began treatment at the National Oncology Institute where he was also referred to the palliative care service for pain management. There, his pain was finally properly assessed and treated.
But the months of suffering had taken a toll on Zayan. His health had deteriorated and he had lost almost 30 kilograms in weight before receiving proper treatment. As he told Human Rights Watch of his experience, Zayan repeatedly broke down in tears and occasionally became angry at how the healthcare system had failed him.
While the palliative care service in Rabat was able to finally control his pain, Zayan still faces challenges. Because neither cancer treatment nor palliative care is available in his hometown, he has been forced to uproot his life and move into an apartment of a friend who lives in Rabat.
***
Every year, more than 150,000 Moroccans face advanced—and often incurable—chronic illnesses such as cancer; heart, lung, or renal disease; dementia; and AIDS. Over 62,000 Moroccans, including 6,000 children, suffering from these illnesses will experience debilitating symptoms such as pain, breathlessness, and depression.
These symptoms can often be treated well through palliative care, a health service that focuses on relieving them and ensuring that people with life-limiting illnesses and their loved-ones can enjoy the best possible quality of life during the course of their disease up until their last moments.
Ensuring the availability of palliative care has become an increasingly important global health priority in recent years. As populations age and the prevalence of chronic illnesses increases in most low and middle income countries, the need for palliative care has risen drastically. The World Health Organization (WHO) estimates that more than 40 million people require palliative care annually at the end of life.
Morocco is no exception. Non-communicable diseases such as cancer, heart disease, diabetes, and respiratory illnesses account for 75 percent of an estimated 206,000 annual deaths. And the burden of chronic illness is likely to rise. The percentage of people over 65, the segment of the population most affected by these illnesses, is expected to nearly double over the next 15 years. In that same period, the incidence of cancer is expected to nearly triple.
This report identifies challenges people with life-limiting illnesses in Morocco face accessing palliative care, with a special focus on access to pain treatment. The report is based on research Human Rights Watch conducted in Morocco from September 2014 to January 2015, interviewing 85 individuals, including healthcare workers, government officials, and patients and their family members in five regions. We also reviewed relevant legislation, insurance policies, medicines lists, and other policy documents.
Our research found that the government of Morocco has taken several positive steps in recent years to develop palliative care services and to expand access to pain medicines. Significantly, the government released two national health policies that together set out a vision for the development of palliative care; reformed the undergraduate medial curriculum to include a module on pain and palliative care; and removed a large regulatory barrier to accessing opioid analgesics—strong pain medications that are indispensable for pain management.
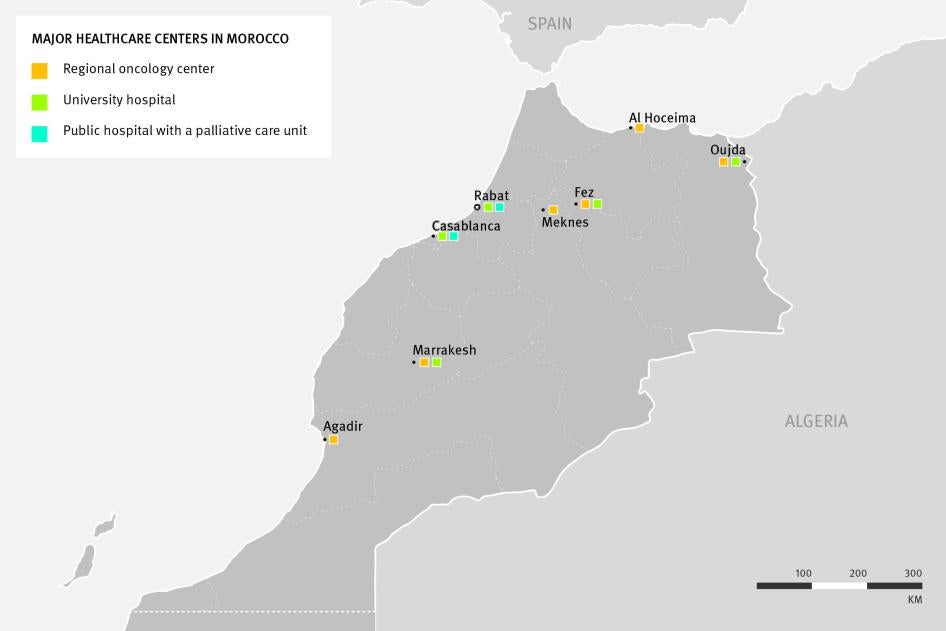
However, the availability of palliative care in Morocco is very limited. At present, only two public hospitals in the country—both tertiary level cancer hospitals—have established palliative care units. As a result, cancer patients have some access to palliative care but often have to travel long distances to get it, a great burden on them that often becomes insurmountable as their disease progresses and enters the final stages.
No palliative care units are available for people with non-oncological conditions, even though the WHO and Worldwide Hospice and Palliative Care Alliance estimate that over 70 percent of adults in need of palliative care from the WHO’s Eastern Mediterranean region have chronic illnesses other than cancer. In other words, around 40,000 adults in Morocco require palliative care each year for conditions other than cancer.
Human Rights Watch was unable to identify any palliative care services at lower levels of the healthcare system, such as regional, provincial, and local hospitals, even though these healthcare facilities are closest to where people who require palliative care live.
Although some healthcare providers, particularly tertiary level hospitals, have integrated palliative care interventions into their general practice, Human Rights Watch believes that to be the exception, as most facilities simply do not have staff trained in palliative care or access to key palliative care medications such as morphine.
Moreover, although the use of opioid analgesics is increasing in Morocco, government data suggests that there is still a major gap in the treatment of moderate to severe pain. The amount of opioids used in Morocco is only sufficient to provide pain relief to one in five patients with cancer or AIDS, without taking into account the opioid needs of patients with illnesses such as heart and lung disease or diabetes. The result is that tens of thousands of Moroccans with life-limiting illnesses pass their last weeks and months in great unnecessary suffering.
Despite the severe suffering he faced due to untreated pain, Zayan is one of the privileged Moroccans who eventually did gain access to palliative care, even if delayed and far from his home.
***
The WHO considers palliative care to be an essential health service and has urged countries to ensure that it is integrated into all levels of the healthcare system. It has recommended that countries implement health and health financing policies to promote it, ensure adequate training of health professionals, make available essential palliative care medicines, including opioid analgesics, and encourage research to assess needs and identify standards and models of care. As palliative care does not need expensive equipment or medications, it can generally be provided at relatively low cost. A World Health Assembly (WHA) resolution on palliative care unanimously adopted on May 23, 2014, closely mirrors these recommendations.
Morocco has taken important steps in each of the four areas the WHO and WHA identifies as fundamental for the development of palliative care. However, our research shows that much remains to be done.
Policy: The government has included specific palliative care goals in the Sectoral Health Strategy (SHS) 2012-2016, Morocco’s national health strategy, as well as in its National Cancer Prevention and Control Plan (NCPCP) 2010-2019. The documents call for the creation of palliative care networks; the development of external palliative care consultations; and the institutionalization of pain treatment at all levels of the healthcare system—all very much in line with WHO and WHA recommendations.
However, neither strategy appears designed to succeed. Neither sets a specific timeline nor identifies clearly what agencies are responsible for implementing the measures. Nor does it appear that the government has a clear process for tracking implementation progress. While the NCPCP breaks down its overall objectives into specific action points, the SHS only contains broad measures. The SHS does not contain a budget; palliative care makes up just 1 percent of the NCPCP’s overall budget.
Given the above, it is perhaps not surprising that Human Rights Watch analysis of the implementation effort has found that progress has been uneven and limited in many areas.
Key findings include:
- Little progress has been made to date developing the decentralized palliative care network that the NCPCP envisions. While a palliative care center was created in Casablanca, none have been established anywhere else in the country (despite plans in the NCPCP to begin building centers in Fez and Marrakesh in 2011 and 2012, respectively);
- Opioid analgesics remain largely unavailable outside tertiary health facilities. The controlled substances law has been amended to increase the maximum prescription period for opioid analgesics, but few steps have been taken to counter physicians’ and pharmacists’ fears and misconceptions around these medicines or to increase the number of physicians with prescription privileges; and
- progress towards decentralizing pain management has been limited. Our research suggests pain management committees at regional and provincial hospitals have either not yet been established or are not functioning effectively.
Insurance: Since 2005, the government has instituted two major health insurance reforms: a compulsory health insurance program (Assurance Maladie Obligatoire or AMO) for salaried public and private sector employees; and a public insurance scheme (Regime d’Assistance Medicale or RAMED) for the poor. These insurance programs cover close to 50 percent of Moroccans. Both insurance schemes cover the provision of palliative care and a fairly comprehensive set of essential palliative care medicines. However, in practice, this insurance coverage is not effective as very few healthcare providers offer palliative care and RAMED does not cover medications for outpatients.
Education: In September 2015, Morocco’s medical schools will begin teaching a mandatory 20-hour segment on palliative care for 5th year medical students, a major step toward ensuring all physicians have at least basic palliative care knowledge and skills. However, continuing medical education programs and intermediate and advanced training opportunities in palliative care remain limited and only meet a fraction of the need.
Medicine availability: In 2013, Morocco changed its controlled substance law to increase the number of days a prescription for an opioid analgesic can cover from 7 to 28 days, removing a key barrier to the availability of these medicines. The seven-day limitation meant that patients who required opioid analgesics or their relatives had to travel to their physician every single week to obtain and fill a new prescription.
Our analysis of Morocco’s drug regulations shows that while they are more restrictive than required by the United Nations drug conventions and generate additional work for physicians, pharmacists, and hospital administrations, the requirements do not appear to be excessively burdensome.
However, use of opioid analgesics remains very limited. Few pharmacies and hospitals stock oral morphine and only a small fraction of physicians have the ability to prescribe opioids. The government itself has identified physician’s exaggerated fear of the risks associated with opioid analgesics—known as opiophobia or morphineophobia—as a significant barrier to adequate prescribing. Indeed, we found that many of the physicians and pharmacists we interviewed had misconceptions about opioid analgesics.
Problematically, Morocco’s controlled substances law itself appears to stigmatize these medications by labeling them “poisons” (vénéneux)—an outdated designation used in many Francophone countries.
***
In order to fulfil their obligations under international human rights law, governments should remove unnecessary barriers facing patients who need access to palliative care. The International Covenant on Economic, Social and Cultural Rights, to which Morocco is a party, requires that the government of Morocco act expeditiously to ensure access to palliative care and pain medicines.
Morocco has clearly identified palliative care as an important health issue. It has already eliminated a number of key barriers to providing this health service and has initiated steps to boost its availability, especially at the tertiary level. As a result, it is well positioned to take on the important task of ensuring palliative care is available to all Moroccans who need it.
But that will require the government to remove remaining barriers to the provision of palliative care and to significantly step up its efforts to ensure palliative care services become available throughout the public healthcare system. In doing so, Morocco has the potential to be a leader in Francophone Africa, a region where palliative care is extremely limited.
Key Recommendations
To the Government of Morocco
- Establish general palliative care centers at each of the five university hospitals.This is an essential step in Morocco’s efforts to integrate palliative care into its healthcare system. Not only do these hospitals attend to all types of patients with chronic illnesses, they also play a key role in the academic and clinical training of healthcare workers and in conducting research, thus addressing three urgent needs identified in this report.
- Establish palliative care centers at all regional oncology centers and the pediatric oncology hospital in Rabat. Ensure that all currently operational regional cancer centers, as well as ones that are newly opened, have palliative care units. These centers can then serve as the basis for the further decentralization of palliative care. A palliative care unit at the pediatric oncology unit in Rabat could form the basis for developing pediatric palliative care and decentralizing it over time.
- Integrate pain treatment and ensure the availability of oral opioid analgesics at secondary care facilities. Ensure that all local, provincial, and regional hospitals have staff adequately trained in assessing and managing pain and that oral morphine is available. It should ensure that there are pharmacies near these hospitals that stock oral morphine or, alternatively, the hospital pharmacies should dispense it to outpatients.
- Remove remaining structural barriers to palliative care. In particular, develop a program of continuing medical education for active healthcare workers; ensure medical insurance covers medications for outpatients requiring palliative care; counter misunderstandings and fear around opioid analgesics; and increase the number of physicians with prescription privileges.
Methodology
This report is based on an assessment conducted between September 2014 and March 2015, including visits to Morocco in September 2014 and January 2015. Field investigation was conducted primarily in Casablanca and Rabat. Additional research was conducted in regional capitals and smaller cities in four northwestern regions. We also conducted extensive desk research regarding palliative care availability in various other parts of the country.
Over a total of five weeks in Morocco, three Human Rights Watch researchers conducted 85 interviews with a wide variety of stakeholders, including 24 people with cancer or their relatives; 35 healthcare workers, including oncologists, anesthesiologists, and palliative care doctors; 17 private pharmacists; and representatives of the WHO; the Ministry of Health; the Lalla Salma Foundation; Laprophan, a pharmaceutical company; national pharmaceutical associations; and The National Order of Doctors.
Interviews with patients and their relatives were conducted at a variety of hospitals. They were conducted in private whenever possible. Interviews were semi-structured and covered a range of topics related to palliative care and pain treatment. Before each interview, we informed interviewees of its purpose, the kinds of issues that would be covered, and asked whether they wanted to participate. We informed them that they could discontinue the interview at any time or decline to answer any specific questions, without consequence.
No incentives were offered or provided to persons interviewed. We have disguised the identities of all patients, relatives, and healthcare workers we interviewed in this report to protect their privacy, except when they specifically agreed that their real name could be used.
Most interviews were conducted in French or Arabic with the assistance of an interpreter. Some interviews were done in English.
Between October 2014 and January 2015, Human Rights Watch repeatedly sought permission from government officials in the Ministry of Health to conduct interviews with Ministry of Health officials, as well as healthcare providers, hospital administrators, and patients in government health facilities. Although the Health Ministry initially indicated that it would issue a written permission for us to conduct interviews in public hospitals, as of June 2015, no such permission was issued. As a result, we were unable to interview all of the personnel whose views we sought.
In April 2015, Human Rights Watch presented a written memorandum with preliminary findings to the Ministry of Health along with a list of specific questions.
In June 2015, Human Rights Watch received a response from Dr. Abdelali Belghiti Alaoui, secretary general of the Ministry of Health. The response answered a number of our questions and raised issue with some of our preliminary findings and recommendations. The ministry’s response emphasized Morocco’s progress in expanding access to palliative care to date and stated a commitment to further steps. We have incorporated the ministry’s response in the relevant sections of the report.
This report builds on previous research by Human Rights Watch on access to palliative care in Morocco, published in the 2011 report, The Global State of Pain Treatment: Access to Palliative Care as a Human Right.
All documents cited in the report are either publicly available or on file with Human Rights Watch.
I. Background
Importance of Palliative Care and Pain Relief
With life expectancy increasing worldwide, the prevalence of non-communicable diseases (NCDs) and chronic illnesses is rising rapidly.[1] NCDs, such as cancer, heart disease, diabetes, and respiratory illnesses, are by far the leading cause of mortality in the world, accounting for 63.5 percent of all deaths.[2] They and other chronic illnesses are often accompanied by pain and other distressing symptoms, such as breathlessness, nausea, anxiety, and depression (see Table 1).
Table 1: Prevalence of Symptoms for Chronic Illnesses
|
Symptom |
Cancer |
COPD* |
Chronic Heart Failure |
Renal Disease |
Dementia |
AIDS |
Parkinson’s |
Motor Neuron Disease |
MS* |
|
Pain |
30-94% |
21-77% |
14-78% |
11-83% |
14-63% |
30-98% |
42-85% |
52-76% |
68% |
|
Dyspnea |
16-77% |
56-98% |
18-88% |
11-82% |
12-52% |
43-62% |
--** |
81-88% |
26% |
|
Nausea |
2-78% |
4% |
2-48% |
8-52% |
8% |
41-57% |
-- |
-- |
26% |
|
Fatigue |
23-100% |
32-96% |
42-82% |
13-100% |
22% |
43-95% |
42% |
-- |
80% |
|
Confusion |
2-68% |
14-33% |
15-48% |
35-70% |
-- |
-- |
24% |
24% |
-- |
|
Constipation |
4-64% |
12-44% |
12-42% |
8-65% |
40% |
19-35% |
24% |
52-56% |
46% |
|
Diarrhea |
1-25% |
-- |
12% |
8-36% |
-- |
29-53% |
-- |
-- |
-- |
|
Depression |
4-80% |
17-77% |
6-59% |
2-61% |
46% |
17-82% |
15-50% |
23% |
15% |
|
Anxiety |
3-74% |
23-53% |
2-49% |
7-52% |
8-72% |
13-76% |
5-62% |
19% |
24% |
*COPD: Chronic Obstructive Pulmonary Disease; MS: Multiple Sclerosis.
**Indicates that no data was available for this specific symptom.
Red: Indicates an average of the lowest and highest available data on the prevalence of a specific symptom of 50 percent or greater.
Yellow: Indicates an average of the lowest and highest available data on the prevalence of a specific symptom of 25 percent or greater.
Palliative care seeks to improve the quality of life of patients, both adults and children, facing life-limiting or advanced illness. Its purpose is not to cure a patient or extend his or her life, but rather to relieve pain and other physical and psychosocial problems. In the much-quoted words of Dame Cicely Saunders, the founder of the first modern hospice and a lifelong advocate for palliative care: palliative care is about “adding life to the days, not days to the life.” Although curative treatment may sometimes be available, palliative care seeks to reduce the burden and impact of these physical symptoms regardless of whether the underlying cause can be cured.
The World Health Organization (WHO) recognizes palliative care as an integral part of healthcare that should be available to those who need it.[4] While palliative care is often associated with cancer, a much wider circle of patients can benefit from it, including patients in advanced stages of neurological disorders and cardiac, lung, liver, or renal disease.[5] Indeed, the WHO and Worldwide Hospice and Palliative Care Alliance (WHPCA) estimate that over 65 percent of adults in need of palliative care have a chronic illnesses other than cancer.[6]
An important aspect of palliative care is addressing chronic, severe pain. Persistent pain has a profound impact on quality of life and can have physical, psychological, and social consequences. It can lead to reduced mobility and consequent loss of strength; compromise the immune system; and interfere with a person’s ability to eat, concentrate, sleep, or interact with others.[7] The physical effect of chronic pain and the psychological strain it causes can even influence the course of disease: as the WHO notes in its cancer control guidelines, “pain can kill.”[8] Social consequences include the inability to work; care for oneself, children, or other family members; participate in social activities; and find closure at the end of life.[9]
According to the WHO, “Most, if not all, pain due to cancer could be relieved if we implemented existing medical knowledge and treatments” (original emphasis).[10] The mainstay medication for the treatment of moderate to severe pain is morphine, an inexpensive opioid that is made of an extract of the poppy plant. Morphine is a controlled medication, meaning that its manufacture and distribution is strictly regulated both at the international and national levels.
Medical experts have recognized the importance of opioid pain relievers for decades. The 1961 Single Convention on Narcotic Drugs, the international treaty that governs the use of narcotic drugs, explicitly states that “the medical use of narcotic drugs continues to be indispensable for the relief of pain and suffering,”[11] and the WHO has recognized that strong opioids, such as morphine, are “absolutely necessary.”[12]
While pain is often a key symptom in people with life-limiting illnesses, palliative care is broader than just relief of physical pain. For example, many people with chronic illness experience shortness of breath—or dyspnea—a distressing symptom that makes the patient feel they can never get enough air.[13] The physical and psychological effects of dyspnea can cause depression, anxiety, and insomnia.[14] The psychological effects of dyspnea are particularly pronounced, as even mild alterations in breathing patterns may be “cognitively and emotionally interpreted as serious threats to health and life….”[15] Treatment protocols, such as breathing techniques, oxygen, and relaxation, have been shown to provide significant relief for some patients with dyspnea.[16] Increasingly, morphine has also been recommended to reduce the symptoms of dyspnea.[17]
People with life-limiting illness and their relatives also frequently confront profound psychosocial and spiritual questions as they face life-threatening, incurable, and often debilitating illness. Anxiety and depression are common symptoms.[18] Palliative care interventions like psychosocial counseling and spiritual support have been shown to considerably diminish the incidence and severity of such symptoms and to improve the quality of life of patients and their families.[19]
The WHO has urged countries, including those with limited resources, to make palliative care services available. The WHO recommends that countries prioritize implementing palliative care services both in medical institutions that deal with large numbers of patients requiring palliative care and in the community where it can be provided at low cost to people with limited access to medical facilities.[20]
The WHO has observed that these measures cost very little but can have a significant effect.[21] Indeed, as many countries face difficulty accommodating the increased demand for NCD services,[22] some studies have found that offering palliative care leads to overall cost savings for health systems by reducing the pressure on medical systems.[23]
In recent years, the World Bank and the WHO have urged countries to implement free universal health coverage to ensure that all people obtain the health services they need without suffering financial hardship.[24] Palliative care is one of the basic health services that the WHO says should be available under universal health coverage.[25]
Global and Regional Availability of Palliative Care
Despite the importance of this essential healthcare service, access to palliative care has lagged behind the development of other health services due to well-documented barriers in the areas of healthcare policy, healthcare education, and medication availability.[26] Indeed, a joint report by the WHO and WHPCA states that 98 countries have no known palliative care services.[27]
According to the International Narcotics Control Board (INCB)—the body charged with monitoring the 1961 Single Convention on Narcotic Drugs— “approximately 5.5 billion people, or three quarters of the world’s population … have inadequate access to treatment for moderate to severe pain….”[28] Due to limited access to essential medications, the WHO estimates that tens of millions of people around the world, including around 5.5 million end-stage cancer patients and one million people with AIDS, suffer from moderate to severe pain each year without treatment.[29]
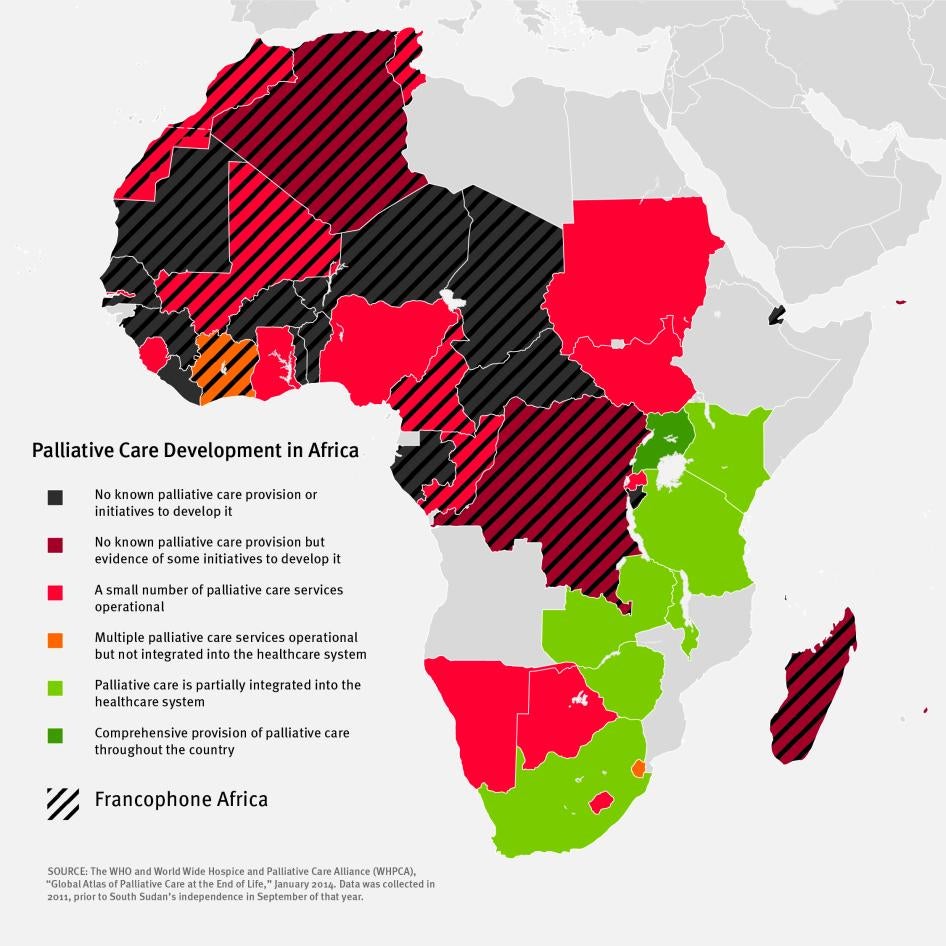
Palliative care development is particularly weak in Francophone Africa. A 2012 study, for example, found that 16 out of 22 Francophone African countries do not have any healthcare providers that offer palliative care. In contrast, the same study found that nearly all Anglophone African countries had at least some palliative care services (see Table II).
Francophone Africa also has some of the lowest rates of morphine consumption globally. The INCB classifies each country in the region, with the exception of Tunisia, as having “very inadequate” opioid availability.[30] More than two-thirds of the countries in the region for which data is available use so little morphine that it is not even sufficient to treat 5 percent of people dying in pain from cancer and AIDS (see Table III). In 2013, Human Rights Watch documented the devastating impact that lack of palliative care services had on patients and their families in Senegal, where many patients said they felt they had been abandoned in their agony.[31]
|
Table II: Comparison of Palliative Care Development in Francophone and Anglophone Africa[32] |
||||
|
Francophone Africa[33] WHPCA/WHO Level of Palliative Care Development |
Anglophone Africa WHPCA/WHO Level of Palliative Care Development |
|||
|
Benin |
Liberia |
|||
|
Burkina Faso |
Mauritius |
|||
|
Burundi |
|
Seychelles |
||
|
Central African Republic |
|
Botswana |
||
|
Chad |
The Gambia |
|||
|
Comoros |
Ghana |
|||
|
Djibouti |
Lesotho |
|||
|
Gabon |
Namibia |
|||
|
Guinea |
Nigeria |
|||
|
Mauritania |
Rwanda |
|||
|
Niger |
Sierra Leone |
|||
|
Senegal |
Sudan* |
|||
|
Togo |
Swaziland |
|||
|
Algeria |
Kenya |
|||
|
Democratic Republic of the Congo |
Malawi |
|||
|
Madagascar |
South Africa |
|||
|
Cameroon |
Tanzania |
|||
|
Congo |
|
Zambia |
||
|
Mali |
|
Zimbabwe |
||
|
Morocco |
|
Uganda |
||
|
Tunisia |
|
|
||
|
Côte d'Ivoire |
|
|
||
*Data was collected in 2011, prior to South Sudan’s independence in September of that year.
Grey: No known palliative care provision or initiatives to develop it.
Dark Red: No known palliative care provision but evidence of some initiatives to develop it.
Bright Red: A small number of palliative care services operational.
Yellow: Multiple palliative care services operational but not integrated into the healthcare system.
Light Green: Palliative care is partially integrated into the healthcare system.
Dark Green: Comprehensive provision of palliative care throughout the country.
|
Table III: Opioid Consumption Data for Francophone Africa[34] |
|||
|
Country |
Estimated Annual Cancer and AIDS Deaths with Moderate to Severe Pain (2012) |
Estimated Number of Terminal Cancer and AIDS Patients who: |
|
|
Are not Receiving Adequate Pain Treatment (Minimum Number) |
Could be treated with all Strong Opioids Consumed (percentage) |
||
|
Burundi |
6,933 |
-- |
-- |
|
Central African Republic |
7,237 |
-- |
-- |
|
Comoros |
329 |
-- |
-- |
|
Congo |
3,796 |
-- |
-- |
|
Djibouti |
848 |
-- |
-- |
|
Guinea |
5,931 |
-- |
-- |
|
Mauritania |
1,576 |
-- |
-- |
|
Niger |
5,419 |
-- |
-- |
|
Burkina Faso |
7,722 |
7,681 |
<1% |
|
Côte d'Ivoire |
22,939 |
22,827 |
<1% |
|
Gabon |
1,645 |
1,637 |
<1% |
|
Chad |
10,787 |
10,634 |
1% |
|
Democratic Republic of the Congo |
40,626 |
40,122 |
1% |
|
Mali |
7,991 |
7,915 |
1% |
|
Togo |
5,808 |
5,732 |
1% |
|
Cameroon |
25,049 |
24,497 |
2% |
|
Madagascar |
13,473 |
12,269 |
2% |
|
Senegal |
4,832 |
4,757 |
2% |
|
Benin |
4,568 |
4,402 |
4% |
|
Morocco |
18,838 |
15,163 |
20% |
|
Algeria |
17,860 |
13,971 |
22% |
|
Tunisia |
5,921 |
0 |
124% |
Grey: Country did not report opioid consumption to the INCB during 2010-2012.
Dark Red: Consumption of less than or equal to 2 percent of that needed to treat all cancer and HIV/AIDS patients with pain.
Bright Red: Consumption of between 2.1 and 5 percent of that needed to treat all cancer and HIV/AIDS patients with pain.
Yellow: Consumption of between 5.1 and 25 percent of that needed to treat all cancer and HIV/AIDS patients with pain.
Light Green: Consumption of between 25.1 and 99 percent of that needed to treat all cancer and HIV/AIDS patients with pain.
Bright Green: Consumption of equal to or greater than 100 percent of that needed to treat all cancer and HIV/AIDS patients with pain.
Map Comparing Francophone and Anglophone Africa
Background on Morocco’s Healthcare System
Morocco’s healthcare system is comprised of a public sector, a private non-profit sector, and a private for-profit sector.[35]
The public sector makes up the majority of the overall healthcare system, although the private sector is growing rapidly and now represents 32 percent of the healthcare system.[36] The public sector includes specialty hospitals and university hospitals (centres hospitaliers universitaires); regional, provincial, and local hospitals; and basic healthcare centers.[37] Although private sector options are available and offer higher quality care compared to their public counterparts, the services are much more costly, particularly for the approximately 21 million Moroccans who do not have health insurance or whose insurance only covers care at public health facilities.[38]
Morocco’s public healthcare system consists of three levels of care (see Chart I).[39] University hospitals and specialty hospitals, all tertiary care facilities, are the most sophisticated healthcare facilities with generally well-stocked pharmacies and a broad range of specialists, advanced medical equipment, and treatment options. These facilities are located only in major cities. Many smaller cities have regional, provincial, or local hospitals. These secondary care facilities have inpatient and outpatient facilities available but may only have a limited number of key specialists. Local hospitals, for example, have essential medical disciplines, such as obstetrics, general medicine, and general surgery, but no specialist in ophthalmology, gastroenterology, or cardiology.[40] Finally, at health centers, available in small towns, there may only be a general care physician or a traveling nurse or midwife who offers basic care.
The ratio of healthcare workers and facilities to the population is comparatively low in Morocco. According to the WHO’s most recent data, Morocco had a substantially lower number of hospital beds, physicians, and nurses and midwifes per citizen than its North African neighbors.[41] In 2005-2012, for example, the WHO reports that Morocco had approximately 6 physicians for every 10,000 individuals, compared to 12 physicians per 10,000 in Algeria and Tunisia, 19 in Libya, and 28 in Egypt.[42]
As of 2012, Morocco’s per capita health expenditure was US$190 per person and its total health expenditure was 6 percent of GDP.[43] Although Morocco’s health expenditure is relatively similar to that of its North African neighbors, a significantly smaller proportion comes from public funds. In 2012, for example, Morocco’s state budget accounted for approximately 34 percent of total health expenditures, compared to 59 percent in Tunisia, 77 percent in Libya, and 84 percent in Algeria.[44]
***
Since 2005, the Moroccan government has sought to broaden health insurance coverage for its population. Prior to the reforms initiated that year, formal health insurance coverage in Morocco was voluntary and only 17 percent of the population—more than two-thirds of them government employees covered by a public insurance scheme—was insured.[45]
A small percentage of the population was covered through private insurance, while the vast majority of the population did not have health insurance. Low-income citizens could qualify for a “certificate of indigence” (certificate d’indigence) from their local government, which provided them with either free or low cost healthcare from public facilities. Those who did not qualify for this certificate could receive healthcare in public facilities at a subsidized rate.[46]
Since 2005, the government has instituted two major health insurance reforms. First, it introduced a compulsory health insurance program known as Assurance Maladie Obligatoire (AMO) that covers both salaried public and private sector employees.[47] Premiums for AMO are roughly split by employees and employers. AMO covers a fixed percentage—ranging from roughly 70 to 90 percent—of the cost of a number of medical interventions and medicines.[48] By 2012, 7.6 million Moroccans were covered by AMO (approximately 23 percent of the population).[49]
In 2011, the government launched another major reform establishing the Regime d’Assistance Medicale (RAMED), a public insurance scheme that provides coverage to low-income populations. RAMED largely replaces the “certificate of indigence” with a more formal system for providing free or reduced-cost healthcare services to those living in poverty. Candidates for the program are divided into two categories—urban and rural—and qualify based on factors such as household income or living conditions. Urban residents, for example, can receive free healthcare services if, among other qualifications, they make less than 3,767 MAD (US$423) per year.[50]
In theory, people who qualify for RAMED can receive essential healthcare services in public hospitals and public health centers around the country, but the facilities that they have access to may not always provide them with the care and medicines that they need.[51] Indeed, public health facilities often suffer from underfunding,[52] poor quality of reception and care,[53] and are difficult to access for rural Moroccans.[54] Similarly, RAMED only covers medications dispensed from public pharmacies. With few exceptions, public pharmacies only supply medications to patients during hospitalization.[55] Thus, RAMED’s coverage only extends to “drugs and pharmaceuticals administered during [inpatient] treatment.”[56] Outpatients have to fill and pay for their prescriptions at private pharmacies.
As of 2013, 5.6 million Moroccans were covered by RAMED—approximately 17 percent of the population—bringing the total of medically covered Moroccans to just over 50 percent of the population.[57] The other nearly 50 percent of the Moroccan population is uninsured. In particular, insuring those who are eligible but not receiving RAMED (approximately 2.5 million people) and those working within the informal economy (approximately 10 million people) remain large obstacles to achieving universal health coverage.[58]
In the coming years, Morocco plans to continue efforts to expand health coverage to larger segments of the population, including those noted above.[59] Notably, the government sought and received a combined US$166 million in financing from the African Development Bank and European Union for continued health insurance reform efforts.[60]
History of Palliative Care in Morocco
In the early 1990s, palliative care and pain treatment were virtually non-existent in Morocco.[61] In 1994, Dr. Mati Nejmi, then chief of anesthesiology at the National Oncology Institute, recognized the urgent need for this health service and engaged Morocco’s health policy makers and international groups in an effort to introduce palliative care in Morocco. Over the following years, this work achieved a number of significant milestones, including:
- Introducing oral morphine for the first time in Morocco (1995);
- Opening the Moroccan Society of Pain and Palliative Care (1996);
- Constructing the first palliative care unit in Morocco, adjoining the National Oncology Institute in Rabat (2005); and
- Developing the Sectoral Health Strategy (SHS) (2012) as well as in its National Cancer Prevention and Control Plan (NCPCP) (2010), which include specific palliative care goals.[62]
These improvements make clear that Morocco is well positioned to take on the important and necessary task of ensuring palliative care and pain treatment is available to all Moroccans who need it. In doing so, Morocco has the potential to be a regional leader in Francophone Africa, a region where palliative care is extremely limited.
II. Palliative Care in Morocco and Patients’ Experiences
Availability of Palliative Care in Morocco
Like many low and middle income countries, Morocco is currently experiencing an epidemiological transition with a decreasing prevalence of infectious diseases and an increased burden of NCDs and other chronic illnesses. In 2013, the WHO estimated that NCDs were responsible for 75 percent of deaths in the country.[63] As a result, more Moroccans than ever develop chronic conditions that are accompanied by pain and other symptoms that, if left untreated, can seriously undermine their quality of life.
And the burden of chronic illness is likely to rise. The percentage of people over 65, the segment of the population most affected by these illnesses, is expected to nearly double over the next 15 years.[64] In that same period, the incidence of cancer is expected to nearly triple.[65] As Morocco’s health strategy puts it, “this will lead to a progressive increase in demand for major hospital care to provide treatment for chronic and degenerative diseases.”[66] This transition has resulted in a significant and sustained increase in the need for palliative care.[67]
Based on WHO estimates for palliative care needs in the Middle East region, around 62,000 Moroccans, including 6,000 children, require palliative care each year.[68] Tens of thousands of them will experience significant pain and may need treatment with opioid analgesics, such as morphine. Advanced cancer and AIDS alone cause moderate to severe pain in nearly 19,000 Moroccans annually.[69]
Morocco’s healthcare system currently does not have nearly the palliative care capacity to attend to all these patients. Our research identified two palliative care units within Morocco’s public healthcare system, in Casablanca and Rabat. Each of these units is based in a tertiary-level cancer hospital and attends only to people with cancer (see Map I below).
While the WHO recommends that countries integrate palliative care at all levels of care, including in the community, our research did not find any palliative care providers at secondary levels of care. Indeed, interviews with medical personnel at eight secondary care facilities in eight different cities and towns, some as far as 150kms from the nearest tertiary care facility, revealed that none were offering palliative care or had oral morphine.
Our research also revealed that few private facilities offer palliative care.[70] In 2013, Dr. Mati Nejmi, former head of anesthesiology at the National Oncology Institute, opened the first private palliative care practice in the country in Casablanca.[71] This means that there are large parts of Morocco—especially the south and the northeast—without any palliative care providers at all.
Although some healthcare providers have integrated palliative care interventions into their general practice, particularly tertiary level hospitals, Human Rights Watch believes that to be the exception, as most facilities simply do not have staff trained in palliative care or access to key palliative care medications, such as morphine.
Data on the use of opioid analgesics suggests that there is a major gap in the treatment of moderate to severe pain in Morocco. The latest available data indicates that Morocco consumes an annual amount of morphine sufficient to treat approximately 3,700 patients with terminal cancer or AIDS per year—around 20 percent of those who need it.[72] This estimate does not take into account the morphine needs of people with pain due to illnesses such as heart and lung disease or diabetes, even though it is a common symptom of each of these conditions. Since morphine is also used to treat pain caused by trauma and surgery, a considerable proportion of the morphine that Morocco consumes is not actually used in palliative care.
Despite this major gap, Morocco has made considerable progress in increasing morphine availability. Consumption has consistently increased since 1995, when morphine was first introduced in Morocco (see Graph I below). Significantly, between 2012 and 2013, Morocco nearly doubled its morphine consumption. However, using INCB classification, Morocco’s 2013 morphine consumption is still considered “very inadequate.”[73]
|
The Fate of Patients with Non-Oncological Disease While patients with advanced cancer have very limited access to palliative care in Morocco, those with advanced non-oncological illnesses have almost none. Yet, the WHO and WHPCA estimate that over 70 percent of adults in need of palliative care from the WHO’s Eastern Mediterranean region have a chronic illness other than cancer.[74] In other words, around 40,000 adults in Morocco require palliative care each year for conditions other than cancer. The WHO has identified the following non-oncological diseases as conditions in which palliative care may be required: cardiovascular diseases, chronic obstructive pulmonary diseases, kidney failure, chronic liver disease, multiple sclerosis, Parkinson’s disease, rheumatoid arthritis, neurological diseases, Alzheimer’s disease and other dementias, and congenital anomalies and infectious diseases such as HIV/AIDS and drug-resistant tuberculosis.[75] As Table I (see page 10) demonstrates, people with these conditions often face multiple symptoms that undermine their quality of life. For example, up to 78 percent of people with end-stage chronic heart failure, Morocco’s number one killer, experience pain; up to 88 percent experience breathlessness; up to 48 percent experience nausea; and up to 59 percent experience depression.[76] |
Experience of People in Need of Pain Treatment
Over the course of our research, we collected testimony from two dozen patients and their families about the challenges they faced while accessing palliative care. While a few patients reported having access to comprehensive palliative care—mostly those from Rabat and Casablanca—most had limited access or accessed it only with difficulty, often with long delays and after significant suffering from pain and other symptoms.
Yet, even they were the fortunate ones as they ultimately accessed palliative care. With opioids reaching a small fraction of those who need it, many more spend their last weeks and months without access to adequate care and often die under excruciating circumstances.
Suffering Caused by Untreated Pain
My mother would cry out in pain. My mother is a very strong woman. She wanted to reach inside her own body to take the pain away.
—Daanya Kassem, daughter of a woman with abdominal cancer[77]
As noted above, pain has devastating physical, psychological, and social consequences for the people it affects and their loved ones. In interviews with Human Rights Watch, patients in Morocco who had experienced pain described in stark terms these consequences and the resulting suffering.
Adil Akram, a 29-year-old man who battled cancer in his leg for years, told Human Rights Watch: “Four months ago I started feeling pain…. Because of the pain I couldn’t sleep. I couldn’t talk to my friends. I wanted to crush my head against the wall and shake…. …. My pain tears me apart.”[78] Adil said that the pain made it difficult for him to sleep, move around, and eat, and had forced him to stop working. He had become socially isolated, no longer wanting to meet with friends or loved ones.
Habib Saad, a 59-year-old man with lung cancer, echoed Adil’s story: “I just endured the pain, barely sleeping, barely watching television, barely talking to my family…. [When I’m in pain], I can’t think about anything. I think only about myself.”[79]
Pain also takes a heavy toll on caregivers. Maya Jalali, for example, the daughter of Haydar Jalali, a man with abdominal cancer, described the heavy burden of watching her father in pain without being able to help. She told Human Rights Watch:
Before the morphine, he couldn’t sleep, he couldn’t even sit…. He used to scream all the time and would require us to stay with him…. When you see someone feeling pain, you feel pain too. He is your father and you don’t know what to do to help him. If I could take part of the pain, I would.[80]
Delayed Access to Palliative Care
Some patients have received pain treatment before arriving here, but there is morphineophobia in Morocco. Before patients come here, they would usually only get paracetamol, tramadol, or codeine. Sometimes that is inadequate—frequently we need to prescribe morphine.
—Medical oncologist, regional oncology center[81]
Many people we interviewed described significant delays in accessing palliative care. As it is available only in a few major cities, these people initially sought care at hospitals that did not have any staff trained in providing this health service and who, as a result, did not properly assess or treat their symptoms. These people described severe suffering and intense anguish as the doctors at these healthcare institutions struggled to attend to their urgent health needs. The case of Zayan Ebrahim, presented in the summary, is illustrative.
Even at hospitals that do have trained palliative care physicians, patients may suffer significant untreated pain when they are not referred in a timely manner. For example, Aadam Khalil, a 75-year-old imam with skin cancer that had spread to his prostate and bones, experienced pain for several months before his treating physician at one of Morocco’s regional oncology centers sent him to the palliative care unit. We interviewed Aadam’s son-in-law, Mahmud, because Aadam could not speak due to his illness.
Mahmud told Human Rights Watch that Aadam had been receiving curative treatment at a regional oncology center when he began to experience severe pain. Although the hospital had a palliative care specialist, his physician initially did not refer him but tried to manage his symptoms himself. Mahmud said:
He has pain in his arms and private parts. He only cries when he suffers pain. He cannot speak…. He was suffering with pain for six months before receiving morphine. The doctors administered other sorts of medications before the morphine. They were not adequate. Maybe they would take away the pain for a few minutes.[82]
When Human Rights Watch saw Aadam he had eventually been sent to the palliative care specialist. Mahmud said treatment of his father-in-law’s pain had improved, but was still not fully under control.
Physicians echoed this testimony. Dr. Zakaria Belkhadir, chief of anesthesiology at the National Oncology Institute in Rabat, told Human Rights Watch: “We see a lot of patients who arrive on paracetamol and they need stronger pain medications. But doctors [especially outside of the main city] don’t prescribe morphine.”[83] Dr. Laila Hessissen of the children’s hospital in Rabat said: “When patients come in from other areas they often come into [the hospital] with pain. The first thing people do is ask for pain treatment.”[84]
Long Distances to Palliative Care Providers
We are only at the beginning of our goal, which is to provide people experiencing the most difficult times in their lives the opportunity to receive appropriate care nearby their families.
—Dr. Mati Nejmi, former chief of anesthesiology at the National Oncology Institute in Rabat[85]
As only a few specialty hospitals in Morocco offer palliative care, many patients who require it live far from the nearest provider. This means they often have to travel long distances to access palliative care, frequently on public transport. For curative care, the cost and inconvenience of such travel may be unavoidable as primary and many secondary care facilities do not have the specialists, diagnostic equipment, and/or laboratory capacity to properly manage patients with complex illnesses. This is not true, however, for palliative care, which for most patients does not require any complex interventions and can be easily and inexpensively provided at lower levels of care.
Morocco’s Sectoral Health Strategy and National Cancer Prevention and Control Plan clearly both call for decentralized palliative care provision and the establishment of palliative care networks. Yet, palliative care services have not yet been decentralized, making it impossible for many people to receive it close to their homes.
Distance poses a dilemma for patients, particularly for patients with advanced illness for whom travel can become increasingly difficult—if not impossible. They often end up having to choose between three unenviable options:
- Enduring the hardships of traveling, even in a fragile condition, in order to receive optimal care;
- Sending relatives—often their only caregivers—to get medications. In such cases, they do not see the physician themselves, compromising the ability of the palliative care team to provide proper care; or
- Staying home and getting no care at all.
The cost of travel is a second dilemma. Patients and their families have often already incurred extensive costs, frequently accumulating considerable debt, paying for diagnostic tests and curative care. Even when the palliative care services and medications are offered free of charge, travel often drives them deeper into poverty.
Various people interviewed by Human Rights Watch described the hardships of having to travel long distances to get access to palliative care and pain management. Maya Jalali told Human Rights Watch she had to frequently make the 120km trips from her home in central Morocco to receive palliative care medications for her father:
I only come to get medication, or when his pain is difficult to control. I take a bus. When I’m bringing my father, I take a private car because the bus is uncomfortable for him and the station is far from the hospital…. When I come alone, I pay 150 MAD (US$15.71). More when my father comes.
She said that she had stopped working when her father became ill, making the cost of transportation all the more burdensome.[86]
Rajiya Azam, the daughter of Luja Azam, a 75-year-old women with pancreatic cancer from Beni Mellal, central Morocco, echoed this sentiment. She said:
I have to come here for the medications. There is not a place near me to get them. Each time I come it’s a little different, sometimes I rent a car, sometimes I borrow a car, sometimes I take the bus. It takes about three hours by car and four hours by bus.[87]
Because of the long distances traveled to access palliative care services, many patients do not come to the hospital at all or as frequently as necessary. This creates significant challenges for palliative care providers and may result in lower quality care for the patient. As Dr. Asmaa El Azhari, the head of the palliative care unit at the regional oncology center in Casablanca, noted:
Apart from the difficulty for patients having to come all the way to Casablanca, I must manage these patients by phone. If a patient’s son call me and says, “the pain has gotten worse,” I don’t know why the pain has gotten worse and what I should do to treat it.[88]
Another important consequence of the lack of a decentralized approach to palliative care is the fact that highly specialized healthcare providers at tertiary hospitals end up caring for patients with health issues that could be addressed at lower levels of the healthcare system. This limits their capacity to treat patients with complex symptoms, to conduct research, and to teach—all critical functions of specialists as identified in Morocco’s National Cancer Prevention and Control Plan.[89]
Recognizing the burden excessive travel has on patients, the WHO recommends the provision of community-based palliative care. In line with that goal, Professor Abdellatif Benider, the chief oncologist at Casablanca’s regional oncology center said: “In Morocco the characteristic of the family is that they show solidarity. They prefer the patient to die in their home. But they need the assistance of doctors.”[90] Professor Khalid Hassouni, the chief oncologist at Fez’s regional oncology center, describing his desire to develop home-based care in Fez, adds: “I just don’t want to see patients suffer. I don’t tolerate this. It is better to treat patients at their homes with their family. It’s difficult for them to come to the hospital.”[91]
The Positive Effect of Palliative Care on Patients’ Lives
I thank God for morphine. My life is better.
—Rabail Mannan, 30-year old women with cervical cancer[92]
As noted above, palliative care providers can generally control symptoms from life-limiting illnesses well, often with basic medications and interventions. Morphine and other opioid analgesics are highly effective in relieving cancer pain. Similarly, basic counseling and other palliative care interventions can prevent or greatly mitigate suffering due to psychosocial and other symptoms. Several of the people we interviewed told us how dramatically their quality of life had improved once they received access to palliative care services and their pain or other symptoms were under control.
For example, Habib Saad, a man with lung cancer, told Human Rights Watch: “I would die if not for the [palliative care unit]. There’s no other place I can go…. I’m happy because I’m [mostly] free of pain.”[93]
Jaleel Mannan, a 40-year-old women with breast cancer, shared this sentiment:
Because of the pain, I could not sleep. I could not even drink water. The pain started at my abdomen and went down to my feet…. My pain was a ten. Now the pain is a five. If it wasn’t for the medications, I couldn’t stay here and talk to you. Now from time to time I feel pain, but it was nothing like it was during the time before I received morphine.[94]
III. Barriers to Accessing Palliative Care in Morocco
The WHO and its decision-making body, the World Health Assembly (WHA), recommend the integration of palliative care into national health systems. To achieve this, the WHO recommends that governments formulate and implement a number of specific policies that it considers essential for expanding palliative care, including:
- Health system policies to ensure the integration of palliative care into the structure and financing of national health care systems at all levels of care;
- Policies for strengthening and expanding human resources, including education and training of health care professionals, in order to ensure adequate responses to the palliative care needs, together with training of volunteers and education of the public;
- A medicines policy in order to ensure the availability of essential medicines for the management of symptoms, including pain and psychological distress, and in particular, opioid analgesics for relief of pain and respiratory distress; and
- A policy for research into assessing the needs for palliative care and identifying standards and models of service that work, particularly in limited resource settings.[95]
The WHO has noted that such measures, fundamental for the development of palliative care, “cost very little but can have a significant effect.”[96] A WHA resolution on palliative care unanimously adopted on May 23, 2014, closely mirrors these recommendations.[97]
These recommendations also correspond closely with several obligations under the right to health. The Committee on Economic, Social and Cultural Rights, the body that monitors the implementation of the right to health as articulated in the International Covenant on Economic, Social and Cultural Rights (ICESCR),[98] has held that countries must adopt and implement a national public health strategy and plan of action and ensure access to essential medicines as defined by the WHO.[99] It has identified providing appropriate training for health personnel as an obligation “of comparable priority.”[100] Failure to take steps in these areas may result in a violation of the right to health.
Integrating Palliative Care into the Healthcare System
According to the WHO, national health system policies should promote the integration of palliative care into the structure and financing of national healthcare systems at all levels of care. In these policies, the emphasis should be on primary, community, and home-based care.[101]
The right to health requires states to take the steps necessary for the “creation of conditions which would assure to all medical service and medical attention in the event of sickness” (emphasis added).[102] The Committee on Economic, Social and Cultural Rights has held that people are entitled to a “system of health protection which provides equality of opportunity for people to enjoy the highest attainable level of health.”[103] In other words, health services should be available for all health conditions, including chronic or terminal illness, on an equitable basis.
The basic idea behind the WHA resolution and WHO recommendations is that patients should receive palliative care as close to their homes as possible. A patient who receives curative cancer treatment at a tertiary care facility should be able to receive palliative care at that facility while in curative treatment but should, if their condition allows, be referred to their primary care provider near their home should their cancer become incurable. Conversely, a palliative care patient who is attended to at primary care level but has complex symptoms that a primary caregiver cannot properly address should be referred to secondary or tertiary levels of care.
To receive palliative care near their home, patients must have access to a doctor who is trained to treat at least basic symptoms common in patients with life-limiting illnesses and has the ability to prescribe essential medications for the treatment of these symptoms. At higher levels of care, where many patients with complex symptoms are seen, multidisciplinary palliative care teams should be available.
Morocco has clearly identified developing palliative care as a priority. Its Sectoral Health Strategy (SHS) for 2012-2016 and National Cancer Prevention and Control Plan (NCPCP) for 2010-2019 set out a vision for the development of a palliative care system that is broadly aligned with WHO and WHA recommendations. The documents call for the creation of palliative care networks; the development of external palliative care consultations; and the institutionalization of pain treatment at all levels of the healthcare system.
The NCPCP notes that “an overview of palliative care reveals major problems” that need to be addressed, identifying, among others:
- Insufficient training of professionals in the palliative care field;
- Lack of human resources: doctors, nurses, physiotherapists, auxiliary nurses, etc.;
- Lack of recovery centers adapted to general and terminal palliative care;
- Insufficient follow-up of palliative care after return to the home; and
- Absence of supportive care and civic culture regarding end-of-life and death issues.[104]
The NCPCP sets two ambitious goals, to be achieved by 2019: “To have a nationwide palliative care network” and “support 100 percent of [cancer] patients requiring palliative care.”[105] The SHS does not provide any analysis of the current palliative care situation or set specific goals, although the action points it identifies are similar to those of the NCPCP (see Sectoral Health Strategy text box).
The NCPCP contains a detailed breakdown of specific measures required to realize the broad vision for Morocco’s palliative care system for people with cancer, organized in four categories: develop pain management; ensure family and social assistance; ensure development and extension of care networks in palliative care; and develop research on palliative care.
These action points cover each of the four areas—policy, education, medicine availability, and research—that the WHO identifies as essential for the development of palliative care and support a decentralized approach to palliative care. For example, the measures under the category on pain management cover the institutionalization of pain management across the healthcare system; legal and regulatory change to improve access to pain medicines; development of educational materials and protocols; and public information campaigns to educate the public.
The NCPCP, however, does not clearly determine a specific timeline or determine what government or other agencies are responsible for the implementation of these measures, except for the construction of palliative care units in Casablanca, Marrakesh, and Fez, planned for 2011-2013 (the palliative care centers in Marrakesh and Fez have not yet been built).[106]
The plan allocates a total of 86 million MAD (approximately US$8.7 million) to the implementation of the palliative care components over the course of the 10-year period it covers, including 5 million MAD for developing pain management, 6 million for social support, and 75 million for developing the palliative care network.[107] No budget is allocated to palliative care research. The budget does not indicate which government agencies will receive these funds.
The budget allocations for palliative care make up 1 percent of the overall budget under the NCPCP—compared to 88 percent for diagnosis and curative treatment.[108] This seems a paltry sum given that the NCPCP itself recognizes that the difficulties with access to healthcare services results in many patients being “diagnosed at very advanced stages of the disease,” when curative interventions are of limited utility.[109] According to Dr. Mati Nejmi and Dr. Laila Hessissen, 60-70 percent of cancer patients are diagnosed in late stages of the disease.[110] The NCPCP notes that 96 percent of individuals with lung cancer, the most common form of cancer in Moroccan men, are diagnosed in stages III and IV.[111]
In contrast to the Moroccan plan, the WHO has pointed out that in “countries with limited resources, it is not logical to provide extremely expensive therapies that may benefit only a few patients, while the majority of patients presenting with advanced disease and urgently in need of symptom control must suffer without relief.”[112]
Given the above, it is perhaps not surprising that Human Rights Watch’s analysis of the implementation effort—to the extent we have been able to check progress given limitations on our access to healthcare facilities and government officials—has found that, more than halfway through the NCPCP’s cycle, progress has been uneven and limited in many areas. A number of key findings include:
- Little progress has been made to date on the development of the decentralized palliative care network the NCPCP envisions. While a palliative care center was created in Casablanca, none have been anywhere else in the country;
- Opioid analgesics remain largely unavailable outside tertiary health facilities. The controlled substances law has been amended to increase the maximum prescription period for opioid analgesics, but few steps have been taken to counter physicians’ and pharmacists’ fears and misconceptions around these medicines or to increase the number of physicians with prescription privileges;
- Limited progress toward the decentralization of pain management. Our research suggests pain management committees at regional and provincial hospitals have either not yet been established or are not functioning effectively; and
- While NCPCP identifies developing research on palliative care needs and practices as an area for action, we were unable to identify any efforts by the government to conduct research on palliative care. The NCPCP does not allocate any budget to palliative care research.
|
The Sectoral Health Strategy In 2012, Morocco adopted a Sectoral Health Strategy (SHS) for 2012-2016 that focuses on a number of key health priorities for the country, including access to health services, maternal and child health, care for vulnerable populations, epidemiological surveillance, non-communicable diseases, development of resources, and health governance. The strategy formulates action points for each of these areas. The section on non-communicable diseases (NCDs) sets out a number of action points on pain treatment and palliative care. In particular, it states: Action 80: Establishment of a pain management strategy.
Action 81: Establishment of a palliative-care development strategy.
Action 80 and 81 are critically important to addressing the needs of non-cancer patients who require palliative care and were welcomed by the INCB.[114] While they identify the elements of palliative care and pain treatment strategies, it is not clear who should develop the actual strategies and implement them, nor does the SHS specify a budget for doing so. To date, these strategies have not yet been developed. |
With four-and-a-half years left in the cancer strategies cycle, however, the government still has an opportunity to refocus its efforts and make considerable progress towards its palliative care goals. Significantly, the Ministry of Health told Human Rights Watch that they are undertaking a review of the NCPCPs progress to date and anticipate that palliative care will arise as a priority issue.[115]
Integrating Palliative Care into Healthcare Financing
Although the right to health does not require states to offer health services and medications free of charge, they should be “affordable for all.”[116]The WHO adds that the use of palliative care services “must not lead to financial hardship, especially among … populations living in vulnerable situations” and recommends that national health systems promote the integration of palliative care into healthcare financing as part of efforts to promote universal health coverage.[117]Since 2011, Morocco’s constitution explicitly recognizes a right to health coverage for its citizens, but to date, health insurance schemes cover only about 50 percent of the population.[118] The remainder of the population has to pay for health services out of pocket.
Palliative Care Coverage under Morocco’s Insurance Schemes
In principle, both of Morocco’s public insurance schemes, RAMED and AMO, cover the provision of palliative care. Our research, however, found that coverage of palliative care for many RAMED and AMO clients is not effective. In other words, while palliative care is theoretically covered, they cannot actually get it or key elements are not included in the coverage.
The biggest single impediment to effective insurance coverage of palliative care is the fact that the number of healthcare providers that offer it is extremely limited. People with cancer who live outside major cities have no option but to travel in order to receive care. For patients who require palliative care for other illnesses, the services are almost entirely unavailable. Patients with AMO could seek care from private palliative care providers, as their insurance covers service provided by private hospitals, but there is only one known private palliative care service in the country.
As noted above, RAMED covers medications used during hospitalization as long as they are included within a list of reimbursable medicines. However, it provides no coverage for medications prescribed to outpatients (cancer patients who are receiving outpatient care at regional cancer centers can get free medications through the joint Lalla Salma Foundation/Ministry of Health ACCESS program).[119] Thus, outpatients with RAMED coverage have to fill prescriptions at private pharmacies even for medications that are on the RAMED list. As palliative care patients tend to receive most of their care as outpatients, this significantly limits the effectiveness of the coverage of palliative care through RAMED.[120] AMO does cover medicines prescribed to outpatients and provides patients with substantial reimbursements.
Finally, neither RAMED nor AMO covers any costs incurred by patients who need to travel to other cities in order to receive care or treatment that is not available where they live. As noted above, the fact that palliative care services are only available in major cities means that many patients or their relatives must travel long distances, sometimes as far as five hours, to receive palliative care. One patient noted that her monthly trips to the regional oncology center cost 150 MAD (US$15.71) or more, roughly two-thirds of the monthly cost of
the morphine she was purchasing.[121] Measure 68 of the NCPCP recognizes the burden of travel expenses borne by patients and calls for “financial coverage for safe transport from the hospital to the home, and from the home to the hospital.”[122]
|
Integrating Palliative Care into the Healthcare System: Panama Through a combination of legal and regulatory reform, Panama, a middle-income country, has taken large strides to improve access to palliative care. Panamanian law grants patients a right to receive palliative care, requires all hospitals to have palliative care units, and places responsibility on primary health centers for providing palliative care to patients who require it over extended periods of time.[123] In 2011, Panama’s Health Ministry adopted a national palliative care strategy to help implement the law.[124] The philosophy behind the strategy is that patients should always receive care as close to home as possible. It sets out a model that links the different levels of the healthcare system so that patients can move easily between them depending on their situation. A key role in this model is assigned to Panama’s regional hospitals, all of which must have multidisciplinary palliative care teams. These teams not only offer clinical care but are responsible for training healthcare workers at the primary level of care; offering them ongoing support in the care for patients; and working with nongovernmental groups, such as NGOs and churches, to develop community support for palliative care. The multidisciplinary teams are also the link between the different levels of care, facilitating referrals up and down the chain. Panama has made significant progress with implementing this strategy. Each of the country’s nine regions has a palliative care coordinator, more than half of the regions have active palliative care programs, and the number of patients receiving palliative care has risen steadily. Even so, challenges remain, especially in remote regions, within the social security system, and in the provision of palliative care to children.[125] |
Palliative Care Education for Healthcare Workers
[Doctors] are not aware of the importance of palliative care. We must add palliative care now to the training of doctors.... If we start now, the next generation of doctors will all know how to [provide] palliative care.
—Dr. Mati Nejmi, former chief of anesthesiology at the National Oncology Institute in Rabat[126]
Adequate training and education for healthcare workers in palliative care is essential to rolling out this healthcare service.[127] Indeed, in many countries, the lack of such training is the single greatest barrier to providing palliative care.
The Committee on Economic, Social and Cultural Rights considers appropriate training of healthcare workers an obligation of key importance.[128] Accordingly, the WHO recommends that “education about palliative care (including ethical aspects) is offered to students in undergraduate medical and nursing schools and to healthcare providers at all levels….”[129] The May 2014 World Health Assembly resolution calls on countries to include palliative care as an “integral component of the ongoing education and training offered to care providers” and specifies:
- basic training and continuing education on palliative care should be integrated as a routine element of all undergraduate medical and nursing professional education, and as part of in-service training of caregivers at the primary care level, including health care workers, caregivers addressing patients’ spiritual needs and social workers;
- intermediate training should be offered to all health care workers who routinely work with patients with life-threatening illnesses, including those working in oncology, infectious diseases, paediatrics, geriatrics and internal medicine; and
- specialist palliative care training should be available to prepare health care professionals who will manage integrated care for patients with more than routine symptom management needs.[130]
The European Association for Palliative Care (EAPC) has developed a model curriculum for undergraduate and specialist palliative care training. It recommends that undergraduate medical students receive 40 hours of training in palliative care and pain management, including some clinical aspects of palliative care, and should be tested on their knowledge of the subject matter.[131] They also recommend that specialists receive an additional 40 hours of theoretical training and 160 hours of clinical training after specializing in another field, such as internal medicine.[132] The EAPC has not made any recommendations regarding the content of intermediate level training.
This layered approach to palliative care education is essential to integrating palliative care across all levels of the healthcare system, as the WHA resolution recommends. A healthcare system in which all healthcare workers have training in palliative care appropriate for their role allows patients to receive care as close to home as possible, thus sparing them arduous, expensive, and time-consuming trips to specialists. It also allows specialists to focus on the most complex cases while general practitioners can attend to routine ones, thus improving the efficiency of the system.[133] As Dr. Hessissen, a pediatric oncologist at the pediatric oncology hospital in Rabat, noted: “The best doctor to manage the patients is the proximate doctor. [But they] need to be trained.”[134]
Medical Education
Undergraduate Training
Morocco has five public universities with medical school programs located in Rabat, Casablanca, Marrakesh, Fez, and Oujda. Obtaining a degree in medicine from one of these universities involves a seven-year education and training program.[135] The first five years of the program consist mainly of theoretical instruction in essential sciences and medicine.[136] In the sixth and seventh year, students engage in a full-time externship and internship positions.[137]
Prior to 2015, as noted in Human Rights Watch’s 2011 report on the global state of pain treatment, palliative care had not been formally integrated into the undergraduate curricula for medical students.[138] While some medical schools offered content that touched on palliative care, there were no mandatory courses on the topic.[139] As a result, most current physicians in Morocco have no or limited knowledge of palliative care and lack any clinical exposure to this health service, greatly complicating efforts to integrate palliative care into the healthcare system.
This is about to change. Based on a recommendation by a joint Ministry of Health and the Ministry of Higher Education commission established in 2005 to reform medical studies in Morocco, the government is introducing changes to the national medical curriculum, which all public medical schools and two private medical schools located in Casablanca and Rabat must follow. Under the new curriculum, which will be taught starting in late-2015, all medical students will receive 20 hours of mandatory instruction on pain and palliative care during the fifth year of their medical training.[140]
As far as Human Rights Watch is aware, at time of writing, the exact content of the palliative care component of the new curriculum has yet to be developed. For successful implementation, it is essential that experienced palliative care providers participate in that process; that they teach the content to medical students; and that palliative care is included in examinations of the students. The new curriculum also does not include mandatory clinical exposure in palliative care for medical students in their final two years. Clinical work should be progressively incorporated into medical students’ training.
Although it will take some time for doctors who have taken this course to enter the workforce in meaningful numbers, the new curriculum has the potential to make a significant impact on access to pain and palliative care in Morocco. A similar 20-hour curriculum was implemented in France in the mid-1990s.[141] According to the INCB, France’s education reforms were a major component of its successful effort to increase access to opioids.[142]
Continuing Medical Education
Whilethe new undergraduate curriculum is a great leap forward, it is essential that Morocco also invest in training doctors who are currently practicing but have not had any training in palliative care. Developing continuing education on palliative care was a key part of the “Morocco action plan” adopted during a workshop on palliative care hosted by the WHO in collaboration with the Moroccan Society of Palliative Care and the African Palliative Care Association in 2010.[143]
Unlike intermediate training, described below, continuing education should provide basic training in pain and palliative care to large portions of the medical community. The Moroccan Society of Pain and Palliative Care conducted pain management trainings in numerous cities in Morocco in 2006-2007. The trainings were held in a number of major cities across Morocco and attracted over 2000 medical practitioners.[144]Although impressive in their reach, these trainings focused on pain management rather than palliative care more broadly and have not been held for years.
In September of 2015, the American Society of Clinical Oncology and the regional oncology center in Fez, in collaboration with the Lalla Salma Foundation, will host a first of its kind palliative care workshop in Fez. The three-day workshop will cover a range of topics, including managing pain and other common symptoms and communicating prognosis to patients.[145] Although held after the writing of this report, the workshop may provide a model that can be expanded to reach larger segments of the medical profession.
Intermediate Training
There is a notable dearth of mandatory, intermediate training in palliative care. Human Rights Watch was able to identify one such program for doctors specializing in anesthesiology at Mohammed V University (Souissi) in Rabat. There, anesthesiology residents are required to take part in a six-month anesthesiology residency at the National Oncology Institute in Rabat, which includes a two-month rotation within the palliative care unit.[146]
Physicians specializing in other fields of medicine that see many palliative care patients, such as oncology, internal medicine, and cardiology, do not receive any mandatory academic or clinical training in palliative care. Indeed, physicians specializing in anesthesiology in places other than Rabat do not either.
Our research was able to identify three optional certificate or diploma programs that provide intermediate training to general practitioners and specialists in pain management and/or palliative care at medical schools in Rabat, Casablanca, and Oujda. In Rabat, the university offers a one-year certificate in pain treatment and palliative care, consisting of 60-hours of theoretical course work as well as some clinical exposure to palliative care within the National Oncology Institute.[147]
In Oujda, the university offers a diploma program, open to 30 candidates, in pain management. While the course has more training hours—120 theoretical hours and 20 “practical training” hours—than the program in Rabat, it does not offer training on palliative care.[148] Similarly, the pain certificate program in Casablanca does not provide course hours on palliative care.[149] Although these certificate or diploma programs are important for those who take advantage of them, more needs to be done to ensure that practitioners who interact frequently with palliative patients are required to receive training in both pain treatment and palliative care.
A major barrier to increasing intermediate training programs in palliative care for physicians who regularly encounter patients with life-limiting illnesses is the dearth of palliative care services in the country that can serve as resources for such programs. As Morocco increases the number of hospitals that offer palliative care, as planned under the national cancer plan, it should be possible to establish additional intermediate training programs.
Specialist Training
A ministerial decree from 1993 sets out an exhaustive list of the medical specialties available in Morocco.[150] In 2008, through a decree issued by the minister of higher education, internal medicine, aviation medicine, medical informatics, and pediatric psychiatry were added as medical specialties.[151]
Palliative care is not currently a medical specialty in Morocco. Beginning in 2015, Mohammed V University plans to offer a university diploma in pain and palliative care, which will include 152 hours of theoretical training on pain treatment and 28 hours on palliative care as well as a 40-hour clinical internship at the palliative care unit at the National Oncology Institute in Rabat.[152] This new diploma course will be the educational opportunity closest to a medical specialty in palliative care available in Morocco, although it will not result in the title of specialist in palliative care and still falls well short of the EAPC’s recommendation of 160 hours of clinical training for palliative care specialists.
Nursing Education
The World Health Assembly resolution recommends that all nursing personnel receive training in palliative care.[153] Indeed, nurses are often closest to the patients and their families and most aware of the physical and emotional symptoms patients are experiencing.[154] As such, they play a critical role in identifying patients who need to be referred for more complex interventions and providing basic care, assessing pain, and offering social support and comfort. In Uganda, specially trained nurses are authorized to prescribe opioid analgesics to patients, which has greatly expanded access to palliative care in rural communities where no physicians are available.[155]
There is little literature about palliative care education for nurses in Morocco. A small 2008 survey conducted at the regional oncology center in Rabat, however, suggests that palliative care training for nurses in that city was not adequate at the time. Among the 21 nurses surveyed, 20 said there were no undergraduate courses available in caring for palliative patients and 16 felt they were inadequately trained in end-of-life care. Out of all nurses surveyed, only five nurses said they had participated in any form of continuing training to care for dying patients.[156]
Medicine Availability
The WHO recommends that countries adopt a “medicines policy in order to ensure the availability of essential medicines for the management of symptoms, including pain and psychological distress, and in particular, opioid analgesics for relief of pain and respiratory distress.”[157] In 2013, the WHO created sections on pain and palliative care in its Model List of Essential Medicines and its Model List of Essential Medicines for Children. These sections contain medicines and specific formulations that the WHO considers essential for pain management and palliative care.
In order to fulfill the right to health, countries should ensure the availability and accessibility of all medicines included in the WHO Model List of Essential Medicines. The Committee on Economic, Social and Cultural Rights has held that providing essential medicines as determined by the WHO is a core obligation that cannot be limited by claims of limited resources.[158]
Availability and Accessibility of Opioid Analgesics
Opioid analgesics are essential for the management of pain, shortness of breath, and several other common symptoms among people who need palliative care. Because opioid medicines are controlled substances, countries have obligations to regulate how they can be produced, distributed, prescribed, and dispensed.
In many countries, including Morocco, access to these medications is very limited. As previously mentioned, the International Narcotics Control Board noted in its 2014 annual report that 5.5 billion people live in countries with no or limited access to these medicines.[159]
The 1961 Single Convention on Narcotic Drugs, the international agreement that provides the framework for national drug control efforts, contains four basic requirements for national regulations of controlled medicines:
- Individuals dispensing the medication must be licensed, either by virtue of their professional license or through a special licensing procedure;
- The medications may only be transferred between authorized institutions or persons;
- The medications can only be dispensed to a patient upon a medical prescription; and
- Records on the movement of these medications are kept for no less than two years.[160]
The Single Convention specifically allows countries to put in place additional requirements, including a special prescription form for controlled medications. However, countries have a dual obligation with respects to these medicines: they must ensure their adequate availability for medical and scientific use while preventing their misuse and diversion.[161] Countries must take care that any requirements beyond those specified in the 1961 Single Convention do not unnecessarily impede medical access.[162]
International human rights standards also require that countries ensure that opioid analgesics that are included in the WHO Model List of Essential Medicines are available and accessible. As manufacturing, prescribing, and dispensing controlled medicines is subject to strict regulation by governments, states have an obligation to ensure these regulations do not unnecessarily restrict patient access to them for medical purposes. Regulations that arbitrarily impede procuring and dispensing these medications for medical purposes can violate the right to health.
***
The Moroccan government has clearly identified increasing access to opioid analgesics as a priority. The SHS contains a specific action point for “training and provision of information to healthcare personnel and the fight against morphineophobia.”[163] This point closely mirror measures called for in the NCPCP.[164]
However, the availability and accessibility of opioid analgesics remains very limited. Our research found that most regional oncology centers and some pharmacies in their immediate vicinity have morphine available and that at least some physicians could prescribe them.[165] However, visits to four regions found that few secondary care facilities had oral morphine; that doctors there did not have special prescription forms to prescribe opioids; and that pharmacies did not stock them.
Analysis of Regulatory Framework
We analyzed in detail Morocco’s regulations on opioid analgesics and their application in practice to determine to what extent they contribute to the limited availability of these medications.
In 2013, Morocco changed its controlled substance law to increase the number of days a prescription for an opioid analgesic can cover from 7 to 28 days, removing a key barrier to the availability of these medicines.[166] The seven-day limitation meant that patients who required opioid analgesics or their relatives had to travel to their physician every single week to obtain and fill a new prescription. Human Rights Watch’s 2011 report on the global state of palliative care identified this regulatory requirement as an important barrier to opioid access.[167]
Our research shows that Morocco’s current regulations go beyond the requirements of the 1961 Single Convention on Narcotic Drugs. Although additional administrative requirements by definition create extra hurdles for the use of these medicines, we did not find that they imposed an excessive burden for physicians or pharmacists, especially those working within the public healthcare system.
A Moroccan law from 1922, from when the country was a French protectorate, still governs the handling, prescribing, and dispensing of opioid analgesics. Under the law, only doctors are allowed to prescribe opioids, although all physicians can obtain prescribing rights.[168]
Special Prescription Forms: Moroccan law requires that all outpatient prescriptions for opioids be written on special prescription pads.[169] While the Single Convention specifically allows countries to require their use, the WHO has noted that requirements for special prescription forms increases the administrative burden both for healthcare workers and drug control authorities.[170] It has stated that this problem is “compounded if forms are not readily available, or if health professionals need to pay for them.” It recommends that countries “ensure that this system does not impede the availability and accessibility of controlled medicines.”[171]
Physicians must obtain the special prescription pad, called a “carnet à souche,” from the Ministry of Health’s Department of Medicines and Pharmacy. Importantly, physicians can apply for the special prescription pad by mail rather than having to go in person. The Department of Medicines and Pharmacy can also issue two prescription pads at a time, each containing 50 scrips. The pad must be returned to the Ministry of Health before a new one can be obtained, but the fact that physicians are allowed to have two prescription pads at a time helps minimize the risk of a physician being left without prescription forms for opioid analgesics during the application process.[172]
Physicians at several tertiary level public hospitals told Human Rights Watch that the process for obtaining the special prescription pads was relatively easy and was most often carried out by the hospital administrators on their behalf. Significantly, many of the public regional oncology centers order numerous prescription pads at a time, making them readily available.[173]
The process for obtaining special prescription pads is a larger obstacle for physicians outside the public healthcare system. Unlike public physicians, private physicians must make their initial request for a carnet à souche through an intermediary: the president of The National Order of Doctors, a professional association. The president, in turn, must make a written request to the Ministry of Health.[174] According the Dr. Mati Nejmi, who has been working in private practice since 2013, this process can take over a month.[175] Although private physicians can obtain subsequent prescription pads by writing directly to the Ministry of Health, the initial process may act as a deterrent.
In 2014, the Ministry of Health dispensed 409 special prescription pads, 310 to public physicians and 99 to private physicians.[176] Human Rights Watch does not know how many individual physicians have a carnet à souche but given that many use more than one per year it is likely to be substantially lower than 409.
Morocco has recently made significant progress in increasing the reach of opioid prescription privileges—the number of pads distributed increased by 32 percent between 2013 and 2014. However, only a small fraction of the approximately 20,500 physicians in Morocco have them,[177] making it problematic for patients to find a doctor who even has the ability to prescribe opioids.
Regulations on Opioid Analgesics for Pharmacies: Under Moroccan law, any pharmacy can stock opioid analgesics.[178] However, they must comply with a number of regulatory requirements.[179] Pharmacists described requirements to keep detailed records of any purchases and sales in several special log books, one containing detailed descriptions of all sales, another recording current stock, and a third for purchases of controlled medicines.[180]
Each book must be separately purchased, in-person (by the pharmacist or a representative), from a different organization—The National Council of Pharmacists, the Regional Council of Pharmacists, and the Union of Pharmacists—although these are all located in the same building in Rabat. Pharmacists must also pay for the books, which range from 200 to 500 MAD (US$21 to $53).[181] The three books must all be kept for up to 10 years for possible government audits.[182]
|
Increasing Access to Opioid Analgesics: Colombia and Vietnam A dearth of pharmacies stocking oral morphine is a major challenge in many countries. While one pharmacist in Morocco told us he carries morphine because he feels it is his “professional obligation” to ensure the public has access to the medication, the administrative requirements, low demand, concerns about potential misuse or diversion, and the potential for scrutiny from law enforcement deter many others from stocking it. Several countries have actively tried to address this issue. In Colombia, for example, intensive engagement between the government, NGOs, and academics led to a revised regulation for regional medicines procurement in 2008. Under that regulation, all 32 Colombian states must have at least one place where opioids are guaranteed to be in stock at all times.[183] This commitment to opioid availability was solidified in article eight of Colombia’s recently passed palliative care law.[184] Following these and other efforts to increase access to palliative care in Colombia, opioid consumption has increased dramatically. Between 2006 and 2012, the government reported a 270 percent rise in opioid consumption[185] Vietnam has successfully undertaken similar efforts to increase access to palliative care and pain treatment. In 2005, its Ministry of Health launched a palliative care initiative and created a working group on palliative care, which included the ministry, physicians, and international experts.[186] Based on the working group’s findings, the Ministry of Health implemented educational and regulatory reforms beginning in 2006. Significantly, in 2008, the Ministry of Health eased a number of key regulatory barriers to accessing opioids: the maximum daily opioid dose was abolished; the opioid prescription period was increased from 7 to 30 days; assistant doctors in remote areas were given authority to obtain a license to prescribe morphine; and district hospitals and commune health posts were authorized to prescribe and dispense morphine.[187] Similar to Colombia, the new regulations also specify that opioids should be available in each district and charge hospital pharmacies with providing oral morphine to outpatient’s when it is not otherwise available.[188] Following these and other efforts to increase access to palliative care in Vietnam, opioid consumption increased by over 400 percent between 2005 and 2012.[189] |
Despite the complexity of the process, most pharmacists Human Rights Watch interviewed said they did not feel these requirements were unnecessarily burdensome. Interviews with 16 private pharmacies in 6 cities, 14 of whom did not stock morphine, suggested that the regulatory requirements were not the primary reason why pharmacies did not to carry the medication. In fact, a number of pharmacists said they had all the necessary books to buy and dispense morphine but did not carry it because of concerns about drug dependence, potential misuse, and a lack of demand for the medication. The pharmacists who did carry and regularly dispense opioids felt that clientele misuse could be handled through proper administration, but did echo some of the economic concerns raised by other pharmacist, including low-profit margins and demand.[190]
Dr. Laghdaf Rhaouti, for example, the owner of a pharmacy outside the National Oncology Institute that stocks oral morphine, explained to Human Rights Watch why he carries morphine despite its low profit margins:
I carry morphine because it is my professional obligation…. It is a humanitarian act…. As a pharmacist isn’t this my job? As a human being, isn’t this my conscience?… I don’t just think of the profit, I think of the public need for these medications.[191]
However, the vast majority of pharmacies choose not to carry these medications, and the dearth of them in small cities is a major barrier to the use of these medications. To fulfill the right to health, the government has a duty to ensure this essential medication is available to patients, even if market forces make it unattractive for private pharmacies to carry.
Opiophobia and Misunderstandings
Numerous interlocutors identified fear of opioid analgesics and a lack of training in their use as the main reasons for the limited availability of these medicines in much of the country. The government itself also identified this as a significant barrier in the Sectoral Health Strategy and the National Cancer Prevention and Control Plan.[192]
Many doctors and hospital administrators we interviewed at secondary care facilities said they did not have special prescription forms because they believed opioids were addictive and could only be prescribed by specialists or at tertiary care facilities.[193] In most of these facilities, morphine was used exclusively by anesthesiologists for surgical procedures.
Fear of and misconceptions about morphine and other opioid analgesics may not be surprising given that the law regulating them is called the Law on the Regulation of Import, Commerce, Holding and Use of Poisonous Substances (emphasis added).[194] Under the law, opioid analgesics are included in a schedule called “Table B Poisonous Substances.” While Morocco shares this labeling practice with some other Francophone countries,[195] many Francophone countries use the term narcotics (stupéfiants),[196] the designation in the Single Convention.[197]
|
Impact of Colonial-Era Controlled Substance Regulations in Francophone Countries In the early 20th century, France adopted stringent regulations on the provision of opioid medications, requiring the use of special prescription pads and limiting each prescription to a seven-day period.[198] It imposed the same regulations on many of its colonies. Since the late 1980s, France has gradually simplified its regulatory requirements to ensure opioid analgesics were available for pain management and palliative care. In 1999, it eliminated the special prescription pad altogether, allowing prescriptions to be made on widely available secure ordinances, and increased the time limit for prescriptions for opioid analgesics to 28 days.[199] While France has substantially simplified its regulatory requirements, numerous Francophone countries continue to live by the strict regulations they inherited in colonial times.[200] Until 2013, Morocco also maintained a seven-day limit on prescriptions for opioid analgesics, meaning patients or their relatives needed to visit their physician every week to get a new prescription, a heavy burden for people with a life-limiting illnesses and their families.[201] However, in an important move, Morocco removed this legal barrier, increasing the opioid prescription period from 7 to 28 days.[202] Human Rights Watch encourages other Francophone countries that retain this limit to follow Morocco’s lead, and review and amend regulations to improve access to these essential medicines. |
Designating essential medicines as poisons clearly stigmatizes them and contravenes WHO guidelines on controlled substance policies that urge states to remove terminology in national medicine control policies that has“the potential to confuse the medical use of opioids for pain with drug abuse or drug dependence.”[203]
Availability of Other Opioid Analgesics
Many doctors and pharmacists noted that alternatives to morphine, such as oxycodone and methadone, were not available for pain treatment in Morocco. Methadone is available to treat opioid dependence but not for pain management. As a result, physicians have no alternatives to morphine which complicates the management of patients who do not tolerate the medication or whose pain does not respond to it. One medical oncologist commented:
Not having a range of pain medications is also a problem if a patient has intolerance or side effects with morphine, such as nausea or dizziness. We have morphine, so we can treat severe pain, but we have a problem if we need to rotate to another pain medicine.[204]
Oxycodone is included in the WHO’s Model List of Essential Medicines’ section on pain and palliative care as an alternative to morphine. Methadone is only included in the section on substance-use disorders but is frequently used in pain management in many countries.[205]
Moreover, doctors noted that oral liquid morphine (forme buvable in French) is not available in Morocco. This complicates administration to patients who have trouble swallowing or uncontrollable nausea, neither of which is uncommon in palliative care patients. Dr. Hessissen, the pediatric oncologist, noted that this is a problem in treating children with pain: “Small children can’t swallow pills. [We] give them codeine instead.”[206] The WHO removed codeine from its clinical guideline on treatment of persistent pain in children in 2012 because of safety and efficacy concerns.[207]
|
Availability of Neuropathic Pain Medications Neuropathic pain (NP) is pain caused by a lesion or disease affecting the nervous system.[208] Like non-neuropathic pain, NP is common among individuals with chronic illnesses, including people with HIV, diabetes, and multiple sclerosis.[209] NP is “associated with significant decreases in quality of life and socioeconomic well-being, sometimes even more so than non-neuropathic chronic pain.”[210] Because NP differs from non-neuropathic pain, different medications are required to treat it. Significantly, strong opioids are not recommended as a first-line treatment for NP. In 2015, a systematic review by the International Association for the Study of Pain (IASP) Special Interest Group on Neuropathic Pain (NeuPSIG) recommended 15 key medications to treat NP, grouped in 6 categories.[211] To effectively treat NP in all patients, doctors need access to at least one medication in each of these categories. This provides physicians alternatives, should a patient fail to respond to an available medication, as is common when treating NP.[212] A comparison of the Moroccan essential medicine list and AMO and RAMED’s reimbursable medicines list to the medications identified in the NeuPSIG study, however, reveals a number of important differences. Significantly, the Moroccan list is missing two full categories of medications: serotonin noradrenaline reuptake inhibitors (SNRIs) and alpha-2-delta antagonists. Both categories are recommended as first-line treatment for NP. While the reimbursable medicines list includes SNRIs, it is also missing alpha-2-delta antagonists (see Appendix I for details). |
IV. Morocco’s Obligation to Improve Palliative Care
National Law
Following reforms in 2011, Morocco’s Constitution for the first time guarantees a number of economic and social rights to all its citizens, including the right to health.[213] Article 31 states, among others:
The State, the public establishments and the territorial collectivities work for the mobilization of all the means available to facilitate the equal access of the citizens to conditions that permit their enjoyment of the right: to healthcare; … to social protection, [and] to medical coverage….[214]
Article 34 of the constitution adds that particular care must be taken to “provide for the vulnerability of certain categories” of people, including the elderly.[215]
The Sectoral Health Strategy, which includes action points on palliative care and pain treatment, highlights the fact that Morocco’s 2011 constitution “makes access to healthcare and medical coverage fundamental rights of all citizens.”[216] In this context, the SHS specifically adopts a “rights based approach that aims to integrate the right to health provisions contained in the new constitution.”[217]
Right to Health
The International Covenant on Economic Social and Cultural Rights (ICESCR), which Morocco ratified in 1979, specifies in article 12 that everyone has a right “to the enjoyment of the highest attainable standard of physical and mental health.”[218] The Committee on Economic, Social and Cultural Rights, the body charged with monitoring compliance with the ICESCR, has held that states must make available in sufficient quantity “functioning public health and health-care facilities, goods and services, as well as programmes,” and that these services must be accessible.[219]
Because states have different levels of resources, international law does not mandate the kind of healthcare to be provided. The right to health is considered a right of “progressive realization.” By becoming party to the international agreements, a state agrees “to take steps … to the maximum of its available resources” to achieve the full realization of the right to health.[220] In other words, high-income countries will generally have to provide healthcare services at a higher level than those with limited resources. But all countries are expected to takeconcrete stepstoward increased services, and regression in the provision of health services will, in most cases, constitute a violation of the right to health.
Notably, the United Nations Committee on Economic, Social and Cultural Rights has also held that there are certain core obligations that are so fundamental that all states must comply with them. While resource constraints may justify only partial fulfillment of some aspects of the right to health, the committee has observed vis-à-vis the core obligations that “a State party cannot, under any circumstances whatsoever, justify its non-compliance with the core obligations…, which are non-derogable.” The committee has identified, among others, the following core obligations:
- To ensure the right of access to health facilities, goods and services on a non-discriminatory basis, especially for vulnerable or marginalized groups;
- To provide essential drugs, as from time to time defined under the WHO Action Programme on Essential Drugs;
- To ensure equitable distribution of allhealth facilities, goods and services; and
- To adopt and implement a national public health strategy and plan of action, on the basis of epidemiological evidence, addressing the health concerns of the whole population.[221]
The committee lists the obligation to provide appropriate training for health personnel as an “obligation of comparable priority.”[222]
Palliative Care and the Right to Health
Given that palliative care is an essential part of healthcare, the right to health requires that countries take steps to the maximum of their available resources to ensure that it is available. Indeed, the Committee on Economic, Social and Cultural Rights has called for “attention and care for chronically and terminally ill persons, sparing them avoidable pain and enabling them to die with dignity.”[223] Two different state obligations flow from this:
- A negative obligation to refrain from enacting policies or undertaking actions that arbitrarily interfere with the provision or development of palliative care; and
- A positive obligation to take reasonable steps to ensure the integration of palliative care into existing health services, both public and private, through the use of regulatory and other powers as well as funding streams.
No Interference with Palliative Care
The Committee on Economic, Social and Cultural Rights has stipulated that the right to health requires states to “refrain from interfering directly or indirectly with the enjoyment of the right to health.”[224] States may not deny or limit equal access for all persons, enforce discriminatory health policies, arbitrarily impede existing health services, or limit access to information about health.[225] Applied to palliative care, this obligation means that states may not put in place medicine control regulations that unnecessarily impede the availability and accessibility of essential palliative care medications, such as morphine and other opioid analgesics.
Ensuring Integration of Palliative Care into Health Services
The right to health requires states to take the steps necessary for the “creation of conditions which would assure to all medical service and medical attention in the event of sickness.”[226] The Committee on Economic, Social and Cultural Rights has held that people are entitled to a “system of health protection which provides equality of opportunity for people to enjoy the highest attainable level of health,”[227] including patients with chronic or terminal illnesses.
The committee has called for an integrated approach to the provision of different types of health services that includes elements of “preventive, curative and rehabilitative health treatment.”[228] It has also held that investments should not disproportionately favor expensive curative health services, which are often accessible only to a small, privileged fraction of the population, rather than primary and preventive healthcare benefiting a far larger part of the population.[229] The same principle applies to palliative care services. Given the large percentage of cancer and other patients who require palliative care services, particularly in low and middle income countries, considerable urgency needs to be given to developing palliative care services for these patients.
Pain Treatment Medication and the Right to Health
As injectable and oral morphine are on the WHO List of Essential Medicines for adults and for children, countries have to provide these medications as part of their core obligations under the right to health.[230]States should make sure these medicines are both available in adequate quantities and physically and financially accessible for those who need them.
In order to ensure availability and accessibility, states have, among others, the following obligations:
- Since regulating the market for controlled medicines like morphine is completely in government hands, states must put in place regulations to ensure an effective procurement and distribution system and create a legal and regulatory framework that enableshealthcare providersin both the public and private sector to obtain, prescribe, and dispense these medications. Any regulations that arbitrarily impede the procurement and dispensing of these medications may lead to a violation of the right to health;
- States need to adopt and implement a strategy and plan of action for the roll out of pain treatment and palliative care services. Such strategy and plan of action should identify obstacles to improved services as well as steps to eliminate them;
- States should regularly measure progress made in ensuring availability and accessibility ofpain relief medications; and
- The requirement of physical accessibility means that these medications must be “within safe physical reach for all sections of the population, especially vulnerable or marginalized groups.”[231]States need to ensure that a sufficient number of healthcare providers or pharmacies stock and dispense morphine and that an adequate number of healthcare workers are trained and authorized to prescribe these medications.
Although the right to health does not require states to offer medications free of charge, financial accessibility means that medications should be “affordable for all.”In the words of the committee:
Payment for health-care services … has to be based on the principle of equity, ensuing that these services, whether privately or publicly provided, are affordable to all, including socially disadvantaged groups. Equity demands that poorer households should not be disproportionately burdened with health expenses as compared to richer households.[232]
Pain Treatment and the Right to Be Free from Cruel, Inhuman, or
Degrading Treatment
The right to be free from torture, cruel, inhuman, or degrading treatment or punishment is a fundamental human right that is recognized in numerous international human rights instruments.[233] Apart from prohibiting the use of cruel, inhumane, or degrading treatment, the right also creates a positive obligation for states to protect persons in their jurisdiction from such treatment.[234]
This obligation has been interpreted to include protecting people from unnecessary pain related to a health condition. As Manfred Nowak, then UN Special Rapporteur on torture, cruel, inhuman or degrading treatment or punishment wrote in a joint letter with the UN Special Rapporteur on the right to health to the Commission on Narcotic Drugs in December 2008:
Governments also have an obligation to take measures to protect people under their jurisdiction from inhuman and degrading treatment. Failure of governments to take reasonable measures to ensure accessibility of pain treatment, which leaves millions of people to suffer needlessly from severe and often prolonged pain, raises questions whether they have adequately discharged this obligation.[235]
In a report to the Human Rights Council, Nowak later specified that, in his expert opinion, “the de facto denial of access to pain relief, if it causes severe pain and suffering, constitutes cruel, inhuman or degrading treatment or punishment.”[236]
Not every case where a person suffers from severe pain but has no access to appropriate treatment will constitute cruel, inhuman, or degrading treatment or punishment. In a 2013 report to the Human Rights Council, UN Special Rapporteur on torture Juan Mendez stated that this will only be the case when the following conditions are met:
- The suffering is severe and meets the minimum threshold required under the prohibition against torture, cruel, inhuman, or degrading treatment or punishment;
- The state is, or should be, aware of the level and extent of the suffering;
- Treatment is available to remove or lessen the suffering but no appropriate treatment was offered; and
- The state has no reasonable justification for the lack of availability and accessibility of pain treatment.[237]
V. Full Recommendations
The introduction of palliative care in Morocco, at major hospitals as well as within in the community, is urgently needed to prevent the unnecessary suffering of thousands of people throughout the country. As a signatory to various international human rights treaties and the UN drug conventions, the government has an obligation to ensure that its citizens have access to affordable palliative care and essential palliative care medications.
The Moroccan government has made significant strides in removing barriers to the development of palliative care. It is thus well positioned to begin implementing the vision articulated in its National Cancer Prevention and Control Plan (NCPCP) and Sectoral Health Strategy (SHS) for the provision of palliative care at all levels of the healthcare system, which would provide enormous benefits to tens of thousands of Moroccans annually. Human Rights Watch believes the following steps are essential for this purpose:
- Establish general palliative care centers at each of the five university hospitals. These units should have multidisciplinary teams, including doctors, nurses, and psychologists, all trained in palliative care. This step is of pivotal importance as it would allow Morocco to advance in three important areas:
- The need to offer palliative care to non-cancer patients;
- The staff of these services could help teach the palliative care component of Morocco’s new medical school curriculum and allow for clinical rotations in palliative care; and
- These academic institutions could help develop and implement a much-needed palliative care research agenda to determine standards and models of care appropriate for Morocco.
- Establish palliative care centers at all regional oncology centers and the pediatric oncology hospital in Rabat. The government should ensure that all currently operational regional cancer centers, as well as ones that are newly opened, have palliative care services. These centers can then serve as the basis for the further decentralization of palliative care. A palliative care unit at the pediatric oncology unit in Rabat could form the basis for developing pediatric palliative care and decentralizing it overtime.
- Integrate pain treatment and ensure the availability of oral opioid analgesics at secondary care facilities. The government should ensurethat all local, provincial, and regional hospitals have staff adequately trained in the assessment and management of pain and that oral morphine is available. It should ensure that there are pharmacies near these hospitals that stock oral morphine or, alternatively, the hospital pharmacies should dispense it to outpatients.
To implement these steps, we make the following specific recommendations:
In the Area of Integrating Palliative Care into the Structure of the Healthcare System
- Implement the palliative care and pain treatment measures identified in the SHS and NCPCP. The Ministry of Health should set benchmarks and timelines for implementing the palliative care measures called for in the SHS and NCPCP and clearly identify the agencies or actors responsible for their implementation. It should set a clear budget for implementing the palliative care component of the SHS. It should do so through an inclusive process with relevant stakeholders. The Ministry of Health should also regularly review progress.
- Develop and implement a model for palliative care delivery at primary and secondary care facilities. This should include a model for mobile teams and home-based palliative care.
- Develop palliative care networks. The government should develop models and protocols to allow for efficient communication between various palliative care providers at different levels of the healthcare system. The purpose should be to allow patients to receive palliative care at the closest facility that can provide an appropriate level of care.
- Include palliative care in the next WHO country cooperation strategy. This step would ensure Morocco benefits from the WHO’s current work on implementing the World Health Assembly resolution on palliative care.
- Implement the WHO Global Action Plan on NCDs and the WHA resolution on palliative care.
In the Area of Integrating Palliative Care into Healthcare Financing
- Review RAMED’s coverage of essential medications. RAMED’s coverage should be reformed with a view of ensuring that medication costs do not constitute an undue barrier to obtaining essential palliative care medications.
- Reimburse low-income patients for travel expenses. Whilethe government works to decentralize the provision of palliative care, it should establish a mechanism to support patients who have to travel to access palliative care to ensure that travel costs do not place an excessive burden on them. Measure 68 of the NCPCP recognizes the burden of travel expenses borne by patients and calls for “financial coverage for safe transport from the hospital to the home, and from the home to the hospital.”[238]
- Progressively expand health insurance to Morocco’s uninsured. In accordance with Morocco's constitution and recommendations of the WHO and World Bank, Morocco should progressively expand health insurance to ensure coverage of those presently lacking coverage.
In the Area of Education
- Progressively expand the undergraduate, palliative care curriculum to include clinical aspects. The Ministry of Higher Education and Ministry of Health should develop, jointly with relevant stakeholders, a detailed outline of the palliative care component of the new medical school curriculum. They should also develop and implement a plan for clinical exposure to palliative care for medical students in their 6th and 7th year.
- Sponsor continuing education trainings in palliative care. Although the new undergraduate, palliative care curriculum will prepare future doctors to provide palliative care, it is essential that Morocco invest in training the thousands of active doctors who did not benefit from the reformed medical curriculum. The Ministry of Health should sponsor continuing education seminars designed to reach a broad audience of practicing medical personnel.
- Develop mandatory, intermediate, clinical training in palliative care. The Ministry of Higher Education in partnership with relevant public universities should develop a plan to mandate rotations in palliative care units for doctors of certain postgraduate programs, including oncology, internal medicine, anesthesiology, and geriatrics (when added as a medical specialty, as identified in the SHS) to ensure clinical exposure to palliative care.
- Recognize palliative care as a medical specialty.Palliative care specialists are essential to providing a full-range of palliative care interventions at tertiary care facilities, coordinating palliative care services within regions, and training other doctors to provide basic palliative care interventions. The Moroccan government should recognize palliative care as a medical specialty, and the Ministry of Higher Education in partnership with relevant public universities should begin developing a curriculum for the specialty.
- Develop a plan for integrating palliative care into the healthcare worker education system.The Ministry of Higher Education should convene an inclusive meeting of relevant stakeholders to jointly develop a plan of action for the gradual introduction of palliative care instruction into the curricula for nursing, psychology, and social work programs.
In the Area of Medicine Availability
- Develop and implement a program to counter misunderstandings and fear around opioid analgesics and to increase the number of physicians with prescription privileges. The government should actively combat “morphineophobia” by developing trainings in the use of opioid analgesics and outreach programs to ensure that doctors at secondary care facilities have special prescription pads for opioids.
- Streamline the process for private physicians to obtain prescription privileges. The process for obtaining opioid prescription privileges is more difficult for physicians working in private hospitals than for those in public hospitals. The Ministry of Health should modify these procedures to ensure that private physicians are not deterred from obtaining special prescription pads.
- Amend the controlled substances law and any relevant regulations to ensure that opioid analgesics and other medicines are not categorized as poisons.
- Ensure the availability of opioid analgesics outside major cities. The governmentshould ensure that each region in Morocco has pharmacies that stock opioid analgesics. In regions where that is not the case, hospital pharmacies should provide these medications to outpatients.
- Include in Morocco’s essential medicines list and in the RAMED/AMO list all palliative medications from each medicine category recommended for neuropathic pain by NeuPSIG.
- Expand the variety of opioid analgesics available and approved for use in palliative care. The governmentshould ensure that alternatives to oral tablet morphine, such as liquid morphine, methadone, and oxycodone, are available for patients.
- Begin utilizing the electronic import/export system for controlled medicines launched by the INCB in March 2015.[239]The Ministry of Health informed Human Rights Watch that utilizing this system will require changes to regulatory and administrative procedure, but that it plans to carry out the necessary reforms.[240]
Acknowledgments
Research for this report was conducted by Matthew Simon, New York University School of Law fellow in the Health and Human Rights Division of Human Rights Watch; Joseph Amon, director of the Health and Human Rights Division of Human Rights Watch; Diederik Lohman, associate director of the Health and Human Rights Division of Human Rights Watch; and Laura Thomas, consultant for the Health and Human Rights Division of Human Rights Watch. Matthew Simon wrote the report. Brahim Elansari, research assistant in the Middle East North Africa Division of Human Rights Watch, provided invaluable research and translation assistance. The report was reviewed by Diederik Lohman; Joseph Amon; Aisling Reidy, legal advisor at Human Right Watch; Eric Goldstein, deputy director of the Middle East North Africa Division of Human Rights Watch, and Danielle Haas, senior editor in the Program Office.
Jennifer Pierre, senior associate in the Health and Human Rights Division; Meg Mszyco, associate in the Health and Human Rights Division; and Thierno Adenhof, Jeff Eamon, and Stephanie Martinez, interns in the Health and Human Rights Division of Human Rights Watch, provided invaluable assistance. Translation into French was provided by Hervé Couturier and Peter Huvos. Production assistance was provided by Kathy Mills, Jessie Graham, Pierre Bairin, and Fitzroy Hepkins.
We are deeply grateful to the many palliative care patients in Morocco who, despite being gravely ill, agreed to be interviewed for this report. Without them and their relatives, this manuscript would not have been possible. We are committed to using this report to try to make sure that others who develop life-threatening illness—and pain and other symptoms associated with it—will not have to endure the suffering many of these patients faced.
We are also greatly indebted to the many palliative care advocates and medical professionals in Morocco and elsewhere who helped us conduct our research, understand our findings, and write this report. Their commitment to serving people at the most vulnerable time of their lives is both humbling and inspiring. We are particularly grateful for the assistance of Dr. Mati Nejmi—the former chief of anesthesiology at National Oncology Institute and a pioneer in the effort to bring palliative care to Morocco—whose advocacy and clinical work has improved the lives of thousands of Moroccans.
Appendix: Comparison of Neuropathic Pain Medicines with the WHO and Moroccan Essential Medicines Lists
|
Medication Category |
Medication
|
WHO Essential Medicines List |
Morocco’s Essential Medicines List |
AMO/RAMED List |
|
First-line Medications |
||||
|
TCA* |
Amitriptyline |
|||
|
Clomipramine |
||||
|
Desipramine |
||||
|
Imipramine |
||||
|
Nortriptyline |
||||
|
SNRI* |
Duloxetine |
|||
|
Venlafaxine |
||||
|
α2δ antagonist* |
Gabapentin |
|||
|
Pregabalin |
||||
|
Second-line Medications |
||||
|
Opioid |
Tramadol |
|||
|
Topical |
8% Capsaicin |
|||
|
5% Lidocaine** |
|
|
||
|
Strong Opioid Medications |
||||
|
Methadone |
||||
|
Morphine |
||||
|
Oxycodone |
Listed as morphine alternative |
|||
* TCA: tricyclic antidepressants; SNRI: serotonin noradrenaline reuptake inhibitors; and α2δ: Alpha-2-Delta.
**Lidocaine was not recorded as being listed on the WHO/RAMED list because it’s topical formulation was a concentration of less than 5 percent.
Indicates medicine formulation that is not included on list.
Indicates medicine formulation that is included on Morocco’s list but is not available in Morocco for neuropathic pain treatment.