Barred from Treatment
Punishment of Drug Users in New York State Prisons
Executive Summary
"I've been in 14 months straight, and just got another 20 months for possession... It's really taking a toll on me. . . . I need some kind of therapy because the cell is closing in on me. I feel paranoid, I can't sleep. I feel like people are against me. I'm restless, I'm talking to myself."
- Nathan T, 32, prisoner at the Upstate Correctional Facility in Malone, New York [1].
When Human Rights Watch met with Nathan in July 2008, his hands and feet were shackled with heavy chains. He had been in disciplinary confinement ("the box")-punishment reserved for serious prison offenses-for 14 months. When Nathan entered prison in 2000, he was identified as in need of substance abuse treatment and placed on a waiting list. Because he relapsed into drug use in violation of prison rules, he lost his place on the waiting list, and was sent to the box. Nathan is addicted to opiates and other drugs, and continues to relapse, as is common for people with drug addiction. There is no treatment in the box. Indeed, Nathan has never received any treatment in prison. He now faces another 20 month sentence in the box for using drugs, without access to treatment.
New York State prison officials have identified three out of four prisoners as in need of substance abuse treatment. With the number of prisoners living with HIV and hepatitis C among the highest in the nation, New York State prisons have an obligation under international, US and state law to protect prisoners' right to health. Under these standards, prisons must provide drug dependence treatment and harm reduction programs equivalent to those available in the community. International and national standards for prison health care reflect the fundamental principle that "good prison health is good community health," as 26,000 people rejoin New York communities from prison each year. This Human Rights Watch report documents New York's failure to ensure access to substance abuse treatment while pursuing a program of harsh punishment for drug use that bars prisoners from treatment as part of the disciplinary sanction.
Drug dependence is a chronic, relapsing disease. Drug users, both in and out of prison, have a right to access health care that should include drug dependence treatment and harm reduction measures to reduce health risks such as transmission of HIV and hepatitis B and C. Prison treatment programs should be available, accessible, appropriate and of good quality. But in the New York State prisons, drug treatment programs are filled to capacity. Prisoners face long waiting lists for substance abuse treatment. Despite overwhelming evidence that Medication-Assisted Therapy is the most effective treatment for opioid dependence, the majority of New York State prisoners dependent on heroin or other opioids have no access to methadone or buprenorphine. Between 1996 and 2005, twenty-seven prisoners died of overdose of illegal drugs in New York State prisons.
At the same time, punishment for drug use in the New York State prisons is severe and out of proportion to the seriousness of the offense. Thousands of New York State prisoners, many of them struggling with addiction, are sentenced to "the box"- a disciplinary sanction that removes them from the general population, restricts many activities of daily life, and where they have no access to drug dependence treatment. In New York State prisons, drug users are locked in "the box" for months, even years, barred from treatment. New York's severe punishment of drug use in prison, while delaying or denying access to treatment and harm reduction services, violates prisoners' right to health and the right to be free from cruel and inhuman treatment under international law.
Human Rights Watch's investigation of New York State's treatment of drug users in prison included interviews with more than 50 current and recently released prisoners at 8 correctional facilities, including the "supermax" facilities where prisoners are held in disciplinary segregation. The investigation also included visits to prison drug treatment facilities, review of documents obtained from Freedom of Information Law requests, and meetings with drug and alcohol treatment officials, judges, legislators, advocates and other experts on New York State substance abuse, criminal justice and prison health law and policy.
Human Rights Watch found that the New York State Department of Correctional Services (DOCS) failed in the following ways to provide adequate health services for prisoners who use drugs:
- Drug dependence treatment is frequently delayed and, for prisoners in disciplinary confinement, denied altogether. Long waiting lists result in treatment delays of months, sometimes years, for many prisoners.
·DOCS fails to provide Medication-Assisted Therapy to the majority of opioid-dependent prisoners. Despite having identified thousands of prisoners as opioid users in need of treatment, New York State continues to ignore well-established evidence that methadone and buprenorphine are the most effective treatment for opioid dependence and increasing evidence of its successful implementation in prison settings.
·DOCS fails to provide translation services to ensure that drug dependence treatment programs are accessible to non English-speaking prisoners. DOCS further fails to make accommodations in these programs for prisoners with low literacy skills.
·New York State fails to make essential harm reduction services available in prison. New York's failure ignores well-established evidence that condom distribution, sterile syringes, bleach, tattoo education, and Medication-Assisted Therapy and overdose prevention programs for opioid dependence reduce prisoners' exposure to HIV and hepatitis, sexually transmitted diseases, and death from overdose.
New York State's forms of punishment for prisoners who use drugs constitute cruel, inhuman and degrading treatment in violation of international human rights law in several ways:
The penalties provided for and imposed for punishment of drug use and possession are grossly disproportionate to the severity of the offense. Internal guidelines for sanctions are often exceeded, resulting in months, even years, of isolation and confinement. Disciplinary sanctions for drug use also result in the loss of good time accrued toward early release, imposition of special diets, restricted recreation, visits, packages, showers and telephone calls, and denial of access to educational and other rehabilitative programming. Extended isolation and harsh conditions of confinement violate international standards for the humane treatment of prisoners.
New York State prisons pursue a mandatory urine testing program that carries harsh penalties upon detection of drug use. This program removes many prisoners from treatment and results in disciplinary charges for what may be the symptom of a chronic, relapsing disease. Further, this program may endanger prisoners' health by moving them toward use of injection drugs that are less easily detected by urinalysis, increasing their risk of contracting HIV and hepatitis C through shared needles.
In addition to raising serious human rights concerns, punitive approaches to drug use that remove patients from treatment, encourage use of more dangerous drugs and continue to punish prisoners whose behavior may indicate severe addiction are counterproductive from a policy perspective. New York prisons spend millions of dollars annually on an array of alcohol and drug treatment programs. These programs are less effective, and demand for drugs in prison is increased, when treatment for drug dependent prisoners is denied or delayed. Support offered to prisoners at re-entry, a substantial investment on the part of New York State, will be undermined if adequate drug treatment is not available during incarceration. Without treatment both during and after time in prison, a drug dependent person is likely to return to the criminal justice system.
In recent years, many correctional systems in the United States and throughout the world have responded to high rates of HIV and hepatitis in prisons by implementing harm reduction measures that focus on preventing and reducing the harmful consequences of drug use through a range of targeted interventions. Medication-Assisted Therapy for prisoners addicted to opiates and condom distribution programs to reduce transmission of HIV and other sexually transmitted diseases are operating successfully in US jails and prisons without compromising security. Based on a pragmatic and therapeutic response to drug use in prison, these measures are endorsed by US and international experts on drug use and correctional health, including the National Institute on Drug Abuse, the National Commission on Correctional Health Care, and the United Nations Office on Drugs and Crime.
Without delay, New York State prisons must increase access to drug dependence programs and implement evidence-based harm reduction programs, including Medication-Assisted Therapy and overdose prevention for prisoners dependent on heroin and other opioids. Disciplinary procedures for drug use must be proportional to the offense and disciplinary sanctions should never prevent prisoners from accessing necessary drug treatment and harm reduction services.
Recommendations
To the New York State Department of Correctional Services
·Ensure timely access to evidence-based drug treatment and HIV prevention services for incarcerated drug users:
oTake immediate steps to ensure prisoners' access to care equivalent to that provided in the community (including access to evidence-based drug treatment, harm reduction, and overdose prevention services) and that this care is continuous on transfer into and out of places of detention. Expand current programs to provide overdose prevention education and services to prisoners due to be released.
oTake immediate steps to ensure that drug users can enter treatment without delay, including by expanding existing evidence-based treatment, and providing translation services for non-English speaking prisoners and services for low-literacy prisoners.
oTake immediate steps to ensure that opioid-dependent prisoners have access to Medication-Assisted Therapy.
·Reform disciplinary policies related to substance use:
oTake immediate steps to ensure that disciplinary sanctions for substance use do not subject prisoners to cruel, inhuman or other degrading treatment or punishment or compromise their right to health, including by: 1. revising current disciplinary guidelines to ensure that sanctions for substance use are proportionate to the seriousness of offenses committed; 2. providing oversight to ensure that sanctions imposed do not exceed those permitted by guidelines; and 3. screening prisoners who commit drug offenses for drug dependence and assigning those who are in need of drug treatment to treatment programs rather than punishment.
oEliminate disciplinary segregation as a punishment for substance use, and ensure that disciplinary sanctions for substance use are otherwise proportionate to the seriousness of the offense and do not compromise prisoners' right to health.
oEnsure that urinalysis testing, to the extent that it is used at all, is used in a manner that is consistent with prisoners' right to health and recognition of drug dependence as a chronic, relapsing disease.
To the New York State Commission on Correction
·Review DOCS disciplinary policies related to substance use to ensure that sanctions are proportionate to the seriousness of the offense and consistent with prisoners' right to health.
·Review DOCS substance abuse treatment programs to ensure that all prisoners have timely access to evidence-based substance abuse treatment and harm reduction services, including Medication-Assisted Therapy for opioid users.
To the Governor of New York
·Support comprehensive reform of New York's mandatory sentencing laws for drug offenders (commonly called the Rockefeller drug laws) that would reduce prison sentences for low-level drug offenders and restore discretion to courts to determine appropriate punishments for drug-related crimes and increase use of alternatives to incarceration for offenders who pose no appreciable risk to public safety.
To the New York State Legislature
·Reform the Rockefeller drug laws:
oReform the Rockefeller Drug Laws to eliminate mandatory minimum sentencing, restore judicial discretion and promote increased availability and use of alternatives to incarceration sanctions for low-level drug offenders that emphasize public health, harm reduction and human rights.
·Provide oversight and review to ensure evidence-based substance abuse treatment for New York State prisoners:
oTake immediate steps to ensure that the Department of Correctional Services provides timely access to evidence-based drug treatment and HIV prevention services to drug users and reforms disciplinary policies related to substance use.
oRequire an independent review of Department of Correctional Services' substance abuse programming to evaluate its availability, accessibility, appropriateness, quality and conformance to evidence-based practices.
oSupport ongoing efforts to increase the involvement of the Office of Alcohol and Substance Abuse Services (OASAS) in programs operated in the Department of Correctional Services.
oSupport legislation:
§Promoting expansion of evidence-based substance abuse treatment programming in New York State prisons.
§Promoting expansion of health and harm reduction services in New York State prisons, including Medication-Assisted Therapy for opioid dependence.
§Ensuring that disciplinary sanctions for substance use are proportionate and do not undermine prisoners' access to essential health and harm reduction services.
To the United States Congress and Executive Branch
·Enact legislation, regulations and policies promoting harm reduction programs in prisons, including needle exchange, drug dependence treatment, condom distribution, Medication-Assisted Therapy and other efforts to reduce transmission of HIV and hepatitis B and C in prison and upon release.
·Ratify the International Covenant on Economic, Social and Cultural Rights.
To the United Nations Human Rights Treaty Bodies, Special Rapporteurs and Human Rights Council
·In accordance with a human-rights based approach to drug policy, prioritize the protection of human rights for people who use drugs in prison. Call upon state parties to specifically address:
oWhether prisoners who use drugs have access to evidence-based drug treatment and harm reduction services and
oWhether disciplinary sanctions for drug use are disproportionate or excessive, prevent access to health and harm reduction services, or otherwise constitute cruel, degrading or inhuman treatment and interference with the right to health.
Methodology
This investigation began with a review of hundreds of letters received by Human Rights Watch from New York State prisoners describing their experiences with substance use, in-prison treatment programs and disciplinary confinement for substance use. Human Rights Watch then conducted interviews of 50 current and recently released prisoners. Interviews were conducted at Attica, Great Meadow, Gowanda, and Sing Sing, as well as two women's prisons (Albion and Bedford Hills) and two "supermax" facilities (Southport and Upstate Correctional Facility.) Prisoners at these facilities were interviewed in conditions that ensured confidentiality. Pseudonyms are used in this report to ensure privacy and safety for those interviewed.
Documents were obtained under Freedom of Information Law (FOIL) requests to the New York State Department of Correctional Services, the New York State Commission on Corrections, the New York State Department of Health, and the New York State Division of Parole. Portions of the FOIL request to the Department of Correctional Services were denied, and are under appeal at the time of this writing.
Human Rights Watch interviewed New York State legislators and attended a series of public hearings sponsored by the legislature in spring 2008 to address issues of prison substance abuse programming and efforts to reform the Rockefeller Drug Laws. Human Rights Watch met with representatives of the New York State Office of Alcohol and Substance Abuse (OASAS,) public health and harm reduction experts, public defenders, judges, drug court officials and social workers, jail medical personnel and advocates and attorneys for prisoners in New York State.
Human Rights Watch also interviewed administrators of jail Medication-Assisted Therapy programs in New York, Connecticut, Rhode Island, Washington, and New Mexico. In Albuquerque, New Mexico, Human Rights Watch observed the methadone maintenance program in Bernalillo Metropolitan Detention Center. Human Rights Watch met with the Medical Director of the New Mexico State prison system as well as state and local public officials to discuss the challenges and feasibility of delivering Medication-Assisted Therapy in a correctional setting.
Human Rights Watch found access to the staff, administrators and top officials at the New York State Department of Correctional Services to be limited. Human Rights Watch visited the Willard Drug Treatment Campus in Romulus, New York and met with the Superintendent, Deputy Superintendent, substance abuse counselors and prisoners at that facility. However, Human Rights Watch's request to meet with substance abuse counselors from other facilities was declined, though one counselor contacted us voluntarily during the course of the investigation. Our requests for meetings with the Commissioner of the Department of Correctional Services and the Deputy Commissioner of Program Services to discuss this report were declined, on the grounds that the report was not "authorized" under the Department's research directive.
As a human rights organization documenting abuses of international human rights law since 1978, Human Rights Watch research does not fall under the category of scientific study covered by the DOCS research directive. Human Rights Watch research methodology is subject to internal ethical and legal review, based on strict standards to protect informants and ensure the integrity of the research process. Human Rights Watch remains open to communication with the Department of Correctional Services at any time.
Background
Incarceration, Drug Use, and HIV in New York State
With nearly 63,000 prisoners in 69 facilities, New York State operates the nation's fourth-largest prison system. An estimated 11,936 New York State prisoners are incarcerated for drug-related offenses.[2] The majority of individuals sent to prison for committing drug crimes have never been convicted of a violent offense and 40 percent are in prison for possession, rather than sale, of illicit drugs. [3] Many more are in prison for committing property crimes often related to supporting a habit of drug use.[4]
According to New York State's Department of Correctional Services (DOCS), more than 80 percent of prisoners are in need of substance abuse treatment, including a significant number of people who use heroin.[5] A 2007 DOCS study found, for example, that 83 percent of prisoners were "identified substance abusers" in need of treatment services (49,326 men and 2,422 women). Of 36,000 prisoners who identified a "primary" drug used, 10 percent were heroin users.[6]
The HIV prevalence in state and federal prisons is two and a half times higher than in the general population. [7] New York has higher numbers of HIV-positive prisoners than most states, far exceeding the national average for prisoners living with HIV. In 2005, the last year statistics were released, 3.9 percent of New York State prisoners – 4,400 individuals – were living with HIV or AIDS, compared to 1.9 percent among prisoners nationwide. Approximately 20 percent of all prisoners living with HIV in the United States are in New York State prisons.[8]
Hepatitis C rates among New York State prisoners are even higher. 10 percent of male and 20 percent of female prisoners in New York have hepatitis C, many times the national average of 1-2 percent of the population.[9] Many prisoners are co-infected with HIV and hepatitis C. [10]
The prevalence of HIV, hepatitis C, and drug dependence among New York State prisoners is linked to New York's harsh anti-drug laws. Known as the Rockefeller Drug Laws, New York's mandatory minimum sentencing laws are among the most punitive in the United States, consigning thousands of drug users to prison. Prison sentences are required for even minor offenses; judges lack the authority to impose alternatives to incarceration such as community-based sanctions or substance abuse treatment.[11] Amendments in 2004 and 2005 modified the sentence structure and provided some relief for non-violent offenders, but mandatory minimum sentences remain the norm and significant barriers remain to placing drug users in treatment rather than prison.[12]
Incarceration of injection drug users contributes to higher rates of HIV, hepatitis B and hepatitis C among prisoners than in the general population.[13] Sharing of needles among injection drug users is a major source of HIV and hepatitis C transmission. In the United States, 22 percent of people living with HIV contracted the disease through injection drug use.[14] The majority of people living with hepatitis C (54 percent) contracted the disease through injection drug use.[15] In New York State, a 2005 screening of entering prisoners for HIV and hepatitis C showed that 11 percent of entering prisoners found to have HIV and 45 percent of those found to have hepatitis C had a history of injection drug use.[16]
While most prisoners living with HIV contract their infection prior to incarceration, the risk of being infected in prison, particularly through sharing injection equipment or through unprotected sex, is significant. Studies show that many prisoners continue injection while incarcerated, often sharing syringes, thus risking HIV and other diseases. [17] As the World Health Organization reports:
Studies from around the world show that many prisoners have a history of problematic drug use and that drug use, including injecting drug use, occurs in prison. Outbreaks of HIV infection have occurred in a number of prison systems, demonstrating how rapidly HIV can spread in prison unless effective action is taken to prevent transmission.[18]
Medication-Assisted Treatment for Opioid Dependence in Prisons and Pre-Trial Detention
"The only time I've had my life together was when I was on methadone. I lived for a year in Florida with my daughter, and worked as a cocktail waitress. It's the only time I ever did my life right. It was my only happy time. For me, it's either methadone or a needle."
–Susan R., Rikers Island Correctional Facility.[19]
Medication-Assisted Therapy (MAT) for opioid dependence, for example with methadone or buprenorphine, prevents opioid withdrawal, decreases opiate craving, and diminishes the effects of illicit opioids. Often called "opioid substitution therapy," MAT is one of the most effective and best-researched treatments for opioid dependence. Once a patient is stabilized on an adequate dose, he or she can function normally.[20]
The World Health Organization (WHO), the United Nations Office on Drugs and Crime (UNODC) and the Joint United Nations Programme on HIV/AIDS (UNAIDS) have each supported the expansion of MAT because it is an evidence-based therapy that has proven effective for HIV and hepatitis C prevention, as well as reducing illicit opioid use and deaths due to overdose, improving uptake and adherence to antiretroviral treatment for HIV-positive drug users, and is cost-effective to society.[21]
In 2005, the WHO added buprenorphine and methadone to the list of essential medicines and in 2006, together with UNODC and UNAIDS, recommended that governments ensure access to MAT free of charge to opioid-dependent prisoners where it is available outside of prison, and that where no MAT is available in the outside community, "prison authorities add their voice to lobby for changes in policy to make such treatment nationally available, including within prisons."[22]
Upon incarceration, many opioid-dependent people are forced to undergo abrupt opioid withdrawal (both from legally prescribed therapy, such as with methadone, as well as from illicit opioids). Forced or abrupt opioid withdrawal can cause profound mental and physical symptoms (including severe abdominal cramping, nausea, diarrhea, anxiety, and convulsions), and can have serious medical consequences for pregnant women and their fetuses, immunocompromised people, and people suffering from both mental health and medical disorders. [23] Indeed, the US Department of Health and Human Services has recognized that the trauma of imprisonment, coupled with sudden, severe opioid withdrawal, can endanger mental and physical health, including by increasing the risk of suicide in opioid-dependent individuals with co-occurring disorders.[24]
There is evidence that MAT programs are feasible in a wide range of prison settings, and that prison-based MAT programs are effective in reducing frequency of drug use, mortality from overdose, and recidivism and reincarceration. [25] MAT also facilitates entry into and retention in post-release treatment; reduces drug-seeking behavior; and has a positive effect on institutional behavior and therefore prison safety.[26] MAT is cost-effective. For example, an Australian study showed that the program paid for itself when prisoners leaving the system avoided just 20 days of incarceration. [27]
The number of prison systems providing MAT has increased steadily since the early 1990s, and there are now many models for providing MAT in the New York State prisons. At this writing, prisons in at least thirty-three countries, including Spain, Brazil, Canada, New Zealand, the Czech Republic, Albania, and the United States (Puerto Rico)have successfully implemented methadone maintenance programs. Large urban jails in the United States, including in Albequerque, New Mexico (see highlight box); Orange County, Florida; Rikers Island Jail in New York City and jails in three counties in Pennsylvania, are successfully implementing methadone maintenance for prisoners who were on methadone before their arrest.[28] Buprenorphine, a partial opiate agonist that can be prescribed by primary care physicians without the more complex licensing requirements of methadone, is currently provided prior to or post-release in correctional facilities in Connecticut, Maryland, Rhode Island, New York City and in Tompkins County, New York. [29]
Legal Obligations
Access to Drug Dependence Treatment in Prison
A significant number of New York state prisoners used illicit drugs prior to incarceration. Many of these people have developed drug dependence, a serious, chronic, and often relapsing disease as a result of their drug use.[30] Many prisoners continue to use drugs while incarcerated; some stop using, while others initiate drug use.[31]
As is the case with people affected by other diseases, persons dependent on drugs – including prisoners – have a right of access to medical care for their condition, both under international human rights law and US law. International law is clear that prisoners are entitled to health care services that are at least equivalent to those available in the general community, which should be available, accessible, acceptable and of good quality. New York state law requires that New York prisons provide "adequate health care and health services to all inmates in order to protect their physical and mental well-being."[32]
The International Covenant on Economic, Social and Cultural Rights (ICESCR), a treaty signed but not ratified by the United States, recognizes the "right of everyone to the highest attainable standard of health."[33] Under the ICESCR, states must take steps to ensure that health care services are available, accessible, acceptable and of good quality. [34] For drug users, the availability of drug dependence treatment is a key element of this right, as is the availability of harm reduction services.
Harm reduction programs attempt to minimize the harmful effects of drug use through pragmatic, evidence-based practices such as sterile syringe exchange and Medication-Assisted Therapy that are proven to reduce use of shared needles that can transmit blood-borne diseases such as HIV and hepatitis C. Thus, drug dependence treatment, both as medical care for illness and, in the case of Medication-Assisted Therapy for opioid dependence, as a harm reduction strategy, constitutes a fundamental element of the right to health for people who use drugs.[35]
The United States is a party to the International Covenant on Civil and Political Rights (ICCPR)[36], which guarantees to all persons the right to life, and to be free from cruel, inhuman or degrading treatment; and if deprived of their liberty to be treated with humanity and with respect for the inherent dignity of the human person. Under the ICCPR, governments must provide "adequate medical care during detention." [37]
The United States is also a party to the Convention Against Torture and other Cruel, Inhuman or Degrading Treatment or Punishment (CAT)[38], which protects all persons from torture and ill-treatment. Failure to provide medical care to prisoners may violate the Convention Against Torture. Article 16 of the CAT prohibits acts of cruel, inhuman or degrading treatment, and the Committee Against Torture has found that a failure to provide adequate prison medical care can violate article 16.[39]
The United States is party to UN drug control conventions obliging it to establish rehabilitation and social reintegration services for drug users according to international standards, and to make provisions for treatment systems.[40] The UN Special Rapporteur on torture and other cruel, inhuman or degrading treatment recently addressed the importance of ensuring that international drug control policy meaningfully protects the human rights of drug users. Noting that "drug users are particularly vulnerable when deprived of their liberty," the Special Rapporteur urged member states to ensure that detained drug users have access to medical treatment, including opioid substitution therapy such as methadone and buprenorphine. [41] The Special Rapporteur concluded:
…drug dependence should be treated like any other health-care condition. Consequently…denial of medical treatment and/or absence of access to medical care in custodial situations may constitute cruel, inhuman or degrading treatment or punishment and is therefore prohibited under international human rights law. [42]
United States law also protects prisoners' health, and legal standards related to drug dependence are evolving. (See highlight box) In the United States, prisons that exhibit "deliberate indifference to serious medical needs" may be liable for violations of the 8th Amendment prohibition of cruel and unusual punishment.[43] A lack of medical care is unconstitutional when it involves the "unnecessary and wanton infliction of pain."[44]
A Right to Medication-Assisted Therapy Under US Law
In the United States, withdrawal from drugs and alcohol in prison has been found to be a "serious medical need" that gives rise to an obligation to provide adequate medical care.[45]Courts in the US generally have not upheld the right of prisoners to methadone maintenance treatment, though relief has been granted in individual cases.[46]However, decades have passed since the majority of those cases were decided, and during these years significant advancements have been made in the scientific, medical and behavioral approaches to addiction as a disease. The American Psychiatric Association defines "substance dependence" as a "maladaptive pattern of substance use." [47]If physical or mental impairment results, a diagnosis under this definition can be the basis for a finding of disability, and entitlement to benefits, under the Social Security Act.[48] Similarly, drug addiction is a 'protected impairment' under the Americans with Disabilities Act.[49]Today, it is increasingly difficult to argue that clinically diagnosed addiction is not a "serious medical need" triggering a level of obligation under the 8th Amendment.
Methadone maintenance is now a therapeutic modality with a thirty-year track record and successful implementation in many prison systems. It is time to re-examine US legal approaches to the rights of drug dependent prisoners to evidence-based treatment for their condition.
As stated in one recent analysis:
"Courts facing inmate claims of cruel and unusual punishment for being denied methadone in prison must reexamine the case law in the light of modern conclusions about Methadone Maintenance Therapy. Courts are correct to be cautious with competing science, but they should not shy away from making decisions when presented with a consensus of medical specialists and scientists. Courts should not be afraid to step out of narrow methadone precedent and examine opioid dependence disorder in a new light, as a medical illness requiring MMT rather than a moralist debate."[50]
Findings
New York State's policy decisions relating to substance abuse in prison are inconsistent with its domestic and international obligations to prevent cruel, inhuman and degrading treatment, provide adequate medical care to prisoners and protect the right to health.
New York's Department of Correctional Services has acknowledged that a significant number of prisoners are in need of substance abuse treatment, and New York prisons provide an array of substance abuse-related programs. Despite New York State's recognition of the importance of drug dependence treatment for prisoners, Human Rights Watch's research shows that a substantial number of prisoners who use drugs do not have access to evidence-based care to treat their dependence. New York State has identified thousands of prisoners as opioid users in need of treatment. Heroin overdoses- and overdoses on other drugs-including fatalities-have been documented both in prison and upon release. But Medication-Assisted Therapy (MAT), the most effective treatment for opioid dependence and a treatment proven to prevent overdose, is provided on an extremely limited basis, and unavailable altogether to most prisoners who need it.
A significant number of prisoners-including those identified by the prison system as in need of treatment-either face extended delays in receiving treatment, or are effectively barred from treatment services that do exist because they do not speak English or have limited English literacy skills. Nor do people who use drugs have access to basic harm reduction methods proven to prevent HIV and hepatitis C.
At the same time, punishment for drug use in New York State prisons is severe and out of proportion to the seriousness of the offense. Prisoners who may be drug dependent are punished for symptoms of a chronic, relapsing disease. Drug dependence treatment is withheld from prisoners who may need it as part of the disciplinary sanction.
Lack of Access to Evidence-Based Treatment for Opioid Dependence
In New York State, Medication-Assisted Therapy (MAT) is widely available outside of prison. The New York State Office of Alcohol and Substance Abuse Services (OASAS) licenses the largest methadone treatment system in the US, with 115 clinics operating throughout the state. There are 1,212 licensed buprenorphine providers and 281 buprenorphine programs in New York. [51] The majority of people arrested and detained in New York State, however, have no access to methadone or buprenorphine. Upon entering jail (where individuals are held pending bail, trial and sentencing, or can serve sentences up to one year) most are forced to undergo withdrawal "cold turkey" and face the health risks described above. Upon transfer to prison (where individuals serve sentences longer than one year) MAT is not available to the majority of those who need it.
Jail inmates in New York City have access to MAT. Rikers Island jail in New York City, one of the country's largest correctional facilities, offers short-term detoxification from opioids using Medication-Assisted Therapy. Rikers also maintains prisoners on methadone if they entered the facility while in a methadone program and, if medically warranted, offers it to prisoners without a previous history of methadone treatment. Rikers provides methadone maintenance treatment to approximately 4,000 prisoners per year, linking them to community programs upon release. Rikers Island is a jail facility, however, and inmates whose criminal charges make them eligible for state prison time (more than a one year possible sentence) are offered methadone only for short-term detoxification as there is no opportunity to continue methadone treatment in the New York State prison system. [52]
Detoxification on its own is not a rehabilitative treatment for drug dependence, but it can be a "precursor of treatment" and linkage to treatment is a crucial component of evidence-based detoxification. [53] However, at Rikers Island jail in New York City, State-bound prisoners must be terminated from the most effective form of treatment for opioid addiction, leaving them at risk of relapse, overdose, and blood-borne diseases through sharing of needles. [54]
In Tompkins County jail, severely opioid-dependent prisoners are started on buprenorphine approximately one month prior to their release date and then linked with a licensed buprenorphine provider in the community for continuing care. The facility's mental health director, Dr. John Bezirganian, told Human Rights Watch that the jail program has "saved more than one life" by preventing overdose upon release.[55]
Tompkins County, however, is the only jail outside of New York City that provides Medication-Assisted Therapy. Jails in the other 56 New York counties could correct this problem immediately. In November 2006, the New York State Commission on Correction notified county sheriffs and jail administrators of new federal regulations permitting easier administration of buprenorphine, and noted:
Safe and effective medical treatment in jail for the often dangerous complications of opioid withdrawal is part of the generally recognized standard of adequate medical care in New York and elsewhere… Buprenorphine can be used to provide a safe, effective and inexpensive withdrawal regimen in the jail setting.[56]
In the New York State prisons, only a small program at Bedford Hills Correctional Facility, a maximum security women's prison, provides Medication-Assisted Therapy. At Bedford Hills, pregnant women are maintained on methadone until delivery of their babies. However, the stated goal of the Bedford Hills program is neither treatment nor harm reduction, but protection of the fetus, and the mother is removed from methadone as quickly as possible.[57] Prisoners for whom methadone is available in jail should have the option to remain on maintenance therapy when sentenced to a state facility, if such a course is deemed to be medically appropriate. Buprenorphine therapy could be integrated into existing re-entry programs such as the recent pilot program at the Orleans Correctional Facility near Buffalo, a program slated for expansion that links prisoners to community substance abuse treatment programs. The existence of the Bedford Hills program indicates the feasibility of operating such a program even in New York's maximum security prisons.
The failure to ensure access to MAT puts opioid dependent prisoners at risk of relapse and overdose on release from prison. Human Rights Watch interviewed Susan R., 30, in Rikers Island jail, where she was incarcerated pending transfer to state prison. A self-described "heroin addict" since age fourteen, Susan told Human Rights Watch that she'd been "in and out of jail in Florida, Colorado, New York" and that "all of my crimes have to do with heroin, either copping, using, or stealing."[58] Susan R. had been incarcerated in Albion Correctional Facility, where only abstinence-based treatment (the Alcohol and Substance Abuse Treatment Program, commonly known as ASAT) was provided to treat her heroin addiction. Susan was in a methadone program at Rikers Island, but feared relapse or death from overdose if she were returned to Albion. She told Human Rights Watch:
At Albion, they put me in ASAT. I got out and hooked up with the friend I did my crime with and we copped right away. I overdosed in the office of a methadone clinic waiting for an appointment. When I got out of the hospital they sent me here. I'm on methadone now but they are tapering me off so I can go back upstate. If I go back up there and ASAT is all I have, I'll end up with a needle in my arm, or dead.[59]
Failure to provide MAT is also inconsistent with international guidelines and US correctional health standards, which recommend that MAT be provided in prison. For example, the National Institutes of Health (NIH) and the National Institute for Drug Abuse (NIDA) have endorsed the effectiveness of Medication-Assisted Therapy and urged federal and state authorities to increase its availability in criminal justice and prison settings.[60] The National Association of State Alcohol and Drug Abuse Directors promotes the use of Medication-Assisted Therapy in correctional settings.[61] The National Commission on Correctional Health now offers an accreditation program and provides technical assistance for methadone maintenance in US prisons and jails.[62]
New York State's resistance to MAT may be based upon a lack of understanding. The Superintendent of the Willard Drug Treatment Campus, a 900-bed facility operated by DOCS and the Division of Parole for parole violators, told Human Rights Watch that "the jury is still out" on methadone, and that he was unfamiliar with buprenorphine.[63]
New York State's failure to ensure MAT for opioid-dependent prisoners denies them access to the most effective treatment for their condition, and violates New York's obligation, and its promise to the public, to ensure a level of health care equivalent to that available in the community. Failure to ensure MAT to prisoners also threatens fundamental rights to life, health, and freedom from ill-treatment by putting prisoners at risk of premature death by overdose, HIV/AIDS and other life-threatening illnesses.
Case Study: Medication-Assisted Therapy in a New Mexico Jail
New Mexico has rates of injection drug use, opioid addiction and overdose that are among the highest in the United States. New Mexico also leads the nation in addressing the problem with evidence-based treatment and harm reduction. Bernalillo Metropolitan Detention Center, New Mexico's largest jail, has offered methadone maintenance therapy to prisoners who were on methadone before they were sentenced to jail since 2005. 1,800 prisoners have received MAT since the program began. When Human Rights Watch visited the Center in July 2008, there were 55 prisoners receiving MAT.
MAT is dispensed daily to prisoners by a nurse who observes each prisoner swallowing his or her dose to ensure that it is ingested. Medical staff told Human Rights Watch that "methadone is medicine." In their view, they were obligated to continue their patients on methadone just as they would any prescriptions taken by inmates before they entered the jail. [64]
The word most often used by the prisoners interviewed by Human Rights Watch was "grateful"- for allowing them to avoid a difficult detoxification process and for a feeling of normalcy that allowed them to hold jobs in the prison, participate in programming, and make decisions in their legal cases. As one prisoner told Human Rights Watch, "Without the methadone I'd be real sick and just trying to score. Now I can think straight and figure out how I'm going to turn my life around."[65] New Mexico corrections officials told Human Rights Watch that the program had no negative effect on jail security.
A jail program also provides overdose education sessions to opioid dependent prisoners before they leave the jail, and links those not already on methadone to community-based MAT providers. State officials are currently considering implementing a buprenorphine program in New Mexico's state prison system.[66]
Risk of Overdose During Incarceration and After Release
Prisoners who use illicit drugs face significant risk of overdose during incarceration and upon release to the community.[67] Periods of abstinence may diminish tolerance to drugs, and thus increase the risk of fatal and nonfatal overdose for individuals who relapse to drug use, as is often the case.[68] The New York State Department of Corrections reported that between 1996 and 2005, 27 prisoners died from overdoses of illegal drugs while incarcerated, and that "[n]umerous other inmates had to be taken to outside hospitals for treatment of drug overdoses from which they recovered."[69] The New York State Commission on Corrections documented at least 13 drug overdose deaths among New York State prisoners between 2001 and 2007, including deaths due to heroin overdose.[70]
Reentry to the community provides a critical opportunity for overdose prevention education. Overdose prevention programs in other jurisdictions include education, linkage to treatment and, increasingly, distribution of Naloxone, a drug that can prevent fatality in the case of opioid overdose. In New Mexico, for example, jail inmates are provided specific overdose education sessions just prior to release and linked to facilities in the community that distribute Naloxone. Similar programs operate in San Francisco and at Rikers Island. [71]
The New York State prison system, however, offers no overdose prevention programs directed at those at high risk of relapse or overdose (such as opioid users) on release. Instead, The New York State prison system's substance abuse curriculum includes overdose as one of many topics discussed in the class.[72] For example, at the Willard Drug Treatment Facility run by the Department of Correctional Services for parole violators, a counselor told Human Rights Watch, "We tell them about overdose as part of the program but there is nothing directed toward opiate addicts specifically."[73] According to this counselor, a heroin addict died of overdose in 2007 shortly after leaving the Willard facility. The counselor also stated that she would be open to considering buprenorphine for use at Willard.[74]
To its credit, DOCS has recently trained re-entry staff in each of its facilities on overdose prevention using a curriculum provided by the AIDS Institute of New York State.[75] If drug dependent prisoners begin to receive potentially life-saving prevention education as they leave prison, New York will have taken a positive step toward meeting its obligation to provide necessary health services and information for this population.
Susan R.'s experience with relapse, overdose, and reincarceration (described above) illustrates the serious health and legal risks faced by New York State prisoners denied access to MAT in prison and provided inadequate overdose prevention education and services on release. Malcolm A., a prisoner at Great Meadow Correctional Facility, told Human Rights Watch about the overdose of his friend Theo, who was "a heavy heroin user, he did 18 years in here, and was dead within days of getting out."[76]
Barriers to Access to Available Substance Abuse Treatment
New York State offers an array of prison substance abuse programs. These include programs directed to specific populations, including pregnant women, domestic violence offenders, and persons in prison for driving while intoxicated. "Shock incarceration" programs are offered to young, non-violent, first-time drug offenders. The Department of Correctional Services (DOCS) also contracts with treatment programs in the community to provide services to prisoners on work release. The Willard Drug Treatment Campus and the Edgecombe Correctional facility provide residential treatment programs to parole violators.[77] As is true in prisons throughout the United States, many prisoners have serious mental illness as well as substance abuse disorder.[78] For this dual diagnosis population, DOCS offers the Mentally Ill/Chemically Dependent (MICA) program. The New York State prison programs are abstinence-based, providing Medication-Assisted Therapy only to pregnant women as described above.
Most facilities offer one or more substance abuse-related program and many prisoners have access to some type of program during their incarceration. DOCS reports indicate that of inmates identified as needing treatment, 45 percent were receiving services and another 18 percent were on a waiting list. [79] The Correctional Association, a prison monitoring agency created by the New York State Legislature, reports that 33,000 prisoners had access to some substance abuse programming in 2007.[80] However, this is still significantly fewer than the 45-53,000 prisoners determined by DOCS to need substance abuse services.
Moreover, very few of these programs are certified or licensed by the New York State Office of Alcohol and Substance Abuse Services (OASAS), the agency responsible for ensuring that treatment programs in New York meet minimum standards.[81] According to correctional health experts, most prisoners in the United States receive substance abuse education rather than evidence-based treatment.[82] Evidence-based treatment includes programs targeted toward individual needs that offer flexible and various treatment modalities such as psycho-social therapy, cognitive-behavioral intervention, and Medication-Assisted Therapy for opiate addiction. Ninety days is considered a minimum threshold for effectiveness and continuity of care and follow up services are essential. [83] Prison drug treatment is cost effective. Recent studies indicate that for every dollar invested in treatment programs, states save between two and six dollars in reduced recidivism and health care costs. [84]
Other than the failure to provide Medication-Assisted Therapy for opioid dependence, the extent to which New York's substance abuse programming complies with evidence-based standards for dependence treatment is not examined in this report. However, Human Rights Watch found that in many cases, prisoners do not receive access to these programs when they need them most.
A significant number of New York prisoners-including many identified by the prison system as in need of treatment-face lengthy delays in receiving substance abuse treatment, sometimes waiting years before being put into a treatment program. Many prisoners are also barred from meaningful participation in available substance abuse treatment because no accommodation is made for people who have limited or no English literacy skills. This includes foreign-born prisoners (who comprise 10 percent of the prison population), and prisoners who read and write at low levels (an estimated 33 percent of the prison population).
Delayed Access to Treatment
In New York, many prisoners experience lengthy delays in admission to treatment programs, even in cases where the prison system has determined their addiction to be severe and thus identified them as persons in need of substance abuse treatment. Delaying access to necessary medical services threatens the fundamental right to health and may violate the protection against cruel, inhuman and degrading treatment or punishment by subjecting drug dependent prisoners to unnecessary mental and physical suffering. In addition to human rights concerns, failure to treat drug dependent prisoners is bad public policy, as failure to treat drug dependent prisoners increases the likelihood of return to prison. [85]
DOCS screens incoming prisoners for substance abuse treatment needs. However, the screening process does not provide for immediate admission to treatment even when addiction is found to be severe. Many prisoners identified as in need of treatment are placed on waiting lists for the ASAT or Residential ASAT (RSAT) (the abstinence-based programs described above) or the smaller, specialized programs if appropriate. [86] There are indications that DOCS screening processes may be over-inclusive in its identification of prisoners in need of treatment, leading to larger waiting lists. [87]
DOCS policy is to give priority for these programs to prisoners who are within 2 years of their release dates.[88] This policy is designed to facilitate participation in treatment programs in some proximity to re-entry to the community – an important goal. However, by design, it also delays necessary treatment for prisoners with longer sentences, solely by virtue of the length of their remaining prison time, and thus can delay care for prisoners in urgent need of treatment. As of January 2008, for example, there were 540 participants in the Residential Substance Abuse Treatment (RSAT) program and 2,065 persons on the waiting list. The Comprehensive Alcohol and Substance Abuse Treatment Program (CASAT), a program with a work release component, had 1,462 persons on the waiting list as of September 2007. [89]
Human Rights Watch found – consistent with DOCS' own reports – that many prisoners waited years for admission to substance abuse treatment programs. [90]
Carlos R., a prisoner at Great Meadow Correctional Facility, told Human Rights Watch:
I waited 12 years for an ASAT program- I kid you not. I kept being transferred to other units before I got in, and at your new unit they start you on the list again. If you get a [disciplinary] ticket, you get kicked off for a period of time. Then I finally got a spot but they needed me to work in the kitchen so they put me there instead. [91]
Peter G., a prisoner at Southport Correctional Facility, had not been enrolled in a treatment program, despite having been disciplined for drug-related offenses on numerous occasions. He said, "I've had 15, 16 drug tickets. No assaults or anything like that. I've never been in a treatment program. Guys get frustrated, waiting years on the list for ASAT. Forget getting into RSAT." [92]
Access to ASAT is to some degree a matter of chance, as staff shortages at some facilities exacerbate the wait. James W., a prisoner at Attica Correctional Facility, reported:
I was in the ASAT program at Attica until a few weeks ago. They discontinued the program because staff was transferred, and now the waiting list is over 1,000. Even though I get priority, here's a notice telling me that "it could be a long time" until I get into treatment again. [93]
Lack of Access to Treatment for Non-English Speaking and Low Literacy Prisoners
New York State substance abuse treatment programs do not ensure translation for non-English speakers, nor are provisions made for prisoners with low literacy levels. This is inconsistent with the obligation to respect prisoners' right to "seek, receive and impart information" as it pertains to vital information about their health and life. This right is protected by the International Covenant on Civil and Political Rights (article 19) and in the context of health care services imposes an obligation to ensure that prisoners can obtain information about treatment services, and at a minimum that they should not be deprived of access to such information on an arbitrary basis such as literacy or language skills.[94] Access to appropriate information about health issues that will enable prisoners to make informed decisions about their personal health has also been categorized as an element of the right to private life, which is also guaranteed under the ICCPR. [95]
In New York State, 10 percent of the prison population, about 6,300 prisoners, is foreign born. Of these, only 28 percent come from countries where English is the primary language.[96]
DOCS has identified the language barrier as problematic:
One of the major concerns centers on language. Successful programming and institutional security depend on effective communication….Given the significant number of foreign-born inmates under custody, the Department may have to expand its capacity to deal with a diversity of languages. [97]
Human Rights Watch spoke with several prisoners who described problems faced by Spanish-speaking prisoners in understanding materials presented in prison substance abuse treatment programs.
Prisoners who had participated in ASAT classesreported, for example, that Spanish-speaking prisoners had difficulty understanding them. Alfredo F., a prisoner at Attica, told Human Rights Watch, "Some guys can't understand English and nobody helps. Things are written on the board and people can't read it." [98] Carlos R., a prisoner at Great Meadow Correction Facility, said that in his ASAT program, "One Spanish guy sometimes translated, but they just assume you speak English. None of the written materials are in Spanish."[99]
1 of 3 New York State prisoners reads below an 8th grade level. [100] Prisoners who read and write at low levels told Human Rights Watch that they failed to understand much of the instruction that was written on the board.
Ron L., for example, told Human Rights Watch, "I was young when I first went to treatment. I couldn't read or write much, so I missed most of what was going on in the class, but I didn't want to admit it. I think that happens to a lot of guys.[101]
Lack of Access to Harm Reduction Services
International drug and health organizations, including the UN Office on Drugs and Crime, the World Health Organization, and UNAIDS, recommend that comprehensive harm reduction services – including Medication-Assisted Therapy (for example with methadone or buprenorphine), and the provision of condoms and of sterile needles and syringes – be provided to prisoners to help reduce HIV transmission and other harms related to injection drug use. Yet notwithstanding these recommendations, and despite mounting evidence that harm reduction measures have proven effective in reducing HIV risk behaviors in a wide range of prison environments without negative consequences for prisoners or prison staff, harm reduction services are unavailable to the vast majority of New York's prisoners.
Despite a population with a high proportion of drug users, prisoners living with HIV and prisoners living with hepatitis C, New York State fails to provide any of the leading evidence-based harm reduction measures proven to protect their health. Neither condoms, nor bleach, nor sterile syringes are available in the New York prison system. As described above, Medication-Assisted Therapy is not provided to the majority of opioid-dependent prisoners despite its proven effectiveness in reducing harms related to injection drug use.
Although the majority of prisoners with HIV and hepatitis acquired the infection outside of prison, the transmission of HIV and hepatitis C in prison is increasingly well documented. [102] There is strong evidence that although prisoners inject drugs in prison to a lesser degree than on the outside, when they do inject they are much more likely to share needles, thus greatly increasing the risk of transmission of HIV, hepatitis B and hepatitis C. [103] Gary D., a prisoner at Upstate Correctional Facility, told Human Rights Watch, "Guys mostly snort [heroin], but needles are accessible."[104] Robert F., a prisoner at Attica Correctional Facility, stated, "Lots of guys use each other's needles for tattoos." [105]
In recent years, many countries have responded to high rates of HIV and hepatitis in prisons by implementing harm reduction measures. Harm reduction programs focus on preventing and reducing the harmful consequences of drug use through a range of targeted interventions including distribution of bleach, sterile syringes and tattoo safety education, condom availability, and Medication-Assisted Therapy for prisoners addicted to opiates. In contrast to punitive approaches that attempt to eliminate, stigmatize and criminalize drug use, harm reduction emphasizes public health, individual quality of life and respect for human rights. Harm reduction is also a pragmatic approach that acknowledges the reality that prisoners engage in sexual activity and drug use while incarcerated[106], and views prison health as a key component of the health of the larger community.
There are many models for implementation of condom distribution policies in correctional settings, both within and outside the US. In the US, for example, several large urban jails, including in Los Angeles, San Francisco, and Washington, D.C., make condoms available to inmates. In California, a pilot program begun in November 2008 distributes condoms at Solano State Prison. Condoms are also distributed in many prison systems worldwide, in countries as diverse as Mexico, France, Ukraine, Australia and Estonia. [107]
Recent evaluations of programs in the US, Canada and Australia have concluded that condoms can be distributed without disruption of prison security.[108] One study examined the condom distribution program in effect since 1992 at the Central Detention Facility (CDF) in Washington, D.C. The CDF houses approximately 1400 adult males, 100 adult females and 40 juveniles, processing 2800 prisoners per month. The CDF has a staff of 551 corrections officers. No major security infractions related to condoms had been reported since commencement of the program. There was no indication that sexual activity had increased, based upon staff interviews as well as a review of disciplinary reports for the same period. The researchers concluded:
Permitting inmates access to condoms remains controversial among correctional professionals. Even so, no prison or jail in the United States allowing condoms has reversed their policies, and none has reported major security problems. In the Washington, D.C. jail, the program has proceeded since 1993 without serious incident. Inmate and correctional officer surveys found condom access to be generally accepted by both. [109]
Preliminary evaluation of the Solano State Prison program in California indicated "no serious incidents involving harm to staff or inmates or unintended use of condoms have been reported."[110]
More than 50 prisons in twelve countries in Europe and Central Asia have established needle and syringe exchange programs to prevent HIV and other blood-borne diseases among prisoners.[111] A proven method of reducing HIV and hepatitis C transmission outside of prison,[112] needle exchange is now available in prisons in Spain, Switzerland, Luxembourg, Armenia, Kyrgyzstan, and Moldova. Pilot programs are in development in Portugal, Belgium and the United Kingdom.[113] Evaluations of these programs have indicated no increase in drug use or negative impact on prison security. Indeed, staff safety improved as accidental injuries to staff from hidden injection equipment during cell searches declined. [114] Bleach and other disinfectants to sterilize needles and syringes have also been made available in a number of prison systems throughout the world.[115]
New York's failure to enact evidence-based programs proven to protect prisoner health without compromising security threatens the fundamental right to life and undermines New York's legal obligation to provide "adequate health care and services to all inmates in order to protect their physical and mental well being."[116] Contravening the principle that "good prisoner health is good community health," New York's policies create unnecessary health risks for prisoners and for the communities to which they return.
Disciplinary Measures for Drug Use and Possession in Prison
Illicit drug use or possession is prohibited in prisons around the world. As with other infractions, prison authorities may impose disciplinary measures on prisoners who use or possess drugs. However, under international human rights standards, disciplinary sanctions must be proportionate and necessary to maintain prison safety and security. Sanctions that are disproportionately severe risk violating the prohibition of torture and cruel, inhuman and degrading treatment and punishment. The UN Standard Minimum Rules for the Treatment of Prisoners provide: "Discipline and order shall be maintained with firmness, but with no more restriction than is necessary for safe custody and well-ordered community life."[117] In determining disciplinary sanctions prison authorities must also ensure that sanctions do not disproportionately restrict prisoners' enjoyment of other rights, including the right to health.
Human Rights Watch's research has found that the New York State prison system routinely imposes grossly disproportionate disciplinary sanctions on prisoners who use drugs. These sanctions are so severe as to violate the prohibition of cruel, inhuman and degrading treatment and the right to health. Thousands of prisoners are placed each year in solitary or semi-solitary confinement for extended periods of time-sometimes years-for possessing or using illicit drugs. Some of these prisoners are, according to the prison system itself, in need of substance abuse treatment which, as described above, is often delayed or inaccessible. Prisoners are subjected to disciplinary sanction without regard to whether they may be clinically drug dependent and thus unable to control their drug use behavior. Prisoners who are in drug dependence treatment when committing the drug-related offense are removed from the treatment program and disciplined rather than provided with therapeutic support. No treatment is offered in disciplinary confinement. Finally, the screening system the New York State prison system uses to monitor illicit drug use is problematic as it encourages drug use practices that increase the risk of HIV and hepatitis C transmission.
New York State's Disciplinary System for Drug Use
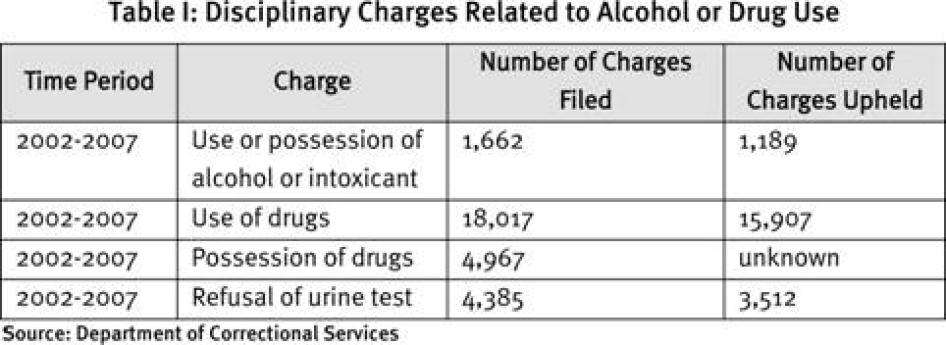
New York State prisons strictly prohibit the possession, use or transfer of drugs and alcohol. Records obtained by Human Rights Watch through the New York State Freedom of Information Law suggest that New York State prisons aggressively enforce this prohibition. Between 2002 and 2007, almost 18,000 charges of drug use were brought before internal disciplinary hearings; nearly 5,000 charges were brought for drug possession and another 4,385 were filed for refusing a urine test, which also constitutes a disciplinary offense (See Table I).
Under New York State prison regulations, possession and use of drugs or alcohol[118] - or refusal to be tested for them[119] - are considered "Tier II or III" offenses. For Tier II offenses, prisoners can receive up to 30 days in a disciplinary confinement area called the "Special Housing Unit" and lose numerous privileges, including recreation, visitors, correspondence, and possession of personal items. Tier III offenses may be punished by unlimited time in a Special Housing Unit, the loss of "good time"- time prisoners accumulate over the course of their incarceration that can permit their early release-and of numerous privileges, and the imposition of a special diet-popularly known as "the loaf"- which consists of dry, dense bread and cabbage.[120] The determination whether a specific offense qualifies as a Tier II or III violation, and the specific punishment given, falls within the discretionary power of prison officials.
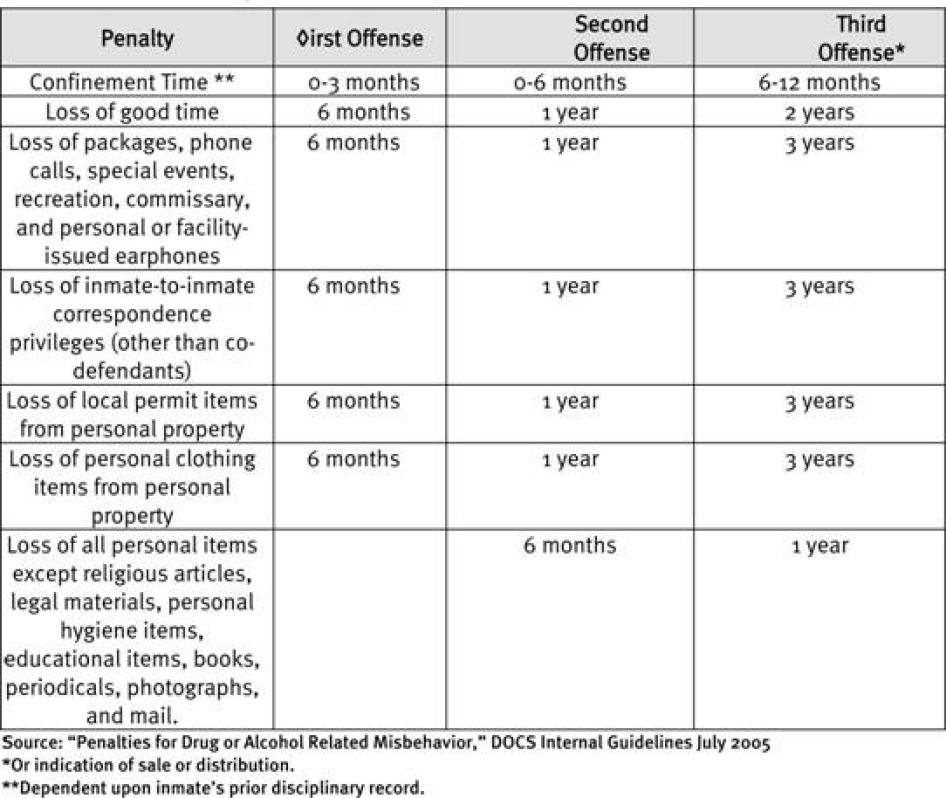
The Department of Correctional Services has issued non-binding guidelines for correctional officers on penalties for drug-related offenses (see Table II). These guidelines recommend that first time offenders be sentenced to disciplinary confinement for zero to three months, along with loss of privileges and "good time" for six months; that second time offenders get zero to six months of disciplinary confinement and six months to a year of lost privileges and good time; and that third time offenders be sent to disciplinary confinement for six months to a year of confinement, and get two years of lost good time and one to three years of lost privileges. However, since the guidelines are only a recommendation, correctional officials are free to impose more stringent or lenient penalties at their discretion.[121]
New York is among the nation's leaders in the use of 23-hour disciplinary segregation in its prisons. In 2003, 5,000 prisoners, or 7.6 percent of the prison population, spent time in disciplinary confinement, far exceeding the national average of 2.6 percent.[122] Although the number fell to 4,426 in 2007 only two states-Texas and California-placed more prisoners in disciplinary segregation than New York.[123] New York State's prison system uses Special Housing Units (known as SHU or "the box") for disciplinary confinement. SHU areas are attached to several of the older prisons, but in recent years New York has constructed 11 "supermax" prisons dedicated solely to disciplinary confinement. These high-tech, electronically surveilled units have the capacity to segregate 3,700 prisoners from the general prison population.[124] In addition, thousands of inmates are confined in their own cells under a similar regime in what the Department of Correctional Services calls "keeplock."[125]
In the Special Housing Units prisoners spend 23 hours a day in a cell measuring six by ten feet (if a single cell) and eight by thirteen feet (if a double cell). They are "cell-fed" by guards who push a tray through a slot in the door. Recreation takes place in an empty, similarly-sized concrete pen located off the rear of the cell itself. Here, the chain link fencing along one side offers the only natural light and view to the outside. A prisoner's access to educational or any other type of program, packages, visits, showers, letters, personal property and telephone calls are all extremely limited.
Table II: Penalties for Drug or Alcohol Related Misbehavior
·The following penalties may be imposed for any inmate found guilty of drug or alcohol related misbehavior
·These are recommended penalties, which may be mitigated or aggravated including, but not limited to the following factors:
oThe inmate's prior record
oThe type of facility
oThe nature of the present offense
While in disciplinary confinement, prisoners who violate Special Housing Unit regulations may be subjected to further "deprivation orders" on top of the original disciplinary sanctions. This can include shackling while recreating, denial of showers and haircuts, and the assignment of "the loaf." This dry, dense diet of bread and cabbage does not meet daily nutritional requirements and violates standards of correctional accreditation in the United States. [126]
In 2003, 1,100 prisoners spent time in disciplinary confinement for drug use or possession, comprising 20 percent of the total population in Special Housing Units.[127] Prisoners' Legal Services of New York, a leading public interest law group that works on behalf of prisoners in New York State, believes that the percentage of people in disciplinary confinement for drug related offenses has grown dramatically in recent years, based on the increasing caseload of prisoners seeking relief from disciplinary charges related to drug use and possession.[128] Documents requested by Human Rights Watch under the Freedom of Information Law show an upward trend in both numbers of drug-related disciplinary hearings held and severity of sanctions imposed during the period 2005-2007. (See Graphs III and IV)
Disproportionate Severity of Disciplinary Sanctions
Confinement in conditions that are disproportionate to the offense may violate the International Covenant on Civil and Political Rights' prohibition against torture or cruel and degrading treatment (article 7). In interpreting article 7, the Human Rights Committee has stated that "prolonged solitary confinement of the detained or imprisoned person may amount to acts prohibited by article 7."[129] Factors to be considered include the grounds for imposition of solitary confinement, the conditions endured in confinement and the duration of the sentence. [130] The UN Special Rapporteur on Torture recently addressed solitary confinement:
The practice has a clearly negative impact on mental health, and therefore should be used only in exceptional circumstances or when absolutely necessary…In all cases, solitary confinement should be used for the shortest period of time.[131]
The Standard Minimum Rules for the Treatment of Prisoners prohibits punishment of prisoners that is cruel or inhuman, not in accordance with law and prison regulations, and that is "prejudicial to the physical or mental health of the prisoner." [132]
Confinement for extended periods of time in near complete isolation from the outside world, as recommended in New York State's prison regulations and the Department of Correctional Services guidelines, for the non-violent offense of drug use or possession in prison is excessive. Aspects of drug use such as trafficking and gang activity may legitimately threaten the security of the prison environment and authorities may reasonably regulate drug use within the prison walls. However, New York prisons punish even minor drug-related infractions with severity. Isolation or near-isolation is used as a matter of routine rather than as a last resort after imposition of lesser sanctions. This approach has not been shown to be effective in reducing drug use or otherwise necessary to ensure "the safe custody and well-ordered community life" and also significantly undermines the mental health of prisoners subjected to it. As such, this type of disciplinary punishment violates both the prohibition of cruel, inhuman and degrading treatment and the right to health.
Our research found that in practice, prison officials routinely exceed the recommendations for disciplinary confinement contained in the Department of Correctional Services guidelines. Many prisoners we interviewed had received disciplinary sentences that went well above and beyond the recommended punishment.
For example, Michael L., a prisoner at Great Meadow Correctional Facility, told us: "I got 8 months for my first ticket for marijuana. I got it reduced, but lots of guys who don't read or write can't do the appeal."[133]
Nathan T., a prisoner at Upstate Correctional Facility, told us:
"I've had six or seven dirty urines. Never any violence. Just drugs. I got a year in SHU, then 18 months, then a year…I've been in the box 14 months on the last ticket and I just got another 20 months in here for possession."[134]
Prison rights advocates in New York believe that over the last few years prison officials have imposed increasingly severe disciplinary sanctions for drug-related offenses. As Karen Murtagh-Monks, Executive Director of Prisoners' Legal Services of New York (PLS), recently told legislators in Albany: "It is common for PLS to review cases where inmates have received 18 to 24 months in solitary confinement and lost 18 to 24 months of good time for having dirty urine."[135]
Graphs III and IV below show that in New York State, prisoners were sentenced to 2,561 years of time in SHU solely for drug-related offenses (i.e. excluding assault, disobeying orders, or any other charges) in the three year period 2005-2007. In addition, New York prisoners lost 2,561 years of good time solely for drug-related offenses during the same period (see Graph IV.) [136] The number of disciplinary hearings held solely for drug offenses increased each year, from 2,400 in 2005 to 2,600 in 2007. [137]
Graph I: New York State Prisons: Years in SHU for Drug-related Discipline
Source: Department of Correctional Services
Graph II: New York State Prisons: Years of Good Time Lost for Drug-related Discipline
Source: Department of Correctional Services
Many prisoners receive additional disciplinary sanctions-and further time in disciplinary confinement-because they commit new drug-related offenses while in Special Housing Units. According to the Department of Correctional Services, between 2002 and 2007 more than 2,186 charges were brought against prisoners for drug and alcohol use-or for refusing the urine test-while in Special Housing Units (see Table V). The consecutive disciplinary sentences many of these prisoners receive result in years of disciplinary confinement.
As a result of the harsh disciplinary regime, some prisoners end up "maxing out" by serving their full criminal sentences as they lose all "good time" that would normally allow for their early release. Because prisoners are ineligible for parole while under disciplinary charges, prisoners who "max out" their sentences are released directly from the Special Housing Unit to the community. Some prisoners in the general population have access to re-entry programs that include linkage with community services, including drug treatment programs. Prisoners who complete their sentences after years in SHU are at risk of losing important re-entry services afforded to members of the general population.
This policy is particularly problematic because prisoners who continue to use drugs while in SHU may suffer from drug dependence, and thus have the most acute need for treatment. Lawrence Y., a prisoner at Southport Correction Facility, for example, told us that he had been "in the box since 2004 for one drug ticket after another. I'm going to max out in here. I'll go home with the same habit I came in with." [138]
Interference with the Right to Health
The disciplinary regime of New York State's prison system interferes with prisoners' right to health in four respects: the confinement itself creates and exacerbates mental health problems; prisoners who are dependent on drugs are subjected to disciplinary punishment even though their drug use is related to a medical condition; prisoners are denied drug treatment when they commit drug related disciplinary offenses; and the drug testing procedure used encourages risky drug use and increases the risk of HIV and hepatitis C transmission.
Mental Health Impact of Special Housing Unit Confinement
Confinement in the conditions of Special Housing Units has a profound negative impact on the mental health of prisoners. Human Rights Watch has previously documented the psychological and emotional effects upon prisoners of the special confinement regime known as "supermax" in which conditions are similar to those in Special Housing Units.[139] In a 2000 report, we found that:
There is no way, of course, to measure the misery and suffering produced by prolonged supermax confinement. Inmates have described life in a supermax as akin to living in a tomb. At best, prisoners' days are marked by idleness, tedium and tension. But for many, the absence of normal social interaction, of reasonable mental stimulus, of exposure to the natural world, of almost everything that makes life human and bearable, is emotionally, physically and psychologically destructive.[140]
The New York State Correctional Association, an organization with a statutory mandate to oversee prison conditions in New York State, has been highly critical of the state's use of supermax-like conditions to discipline prisoners. In a 2003 report the monitoring agency wrote that their visits to the lockdown units "reveal a disturbing picture characterized by emotional and physical distress, a reliance on warehousing instead of treatment, high rates of mental illness, suicide and self-mutilation, low staff morale and unsafe working conditions for prison and administrative staff."[141]
Prisoners interviewed for this report repeatedly described the effects of prolonged incarceration in disciplinary confinement on their mental health. Nathan T., for example, said:
I've been in 14 months straight, and just got another 20 months for possession... It's really taking a toll on me. I wrote to the people from mental health. I need some kind of therapy because the cell is closing in on me. I feel paranoid, I can't sleep. I feel like people are against me. I'm restless, I'm talking to myself." [142]
Lawrence Y. told us:
I was in the box at another unit and I started cutting myself. I couldn't take it. 23 hours a day with a cellie, both of us stuck there all the time. Now I'm here and mental health does watch out for me. They put me on medication. I'm by myself. But I never leave my cell, I won't go out even for rec. And I'll be going home right from here in two years. That worries me.[143]
In 2003, Human Rights Watch also documented the deleterious effects of supermax confinement upon prisoners suffering from mental illness.[144] The report found that prisoners suffering from mental health problems are often disciplined for behavior resulting from their illness. Placing these prisoners in solitary confinement exacerbates their illness and leads to deterioration of their condition. In many states, access to mental health treatment is limited, inadequate, or denied altogether once prisoners enter disciplinary confinement.
In New York State, mental health and prisoners' rights advocates brought a class-action lawsuit challenging the New York State practice of confining seriously mentally ill prisoners in Special Housing Units, seeking reform of policies that discipline inmates for behavior symptomatic of their illness as well as prolonged and repeated confinement that exacerbated their condition. As part of the settlement agreement reached in this lawsuit, the New York State Office of Mental Health now screens inmates entering SHU for severe mental illness in order to divert them from the Special Housing Units.[145] In March 2008 the New York State legislature passed a law requiring that seriously mentally ill prisoners be removed from SHU and placed in designated treatment centers under the care of the State Office of Mental Health.[146]
These reforms highlight the need for similar screening for drug dependence to ensure that prisoners are treated, rather than disciplined, for behavior resulting from the clinical condition of addiction.
Punishment of Drug Dependent People
The New York State prison system imposes disciplinary punishment on prisoners for use or possession of drugs even if they are drug dependent. Thus, it punishes some prisoners for behavior that is related to a clinical condition and over which they have no control. Often, these prisoners have not been receiving any treatment for their drug dependence, even though the prison system has identified their need for treatment services. Under the right to health, New York State should offer these prisoners treatment rather than punishment.
Human Rights Watch interviewed numerous prisoners who said that upon entry into the prison system they were assessed as needing substance abuse treatment. Yet when they were found to be in possession of illicit drugs, or a urine test showed they had used illicit drugs, prison authorities failed to take their dependence into consideration, handing them the same sanctions as other prisoners received.
For example, Peter G., a prisoner at Southport Correctional Facility, told Human Rights Watch:
I've had 15, 16 drug tickets. No assaults or anything like that. I've never been in a treatment program. Guys get frustrated, waiting years on the list for ASAT. Forget getting into RSAT. There's a lot of drugs out there and the pressure builds up. Now I'm in the box until 2012. In 17 years in prison, I've spent a total of 14 years in SHU, lost 186 months of good time. I'm a drug addict. If you know I'm a drug addict, why are you putting me in a box?[147]
Karen Murtagh-Monks, Executive Director of Prisoners' Legal Services of New York (PLS), recently told legislators in Albany about one of her organization's cases:
In one PLS case, we represented an inmate on a drug use charge. He was given 24 months in solitary confinement and received a recommendation of 30 months loss of good time. After we filed an administrative appeal in this case, pointing out that our client had a drug addiction and that placement in a drug program was more appropriate than placement in solitary confinement, the sentence was modified to 12 months in solitary confinement and 24 months recommended loss of good time, but still no drug treatment.[148]
The New York State prison system should screen prisoners who commit drug offenses for drug dependence and assign those who are in need of drug treatment to treatment programs rather than punishment.
The Case of David A: In SHU Until 2012
In February 2008 David A. committed his second drug offense in prison. David was found guilty of heroin possession and refusing to submit to a urine test. Though he was not charged with intent to distribute, David's previous drug offense and the amount of heroin found were cited as "aggravating factors" to justify a sentence of 40 months in SHU and loss of 4 years of good time. While serving this sentence in SHU David was again found guilty of drug possession, this time a small amount of marijuana. For this offense David was sentenced to 2 years in SHU, to begin after his current SHU sentence is complete. Thus it will be 2012 before David is released from disciplinary confinement for drug-related offenses.
HRW obtained a copy of the audiotape of David's disciplinary hearing held in June 2008 at the Upstate Correctional Facility. Excerpts from the audiotape are presented below:
The hearing officer reviews the charge of drug use and asks if David has any statement to make in his defense.
David: "There is no defense. I have an addiction and I keep getting keeplock for it. That's it."
The hearing officer sentences David to 24 months of SHU time to be served after completion of his present sentence.
Hearing officer: "This disposition is intended to impress upon inmate A. that drug use is a serious violation and cannot be tolerated. Do you understand the disposition?"
David: "What I don't understand is why I keep being punished for the drug offense instead of being treated for my drug addiction."
The hearing officer: "Your statement has been recognized on the tape. However, I as a Hearing Officer have no control over that and I suggest that you write to someone."
David is now sentenced to SHU until February, 2012.
To listen to the audiotape of David's disciplinary hearing, see www.hrw.org
Discontinuation and Denial of Drug Treatment for Disciplinary Offenses
Prisoners who are in substance abuse treatment programs when they are found to be in possession of, or to have used, drugs receive not just disciplinary punishment but are also removed from regular treatment. Upon release from disciplinary confinement their names fall to the bottom of the waiting list for admission to drug treatment. As a result of this practice, DOCS substance abuse programs often remove more prisoners than successfully complete them.[149]
This approach makes no sense from a public health perspective and violates the right to health. Drug dependence is a chronic condition and relapses are common in the recovery process. Thus, the New York State prison system terminates people's treatment for behavior that is part of the normal recovery process. This policy undermines efforts to treat prisoners for drug dependence and results in people being released into the community with an addiction that might have been successfully treated. This approach also undermines the effectiveness of New York State's substantial efforts in recent years to improve prison re-entry support programs. [150]
Alfredo F., a prisoner at Attica Correctional Facility, told Human Rights Watch: "I've had six dirty urines. On this last one...they gave me two years in the box and 1 year lost good time… I was in ASAT [treatment program] but they kicked me out for this last ticket."[151]
Special Housing Units themselves do not offer any treatment programs. The only substance abuse related programming available is the so-called "workbook" program, which the Department of Correctional Services considers a "pre-treatment program."[152] Prisoners told Human Rights Watch that the workbook program consists of a manual that is dropped off by a counselor once a week, filled out by the prisoner, and picked up a week later for review by the counselor. They said that counselors in some facilities "might" stay for a few minutes to talk with them about it.Nathan T. told Human Rights Watch:
I did the workbook but it wasn't much good- they just talk to you for a few minutes through the door. Then I got a dirty urine and they stopped it anyway. After my next dirty urine in the box I just said never mind, because I am in bad shape now. I will use whatever I can get my hands on in here- pot, heroin, whatever. I'm in a bad way.[153]
Adam J. who was recently released after serving 25 years in the New York State prison system said:
Guys went into the box like a revolving door. They were addicts- they needed help. But unless they were "short to the board" (their parole date was pending) they couldn't get into the programs. And once in the box, they've got no treatment.[154]
James W., prisoner at Attica Correctional Facility, stated, "They should treat us instead of sending us over and over to the box. There's plenty of room for me in the box, but not in a program." [155]
Numerous prisoners told Human Rights Watch that they had entered prison with drug addiction and were worried that they would leave with it as well because the lack of availability of drug treatment and the disciplinary system made it impossible for them to recover. For example, Lawrence Y., a prisoner at Southport Correction Facility, told us that he will "max out" his sentence in SHU for drug use, so had taken the initiative to write to a treatment program in his hometown, begging them to accept him. "I'm trying to get some help," he said. [156]
Ron L., prisoner at Great Meadow Correctional Facility, wondered how he could be expected to stay clean after his release if he did not receive treatment in prison. He said: "It's got to start in here. They can't just throw you out on the street and expect you not to do drugs out there."[157] Denial of treatment makes little sense from a security standpoint, as leaving drug dependent inmates untreated is likely to increase demand for drugs and drug-seeking behavior inside the prison.
Use of Urinalysis Testing
In its efforts to combat drug use in prisons, New York State uses an aggressive mandatory urine testing regimen for prisoners-in 2006, it conducted 79,101 urinalysis tests[158]-despite a recommendation by the World Health Organization, UNAIDS and the United Nations Office of Drugs and Crime (UNODC) to avoid mandatory and random drug testing because it is likely to increase unsafe injection practices and thus the risk of HIV and hepatitis C transmission.[159]
Prisoners who refuse to submit to urinalysis testing are subject to disciplinary charges as if they had tested positive for drugs.[160] Even during substance abuse programs, urinalysis results are not used therapeutically-to support or modify treatment regimens-as recommended by the National Institute on Drug Abuse.[161] With the exception of some prisoners participating in work release programs who are given a second chance, most prisoners testing positive for drug use are subject to automatic removal from substance abuse programs.
According to the WHO, UNAIDS, and UNODC, the evidence indicates that prisoners are more likely to use injectable drugs such as heroin and cocaine when they may be subjected to mandatory drug tests because smoked cannabis is detectable for up to one month by most urinalysis testing methods while heroin leaves the body within one to two days. Thus, by using heroin prisoners can better avoid the negative consequences of a positive urinalysis.[162]
Needles are scarce in prison, and prisoners injecting drugs are likely to share. [163]
Punitive urinalysis testing for drugs can thus undermine efforts to prevent the transmission of HIV and hepatitis C among prison populations. One former prisoner, Barry, who was released in 2007 after 37 years in New York state prisons, illustrated this in his testimony:
Heroin is definitely the drug of choice, because it leaves your body faster so you're less likely to get a dirty urine….It's hard to get the works, so guys mostly snort it. But once in while guys can get a needle from medical or something, and they're easy to sell.[164]
Other prisoners also told Human Rights Watch that heroin was "the drug of choice."[165]
The movement of some prisoners to use of injection drugs is troublesome from a public health perspective. At the same time, the evidence that mandatory drug testing in prison reduces drug use is limited. While such programs may contribute to a reduction in use of cannabis, they appear to have little effect on the use of opiates. [166] While prison systems may employ means to ensure that prisoners do not violate regulations, New York State's urinalysis testing unnecessarily exposes prisoners to health risks. New York State prison policy particularly undermines the right to health by using urinalysis test results to remove drug users from treatment and place them in disciplinary segregation where treatment is unavailable.
Conclusion
New York State's policy decisions relating to substance abuse in prison are inconsistent with its domestic and international obligations to prevent cruel, inhuman and degrading treatment and protect the right to health.
New York State prison officials have identified 3 of 4 prisoners as needing substance abuse treatment. Yet many of these prisoners face lengthy delays, language barriers and other obstacles to necessary drug dependence treatment. Most New York State prisoners dependent on heroin and other opioids have no access to Medication-Assisted Therapy, proven to be the most effective treatment for opioid dependence. Despite the high prevalence of HIV and hepatitis C among the prison population, New York State prisons continue to resist implementing evidence-based harm reduction measures proven effective in reducing disease transmission and overdose in prisons around the world.
At the same time, prisoners who use drugs are punished with disproportionate severity, facing months, even years, locked down in harsh conditions. Drug dependence treatment is not available to prisoners charged with drug use or possession, thus denying necessary health services to those who may need it the most.
Without delay, New York State prisons must increase access to evidence-based drug dependence and harm reduction programs, including Medication-Assisted Therapy and overdose prevention for prisoners dependent on heroin and other opioids. Disciplinary procedures for drug use must be proportional to the offense and disciplinary sanctions should never prevent prisoners from accessing drug dependence treatment and other necessary health services.
Acknowledgments
This report was researched and written by Megan McLemore, Researcher in the Health and Human Rights division of Human Rights Watch. Joseph Amon, director of the Health and Human Rights division, Rebecca Schleifer, Advocate in the Health and Human Rights division, and Diederik Lohman, Senior Researcher in the Health and Human Rights division made significant contributions during the editing process. The report was reviewed by David Fathi, director of the US Program, Jamie Fellner, Special Counsel to the US Program, Aisling Reidy, Senior Legal Advisor, and Iain Levine, Program Director at Human Rights Watch. Support was provided by intern Emily Dauria. Production assistance was provided by Mignon Lamia, Grace Choi and Fitzroy Hepkins.
The author would like to extend special thanks to Karen Murtagh-Monks of Prisoners' Legal Services of New York, Ed Wasserman, Jack Beck of the Correctional Association of New York, Karima Amin of Prisoners are People Too, Sharon Stancliff of the Harm Reduction Coalition, Holly Catania of the International Center for Advanced Addiction Treatment, Patricia Warth of the Center for Community Alternatives, The Fortune Society, and Bruce Trigg of the New Mexico Department of Health, each of whom provided invaluable assistance and support.
Most of all, many thanks to the current and former prisoners who were courageous enough to share their experiences for this report.
[1] Nathan T. is a pseudonym used to protect confidentiality and safety.
[2] Testimony of Brian Fischer, Commissioner of the Department of Correctional Services, before Joint Legislative Fiscal Committees, January 27, 2009, http://www.docs.state.ny.us/commissioner/testimony/09budget/html (accessed February 19, 2009). In January 2008, 24 percent of male and 33 percent of female prisoners were incarcerated for drug-related offenses. Department of Correctional Services (DOCS), "Hub System: Profile of Inmate Population Under Custody on January 1, 2008," http://www.docs.ny.st.us/research/reports/2008/Hub_report_2008.pdf (accessed February 19, 2009). These and other statistical reports relating to the New York State Department of Correctional Services may be found at http://www.docs.state.ny.us/research/research.html (accessed February 19, 2009). In the US, the national average of prisoners incarcerated for drug-related crimes is 20 percent. See US Department of Justice, Bureau of Justice Statistics Prison Statistics, http://www.ojp.usdoj.gov/bjs/prisons.htm (accessed September 29, 2008).
[3]DOCSHub System Profile; "New York State Assembly Committee on Codes, Joint Public Hearing re: the Rockefeller Drug Laws," April 2008, p. 1.
[4] See, e.g. US Department of Justice, Bureau of Justice Statistics, Drug Use and Dependence, State and Federal Prisoners, 2004, p.1.
[5]Department of Correctional Services, "Identified Substance Abusers," 2007, indicates that 83 percent of prisoners need substance abuse services; Department of Correctional Services, "Targeted Programs: An Analysis of the Impact of Prison Program Participation on Community Success," 2007, indicates that 85 percent of prisoners need substance abuse programming. DOCS determines that scores above 5 on the Michigan Alcohol Screening Test (MAST) and above 4 on the Simple Screening Instrument (SSI) are indicative of alcohol and drug "abuse" that necessitates treatment services.
[6] DOCS, "Identified Substance Abusers," p.2- 5.
[7] US Bureau of Justice Statistics, "HIV/AIDS Cases Among State and Federal Inmates," September 2007; according to National Minority AIDS Council, "African-Americans, Health Disparities and HIV/AIDS: 2006 Report," p. 8, 51 of every 10,000 inmates is HIV positive, compared to 15 of every 100,000 non-incarcerated persons.
[8] Wang, et al., "HIV Prevalence Trends by HIV Testing History, Injection Drug Use and Sexual Risk Behaviors among Inmates Entering New York State Correctional Facilities from 1988 to 2005," 2008 (abstract presented at the 15th Conference on Retroviruses and Opportunistic Infections ); Smith, L.., "HIV and AIDS Epidemiology in New York State: Trends in Incarcerated Persons," New York State Department of Health, 2007 (powerpoint on file with Human Rights Watch.)
[9] Wang, et al., "HIV Prevalence Trends."
[10] A 2005 study showed that 40 percent of inmates testing positive for HIV were co-infected with hepatitis C.. Wang, et. al., "HIV Prevalence Trends."
[11] New York Penal Law, Controlled Substance Offenses, Art. 220; New York Penal Law Sec. 70.00, Sentence of Imprisonment for Felony. Human Rights Watch has documented the severe impact of the Rockefeller Drug Laws on drug users, their families and their communities. See Human Rights Watch, US – Cruel and Usual: Disproportionate Sentences for New York Drug Offenders, vol. 9, no. 2(B), March 1997, http://www.hrw.org/legacy/reports/1997/usny/; Human Rights Watch, Collateral Casualties: Children of Incarcerated Drug Offenders in New York, vol. 13, no. 3(G), June 2002, http://www.hrw.org/legacy/reports/2002/usany/. For a recent examination of the disproportionate incarceration of minority communities under the Rockefeller and similar US drug laws, see Human Rights Watch, Targeting Blacks: Drug Law Enforcement and Race in the United States, May 2008, http://hrw.org/reports/2008/us0508/index.htm.
[12] The Drug Law Reform Acts of 2004 and 2005 modified the sentence structure by giving some individuals in prison for Class A-I and A-II felonies the opportunity to seek reduction in their sentences. Mandatory minimum sentences and limited judicial discretion however, continue to limit implementation of alternatives to incarceration for drug users. See Testimony of the New York City Bar Association on the Rockefeller Drug Laws before the New York State Assembly Committees on Codes, Judiciary, Correction, et.al., May 8, 2008; Testimony of the Legal Aid Society of New York on the Rockefeller Drug Laws before the New York State Assembly Committees on Codes, Judiciary, and Correction, et.al., May 8, 2008. The New York State Commission on Sentencing Reform recently endorsed additional modifications of the drug laws. See New York State Commission on Sentencing Reform, "The Future of Sentencing in New York State: Recommendations for Reform," January 30, 2009.
[13] C. Weinbaum et al., "Hepatitis B, hepatitis C, and HIV in Correctional Populations: a Review of Epidemiology and Prevention," AIDS, vol. 19(3), October 2005, p. 41; US Centers for Disease Control, MMWR, "Prevention and Control of Infections with hepatitis Viruses in Correctional Settings," January 2003; UNODC, HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings: A Framework for Effective National Response,2006.
[14] Centers for Disease Control, "HIV/AIDS in the United States," http://www.cdc.gov/hiv/topics/surveillance/united_states.htm (accessed December 8, 2008).
[15] Centers for Disease Control and Prevention, "Surveillance for Acute Viral Hepatitis, United States, 2006," Surveillance Summaries, MMWR, vol. 57, 2008.
[16] Wang, et al., "HIV Prevalence Trends."
[17] See for example, R. Jurgens and G. Betteridge, "Prisoners who inject drugs," Health and Human Rights: vol. 8 (2005); R. Douglas Bruce and Rebecca A. Schleifer, "Ethical and human rights imperatives to ensure medication-assisted treatment for opioid dependence in prisons and pre-trial detention," The International Journal of Drug Policy (2008), vol. 19, no. 1, p. 19 (citing studies).
[18] WHO/UNODC/UNAIDS, Evidence for Action Technical Papers, "Interventions to Address HIV in Prisons: Needle and Syringe Programmes and Decontamination Strategies," 2007, p. 5.
[19] Human Rights Watch interview with Susan R. at Rikers Island Correctional Facility, Rikers Island, New York, July 11, 2008.
[20] WHO, "Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention," (Position Paper Geneva 2004), p.13. See also, e.g., NIDA, "Principles of Drug Abuse Treatment," principle 12; National Association of State Alcohol and Drug Abuse Directors (NASADAD) Issue Brief, "Methadone Maintenance and the Criminal Justice System," April 2006; New York State Office of Alcohol and Substance Abuse Treatment Services, "Managing Addiction as a Chronic Disease," Addiction Medicine Educational Series, 2008, http://www.oasas.state.ny.us/AdMed/edseries.cfm (accessed January 12, 2009).
[21] WHO/UNAIDS/UNODC, "Substitution maintenance therapy," p. 13.
[22]United Nations Office on Drugs and Crime (UNODC)., HIV/AIDS prevention, care, treatment and support in prison settings. A framework for an effective national response, (Vienna 2006), p. 26.
[23] K. Fiscella, et al., "Management of opiate detoxification in jails,"Journal of Addictive Diseases, 24, 61–71 (2005).
[24] USHHSA, SAMSHA, "Detoxification and Substance Abuse Treatment," Treatment Improvement Protocol (TIP) 45 (2006). See also, K. Fiscella, et al., "Alcohol and Opiate Withdrawal in US jails," American Journal of Public Health 94:9, 1522-24 (2004).
[25] R. Jurgens, et.al., "Interventions to reduce HIV transmission related to injecting drug use in prison", Lancet Infectious Diseases, 9: 57-66 (2009).
[26] R. Chandler, et al., "Treating Drug Abuse and Addiction in the Criminal Justice System: Improving Public Health and Safety," JAMA, 2009: 301(2): 183-190.
[27] E. Warren and R. Viney, "An Economic Evaluation of the Prison Methadone Program in New South Wales," Centre for Health Economics Research and Evaluation, January 2004.
[28] For a description of countries with prison methadone programs, see International Harm Reduction Association, "Global State of Harm Reduction 2008: Mapping the Response to Drug-Related HIV and Hepatitis C Epidemics," August 2008; and R. Jurgens, "HIV/AIDS in prisons: a select annotated bibliography," Health Canada website, November 2005, http://www.hc-sc.gc.ca/ahc-asc/pubs/int-aids-sida/hiv-vih-aids-sida-prison-carceral-eng.php (accessed January 22, 2009). For an overview and updated information about medication-assisted therapy programs in correctional settings in the US, see "Medication-Assisted Therapy Law Enforcement Bulletin, a project of the US Substance Abuse and Mental Health Services Administration (SAMHSA)," http://csat.samhsa.gov/publications/law.aspx#info (accessed January 15, 2009).
[29] Human Rights Watch interview with John Bezirganian, M.D., Medical Director of the Tompkins County Mental Health Center and Medical Officer for the Tompkins County Jail, Ithaca, New York, May 28, 2008. For a description of the methadone and buprenorphine programs in the Rhode Island correctional system, see "Heroin in the Corrections System," a special issue of Medicine and Health Rhode Island, vol.90(5),May 2007. For information relating to the Connecticut buprenorphine in prison program, see "Enhancing Linkages to HIV Primary Care and Services in Jail Settings Initiative," Yale University AIDS Program, 2007, http://hab.hrsa.gov/special/bup_index.htm (accessed January 16, 2009).
[30] While Human Rights Watch is aware that there is some debate among experts about how to characterize drug dependence, we follow the American Medical Association (AMA) and the US National Institute on Drug Abuse in using the term "disease." See American Medical Association, "Science of Addiction," Fact sheet, http://www.ama-assn.org/ama/pub/category/3337.html (accessed Januray 15, 2009).
[31] Drug use in prison is a reality worldwide. For an overview of rates of injection drug use in prisons around the world, see World Health Organization, Evidence for Action: Effectiveness of Interventions to Address HIV in Prisons , 2007; New South Wales Department of Corrective Services, "Addressing the Use of Drugs in Prison: Prevalence, Nature and Context," June 2003, details rates of cannabis, amphetamine and opiate use in Australian prisons; T. Feucht and A. Keyser, "Reducing Drug Use in Prisons: Pennsylvania's Approach," National Institute of Justice Journal, October 1999, details rates of cannabis, amphetamine and opiate use in Pennsylvania state prisons.
[32] 9 NY Code of Rules and Regulations (NYCRR), 7651.1.
[33] International Covenant on Economic, Social and Cultural Rights (ICESCR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 UN GAOR (no. 16) at 49, UN Doc. A/ 6316 (1966), 99 UNTS 3, art. 11, entered into force January 3, 1976, signed by the US on October 5, 1977. As the US has not ratified the ICESCR it is not legally binding in total on the US, however as a signatory the US does undertake a number of legal obligations including, at a minimum, to take no action that would undermine the intent and purpose of the treaty. Vienna Convention on the Law of Treaties, adopted May 23, 1969, entered into force January 27, 1980, article 18.
[34] UN Committee on Economic, Social and Cultural Rights, "Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights," General Comment No. 14, The Right to the Highest Attainable Standard of Health, E/C.12/2000/4 (2000), http://www.unhchr.ch/tbs/doc.nsf/(Symbol)/40d009901358b0e2c1256915005090be?Opendocument (accessed May 11, 2006). The Committee on Economic, Social and Cultural Rights is the UN body responsible for monitoring compliance with the ICESCR.
[35] For a detailed discussion of drug dependence treatment as a key component of the right to health, see Canadian HIV/AIDS Legal Network, "Dependent on Rights: Assessing Treatment of Drug Dependence from a Human Rights Perspective," July 2007. For a comprehensive analysis of the interpretation of the elements of availability, accessibility, acceptability and good quality in relation to drug dependence treatment and the right to health, see Human Rights Watch, Rehabilitation Required: Russia's Human Rights Obligation to Provide Evidence-Based Drug Dependence Treatment, vol. 19, no. 7(D), November 2007, www.hrw.org/en/node/10608/section/2.
[36] International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 UN GAOR Supp. (No. 16) at 52, UN Doc. A/6316 (1966), 999 UN T.S. 171, entered into force March 23, 1976, ratified by the US on June 8, 1992, arts. 6, 7, 10(1).
[37]Pinto v. Trinidad and Tobago (Communication No. 232/1987) Report of the Human Rights Committee, vol. 2, UN Doc A/45/40, p. 69.
[38] Convention Against Torture and Other Cruel Inhuman or Degrading Treatment or Punishment (CAT), adopted December 10, 1984, G.A. Res. 39/46, annex, 39 UN GAOR Supp. (no. 51) at 197,UN Doc. A/39/51 (1984) entered into force June 26, 1987, ratified by the US on October 14, 1994, article 16(1).
[39] United Nations Committee against Torture (CAT), "Concluding Observations: New Zealand," (1998) UN Doc. A/53/44, para. 175.
[40] United Nations Economic and Social Council (ECOSOC), "Single Convention on Narcotic Drugs of 1961, as amended by the 1972 Protocol amending the Single Convention on Narcotic Drugs, 1961," art. 38, http://www.incb.org/incb/convention_1961.html (accessed February 2, 2009); ECOSOC, "Convention on Psychotropic Substances of 1971," art. 20, http://www.incb.org/incb/convention_1971.html (accessed February 2, 2009); ECOSOC, "Convention against Illicit Traffic in Narcotic Drugs and Psychotropic Substances of 1988," art. 3, http://www.incb.org/incb/convention_1988.html (accessed February 2, 2009).
[41] Report of the Special Rapporteur on torture and other cruel, inhuman or degrading treatment or punishment, "Promotion and Protection of all Human Rights, Civil, Political, Economic, Social and Cultural Rights, Including the Right to Development," A/HRC/10/44, January 14, 2009, p. 18.
[42] Ibid, p. 23.
[43]Estelle v Gamble, 429 US 97 (1976).
[44]Gregg v. Georgia, 428 US 153, 173 (1976).
[45]Kelley v. County of Wayne, 325 F.Supp.2d 788 (E.D. Mich. 2004).
[46] Cases denying a right to methadone treatment include: Fredericks v. Huggins, 711 F.2d 31 (4th Cir. 1983) and Inmates of Allegheny Jail v. Pierce, 612 F. 2d 754 (3d Cir, 1979). A claim for the right to continue methadone treatment was upheld in Cudnik v. Krieger, 392 F.Supp. 305 (N.D. Oh. 1974).
[47] American Psychiatric Association, Diagnostic and Statistical Manual-IV, 4th ed., text Revision 2000.
[48] 20 Code of Federal Regulations (CFR) 404, Subpart P, App. 1, 12.09.
[49] SeeReg'l Econ. Cmty. Action Program, Inc. v. City of Middletown, 294 F.3d 35, 46-47 (2d Cir. 2002); Altman v. New York City Health and Hosp. Co., 903 F. Supp. 503, 508 (S.D.N.Y. 1995).
[50] R. Boucher, "The Case for Methadone Maintenance Treatment in Prisons," Vermont Law Review, vol. 27, 2003, p. 453, 482 .
[51] New York State Office of Alcoholism and Substance Abuse Services (OASAS), "Statewide Comprehensive Plan 2008-2012," October 1, 2008, http://www.oasas.state.ny.us/pio/documents/5YPlan2008-2012.pdf (accessed January 16, 2009); Substance Abuse and Mental Health Services Administration (SAMSHA), "Buprenorphine Locator," http://buprenorphine.samhsa.gov/pls/bwns_locator/!provider_search.process_query?alternative=CHOICEG&one_state=NY (accessed January 15, 2009).
[52] J. Mellow, et al., "Mapping the Innovation in Correctional Health Care Service Delivery in New York City," John Jay College of Criminal Justice Spring, 2008, http://www.jjay.cuny.edu/centersinstitutes/pri/pdfs/NYCMappingHeathCare.pdf (accessed January 15, 2009).
[53] See SAMSHA, "Detoxification and Substance Abuse Treatment," Treatment Improvement Protocol (TIP) 45, 2006.
[54] J. Mellow, "Mapping the Innovation," 2008; V. Tomasino, et al., "The Key Extended Entry Program (KEEP)," Mount Sinai Journal of Medicine, vol. 68(1), January 2001, pp. 14-20. .
[55] Human Rights Watch interview with John Bezirganian, M.D., Medical Director of the Tompkins County Mental Health Center and Medical Officer for the Tompkins County Jail, Ithaca, New York, May 28, 2008.
[56] NYS Commission on Correction, "Chairman's Memorandum," No 9-2006, November 10, 2006.
[57] DOCS, "Substance Abuse Treatment Services," description of Clean Start Program, http://www.docs.state.ny.us/ProgramServices/substanceabuse.html#clean (accessed February 2, 2009).
[58] Human Rights Watch interview with Susan R., Rikers Island Correctional Facility, New York City, July 11, 2008.
[59] Ibid.
[60] National Institute on Drug Abuse (NIDA), "An Examination of Drug Treatment Programs Needed to Ensure Successful Re-Entry," a statement to the House Subcommittee on Crime, Terrorism and Homeland Security, February 8, 2006, http://www.drugabuse.gov/testimony/2-08-06testimony/html (accessed September 29, 2008).
[61] National Association of State Alcohol/Drug Abuse Directors (NASADAD) Issue Brief, "Methadone Maintenance and the Criminal Justice System," p. 4.
[62] National Commission on Corrective Healthcare (NCCHC),"NCCHC Accreditation Paves the Way for Opioid Treatment Programs," http://www.ncchc.org/accred/otp.html (accessed September 29, 2008).
[63] Human Rights Watch interview with Superintendent Melvin Williams, Romulus, New York, March 18, 2008.
[64] Human Rights Watch interview with Dr. B. Castro, Bernalillo Metropolitan Detention Center, Albuquerque, New Mexico, July 15, 2008.
[65] Human Rights Watch interview with prisoner at Bernalillo Metropolitan Detention Center, Albuquerque, New Mexico, July 15, 2008.
[66] Human Rights Watch interviews with Matt Elwell, Deputy Chief of Bernalillo Metropolitan Detention Center, and Dr. Steve Vaughan, Medical Director, New Mexico Department of Correctional Services, Albuquerque, New Mexico, July 16, 2008.
[67] Death from drug overdose is the second leading cause of accidental death in the United States. See Harm Reduction Coalition, "Overdose," http://www.harmreduction.org/article.php?list=type&type=51 (accessed Januray 16, 2009). Death from drug overdose is a serious problem in New York State, with more than 900 deaths in New York City alone in 2006. 70 percent of these deaths were from heroin overdose. New York State Department of Health, "Opioid Overdose Prevention", http://www.health.state.ny.us/diseases/aids/harm_reduction/opioidprevention/ (accessed January 16, 2009).
[68] Studies in jurisdictions in the US and elsewhere have found that former prisoners were at high risk of overdose death, particularly within the first two weeks after release. See, e.g., I. Binswanger, et al., "Release from Prison-A High Risk of Death for Former Inmates," New England Journal of Medicine , vol. 356(52), 2007, p. 157.
[69] DOCS, "Prison Safety in New York," April 2006.
[70] New York State Commission on Corrections, Reports of Deaths in Custody, obtained by Human Rights Watch through Freedom of Information Law requests and on file with Human Rights Watch. It is unclear whether the 27 deaths cited in the DOCS report include the 13 deaths cited by the Commission on Corrections.
[71] J. Farrell, "Overdose Prevention HIV/HCV Transmission Education in New York City Jails," IHRA powerpoint presentation, 2008, http://www.ihra.net/Assets/228/1/2008_Tuesday_Concurrent_ODPrevention_Farrell.pdf (accessed January 22, 2009); Human Rights Watch telephone interview with Bruce Trigg, M.D., New Mexico Department of Health, January 16, 2009.
[72] DOCS, "Alcohol and Substance Abuse Treatment Program Operations Manual," 2002; DOCS, "Alcohol and Substance Abuse Relapse Treatment Workbook"; DOCS, "Counselor Manual for Returned Parole Violators," 2004; DOCS, "Willard Drug Treatment Program Policy and Procedures Manual," 2005.
[73] Human Rights Watch interview with O. Gadsden, Corrections Counselor/ASAT, Willard Drug Treatment Campus, Romulus, New York, March 18, 2008.
[74] Ibid.
[75] Human Rights Watch telephone interview with Karen McDaniel, Director of Training Services, Department of Correctional Services, March 3, 2009.
[76] Human Rights Watch interview with Malcolm A., Great Meadow Correctional Facility, Comstock, New York, May 2, 2008.
[77] For an overview of all DOCS substance abuse programming, see DOCS, "Substance Abuse Treatment Services2008," 2008.
[78] A. Simpler, et al., "Substance Use in Prison: How Much Occurs And Is It Associated with Psychopathology?" Addiction Research and Theory, vol. 13(5), 2005, pp. 503-11.
[79] DOCS, "Identified Substance Abusers," p.1.
[80] Testimony of the Correctional Association of New York before the Assembly Standing Committees on Codes, Alcoholism and Drug Abuse and Corrections, March 2, 2007.
[81] OASAS certifies the Edgecombe Correctional Facility, a 100-bed facility in Manhattan and the substance abuse treatment component (as distinguished from the "shock incarceration" component) of the Willard Drug Treatment Campus. OASAS also works with DOCS to support the use of OASAS-certified outpatient services for prisoners in work release and upon re-entry. See, NY OASAS, Five Year Comprehensive Plan for a Premier System of Addiction Services for Prevention, Treatment, Recovery, 2007 Annual Update, p. 16.
[82] See, e.g., F. Taxman, et al., "Drug Treatment Services for the Adult Offender: The State of the State," Journal of Substance Abuse Treatment, vol. 32, 2007.
[83] See, e.g., Mears, et.al., "Drug Treatment in the Criminal Justice System: The Current State of Knowledge," Urban Institute Justice Policy Center,2003; WHO/UNODC, "Principles of Drug Dependence Treatment," Discussion Paper, March 2008; National Institute on Drug Abuse, "Principles of Drug Abuse Treatment for Criminal Justice Populations," 2006.
[84] Chandler, "Treating Drug Abuse and Addiction in the Criminal Justice System," p. 185.
[85] F. Taxman, et al., "Drug treatment services for adult offenders: the state of the state," p. 241; R. Chandler, "Treating Drug Abuse and Addiction in the Criminal Justice System," p. 183; "TRIAD Drug Treatment Evaluation Project Final Report of Three Year Outcomes: Part 1," Federal Bureau of Prisons,2000. Prison methadone programs, particularly, show significant results in reducing recidivism. Chandler, p. 184; WHO/UNODC/UNAIDS, "Evidence for Action Technical Papers: Interventions to Address HIV in Prisons: Drug Dependence Treatments," 2007,p. 14.
[86] There are exceptions, for example, prisoners determined to have serious mental health needs who are placed on a special mental health caseload.
[87] Correctional Association testimony, p.2.
[88] Correctional Association Testimony, p. 2; Coalition for Criminal Justice Reform, "Blueprint for Criminal Justice Reform: Bringing Justice to Scale," February 2007, p. 18.
[89] Many prisoners on the CASAT waiting list are low-level drug offenders with court orders to participate in the program. DOCS, "The Comprehensive Alcohol and Substance Abuse Treatment Program," 2007.
[90] DOCS, "Participants in Residential Substance Abuse Program, January 5, 2008", on file with Human Rights Watch; Correctional Association Testimony, p. 2 ("Indeed, we have met many inmates who complain that they have been on a waiting list for substance abuse treatment for many years…").
[91] Human Rights Watch interview at Great Meadow Correctional Facility, Comstock, New York, May 2, 2008.
[92] Human Rights Watch interview at Southport Correctional Facility, Pine City, New York, September 5, 2008.
[93] Human Rights Watch interview at Attica Correctional Facility, Attica, New York, July 9, 2008.
[94] The ICCPR guarantees freedom to seek and receive information, and in the context of the right to health the UN Committee on Economic, Social and Cultural Rights has made clear that ensuring access to seek, receive and impart information and ideas concerning health issues is critical to ensuring the right to health. CESCR, General Comment No. 14: The right to the highest attainable standard of health, para. 12(b) and note (8).
[95] The ICCPR provides in Article 17 that everyone has the right to protection of the law against attacks or interference on their privacy, which includes physical integrity. See Manfred Nowak, UN Covenant on Civil and Political Rights: CCPR Commentary, (Kehl am Rein: N.P. Engel, 2nd ed., 2005), p. 386. In a series of jurisprudence, the European Court of Human Rights has repeatedly held that the same provision in the European Convention on Human Rights imposes positive obligations to ensure effective respect for private life, that includes provision of necessary information that relates to potential harm to the individual. European Court of Human Rights, Lόpez Ostra v. Spain, 1994, Application No. 16798/90, judgment of 9 December 1994, Series A, no. 303-C, and Guerra and others v. Italy, Application No. 14967/89, judgment of February 19, 1998, Reports 1998-I.
[96] DOCS, "The Impact of Foreign-Born Inmates on the New York State Department of Correctional Services," July 2008, p. 4.
[97]Ibid.
[98] Human Rights Watch interview at Attica Correctional Facility, Attica, New York, July 9, 2008.
[99] Human Rights Watch interview with Carlos R., Great Meadow Correctional Facility, May 2, 2008.
[100] DOCS, "HUB System: Profile of Inmates Under Custody on January 1, 2008."
[101] Human Rights Watch interview with Ron L. at Great Meadow Correctional Facility, Comstock, New York, May 1, 2008.
[102] See, e.g., CDC Morbidity and Mortality Weekly Report (MMWR), "HIV Transmission among Male Inmates in a State Prison System- Georgia 1992-2005", vol.55, no. MM15, April 21, 2006, p. 421. For a review of HBV, HCV and HIV transmission studies for both international and US prisons, see R. Jurgens, "HIV/AIDS and HCV in Prisons: A Select Annotated Bibliography," International Journal of Prisoner Health, vol. 2(2), June 2006, p. 131. For a review of the US literature in this area see T. Hammett, "HIV/AIDS and Other Infectious Diseases Among Correctional Inmates: Transmission, Burden and an Appropriate Response," American Journal of Public Health, vol. 96(6), June 2006, p. 974 and S. Okie, "Sex, Drugs, Prisons and HIV," New England Journal Of Medicine, vol. 356(2), January 2007.
[103] R. Jurgens and G. Betteridge, "Prisoners who inject drugs," Health and Human Rights, vol. 8(2), 2005, p. 52; Lines, et al., Prison Needle Exchange: Lessons Learned from a Comprehensive Review of International Evidence and Experience, 2nd ed., Canadian HIV/AIDS Legal Network, 2006.
[104] Human Rights Watch interview with Gary D., Upstate Correctional Facility, Malone, New York, July 2, 2008.
[105] Human Rights Watch interview with Robert F., Great Meadow Correctional Facility, Comstock, New York, May 6, 2008.
[106] Drug use in prison is a reality worldwide. See WHO, "Evidence for Action: Effectiveness of Interventions to Address HIV in Prisons," 2007, for an overview of rates of injection drug use in prisons around the world; New South Wales Department of Corrective Services, "Addressing the Use of Drugs in Prison: Prevalence, Nature and Context," June 2003, details rates of cannabis, amphetamine and opiate use in Australian prisons; T. Feucht and A. Keyser, "Reducing Drug Use in Prisons: Pennsylvania's Approach," National Institute of Justice Journal, October 1999, details rates of cannabis, amphetamine and opiate use in Pennsylvania state prisons.
[107] International Harm Reduction Association, "Global State of Harm Reduction 2008," August 2008; California Department of Corrections and Rehabilitation, "Prisoner Condom Access Pilot Program," December 2008.
[108] J. May and E. Williams, "Acceptability of Condom Availability in a US Jail," AIDS Education and Prevention, vol. 14, supp. B., 2002; L. Yap, et al., "Do Condoms Cause Rape and Mayhem? The Long-Term Effects of Condoms in New South Wales Prisons," Sexually Transmitted Infections (STI) Online, December 19, 2006, http://sti.bmj.com/cgi/content/abstract/sti.2006.022996v1 (accessed February 1, 2007); Correctional Services of Canada, "Evaluation of HIV/AIDS Harm Reduction Measures in the Correctional Service of Canada," April 1999.
[109] May and Williams, p. 85.
[110]CDCR "California Department of Corrections and Rehabilitation Prisoner Condom Access Pilot Program," December 2008, p. 1.
[111] R. Jurgens, et.al., "Interventions to reduce HIV transmission related to injecting drug use in prison," Lancet Infectious Diseases, vol. 9, 2009, pp. 57-66 ; International Harm Reduction Association, "Global State of Harm Reduction 2008," August 2008.
[112] For example, a worldwide survey indicated that in cities with needle exchange or distribution programs, the seroprevalence of HIV dropped by 5.8 percent per year, T. Kerr and R. Jurgens, Needle Exchange Programs in Prisons: Reviewing the Evidence, Canadian HIV/AIDS Legal Network, 2004, p.19.
[113] International Harm Reduction Association, "Global State of Harm Reduction 2008."
[114] Kerr and Jurgens, Needle Exchange Programs in Prisons: Reviewing the Evidence, p.14; WHO/UNODC/UNAIDS, "Interventions to Address HIV in Prisons: Needle and Syringe Programmes and Decontamination Strategies," Evidence for Action Technical Papers, 2007, p. 14.
[115] WHO/UNODC/UNAIDS, Interventions to Address HIV in Prisons: Needle and Syringe Progammes and Decontamination Strategies, p. 19.
[116] 9 NYCRR 7651.1.
[117] "Discipline and order shall be maintained with firmness, but with no more restriction than is necessary for safe custody and well-ordered community life," UN Standard Minimum Rules for the Treatment of Prisoners, rule 27.
[118] DOCS disciplinary charges for drug and alcohol use and possession are codified in 7 NYCRR 270.2, sub-sections 113.13 (use of alcohol or intoxicant), 113.24 (use of illicit drugs) and 113.25 (possession of drugs or alcohol.)
[119] 7 NYCRR 1020 ("Urinalysis Testing") provides that a urinalysis can be used a) when drugs or alcohol substance is found in the possession of an inmate, to substantiate a charge of substance use; b) when there is reason to believe than an inmate has used drugs or alcohol ; c) when an inmate is involved in an act of violent misconduct or d) as part of random urinalysis testing. The section further provides that non-compliance with urinalysis testing requirements shall result in disciplinary charges.
[120] 7 NYCRR 253,254.
[121] "Penalties for Drug or Alcohol Related Misbehavior" DOCS internal guidelines July 2005, on file with Human Rights Watch.
[122] Correctional Association of New York, "Lockdown New York: Disciplinary Confinement in New York State Prisons," October 2003, p. 2; Correctional Association Fact Sheet, "Disciplinary Confinement in New York State Prisons," March 2004.
[123] "New York State DOCS Daily Population Capacity Report 1/1/07," on file with Human Rights Watch.
[124] Correctional Association of New York, "Lockdown New York," p. 9. DOCS maintains that these prisons are not "supermax" units as they are used solely for disciplinary purposes rather than as general housing units. In New York, prisoners can also progress to less restrictive conditions of confinement in SHU by maintaining good behavior. DOCS, "Prison Safety in New York," April 2006, p. 16. Even the least restrictive conditions in SHU, however, are similar to those in prisons designated as "supermax."
[125] Human Rights Watch's Freedom of Information Law request for current SHU and keeplock population data is under appeal as of this writing.
[126] The American Correctional Association (Standard 4-4320) prohibits using food as a disciplinary measure. The Federal Bureau of Prisons has discontinued the use of restricted diets.
[127] Correctional Association of New York, "Lockdown New York," p. 18.
[128] Written Testimony of Prisoners' Legal Services at a Public Hearing on The Rockefeller Drug Laws, "35 Years Later," New York State Assembly Standing Committee on the Judiciary, May 15, 2008, p.11.
[129] UN Human Rights Committee, General Comment no. 20, Prohibition of torture or cruel, inhuman or degrading treatment or punishment, UN Doc. HRI/GEN/1/Rev.1 at 30, 1994, para. 6.
[130] Nigel S. Rodley, The Treatment of Prisoners Under International Law, (Oxford:Oxford University Press, 1999) 2nd ed., p. 295.
[131] United Nations, "Interim Report of the Special Rapporteur on Tortureand Other Cruel, Inhuman or Degrading Treatment or Punishment," UN Doc. A/63/175, July 2008, p.2.
[132] UN Standard Minimum Rules for the Treatment of Prisoners, rules 27-31.
[133]Human Rights Watch interview at Great Meadow Correctional Facility, Comstock, New York May 6, 2008.
[134] Human Rights Watch interview at Upstate Correctional Facility, Malone, New York, July 2, 2008.
[135] Written Testimony of Prisoners' Legal Services, p. 11.
[136] Documents obtained under the Freedom of Information Law and on file with Human Rights Watch. Disciplinary hearing officers make recommendations for reduction of good time; final calculations of good time are made by the Time Allowance Committee before release.
[137] Documents obtained under Freedom of Information Law and on file with Human Rights Watch.
During each of those years, an additional 662, 669 and 653 prisoners were sentenced to "keeplock" status in their cells solely for drug related rule infractions.
[138] Human Rights Watch interview at Southport Correctional Facility, Pine City, New York, September 5, 2008.
[139] Human Rights Watch, US-Out of Sight: Briefing Paper on Supermax Prisons, February 2000, http://www.hrw.org/legacy/reports/2000/supermax/;New York State officials maintain that "supermax" is an inappropriate term for these facilities due to their use primarily for disciplinary confinement as opposed to generalized housing for certain classes of prisoners, and the opportunity for prisoners to earn early release for good behavior. See DOCS, "Prison Safety in New York," April 2006. However, Human Rights Watch defines "supermax" in relation to the severity of conditions experienced by prisoners housed in these areas, as well as the length of sentences imposed.
[140] Human Rights Watch, Out of Sight, 2000.
[141] Correctional Association, "Lockdown New York," p. 2.
[142] Human Rights Watch interview, Upstate Correctional Facility, Malone, N.Y., July 2, 2008.
[143] Human Rights Watch interview, Southport Correctional Facility, Pine City, N.Y., September 5, 2008.
[144] Human Rights Watch, Ill-Equipped: U.S. Prisons and Offenders with Mental Illness, 2003, http://www.hrw.org/reports/2003/usa1003
[145]Disability Advocates, Inc., vs. New York State Office of Mental Health, et al., (02 Civ. 4002, Southern District of New York.)
[146] New York State Legislature, A-9342/S6422, signed into law January 28, 2008.
[147] Human Rights Watch interview at Southport Correctional Facility, Pine City, New York, September 5, 2008.
[148] Written Testimony of Prisoners' Legal Services, p. 11.
[149] For example, RSAT Program Project Reports from DOCS medium security facilities indicate that for 2005-2006, 69 percent of their RSAT participants were removed (4,869 out of 7,042.) Maximum security facilities removed 51 percent of their participants from RSAT during this period (5,872 out of 11,440).
[150] Current state-wide efforts include the Transition from Prison to Community Initiative (TPCI) and the Interagency Re-entry Task Force. See New York State Commission on Sentencing Reform, "The Future of Sentencing in New York State: Recommendations for Reform," January 30, 2009, Part 4.
[151] Human Rights Watch interview at Attica Correctional Facility, Attica, New York, July 9, 2008.
[152] The workbook program is not credited by DOCS toward any of its internal substance abuse programming requirements. DOCS, "Substance Abuse Treatment Services," 2008, p. 21, http://www.docs.state.ny.us/ProgramServices/substanceabuse.html (accessed September 29, 2008).
[153] Human Rights Watch interview, Upstate Correctional Facility, Malone, NY, July 2, 2008.
[154] Human Rights Watch interview in New York City, June 6, 2008.
[155] Human Rights Watch interview at Attica Correctional Facility, Attica, N.Y., July 9, 2008.
[156]Human Rights Watch interview at Southport Correctional Facility, Pine City, New York, September 5, 2008.
[157] Human Rights Watch interview at Great Meadow Correctional Facility, Comstock, New York May 2, 2008.
[158] DOCS, "Prison Safety in New York," April 2006.
[159] UNODC, HIV/AIDS Prevention, Care, Treatment and Support, p.18.
[160]Section 1020.4 (c) and (d) (2) (3) (4) of Title 7 NYCRR provide: (c) Ordering the inmate to be tested. The inmate ordered to submit a urine specimen for urinalysis testing shall be informed of the underlying reason (whether suspicious, routine, or random) why s/he is being ordered to submit the specimen. If the inmate refuses to submit the specimen s/he shall be informed that this refusal constitutes a violation of facility rules and that s/he may incur the same disciplinary disposition that a positive urinalysis result could have supported. The resultant misbehavior report shall indicate that the inmate was informed of the above.
[161] NIDA, Principles for Drug Abuse Treatment for Criminal Justice Populations: A Research-Based Guide, July 2006, Principle 6. There is debate as to whether urinalysis testing is necessary or more effective than self-reporting in detecting drug use during treatment. See Ward, J., Hall, W. and Mattick, R.P., "The Use of Urinalysis During Opioid Replacement Therapy," in Ward, et. al., eds., Methadone Maintenance Treatment and Other Opioid Replacement Therapies (Sydney: Harwood Academic Press, 1998).
[162]UNODC/WHO/UNAIDS, "HIV/AIDS Prevention, Care, Treatment and Support: A Framework for an Effective National Response," 2006, p.18; R. Lines, et. al., "Prison Needle Exchange," p. 30.
[163] R. Jurgens and G. Betteridge, "Prisoners who inject drugs," Health and Human Rights, vol 8, no. 2, 2005, p. 52.
[164] Human Rights Watch interview with Barry M., Buffalo, New York, May 23, 2008.
[165] For example, Human Rights Watch interview with Deborah A., Bedford Hills Correctional Facility, Bedford Hills, New York, September 4, 2008; Human Rights Watch interview with David A., Upstate Correctional Facility, Malone, New York, July 2, 2008.
[166]R. Jurgens, et al., "Interventions to reduce HIV transmission related to injecting drug use in prison," Lancet Infectious Diseases, vol. 9, 2009, p. 60; WHO/UNODC/UNAIDS, "Evidence for Action Technical Papers: Interventions to Address HIV in Prisons: Drug Dependence Treatments," 2007, p. 25. In addition, mandatory drug testing in prison has been found to have unintended consequences such as increased tension and violent incidents, and raises concerns about cost-effectiveness in light of the limited evidence that it reduces drug use, WHO/UNODC/UNAIDS, "Evidence for Action Technical Papers: Effectiveness of Interventions to Address HIV in Prisons," 2007, p. 115.