Summary
Two years ago my left hand got paralyzed from the tumor and I started to develop severe pain. It felt as though it was burning, as if my arm was on fire. It was hellish pain. . . . Now I have pain 24 hours a day, but at night it becomes unbearable, when pain gets even worse, and I just start screaming. Two months ago I was prescribed one ampoule of injectable omnopon [opioid pain medication]. It was then enough to sooth my pain for four hours, but now it helps only for maximum of two. I keep it for nights, so that I can sleep for those two hours. The pain attacks start unexpectedly and I start screaming and become a different person. … When it starts I [can’t speak], I have pain attacks every night.… It’s inhumane pain, unbearable pain for a human being….[1]
This is how Lyudmila, a 61-year-old retired kindergarten teacher in Armenia, described to Human Rights Watch the pain she had been enduring for about two years from her inoperable breast cancer. Her words were deeply personal. But her experience is not an exception. The World Health Organization (WHO) estimates that over 80 percent of people with advanced cancer worldwide develop moderate to severe pain at the end of life.
Cancer is on the rise in Armenia. Some 8,000 people die from it annually, and many of them do so in excruciating pain. But it does not have to be this way. Most of the pain endured by Lyudmila and others like her can be easily alleviated. Morphine, the mainstay medication for treating severe pain, is inexpensive and easy to administer, but widely inaccessible to people who need it in Armenia. Other palliative care services that help people ease pain and end-of-life suffering are also largely unavailable in Armenia.
Palliative care is a field of medicine that seeks not to cure disease but to prevent suffering and improve quality of life. It focuses on treating pain and other physical symptoms, and providing psychosocial support, complementing curative treatment. The two should be provided in parallel from the moment of diagnosis. Palliative care may even help curative treatment to succeed, for example, by enabling a patient to eat, exercise, communicate, or adhere to a medication regimen.
The lack of palliative care in Armenia condemns thousands of patients with life-limiting illnesses to chronic pain and great suffering. Most patients with advanced cancer in Armenia are simply sent home when curative treatment is no longer effective. Abandoned by the health care system at arguably the most vulnerable time of their lives, they face pain, fear, and anguish without professional support. This is particularly devastating given that over half of all cancer patients in Armenia are at a late stage of the disease when they receive their diagnosis, when curative treatment is ineffective and palliative care and pain management are the only services that may still benefit them.
In recent years, the government of Armenia has recognized the need for palliative care and taken important steps to develop it. But much remains to be done. This report documents these gaps: overly restrictive government regulations on accessing strong pain medication, ingrained practices among health care professionals that impede adequate pain relief, the lack of training and education of health care professionals on palliative care, and the overall absence of palliative services in Armenia. It focuses on the devastating impact of untreated pain and lack of support services for cancer patients and their families on the quality of their lives. It is based on dozens of interviews with patients, their families, health care professionals, government officials, and patients’ advocacy groups, and other nongovernmental organizations from 2012 to 2o14.
Medicines Availability
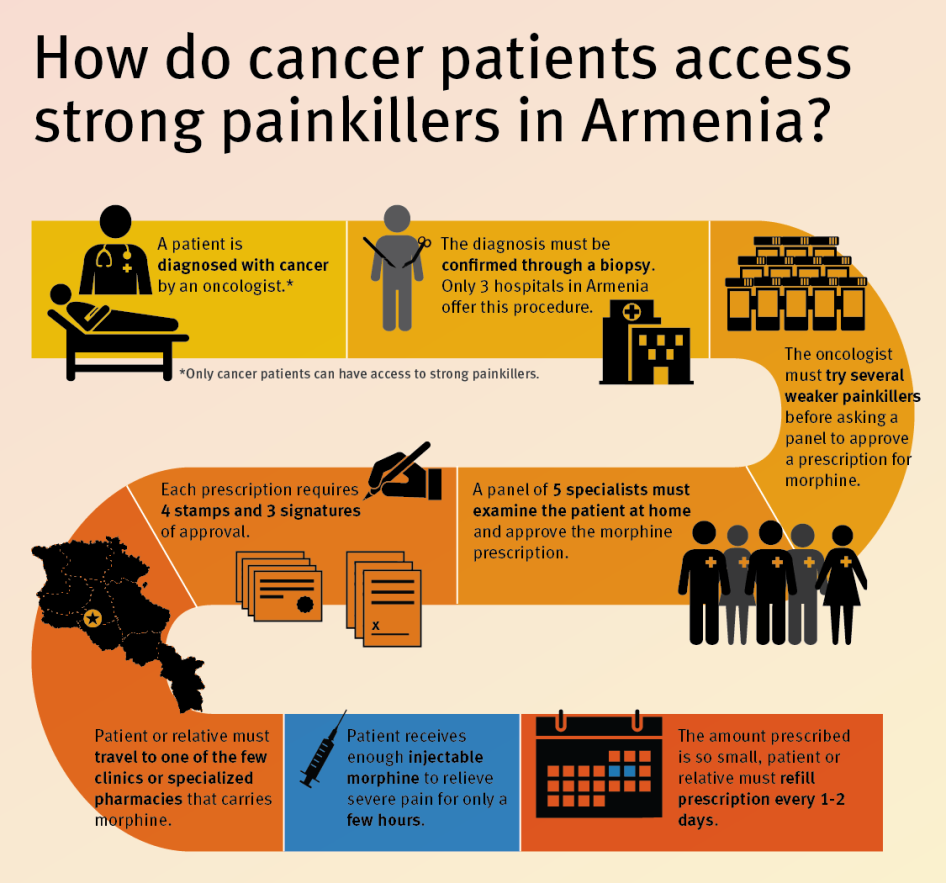
The key obstacle to effective pain treatment in Armenia remains an overly restrictive legislative basis governing the distribution of opioids for medical purposes. The country’s pain treatment practices deviate fundamentally from World Health Organization (WHO) standards on pain management. Oral morphine, the medicine of choice for the treatment of severe chronic pain, is unavailable in Armenia. Oncologists lack awareness, guidance, and training on the medicinal use of opioids and often perceive morphine as dangerous.
Under current government regulations, the procedure for prescribing injectable opioids is complex, time-consuming, and involves significant bureaucracy. Only oncologists may prescribe opioids to outpatients, and only to cancer patients. Oncologists can prescribe opioids only after multiple doctors have signed off on the decision; and even after that multiple signatures and seals are necessary for each prescription.
Another problem is inadequate dosage. Although Armenian regulations do not establish maximum dosages, the standard practice is to start a patient on a single opioids injection per day and then add a second daily injection after about two weeks. The analgesic effect of injectable morphine lasts up to four hours, leaving even patients like Lyudmila, who are fortunate enough to have been prescribed opioids, without adequate pain relief for most of the day. While doctors often supplement opioids with weaker pain medicines and other medications for the intervals, these are not potent enough to provide effective relief and expose patients to unnecessary side effects.
Once opioid analgesics are prescribed, cancer patients or their caregivers must go to the clinic to collect the prescription with its four different stamps, fill it at one specialized pharmacy in Yerevan or at large regional medical centers outside of the capital, and return the empty ampoules before a new prescription is issued. They must repeat the process every other day or in some cases every day because in practice doctors will prescribe only enough strong opioids to last 24 or 48 hours. This is enormously time-consuming and takes a severe toll on patients’ families, who are often already under severe emotional distress.
Police control over the prescription and dispensing process is tight, invasive, and generates a sense of trepidation among oncologists and pharmacists. All oncologists interviewed for this report said that they provide written monthly reports to the police about patients who receive opioid painkillers. In violation of patient confidentiality, such reports include the patient’s name, address, ID number, diagnosis, prescribed dosage and the name and other information of the person who picks up the prescription and fills it. Police also conduct regular, informal inspections at polyclinics, participate in destruction of full ampoules and sometimes also empty ampoules. While police and other law enforcement bodies have a legitimate interest in ensuring opioid analgesics do not enter black markets, the right to health protects against improper interference with appropriate medical practice. Under the right to privacy, law enforcement officials may not routinely require confidential medical information on patients who receive opioid analgesics from hospitals, clinics or pharmacies.
Training and Education
At Armenia’s medical schools medical and nursing students receive virtually no training on palliative care and adequate pain treatment. As a result, health workers lack skills in assessing and treating pain, and communicating appropriately with patients and their families about the patient’s illness. Oncologists often do not disclose a cancer diagnosis and often hide key medical information, leaving the patient to suffer without knowing the cause, unable to ask questions and find answers, deprived of the chance to put their affairs in order.
Since at least 2012 independent groups have been providing palliative care and pain management trainings for oncologists in Armenia, but it is neither systematic, nor mandatory. The mandatory curriculum in medical schools does not include any specific instruction on palliative care. Palliative care residency or fellowship programs that would lead to specialization in palliative care have not yet been implemented in Armenia’s medical schools.
Policy Reforms
The WHO has recommended that countries establish a national palliative care policy or program and that palliative care services be made available at the community level and in specialized hospitals for low- and middle-income countries. The Armenian government has clearly recognized the need for palliative care. In 2009, palliative care services were for the first time included in the government’s list of recognized medical services. In 2010, the government established a palliative care working group, consisting of relevant government agencies and expert civil society groups, which developed a concept paper and a national strategy for palliative care. In August 2012, the government approved the concept paper, which is largely a needs-assessment study on palliative care. In 2013, the working group developed the national strategy, an operative plan for implementing palliative care, but the government has yet to approve it. From 2011 to 2013, the Global Fund to Fight AIDS, Tuberculosis and Malaria, together with the Open Society Institute Assistance Foundation Armenia and the Health Ministry ran four palliative care pilot projects in order to estimate the costs of eventually incorporating palliative care into the public health care system.
In December 2014, the Ministry of Health approved three policy documents establishing the structure and organization of palliative care services and professional qualifications for doctors and nurses in palliative care; the standards for palliative medical care and services; and clinical guidelines for pain management. These steps are important but without reforms of policies on controlled substances and education of health care workers on palliative care, the impact of these measures on the availability of palliative care will be limited at best.
Barriers to effective pain treatment place Armenia in violation of the right to health and create a risk that patients will be subjected to cruel, inhuman, or degrading treatment in violation of Armenia’s international obligations. Moreover, the World Health Assembly, the WHO’s governing body, unanimously adopted a resolution in May 2014, calling the provision of palliative care an “ethical responsibility of health systems” and urging UN member states to integrate palliative care into their health care systems. The Armenian government therefore should take the lead in addressing the barriers that currently impede the availability of good palliative care and pain treatment in Armenia.
Most importantly, the government of Armenia should adopt without further delay and implement the national strategy on palliative care, which addresses all major areas of palliative care policy: education, medicines availability, and implementation of palliative care services. It should also urgently address serious gaps in education of health care professionals on palliative care.
Key Recommendations to the Government of Armenia
On Availability of Medicines
- Work with manufacturers and importers to facilitate the registration of oral opioid painkillers. The public health care system should carry oral morphine, once it is registered, at all levels of care.
- Abolish the restriction that allows only oncologists to prescribe opioid painkillers. Allow all physicians with proper clinical training and working in palliative care to prescribe opioid painkillers.
- Remove the restriction that allows only outpatients with cancer to receive prescriptions for opioid painkillers. Any patient with a life-limiting condition with moderate to severe pain should have access to adequate pain medication.
- Reform the overly onerous procedure for the prescription of opioid painkillers by allowing doctors to make individual decisions to prescribe opioids medications and reducing bureaucratic requirements.
- Cease excessive police interference in the prescription process. Doctors should stop the current practice of filing reports on patients’ prescriptions with police. Police should make clear to doctors that they do not require such reports, formally or informally, and will no longer accept them, unless there is evidence that a crime has been committed.
On Policy Development
- Without further delay, adopt the National Strategy and Action plan for the Introduction of Palliative Care and Services in Armenia.
- Develop and incorporate palliative care services throughout the public health care system.
On Awareness Raising and Education
- Introduce palliative care instruction into medical and nursing curricula.
- Ensure that doctors and other relevant health care workers are trained in how to communicate to patients about their diagnoses and other information on life-limiting illnesses. Ensure that they are trained and supported in holding end-of-life conversations with patients and their families.
- Raise public awareness around the right to pain relief and on the availability of treatment for severe pain.
Map of Armenia
Key Terms in Palliative Care and Pain Treatment
Palliative care: Health care that aims to improve the quality of life of people facing life-limiting illness, through pain and symptom relief, and through psychosocial support for patients and their families. Palliative care can be delivered in parallel with curative treatment, but its purpose is to care, not to cure.
Life-limiting illness: A broad range of conditions in which painful or distressing symptoms occur; although there may also be periods of healthy activity, there is a strong possibility of premature death.
Psychosocial support: A broad range of services for patients and their families to address the social and psychological issues they face due to life-limiting illness. Psychologists, counselors and social workers often provide these services. Many kinds of psychosocial support can be performed by volunteers.
Hospice: A specialist palliative care program for patients close to the end of life. There are no specialized hospices in Armenia.
Chronic cancer pain: Defined in this report as pain that occurs over weeks, months, or years rather than a few hours or days. Because of its duration, moderate to severe chronic cancer pain should be treated with oral opioids rather than repeated injections, especially for people emaciated by the disease.
Analgesic: medicine used to relieve pain. In the plural form (analgesics) they denote a class of medicines that relieve pain. Analgesics provide symptomatic relief, but have no effect on the cause.
Opioid: Substance derived from the opium poppy and similar synthetic drugs. All strong pain medicines, including morphine, are opioids. Weaker opioids include codeine, tramadol, and dihydrocodeine.
Morphine: A strong opioid medicine and the mainstay medication for treatming moderate to severe pain. Morphine is considered an essential medicine by the World Health Organization in its injectable, tablet, and oral solution formulations. Oral solution mixed from morphine powder is the cheapest formulation. At this writing Armenia has registered only injectable morphine.
Dependence: In 1964, a WHO Expert Committee introduced the term “dependence” to replace the terms “addiction” and “habituation.” Dependence refers to both physical and psychological elements. Psychological or psychic dependence refers to the experience of impaired control over drinking or drug use while physiological or physical dependence refers to tolerance and withdrawal symptoms.
Dependence or physical dependence is also used in the psychopharmacological context in a narrower sense, referring solely to the development of withdrawal symptoms on cessation of use of drugs or medications.
Internationally controlled substances: Substances that are listed as subject to international control in one of the three international drug control conventions: the Single Convention on Narcotic Drugs of 1961 as amended by the 1972 Protocol; the Convention on Psychotropic Substances of 1971; and the United Nations Convention against Illicit Traffic in Narcotic Drugs and Psychotropic Substances, 1988.
Diversion: The movement of controlled drugs from licit to illicit distribution channels or to illicit use.
Curative treatment or curative care: Health care given for medical purposes when a cure is considered achievable or possibly achievable, and directed to this end.
Polyclinic: a health care facility in Armenia that is primarily devoted to the care of outpatients; it typically covers the primary health care needs of populations in local communities, in contrast to hospitals and clinical centers, which offer specialized treatments and admit inpatients for overnight stays.
Dispensary: a medical institution in Armenia for specialized hospital and outpatient care, such as oncology, mental health, endocrinology, etc.
Symptomatic treatment: a medical therapy that seeks to alleviate symptoms. It is usually aimed at improving the comfort and well-being of the patient. Symptomatic treatment largely focuses on physical symptoms, while palliative care also includes psychosocial and spiritual care.
A pain scale: a numeric scale for measurement of patient’s pain intensity, based on self-report mostly, with zero being no pain and 10 being the worst pain imaginable. This measurement approach is the most common method used internationally for determining patient reported pain. Pain severity of 5 to 6 is considered a moderate pain and generally interferes significantly with daily living activities; pain severity of 7 and higher is considered severe pain, which is generally disabling, and often renders a patient unable to perform basic everyday activities.
Essential medicines: Those medicines that are listed on the World Health Organization’s (WHO) Model List of Essential Medicines or the WHO Model List of Essential Medicines for Children. Both model lists present a list of minimum medicine needs for a basic health care system, listing the most efficacious, safe, and cost-effective medicines for priority conditions.
Misuse (of a controlled substance): Defined in this report as the non-medical and non-scientific use of substances controlled under the international drug control treaties or national law.
Over-the-counter pain medicines: Non-opioid pain medicines suitable for mild pain, including paracetamol (also known as acetaminophen), aspirin, and ibuprofen that can be obtained without a prescription.
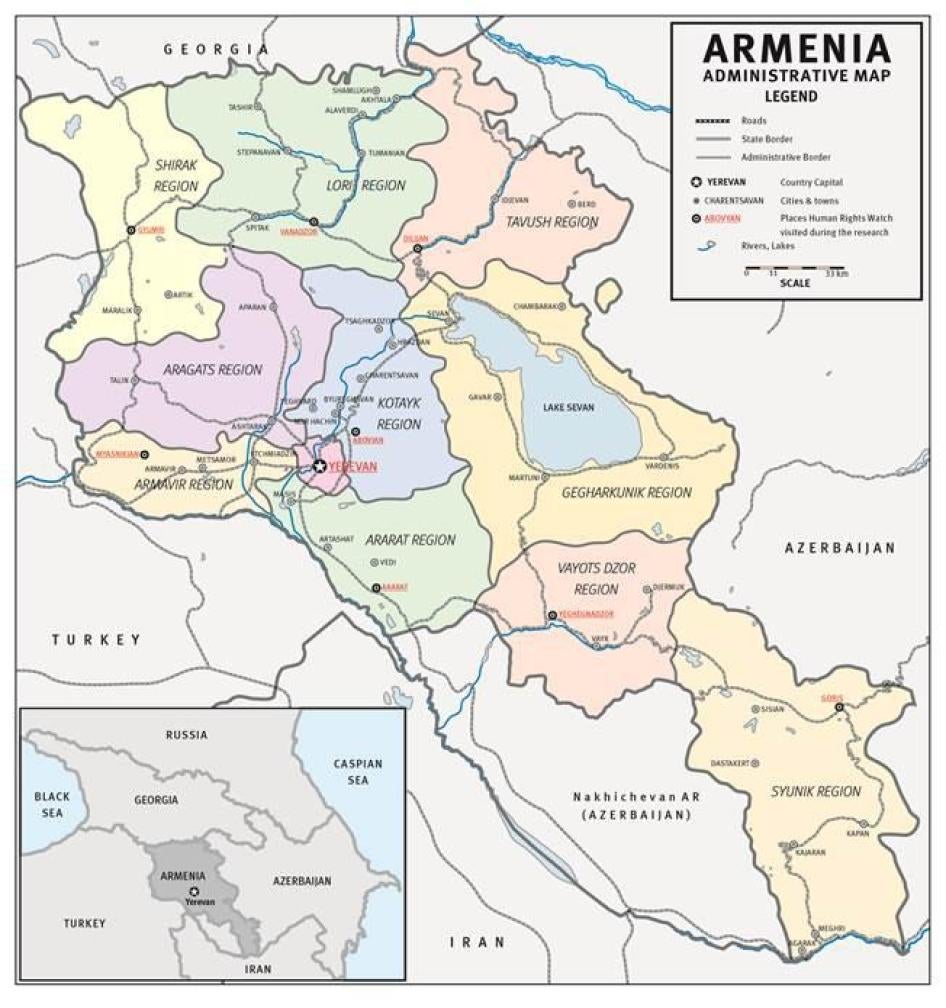
Methodology
This report is based on research conducted between July 2012 and October 2014, including three field visits to Armenia in July and November 2012 and October 2014. Field research was conducted in the capital, Yerevan, and other towns and villages throughout Armenia, including Ararat, Yeghegnadzor, Goris, Abovyan, Dilijan, Vanadzor, Gyumri, and Myasnikyan.
While this report is about palliative care generally, our research focuses on people who have cancer and who need pain treatment. The need for palliative care is most visible in people with cancer because of their sheer numbers and the severe and chronic pain and suffering they endure; and we focus mostly on the pain treatment component of palliative care because it is often the first symptom on patients’ minds.
During the three field research trips, Human Rights Watch researchers conducted 90 interviews with a wide variety of stakeholders, including 17 oncologists, 18 nurses and other medical professionals, including anesthesiologists and hospital administrators, and 26 people with cancer or their relatives.
Most interviews with patients and their relatives were conducted in their homes; some were conducted at hospitals. Interviews with patients were conducted in private whenever possible; in some cases the patient’s relatives were also in the room. All ages of the patients interviewed are as of the date of the interview.
Interviews were semi-structured and covered a range of topics related to palliative care and pain treatment. Before each interview we informed interviewees of its purpose, informed them of the kinds of issues that would be covered, and asked whether they wanted to participate. We informed them that they could discontinue the interview at any time or decline to answer any specific questions without consequence. Human Rights Watch made no promises of personal service or benefit to those whom we interviewed for this report and told all interviewees that the interviews were completely voluntary and confidential.
We concealed the identities of all patients, relatives, and health care workers interviewed to protect their privacy, except when they specifically asked for their identity to be used. Similarly, we have concealed the names of health care workers who, as government employees, may have legitimate concerns about possible negative consequences to their speaking out about problems with pain treatment.
We also met health officials, including the chief of staff of the Health Ministry, the deputy health and justice ministers, the head of the Parliamentary Committee on Health, and high-level officials from Police of the Republic of Armenia, including a deputy police chief, to present and discuss preliminary findings of our research. We also requested and obtained cancer morbidity statistics from the National Oncology Center.
Most interviews were conducted in Russian by Human Rights Watch researchers who are fluent Russian speakers. Some interviews were conducted in Armenian, during which a translator for Human Rights Watch (a native speaker of Armenian) translated into Russian or English.
All documents cited in this report are publicly available or on file with Human Rights Watch.
I. Background
The Importance of Palliative Care and Pain Treatment
Palliative care seeks to improve the quality of life of patients, both adults and children, facing life-limiting or terminal illness. Its purpose is not to cure a patient or extend his or her life. Palliative care prevents and relieves pain and other physical and psychosocial problems. In the words of Dame Cicely Saunders, the founder of the first modern hospice and a lifelong advocate for palliative care, palliative care is about “adding life to the days, not days to the life.” The World Health Organization (WHO) recognizes palliative care as an integral part of health care that should be available to those who need it.[2] While palliative care is often associated with cancer, a much wider circle of patients with health conditions can benefit from it, including patients in advanced stages of neurological disorders, cardiac, liver, or renal disease.[3]
One key objective of palliative care is to offer patients effective treatment for their pain. Chronic pain is a common symptom of cancer and HIV/AIDS, as well as other health conditions, especially in the terminal phase of illness.[4]The WHO estimates that around 80 percent of both cancer and AIDS patients and 67 percent of patients with both cardiovascular diseases and chronic pulmonary diseases will experience moderate to severe pain at the end of life.[5] A recent global review of pain studies in cancer patients found that 60 to 90 percent of patients with advanced cancer experience moderate to severe pain.[6]
Moderate to severe pain has a profound impact on quality of life. Persistent pain has a series of physical, psychological, and social consequences. It can lead to reduced mobility and consequent loss of strength; compromise the immune system; and interfere with a person’s ability to eat, concentrate, sleep, or interact with others.[7] A WHO study found that people who live with chronic pain are four times more likely to suffer from depression or anxiety.[8] The physical effect of chronic pain and the psychological strain it causes can even influence the course of disease: as the WHO notes in its cancer control guidelines, “Pain can kill.”[9] Social consequences include the inability to work, care for oneself, children or other family members, participate in social activities, and find closure at the end of life.[10]
According to the WHO, “Most, if not all, pain due to cancer could be relieved if we implemented existing medical knowledge and treatments” (original emphasis).[11] The mainstay medication for the treatment of moderate to severe pain is morphine, an inexpensive opioid that is made of an extract of the poppy plant. Morphine can be injected, taken orally, delivered through an IV or into the spinal cord. It is mostly injected to treat acute pain, generally in hospital settings. Oral morphine is the medicine of choice for chronic cancer pain, and can be taken both in institutional settings and at home. Morphine is a controlled medication, meaning that its manufacture, distribution, and dispensing is strictly regulated both at the international and national levels.
For decades, medical experts have recognized the importance of opioid pain relievers. The 1961 Single Convention on Narcotic Drugs, the international treaty that governs the use of narcotic drugs, explicitly states that “the medical use of narcotic drugs continues to be indispensable for the relief of pain and suffering” and that “adequate provision must be made to ensure the availability of narcotic drugs for such purposes.”[12] The WHO has included morphine in its Model List of Essential Medicines, a list of the minimum essential medications that should be available to all persons who need them, since it was first established.[13]
Yet, approximately 75 percent of the world population has either no or insufficient access to treatment for moderate to severe pain and tens of millions of people around the world, including around 5.5 million cancer patients and one million end-stage HIV/AIDS patients, suffer from moderate to severe pain each year without treatment.[14]
Palliative care is broader than just relief of chronic physical pain. Other key objectives of palliative care include the provision of care for other physical symptoms and psychosocial and spiritual care to both the patient and his or her family. Life-limiting illness is frequently associated with various other physical symptoms, such as nausea and shortness of breath, that have significant impact on a patient’s quality of life. Palliative care seeks to alleviate these symptoms.
People with life-limiting illness and their relatives often confront profound psychosocial and spiritual questions as they face life-threatening or incurable and often debilitating illness. Anxiety and depression are common symptoms.[15] Palliative care interventions like psychosocial counseling have been shown to considerably diminish incidence and severity of such symptoms and to improve the quality of life of patients and their families.[16]
The WHO has urged countries, including those with limited resources, to make palliative care services available. It recommends that countries prioritize implementing palliative care services in the community—providing care at people’s homes rather than at health care institutions—where it can be provided at low cost and where people with limited access to medical facilities can be reached, and in medical institutions that deal with large numbers of patients requiring palliative care services.[17]
In recent years, the WHO and the World Bank have urged countries to implement free universal health coverage to ensure that all people obtain the health services they need without suffering financial hardship when paying for them.[18] Palliative care is one of the basic health services that the WHO and the World Bank say should be available under universal health coverage, along with “promotive, preventive, curative, and rehabilitative” health services.[19]
In May 2014, the World Health Assembly, the WHO’s governing body, unanimously adopted the resolution “Strengthening of palliative care as a component of comprehensive treatment within the continuum of care,” calling the provision of palliative care an “ethical responsibility of health systems.” It made detailed recommendations to UN member states with regard to development of policies supportive of palliative care; the provision of training and education for health care workers; and drug regulatory reforms to ensure the adequate availability of opioid analgesics.[20]
Background on Armenia
Armenia’s Health Care System
After the collapse of the Soviet Union, Armenia inherited a centralized health care system with free medical care for the entire population and access to a comprehensive range of primary, secondary, and tertiary services funded by general government revenues.[21] Since then, Armenia has undertaken extensive health care reforms to decentralize the health care system, to make it more efficient, and implement new approaches to health care financing, including through privatization.[22] One of the core elements of the reform was changing the primary care system and the introduction of the family doctor. Armenia still has a highly centralized health care system, in which the central government makes most decisions on resource allocations.
Institutional Structure of Health Care
Primary outpatient health care services in Armenia consist of city polyclinics, regional health centers, small village health clinics, and nursing/obstetric units. Provision of services is based on the population levels in a given community. Secondary care is provided by regional hospitals and dispensaries, or facilities that provide both inpatient and outpatient care in a single field of specialization, such as oncology, mental health, endocrinology, etc. National hospitals and specialized national institutions, such as the National Oncology Center in Yerevan, provide tertiary or further specialized care.[23]
Oncology services in polyclinics are free of charge. They perform cancer prevention and early detection, refer patients to specialized secondary and tertiary institutions for surgery and other curative treatment, and provide symptomatic treatment to oncology patients after curative care becomes ineffective. Polyclinics also register and keep track of oncology patients in the community and report statistics to the National Oncology Center.
The state is the exclusive provider of opioid pain medications. It purchases them from importers and provides them free of charge to pharmacies and health care facilities, which in turn do not charge patients for them.
Financing
Health care is financed by the state from tax revenues. Data on public spending on health care are difficult to assess because “[l]egislation does not require the systematic collection of comparable data, and existing data collection systems are fragmented.”[24] World Bank data estimates health care spending at 1.9 percent of Armenia’s GDP for the period 2010-2014.[25] The IMF estimated that public health care spending stood at 2.5 percent in 2012, but also noted the figure was an estimate because data on government spending by functional classification was not available for Armenia. [26]
While the government has almost doubled its health care expenditures since 2008, current spending still amounts to a small percent of the overall government spending budget and reflects a low priority in public spending.[27] Inadequate health care financing has increased institutional dependency on both formal and informal payments by patients. Formal payments include fees for medical services set by law; informal payments are usually “gratuities” to doctors, as well as purchases by the patients themselves of medicines that are not state-subsidized. Private health expenditures compose 48.3 percent of total health expenditures, with 84.6 percent paid out of pocket at the point of service.[28] With 35.8 percent of Armenians living below the poverty line in 2010, poverty is a large barrier to health care access for many Armenians. As a result, people often postpone necessary consultations or do not make use of medical services in first place.[29]
Noncommunicable and Chronic Illnesses and Palliative Care Needs
Like other low- and middle-income countries, Armenia faces both an increasing burden of chronic illness and major challenges in responding to them. As of 2013, Armenia’s population was 2,977,000.[30] According to World Health Organization statistics, the majority of deaths are due to non-communicable diseases (92 percent, total deaths 37,000): cardiovascular diseases (54 percent), cancers (22 percent), chronic respiratory diseases (5 percent), diabetes (3 percent), and other NCDs (non-communicable diseases) (8 percent).[31] According to 2012 data, the age-standardized mortality rate for malignant neoplasms for both Armenian males and females was 219.6 per 100,000 of the population.[32] In 2012, the top three causes for mortality per 100,000 of the population were: 1. noncommunicable diseases (847.5); 2. communicable diseases (45); and 3. injuries (49.2).[33] In addition, there is prevalence of lifestyle-associated health problems, such as tobacco smoking, with, according to WHO data, 47 percent of males and 2 percent of females engaging in this practice in 2011.[34] Tuberculosis (TB) continues to be a public health issue with 2,000 TB cases in 2013.[35] The prevalence of HIV/AIDS in the adult population aged 15-49 was 0.1 percent from 2001-2009 and increased to 0.2 percent in 2013.[36]
In Armenia, knowledge about noncommunicable diseases and cancer is limited, leading to frequent misdiagnosis and late referral of patients. It should be noted that Armenia does not have a national cancer registry, and data on cancer mortality varies. According to a WHO estimation, 8,100 people died of cancer in Armenia in 2012.[37] Data also shows that a high percentage of cancer is diagnosed only in advanced stages. According to the deputy head of the National Oncology Center, about 46 percent of patients are diagnosed at stage three or four in Armenia, when treatment is ineffective and palliative care is needed.[38] That figure, however, does not appear to include a significant number of those diagnosed post-mortem. According to statistics provided by the National Oncology Center, 7,911 people were diagnosed with cancer in 2013 in Armenia. Of these 2,949 were diagnosed at stage three and four, while 1,274 were diagnosed post-mortem (see Table 1).[39]
Table 1. Malignant Neoplasm Morbidity Rate[40]
1. Number of newly registered patients with malignant neoplasm:
|
2012 |
Armenia – 7,877 |
Men – 3,961 |
|
Women – 3,916 |
||
|
Yerevan – 2,747 |
Men – 1,301 |
|
|
Women – 1,446 |
||
|
2013 |
Armenia – 7,911 |
Men – 3,942 |
|
Women – 3,969 |
||
|
Yerevan – 2,863 |
Men – 1,341 |
|
|
Women – 1,522 |
2. Number of patients who died from malignant neoplasm:[41]
|
2012 |
Armenia |
TOTAL |
Registered |
Discovered post-mortem |
|
5,705 |
4,377 |
1,328 |
||
|
Yerevan |
1,992 |
1,411 |
581 |
|
|
2013 |
Armenia |
5,581 |
4,307 |
1,274 |
|
Yerevan |
2,085 |
1,464 |
621 |
3. Number of newly registered patients with malignant neoplasms based on stage of the disease:
|
2012 |
Stages one and two – 2,261 |
|
Stage three – 1,119 |
|
|
Stage four – 1,903 |
|
|
2013 |
Stages one and two – 2,247 |
|
Stage three – 985 |
|
|
Stage four –1964 |
II. The Plight of Patients
Cancer patients in Armenia, their family members, and health workers told Human Rights Watch of experiences of untreated pain and lack of psychosocial support and the impact of pain on the quality of their lives. They described how untreated pain led to reduced mobility, loss of strength, inability to eat, speak, concentrate, sleep, or interact with others, as well as anxiety, despair, and in some cases thoughts of suicide. Pilot projects in palliative care that ran in Armenia in 2011 through 2013 showed that such suffering can be largely avoided.
Availability of and Need for Palliative Care in Armenia
A needs-assessment study on palliative care commissioned by the Open Society Foundations and conducted in 2012 estimated that approximately 18,000 patients, including 5,500 cancer patients, need palliative care annually in Armenia.[42] In addition, at least twice as many family members require palliative care support.[43] The same study estimated that up to 60 palliative homecare teams are needed for the country, including 24 for Yerevan.[44]
However there are essentially no publicly-funded palliative care services in Armenia. Private palliative care services are available in at least two hospitals in Yerevan but they are unaffordable for most Armenians.
It is currently standard practice in Armenia that when cancer patients are no longer curable, they are sent for “symptomatic treatment” with oncologists at primary health facilities, who provide only minimal and mostly inadequate pain treatment.
People with advanced cancer have extensive health care needs, even if their disease can no longer be cured. They are likely to face various physical and psychosocial symptoms, including pain, difficulty breathing, bed sores, and anxiety. In Armenia, families traditionally care for their ill relatives at home. However, families are generally poorly equipped to do so because the health care system does not provide them any support.
There are no services for outpatients and their caregivers to provide psychosocial support and information about the course of the disease and potential symptoms; to teach family members about basic care and help them provide it; or to prepare the patient and family for what may/will come. Also, despite years of health care reform, Armenia’s health care system is still not set up to deliver general, regular homecare services, except for a mobile ambulance service, which does rapid assessment of patients and if need be transfers them to a hospital. As a result, families often have to scramble to try to take care of a dying loved one without any knowledge of how best to do so, leading to tremendous suffering for both patients and caregivers.
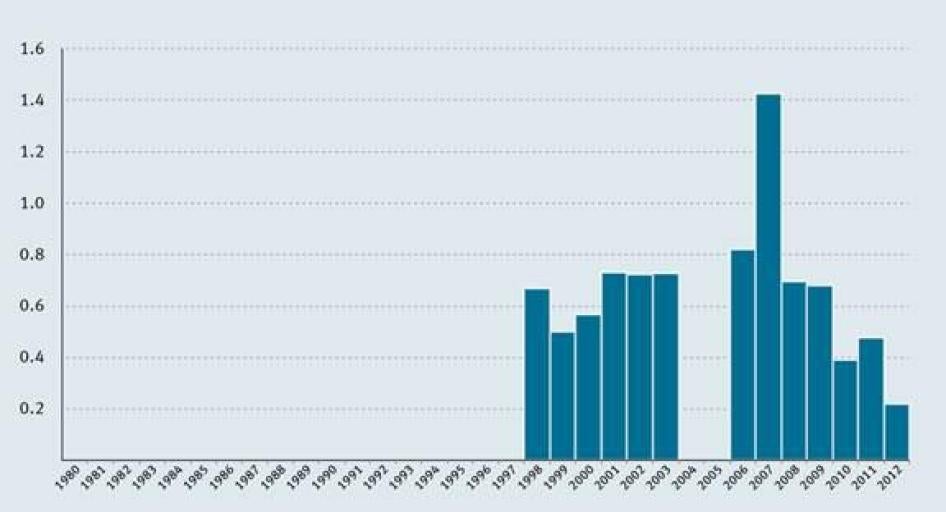
Furthermore cancer patients in Armenia are not getting adequate opioid pain treatment. As noted above, the WHO estimates that around 80 percent of cancer patients will experience moderate to severe pain at the end of life and will require morphine for an average period of 90 days before death.[45] In contrast to these estimates, from 2010 through 2012 Armenia consumed an average of 1.1 kg of morphine per year.[46] This is sufficient to adequately treat moderate to severe pain in about 180 patients with terminal cancer or AIDS, which is about 3 percent of those estimated to require such treatment in Armenia.[47]
Consumption data reported by the Armenian government to the International Narcotics Control Board (INCB) shows a clear decline in per capita consumption of morphine in the country in the last five years, in contrast to significant increases in the use of the medicine globally and in the region over the same period (see Chart 1. Armenia Morphine Consumption 1980-2012). In 2012, Armenia used less than 0.25 milligrams of morphine per person, 50 times less than the European average and 25 times less than the global average.[48] Given rising cancer mortality, the decline in morphine usage suggests that the gap between the need for opioid medications among cancer patients in Armenia and actual access is growing rapidly.
Chart 1. Armenia Morphine Consumption (mg/capita) 1980-2012[49]
Data collected by Human Rights Watch from nine polyclinics throughout Armenia shows that only 47 patients (i.e. less than 8 percent) out of 594 who died of cancer in 2011 received strong opioids before they died (see Table 2).
Moreover, as described elsewhere in this report, those who do receive opioid analgesics in Armenia generally do so for far fewer than 90 days. This suggests that many patients in Armenia who face moderate to severe pain are started late on opioids, do not receive the medication in sufficient quantities, or do not receive the medication at all even when it is available.
Table 2. Population, Cancer Morbidity, and Access to Opioids[50]
|
District |
Population Residing in the Area[51] |
Number of Registered Cancer Patients for 2012 |
Cancer Mortality for 2011 |
Number of Patients Who Received an Opioid Analgesic in 2011 |
|
Yerevan Polyclinic no.1 |
25,000 |
177 |
41 |
2 |
|
Polyclinic no. 4 |
26,000 |
400 |
18 |
4 |
|
Polyclinic no. 17 |
44,000 |
492 |
98 |
6 |
|
Polyclinic no. 9 |
20,000 |
239 |
73 |
12 |
|
Polyclinic no. 14 |
80,000 |
>2,000 |
132 |
3 |
|
Ararat Clinical Center |
40,000 |
340 |
No data |
2 |
|
Yeghegnadzor town polyclinic |
No data |
288 |
29 |
6 |
|
Abovyan District |
112,000 |
937 |
153 |
12 |
|
Dilijan Medical Center |
22,000 |
250 |
50 |
2 |
The Suffering Caused by Untreated Pain
Patients’ Suffering
Sixty-one-year-old Lyudmila, the retired kindergarten teacher quoted at the beginning of this report, discovered a lump in her breast around 2002, but did not seek medical help for about five years. She was diagnosed with breast cancer in 2007, when the tumor was inoperable and the cancer had already spread to her armpit and left shoulder. Lyudmila started to develop severe pain in 2010. When Human Rights Watch interviewed Lyudmila in 2012 she was receiving one ampoule of omnopon (an opioid analgesic similar to morphine) per 24 hour period, which was enough to sooth her pain only for two hours, while she continued to experience excruciating pain for the rest of the day.
Lyudmila explained that pain never fully leaves her, but when it decreases she feels like a normal person, able to communicate with her children and do some household work, but she said:
[when] pain attacks start unexpectedly and I start screaming and become a different person. When my hand starts burning like I hold it over a fire, I know the pain attack is about to start. When it starts I lose verbal communication skill and can only point to things with my right hand. I have the pain attacks every night, but sometimes it happens also during the day. Often I drink really hot water as it helps me to forget about the pain for a bit. It’s inhumane pain, unbearable pain for a human being.[52]
Seventy-five-year-old Tigran T., a Vanadzor resident, is a father of two and grandfather of five. He developed sudden pains in the shoulder area in 2011, and was soon thereafter diagnosed with a malignant tumor. He explained to Human Rights Watch that usually he had a high tolerance for pain, but never before had he felt anything like the pain from the tumor:
The pain starts in the back then the shoulder, continues to the right hand and I can’t move my fingers any more. I’ve seen a lot of pain in my life, but this pain is nothing I’ve felt before. I can’t lie on my side longer than five minutes. The pain gradually goes away when I get an injection [with an opioid analgesic], but never fully, and in about four hours it comes back again. I can’t do without strong pain killers.[53]
In 2008, Gayane G., a 46-year-old widow, was diagnosed with a rectal tumor that later spread to her bones. She had two surgeries and underwent a round of chemotherapy and eight rounds of radiation therapy, before she was referred for symptomatic treatment in 2011. That was when she developed severe pains. At the time Human Rights Watch visited her, Gayane was receiving tramadol pills (an opioid analgesic that is generally not sufficiently potent to treat severe pain), which did little to mitigate her pain. She explained:
The pains are unbearable; I cry, scream, feel like I’m walking on fire all the time. My left side fully and my left leg would ache. I try to endure the pain when someone is at home, but when I am alone, all I can do is cry… I can’t sleep at nights and can only do so after several sleepless nights, when I am fully exhausted. I live in pain all the time, as if the pain is with me always. It’s part of my life.[54]
Karine K., a resident of Ararat, has four children and six grandchildren. She worked as a nanny in a local kindergarten her entire adult life. She had surgery in 2009, when she was 57, for an abdominal tumor, and was in remission for three years. In 2011 she developed severe pain, 8 on a scale of 10, as she described to Human Rights Watch:
I felt like I was walking on needles. The pain would start from my hip and extend down to the entire right leg. I felt really bad, crying all the time. I did not know what sleep was during those pains. All I could dream of was a time when the pain would disappear, so that I would feel free. I felt so bad that I wanted to die; once I even asked to be given something so that I could die.[55]
Like Karine, several others told us that they wanted to end their lives to stop the pain, prayed for death, or told doctors or relatives that they wanted to die. As a doctor involved in a palliative care pilot project explained, often patients ask him for enough medication to allow them to die without pain. He said: “I tell them that I’ll prescribe you pain medication and let’s get back to the issue afterwards. And when the pain is gone, they don’t remember it anymore.”[56]
Families’ Suffering
The toll on family members caused by their loved ones’ untreated pain can be severe. As a daughter of 62-year-old Syranush S., who was suffering from an abdominal tumor, explained to Human Rights Watch, she feels she wants to die when seeing a person so dear to her in excruciating pain. She went on to say that her mother experiences sudden mood swings associated with pain:
My mother is a very kind person, loves to play with her grandchildren, when not in pain, she is lively, jokes, takes care of herself, makes coffee or something sweet for everyone, but when pain strikes she can’t cope, she becomes very nervous, does not want to see anyone, including kids.[57]
Another person who lost two family members to cancer, told Human Rights Watch, “When someone is sick in a family, everything is on the shoulders of his or her relatives, finding doctors, treatment, drugs…. You really need someone to support the relatives in such situations. When we were sent for symptomatic treatment, we did not get any guidance, any instructions on what to expect or how to help.”[58]
The Positive Effect of Palliative Care Pilot Projects
From 2011 to 2013 the Global Fund to Fight AIDS, Tuberculosis and Malaria, together with the Open Society Institute Assistance Foundation Armenia and the Health Ministry, ran four palliative care pilot projects in Armenia.[59] Two operated in Yerevan (one in the National Oncology Center, and another one at the University Hospital), while two others operated in the towns of Ararat and Vanadzor. The projects’ main goal was to establish model palliative care programs, and estimate its costs and effectiveness in order to eventually replicate them throughout Armenia’s public health care system.[60]
In the first year, the pilot project offered symptomatic treatment and psychological support services to a total of 132 patients and their families, and dispensed pain medication, including opioids, in line with WHO guidelines.[61] An assessment of the project conducted in 2012 found improvement in the patients’ pain management and quality of life.[62] The assessment report, however, acknowledges the limitations of its own findings, stating that patients’ experiences were not measured against those of a control group.[63]
Human Rights Watch visited all four pilot project sites and interviewed doctors, nurses, and other medical personnel involved in the project implementation. We also interviewed over a dozen of patients who participated in the projects. All patients and families spoke highly of the care they were receiving and described the transformative impact palliative care had on their quality of life. They described stark differences before and after they started receiving palliative care. One family member of a patient suffering from cancer told Human Rights Watch that she found pain treatment to be the “key and most important component of palliative care,” which had a transformative effect on everyone involved.[64]
Fifty-five-year-old Satenik Alexanyan discovered a tumor in her breast in 2011. Because the tumor was inoperable, she underwent six rounds of chemotherapy, after which a wound opened up on her breast that would not heal. At that point she developed severe pain in her left arm and hand:
It was a constant pain. I wanted to sleep, but could not, the pain would not let me. This lasted for a year or so. I bought some [over-the-counter] pain killers myself, but they would not help for long. When I told my doctors about the pain, they were telling me that it was normal; that’s how it should be.[65]
Satenik’s oncologist referred her to the palliative care pilot project in the Ararat Regional Hospital. When Human Rights Watch interviewed Satenik, she was still a patient with the pilot project and was getting tramadol, a weak opioid, and benefitting from psychosocial services, the combination of which helped her manage her pain:
I did not want to see anyone or do anything before. I was in another world. When I had pain, I could not feel anything else. I could not even hear anything. Then these people [referring to medical personnel involved in the pilot project] started to come, talk to me. They helped me to come back to this world. It’s good that there is such a group. They helped me a lot. I feel better.[66]
Karine K., whose experience with pain, as described above, led her to feel suicidal, also participated in the pilot project in Ararat.[67] She started receiving opioids after enrolling in the program in June 2012. Karine described the stark difference the pain medication and palliative care made in her life:
I used to be very depressed. I find the talks with them [palliative care group members] very useful. They make me want to live longer. I now want to live for my grandchildren.[68]
While relieving pain is a critical part of palliative care, many patients participating in the pilot projects highlighted human attention and interaction as key components they appreciated most.[69] For example, a patient from town of Ararat said that staff of the palliative care group brought “hope and faith” and she particularly valued “human interaction.” “They come and talk to me, spend time with me,” she explained.[70]
The family member of one patient recalled how surprised she was when palliative care staff members were calling proactively, inquiring, and listening to what the caregivers had to say; “she [palliative care group nurse] was always very calm, very supportive. I particularly liked their humanity,” she said.[71]
III. Comparing Armenia’s Pain Treatment Practices with WHO Principles
The WHO Cancer Pain Ladder, a treatment guideline first published in 1986, is an authoritative summary of international best pain treatment practices.[72] Based on a wealth of pain treatment research that spans decades, it has formed the basis for cancer pain treatment in many countries around the world. It has also been used successfully to treat other types of pain.[73] The treatment guideline is organized around five core principles for treating pain (see Table 3). The European Society for Medical Oncology (ESMO) and the European Association of Palliative Care (EAPC) have also developed cancer pain treatment guidelines that follow these same core principles.[74] If followed, WHO estimates, the ladder can result in good pain control for 70 to 90 percent of cancer patients.[75]
Under the right to health, governments must ensure that pain treatment be not only available and accessible, but also that it be provided in a way that is scientifically and medically appropriate and of good quality.[76] This means that health care providers should provide pain management in a way that is consistent with internationally recognized standards. Governments, in their turn, should create conditions which allow health care providers to provide such treatment.
This chapter describes the five core principles and summarizes how standard pain treatment practices in Armenia deviate fundamentally from them.
Table 3. Comparing the Core Principles of Cancer Pain Treatment with Armenia’s Pain Treatment Practices
|
WHO Recommendation |
Armenia’s Practice |
|
Principle 1: Pain medications should be delivered in oral form (tablets or syrup) when possible. |
Patients receive morphine by injection only. Oral morphine is not available or registered. |
|
Principle 2: Immediate release pain medications should be given every four hours. |
Most patients interviewed by Human Rights Watch received morphine once or twice per day. Oncologists could recall only a few cases of higher dosages. |
|
Principle 3: Morphine should be started when weaker pain medications prove insufficient to control pain. |
Many oncologists in Armenia interviewed by Human Rights Watch suggested that strong opioids can be prescribed only to a dying patient in his/her last days of life. Cancer mortality and opioid prescribing data from nine Armenian polyclinics show that in 2011 only 7.9 percent of terminal cancer patients attended by those clinics received a strong opioid analgesic, whereas research suggests about 80 percent of people with advanced cancer suffer from moderate to severe pain and may require opioid analgesics. |
|
Principle 4: Morphine dose should be determined individually. There is no maximum daily dose. |
All oncologists interviewed by Human Rights Watch said that when they start patients on morphine they start them with one ampoule, irrespective of need. If they were to increase the dosage to two ampoules they would do so only after two weeks. |
|
Principle 5: Patients should receive morphine at times convenient to them. |
Patients can take the little morphine they are given at a convenient time for them. Most said they take it at night so they can at least sleep for some hours. This means many suffer with inadequate pain management throughout the day. |
Principle 1: “By Mouth”
If possible, analgesics should be given by mouth. Rectal suppositories are useful in patients with dysphagia [difficulty swallowing], uncontrolled vomiting or gastrointestinal obstruction. Continuous subcutaneous infusion offers an alternative route in these situations. A number of mechanical and battery operated pumps are available.
—WHO Treatment Guideline[77]
The first principle of the WHO cancer pain treatment guideline reflects a fundamental principle of good medical practice: the least invasive medical intervention that is effective should be used when treating patients. As injectable analgesics provide no benefit over oral pain medications for most patients with chronic cancer pain, the WHO recommends the use of oral medications. Also, using oral medications eliminates the risk of infection that is inherent in injections and is particularly elevated in patients who are immuno-compromised due, for example, to HIV/AIDS, chemotherapy, or certain hematologic malignancies. Hence, oral morphine, which the WHO considers an essential medicine that must be available to all who need it, is the cornerstone of the treatment guideline.[78]
When patients cannot take oral medications and injectable pain relievers are used, it recommends subcutaneous administration (under the skin) to avoid unnecessary repeated sticking of patients.[79]
Principle 2: “By the Clock”
Analgesics should be given “by the clock,” i.e. at fixed [four hours for immediate release] intervals of time. The dose should be titrated against the patient’s pain, i.e. gradually increased until the patient is comfortable. The next dose should be given before the effect of the previous one has fully worn off. In this way it is possible to relieve pain continuously.
Some patients need to take “rescue” doses for incident (intermittent) and breakthrough pain. Such doses, which should be 50-100% of the regular four-hourly dose, are in addition to the regular schedule.
—WHO Treatment Guideline[80]
The second principle reflects the fact that the analgesic effect of immediate release morphine lasts four to six hours. Thus patients need to receive doses of morphine at four-hour intervals to ensure continuous pain control. Slow release morphine, which is often used once a patient is titrated to the proper dose, should be given at the manufacturers recommended intervals (usually 8 to 12 hours).
Principle 3: “By the Ladder”
The first step is a non-opioid. If this does not relieve the pain, an opioid for mild to moderate pain should be added. When an opioid for mild to moderate pain in combination with non-opioids fails to relieve the pain, an opioid for moderate to severe pain should be substituted. Only one drug of each of the groups should be used at the same time. Adjuvant drugs should be given for specific indications….
If a drug ceases to be effective, do not switch to an alternative drug of the same efficacy but prescribe a drug that is definitely stronger.
—WHO Treatment Guideline[81]
According to the WHO guideline, the intensity of the pain should determine what type of pain medications a patient receives.
For mild pain, patients should receive over-the-counter medications like Ibuprofen or Paracetamol; for mild to moderate pain a weak opioid, like codeine or tramadol; and for moderate to severe pain a strong opioid, like morphine or methadone. If over-the-counter pain medications or weak opioids are ineffective or pain is severe, a stronger type of pain medication should be provided.
The guideline emphasizes that “the use of morphine should be dictated by the intensity of pain, not by life expectancy.”[82]
Principle 4: “For the Individual”
There are no standard doses for opioid drugs. The “right” dose is the dose that relieves the patient’s pain. The range for oral morphine, for example, is from as little as 5 mg to more than 1000 mg every four hours. Drugs used for mild to moderate pain have a dose limit in practice because of formulation (e.g. combined with ASA or paracetamol, which are toxic at high doses) or because of a disproportionate increase in adverse effects at higher doses (e.g. codeine).
—WHO Treatment Guideline[83]
Pain is an individual experience. Different people perceive pain differently; they metabolize pain medications in different ways; and cancers vary from person to person, leading to vastly divergent types and intensities of pain. With so many variables, only an individualized approach to pain treatment can ensure the best relief to all. The WHO therefore recommends that doctors “select the most appropriate drug and administer it in the dose that best suits the individual.”[84]
Finding the right dose of morphine for the individual patient is crucially important: if the dose is too low, the patient's pain will be poorly controlled, if too high, the patient will experience unnecessarily severe side effects, including drowsiness, constipation, and nausea. With the right dose, relief is maximized, side effects are minimized.
Slow release morphine (currently not available in Armenia) is often used once a patient’s dose has been properly titrated. It is much more convenient for patients and their care givers as it provides relief over a longer period of time, allowing them, for example, to have a full night’s sleep without having to take medications in the middle of the night.
Principle 5: “Attention to Detail”
Emphasize the need for regular administration of pain relief drugs. Oral morphine should be administered every four hours. The first and last dose should be linked to the patient’s waking time and bedtime. The best additional times during the day are generally 10:00, 14:00 and 18:00. With this schedule, there is a balance between duration of analgesic effect and severity of side effects.
—WHO Treatment Guideline[85]
To ensure quality of life for patients with pain, it is important not only to get pain medications regularly but to get them at times that fit their schedule. In order to maximize sleep at night, for example, patients should take their medications shortly before bed time.
Principle vs. Practice
Due to the many obstacles documented in Chapter IV of this report, few patients have the luxury of taking opioid medication in a manner that allows them to benefit maximally from its effects.
First, oral morphine is not available at all in Armenia. In fact, it is not even a registered medication.[86] Clinical palliative care guidelines clearly recommend against the use of intramuscular injections for pain relief in favor of oral medications.[87] The authorities briefly allowed the use of methadone—an oral synthetic opioid often used in substitution therapy for drug addiction—at two palliative care pilot project sites. Marine Khachatryan, whose mother participated in one of the pilot projects, recalled how her mother suffered from severe pain for almost a year because she would panic at the thought of needles and could not take injectable opioids. She was diagnosed in 2010 with stage four abdominal cancer and underwent several rounds of chemotherapy that were not successful. In 2011 she developed severe pain, “it was a permanent pain,” Marine recalled.
She could not walk and she would scream from pain. She was prescribed injectable Tramadol, but we could not administer it as she was so afraid of needles. It was only after she was included in the pilot project and started receiving methadone that she started to feel normal again. For six hours after taking methadone, she would be calm and communicate with us again. She died a month after she started to receive methadone, but that was the only month in several years that she slept like a normal person.[88]
Second, while the WHO recommends that injectable pain relievers should be injected under the skin, standard practice in Armenia is to give morphine by intramuscular injection, which often results in a large number of unnecessary intramuscular injections. Such injections can become difficult as some patients are emaciated due to their illness and have little muscle tissue left. As one doctor put it, “sometimes you don’t know whether you end up injecting in muscle or bone. If there’s no muscle tissue at all, which also happens, then it’s a problem.”[89] One oncologist told us that she does not like prescribing injections, as she herself dislikes injections and does not want others to suffer from them.[90] Another explained that there are cases when relatives of a patient refuse it, as injections are associated with pain and they do not want to cause further pain to the patient, and prefer to use weaker, oral pain killers.[91]
Human Rights Watch interviewed several patients and family members of patients, like Marine Khachatryan, who refused to take injections because of their severe fear of needles.
Third, in stark contrast to principles 2 through 5, doctors almost never perform clinical titration of pain medication; in other words, they do not seek to determine the right dose for each individual patient. Nearly all oncologists interviewed for this report said that if they start a patient on opioids, they more or less automatically start with a dose of one ampoule daily, even though there is no regulation limiting the initial daily dose of opioids. Almost all patients Human Rights Watch spoke to who were prescribed opioids received an initial dose of one ampoule per day which, they said, was not enough to mitigate their pain around the clock. A few said they were started on two ampoules.
Many doctors said they would increase the dosage to two per day only about two weeks later, even if it was clear that the single ampoule was insufficient to control the patient’s pain prior to two weeks. An oncologist in one of Yerevan’s polyclinics explained to Human Rights Watch:
We start with one ampoule of morphine and increase later if need be. In about two weeks or twenty days we usually increase the dosage. This might not be very humane, but that’s how it is. We know that 1 ampoule is enough for 4 to 6 hours, but we always start with 1 ampoule and give other painkillers too. I might not agree with it, but that’s how it is.[92]
Although Armenian regulations do not set out a dosage limitation for opioids, in practice there is an informal understanding among oncologists that no more than 10 ampoules can be prescribed per prescription.[93]
Another Yerevan-based oncologist said that in order to extend the effects of morphine, oncologists split one ampoule into two parts and have it administered twice during a day, supplemented with other weaker pain medications: “We start with one ampoule and then increase gradually, maybe in a month or 20 days. With one ampoule, we prescribe half in the morning and half in the evening. The minimum period before we can increase is one week.”[94]
Health care workers and patients told Human Rights Watch that they often supplement opioids with weaker pain medications, weak opioids, muscle relaxants and sedatives, to try to dull the pain in the intervals between morphine doses. However, these are often not potent enough or even appropriate to provide effective relief and expose patients to unnecessary side effects. For example, a physician in a southern town of Armenia told Human Rights Watch: “One ampoule is not enough, we know. But we combine opioids with other analgesics, like Ketonal, Diclofenac, and others.”[95]
While the WHO treatment guideline provides for the use of weak pain medications and other adjuvant medications in addition to a strong opioid analgesic to enhance the latter’s analgesic effect or treat specific problems, they are not recommended to be used as an alternative as they are incapable of providing adequate relief.[96]
Because of these practices, many patients with life-limiting illnesses have to make hard choices about how to use their dosages. For example, Lyudmila L., who was prescribed only one ampoule of opioid per 24-hour period, kept it only for nights as the dose was hardly enough for two hours and she preferred to sleep those hours. She explained:
During the day I endure the pain. What else can I do? I have a prescription only for one ampoule. I take it the way it’s prescribed.[97]
A doctor at a medical center in Abovyan, a town 16 kilometers northeast of Yerevan, who confirmed the dosage pattern described above, recalled that in the first seven months of 2012, six out of about 950 registered oncology patients received opioid analgesics, five of whom had passed away.[98] The remaining patient had had both of his legs amputated and was already receiving five ampoules of opioids a day at the time when he was registered with the clinic. The doctor felt clearly uncomfortable about this patient and explained to Human Rights Watch that once every 10 days, a family doctor would visit him unannounced, write up a report on how many empty and full ampoules he had remaining, and inform police if he had consumed more than his prescribed dose.[99]
Another doctor confirmed that it is very rare for a patient to receive opioids for an extended period of time, reflecting the common belief in Armenia that opioids can be prescribed only to a dying patient in his or her last days of life. “Usually, our patients get opioids for a week, some even less, we had a case when a patient got it for only a day before she died,” explained the doctor.[100] A pharmacy official also referred to the informal understanding among medical personnel to prescribe opioids as late as possible and at the lowest possible dosage.[101] According to the main importer of opioids, it is rare for any patient to receive opioids for longer than a month. Usually, the importer said, a patient only receives opioids for a few days or a week.[102]
Finally, pain affects not only terminal cancer patients. However, in Armenia patients who are still receiving outpatient curative treatment are not eligible for opioids; only terminal cancer patients who are referred for “symptomatic treatment” can receive opioids, and only after going through an extremely onerous process described in this report in chapter IV. Several medical personnel interviewed by Human Rights Watch stressed the prevalent belief in Armenia that opioids can only be prescribed to a dying patient for limited time.[103]
Some of the doctors interviewed by Human Rights Watch explained their reluctance to prescribe morphine out of fear that patients will become drug dependent. This fear was also expressed by some patients who refused higher doses of morphine. However, these fears are scientifically unfounded. The WHO treatment guidelines state that “wide clinical experience has shown that psychological dependence [drug dependence] does not occur in cancer patients as a result of receiving opioids for relief of pain.”[104]
IV. Medicines Availability
The WHO recommends that countries adopt a “medicines policy in order to ensure the availability of essential medicines for the management of symptoms, including pain and psychological distress, and in particular, opioid analgesics for relief of pain and respiratory distress.”[105] In 2013, the WHO created sections on pain and palliative care in its Model List of Essential Medicines and its Model List of Essential Medicines for Children. These sections contain medicines and specification for formulations that the WHO considers essential for pain management and palliative care. The 2014 World Health Assembly resolution on palliative care urges countries to “review and, where appropriate, revise national and local legislation and policies for controlled medicines, with reference to WHO policy guidance, on improving access to and rational use of pain management medicines, in line with the United Nations international drug control conventions.”[106]
Under the right to health, countries are required to ensure the availability and accessibility of all medicines included in the WHO Model List of Essential Medicines. The Committee on Economic, Social and Cultural Rights holds that providing essential medicines as determined by the WHO is a core obligation that cannot be limited by claims of constraints on resources, but that states should fulfill immediately.[107]
For an opioid analgesic to be available in Armenia (or any other country), the medication first needs to be registered. As noted above, oral morphine is currently not registered in Armenia and can thus not be imported, produced, prescribed, or sold. In fact, not a single strong oral opioid analgesic (except for methadone, which is used in substitution therapy for drug addiction) is currently registered in the country, meaning that these medicines are only administered by injection, which is inconsistent with WHO recommendations.
Table 4. Opioid Analgesics Registered in Armenia
|
Name |
Dosage, Prescription Form |
Recommended Use |
Producer |
Registration Date |
Valid through |
|
Morphine hydrochloride 1% solution for infusion |
10 mg/ml; (100/20x5/) 1 ml ampoule |
Management of moderate to severe pain |
“Zdorovye narodu”, Ukraine |
05/12/2011 |
05/12/2016 |
|
Omnopon-ZN (Morphine hydrochloride, papaverine hydrochloride, codeine, noscapine, thebaine) |
11.5mg/ml + 0.72mg/ml + 1.44mg/ml + 5.4mg/ml + 0.1mg/ml; (100/20x5/) 1 ml ampoule |
Management of moderate to severe pain |
“Zdorovye narodu”, Ukraine |
07/09/2012 |
05/12/2016 |
|
Promedol-ZN (Trimeperidine hydrochloride) |
20mg/ml; (100/20x5/) 1 ml ampoule |
Management of moderate to severe pain |
“Zdorovye narodu”, Ukraine |
07/09/2012 |
05/12/2016 |
|
Fentanyl |
0.05mg/ml; (100/20x5/) 2 ml ampoule |
Anesthesia |
“Zdorovye narodu”, Ukraine |
05/12/2011 |
05/12/2016 |
|
Tramadol, solution for injection |
100 mg/2ml; (5) ampoules 2ml |
Management of moderate pain |
CRCA, Novo Mesto, Slovenia |
27/03/2012 |
27/03/2017 |
|
Tramadol, solution for injection |
100mg/2ml; (5) ampoules |
Management of moderate pain |
Hemopharm AD – Serbia |
14/09/2011 |
14/09/2016 |
|
Methadone Oral Tablets (Methadone hydrochloride) Tablets, USP |
5, 10, and 40 mg tablets |
Used in substitution therapy for drug addiction; also in 2012 it was used at palliative care pilot sites for pain management. |
Mallinckrodt Inc., USA |
26/11/2014 |
26/11/2019 |
Barriers to the Accessibility of Opioid Medications
Armenia’s drug regulations are at the heart of problems with availability and accessibility of palliative care and pain management identified in this report. The procedure for prescribing opioids is complex, time-consuming, and involves significant bureaucracy.[108] Only oncologists may prescribe opioids to outpatients, and only to cancer patients. Pharmacies and polyclinics that dispense opioids do so free of charge but must install costly security measures at their own expense. Police control over the prescription and dispensing process is tight, invasive, and generates a sense of trepidation among oncologists and pharmacists.
Such onerous regulations appear to contribute to the reluctance among many oncologists to prescribe opioid pain medication. As one former Health Ministry official explained, “One of the main problems in our system is that doctors are afraid to prescribe opioids or prescribe [inappropriately] low dosages.”[109]
This excessively restrictive and non-evidence based approach to dosage also negatively affects demand for strong pain medication and impedes suppliers from importing more opioids or registering oral opioids, as the demand is highly unpredictable.[110] According to Arpharmacia, the only company that imports injectable morphine, the usage of morphine in the country has been declining in the past five years.[111]
Limiting Prescribing of Opioids to Oncologists and Cancer Patients Only
Under regulations issued by the Health Ministry in 1994, only oncologists at local polyclinics can prescribe opioid medicines for outpatients with cancer.[112] The directive clearly states that only cancer patients under the supervision of polyclinics could be prescribed opioids and provides detailed instruction on the prescription process.[113]
In 2002 Armenia passed a revised law “On Narcotic Drugs and Psychotropic Substances,” which sets out a broad framework for the release of such medications for medical use, and authorizes the government to establish the procedures for doing so.[114] However, all oncologists interviewed by Human Rights Watch said that they follow the 1994 regulations.[115] Indeed, Human Rights Watch was not able to identify any implementing regulations pursuant to the 2002 law that have changed the opioid prescription process as it is described in this report.
The 1994 regulations exclude patients with moderate or severe pain due to diseases other than cancer from receiving these medicines. Even the palliative care pilot projects described elsewhere in this report could not prescribe opioids for the 13 participating non-cancer patients who reported moderate to severe pain.[116] As noted above, moderate to severe pain is a common symptom in numerous health conditions other than cancer and the legal ban on prescribing opioid analgesics to outpatients with these conditions condemns thousands of Armenians to needless suffering each year.
Equally problematic is the unusual provision that limits prescribing of opioid analgesics to oncologists only. A 2009 study on opioid regulations in 43 countries in Europe, which did not include Armenia, found that only Montenegro and Ukraine restricted prescribing of opioids to oncologists.[117] Human Rights Watch interviewed several physicians, including anesthesiologists, who teach students and train oncologists on pain management, but who themselves are not authorized to prescribe opioids to outpatients.[118]
Armenia’s restrictive regulation goes against WHO guidance on nationally controlled substance policies, which says that “when balancing drug control legislation and policies, it is wise to leave medical decisions up to those who are knowledgeable on medical issues.” In other words, medical professionals should make clinical decisions on what medications to prescribe to what patients. The guidance also holds that “countries should ensure that availability and accessibility of controlled medicines is addressed for the following disease-specific policies: cancer control, HIV/AIDS, and mental health.”[119] Furthermore, the WHO guidance stipulates that “access to controlled medicines should not be restricted to the above groups only.”[120]
Requirement of a Biopsy-Confirmed Cancer Diagnosis
As noted above, polyclinic oncologists are responsible for registering cancer patients and providing curative or symptomatic treatment. However, in order for a local polyclinic to register cancer patients, and therefore be able to eventually prescribe strong opioid analgesics, the health care system must first confirm their diagnosis through a biopsy. In other words, a diagnosis based on clinical observation is not sufficient to initiate pain management with opioid analgesics. This highly unusual requirement condemns thousands of cancer patients to unnecessary suffering.
Only three institutions, the National Oncology Center in Yerevan and two oncology dispensaries in the towns of Gyumri and Vanadzor, have the necessary equipment and specialists to establish such diagnosis. In practice this means that in order for patients to receive opioid medication they must go to one of these three centers to have their diagnosis confirmed.
This puts patients living in remote rural areas in a particularly strenuous situation when they need strong pain medication. A doctor in Dilijan, a town about 95 kilometers northeast of Yerevan, explained that a patient is first examined by a general practitioner, who then refers him or her to a local oncologist. If the latter establishes a clinical diagnosis or a suspicion of cancer, the patient is re-directed to the National Oncology Center in Yerevan, where the diagnosis needs to be confirmed before the patient is registered as a cancer patient at a local polyclinic.[121]
Almost half of Armenia’s cancer patients are at stage three or four of the disease when they receive their initial diagnoses, and many are not able to travel to one of the oncology centers to be formally diagnosed. A doctor in Armavir Marz, a province about 60 kilometers west of capital Yerevan, told Human Rights Watch about a patient he was treating for pancreatic cancer who needed opioids for pain management. However, the patient was too weak to travel or be transported to Yerevan and could thus not be officially registered as a cancer patient. As a result, the doctor could not prescribe opioid analgesics and the patient remained in pain.[122] He also recalled a story of another patient who required opioids but could not travel to Yerevan. The doctor called a conference of specialist doctors in his clinic to try to get around the requirement of a confirmed diagnosis but was not allowed to prescribe anything stronger than tramadol, an opioid analgesic that is generally not sufficiently potent to treat severe pain.[123]
Human Rights Watch spoke to an 84-year-old woman, Amalya A., in the town of Myasnikyan who had severe pain in the stomach area but was unable to make the 60 kilometer trip to Yerevan to be diagnosed. She told Human Rights Watch that she started to develop pain in summer 2012: “The pain lasts for three to four hours at a time, I can’t sleep most nights, I can’t even turn from side to side, it hurts so much.”[124] She explained that she cannot afford the trip to Yerevan: “We have to pay for a cab, then in the Oncology Center for the medical history, pay doctors at various places, tests, exams, etc… we don’t have such money.”[125] She was using various over-the-counter analgesics, but they helped only enough for the pain to become bearable for short period of time, without ever fully going away. Amalya’s doctor, who operated on her a year earlier, told Human Rights Watch that he knows that she requires opioids, but he cannot prescribe them without the confirmed diagnosis.[126]
As noted above, of 5,581 patients who died of cancer in 2013, 1,274 were diagnosed post-mortem, according to the data provided by the National Oncology Center. None of these people received a formal confirmed diagnosis yet a large percentage of them are likely to have had serious pain.
Armenia should not restrict opioids to cancer patients only or require a biopsy-confirmed diagnosis. A determination by a physician based on a clinical examination of the patient should be sufficient to prescribe opioids.
Onerous Prescription Procedure
In Armenia the procedure for prescribing opioids is complex, time-consuming, and involves significant bureaucracy. Article 6 of the 1994 Health Ministry directive regulates opioid prescriptions for oncology patients. It requires any doctor who wishes to prescribe opioids to first secure approval from a standing commission consisting of the patient’s oncologist, the polyclinic’s chief and/or deputy chief doctor, chief nurse, general practitioner, and in some cases one or two other specialized doctors who work at the clinic. Once a patient has been on regular analgesics, followed by psychotropic pain medication, and pain persists, the commission visits the patient at home and decides whether to prescribe opioids. The standing commission’s decision must be in writing, must include the name of the medication and dosage, and must be recorded in a special journal and also transferred to the patient’s medical record.[127] While countries like Russia and Ukraine also require a commission to sign off on prescriptions, those commissions are smaller—the treating physician and the chief or deputy chief of the clinic in Ukraine, for example—and there is no requirement to visit the patient at home.[128] According to Professor Lukas Radbruch, a leading German palliative care physician and president of the International Association for Hospice and Palliative Care, all European Union countries allow physicians to prescribe opioid analgesics individually.[129]
The standing commission’s approval is required for any change in the patient’s prescription, and, according to the regulation, the commission can issue such an approval only after it has examined the patient. Human Rights Watch found that there is some variation in practice across the country. At least one oncologist said that she could change the dosage if necessary without the standing commission’s repeat visit; but the commission would still need to approve it formally.
Opioid prescriptions are issued on a special form approved by the government of Armenia and must have four separate stamps.[130] The form itself must bear the Health Ministry’s stamp. The oncologist who writes the prescription signs and stamps it with his or her personal stamp.[131] The prescription must also include the prescription stamp, the signature and stamp of the chief or deputy chief of the institution, and the round seal of the facility.
If a patient receiving opioids enters in-patient care either for specialized or symptomatic treatment, the clinic stops issuing opioid prescriptions because the patient would get opioids through the hospital or other inpatient facility.
The standing commission’s decisions on when opioids are needed for pain management are arbitrary at best. In one case documented by Human Rights Watch, an oncologist in Yerevan polyclinic recalled that the standing commission refused to prescribe a stronger opioid because a patient spoke too loud: “We had a case not long ago—a patient thought tramadol was not helping anymore and was asking for a stronger pain medication. The commission went to his place and gave him tramadol first to see whether it was indeed insufficient. He spoke so loudly that we thought it was too early to give him that ‘filth’ [opioids].”[132]
Several medical personnel interviewed by Human Rights Watch said that they would welcome a simpler prescription procedure that was less time-consuming for all involved and required fewer forms and reports to file. “Sometimes the procedures are so burdensome and take such a long time that by the time it is all cleared there is no need for it anymore. Needs are great for pain medications like opioids, but the amount of paper-pushing associated with it is not often worth it.”[133]
Because the prescription procedure is so onerous, patients sometimes die in agonizing pain before opioids are prescribed. Human Rights Watch interviewed Anahit Garibyan, whose 79-year-old father, Sergey, died in September 2012, a month after he was diagnosed with a stage four lung tumor. As his condition deteriorated rapidly, over-the-counter painkillers did not help. Anahit’s attempts to obtain a prescription for an opioid analgesic for him were unsuccessful, and her father died before a standing commission could visit and assess him. She explained:
My father was in agonizing pain. He kept screaming for six or eight hours before he died. His voice got weaker as the hours went by. The pain affected him a lot; he did not want to see anyone, including grandchildren. We called an ambulance, but they could not help much as they could only administer dimedrol [a weak painkiller] injection, which did not do much. It just so happened that it was a weekend and Monday was also a public holiday, and our oncologist was off on Tuesday. When I went to see him on Wednesday, he told me that it was not that easy to prescribe opioids, and that a standing commission was to visit him first. When I asked him to initiate the process, he told me that a tramadol injection should be prescribed first, which I got, but it did not help much, and he died in pain.[134]
Anna A., whose uncle died of a stomach tumor in summer 2014, shared a similar story. When her uncle developed severe pain, he was already immovable, so Anna, herself a medical professional, tried to collect all the necessary documents to request an opioid prescription from an oncologist at a local clinic. She managed to obtain a written diagnosis from the National Oncology Center confirming that her uncle’s condition was inoperable and incurable, and recommending symptomatic treatment. She took the written confirmation to a local oncologist, explaining that her uncle was in severe pain and regular painkillers were not effective. The clinic’s oncologist told her that the standing commission would be able to visit in three to four days and that meanwhile she should try over-the-counter pain medication. Meanwhile the pain persisted, and he died before the commission could visit him.[135]
Recordkeeping
Prescribing opioid medications in Armenia also involves a significant reporting burden for oncologists. They must record each opioid prescription transaction in several different registries, including one that must be kept in a fireproof safe.
A 2002 Ministry of Health Decree regulates the procedure for writing prescriptions for opioid analgesics, including the procedure clinics must follow to maintain records on each opioids prescription they issue. The decree states:
To account for narcotic drug prescriptions, a book shall be kept, where the following data shall be recorded: entry order number, date received, place received from, serial number, quantity, administration, to whom it was given (patient’s first, middle, and last names), the patient’s medical record number, content of the prescription, serial number of the prescription, and signature of the person collecting the prescription. Pages of the book shall be numbered, stamped and verified by the stamp and signature of the institution’s director. The content of the opioid prescription and its serial number should also be recorded by the physician in the patient’s medical record. Unused prescription forms shall be kept in metallic fireproof safe.[136]
Many oncologists interviewed for this report said that the recordkeeping requirements for opioid prescriptions were onerous. As noted by one of the oncologists, “It feels like all we do is write various documents, fill various journals and registries, leaving less time for actual patient care.”[137]
Dispensing of Opioids
Once opioids are prescribed, patients with a life-limiting illness or their caregivers must go to the clinic to collect the prescription with its four different stamps, fill it at a specialized pharmacy, and return the empty ampoules before a new prescription is issued. They must repeat the process every other day or in some cases every day because in practice doctors will prescribe only enough opioids to last 24 or 48 hours (see below). Although most oncologists Human Rights Watch interviewed prepare the prescriptions in advance or have a nurse help a relative in collecting all the necessary stamps, the whole process can take several hours. This represents a serious burden for family members of a patient with life-limiting illness.
In Yerevan only one pharmacy fills opioid prescriptions. Elsewhere in Armenia patients can fill such prescriptions at the prescribing polyclinic, which is usually located in larger medical centers.
As noted above, if opioids are prescribed they are dispensed free of charge.
Government regulations governing how long opioid prescriptions are valid for are inconsistent. The 2001 government decree regulating prescription forms envisages a 20-day validity period.[138] But the 2002 law “On Narcotic Drugs and Psychotropic Substances” sets out a validity period of 10 days for opioid prescriptions. The 2002 law does not explicitly state that it annuls the 2001 governmental decree. And in practice, pharmacists at the Arpharmacia, the only company that imports injectable morphine, fill opioid prescriptions only if they are written the same day.
Lyudmila, the retired kindergarten teacher cited above, who was diagnosed with breast cancer in 2002 and developed severe pain in 2010, was receiving one ampoule of omnopon at the time Human Rights Watch visited her in 2012. Although opioids provided short relief from severe pain, obtaining it every other day was a challenge for her and her family:
It’s very inconvenient. Somebody has to go to a polyclinic every other day to return empty ampoules, get a new prescription and then fill it in a different pharmacy. It takes several hours. Today, I had no one to go for me and I had to do it myself. My doctor was shocked to see me, but what could I have done? I wish it was possible to do this at least once a week instead of every other day.[139]
One oncologist told Human Rights Watch that when she explains the procedures for obtaining and filling prescriptions for opioid analgesics to patients’ relatives, they sometimes decide against them because they simply do not have enough time or the money to pay for transportation.[140]
Patients, their families and oncologists said these onerous procedures were taking a heavy toll on patients’ family members. One oncologist from a Yerevan suburb recalled a patient whose daughter had to quit her job in order to have enough time to keep her dying mother’s pain prescriptions filled. She had to go to the polyclinic every other day to return the empty ampoules, get a new prescription and then go to the special pharmacy in Yerevan to fill the prescription. The entire process took three to four hours each day. There was no one else who could take care of her mother, which meant that the mother was unattended while the daughter was out getting the pain medication.[141] The oncologist said:
It’s an extremely difficult procedure to get opioids. We write the prescription every other day [to last] for two days. It usually takes 15 to 20 minutes for a patient’s relative to get to the polyclinic from the neighborhood, another 20 minutes or so to return the ampoules, get a new prescription with all its stamps and then about an hour to get to central Yerevan, where the pharmacy is located, and then [another hour] back home. All of it can be at least three hours, plus transportation costs, which can often be an additional burden.[142]
In one case documented by Human Rights Watch, a doctor recommended that her patient not send her 20-year-old son to collect the prescription because he was considered too young to handle opioids. Her son was allowed to return empty ampoules, but her sister had to step in to collect the prescription and get it filled.[143] In the town of Ararat, about 50 kilometers south of Yerevan, prescriptions for opioids are issued for just one day at a time, except on Fridays, when a three-day dose is prescribed. Even though the prescriptions are filled in the same medical center as they are issued, some patients’ family members still find the entire process onerous and unnecessarily time-consuming. The husband of one patient said that he spent about an hour every day dealing with his wife’s pain prescription, which meant leaving his wife unattended during the time he is gone.[144] He said he would find it extremely useful if he could pick up a weekly dose and even tried to convince the local police chief to allow him to do so, but without success.[145]
In Gorisi, a town 254 kilometers south of Yerevan, opioids prescriptions are also issued only for one day at a time and they must be filled the same day they are issued. Some of the medical personnel Human Rights Watch spoke to justified the need for tighter control by pointing to the fact that there is a closed penitentiary institution located in the district. The need for strong pain medications appears to be especially high in Gorisi than in other locations because more than twice as many oncology patients are registered in the region than in other parts of Armenia.[146]
Most oncologists Human Rights Watch spoke to said that opioids are prescribed at the last stage of life and almost never longer than one month. The Gorisi clinic chief doctor confirmed this, saying that was the result of the amount of paperwork required and the fears of oncologists prescribing these medications.[147]
The chief doctor also acknowledged particular difficulties patients and their family members face in remote rural areas, as opioids are stocked only in regional medical centers. Small local health clinics – known as ambulatoria – and even small hospitals do not have the license that is required to stock and prescribe strong opioids analgesics. This means that patients or their relatives often have to travel long distances to the regional centers, frequently on poor roads with limited public transport, to obtain and fill prescriptions for strong pain medications. In one exception to the regular practice, the Gorisi chief doctor said he authorized a family doctor from a remote village to collect a weekly dose of strong opioid analgesics and then issue it daily to a patient in that village.[148]
A doctor from Armavir province, about 70 kilometers west of Yerevan, explained that the farthest village from the regional center of Myasnikyan, where opioid prescriptions are issued and filled, is about 43 kilometers away. There is a bus twice a day at 9 a.m. and 1 p.m., but it would be difficult for someone to get to the town every other day, particularly in inclement weather.[149]
Human Rights Watch also visited the town of Gyumri, about 130 kilometers northwest of Yerevan, with a population of 250,000. Gyumri has five polyclinics and an oncology dispensary, which diagnoses and treats cancer patients. However, local polyclinics did not have an oncologist on staff when Human Rights Watch visited. Instead, an oncologist from the dispensary participated in the standing commissions maintained in those polyclinics for the purpose of approving opioid prescriptions. Patients or their caregivers had to first collect a prescription from the dispensary, then go to the polyclinic, obtain necessary stamps, and then fill it at a separate pharmacy.[150]
Armenia’s practice of issuing prescriptions for opioid analgesics for just one or two days at a time is one of the most restrictive dispensing regimens in all Council of Europe member states. The 2009 study on opioid regulations in Europe found that of the 41 countries for which dispensing information was collected, 27 allowed prescribing of opioid analgesics for 28 days or more per prescription; 5 for 10-15 days; and 9 for 7 days or fewer.[151] Russia, Ukraine, and Albania which allowed prescribing for 5, 1, and 7 days respectively, have since increased the dispensing period to 15 days in Russia and Ukraine and 28 days in Albania.
Onerous Licensing Procedures
Although all central district hospitals are licensed to dispense opioids for inpatients, only one pharmacy in Yerevan and a few regional clinics with pharmacies, mostly in regional centers, are licensed to fill opioids prescriptions for outpatients. Few health clinics and pharmacies seek the relevant licenses because of the paperwork required and the cost of the security measures required by law to prevent break-ins and theft. Since the state provides opioids free of charge and pharmacies and clinics must bear the costs of installing and maintaining security equipment, they have little incentive to seek the license. Scrutiny by police and potential criminal liability may further serve to dissuade pharmacies and clinics from seeking licenses. One pharmacy official described the anxiety experienced by health care personnel dealing with opioids, “you lose one ampoule and prison is waiting for you….”[152]
Government regulations issued in 2010 require pharmacies seeking a license to store and dispense opioids to have a storeroom with an iron door and windows with iron grids; a fireproof iron safe welded to the floor and wall; the storeroom should also have a humidity meter and audio or light alarm system with a backup energy supply system.[153]
The chief doctor at the Gorisi central district hospital explained the cost and other onerous requirement for obtaining the license:
We need to collect a pile of documents, including 16 different certificates and reference documents… We pay US$1,500 a year for an alarm system directly linked to police; the safe in a separate room and other things… This is a headache.[154]
The owner of the only pharmacy in Yerevan that fills opioids prescriptions told Human Rights Watch that he spends over US$2,000 a month on security.[155]
While Armenia clearly has a right—even a duty under the 1961 Single Convention on Narcotic Drugs—to regulate the handling and storage of opioid analgesics, it must also ensure that its regulatory requirements do not needlessly or disproportionately impede the availability of these essential medicines. The requirements described above clearly constitute a significant impediment to their availability and should be reviewed to ensure a proper balance is found between safeguarding these medicines and ensuring their availability.
Tight Police Control
Police in Armenia exercise an extraordinary level of control over the prescription process of opioid analgesics. The specific control practices, which vary somewhat from region to region, are not provided for under Armenian law. While police and other law enforcement bodies have a legitimate interest in ensuring opioid analgesics do not enter black markets, they may not interfere with proper medical practice or routinely require confidential medical information on patients who receive opioid analgesics from hospitals, clinics or pharmacies.
All oncologists Human Rights Watch interviewed said that they provide written monthly reports to the police about patients who receive opioid analgesics. Such reports include the patient’s name, address, ID number, diagnosis, prescribed dosage and the name and other information of the person who picks up the prescription and fills it. Pharmacies that fill opioid prescriptions also send police written reports with similar information. Police also conduct irregular, informal inspections at polyclinics, participate in destruction of full ampoules and sometimes also of empty ampoules. The routine reporting of the names of patients who receive opioid analgesics violates the right to privacy and is a breach of confidentiality which is an integral aspect of the right to health.[156]
An oncologist in one of Yerevan’s polyclinics explained: “We provide monthly reports to the district police department about patients who are prescribed opioids, including their diagnoses, dosage, addresses, and information about the family member picking up the prescription.”[157] All of the 17 oncologists Human Rights Watch spoke with in Yerevan and other parts of Armenia said they followed the same procedure.
One oncologist said that she informs police on each patient, and sends another report if the prescription dose has changed: “As soon as I prescribe narcotics, I inform the pharmacy and police in writing that an individual at this address gets narcotics and the dosage. I also inform about the dosage change.”[158]
One doctor told Human Rights Watch that she felt uncomfortable about these police reports as she did not know legal basis for submitting such information and felt it was not appropriate to divulge confidential patient information. In 2011 she even tried to stop the monthly reports, but started them again after police asked her to do so: “When they [police] asked me why I stopped submitting reports, I told them that they had to officially request this information, which they did and I had to renew submitting the information based on their written request sent on the name of the clinic director.”[159]
Police also inspect institutions that fill opioid prescriptions.[160] According to one pharmacy employee, police regularly check prescriptions the pharmacy fills.[161]
Patients’ caregivers must return empty opioid ampoules to the polyclinic that issued the prescription. As a matter of practice, staff generally destroy the empty ampoules every 10 days or so.[162] Unused ampoules that remain after a patient passes away must be destroyed in a separate process.[163] A 2010 government of Armenia decision requires the police to be present when full ampoules are destroyed.[164] Staff at several polyclinics told Human Rights Watch that police also are present to observe the destruction of empty ampoules and ensure that the serial number on the ampoule matches the ampoule number recorded in the pharmacy’s journal.
A doctor in one of Armenia’s regions told Human Rights Watch that police come every 10 days to the clinic to check all journals that contain information about opioid prescriptions and witness the destruction of empty ampoules. The doctor felt police did not trust physicians, and that this perception makes them less likely to prescribe opioids:
Doctors are not trusted here. No one wants to work as an oncologist and those who do, prefer not to prescribe opioids, as they don’t want to deal with police. Why should police be controlling us?[165]
He further explained that in his medical practice he had prescribed several ampoules for an extended period of time, which resulted in a patient with a life-limiting illness leading a normal life, working, and playing with his grandchildren. “Police were extremely surprised and came to me asking how come that person was getting opioids when he was walking around and playing with grandchildren. I had to argue and explain that I did nothing criminal, but not every doctor would want to deal with the police in such a manner,” he said.[166]
Several doctors thought that informing police was necessary to prevent the illicit spread or use of narcotics. For example, a doctor in Dilijan told Human Rights Watch: “We are interdependent of police and regularly submit reports about narcotic prescriptions. We are not pressured, we just cooperate voluntarily and I think this is good as it allows for better control.”[167]
Police perspective
Police officials told Human Rights Watch that they did not think police exercised excessive control over physicians and medical institutions that prescribe and dispense opioids. They said that the Health Ministry was in charge of this and characterized the police role as only monitoring to ensure that patients or their relatives are not abusing drugs or illegally selling them.[168] They explained that while police participate in the destruction of ampoules, they try not to bother medical institutions with unannounced inspections unless they receive reports about criminal activity. The deputy police chief of Armenia said that in the last two years police had not found a single case of abuse of opioids in the health care system, and attributed this to the control police exercised.[169] Regarding the mandatory reporting process, including private medical information on patients, the police official responded that they merely keep record of all the reports: “When a person is prescribed opioids, we get a notice, including the name of an individual. […] Even if we get information on diagnosis, we don’t need it, we don’t spread it.”[170]
The right to respect for confidentiality of medical information is a core principle of the right to health. The UN Committee on Economic, Social and Cultural Rights has advised states that while “accessibility of information” is an aspect of the right to health this “should not impair the right to have personal health data treated with confidentiality” and in terms of acceptability that “[a]ll health facilities, goods and services must be … designed to respect confidentiality”.[171] This right is also separately protected as an aspect of the right to privacy under the European Convention on Human Rights and Fundamental Freedoms (ECHR) and the International Covenant on Civil and Political Rights (ICCPR), to both of which Armenia is also a party.[172]
While collection of statistical data about opioid prescription might serve an important and legitimate purpose, the evidence collected for this report suggests that in many polyclinics oncologists routinely disclose specific information on patients to law enforcement agencies, which contains confidential and private medical information, including a person’s diagnosis. While the right to privacy does not establish an absolute rule of confidentiality of medical information, interference with this rule or breaches of it must be strictly justified, which is not the case of the practice of reporting opioid patients in Armenia.[173]
Given that medical data may be highly intimate and sensitive in nature, the necessity for any state measure compelling communication or disclosure of such information without the consent of the patient must be carefully scrutinized and convincingly established.[174]
Barriers to Introduction of Oral Opioids
The process of registering oral morphine in Armenia has been stalled for at least five years. Introducing oral morphine in Armenia requires a significant investment of funds and resources on the part of importers and manufacturers, yet the government is the only entity that can purchase from the importer and dispense a sufficient amount of opioid analgesics to health care facilities. To date, however, the government is not willing to commit to purchase a certain amount of oral morphine if Arpharmacia imports it.
The director of Arpharmacia, Stephan Avanesyan, told Human Rights Watch that he has been interested in having oral opioids registered in and imported to Armenia since 2010.[175] Yet, without a government commitment to purchase a certain amount of imported oral morphine, he explained, it does not make business sense for Arpharmacia to register and import it, or for manufacturers to go through the bother of gathering information necessary to submit the registration dossier. “If the government does not purchase the medicine before it expires, I would risk losing my investment.” Considering that medical use of opioid analgesics has been declining steadily in the past eight years Avanesyan is doubtful that registering and importing oral morphine will be commercially viable.[176] To illustrate the risks an importer runs, Avenesyan explained that in about 2009 Armenia registered and imported Fentanyl patches, plasters that release the opioid analgesic through the patient’s skin, but the entire supply had to be fully destroyed as it was not used.[177]
In contrast, the government cited a lack of interest among manufacturers. Hakob Topchyan, the head of the state institution in charge of registering medicines in Armenia, told Human Rights Watch that his agency was ready to consider registration requests from manufacturers for oral morphine but that none have filed a formal dossier requesting the registration.[178]
Under international human rights law, it is the duty of governments to ensure the availability of medications that are included in WHO’s Model List of Essential Medicines. If they fail to do so, they violate the right to health. Armenia’s government thus needs to make arrangements to ensure oral morphine becomes available, either by importing it directly or ensuring conditions exist for pharmaceutical suppliers to do so.
V. Education/Training of Health Care Workers
Lack of knowledge among health care workers about palliative care and pain treatment services is one of the biggest obstacles to palliative care in many countries around the world. A dearth of training on the topic means that many health care workers do not fully understand palliative care or have the skills to provide it and subscribe to a variety of myths and misconceptions about strong opioid analgesics.
The Committee on Economic, Social and Cultural Rights considers appropriate training of health care workers an obligation of key importance.[179] Accordingly, the WHO recommends that “education about palliative care (including ethical aspects) is offered to students in undergraduate medical and nursing schools and to health care providers at all levels…”[180] The May 2014 World Health Assembly resolution calls on countries to include palliative care as an “integral component of the ongoing education and training offered to care providers” and specifies:
- basic training and continuing education on palliative care should be integrated as a routine element of all undergraduate medical and nursing professional education, and as part of in-service training of caregivers at the primary care level, including health care workers, caregivers addressing patients’ spiritual needs and social workers;
- intermediate training should be offered to all health care workers who routinely work with patients with life-threatening illnesses, including those working in oncology, infectious diseases, paediatrics, geriatrics and internal medicine; and
- specialist palliative care training should be available to prepare health care professionals who will manage integrated care for patients with more than routine symptom management needs.[181]
The European Association for Palliative Care (EAPC) has developed a model curriculum for undergraduate and specialist palliative care training. It recommends that undergraduate medical students receive 40 hours of training in palliative care and pain management, including some clinical aspects of palliative care, and should be tested on their knowledge of the subject matter.[182] They also recommend that specialists receive an additional 40 hours of theoretical training and 160 hours of clinical training after specializing in another field, such as internal medicine.[183]
At present, doctors specializing in oncology or anesthesiology in Armenia receive no practical exposure to palliative care and pain management. Almost all health care practitioners interviewed for this report said they had received no training in conveying grave diagnoses or holding end-of-life discussions. Most were unaware or only partially aware of international best practices for pain treatment, particularly with regard to opioid-based pain medications.
Many doctors and nurses expressed the erroneous belief that giving patients morphine would turn them into “drug addicts”; confused physical dependence and tolerance with dependence syndrome (addiction); interpreted patient requests for more morphine as a sign of “addiction” without considering the real possibility that the current dose was insufficient; and believed that one dose of morphine could provide relief far beyond the four to six hours it is active, particularly if combined with other over-the-counter painkillers.
Education and Training
Since at least 2012 independent groups have been providing palliative care and pain management trainings for oncologists in Armenia, but it is neither systematic nor mandatory. The mandatory curriculum in medical schools does not include any specific instruction on palliative care. There are no palliative care residency or fellowship programs in Armenia that would lead to specialization in palliative care, although the ministry of education and science plans to integrate palliative care into training curriculums.
The Armenian Pain Control and Palliative Care Association, a professional association, has organized a number of optional trainings in Yerevan hospitals and regional medical centers, including courses on introduction to palliative care, pain management in palliative care, control of symptoms, and nursing in palliative care.[184]
Professors at Yerevan State Medical University, the leading medical educational institution in Armenia, Narine Movsesyan and Artashes Tadevosyan, in close cooperation with the university management, and supported by the Open Society Institute Assistance Foundation Armenia, have been developing a curriculum on palliative care and planning to establish an education and training center with opportunities for clinical placement. The university plans to offer its first courses on palliative care in the 2015 autumn semester for students concentrating on general practice and to recruit the first cycle of physicians for a 60 hour continuing medical education course.
In September 2014, the government of Armenia approved the creation of a sub-specialization in palliative care in the national health system. However, it still needs to develop professional qualification requirements for a palliative care sub-specialization and then introduce it into the education system. The Armenian government’s action plan in palliative care envisages the creation of a palliative care specialization, which would require approval of the Ministry of Education.
All Armenia’s medical and nursing schools are public institutions that operate under the auspices of the Ministry of Education and Science. The government is thus clearly in a position to ensure that adequate instruction on palliative care is provided. Human Rights Watch believes that all medical and nursing students should receive basic instruction on palliative care and pain treatment. Those who specialize in disciplines that frequently care for people with life-limiting illnesses should be required to receive detailed instruction, including exposure to clinical practice.
Misconceptions about Pain Relief Medications
Lack of education and training is likely one of the key reasons why many doctors interviewed for this report held erroneous notions about the correct dosages and effects of opioid-based pain medications. Some doctors said they believed that giving patients morphine would turn them into “drug addicts.” For example, one oncologist told Human Rights Watch: “Some patients refuse it [opioids]; others want to start it sooner. We have to be careful not to make them drug dependent.”[185] Another physician called morphine “filth.”[186] A third oncologist, who despite over 10 years of clinical experience had not heard of the WHO principles on pain management, told Human Rights Watch that she prescribed opioid analgesics based on her “intuition” rather than the severity of the patient’s pain.[187]
Several oncologists said they believed opioids are supposed to be prescribed only for a patient’s last days, and felt anxious if the patient survived for months after opioids had been prescribed.
Communication of Diagnosis – Conspiracy of Silence
Human Rights Watch found that most oncologists in Armenia do not discuss a diagnosis and prognosis with their patients. This lack of communication with patients, particularly when the prognosis is grave, reflects the absence of training in palliative care. All oncologists stressed to Human Rights Watch that they had no training in holding difficult conversations with patients suffering from life-limiting illnesses, and feared that they would not be able to guide patients after communicating a diagnosis or prognosis.
Almost all oncologists interviewed by Human Rights Watch said that they never discuss the diagnosis with a patient, and that they instead either withhold the truth or strongly mitigate it. They explained that they did not want to take away their patients’ hope or cause them severe distress. At the same time, doctors always inform the patients’ families, while keeping the patient in the dark, often resulting in a “conspiracy of silence.” In some cases, families request physicians not to share the diagnosis or prognosis with the patient. Some doctors told Human Rights Watch that they are not open with their patients even when directly asked. They also said that they believed many of their patients can tell they are withholding information.
For example, an oncologist in one of Yerevan’s polyclinics told Human Rights Watch: “I never tell patients their diagnosis. The patients of course know, they can tell, but no one talks about it. If I am asked directly by a patient, I still don’t tell the truth, I will just say that it’s a post-surgery situation and that he’ll recover soon. We have no training in how to hold a difficult conversation.”[188]
Another oncologist explained that she had no special training in communicating a difficult diagnosis and preferred for it to be done by a special service: “I never tell the patients about their diagnosis. I think everyone knows everything, including the patient and their relatives, but I never tell them. I talk to them only on a positive note. Sometimes I feel like a psychologist talking to them. If there were a separate service, that would talk to the patients, that would be good.”[189]
Another oncologist in Yerevan told us: “I don’t think patients are interested in knowing their diagnoses. They often ask how long they have left to live. I don’t respond to that, just tell them that they are fine, that they will live and that they should think positively.”[190]
Several oncologists told Human Rights Watch that they felt they “prolong patients’ lives by withholding the truth.”[191] Others said that they did not share “bad news” out of fear of a potential misdiagnosis.[192] Several physicians told Human Rights Watch that they find it particularly difficult to deal with the family members. “It’s sometimes easier for me to work with terminal patients than their relatives and their questions.”[193] She also stressed the need for additional training in how to hold difficult conversations with the patients and their families.
While physicians may withhold information about diagnosis or prognosis from patients or even misrepresent the facts in an attempt to protect them or because of their own lack of skill communicating bad news, the result is that patients are left to suffer alone, often consumed by doubt and worry, unable to ask questions and find answers, and maybe even deprived of the chance to say goodbye to their loved ones or put their affairs in order. This practice runs directly counter to the essence of palliative care, which regards dying as a normal part of the life cycle and seeks to help people who are dying maintain the best possible quality of life. This includes helping them and their families cope with the consequences—physical, psychological, social and spiritual—of life-limiting illnesses, including the prospect of death, and addressing the doubts and worries they and their families may have.
WHO emphasizes the importance of psychosocial support for patients and their families.[194]
Under international human rights law, patients with advanced or terminal illness have a right to receive full and accurate information about their diagnosis and prognosis. [195] Likewise, they have a right to participate in decision-making regarding their own health care and to psychological support. Withholding information about the diagnosis and prognosis impedes the exercise of these rights. When a patient specifically requests such information and it is withheld, it constitutes a violation of the right to health.
Breaking Bad News to Patients and FamiliesSharing bad news with patients may be the hardest part of a physician’s job, especially when it involves life-threatening illness. Many physicians do not feel adequately prepared for the task or fear distressing and adversely affecting the patient, family, or the therapeutic relationship. Instruction on communicating bad news is often limited in medical schools as is clinical exposure during training. Yet, sharing bad news is an essential skill—as well as an ethical duty—for physicians. When done in a direct and compassionate way, a leading palliative care training curriculum states, it can “improve the patient’s and family’s ability to plan and cope, encourage realistic goals and autonomy, support the patient emotionally, strengthen the physician-patient relationship, and foster collaboration among the patient, family, physicians, and other professionals.”[1] The Education in Palliative and End-of-Life Care curriculum, which has been used to train palliative care physicians in dozens of countries, recommends a six-step approach to sharing bad news:
[1] L.L. Emanuel, F.D. Ferris, C.F. von Gunten, and J. Von Roenn, “Communicating Effectively”, EPEC-O (Education in Palliative and End-of-life Care for Oncology) curriculum materials, module 7, (EPEC Project: Chicago, IL, 2005), http://www.ipcrc.net/epco/EPEC-O%20M07%20Communicating/EPEC-O%20M07%20Communicating%20PH.pdf (accessed June 22, 2015). 2 Ibid. |
VI. Government Reforms and Gaps in Palliative Care Policy in Armenia
The World Health Organization has urged countries to adopt policies that support pain relief and palliative care, including the introduction of educational programs for the public, health care personnel, regulators, and other relevant parties; and to modify laws and regulations to improve the availability and accessibility of drugs, especially opioid analgesics, noting that these measures “cost very little but can have a significant effect.”[196]
The WHO’s recommendations correspond closely with several core obligations under the right to health, which countries must meet regardless of resource availability. The UN Committee on Economic, Social and Cultural Rights, holds that countries must adopt and implement a national public health strategy and plan of action and to ensure access to essential drugs as defined by the WHO.[197] It has identified providing appropriate training for health personnel as an obligation “of comparable priority.”[198]
The Armenian government has taken some steps towards complying with these recommendations but has a long way to go before it meets them. The government has clearly recognized the need for palliative care. In 2009 palliative care and services were for the first time included in the government’s list of recognized medical services.[199] In 2010 the government established a palliative care working group, consisting of relevant government agencies and expert civil society groups, which developed a national concept paper and strategy for palliative care and presented it to the Ministry of Health in 2013 (see below for details). From 2011 to 2013 it ran four palliative care pilot projects in order to estimate the costs of eventually incorporating palliative into the public health care system.
Finally, in December 2014, the Health Ministry approved three policy documents establishing the structure and organization of palliative care services and professional qualifications for doctors and nurses in palliative care; the standards for palliative medical care and services; and clinical guidelines for pain management.[200]
However, the government has done nothing to change control substance regulations, described in Chapter IV of this report, that currently inhibit availability and access to strong opioid analgesics. One official who has advocated for reform of the regulations attributed this to public officials’ fear of “touching the issue of legalizing any [narcotics].” He said that even though official data show that only 2 to 3 percent of illicit drug use is linked to medical institutions the health ministry has yet to approve an overhaul of the regulations.[201]
The national strategy on palliative care, which addresses all major areas of palliative care policy—education, medicines availability, and implementation of palliative care services—and which the expert presented in 2013 has yet to be adopted and implemented.
Armenia needs to adopt and implement these reforms in order to meet its obligation under the ICESCR to ensure that people with life-limiting illnesses can enjoy their right to health.[202] Barriers to effective pain treatment place Armenia in violation of the right to health and pose the risk of patients being exposed to cruel, inhuman, or degrading treatment in violation of international standards. The government therefore has to take the lead in addressing the barriers that currently impede the availability of good palliative care and pain treatment.
Piloting Palliative Care
As noted above, from 2011 to 2013 the Global Fund to Fight AIDS, Tuberculosis and Malaria, together with the Open Society Institute Assistance Foundation Armenia and the Health Ministry, supported four palliative care pilot projects in Armenia. The projects provided regular home visits to patients, pain management in line with WHO recommendations (to the extent circumstances allowed), psychological support, support for families in caregiving, etc.[203]
Patient Rights and Protection Center, a nongovernment patient’s advocacy group, implemented the pilot projects. Each site had a physician and nursing and psychological staff who received several classroom and clinical trainings in palliative care in Armenia and abroad.[204]
Each pilot project had a quota of 30 patients, but in practice the numbers varied. In 2011 a total of 132 patients participated in the programs and received palliative care in homes and hospital. An assessment of the pilot programs reported that 42 percent of participating patients had severe pain on admission, which, the report noted, is higher than usually seen at established palliative care services, apparently reflecting the limited access to opioids in Armenia.[205] Upon admission patients showed a high level of emotional distress, with over half (51.5 percent) meeting criteria for clinical anxiety, and 56.1 percent for depression.[206]
The pilot projects followed the requirements under Armenian law for the prescription and dispensing of opioid analgesics, impeding to a certain extent the provision of pain management in accordance with WHO recommendations.[207] They were also constrained by the limited availability of registered medications, which included non-steroidal anti-inflammatory medicines, weak opioids such as tramadol, anti-seizure drugs, and injectable morphine, which, according to the report, was underused.[208] Even so, the assessment report found positive effects on pain levels of patients. The effects were attributed to several factors: doctors with the pilot projects prescribed based on pain levels, rather than on the stage of the disease; dosages were titrated to specific amounts needed for the individual patient; and pain medication was prescribed around the clock rather than one or two ampoules per day. The pain management results were particularly high among the four patients participating in the pilot projects who received methadone.[209]
Key recommendations that emerged from the pilot projects were that patients in moderate to severe pain should have access to oral opioids, that physicians working in palliative care programs should be allowed to prescribe opioids, and that the provision that opioid analgesics may only be prescribed to cancer patients should be removed.[210]
The projects’ main goal was to establish model palliative care programs, estimate their costs and possible impact on the state budget, and assess their effectiveness in order to eventually replicate them throughout Armenia’s public health care system.[211] According to the assessment report, “[t]he general view of the cost impact of palliative care indicates that home-based palliative care is more cost effective than inpatient care. Palliative care adds value to health care costs by shortening hospital length of stays and preventing unnecessary readmission.”[212]
The government had planned to create, in 2014, 15 additional palliative care sites following the model set by the pilots. However, as of this writing it has not renewed the program or incorporated the model in the wider health care system.
Palliative Care Concept and National Strategy
In August 2012, the government of Armenia approved a needs-assessment study on palliative care.[213] The study, entitled “Concept on Palliative Care in the Republic of Armenia,” explained the need for palliative care in the country and suggested ways it could be implemented. The concept paper takes a rights-based approach to palliative care, stating that “everyone shall have the right not only to live, but also to die with dignity without physical or mental suffering.”[214] Informed in part by the results of the palliative care pilot projects, the concept paper recommended legislative reforms in a number of areas, including access to strong opioid-based pain medications and including palliative care services in health care legislation; the development of a national strategy for the implementation of palliative care, and educational and public awareness programs.[215]
In 2013, the government-convened palliative care working group drafted the National Strategy and Action Plan for Introduction of Palliative Care and Services in the Republic of Armenia, an operative plan for implementing palliative care in the health care system. The strategy specifies the reforms needed in major areas of policy, education, medicines availability, and designates which state institutions would be responsible for which aspect of the reform. However, as noted above, the government had not approved it as of this writing.
One government official explained to Human Rights Watch that adoption of the National Strategy and Action Plan would require clearance from the Ministry of Finance, which would be reluctant to support it if additional resources would be needed.[216] However, he also stressed that calls to emergency services and ambulances decreased among the patients registered at the pilot sites, which could make palliative services still relatively cost effective.[217] Meanwhile, the international donor community should continue to support the government’s efforts to introduce palliative care services in Armenia.
The Example of UkraineUkraine, with its common history as part of the Soviet Union, has faced many of the same barriers to palliative care present in Armenia. Human Rights Watch research in Ukraine found that, until very recently (see below), oral morphine was not available; multiple doctors had to sign prescriptions for morphine; and physicians were not allowed to give any patients injectable morphine to take at home, requiring nurses to travel to patients’ homes to administer each dose of the medication. Because demands for nurses at hospitals are high, nurses could not do so more than once or twice a day—or at all in most rural settings—leaving most patients without adequate pain medications for most or all of the day. In the last few years, the Ukrainian government has actively sought to address these barriers. In 2013, it registered oral morphine as an approved medicine and two pharmaceutical companies began local production by late 2014. In 2013, the government also introduced major changes to its drug regulations, making them the most progressive of all former Soviet states. Palliative care patients are now allowed to take a 15-day supply of morphine home, so they no longer need nurses to visit them at home to administer doses. The new regulations also reduced the number of people who have to sign off on a prescription for strong pain medicines to two: the treating physician and the management of the hospital or clinic. These prescriptions can now be filled at any licensed pharmacy; previously, they could only be dispensed at one specific pharmacy. Empty ampoules no longer have to be returned to pharmacies or a hospital, as was previously the practice. Ukraine has also integrated palliative care into its national HIV, tuberculosis (TB), and cancer control programs and developed and disseminated a national pain treatment protocol. While significant challenges remain, oral morphine tablets are now available throughout the country (with the exception of the conflict zone in the Donbass) and numerous physicians now prescribe them. Government figures suggest that Ukraine’s careful liberalization of its controlled substance regulations has not resulted in an increase of misuse or diversion of opioid medicines. According to official figures, licitly produced pharmaceutical opioid-based medicines make up only about 1/10 of one percent (0.1 percent) of all narcotic drugs seized by Ukrainian police and that figure has been stable in recent years.[1] [1] Victoria Tymoshevska, the head of the public health program of the International Renaissance Foundation in Ukraine, informed Human Rights Watch that police officials cited these statistics at meetings in July 2013 and April 2015. They do not appear to have been officially published. |
VII. Armenia’s Obligations to Improve Palliative Care
National Law
Armenia’s constitution states that “Everyone shall have the right to benefit from medical aid and service under the conditions prescribed by law.” It provides for the provision of basic health services free of charge.[218] The Law on Medical Care and Services, the main national legal act regulating health care in Armenia, provides the right to receive medical care and services “irrespective of nationality, race, sex, language, religion, age, health status, political or their views, social origin, property ownership, or other status.”[219] The law distinguishes between primary and specialized medical care, and states that primary care is provided free of charge.[220] While cancer and other complex illnesses are not covered under these free services, the government has mandated that medications for the treatment of a number of additional illnesses are to be provided cost-free. This list includes cancer.[221] In 2009, “palliative care” was added to the list of medical services provided in Armenia.[222] In April 2015, the parliament adopted amendments to the Law on Medical Care and Services, to add a definition of palliative care, also stating that the government of Armenia is responsible for standards and implementation of palliative care.[223]
The Right to Health
The right to health is a fundamental human right enshrined in numerous international human rights instruments. Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR) specifies that everyone has a right "to the enjoyment of the highest attainable standard of physical and mental health."[224] Armenia ratified the ICESCR in 1993. Armenia is also a member of the Council of Europe and ratified the European Social Charter in 2004, which also highlights the right to “highest possible standard of health attainable.”[225]
The Committee on Economic, Social and Cultural Rights holds that states must make available in sufficient quantity "functioning public health and health-care facilities, goods and services, as well as programmes," and that these services must be accessible.
Because states have different levels of resources, international law does not mandate the kind of health care to be provided. The right to health is considered a right of "progressive realization." By becoming party to the international agreements, a state agrees "to take steps…to the maximum of its available resources" to achieve the full realization of the right to health. In other words, high-income countries will generally have to provide health care services at a higher level than those with limited resources. But all countries will be expected to take concrete steps toward increased services, and regression in the provision of health services will, in most cases, constitute a violation of the right to health.
Notably, the Committee on Economic, Social and Cultural Rights also holds that there are certain core obligations that are so fundamental that states must fulfill them. While resource constraints may justify only partial fulfillment of some aspects of the right to health, the Committee observes vis-à-vis the core obligations that "a State party cannot, under any circumstances whatsoever, justify its non-compliance with the core obligations…, which are non-derogable." The Committee identifies, among others, the following core obligations:
- To ensure the right of access to health facilities, goods and services on a non-discriminatory basis, especially for vulnerable or marginalized groups;
- To provide essential drugs, as from time to time defined under the WHO Action Programme on Essential Drugs;
- To ensure equitable distribution of all health facilities, goods and services;
- To adopt and implement a national public health strategy and plan of action, on the basis of epidemiological evidence, addressing the health concerns of the whole population.[226]
The Committee lists the obligation to provide appropriate training for health personnel as an “obligation of comparable priority.”
Palliative Care and the Right to Health
Given that palliative care is an essential part of health care, the right to health requires that countries take steps to the maximum of their available resources to ensure that it is available. Indeed, the Committee on Economic, Social and Cultural Rights has called for “attention and care for chronically and terminally ill persons, sparing them avoidable pain and enabling them to die with dignity.” A number of different state obligations flow from this:
- An obligation to refrain from enacting policies or undertaking actions that arbitrarily interfere with the provision or development of palliative care;
- An obligation to take reasonable steps to facilitate the development of palliative care; and
- An obligation to take reasonable steps to ensure the integration of palliative care into existing health services, both public and private, through the use of regulatory and other powers as well as funding streams.
No Interference with Palliative Care
The Committee on Economic, Social and Cultural Rights stipulates that the right to health requires states to “refrain from interfering directly or indirectly with the enjoyment of the right to health.”[227] States may not deny or limit equal access for all persons, enforce discriminatory health policies, arbitrarily impede existing health services, or limit access to information about health.[228] Applied to palliative care, this obligation means that states may not put in place drug control regulations that unnecessarily impede the availability and accessibility of essential palliative care medications, such as morphine and other controlled substances.
Facilitating the Development of Palliative Care
The right to health also includes an obligation to take positive measures that “enable and assist individuals and communities to enjoy the right to health.”[229] Applied to palliative care, this means that states should take reasonable steps in each of the four areas the World Health Organization (WHO) has identified as essential to the development of palliative care: education and training, accessibility of adequate pain medication, inclusion in health care policy, and implementation of palliative care services.[230] These four prongs of WHO correspond closely with several core obligations under the right to health.[231]
Ensuring Integration of Palliative Care into Health Services
The right to health requires states to take the steps necessary for the “creation of conditions which would assure to all medical service and medical attention in the event of sickness.”[232] The Committee on Economic, Social and Cultural Rights holds that people are entitled to a “system of health protection which provides equality of opportunity for people to enjoy the highest attainable level of health,”[233] including chronic or terminal illness.
The Committee has called for an integrated approach to the provision of different types of health services that include elements of “preventive, curative and rehabilitative health treatment.”[234] It also holds that investments should not disproportionately favor expensive curative health services which are often accessible only to a small, privileged fraction of the population, rather than primary and preventive health care benefiting a far larger part of the population.[235] The same principle applies to palliative care services. The WHO recommends that low- and middle-income countries, the cohort to which Armenia belongs, focus on developing community-based palliative care services because they are inexpensive. Given the large percentage of cancer and other patients who require palliative care services, particularly in low- and middle-income countries, considerable urgency needs to be given to developing palliative care services for these patients.
Pain Treatment Medication and the Right to Health
As injectable and oral morphine are on the WHO List of Essential Medicines for adults and for children, countries have to provide these medications as part of their core obligations under the right to health, regardless of whether they have been included on their domestic essential medicines lists.[236] States must make sure these medicines are both available in adequate quantities and physically and financially accessible for those who need them.
In order to ensure availability and accessibility, states have, among others, the following obligations:
- Since the market for controlled medicines like morphine are completely in government hands, states must put in place an effective procurement and distribution system and create a legal and regulatory framework that enables health care providers in both the public and private sector to obtain, prescribe and dispense these medications. Any regulations that arbitrarily impede the procurement and dispensing of these medications will violate the right to health.
- States need to adopt and implement a strategy and plan of action for the roll out of pain treatment and palliative care services. Such strategy and plan of action should identify obstacles to improved services as well as steps to eliminate them.
- States should regularly measure progress made in ensuring availability and accessibility of pain relief medications.
- The requirement of physical accessibility means that these medications should be "within safe physical reach for all sections of the population, especially vulnerable or marginalized groups."[237] States should ensure that a sufficient number of health care providers or pharmacies stock and dispense morphine, and that an adequate number of health care workers are trained and authorized to prescribe these medications.
Financial accessibility means that, while the right to health does not require states to offer medications free of charge, they must be "affordable for all." In the words of the Committee:
Payment for health-care services…has to be based on the principle of equity, ensuring that these services, whether privately or publicly provided, are affordable to all, including socially disadvantaged groups. Equity demands that poorer households should not be disproportionately burdened with health expenses as compared to richer households.
Countries have an obligation to progressively implement palliative care services, which, according to the WHO, must have "priority status within public health and disease control programmes."[238] Countries should take all steps that are reasonable within available resources to execute the plan. Failure to attach adequate priority to developing palliative care will violate the right to health.
Pain Treatment and the Right to Be Free from Cruel, Inhuman and Degrading Treatment
The right to be free from torture, cruel, inhuman and degrading treatment or punishment is a fundamental human right that is recognized in numerous international human rights instruments to which Armenia is a party.[239] Apart from prohibiting the use of torture, cruel, inhuman, and degrading treatment or punishment, the right also creates a positive obligation for states to protect persons in their jurisdiction from such treatment.[240]
This obligation includes protecting people from unnecessary pain related to a health condition. As Manfred Nowak, the UN Special Rapporteur on Torture, Cruel, Inhuman and Degrading Treatment and Punishment wrote in a joint letter with the UN Special Rapporteur on the Right to Health to the Commission on Narcotic Drugs in December 2008:
Governments also have an obligation to take measures to protect people under their jurisdiction from inhuman and degrading treatment. Failure of governments to take reasonable measures to ensure accessibility of pain treatment, which leaves millions of people to suffer needlessly from severe and often prolonged pain, raises questions whether they have adequately discharged this obligation.[241]
In a report to the Human Rights Council, Nowak later specified that, in his expert opinion, “the de facto denial of access to pain relief, if it causes severe pain and suffering, constitutes cruel, inhuman or degrading treatment or punishment.”[242]
Not every case where a person suffers from severe pain but has no access to appropriate treatment will constitute cruel, inhuman, or degrading treatment or punishment. Human Rights Watch believes that this will only be the case when the following conditions are met:
- The suffering is severe and meets the minimum threshold required under the prohibition against torture and cruel, inhuman, or degrading treatment or punishment;
- The state is, or should be, aware of the level and extent of the suffering;
- Treatment is available to remove or lessen the suffering but no appropriate treatment was offered; and
- The state has no reasonable justification for the lack of availability and accessibility of pain treatment.
In such cases, states will be liable for failing to protect a person from cruel, inhuman, or degrading treatment.
Recommendations
To the Government of Armenia
On Availability of Medicines
- Work with manufacturers and importers to facilitate the registration of oral opioid painkillers. The public health care system should carry oral morphine, once it is registered, at all levels of care.
- Allow physicians with proper clinical training to use methadone, which is already registered in Armenia, for pain management purposes throughout the public health system.
- Abolish the restriction that allows only oncologists to prescribe opioid painkillers. Allow all physicians with proper clinical training and working in palliative care to prescribe opioid painkillers.
- Remove the restriction that allows only outpatients with cancer to receive prescriptions for opioid painkillers. Any patient with a life-limiting condition with moderate to severe pain should have access to adequate pain medication, including opioid analgesics.
- Abolish the requirement of a biopsy-confirmed cancer diagnosis in order for opioids to be prescribed. A determination by a physician based on a clinical examination should be sufficient to prescribe opioid analgesics.
- Reform the overly onerous procedure for the prescription of opioid painkillers:
- Abolish the need for approval by a standing commission for opioid prescriptions.
- Eliminate the requirement for multiple signatures on the prescription form. Doctors in most countries can make individual decisions to prescribe opioid medications.
- Simplify and minimize the prescription forms and record-keeping requirements.
- Allow patients to collect a supply of opioids that would ensure at least a fourteen-day supply.
- Revise the requirements pharmacies must meet in order to obtain a license to dispense opioids, including the security requirement, to ensure they are not disproportionately burdensome.
- Cease excessive police interference in the prescription process. The government should explicitly instruct all physicians to end the current practice of filing reports on prescribing of opioids that contain confidential patient information with police. Any routine reporting requirements should contain anonymized information only. Police should make clear to doctors that they do not require such reports, formally or informally, and will no longer accept them.
On Policy Development
- Without further delay, adopt the National Strategy and Action plan for the Introduction of Palliative Care and Services in Armenia.
- Develop and incorporate palliative care services throughout the public health care system.
- Develop a home-based palliative care system that provides services for patients and caregivers that would include home visits, phone consultations, as well as clinic visits and hospitalization when necessary.
- Implement the guidelines for pain management and standards for palliative care approved by the Health Ministry in December 2014.
- Request WHO assistance in implementing the World Health Assembly's May 2014 resolution 67.19 — on Strengthening of Palliative Care as a Component of Comprehensive Care throughout the Life Course.
On Awareness and Education
- Introduce palliative care instruction into medical and nursing curricula. All health care providers should have at least basic training in the discipline. Health care providers who see large numbers of patients in need of palliative care should receive in-depth training and exposure to clinical practice.
- Ensure that physicians receive proper training on pain management including use of oral opioids to treat patients’ pain.
- Ensure that doctors are trained in communicating diagnoses, prognoses and other relevant information on life-limiting illnesses to patients. Ensure that they are trained and supported in holding end-of-life conversations with patients and their families.
- Introduce palliative care into the curriculum for continuing medical education. Palliative care and pain management that follows WHO standards should be included in mandatory continuing education for all general practitioners, oncologists, infectious disease doctors, anesthesiologists, and geriatricians.
- Introduce palliative care as a field of sub-specialization.
- Include questions about palliative care in exams for medical licenses.
- Develop training models for doctors, nurses, social workers, counselors, and volunteers, in cooperation with civil society groups and international palliative medicine experts.
- Raise public awareness around the right to pain relief and on the availability of treatment for severe pain.
To the International Community
To the International Narcotics Control Board
- Raise concern about the limited availability of opioid analgesics in Armenia documented in this report. In particular, the International Narcotics Control Board (INCB) should request information from the government of Armenia about its efforts to ensure adequate availability of controlled substances for medical and scientific purposes and about remaining barriers.
- Establish regular contact with key palliative care leaders in Armenia to ensure the INCB receives information on opioid availability barriers directly from health care providers.
- Offer technical support to the government of Armenia in reviewing and amending current drug regulations.
To the World Health Organization
- Urge the Armenian government to use the WHO guidance on ensuring balance in national controlled substance policies to assess and revise Armenia’s controlled substance policies.
- Offer technical assistance to the government of Armenia on reform of controlled substance regulations and educational barriers.
- Assist the government in implementing the World Health Assembly’s resolution 67.19 – on Strengthening of Palliative Care as a Component of Comprehensive Care throughout the Life Course.
To the European Union
- Include limited availability of palliative care and pain treatment in Armenia among the human rights concerns raised as part of the structured human rights dialogue and other relevant bilateral and multilateral dialogues with Armenia, encouraging the authorities to undertake the specific steps outlined in this report to remedy the problems identified.
- Offer financial and technical assistance to the government of Armenia to introduce and implement palliative care instruction for health care workers and reform controlled substance regulations.
To the Council of Europe
The Council of Europe has recommended that member states ensure the availability of palliative care.[243] However, its recommendations have, to date, not adequately addressed the significant problems that exist in Council of Europe states with regard to availability of opioid medications. To address this shortcoming:
- The Commissioner for Human Rights should take up the issue of access to pain treatment medications and palliative care more generally, as part of his work, including specifically in Armenia.
- The Committee of Ministers should encourage all Council of Europe countries to review their drug regulations using the tool WHO has developed for this purpose.[244]
- The Committee of Ministers should encourage Armenia to implement Recommendation CM/Rec(2014)2 on the promotion of human rights of older persons, including its section on palliative care.[245]
To International Donors
- Provide financial and technical support to the government of Armenia and professional and civil society groups working to promote palliative care reform and its implementation.
Acknowledgments
Research for this report was conducted by Giorgi Gogia, senior South Caucasus researcher at the Europe and Central Asia division of Human Rights Watch, with support from Diederik Lohman, associate director of the Health and Human Rights division of Human Rights Watch. Giorgi Gogia wrote the report. Diederik Lohman wrote sections about international standards and best practices on palliative care.
This report was edited by Rachel Denber, deputy director of the Europe and Central Asia division of Human Rights Watch. It was reviewed by Diederik Lohman, associate director of the Health and Human Rights division, and Veronika Szente Goldston, advocacy director of the Europe and Central Asia division reviewed the summary and recommendations. Aisling Reidy, senior legal advisor, provided legal review, and Tom Porteous, deputy program director, provided Program review. The report was also reviewed by Stephen R. Connor, PhD, International Palliative Care Consultant for the Open Society Foundations.
Kathryn Zehr, associate with the Europe and Central Asia Division, provided invaluable assistance, as did Dariya Golubkova, intern at the Europe and Central Asia Division, and Stephanie Martinez, intern at the Health and Human Rights division. Production assistance was provided by Kathryn Zehr; Grace Choi, publications director; and Fitzroy Hepkins, production manager. Sakae Ishikawa, senior video editor, and Jessie Graham, senior producer, directed and produced the video component of the project. Jenny Catherall, former multimedia coordinator, and Connor Seitchik, associate producer, also helped produce the video. Khachatur Adumyan translated the report into Armenian.
A number of people provided invaluable assistance in the research and preparation of this report. Special thanks go to Anahit Papikyan, senior coordinator of the public health program at the Open Society Foundations – Armenia; Violeta Zopunyan, director of Center for Rights Development NGO; and Stephen R. Connor. Human Rights Watch also gratefully acknowledges the expertise and assistance of Dr. Hrant Karapetyan, president of the Armenian Pain Control and Palliative Care Association; Dr. Narine Movsesyan, assistant professor at Yerevan State Medical University, Dr. Narine Kalashyan, head of the oncology department at Vanadzor hospital number 1, and Dr. Anna Grigoryan, a family physician at the Ararat Medical Center.
We are deeply grateful to the many palliative care patients in Armenia who, despite being gravely ill, agreed to be interviewed for this report. Without them and their relatives, this report would not have been possible. We are committed to using this report to ensure that others who develop life-threatening illness—and pain and other symptoms associated with it—will not have to endure the suffering many of these patients faced.
We are also greatly indebted to the palliative care advocates, doctors, nurses, pharmacists, social workers and volunteers in Armenia and elsewhere who helped us conduct our research and understand our findings, without which this report could not have been written. Their commitment to serving people at the most vulnerable time of their lives is both humbling and inspiring.