The Story of Maria Higginbotham
Maria Higginbotham jokes that she was just born unlucky: in 2003, she was a 43-year-old regional bank manager in a town outside Seattle, Washington with two children and no serious health issues. But one day she went out to get the mail and suddenly found she could not walk. Within weeks, she was admitted to the hospital for the first of what would be 12 operations performed on her spine between 2003 and 2015. Her diagnosis: an aggressive form of degenerative disc disorder. The surgeries would put hardware in her back to prop up her spine and relieve pain, but each time it was only a matter of months before another disc in her back buckled and she found herself back on the operating table. Her spine is now “encased in metal,” she said. A recent operation was required just to remove all the hardware accumulated in her body over the years: she holds up a Ziploc bag full of nuts and bolts.
Those operations not only failed to halt the collapse of her spine — they also left her with adhesive arachnoiditis, a condition caused by inflammation of the membrane surrounding the spinal cord that is often the result of trauma, including from surgery. The National Institute of Neurological Disorders and Stroke acknowledges that it is a rare but extremely painful condition. “Your spinal cord is supposed to hang loose, like worms, in your spinal fluid — [in my case] they glue themselves together,” is how Higginbotham explained it. Because of the arachnoiditis, as well as a number of other more common pain conditions like rheumatoid arthritis, she has “constant pain in the middle of [her] back, and a sharp shooting pain when [she] move[s].”
She has tried the gamut of available pain treatments, from physical therapy to steroid injections to nerve ablations — which heat up a small area of nerve tissue to decrease pain signals from it — but none provide adequate relief. Medical marijuana helped somewhat, but makes her too anxious. She has racked up more than $2,000 in credit card bills paying for treatments that are not reimbursed by insurance, such as medical marijuana and over-the-counter heat patches. Higginbotham cannot take ibuprofen-like drugs due to stomach and liver problems.
Because nothing else works, she relies primarily on opioid analgesics to get through the day. She has been on the medication in doses that have varied only slightly since 2004. She has a pain pump, a device implanted into the body that delivers pain medication directly to the spinal cord, and also uses patches that infuse opioids through her skin, which she replaces every few days. This combination of medications allowed her to function well enough to make meals, take care of her two dogs, tidy her house, and care for her grandchildren for many years.
But in March 2018, Higginbotham’s medical provider said he would be reducing her opioid medications by 75 percent in order to get her down to a dose he said was recommended in a guideline from the US Centers for Disease Control: 90 milligram equivalents of morphine. He told Human Rights Watch he believed Higginbotham had done well on the medication, but that his clinic was implementing a new policy over fears they could be held liable for high-dose opioid prescriptions:
There’s a lot of talk in the pain medicine world that if you do not get people down to 90 morphine equivalents, you set yourself up for a liability, especially if something were to happen to that patient. It doesn’t matter if you did everything appropriately [to prevent abuse] — and we do everything, urine drug testing, prescription monitoring, screening for mental health issues, pill counts. It doesn’t feel like enough. We still feel like we’re vulnerable to being held liable for patients if they’re over that guideline limit, even when you know they’re not addicted and they’re benefitting [from opioids].
When Human Rights Watch interviewed Higginbotham in April 2018, the pain doctor had reduced her dose by more than a third. She said that the effects have been profound: she could be on her feet for just a few minutes at a time and needed her family’s help to get out of bed or go to the toilet. She had lost 70 pounds because of the pain and because she couldn’t stand up long enough to make herself a meal:
Pain has a way of defeating you, taking away any pleasure you used to get. I’m 57 years old and I’m almost completely bedridden due to agonizing pain like torture.
I cannot hold my 15-month-old grandson. I cannot hold my beloved dogs, I can’t bend over to touch them. I cry out in my sleep because I can’t find a way to get comfortable. The sun is shining and my flowers are blooming and I want to just walk outside with my dogs and look at them, but I can’t.
I can barely get myself off of my toilet, sometimes I have to get off the couch by getting on my hands and knees and pulling myself up because I can’t stand up it hurts so badly. I don’t want to leave my home.
Higginbotham’s medical provider told Human Rights Watch that she is not doing well, but has said he has no option but to continue gradually lowering her medication. He has suggested she seek pain relief by undergoing another surgery, this time to remove a screw that may be putting pressure on a nerve in her back. But Higginbotham is terrified of going under the knife again after so many failed and problematic surgeries:
My body is failing me and all I want to do is live a life free of a massive amount of suffering — I know I will never be free from pain but to subject me to even more pain is inhuman. How many times do I have to go through this to prove there isn’t a fix? I can’t be fixed.
Summary
An estimated 40 million adults in the United States suffer from significant levels of chronic pain, making it one of the most common health problems and the leading cause of disability in the country. People with chronic pain tend to have worse overall health than other Americans, experience depression and anxiety disorders at higher rates, and use the health care system more frequently. Unlike people with acute pain, chronic pain patients often experience a sense of hopelessness and catastrophic thoughts brought on by fears that their pain might never go away.
Despite the extent of this problem and its medical, social, and economic impacts, many patients in the US do not have access to adequate treatment for chronic pain. This is in part because chronic pain can be difficult to treat: it can result from a wide range of causes and it affects different people in different ways. But it is also because most clinicians are poorly trained in pain management, health insurance policies often do not adequately cover non-pharmacological treatments, and the health care system does not facilitate multidisciplinary treatment of chronic pain, which is often the most effective option for complex pain.
The opioid overdose crisis that has struck the US in recent years, which claimed more than 70,000 lives in 2017, has further complicated the situation for chronic pain patients. Many overdose deaths involve the same opioid medications commonly prescribed to people in chronic pain. Today, treating chronic pain with opioids is medically controversial because evidence suggests their effectiveness is limited. But in the 1990s, these medications became a go-to option for physicians treating chronic pain. Between 1999 and 2010, prescriptions for opioid analgesics quadrupled in the US.
The government has a duty to address this rapidly unfolding public health crisis: in 2017 alone, more Americans are estimated to have died of a drug overdose than were killed in the Vietnam, Iraq, and Afghanistan wars combined. Given the role prescription opioids have played in the crisis, measures to regulate the use of these medications and to promote more careful prescribing practices are essential.
However, under international human rights standards, actions taken to combat the overdose epidemic should take the needs of chronic pain patients into account. The government should seek to avoid harming chronic pain patients: some patients still have a legitimate need for these medications, while others who have been on these medications for many years but who may not be benefiting from them should be weaned off them safely and in accordance with best medical practice.
If harms to chronic pain patients are an unintended consequence of policies to reduce inappropriate prescribing, the government should seek to minimize and measure the negative impacts of these policies. Any response should avoid further stigmatizing chronic pain patients, who are increasingly associated with — and sometimes blamed for — the overdose crisis and characterized as “drug seekers,” rather than people with serious health problems that require treatment.
This report presents the challenges faced by chronic pain patients like Maria in obtaining appropriate care, examines how the government’s legitimate efforts to address the opioid epidemic have contributed to unintended but serious harm, and fallen short of its responsibilities to address the needs of individuals taking opioid medicines for chronic pain. The report is based on 86 interviews with chronic pain patients, healthcare providers, and officials, which were conducted over the phone or in person during visits to Tennessee and Washington State between March and July 2018. We also reviewed relevant state and federal laws, regulations, and clinical guidelines related to chronic pain management and opioid prescribing.
Public health officials generally agree that the current opioid epidemic is the result of multiple factors, including both a previous over-reliance on opioids to treat chronic pain and aggressive and misleading marketing of opioid medication by pharmaceutical companies. As a result, federal and state governments have made reducing opioid prescribing a major priority in the last five years.
Top government officials, including the President, have said the country should aim for drastic cutbacks in prescribing. State legislatures encourage restrictions on prescribing through new legislation or regulations. The Drug Enforcement Administration (DEA) has investigated medical practitioners accused of overprescribing or fraudulent practice. State health agencies and insurance companies routinely warn physicians who prescribe more opioids than their peers and encourage them to reduce prescribing. Private insurance companies have imposed additional requirements for covering opioids, some state Medicaid programs have mandated tapering to lower doses for patients, and pharmacy chains are actively trying to reduce the volumes of opioids they dispense.
The medical community at large recognized that certain key steps were necessary to tackle the overdose crisis: identifying and cracking down on “pill mills” and reducing the use of opioids for less severe pain, particularly for children and adolescents. However, the urgency to tackle the overdose crisis has put pressure on physicians in other potentially negative ways: our interviews with dozens of physicians, mostly from Tennessee and Washington State, found that the atmosphere around prescribing for chronic pain had become so fraught that physicians felt they must avoid opioid analgesics even in cases when it contradicted their view of what would provide the best care for their patients. In some cases, this desire to cut back on opioid prescribing translated to doctors tapering patients off their medications without patient consent, while in others it meant that physicians would no longer accept patients who had a history of needing high-dose opioids.
The consequences to patients, according to Human Rights Watch research, have often been catastrophic. Patients like Maria were often left with debilitating pain that made them incapable of going about their daily lives — simple activities, such as household chores or taking care of others, were suddenly impossible. In many cases, patients suffered extreme anxiety and others even thoughts of suicide, as they questioned whether their lives would ever be worth living in such extreme pain. Others, particularly those who struggled to find a medical provider if their treatment still involved opioid medications, felt betrayed and abandoned by the medical community.
Amidst the repeated calls for cutbacks in prescribing, new laws and regulations on prescribing, stricter insurance policies, and concerns about criminal sanctions, medical providers lacked clear guidance on the harms of involuntary tapering and their legal and ethical obligations to provide adequate treatment for chronic pain patients. State agency policies on opioids, as well as physicians interviewed for this report, frequently referred to the Centers for Disease Control Guideline for Prescribing Opioids for Chronic Pain as a key resource in this regard. The Guideline, published in March 2016, sought to address gaps in primary care physicians’ understanding of opioids, their risks, and the limited evidence surrounding their effectiveness.
The Guideline proposes a carefully balanced approach. It cautions against the use of opioid analgesics to manage chronic pain, especially at high doses, but leaves decisions about individual patients to clinicians. It advises providers to try alternatives before resorting to opioids, but acknowledges that some patients who do not see their pain resolved by other means might still need opioids, sometimes at high doses. The Guideline also acknowledges that because opioids were frequently used in the US to treat chronic pain from the 1990s onward, many patients may already be on high doses and tapering those patients, who have developed a physical dependency on the medication, may be difficult.
However, the Guideline does not clearly state that physicians should not taper patients off their medications involuntarily, and it has been used by state officials to justify policies that define maximum doses for all patients regardless of their individual medical needs.
Even when medical providers understood that the Guideline was voluntary, they believed they risked punishment or unwanted attention from law enforcement agencies or state medical boards if they maintained patients at high doses. Because the DEA, which licenses all controlled substance prescribers in the country, defines illegal prescribing as anything not within the confines of “professional practice,” a term that has no commonly accepted meaning, providers said they were left to police themselves against risks, and did so by using the CDC Guideline as a red line for prescribing. Twelve physicians told Human Rights Watch that they had made involuntary dose reductions for patients — sometimes hundreds — who were compliant with screening procedures and appeared to be benefiting from their medication. This practice is inconsistent with the Guideline’s recommendations, unsafe, and can severely undermine a patient’s quality of life.
This report found that chronic pain patients, particularly those who have relied on opioid medications for treatment, face increasing difficulty finding clinicians willing to provide them care, and feel abandoned and stigmatized by the healthcare system as a result. Some providers said they refused to take on new chronic pain patients who were on opioids because of the liability, even if they believed that those patients had diagnoses that warranted treatment with opioid medication. In cases where a pain clinic was shut down or a provider’s license revoked, there appeared to be minimal government efforts to ensure continuity of care. Because many patients who take opioids develop a physical dependence on them, abrupt termination of care could, in addition to increased pain, trigger withdrawal.
Patients described harms they have experienced as a result of being involuntarily tapered, including increased pain, decreased mobility, and thoughts of suicide. Indeed, the debilitating physical, mental, and social effects of chronic pain have been well-documented. But involuntary tapering or inadequate treatment can also have a major negative impact on a patient’s quality of life, and can even drive them to self-medicate with alcohol or illicit drugs.
Moreover, patients and physicians told Human Rights Watch that non-opioid treatments for chronic pain are often unavailable or not covered by health insurance. The Guideline recommends that patients use non-opioid therapies to treat chronic pain, and emphasizes the importance of non-pharmacological treatments like massage, acupuncture, and various types of physical therapy. However, many patients and physicians told us these treatments are not an option because they would require patients to incur burdensome out-of-pocket costs.
The government’s efforts to combat the overdose epidemic should be balanced with the interests of chronic pain patients who have a medical need for opioid analgesics. As this report documents, current policies and practices to reduce the use of these medicines have significant unintended negative consequences, which the government should seek to redress. Among others, it should document the pace of involuntary tapering and its impact on chronic pain patients — including patients' mental and physical health as well as hospitalization — and take corrective steps as needed.
More broadly, the government should take proactive steps to ensure that chronic pain patients who have a serious and often debilitating medical condition have access to adequate care. Federal and state governments have a responsibility to ensure that a broad range of pain treatment interventions is available to such patients, including non-pharmacological treatments, and that treatment modalities are covered by insurance plans, including Medicaid and Medicare.
In 2016, the Department of Health and Human Services released a National Pain Strategy, calling it the federal government’s first “coordinated plan for reducing the burden of chronic pain” in the United States.[1] The strategy aims to improve the prevention and management of pain; support the development of an integrated, patient-centered, approach to pain management; reduce barriers to treatment; and improve public awareness. But the strategy does not specifically address the situation of the thousands of chronic pain patients who are already on opioid medicines. To date, implementation of the strategy has primarily focused on a research agenda, rather than reducing the barriers to care chronic pain patients currently face. Congress has not made any appropriations to implement the strategy.
Key Recommendations
To counter harmful trends in the treatment of chronic pain patients and ensure their access to appropriate health services, Human Rights Watch makes the following recommendations:
Implement the National Pain Strategy
- Federal and state governments should fully implement and provide adequate funding for the National Pain Strategy, including the components related to healthcare worker and public education and delivery of services. While research on pain prevention and management is critical, it is essential that steps to improve access to existing interventions are taken right away, as today’s chronic pain patients cannot wait.
Limit the Unintended Consequences of Prescription Reductions for Chronic Pain Patients
- The Centers for Disease Control and Prevention (CDC) should revise its 2016 Guideline for Prescribing Opioids for Chronic Pain to explicitly state that patients should not be involuntarily tapered off opioids and that there is no mandated maximum dose.
- The CDC and DHHS should work with other relevant federal and state government agencies, state medical boards, and professional and civil society groups to ensure that clinicians, including those caring for patients on high doses of opioids, can implement the Guideline’s recommendations without having to fear unwarranted legal scrutiny, arbitrary limits, or administrative barriers.
- The CDC and DHHS should work with the Centers for Medicare and Medicaid Services, the Department of Veterans Affairs, individual states, and private insurance providers to identify and address limits or administrative practices that arbitrarily interfere with the ability of chronic pain patients who need opioid analgesics to access them.
- State Departments of Health and other responsible agencies should take steps to ensure that chronic pain patients are not abruptly forced off their medication when a pain clinic is shut down or a provider removed from practice, and it should involve local medical stakeholders to this end.
Improve the Availability, Accessibility and Affordability of Multimodal Pain Management, Including to Non-Pharmacological Modalities
- The Department of Health and Human Services, the Centers for Medicare and Medicaid Services, the Department of Labor, and state insurance commissioners should seek to expand insurance coverage of treatment modalities for chronic pain, including non-pharmacological interventions.
- The National Institutes of Health, CDC and other relevant government agencies should fund more research into the effectiveness of different modalities for chronic pain.
Improve Data Collection on Involuntary Tapering and the Overdose Crisis to Allow the Most Effective Response Possible
- Federal and state government agencies should collect data about the frequency of involuntary tapering among chronic pain patients, as well as outcomes for those patients: if they have physical and mental health issues as a result, whether they are hospitalized, maintained in care, or commit suicide as a result. To the extent that government agencies have collected such data, they should disclose it to the public at the present time.
- Federal and state government agencies should implement or encourage standardized data collection on overdose deaths, including details relevant to gaining a better understanding of the role of prescribed opioids in such deaths.
- Overdose deaths should be cross-referenced with prescription monitoring data and other statistics to obtain detailed information on current or past prescription history of the overdose victim.
Methodology
This report is based on research conducted from March to July 2018, including field visits to Washington State in April and May 2018 and to Tennessee in June 2018. Human Rights Watch conducted 86 interviews with various stakeholders, including 44 chronic pain patients; 34 health care workers (including physicians, nurse practitioners, physician assistants, psychologists, and pharmacists); four officials from the Departments of Health of Washington (as well as Washington State’s Labor and Industries, a workers’ protection and compensation group that has been instrumental in influencing policy on opioid prescribing in the state); and five experts in medicine, law, and health policy. In addition to interviews in the two states, Human Rights Watch conducted telephone interviews with patients in Maine, West Virginia, Texas, California, and Montana; and physicians in West Virginia, Maine, Utah, Colorado, and Maryland.
Human Rights Watch also extensively reviewed medical literature, using academic databases to find available studies about opioid use for chronic pain, opioid dependence, and tapering practices.
Most interviews with patients were conducted in their homes or at a meeting place convenient for them. Patients were identified primarily through online channels, such as patient support groups on social media. Most interviews with healthcare providers were conducted in their offices or by phone. Interviews were almost exclusively conducted in private, and occasionally in the presence of a patient’s relatives. Interviews were semi-structured and covered a range of topics related to chronic pain management and treatment. Before each interview we informed interviewees of its purpose, the kinds of issues that would be covered, and asked whether they wanted to participate. We informed them that they could discontinue the interview at any time or decline to answer any specific questions without consequence. Human Rights Watch did not offer any incentives to interviewees. In some cases, patients asked their identities to be disguised to protect their privacy, while many healthcare workers declined to be identified for fear of retribution. All interviews were conducted in English.
We chose Washington State for our field research because officials from Washington State’s Labor and Industries (the state’s workers’ compensation program) are sometimes credited with being the first to effectively document the increase in overdose deaths involving opioids,[2] and the state was thus one of the first to implement statewide rules more tightly regulating opioid prescribing in 2011.[3] We eventually chose Tennessee because it was a state where we were able to reach doctors and patients, and also because of new legislation on opioid analgesics enacted in 2018.[4] These two states were also chosen in part to present geographic and socioeconomic diversity.
In addition to asking healthcare providers about conflicts of interest, Human Rights Watch screened all providers for pharmaceutical company funding using available databases, such as ProPublica’s Dollars for Docs.[5] The majority of interviewees did not appear to have significant financial relationships to these companies. Human Rights Watch has noted the small number of cases in which a healthcare provider had received money from pharmaceutical companies (above $1,000 per year).
In July 2018, we sent a summary of the findings of our research to the CDC, inviting them to respond. We received a response on August 28, 2018, a copy of which has been included in an annex to this report. In August 2018, Human Rights Watch sent a request for comments to the DEA, the Federation of State Medical Boards, and several state Medicaid and private insurance providers that are mentioned in this report. In September, the DEA and the Federation of State Medical Boards replied to Human Rights Watch’s requests for comment, but as of when this report went to print in December, none of the contacted insurance companies or officials from the Tennessee Department of Health had responded.
All documents cited in the report are either publicly available or on file with Human Rights Watch.
Background
Chronic Non-Cancer Pain: Prevalence, Impact, and Treatment
Chronic pain, typically defined as pain lasting three months or more, is one of the most common health problems in the United States. An estimated 40 million adults have high levels of pain every day, and these individuals report worse health, use the health care system more frequently, and are more likely receive disability benefits.[6] In 2016, the Global Burden of Disease Study estimated that low back pain and migraines were among the five leading causes of ill-health and disability — and the leading cause in high-income, high-middle-income, and middle-income countries.[7]
Chronic pain has serious ramifications not just physically, but psychologically. Depression and anxiety disorders are much more prevalent in individuals experiencing chronic pain than in those who do not.[8] A number of studies have demonstrated that chronic pain patients have an increased risk of suicide, even when controlling for other factors such as socioeconomic status, general health, and psychological disorders.[9] Chronic pain patients also often experience a sense of hopelessness and catastrophic thoughts brought on by fears that their pain might never go away.[10]
Chronic pain can result from a wide range of causes, such as traumatic injury, medical treatment, inflammation, or neuropathic pain.[11] Chronic pain is highly individualized, meaning patients with the same diagnosis can have different pain levels. Because chronic pain has such diverse causes and wide-ranging effects, it poses challenges to treatment[12]: patients react (and fail to respond) to a wide range of interventions for their pain.[13] Psychological treatments can be an important additional tool in treating chronic pain, and cognitive behavioral therapy and stress-reduction techniques have proven helpful to patients with intractable pain.[14]
The 2011 Institute of Medicine (IOM) report “Relieving Pain in America” suggests that it is for these reasons that a simplistic medical approach, in which doctors diagnose and “cure” patients, might not be the norm for patients suffering chronic pain. It cautions that the “road to finding the right combination of treatments … may be a long one,”[15] and suggests a large number of treatment options, including:
- Medications, including opioids and non-opioid analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs)
- Regional anesthetic interventions (including joint and epidural steroid injections, nerve blocks, and implanted devices that deliver analgesic medications directly to the affected area)
- Surgery
- Physiological therapies
- Rehabilitative/Physical therapy
- Complementary and alternative medicine (including massage therapy, supportive group therapy, music therapy, acupuncture, chiropractic spinal manipulation and yoga[16])
According to the IOM report, many Americans receive inadequate pain prevention, assessment and treatment. The report identifies numerous challenges that impede better pain care, including financial incentives that work against the provision of the best, most individualized care; unrealistic patient expectations; a lack of valid and objective pain assessment tools; a lack of training for clinicians in guiding, coaching and assisting patients with pain; a lack of time of primary care providers to do comprehensive assessments; and a dearth of pain specialists.[17]
The Use of Opioid Analgesics in Treating Chronic Non-Cancer Pain
While opioids are a widely used method for treating acute pain, their efficacy and safety in chronic pain management is hotly debated. Scientific evidence of the effectiveness and risks of opioid treatment for chronic non-cancer pain is contradictory and inconclusive.
One 2010 systematic review found that there was only weak evidence to suggest that patients on opioid pain medicines over long time periods experienced clinically significant pain relief.[18] Another systematic review in 2017 regarding the use of high dose opioids in chronic non-cancer pain treatment similarly found a “critical lack of high quality evidence regarding how well high-dose opioids work for the management of chronic non-cancer pain in adults.”[19] The review also found a lack of high quality evidence regarding the presence and severity of adverse events caused by the medications.”[20] A 2018 trial of veterans with common forms of musculoskeletal pain did not find a difference in pain-related functioning between patients treated primarily with non-opioid treatments (culminating in a low dose opioid for a minority), compared to a group of patients treated with increasingly powerful opioid medications, suggesting opioids were not a uniformly superior treatment.[21]
Even if opioid medications are not effective for a majority of chronic pain patients, there is broad — but not unanimous — agreement that for a subgroup of patients they do provide benefits. The 2016 CDC Guideline states that opioid medications may offer benefits to some patients.[22] Similarly, the Federation of State Medical Boards recommends that while patients should be informed of the limited evidence supporting opioid use for treating chronic pain as well as the risks, opioid medication may be appropriate for those whose pain is not resolved with other methods.[23] A 2014 literature review that was part of Germany’s effort to update its chronic pain treatment guidelines concluded that there was sufficient evidence to recommend long-term opioids as an option for chronic pain patients with certain diagnoses while recommending against their use for others.[24] The 2011 IOM reports suggests that the debate over inconclusive scientific findings about opioids should be “set against the testimony of people with pain, many of whom derive substantial relief from opioid drugs.”[25]
Two systematic reviews of national guidelines on opioid prescribing for chronic non-cancer pain identified several general principles that are present in all guidelines.[26] These include conducting a risk assessment before initiating opioid therapy; informing patients about both its benefits and risks; establishing clear goals with the patient; avoiding monotherapy with opioids; closely monitoring the patient for loss of response to the therapy, adverse events and aberrant drug-related behavior; a regular reassessment of the therapy; and discontinuation in case of loss of response, serious adverse effects or serious or repeated aberrant behavior. See Table 1 for a more detailed overview of these general principles.
|
Table 1. General Principles on Initiation, Continuation, and Discontinuation of Opioid Therapy for Chronic Non-Cancer Pain[27] |
|
Patient Selection and Risk Stratification |
|
|
|
|
|
Initiation and Titration |
|
|
|
|
Continuation |
|
|
|
Discontinuation |
|
Chronic Non-Cancer Pain Treatment in the United States
Chronic pain was often undertreated before the 1990s.[29] During that decade, patient advocates, pain specialists, and medical organizations increasingly drew attention to the suffering of chronic pain patients and began calling on practitioners to take greater steps to alleviate patient suffering, including by prescribing opioid analgesics.[30] In 1996, Purdue Pharma, a privately owned pharmaceutical company, introduced a new long-release opioid called OxyContin which it promoted aggressively for chronic pain management. It claimed that the medication was abuse-resistant, a claim that turned out to be false.[31]
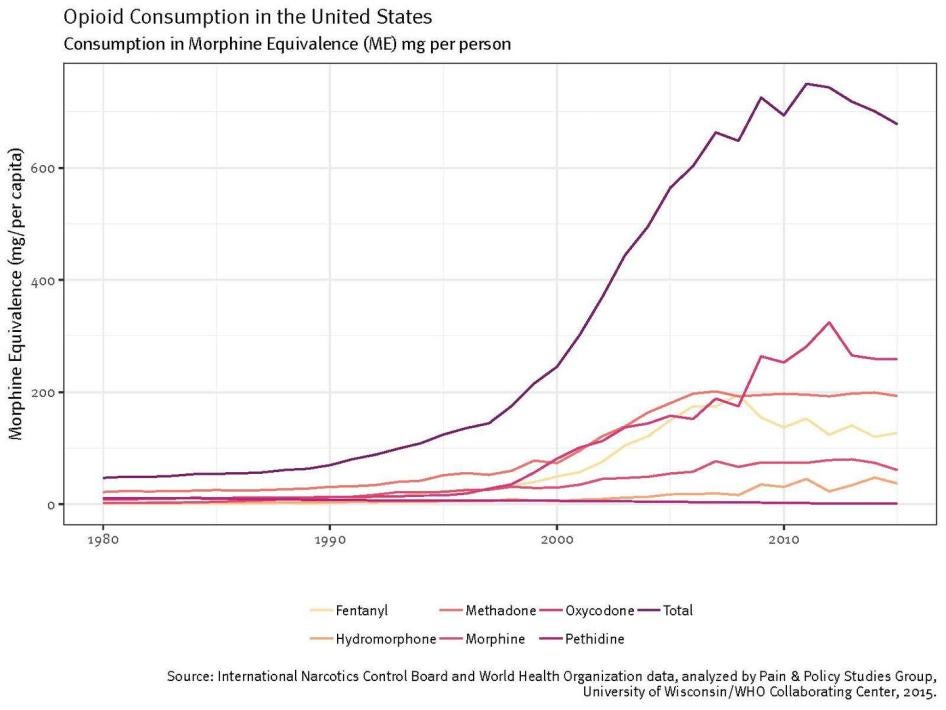
In 2001, the Joint Commission, responsible for accrediting some 21,000 health care organizations in the US, published new standards meant to combat the undertreatment of chronic pain. It encouraged physicians to actively seek to reduce pain levels and treat pain as a “fifth vital sign.”[32] While the Joint Commission did not recommend the use of any specific treatments for pain, in practice healthcare providers began to increase prescribing of opioid analgesics — the quickest and easiest way to address chronic pain. Between 1999 and 2010, prescriptions for opioid analgesics in the US quadrupled.[33] As shown in the graph below, opioid consumption by morphine equivalence — a measurement indicating the strength of a given drug at a given dose — grew astronomically from the 1990s onward: average annual opioid consumption in the US grew from 69.6 morphine equivalents and peaked at 739.8 morphine equivalents in 2011.[34]
Primary care providers, the first point of contact for chronic pain patients, became the main source of opioid prescribing. By 2012, they accounted for nearly half of 289 million opioid prescriptions dispensed by pharmacies.[35] These increases in prescribing happened against a backdrop of a dearth of evidence about the efficacy and safety of opioid medicines in chronic pain management and a widespread lack of training for primary care providers in pain management.[36]
A significant reason for the massive increase in their prescribing appears to have stemmed from providers’ genuine beliefs that they were giving their patients the most financially accessible option to treat their pain. In the 1990s and 2000s, insurance companies tightened reimbursement policies for nonpharmacological interventions, putting many holistic pain clinics out of business;[37] interdisciplinary chronic pain management programs approved by the Accreditation of Rehabilitation Facilities (CARF) declined from 210 in 1998 to 84 in 2005.[38] One retrospective survey found that providers in low-income primary care settings had viewed opioids as the best option to treat pain, partly because it kept patients engaged with the healthcare system and because other treatments like physical therapy were unaffordable.[39] Providers in that study had also been influenced by evidence showing that women and minority groups were more likely to be undertreated for their pain.[40] Research suggests that opioid analgesics are more commonly prescribed long term to patients who are less healthy and experience greater disability: between 2007 and 2016, only three percent of commercially insured individuals were on long-term opioids, versus 14 percent of Medicare patients with disabilities.[41]
These rapid increases in opioid prescribing occurred at a time when government oversight was sorely lacking. Pharmaceutical companies marketed opioid analgesics with misleading claims about their efficacy and risks: for example, the Food and Drug Administration originally approved a label for OxyContin that stated that addiction from the medication was “rare.”[42] While the FDA did enhance warnings about OxyContin’s addictive potential in updated labels from 2001 onward, by that point physicians were writing more than 7 million prescriptions for OxyContin per year.[43] Unscrupulous physicians sold prescriptions in exchange for cash and sometimes for sex.[44] A West Virginia town with just over 3,000 residents was flooded with more than 21 million hydrocodone and oxycodone pills over the span of a decade, or 6,500 pills per person, but that does not seem to have immediately raised red flags for law enforcement.[45] “Pill mills,” or clinics with no real medical purpose other than to write prescriptions in exchange for cash, flourished for years in several states, including in Florida,[46] Ohio,[47] and West Virginia[48] before being shut down. People drove across several states to visit these clinics and re-sell the pills at a huge profit elsewhere.[49] The pharmaceutical industry lobbied against tougher regulation: political action committees (organizations that raise money privately to influence elections or legislation) representing the industry contributed at least $1.5 million to lawmakers who sponsored legislation undermining the DEA’s ability to investigate drug distribution companies that knowingly supplied fraudulent clinics and pharmacies.[50]
The Overdose Crisis
Toward the mid-2000s, public health officials first began noticing an uptick in overdose deaths involving opioids.[51] The scale of the crisis soon became clear, with opioid-related overdose deaths increasing almost threefold from 2002 to 2015.[52] In 2015, 52,404 people died of a drug overdose, more than any previous year on record; 63 percent of these deaths involved opioids. In 2017, the CDC estimated that a record 72,000 people died from accidental overdoses.[53] That same year, President Donald Trump declared the overdose crisis a public health emergency.[54]
The crisis has hit some states and populations particularly hard: opioid overdose deaths tend to be more common among white, poor, and rural populations, and states like West Virginia, Ohio, and Pennsylvania have seen overdose rates skyrocket in recent years.[55] However, there are indications that the impact of the crisis on other communities is growing: opioid-related deaths in African American communities are increasing,[56] and rates of opioid abuse among women are growing much faster than among men.[57]
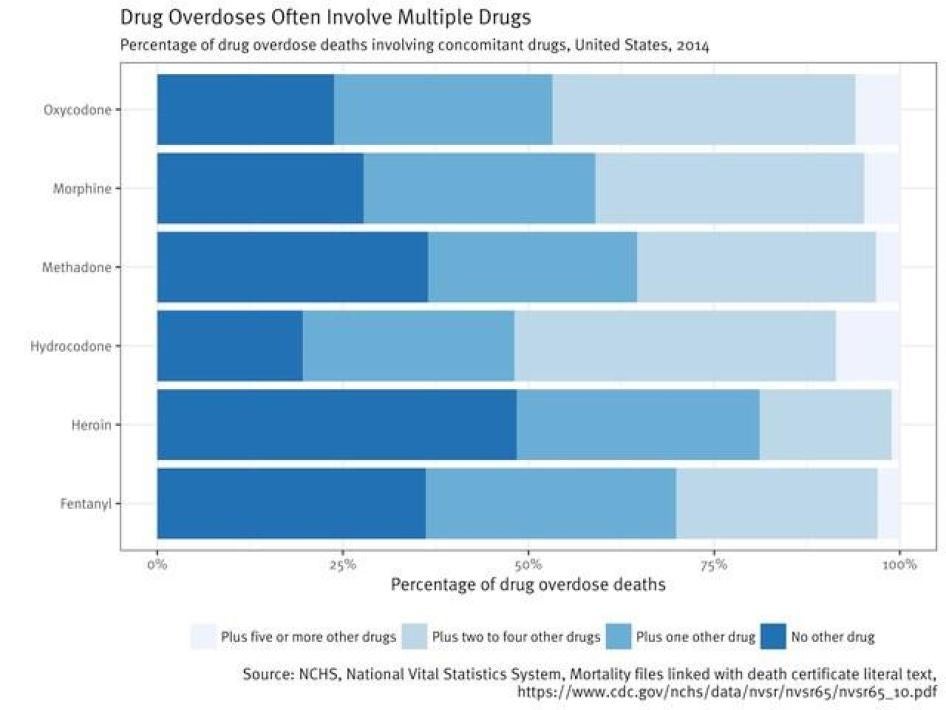
Many overdose deaths have involved prescription opioids. Between 2000 and 2015, opioid overdose deaths were equally split between deaths from heroin, and those from opioid pain medication such as hydrocodone, oxycodone, methadone, and morphine (this is illustrated in Graph 2 below from the CDC).[58] In the last few years, the rate of overdose deaths involving prescription opioids has leveled off but is still a significant contributor to overdose rates, increasing by three percent per year from 2009 to 2016; those deaths have been surpassed by heroin overdose deaths (which increased 33 percent per year from 2010 to 2014 and 19 percent from 2014 to 2016) and fentanyl overdose deaths, which increased by 88 percent per year from 2013 to 2016.[59] Remaining questions about how many deaths are attributable to prescription versus illicit opioids will be discussed in more detail later in this report.
In the 2000s, the growing realization that prescription opioids played a significant role in the overdose crisis set off a major debate about the appropriateness of prescribing these medications for both acute and chronic pain. This period also brought greater scrutiny of pharmaceutical companies that marketed prescription opioids, and patient advocacy groups that accepted money from pharmaceutical companies to campaign for medically appropriate care. The national media began shining a light on rampant abuses by pharmacies and clinics that prescribed and dispensed opioids for no proven medical reason at all.
Government Response
In the face of evidence of the role that prescription opioids played in this public health crisis, government agencies have sought to significantly limit the supply and use of prescription opioids in the US, encourage more conservative prescribing practices, strengthen oversight over the use of these medicines, and crack down on fraudulent prescribing and marketing practices.
Government agencies have imposed greater restrictions on some of the most commonly prescribed opioids,[60] brought high-profile lawsuits against pharmaceutical companies,[61] and cracked down on pharmacies and doctors accused of inappropriately supplying and prescribing opioid medicines.[62] All states but Missouri have implemented prescription monitoring programs, allowing physicians to check whether patients were visiting multiple doctors or pharmacies,[63] and states have cracked down on pill mills.
The government has clearly made cutbacks in prescribing a priority: President Trump, for example, promised to decrease opioid prescriptions by a third in the next three years.[64] The DEA has reinforced these statements with policies meant to limit the manufacturing of opioid analgesics in coming years,[65] and the Justice Department has encouraged insurance companies to help flag above-average prescribers to law enforcement.[66] These efforts have been echoed at the state level: as of 2018, 32 states had passed laws setting limits or guidelines on opioid prescribing.[67]
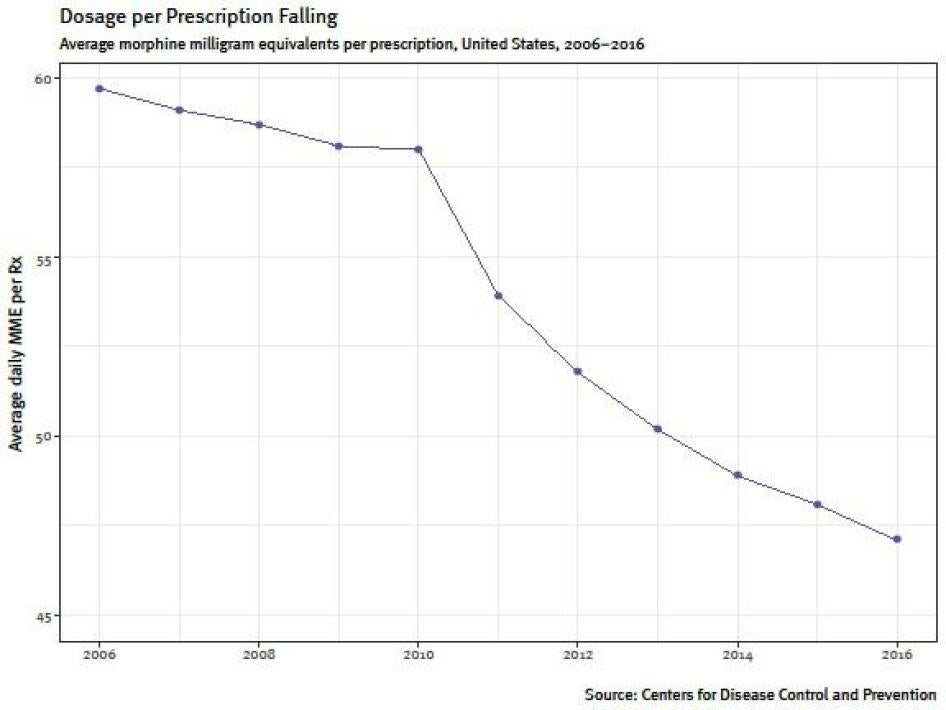
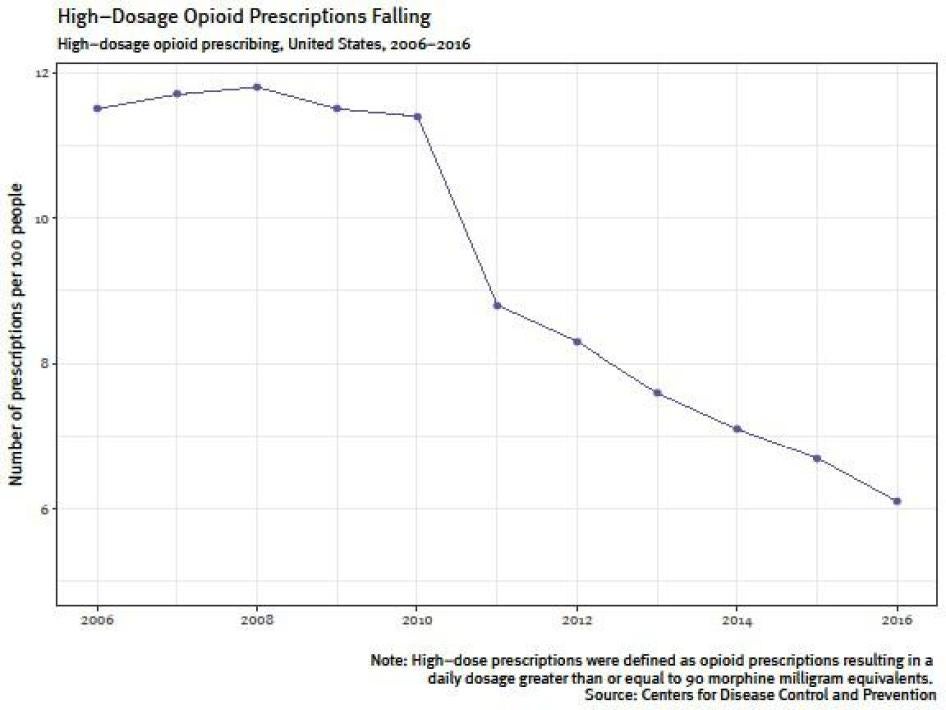
Because a large percentage of the overall volume of prescription opioids used in the country is prescribed for chronic pain — and there is limited evidence as to the efficacy of opioids in treating it — much government rhetoric and policy has focused on long-term prescriptions for that group, and especially on high-dose prescriptions, which studies show are more likely to result in overdose.[68]
However, reducing the prescribing of opioid analgesics poses significant challenges for patients with legitimate medical problems. While these medicines may not be the most effective or safe option for many of these patients, they served a specific purpose: to reduce their pain and improve their quality of life. Any effort to reduce reliance on opioid analgesics for chronic pain management should be accompanied by initiatives to ensure that these patients have access to other treatments for their pain and are not abandoned to suffering without appropriate medical attention.
Moreover, many thousands of chronic pain patients are already taking opioid analgesics, and many have done so for years. These patients should not be abruptly cut off these medicines as that could lead to withdrawal symptoms, anxiety, and increases in pain. Under international human rights standards, actions taken to combat the overdose epidemic should seek to ensure that chronic pain patients are not unnecessarily or disproportionately harmed. If that is unavoidable, the government should implement measures to remedy those harms. Unfortunately, the 2016 National Pain Strategy, a coordinated federal plan to improve prevention and management of chronic pain, does not address this issue at all.
In an effort to address overprescribing and rectify inadequate provider knowledge about the risks versus the benefits of opioid analgesics, the CDC began developing a guideline in 2010 that would help to provide “better clinician guidance on opioid prescribing.”[69] This Guideline is a voluntary set of recommendations aimed at primary care providers. It encourages providers to first try non-opioid alternatives in treating chronic pain, and if they do ultimately resort to opioid prescribing, they are encouraged to avoid prescribing more than 90 milligrams of morphine equivalence (MME) — a value assigned to opioids to signify their strength. However, it also recognizes that some patients will need opioid analgesics, including doses above 90 MME, for their pain and leaves prescribing decisions to the discretion of the physician.
|
Clinical Recommendations: The CDC and VA Guidelines The CDC’s Guideline for Prescribing Opioids for Chronic Pain is addressed to primary care providers — not pain specialists — and is intended to “improve communication between providers and patients about the risks and benefits of opioid therapy for chronic pain, improve the safety and effectiveness of pain treatment, and reduce the risks associated with long-term opioid therapy, including opioid use disorder and overdose.” [70] The following is a summary of the full CDC recommendations:
In 2017, the Department of Veterans Affairs (VA) issued its own clinical guideline as part of a broader initiative to reduce opioid prescribing within the organization. The VA Guideline recommends against initiating long-term opioid therapy for chronic pain, and recommends non-pharmacological or non-opioid treatments instead. The VA Guideline is directive in encouraging providers to “avoid titrating to doses higher than 90 MME.”[71] Unlike the CDC Guideline, the VA Guideline actively encourages tapering, including tapering without patient consent: it says tapers should be initiated by a provider when the “risks of long-term opioid therapy outweigh benefits.” It also states that patients on long-term opioids “may threaten suicide when providers recommend discontinuation of opioids,” but that “continuing (long-term-opioid therapy) to ‘prevent suicide’ in someone with chronic pain is not recommended as an appropriate response if suicide risk is high or increases.” Instead, the VA encourages providers to involve behavioral health providers to “treat a patient who becomes destabilized as a result of a medically appropriate decision to taper or cease [opioids].”[72] The VA asserts that “the CDC Guideline did not form the basis of the deliberations on the strength or the direction of these recommendations,” but the authors state they were aware of the CDC Guideline and came to some similar conclusions.[73] |
The CDC Guideline offers carefully balanced recommendations that safeguard provider discretion and provide exceptions for chronic pain patients in need of opioid analgesics. Unfortunately, some of the regulations, policies and recommendations it appears to have inspired do not. According to the CDC, 46 states have implemented guidelines or other policies aligned with its Guideline. However, in our review, not all states strictly followed recommendations made in the CDC Guideline. For example, Human Rights Watch found that six state Medicaid programs imposed maximum dosages and involuntary tapering on patients. All of these policies were passed after the publication of the CDC Guideline in 2016, and three of them explicitly state that these policies were motivated by the CDC Guideline.[74] As mentioned previously, neither involuntarily tapering nor mandatory dosages are recommended in the CDC Guideline.
The CDC does not say how the Guideline has influenced insurance companies and pharmacy policies, however our research found that these companies publicly prioritize cutbacks in prescribing, without any indication that they are monitoring the impact that such cutbacks have on patients or assurances that alternative treatments are available for those patients.
Our research focused primarily on the effect these policy initiatives have had on chronic pain patients who already receive opioid analgesics, and on the physicians who care for them. Both clinicians and patients told Human Rights Watch that prescribing practices had changed in ways that are frequently inconsistent with the recommendations in the Guideline. Many healthcare providers impose involuntary dose reductions on patients; offer them little or no support in the tapering process; and fail to refer patients to mental health professionals or other services when patients experience a deterioration in their health as a result of tapering. Patients are tapered despite deriving benefits from the medication, having no record of violating risk-screening protocols, and being compliant with clinic regulations like urine drug testing and pill counts.
This kind of tapering is inconsistent with the CDC Guideline. In a letter to Human Rights Watch, the CDC reaffirmed that the Guideline “does not provide support for involuntary or precipitous tapering, and that such practice can be associated with withdrawal symptoms, damage to the clinician-patient relationship, and patients obtaining opioids from other sources. It also emphasized that clinicians have a responsibility to carefully manage opioid therapy and not abandon patients in chronic pain, and that obtaining patient buy-in before tapering is critical.”[75]
While several of the physicians we interviewed who were involuntarily tapering their patients were aware that this practice was not encouraged by the CDC, they described an atmosphere in which they felt that they had no choice but to prescribe at, or below, the 90 morphine milligram equivalent threshold described in the CDC guideline, even when they believed the patient benefited from higher doses of medication. They described a number of prods and pressures that made them feel compelled to taper patients on higher doses: the fear of scrutiny by law enforcement agencies like the DEA, which registers every prescriber of controlled substances in the country and has ready access to information about prescribing practices of most providers; monitoring by state medical boards, which are responsible for licensing practitioners; and state laws and regulations, which in some states mandate dose caps or otherwise reinforce the 90 morphine milligram equivalent threshold defined in the CDC Guideline. Amidst these pressures, providers said they felt that the only way to protect themselves from liability was to stay rigidly at or below the CDC Guideline’s 90 morphine milligram equivalent threshold and to disregard the emphasis on individualized patient care and respect for patient consent that are recognized within the Guideline (see “Patients as Liabilities” for testimonies from providers).
The consequences for chronic pain patients have been real: many told Human Rights Watch they have been forced to quit working, limit their activities, and even in some cases remain housebound due to pain. Some patients said they suffered from intense anxiety and suicidal thoughts during and after the tapering process. Other patients said they faced increasing difficulty finding a doctor willing to accept them as patients because they were on high-dose opioids.
Current data are not available to more precisely indicate the impact involuntary tapering has on chronic pain patients’ physical and mental health. It is also unclear to what extent involuntary tapering and overall inaccessibility of prescription opioids drive illicit drug use, as the few studies on this issue are inconclusive about the causal relationship between the two.[76]
Faced with an overdose crisis of unprecedented proportions, federal and state governments have a duty to respond to protect people from accidental overdose death. Any policy to address the overdose crisis should consider and minimize potential unintended harms, including for patients suffering from chronic pain who have a medical need for opioid analgesics.
|
Involuntary vs. Voluntary Tapering Many thousands of chronic pain patients are currently on high-dose opioid analgesics.[77] For some, these medicines are a lifeline, improving their pain control and allowing them to take part in family, social or work life. For others, the medicines may offer little or no benefit. As the government tries to reduce the volume of prescription opioids in society, this raises complex questions about how to taper off patients who do not benefit from the medicines or get unnecessarily high doses. The 2016 CDC Guideline encourages obtaining buy-in from patients before initiating a taper, and says physicians should engage mental health specialists to help a patient manage potential anxiety, which may be due to the fear that their pain will return or to the fact that they are physically dependent on the medication and could suffer withdrawal. In a letter to Human Rights Watch, CDC officials clarified this position to mean that tapering patients from opioid medicines should always be voluntary, with their consent.[78] Despite this emphasis on consent, many patients report being tapered off their medication without their consent, and the Department of Veterans Affairs/Department of Defense Guideline on opioid prescribing seems to endorse involuntary tapering. In either scenario, patients face significant challenges tapering themselves to off opioids. One 2017 systematic review of 67 studies examined several strategies for reducing long-term opioid prescribing for chronic pain, including multidisciplinary pain care and close follow-up of patients, though it noted that such “team-based, intensive support would require additional resources to implement in primary care settings, where most opioids are prescribed.”[79] The study found limited evidence that patients’ pain became less severe or that their functionality or quality of life improved after tapering.[80] Another 2011 study that examined tapering chronic pain patients who had developed a substance use disorder found high failure rates but concluded that medication assisted treatment, such as buprenorphine, improved the patient success rate.[81] In its guideline, the CDC notes that there is a dearth of high-quality studies on different tapering protocols, but it recommends that primary care physicians adjust the pace of a taper to a patient’s needs, and collaborate with other medical professionals, such as mental health specialists, to manage anxiety that the taper might induce.[82] At the time of writing, few studies had examined outcomes of involuntary tapering on patients. A 2017 survey of 509 Veterans Health Administration chronic pain patients discontinued from opioid medication found that 47 patients (9.2 percent) exhibited signs of suicidal ideation, while twelve patients (2.4 percent) attempted suicide.[83] As the study only captured information reported to medical professionals and only followed patient outcomes for one year, this likely underestimates the actual number of such cases. The authors conclude that patients discontinued from prescription opioids, whether diagnosed with a substance use disorder or not, may require close monitoring and risk prevention. Another study suggests that patients who are involuntarily tapered off opioids are less likely to follow up in primary care than patients who aren’t (65 percent compared to 88 percent) and that “discontinuation of opioids may carry risks that should be thoughtfully assessed and managed.”[84] It is unclear how much research is currently under way to study tapering practices and their consequences. There should clearly be more research into safe methods of opioid tapering, and data should be captured on the consequences of denying adequate medical treatment to chronic pain patients, including in cases where those patients are involuntarily tapered. |
Patient Plight
Involuntary and Inappropriate Tapering of Patients on High Doses of Opioids
Twenty-six patients, mostly in Washington State and Tennessee, told Human Rights Watch that their healthcare providers had involuntarily tapered them or were in the process of doing so. A dozen providers, including both primary care providers and pain specialists, also mostly from those states, said that they were involuntarily tapering all patients who were on opioid doses above — and in some cases even those who were under — the 90 morphine milligram equivalent threshold described in the CDC. Another nine healthcare providers said that they were not planning to wean existing patients off opioids without their consent, but said that they had stopped accepting new chronic pain patients who required opioid analgesics, particularly those patients who were already on high-dose opioids.
Stephanie Miller, 49, told Human Rights Watch that she suffers from spinal stenosis (a narrowing of the spaces in one’s spine that puts pressure on nerves) and cervical radiculopathy (a pinched nerve in her neck), which give her bouts of sharp pain in her neck and an intense ache in her back that feels “like a rod in my spine.” Since 1998, the Washington State resident has been taking a daily dose of oxycodone equivalent to 315 MME, which she says helped her live a stable life. In January 2018, even though Miller had routinely submitted to urine drug testing, pill counts, and other kinds of screening, her provider told her she would have to reduce her dose to 90 morphine equivalents by June, because she feared losing her license if she continued to prescribe high doses.
The lower doses of oxycodone have significantly reduced her quality of life, Miller told Human Rights Watch, leading her to contemplate suicide:
I never had a pain-free life, but I could do little things like washing the dishes, not hiking or dancing. Now [with the reduced dose of medication] it’s: okay, I can’t vacuum today, can’t sweep the floor today. It’s changing everything and it’s terrifying….
I feel like I got a new diagnosis when I got that letter saying I should go down to 90 MME. It felt like a ticking clock for when my life was going to end. If it stays this way, I am going to end my life. I have a locked box where I keep my medications, and there is a note all ready that says I do not blame my providers, I blame the government.
I always thought I would keep fighting, but now I’m facing something that’s completely and totally out of my control. When I’m lying in my bed my heart is beating so fast I’m afraid of a heart attack. Why put it off?[85]
Miller’s health has declined so significantly that she can no longer shower on her own and required assistance taking care of her dog. Her Medicaid plan has since granted her 20 more hours with a home health aide per week.
|
Physical Dependence vs. Addiction Many of the chronic pain patients interviewed for this report have been receiving opioid analgesics for their pain over extended periods of time. That means that their bodies have gotten used to a regular dose of the medications and that abrupt discontinuation of the treatment can lead to withdrawal symptoms, just as would be the case with other prescription medications (or non-prescription substances such as nicotine). Common withdrawal symptoms include anxiety, agitation, aching, nausea and insomnia. The fact that a patient may face such symptoms if their medications are discontinued does not mean that they have a substance use disorder or are “addicted to pain pills.” The National Institute on Drug Abuse (NIDA) — a federal agency that works to advance research about and medical care for drug users — distinguishes between physical dependence, which occurs when a patient takes a certain medication over an extended period and is normal, and substance use disorder.[86] The latter is defined as compulsive drug use despite harmful consequences, including a failure to stop using the drug; failure to meet work, social, or family obligations; and sometimes tolerance and withdrawal. NIDA clarifies that “physical dependence can happen with the chronic use of many drugs — including many prescription drugs, even if taken as instructed.”[87] A similar distinction is made by a host of other US and international medical standards and institutions: the International Classification of Mental and Behavioral Disorders (ICD-10), the Diagnostic Statistic Manual (DSM) of the American Psychiatric Association,[88] and the American Academy of Addiction Medicine.[89] The patients we interviewed all said that they used their medications as prescribed and almost all of them regularly underwent urine tests and pill counts, allowing their physicians to confirm that they took their medications as prescribed. They also told us that their medicines allowed them to participate in family life, social events or work. |
Bob Green, a 67-year-old retiree with the autoimmune disorder Sjogren’s disease, was involuntarily tapered beginning in January 2018 despite being compliant with his physician’s pill count and urine drug test requirements. Sjogren’s disease attacks the body’s mucosal linings, giving him dry eyes and mouth, as well as a “rust-in-the-joints type feeling.” It has exacerbated two previous army injuries. After a neck operation in 2012 his health “really went haywire,” he says. “For whatever reason that rust feeling has been so intense since the surgery — whether it’s directly related, I can’t tell you, but it seems like my nervous system just exploded on me…. I have pain in my back, feet, hands, arms.”
In 2012, he was referred to a pain specialist who prescribed him opioids to keep the pain under control while he was at his job: Green had plans to work until 70, and he worried that he could lose his house if he didn’t, he told Human Rights Watch. In 2016, the Department of Veterans Affairs approved Green for service-connected disability compensation, allowing him to retire earlier than planned. That decision couldn’t have come soon enough: soon afterward, his provider said that she would no longer prescribe him high-dose opioids because she feared punishment by federal law enforcement or state medical board authorities. Green said that he wouldn’t have been able to wean off opioids, which “keep [him] working at 110% and getting up at 5am every day,” if he was still at his job.
It [the weaning] has made my life really difficult, but what are my options?... I have to be grateful for the fact that the VA rated me as 100% service-connected disabled. When I officially retired I have the extra time to sit in a massage chair for half an hour in the morning, to do physical therapy and reiki. Do I have much of a life? No, I have about 10% of a life. The pain that I have pretty much keeps me housebound.[90]
Marty Revolloso, a Medicaid patient from San Antonio, Texas, was hiking in 2011 with friends when he slid on some gravel and fell off a cliff. Both legs were shattered and his left hand severed from his body: “The impact was so great it shattered my ankles, my feet, my shins, and the shock traveled up through my body and shattered my spine like a stack of bricks.”[91] He spent six months in a full-body cast to heal his spine, and his legs have undergone intensive reconstruction.
He suffers from severe pain which doctors have told him will persist for the rest of his life. Prescription opioids provide him some relief: for the past several years, he had been on 180 MME of medication, which he says allowed him to start working part-time in IT and taking online classes. “Before, the days would just blend together. I would get up to go to the bathroom, all I could do was just lie there day after day, it was like being in the hospital again,” he said. “When he [the doctor] increased my medications, my whole life changed — I didn’t even know I could make that kind of progress.”
According to Revolloso, in April 2018, the physician assistant at his doctor’s office said his dose would be cut back to half its current level, because his insurance provider for Medicaid would no longer cover it. Texas Medicaid has a policy that mandates opioid tapering down to 90 MME in 2018, which “will be applied for all clients, except for clients diagnosed with cancer or receiving palliative or hospice care.”[92]
Revolloso said that in the beginning, his clinic was unaware of the change. They attempted prescribe him a lower dose of 120 MME and obtain an override from the insurance company by sending a prior authorization. But when Marty went to the pharmacy, he said he realized the insurance company had rejected this attempt.
In a recorded phone conversation with his doctor’s office, a nurse explained the issue:
It’s not going to go through because [the insurer] is not paying for anybody to have a morphine equivalency over 90. We’ve had to do this for all our 500 to 600 patients of [this insurer], we haven’t been able to get anybody approved for a morphine equivalency over 90…. The only way to get a higher dose approved is if you have cancer.
We’ve had a lot of patients call and just tell us, because member services and the pharmacy services is telling them one thing, but when it comes down to us actually submitting the prior authorization they have denied every single one of them. The only way we’ve been able to get them approved is if we lower them to 90.[93]
Revolloso told Human Rights Watch that the change in medication wiped out much of his recovery: “I was flat on my back from the pain… I couldn’t eat, couldn’t get up, couldn’t bathe, I stank.” He later learned he could pay out of pocket for the medication he needed. But while the $120 he would have to pay might be a small price for some, Marty earns only $740 per month from disability payments. “It was a pretty big struggle, because it caught me totally off guard — this month at least I’ll be able to budget.” Human Rights Watch did not speak with Revolloso’s healthcare provider, because Revolloso said he feared that outside scrutiny might provoke his physician to terminate his care.
While in the above cases, health providers explained the rationale behind decisions to taper their patients off opioids without patient consent, this was not always the path taken by providers, some of whom dramatically reduced a patient’s dose involuntarily, sometimes without even holding an in-person consultation to explain the change.
Jennifer Vinnard of Vancouver, Washington, for example, found out that her prescription had been slashed by more than half from 250 to 100 MME when she showed up at the pharmacy one day for a refill, despite the fact that she had always been a compliant patient and underwent urine drug testing regularly. Vinnard had lifelong hip problems and in 2014 herniated multiple discs in her spine and underwent four surgeries, leading to crippling pain in her neck, for which she was prescribed opioids. After her visit to the pharmacy, she wrote to her provider, asking why her medication had been changed without warning. After several weeks’ delay, her provider finally sent her an email containing the following[94]:
The bottom line of these [CDC] guidelines is that all patient’s [sic] need to be around 100mg of morphine per day… I know you have done better with the way your regimen is but his [sic] is not going to be sustainable. In order to keep prescribing I need to make reductions… We as a clinic need to make changes if we are going to stay open.[95]
The dose reduction has changed Vinnard’s life for the worse: she recently bought a new home with her husband, but was unable to help set up the house because she is often in too much pain to help with even relatively simple chores: “Since the reductions, I have to wait for my husband to do even little things,” she says. “I sit in front of a space heater for hours each day, sit in the sun or take baths in an attempt to help the pain. But life doesn’t stop because I hurt.”[96]
Similarly, Robin Gordon, a 48-year-old veteran from Oakland, Tennessee who receives care from the VA, discovered her dose had been cut only when she received her monthly prescription in the mail. Gordon’s pain stems from a 1996 car accident in which she was hit in the driver side door after pulling out of an apartment complex. For about five years after her accident she didn’t experience much pain, but then things started going downhill: she had problems with the knee impacted by the crash and shooting pain down her neck. She has been diagnosed with degenerative disc disease and has tried nerve ablations, TENS units (a device that sends electrical impulses across the surface of the skin), and heating pads to manage the pain. She has been on opioid analgesics since 2005, at a current daily dose of 105 MME. “I don’t like pain medication, I’ve had family that was addicted and was always leery of it. But if it’s at the point where you have to be in a wheelchair you’re in so much pain, I’ll take the medication,” she said.[97]
But in May 2018, Gordon received fewer pills from her provider than usual: her dose had been cut back to 70 MME. While her provider had noted several times during office visits that opioids were risky, she never suggested that she would involuntarily taper Gordon, who had always complied with random urine drug testing. After Gordon sent an email requesting to know why her dose had been changed, she received a response from her physician, who referred her to the VA Opioid Safety Initiative (which includes the VA guideline for opioid prescribing),[98] and sent her several articles about pain management. But Gordon still felt caught off guard by the change, and found her health deteriorating. She told Human Rights Watch:
They should have done this with an in-person visit. I would have been happy with just a phone call. This is my life you’re playing with and you need to consult me first. I have plenty of other health problems, so this at least was stable.[99]
Gordon’s abrupt and nonconsensual tapering within the VA is not unique: Human Rights Watch spoke to three other veterans in Tennessee, all of whom had been tapered without an in-person consultation with their doctor first, and none of their providers had previously voiced concerns that they might be abusing their medication. Similar stories documented elsewhere in the media have shown that such rapid and unsupported changes in VA facilities appear to have resulted in suicide and drug overdose.[100]
Involuntary Tapering and Suicide
There is a well-studied correlation between chronic pain and suicidal behavior. Involuntarily tapering a patient, particularly those who have been on high-dose opioids for long periods, has major physical and mental health repercussions and has been shown to increase the risk of suicidal behavior. As noted above, one study found that 9.2 percent of involuntarily tapered patients reported suicidal thoughts to their healthcare provider while 2.4 percent attempted suicide.[101] The study’s authors say they believe that these incidents were underreported.
Even if medical practice has changed, and some patients put on high-dose opioids in the 1990s and 2000s would not be today, tapering is still difficult and anxiety-inducing for many patients and may leave them in uncontrolled pain. While there have been some efforts to document individual cases in which pain patients commit suicide following involuntary tapering, there have been no public efforts to study this issue more systematically.[102]
The provider who cared for Maria Higginbotham in Washington State, who was reducing dosages for more than 200 other patients, described the conversations he had with patients he was tapering:
It’s so difficult, it’s emotionally just stressful and time-consuming to explain this to patients every time they come in because it triggers lots of fear and anger. I don’t have a week that goes by that I don’t have at least one patient who insinuates that suicide is a possibility. We start talking about pain pumps and spinal cord stimulator implants, but most of them have already tried all the other medications. They’ve gone through all those things, and we feel like we’re limited as to what we can offer them instead.[103]
Tonya Schuler, a patient in West Virginia, was diagnosed with chronic regional pain syndrome (CRPS) after a routine carpal tunnel surgery. The condition, which is typically the result of traumatic injury or the malfunctioning of the nervous system, causes severe pain and can even result in changes in skin temperature, color, or swelling in the affected limb.[104] Her pain management clinic in Pittsburgh, Pennsylvania is currently weaning her down to a dose of 90 MME despite her concern that she could experience a dangerous increase in her heart rate — an issue common among CRPS patients[105] — as a result.
This is called the suicide disease, and I can see why, because I’m at the early stages of this. There is no way one person can live in this amount of pain. You can’t. You wonder, what’s your purpose?[106]
Abandoned Patients and Overwhelmed Physicians
Of the 44 patients interviewed by Human Rights Watch, ten were struggling to find care at the time they were interviewed. The reasons were varied: in two cases, the patient moved to a new state and was unable to find care. In two cases a physician retired, and in one case a provider ceased practicing without informing the patient why. In three cases, primary care providers determined they were no longer comfortable treating high-dose patients: these providers referred their patients to pain management doctors, but those patients were unable to find a doctor willing to take them on. In one case, a patient had weaned herself off opioids temporarily because she was pregnant — after her pregnancy, she could no longer find a doctor willing to treat her with opioids; and one patient with cancer had her pain medication managed by an oncologist, but upon completing treatment she struggled to find a pain doctor willing to care for her. One patient struggled to find care after the shutdown of his pain clinic, but was able to find care four months later.
Chronic pain patients spoke more generally of the increasing challenges they faced in finding health providers willing to care for them, but this was especially true for patients who required opioids for treatment. The patients who spoke to Human Rights Watch repeatedly said they felt abandoned by the medical community. They expressed anger and frustration over the fact that they felt stereotyped as drug-seekers when they visited a clinic or pharmacy. In many cases, they said the stigma of being a chronic pain patient on opioids had become so great that they avoided telling even close friends and relatives about their medication. In several cases, patients told us they were only able to find a provider a four- or five-hour drive away — a journey that they often had to make monthly to see their doctor or to pick up their prescriptions.
When pain specialist Dr. John Baumeister moved his practice from the suburbs of Seattle to a rural community in eastern Washington a few years ago, many of his patients found themselves unable to find care in the Seattle area. They are forced to make the more than three-hour journey from Seattle once a month to visit him: “Some 50 percent of my patients drive more than 225 miles to see me every two months,” he said. “They do this because doctors in the Seattle area are unwilling to prescribe opioids to chronic pain patients.”[107]
One of Dr. Baumeister’s patients is 51-year-old Nicole Rogers, who makes the journey every month. She has had arthritis and other related conditions since she was 25, and has received opioid medications, the only pain treatment that has provided her significant relief, since the 1990s. In 2014 she was diagnosed with stage-three breast cancer and received pain care from her oncologist. But after her cancer went into remission, she could not find any doctors willing to treat her for pain in the Seattle area: “It’s too hard to find a pain doctor who will prescribe medication, it’s almost impossible,” she said. “I can barely walk to my mailbox and that’s half a block, I’m suffering a lot, and now I have to drive four hours each way once a month.”[108]
One patient said that she felt abandoned by a provider with whom she had a long-term relationship and pushed toward clinics she did not trust. Gail Gray, a 52-year-old from the remote rural town of Celina, Tennessee, was diagnosed with degenerative disc disorder and spinal stenosis when she was 35, and has had four back operations in the last five years. Because other treatments did not provide adequate pain relief, her doctor prescribed low doses of morphine for her 15 years ago. After her second back operation in 2013, her primary care doctor raised her dose to approximately 450 MME in response to her increasing pain. In 2017, however, that same doctor began cutting her back 30 milligrams at a time, citing the CDC Guideline and his fear that the DEA could intervene in his practice. That doctor brought her down to 240 MME, but then said that he was no longer comfortable prescribing her any morphine at all and suggested she transfer her care to a pain clinic. She found a clinic one hour away, but worries that she has given up a caring doctor for a pill mill:
They don’t take any kind of insurance and it costs $175 per visit, cash…. I’m worried it’s a pill mill because they give minimal service and the visit only lasts 15 minutes. [The doctor] barely looked at me…. I’m not comfortable with this. I feel like he [my primary care doctor] has pushed me into doing something that’s not right, and I don’t want to break the law.[109]
Some healthcare providers told Human Rights Watch that they had been flooded with patients because nearby medical clinics had either been shut down or had closed their doors to chronic pain patients who had previously been prescribed opioids.
For example, Dr. Jon Olson[110] in Edmonds, Washington, who has practiced pain management for 33 years, said that his pain clinic had been flooded with patients, as pain clinics in his area shut down and primary care doctors stopped almost all opioid prescribing. Dr. Olson said he tried to employ a holistic approach with his patients, and that he spent 45 minutes or more with many of them. He told Human Rights Watch that he has had to delay retirement because his clinic, where he works with one other physician and a nurse practitioner, was unable to find a younger doctor willing to take over his patients.
Primary care in this neighborhood walked away from prescribing opioids permanently. This trend sped up in the last year and a half or two, when the CDC guidelines kicked in.
In this area I can think up off the top of my head 35 prescribers who have been shut down. The harassment makes practice unpleasant… I could have retired nine years ago but I have close to 1,000 patients who have better lives thanks to our clinic. What would they do? For ten months we tried a replacement [physician] so that I could retire, but he was concerned about prescribing and didn’t want to work with these patients. So I had to come out of retirement because otherwise nobody would take them.[111]
In Maine, where opioid prescribing of over 100 MME for chronic pain is now against state law, primary care doctor Cathleen London says she has been able to treat some chronic pain patients with alternatives like buprenorphine, which is typically used to treat drug dependency but can also be effective for pain. While Dr. London moved to a rural area of Maine with the goal of working primarily in addiction medicine, she says she has been overwhelmed by the number of chronic pain patients seeking help.
A day does not go by when I don’t get a call [from a chronic pain patient]. I don’t want to spend my day just doing pain patients but I’ve done way more of it since I moved here than I did before, because there is such a need and nobody is doing it…. I have patients from an Indian [Native American] reservation two hours away, and the last nurse practitioner they had took everybody off their pain medication, including people with [severe pain].[112]
Several doctors admitted that they were reluctant to treat chronic pain patients and often turned them away out of fear of liability, even when they believed that the patients had legitimate pain issues. According to one physical medicine doctor in Spokane, Washington: “At this point I won’t start anyone new on opioids, and we aren’t taking new chronic pain patients unless it’s something like traumatic injury or brain disorders.”[113] He said this policy applied for all 12 of the physicians he supervises.
“There are more and more doctors who are discontinuing prescribing,” said Dr. Lucinda Grande, a family practitioner from Lacey, Washington. “There is a local practice here that decided as a group that they’re just not going to [treat people with] chronic opioids and maybe not even acute opioids anymore. That is so irresponsible, taking the easy way out. It’s doing the community a disservice and it’s socially irresponsible, but it’s easy for them because all they have to do is say no.”[114]
Some pain specialists suggested that primary care doctors in their area had essentially stopped prescribing opioids, even to patients who only needed very low doses. One Washington pain specialist said:
This morning I had a new patient I’d seen five to six years ago, but he’s back because his family doctor does not want to manage his medication anymore. He takes five to six Tylenol codeine a day, that's 30-40 MME. It’s not even close to the 90 limit, and yet primary care is washing its hands of these patients. That means we [pain specialists] get even more.[115]
The Fate of Patients of Shuttered Pain Clinics
In recent years, government agencies have shut down dozens of pain clinics across the country. Sometimes these closures can affect tens of thousands of patients: the Tennessee-based Comprehensive Specialists closed its doors in July 2018, after potentially fraudulent Medicare billing came to light amidst media scrutiny, leaving some 48,000 patients at 50 different clinics — 30 within Tennessee itself — suddenly deprived of care.[116] In Florida, which became infamous for having hundreds of doctors who provided opioids to patients for no true medical purpose and often in exchange for cash or other favors (“pill mills”), the number of pain clinics went from more than 900 in the 2009-2010 fiscal year to just 371 by 2013-2014.[117]
While some or many of these clinics may not have been legitimate medical practices, the closure of clinics with hundreds and in some cases thousands of patients on opioid medications poses important challenges for continuity of care. If patients who are on opioids are suddenly cut off, they will experience significant withdrawal symptoms as well as a return of their pain. If continuity of care is not ensured, these patients are at increased risk of self-harm, including suicide, or reverting to street drugs or alcohol to stave off withdrawal symptoms or pain.
Government agencies have a duty to take adequate steps to ensure the continuity of care for patients affected when they close down pain clinics or revoke physicians’ licenses, even when those measures against clinics and physicians result from alleged violations of the law. However, media reports across multiple states have documented that patients’ care is often abruptly terminated when pain clinics are closed down.[118] In some of these cases, patients say they were not warned — and in some cases not even informed of the change until arriving to receive a prescription. Other healthcare providers face difficulties rapidly absorbing large numbers of patients. The DEA did not respond to a specific request for information from Human Rights Watch on contingency planning for patients in such cases.[119]
In 2016, the Washington State Attorney General’s Office shut down Seattle Pain Centers, a network of clinics in eight cities, charging medical director Dr. Frank Li with the overdose deaths of 16 patients, many of whom had filled a prescription from his office in the weeks or months before their deaths.[120] The charges state that Dr. Li failed to use risk-screening tools such as mental health screening, urine drug testing, and pill counts and did not hire a sufficient number of qualified staff to deal with Seattle Pain Centers’ patients. The shut-down affected clinics in eight different cities, an estimated 12,000 Medicaid and Medicare patients, and up to a total of 25,000 people across the state.[121] Within a week of the charges being announced, only one location remained open, leaving thousands of patients without care.[122] Ultimately, Dr. Li’s license was suspended by Washington State[123] and his ability to prescribe controlled substances was revoked by the DEA.[124]
While state officials had been aware of overdose deaths among Dr. Li’s patients for several years before shutting down the Seattle Pain Centers, state officials said they were unable to warn any patients or doctors about the shut-down due to legal constraints.[125] The Washington State Department of Health set up a hotline after the shut-down, and large hospitals and clinics in the Seattle area absorbed approximately 2,000 patients, but many others were left without care.[126] Investigations by news media alleged that the shutdown resulted in at least one documented suicide, and at least 1,500 patients sought care in emergency rooms as patients scrambled to find other doctors to take over their care.[127]
Garrett Beyer was one of the patients affected by Seattle Pain Centers’ closure. Beyer suffers from butterfly vertebrae — a rare, genetic spinal anomaly that can lead to intense low back pain — which was discovered after a car crash as a teenager. Now 29 years old and living in Spokane, Washington, he began pain management with his pediatric doctor at 17, trying many different types of treatments, including physical therapy, a TENS unit, and corticosteroid injections.
His doctor eventually put him on opioid pain medication, which reduced his pain enough that he began pursuing an associate’s degree. He told Human Rights Watch that he had been on a dose of 80 MME for six years when in 2016, the branch of Seattle Pain Centers in Spokane where he had been a patient since leaving pediatric care was shut down, abruptly leaving him without medication. Beyer’s life was transformed by the change, and he worried he risked following a path similar to his father’s: his father suffered chronic back pain after a car accident but was cut off his pain medication in 2015 when his doctor retired, and he couldn’t find another physician willing to take him on as a patient. Garrett believes that his father’s suicide, which followed shortly after, was driven by the loss of his pain management.
I thought of suicide: I was sure I would follow in my dad’s footsteps. It’s not just the pain, it’s the hopelessness, the feeling that it will never end. My nerves were on fire. Alcohol was the only way I could cope, I would lay in my room in the dark and drink.[128]
Beyer said that for three months, he drank to dull his pain. It took him four months to find another provider, as he had difficulty recovering his medical records from the clinic that was closed down. To his relief, his new doctor was willing to prescribe him opioid analgesics. He said: “They took a look at my x-rays and it was pretty clear that something was wrong with me.”[129]
Beyer is one of the lucky ones — two patients who spoke to Human Rights Watch spent longer periods without care and admitted to self-medicating with alcohol, buying opioid painkillers illegally, or even pretending to have a substance use disorder in order to be admitted to methadone clinics.[130]
Access to Alternative Treatments
Chronic pain patients can have complex medical histories — multiple coexisting diseases or a history of surgeries and accidents — and often require care from more than one doctor. For this reason, the CDC Guideline recommends that clinicians consider a wide range of treatment options for chronic pain: “multimodal and multidisciplinary therapies (e.g. therapies that combine exercise and related therapies with psychologically-based approaches) can help reduce pain and improve function more effectively than single modalities.”[131] While studies show that the understanding of multimodal pain management is in its infancy, the evidence suggests that patients react to a wide range of interventions.[132] According to at least one study in 2016, cognitive behavioral therapy, a method of treatment that focuses in part on the development of coping behaviors, and stress-reduction techniques have also proven helpful to patients with intractable pain.[133]
The CDC Guideline and various other authorities — such as the Federation of State Medical Boards[134] and the Department of Veterans Affairs — recommend that opioids should only be used to treat chronic pain after or in combination with alternatives.
Our investigation, however, found that many alternative treatment options are not actually accessible to patients. Almost all providers we interviewed said that they had struggled to manage patients’ pain appropriately because alternative and supplemental therapies were not reimbursed by insurance. Likewise, patients said their insurance often did not fully cover non-opioid treatments their doctors discussed with them. This is consistent with the National Pain Strategy observation that:
Access to high-quality integrated care based on clinical evidence is hindered by many challenges. Pain management often is limited to pharmacological treatment offered by a primary care practitioner or to procedure-oriented and incentivized specialty care that is neither coordinated nor aligned with best available evidence or expected outcomes. This situation is especially relevant for people with high-impact chronic pain, where integrated care is likely to be most effective.[135]
When alternatives are not accessible, providers are involuntarily tapering patients off opioids without offering them anything instead.
Few of the patients interviewed said that their providers had offered them any alternatives to opioids to keep their pain under control, as recommended by the CDC guidelines, or at least not ones that they had not already tried and which had failed. Patients said that even when they told their providers they were struggling with involuntary tapering, their providers were unable to offer them additional help, whether that be via other treatment options or referral to a mental health provider who might help them manage the tapering process. Some health providers said that they had turned to buprenorphine, an opioid medication that is often used to treat substance use disorders but is considered less risky. Physicians said that the biggest barrier in offering patients non-pharmacological treatments, in particular mental health treatment, was insurance coverage.
Chris Skeens, a 59-year-old in Olympia, Washington, discovered she had a rare disease called syringomyelia — in which cysts form within the spinal cord fluid — in 1997. She had an operation soon after her diagnosis, but she has lived with chronic pain for the last 20 years. After a few years of treatment her pain specialist put her on a dose of about 220 MME. That prescription was then transferred to and managed by her primary care doctor. But in January 2018, that doctor said he would no longer continue to prescribe her opioids. Skeens could only find another doctor willing to prescribe her a lower dose of 135 MME. While Skeens has always used other treatments to manage her pain, she is frustrated that so many other options aren’t covered by insurance.
I’m on Medicare, which barely covers anything. They cover only $3,000 of physical therapy per year – no homeopathic remedies, no massage, no acupuncture.[136]
Doctors and patients alike also identified the limited amount of time doctors have with patients as a challenge. This was especially, although not exclusively, true in primary care, where physicians are often limited to 15 minutes sessions and have little time to get to know a patient or design a treatment plan. The physical medicine doctor in Spokane, Washington said:
There definitely was overprescribing. Opioids were the easiest way to end a bad date — you have 15 minutes with the patient, you have an awkward appointment, and you’re worried about your ratings…. But if you have patients on Medicaid, which most of mine are, they get minimal reimbursement (for other treatments). Medical marijuana isn’t paid for, cognitive behavioral therapy, acupuncture, guided meditation, physical therapy — hardly anybody pays for it.[137]
Human Rights Watch conducted literature searches and reviewed policy documents of both private and public insurers to determine the extent to which insurers cover non-pharmacological pain interventions. However, data from insurance plans are hard to access: private insurers do not typically publish information about their plans to the public. Even government agencies in charge of regulating insurance plans state that the sheer number of plans available — there are some 5 million different employer-sponsored health plans in the United States — makes it difficult to analyze how many Americans have access to specific kinds of treatment or medication.[138] Human Rights Watch reached out to three insurance providers to learn more about the impact of cutbacks in prescribing to chronic pain patients, and coverage of non-opioid treatments for chronic pain. We did not hear back from any of those companies.
Some barriers to care resulting from lack of insurance coverage have been examined in surveys and in academic literature. One survey by the Department of Health and Human Services found that between 2002 and 2012, only 25 percent of patients who saw a practitioner for acupuncture, and 15 percent of those who saw a practitioner for massage therapy, had coverage for those treatments. Of those, more than 50 percent were likely to have partial rather than full coverage.[139] One study of New Hampshire healthcare providers found that acupuncturists, chiropractors, and naturopathic medicine providers were 60 to 70 percent less likely to receive insurance reimbursement than were primary care doctors.[140] Another study found that adults in the US spend $8.7 billion out-of-pocket on complementary treatments like acupuncture, chiropractic services, and herbal medicines to manage back pain — which accounts for almost one third of the total health care expenditure on back pain ($30.4 billion).[141] The IOM report cited earlier mentioned payment structures as one of the biggest barriers to multidisciplinary care, and thus to adequately treating chronic pain in general.[142]
Even acknowledging that not all non-conventional treatments will necessarily be effective, this lack of parity of reimbursement for pharmacological versus non-conventional treatments has been cited in government analyses as a key barrier to treating chronic pain and combatting the opioid epidemic. In its 2017 report, the President’s Commission on Combating Drug Addiction and the Opioid Crisis stated that while “behavioral programs, acupuncture, chiropractic, surgery, as well as FDA-approved multimodal pain strategies have been proven to reduce the use of opioids while providing effective pain management, current CMS reimbursement policies… create barriers to the adoption of these strategies.”[143] The commission specifically cites CMS payment policies for postoperative pain management, which create an all-inclusive bundled payment to hospitals for “surgical supplies” (including opioids): any opioid medications are included in that bundle, whereas nonopioid or non-pharmacological procedures essentially get deducted from that payment, creating a disincentive for hospitals to use alternative treatments.[144]
Doctors said that reimbursement policies played a large role in defining how they were able to treat chronic pain patients. They said they tended, where possible, to avoid patients with long-term intractable pain who received prescriptions for opioids, because they were often difficult to treat in a cost-effective way. One pain specialist from Utah described how his clinic decided to take on new patients:
Physicians know that high-dose opioid patients are patients who have had all kinds of problems and nothing has ever worked. They can really put a burden on the system … no doctor wants to touch them or take them, and that’s why they have no home… I want primary doctors in my area to send me the good patients. That’s a terrible thing to say, but some patients are more profitable in terms of procedures they might need, they’re really easy to get in and out the door — they need a quick injection and that makes good money.[145]
Obtaining coverage for mental health care was particularly problematic for chronic pain patients. In 2008 Mental Health Parity and Addiction Equity Act, which was later incorporated into the 2010 Affordable Care Act, focused on deterring insurance companies from imposing less favorable benefits for mental health and substance use disorders as compared to surgical and medical benefits.[146] However, providers interviewed by Human Rights Watch said that mental health services were often inaccessible to chronic pain patients.
Various government agencies have noted the failure to create genuine parity for mental health treatment. According to the report of the above-mentioned presidential commission, equal coverage for mental health services is still far from a reality in the US: the Mental Health Parity and Addiction Equity Act “has been the impetus for much progress toward parity for behavioral health coverage; plans and employers have, by and large, done away with policies that are clear violations… such as dollar-limits, visit limits, and outright prohibitions on certain treatment modalities.” But the report notes that enforcement has been inconsistent when it comes to “violations that are murkier and harder for regulators to discern,” including stringent medical necessity reviews, limited provider networks, and onerous prior authorization requirements.[147] The Department of Labor, which is charged with enforcing the Mental Health Parity Act with regard to private, employer-based plans, has echoed these concerns. According to the department, it is limited in its enforcement capacity: it has only 400 investigators and 100 benefit advisors to oversee 5 million health, pension, and other employee benefit plans covering some 143 million workers.[148] The Department also cannot “assess civil monetary penalties in egregious cases of noncompliance to deter bad actors,” making it more difficult to effectively enforce parity for mental health and substance use treatment in many instances.[149]
Studies show that payment structures by insurance companies incentivize mental health practitioners to adopt billing practices that often create more burdens for consumers. One study found that mental health providers, from psychiatrists to psychologists to social workers, were reimbursed 43 to 70 percent more if they billed clients out of network rather than in network. These payment pressures incentivize mental health providers to bill their clients out of network: from 2005 to 2015, the percentage of psychiatrists accepting private insurance declined from 72 percent to 55 percent, significantly below the rate for other specialists (89 percent).[150] A 2017 survey found that insurers paid more than 21 percent more for primary care services than for behavioral health services, and behavioral health services were almost six times more likely to be offered as an out-of-network service than medical or surgical care.[151]
While the insurance industry is minimally transparent about what alternative treatments or mental health services are accessible to patients, insurance companies have made highly publicized efforts to reduce opioid prescribing in recent years. Blue Cross Blue Shield hailed a 29 percent reduction in prescriptions from 2013 to 2017 as “progress towards preventing inappropriate prescription opioid use.”[152] United Healthcare touted a 17 percent decrease in the number of long-term opioid prescriptions in 2016 as a way that the company was “confronting the opioid epidemic,”[153] and other providers such as Aetna[154] and Cigna publicized similar reductions in opioid prescriptions.[155] Blue Cross Blue Shield Tennessee did not respond to questions from Human Rights Watch about how their policies impacted pain patients.
While efforts to reduce overprescribing are important — particularly for the insurance industry, which garnered a great deal of criticism for failing to identify gross overprescribing earlier[156] — they do not appear to be accompanied by greater efforts to measure how reductions in opioid prescribing impact chronic pain patients, or to what extent non-opioid alternatives are accessible to them. This trend is reinforced by the organizations that set the standards for insurance plans. The National Committee for Quality Assurance (NCQA) publishes a performance evaluation tool used by more than 90 percent of the country’s health plans. In 2018, NCQA added new metrics to this tool, urging health care plans to measure the rate of high-dose opioid prescribing among their users as a means of reducing the overdose risks. But NCQA has not released any recommendations to insurance companies encouraging them to also measure the impact of reductions in prescribing on chronic pain patients, or to what extent non-opioid treatments are accessible to them. Insurance companies, similarly, have not publicly made any efforts to measure harms to patients or accessibility to alternative treatments.
|
The Impact of Barriers to Care on Palliative Care and Sickle Cell Patients In medical practice, people undergoing cancer treatment or receiving palliative care or end-of-life care are typically exempt from the cautious opioid prescribing that is recommended for chronic pain patients. For example, the CDC Guideline explicitly states that these patients should not be subject to its recommendations on opioid prescribing, and encourages physicians to use alternative guidelines for sickle cell patients, who also suffer intense pain. The CDC says that medical treatment of the above conditions typically has “unique therapeutic goals, ethical considerations, opportunities for medical supervision, and balance of risks and benefits with opioid therapy.”[157] The World Health Organization considers opioid analgesics an essential medication for the treatment of cancer pain and in palliative care.[158] However, several surveys suggest that logistical barriers and the overall climate around opioid prescribing in the US is affecting palliative care patients. Preliminary data from one study found that a majority of oncology patients felt stigmatized because they used opioids, and faced difficulties in obtaining the necessary medications at the pharmacy.[159] A 2018 survey by the American Cancer Society Cancer Action Network and the Patient Quality of Life Coalition found that 30 percent of cancer patients and survivors were unable to access pain medication because their insurance would not cover it, up from 19 percent in 2016. Twenty-seven percent had been unable to fill a prescription at a pharmacy because the pharmacist would not fill the prescription for unstated reasons, even if it was in stock — up from 12 percent two years before.[160] Dr. Sandy Tun, an assistant professor in palliative medicine at the University of Chicago, said that while she welcomed tighter restrictions on opioid prescribing, they placed an undue burden on her medical practice and her palliative care patients: Every single time I write a prescription for fentanyl, I or my staff actually have to call the insurance [company] to justify every single prescription, every month…. I am frustrated on behalf of my patients and their families. I just had a young man in his 40s who had metastatic gastric cancer and he actually had to come in every two weeks for a prescription because his insurance company wouldn’t cover him for a full month. I feel awful having to insist to this patient who is barely able to get through the day, who wants to spend the time he has left with his [nine-year-old] son, that he come in every two weeks and tick these boxes.”[161] According to Dr. Joseph Rotella, Chief Medical Officer of the American Academy of Hospice and Palliative Medicine, his group’s membership — over 5,000 physicians, nurses, and other health professionals — faced greater difficulties in obtaining appropriate pain management for patients in recent years. [The doctors] are writing prescriptions and then the patient goes to the pharmacy and they can’t fill it. They can’t fill it because the pharmacy didn’t stock enough, or the pharmacy exceeded their quota of that medication, or they run it through the patient’s insurance and the first thing they see is that the insurance requires a prior authorization. The patient walks away with no medicine and the doctor gets a call. [162] Karina Wilkerson, a nurse practitioner at Vanderbilt University’s Hematology Department who specializes in caring for patients with sickle cell diseases, said that while her office had pushed to make patients less dependent on opioid analgesics for their pain, many patients still need opioid medications to function when pain flares up. Sickle cell disease is a group of rare inherited disorders, primarily marked by abnormal formation of red blood cells, that typically cause intense acute pain “crises,” as well as chronic pain in many older patients. Despite exemptions for such patients in the CDC Guideline and Tennessee state law, Wilkerson’s office had seen a major push from state regulators and insurers to get patients down to lower doses: The state is basically encouraging everybody to get them down to 90 MME… Some patients really do better when we wean them, but that’s not everybody… A big problem is insurers, who want us to try medications we know won’t work or see patients every week in some cases. TennCare (Tennessee’s state Medicaid program) has a limit of five prescriptions per month. Private insurers are trying to dictate what we can give them; we have even had to send them articles about what works. One patient was doing really well, an architect; he takes his medication at home but we had such a hard time because for six months, the insurance company didn’t want to approve his medication. Eventually we had to write down how much it would cost to send him to the ER twice a month instead, and they saw that it would be more expensive than medication, so they gave in.[163] |
Exploring the Causes of Involuntary Tapering
Many of the physicians and other clinicians Human Rights Watch interviewed described an environment in which they felt extreme pressure to drastically cut down prescribing of opioid analgesics to chronic pain patients, including in cases where they felt that it was clinically inappropriate. They described a broad variety of push and pull factors that include fears of scrutiny from law enforcement agencies, such as the DEA; uncertainty about what constitutes appropriate prescribing; scrutiny by state medical boards; state legislation and regulations that imposed restrictions on clinical decisions; complex insurance procedures and pushback from individual pharmacists or pharmacy chains also wary of liability.
In this environment, our investigation suggests, the CDC Guideline has often not been used to bring about carefully calibrated corrections to prescribing practices, but rather to push for drastic cuts in the rate of use of these medicines, often without accounting for the cost to chronic pain patients. Our interviews with physicians and nurse practitioners found that the CDC’s guidance around dosages was often not treated as a recommendation but as a mandate. As noted above, many were involuntarily tapering or had already involuntarily tapered all patients to doses at or below the 90 MME threshold described in the Guideline, while others said they did not taper existing patients but no longer accepted new chronic pain patients into their practice if they were on opioid medication at doses above 90 MME. Providers expressed fears that prescribing over 90 MME could attract the scrutiny of enforcement agencies such as the DEA and state medical boards; that any prescribing over 90 MME would not be reimbursed by insurance providers, even if clinically appropriate; and in some cases, that such prescribing would be in conflict with state-level regulations.
|
The Story of Barbara Gray
Barbara Gray, a 25-year-old from Knoxville, Tennessee, went to the hospital for a routine operation for high arches in her feet in February 2017. She was told she would receive an injection meant to numb the nerves down to her foot, when suddenly she felt a sharp, searing pain in her leg: “I screamed so much that I was embarrassed when it happened. But they rolled me back over and didn’t mark anything down in my medical records.”[164] Tests would later show that the injection damaged two key nerves running down her calf to her foot. Within a few weeks, Barbara had excruciating pain from the knee down, and discoloration in her foot and leg. The diagnosis: chronic regional pain syndrome (CRPS), an extremely painful disorder that sometimes results from direct nerve damage. It causes severe pain in the affected limb and can lead to swelling and changes in skin temperature and color.[165] Barbara said the pain feels “like an ice pick is being driven under [her] toenail.” She struggled to balance her graduate studies with her job as a speech therapist in a local school, because she couldn’t make it through a full conversation without suddenly being blindsided by pain. Barbara found a pain clinic and was prescribed a low dose of hydrocodone: 30 MME to start, which was later increased to 40 MME. She took the medication as needed when her pain flared up, but also spent hours researching and trying alternatives, from massage therapy to acupuncture to reiki and even ketamine, a medication more commonly used for starting and maintaining anesthesia. But early into her treatment, Barbara’s doctor said he could not maintain her on opioids indefinitely, and insisted that she try a spinal cord stimulator, a device that is implanted into the body and sends electric pulses to parts of the spine. After the trauma of her first surgery, Barbara was terrified of another invasive procedure, and had discovered through research that there were risks the CRPS could spread to other parts of her body. But she didn’t see how she could say no: “They were so adamant that it was the spinal cord stimulator or nothing that in December, I agreed to do a trial.” It didn’t go well. She explained: I want to avoid any invasive procedures if possible…. Having the spinal cord stimulator pushed on me was gut-wrenching. The trial was horrific — I could feel the doctor threading the wires up my spine. It wasn’t so much painful as it was mentally disturbing. My face was just smeared with black mascara. I cried throughout the whole thing. Barbara’s physician, Dr. Joe Browder,[166] said he felt compelled to comply with the Tennessee Chronic Pain Guidelines that were published in 2017 following the CDC Guideline. Although the Tennessee guidelines say that “reasonable non-opioid treatments should [emphasis added] be tried before opioids are initiated,”[167] Dr. Browder explained that he believed he risked potential liability if he prescribed opioids without exploring viable nonopioid options first, even if those entailed potential risks to patients: This is the most vexing kind of decision I have to make. The guidelines say all therapies have to be tried and failed before opioids. Some modalities are quite invasive, like spinal fusions or spinal cord stimulation — if you have that modality available, it needs to be used. And that is a dilemma with someone on moderate doses of opioids who is doing very well, because then you have to insist that they undergo this invasive procedure that has significant downsides to it…. I see elderly patients quite frequently and they’re doing well on moderate amounts of opioids, but they have herniated discs and surgery might help but that’s a difficult question. When writing prescriptions for opioids is being so strongly discouraged in Tennessee, he said,
It makes you pause before you fail to follow the guidelines explicitly…. If I write [a prescription for] the opioids and something untoward happens, then it’s my problem. Whereas if they go to surgery and have a complication [it’s not]. And it’s really against everything I was trained to do, but it’s the will of the legislators and regulators.[168] |
Fear of Scrutiny: Patients as Liabilities
Several of the healthcare providers we interviewed said that they increasingly see chronic pain patients as a potential source of liability. As in the case of Dr. Browder, they said that they felt they had to adapt their pain management strategy to avoid such liability, even if that departed from what they felt was clinically most appropriate and could cause harm to their patients.
It is impossible to know how justified fears of scrutiny or liability are. The number of prosecutions of individual doctors is small, which may suggest that doctors have more ability to apply their personal judgement to individual patients (in line with the CDC Guideline) than they think. Nonetheless, the relevant concerns of healthcare workers are real and changes they make in their clinical practices can, and clearly sometimes do, harm patients.
Some providers said their prescribing practices changed when doctors they knew became the targets of DEA or medical board intervention. Aileen Wedvik, a registered nurse practitioner and pain specialist in Lakeland, Washington who cares for more than 400 chronic pain patients, was one of the healthcare providers who told Human Rights Watch she was no longer willing to treat patients on high doses due to concerns about liability. She had made the decision after hearing about a DEA raid on a well-known pain doctor who had authored numerous articles on pain management and was also a vocal advocate for patients on high doses.
Regardless of whether that law enforcement action was justified, the arrest stunned Wedvik and helped convince her that the practice of prescribing opioids was simply too risky. In January 2018, she sent a letter to each of her patients telling them she was leaving pain management — which in Washington State requires additional training and registration — to be a primary care practitioner. She decided to bring all her patients on high doses down to the 90 MME threshold described by the Guideline.
When I read that he had been arrested, that was a real game changer for me. He walks on water. I’ve heard him speak at conferences and read his research. But I realized that if they could do that to him, they could do that to anybody. So I made the announcement that I was leaving pain management and bringing everybody down to 90 MMEs. In this climate I just don’t want my name associated with pain… I’ve told my patients: I’m no good to you behind bars.[169]
Several physicians said that it was the fear of being punished by state medical boards or other local authorities, rather than a full-blown criminal investigation, that proved the most effective in pushing them to adhere to lower doses or avoid opioid medications altogether. One family physician in Olympia, Washington spoke about how seeing a colleague’s name mentioned in the state’s Medical Quality Assurance Commission (MQAC) — a quarterly state medical board newsletter — had influenced her prescribing.[170]
It promotes an absolute culture of fear, I’ve seen very good doctors’ names published, and that’s your good reputation gone. If I’m prescribing high amounts [of opioids], I have no protection under the law because everything is [guidelines], nobody knows what is what.
I have a patient who came to me on 500 MME and I’ve gotten her down to 120, but that took me five years — not ten percent every two weeks, which is probably what a lawyer would have told me I should do… I turn away new patients if they are on a high dose. These are folks whose records checked out, they are good citizens. I just felt like if I started to open the floodgates that my exposure and my risk would be too high. I can’t afford to burn down my life and lose my license.[171]
Like federal law enforcement agencies, most state medical boards do not have clearly stipulated rules on prescribing of opioids, and state medical boards do not actively monitor physicians but are “complaint-driven,” meaning they investigate a physician when they are alerted to potential issues by a patient, insurance company, fellow medical provider, or law enforcement.[172] Thus, physicians said they relied on recommendations made by the CDC, Department of Veterans Affairs, or related state guidelines to make decisions about patients, even if they felt they were clinically not appropriate. Some physicians said that they still felt comfortable prescribing for patients with more severe neurological conditions, but that in the event of a criminal or administrative investigation, they would be unable to defend decisions about patients with diagnoses that did not universally result in pain. This is problematic, given that chronic pain is highly individualized — people with similar injuries or conditions may react experience very different levels of pain.
Dr. Joe Browder of Knoxville, Tennessee, said that in 2017, he decided he would “do everything to get all my patients below 120 MME so that I wouldn’t be a major outlier in the state.” While many of his patients had managed the dose reduction well, some suffered from increased pain and a lower quality of life as a result. Dr. Browder had kept a small contingent of his patients at doses above 120 MME. But with other patients, he believed they were in pain but feared prescribing to them because of current regulations and attitudes about opioids:
I have five to six percent of patients who are above 120 [MME]... If I was being as kind as I want to be I would probably have twice that many, but I don’t think it’s appropriate in this climate. I saw that [the patient’s] life was better, and it got worse when I brought them down, but I don’t have a diagnosis that an average reasonable doctor would think requires very high doses of opioids.
Even doctors who insisted on providing the care they felt appropriate for their patients said that they believe they put their licenses at risk when they prescribed opioids at a high dose. Dr. Lucinda Grande, a family practitioner in Lacey, Washington, told Human Rights Watch that she strongly believes in the need to try to avoid using opioid analgesics in chronic pain patients and to rely on alternatives, such as buprenorphine (which is primary used to treat opioid addiction). But she said a small handful of her patients still needed the medications. She gave the example of one patient with “a really nondescript pain syndrome, cervical radiculopathy [a compressed nerve in his neck]” who was on 600 MME of opioids. When she tried to wean him down, his quality of life began to rapidly deteriorate. After consulting with a pain specialist, she said:
I gulped and put him back to 600 [MME], and he immediately went back to his previous stable level of functioning, smiling and comfortable. It was a hard decision because I’m putting my license on the line every time I do something unconventional like that…. There is no formula to solving [the opioid crisis], we’re being shepherded into a formulaic solution, which doesn’t work well for people with chronic pain. Each person is individual, and they have their own story, their own response to opioids.[173]
One Colorado pain specialist who works in a hospital said she had always been a low prescriber and welcomed the Guideline as a way of explaining the risks of high-dose opioids to patients. But she said that she had tapered many patients to below the 90 MME threshold described in the CDC Guideline out of fear she could be held liable for prescribing higher doses, particularly after her hospital told her it would not protect her from malpractice suits if she prescribed opioids. She summarized her fears about prescribing: “They’ve done a good job at scaring the shit out of docs,” she said.[174]
Controlled Substances Legislation and the DEA
While providers cited perceived legal liability, the number of doctors who were officially sanctioned by the DEA is growing, but quite low: the DEA listed 48 such incidents from 2017, up from 37 in 2015 and 21 in 2014.[175] These cases typically reflect the most flagrant examples of inappropriate prescribing.[176] In a response to questions from Human Rights Watch, the DEA said that it was not up to federal agencies to “set forth the standards of medical practice”:
It is up to each DEA-registered practitioner to treat a patient according to his or her professional medical judgment in accordance with a standard of medical practice that is generally recognized and accepted in the United States. Therefore, as long as practitioners are issuing a prescription for a controlled substance for a legitimate medical purpose and they are acting in the usual course of professional practice, they are acting within the law.[177]
But it is precisely this ambiguity that prescribers point to as a source of fear and panic, that is driving them to engage in harmful behavior. Physicians said they struggled to interpret what the DEA and other enforcement bodies meant by the “standard of medical practice,” and thus relied on the CDC Guideline as a red line for prescribing, even though it was not intended as such. That was true even of pain specialists, who technically are not subject to recommendations in the CDC Guideline.
“It’s not always a formal rule that leads to highly destructive behavior by individual physicians and health care systems, but rather a collection of prods and incentives,” said Stefan Kertesz, Professor of Medicine at the University of Alabama at Birmingham.[178] This includes “a potential legal enforcement threat that is always ambiguous… In the face of a liability like that, it becomes very easy for individual clinicians to mistreat their patients. Physicians have no explicit safe harbor that they are protected in treating a patient who needs to remain on a high dose.”
Media reports of DEA raids on medical practices for alleged inappropriate prescribing of opioids, in addition to prescribers’ fears that state medical boards were increasingly scrutinizing doctors for opioid prescribing, reinforced the perception of a real threat of legal penalty. In response to Human Rights Watch inquiries, the DEA declined to state the number of raids it conducted on physician offices and homes per year,[179] while the Federation of State Medical Boards said it did not currently have data on license suspensions or informal reprimands by medical boards.[180]
Laws and Jurisprudence
According to the National Conference of State Legislatures, which monitors state laws, 32 states had passed laws setting out limits or guidelines on opioid prescribing (or authorizing other agencies to do so) as of June 2018.[181] In response to questions from Human Rights Watch, CDC said that as of April 2018, 46 states had implemented activities to improve local prescribing practices “in alignment with aspects of the Guideline.”[182] As far as Human Rights Watch is aware, the impact of these laws and guidelines on prescribing and on opioid overdose rates has not been studied.
The most extreme example is Maine, where a law implemented in 2017 caps prescribing at 100 MME, with exemptions only for treatment of cancer pain, palliative care, hospice care, and substance use treatment.[183] This law has a major impact on prescribers’ practice. Dr. Cathleen London, the primary care physician in Milbridge, Maine, mentioned above, said she was unable to treat patients appropriately given those limitations.
You can’t say that nobody should ever be on something. What are you going to tell somebody with spinal stenosis? Sorry, you have to be in a wheelchair now? I’ve got patients whose hands are totally deformed by rheumatoid arthritis. Should I tell them to expect never to be able to move them again?... Apparently, we’re not allowed to be compassionate.[184]
Other state laws leave more to provider discretion. In 2010, Washington State passed regulations that made it possible for physicians to prescribe more than 120 MME only after consulting with a qualified pain specialist, though it technically allows for providers inheriting patients on higher doses to be exempt from such requirements.[185] New Hampshire has similar regulations for any patients on 100 MME for more than 90 days.[186]
The vast majority of state laws focus on opioid prescribing for acute pain, often imposing a three to seven-day limit on the initial prescription a provider can issue a patient. While meant to address prescribing for acute pain, some of these laws have implications for chronic pain patients as well: for example, a Tennessee law passed in 2018 mandates that patients who have never taken opioids before who have failed other nonopioid treatments be limited to a 30-day prescription of 40 MME per day, unless they meet a series of exemptions.[187] While it is technically possible for physicians to prescribe over this limit, healthcare providers told Human Rights Watch that these laws create a chilling effect: prescribers in Tennessee whom we interviewed said they were reluctant to prescribe over 40 MME to new patients, knowing they could come under scrutiny for doing so.[188]
Administrative Policies and Limits
In an effort to reduce opioid prescribing, state and federal institutions such as Medicaid have encouraged limiting payment to or tapering patients who are on high doses of opioid medications. In early 2018, Centers for Medicare and Medicaid Services attempted to implement a new policy that would have essentially banned payment for long-term doses of opioids upward of 200 MME.[189] This proposal was abandoned after widespread pushback by prominent physicians and negative media coverage.[190]
However, some state Medicaid programs have proceeded with even more restrictive measures. Of 48 opioid-related state Medicaid policies examined by Human Rights Watch, 16 had dose-related quantity limits for opioid prescribing. Some of those allowed for exemptions for chronic pain patients, but six states had policies that mandated tapering and maximum dose limits, practices that are not recommended by the CDC. In the case of Oregon, for example, starting January 2018 Medicaid no longer covers prescriptions over 90 MME except for patients with cancer diagnoses or palliative care, and “no longer cover[s] any opioids for chronic back or spine conditions.”[191] It encourages prescribers to create a tapering plan with their patients. In the first half of 2018, the department of social services in South Dakota[192] and the department of health in Texas[193] announced that the maximum threshold for opioid prescribing paid for by Medicaid would be reduced from 300 MME to 90 MME over the course of a year, with exemptions for cancer patients in Texas and for patients with terminal diagnoses in South Dakota. Both these states cited the CDC guidelines as a rationale for the policy, but they provided for no exception for chronic pain patients and gave no additional instructions or tools about how providers could safely taper patients to prevent negative physical or mental health outcomes. Tennessee and Colorado Medicaid programs implemented maximum dose limits on opioids of 200 MME and 250 MME respectively, and Maine’s state Medicaid program has a 100 MME maximum dose in line with its law on opioid prescribing.
At the time of writing, Human Rights Watch had not received a response to questions about these policies from the Oregon Health Authority or Molina Insurance, a Texas Medicaid provider.
Department of Veterans Affairs
The Department of Veterans Affairs is another government institution that has aggressively pursued reductions in opioid prescribing and adopted inflexible restrictions on high dose prescribing. The VA was widely criticized in the media when it was revealed that opiate prescriptions had surged by 270 percent from 2000 to 2012.[194] The VA announced an Opioid Safety initiative in 2012, meant to provide clinicians with more resources on how to treat chronic pain by using nonopioid therapies. The VA announced that it had successfully reduced opioid prescriptions by 41 percent between 2012 and 2017.[195] In 2017, the VA published new guidelines for practitioners.
The VA guidelines claim they are not defining a specific standard of care for VA facilities, but they strongly recommend against the use of long-term opioids for chronic pain and strongly recommend against doses over 90 morphine milligram equivalents. The VA guidelines overall have a strong emphasis on tapering: unlike the CDC Guideline, which encourages tapers primarily when they are initiated by the patient, the VA encourages tapering whenever the clinician believes risks outweigh benefits. It also states that providers should not refrain from tapering if a patient threatens suicide: “continuing LOT (long-term opioids) to ‘prevent suicide’ in someone with chronic pain is not recommended.”[196] While the VA stated that “the CDC guideline did not form the basis of the deliberations on the strength or the direction of these recommendations,” it said it was aware of the CDC guidelines and had come to many similar conclusions.[197]
Stories in the media suggest that in some cases, rapid and unsupported tapers at VA facilities have resulted in suicide and overdose.[198]
CDC’s Thinking on Using the Guideline
It is unclear to what extent the CDC Guideline itself has encouraged reductions in prescribing. Reductions in high-dose prescriptions have accelerated since implementation of the Guideline: the number of high-dose prescriptions decreased by 3.56 percent per month between January 2012 and March 2016, and by 8 percent per month after March 2016, when the Guideline was passed.[199] It is also unclear what influence the Guideline has had on overdose deaths: while overdose deaths have been declining for the first six months of 2018, many public health experts attribute this to a combination of factors that may include reduced prescribing, but also include greater treatment availability, particularly in states that prioritized access to medication-assisted treatment and to Naloxone, an overdose-reversing drug.[200]
Despite these unknowns, the CDC Guideline serves the legitimate aim of encouraging an approach to patient care that balances the risks of opioids with the individual needs of chronic pain patients. It seeks to help a physician screen for risks and gives vital guidance on how to begin and terminate opioid therapy.
However, when providers reduce patient dose without patient consent, or when insurance policies and state laws set maximum dose threshold that provide no exceptions or mandate involuntary tapering, they are misinterpreting the CDC Guideline. The Guideline sought to assist primary care providers in offering safe and effective treatment for patients with chronic pain, to improve communication between providers and patients, and to decrease adverse outcomes associated with long-term opioid therapy.
The Guideline does caution against the prescribing of high doses of opioids, but it explicitly allows for healthcare provider discretion to make clinical decisions that they feel are appropriate for an individual patient. It recognizes that some patients may warrant treatment with opioids, even at high doses. The Guideline itself encourages providers to work with patients on tapering, but does not explicitly state that involuntary tapers are unsafe. In a response to Human Rights Watch about how the Guideline has been used by physicians or mandated by insurance policies and some state laws, the CDC more explicitly stated its position on involuntary tapering of patients:
CDC does not recommend that physicians taper opioids for chronic pain without patient consent…. The Guideline does not support involuntary tapering. Obtaining patient buy-in before tapering is critical to successful dose reduction.
[The Guideline] is not intended to take away physician discretion and decision-making. The Guideline is designed to help physicians assess how to safely maintain or discontinue opioid use in patients who are currently on an opioid treatment plan or start opioids safely if necessary. CDC encourages physicians to continue to use their clinical judgment and base their treatment on what they know about their patients, including the use of opioids if they are determined to be the best course of treatment.[201]
Poor Data: An Impediment to an Effective Response to the Overdose Crisis
The dominant narrative today is that prescription opioids are still driving overdose death rates, and public officials frequently make wild — and entirely unfounded — claims in this regard. President Donald Trump has claimed that people walk into a hospital and come out addicted a day later.[202] Attorney General Jeff Sessions has stated that 80 percent of heroin addiction starts with prescription drugs.[203] One public advertisement campaign by the Philadelphia Department of Health described prescription pills as “heroin in pill form.”[204]
Statements like these have a negative impact on chronic pain patients who rely on these medications: patients told us that they feel stigmatized by friends, family, and colleagues; they avoid speaking about their conditions and their treatment publicly for fear of being stigmatized as drug seekers; and they encounter embarrassment at the pharmacy, where they are often questioned about their need for these medications in front of others.
This is particularly problematic given that the extent to which opioid prescriptions for chronic pain contributed to the overdose epidemic is in dispute. At present, the data available about this have numerous flaws and limitations that make it difficult for policymakers, public officials, and the media to fully understand how much of the overdose crisis is linked to prescribing to chronic pain patients. In order to avoid further stigmatizing and harming chronic pain patients, the federal government should work to collect and publish more comprehensive data on the overdose crisis.
For example, while current government statements and the media often assert that long-term, high-dose prescription opioids have been the primary driver of overdose deaths, it is not clear that that is the case: while overdose deaths reached a record 72,000 in 2017, opioid prescribing began to plateau in the mid-2000s and has declined significantly each year after 2012. In particular, high dose prescribing, defined by the CDC as prescriptions for more than 90 morphine equivalents per day, has dropped 48.6 percent from 2006 to 2016.[205] The graphs below show reductions both in the dosage per prescription and in numbers of high dose prescriptions between 2006 and 2016. Data from earlier years are not publicly available and CDC did not respond to requests from Human Rights Watch for data from previous years. As noted in the background section above, overdose deaths have continued to rise, largely due to increase in deaths due to fentanyl and heroin, despite declines in high-dose prescribing and in opioid prescribing more generally.
To truly understand the role of prescription opioids in the overdose crisis, it is critical to know at least the following about each individual overdose death (or averted death):
- What substances were involved? Many overdose deaths are attributed to opioid analgesics even though multiple other substances are involved, and it can be difficult to determine which one actually caused a person’s death. In New Hampshire, for example, of the 32 overdose deaths involving an oxycodone prescription, 72 percent of those deaths included alcohol, benzodiazepine, or other drugs.[206] In a study of one county, the average number of drugs involved in an overdose death was six.[207] This phenomenon is called “polypharmacy,” and the extent to which it is prevalent in the current overdose crisis is detailed in the graph below. However, data on polypharmacy is not consistently collected or adequately analyzed. Indeed, data collection standards are widely inconsistent across states. As recently as January 2017, some states had huge numbers of overdose deaths in which no drug was specified at all: Louisiana specified the drug in only 53 percent of cases, Pennsylvania 54 percent, Montana and Alabama 58 percent.[208]
- If an opioid was involved, was it a prescription opioid or a street drug? Many data sets on overdose deaths do not differentiate between prescription opioids and street opioids, making it impossible to analyze the extent to which either one contributes to the overdose crisis. Moreover, some opioids, such as fentanyl, exist both as pharmaceutical products and as illegal substances. It can be hard to tell whether the substance found in someone’s body was legally or illegally produced. This ambiguity can lead to significant errors. For example, in 2018, four CDC officials published an article stating that because a large number of fentanyl deaths were incorrectly attributed to pharmaceutical opioids, the official estimate of deaths due to prescription painkillers might be inflated by as much as 15,000.[209]
- If a prescription opioid was involved, was it prescribed to the individual experiencing the overdose or not? Prescription opioids are frequently diverted from legal channels to the black market or stolen from friends or relatives. Yet there is significant confusion in much of the available data around this question.
- If a street drug was involved, did the individual experiencing the overdose have a prescription for an opioid in the past? In 2016, Massachusetts cross-referenced overdose death data with an individuals’ history in the state’s prescription drug monitoring database, finding that a small minority of people who died from an overdose had a prescription at the time of their death but a much larger portion had a prescription for opioids at some point between 2011 and 2014.[210] Cross-referencing databases in this manner more often would give federal agencies a better understanding of the interaction between prescribing and overdose deaths: whether the person who has died of an overdose death received a prescription at some point (rather than using diverted pain pills on the illicit market), whether that prescription was for chronic pain or acute pain, a high dose or a low dose, long-term or short-term, whether the physician prescribing had screened for addiction risks. Without cross-referencing such databases, it is difficult to understand the dynamic between prescription drugs and overdose deaths: we can only surmise a correlation, rather than a useful causation that would facilitate a more effective policy response. This kind of data analysis could be conducted in most states, as all states but one now have a prescription drug monitoring program. So far few have done so although some other states are now conducting similar studies.[211]
- If a prescribed opioid was involved, was it prescribed for acute pain, chronic pain, cancer pain or for palliative care? Prescription opioids are used for a variety of medical conditions: acute pain, chronic pain, post-operative pain, cancer pain, and at the end of life. We know that a large percentage of the overall volume is prescribed to chronic pain patients.[212] But few studies have examined the risks of developing a substance use disorder associated with prescribing for these different kinds of pain, even though this is obviously critical to mounting an effective response to the overdose crisis. This kind of analysis should be possible: for example, the 2016 report from Massachusetts could have included analysis of the types of prescriptions patients had received in the years leading up to their deaths.
If government officials do not understand to what extent prescription opioids are driving overdose deaths, its policies may not be effective in addressing the crisis. The federal and state governments should identify, based on the above, what gaps exist in data collection, what new data should be collected, and what analyses should be carried out using existing data to better understand how prescription opioids contribute to the overdose crisis. In doing so, the government will also avoid unnecessarily stigmatizing chronic pain patients, who say they are often seen as “drug seekers” and who feel they have been blamed for the overdose crisis.
The Human Rights Analysis
The Right to Health
Heath is a fundamental human right enshrined in numerous international human rights documents. The International Covenant on Economic, Social and Cultural Rights (ICESCR), which the United States has signed but not ratified, specifies that everyone has a right “to the enjoyment of the highest attainable standard of physical and mental health.” Because it is not a state party, the US is not bound by the ICESCR, but the convention remains a useful and authoritative guide to the steps all governments should take to protect and realize the right to health. Its implementation is subject to progressive realization, with countries obliged to implement it according to the “maximum available resources.”[213] The Committee that oversees the ICESR has stated that there are nonetheless several “minimum core obligations” that all countries must uphold regardless of their economic situation, including non-discriminatory access to health facilities and services; access to food, shelter, sanitation, water, and to essential medicines (as defined by the World Health Organization); and an equitable public health strategy.[214]
Under the ICESCR framework, the right to health has been explicitly extended to palliative and end of life pain management: discussing the rights of older people, the Committee has stated that states provide “attention and care for chronically and terminally ill persons, sparing them avoidable pain and enabling them to die with dignity.”[215] The UN Special Rapporteurs on Health and Torture have also argued that “the failure to ensure access to controlled medicines for the relief of pain and suffering threatens fundamental rights to health and to protection against cruel inhuman and degrading treatment.”[216] The Special Rapporteur has specified that, in his expert opinion, “the de facto denial of access to pain relief, if it causes severe pain and suffering, constitutes cruel, inhuman or degrading treatment or punishment.[217]
The Right to Health and Chronic Non-Cancer Pain Management
While a significant body of literature explores the right of palliative care patients to access pain management and government obligations flowing from that right have been described in detail, the same is not the case for chronic non-cancer pain. In fact, several factors make it more complicated to determine precise government obligations with respect to pain management for such patients. First, the World Health Organization has not issued detailed clinical guidelines for chronic non-cancer pain management in adults, unlike with cancer pain management, meaning that there is no internationally agreed standard of care. Moreover, chronic pain is in fact a cluster of different conditions with widely varying diagnoses that require different treatment approaches, and there remains much uncertainty and debate about the most effective treatments. While opioid analgesics are the cornerstone of cancer pain management, these medications do not play a central role in chronic pain management and are, indeed, controversial. The available evidence suggests that effective treatment of chronic pain requires a multidisciplinary approach, using pharmacological and nonpharmacological tools that are not included in the WHO’s essential medicines list.
Nonetheless, the right to health clearly applies to chronic non-cancer pain patients, as does the prohibition of torture, cruel or degrading treatment or punishment, and some of the same broad principles that apply to pain management for palliative care patients apply to chronic non-cancer pain patients. Under the ICESCR’s right to health framework, state parties have an obligation to “respect, protect, and fulfil” the right of chronic non-cancer pain patients to appropriate pain management and to ensure that health services are available and accessible, and that there is “equal and timely access to basic preventive, curative, rehabilitative health services and health education.” As pertains to chronic pain, this includes an obligation to:
- Develop and implement a strategy that responds to this health need. The Committee on Economic and Social Rights has held that governments must adopt and implement a national public health strategy addressing the health concerns of the “whole population.”
- Ensure availability and accessibility to all patients who need medications that are included on the WHO’s essential medicines list, including NSAIDS, muscle relaxants, antidepressants and opioid analgesics — all of which can be effective in treating chronic noncancer pain.
- Ensure that health care providers receive adequate training in the management of chronic non-cancer pain.
- Refrain from arbitrarily interfering with the provision of medical care to chronic non-cancer pain patients, including the non-consensual cessation of pain medicine (involuntary tapering).
While low income countries may face challenges making complex, multidisciplinary treatments widely accessible to chronic pain patients, the United States has the available resources to create and implement a comprehensive strategy to ensure accessibility of services for the management of chronic non-cancer pain and appropriate education for health care providers.
It is important to note that the obligation to ensure access to chronic pain management does not imply a right to opioid medications. It does mean that chronic pain patients who have a medical need for them should be able to access them and that physicians should be able to prescribe them based on their clinical judgment.
National Law
US law mandates that insurance plans provide accessibility for certain key medications and services. The Affordable Care Act mandated coverage for prescription drugs, mental health services, as well as “rehabilitative and habilitative services and devices (services and devices to help people with injuries, disabilities, or chronic conditions gain or recover mental and physical skills).”[218] It is clear many of the modalities that have been proven effective in treating chronic pain would fall into these categories. The government has a mandate to ensure that chronic pain patients receive appropriate prescription drugs and rehabilitative services as part of government-funded Medicare and Medicaid plans, and it also has a mandate to regulate private insurance plans to ensure the same.
A Way Forward
In light of the overdose crisis, questions about the efficacy of opioid analgesics in managing chronic non-cancer pain, and the risks that are associated with their use, the CDC and other government agencies are right to encourage more caution in the use of these medications for chronic non-cancer pain. The CDC Guideline proposes an approach that discourages the use of opioid analgesics as a first resort, encourages the use of alternative treatments, recommends screening of patients for risks prior to prescribing these medicines, and seeks to keep — or bring — dosages down when possible. It also explicitly recognizes that in some cases, opioid analgesics will be needed to keep a patient’s pain under control, and calls for physician discretion to continue prescribing them to such patients.
But this report shows that many individuals with chronic pain are being involuntarily tapered from essential medicines that are vital to their daily functioning, depriving them of their right to health as well as, in many cases, livelihood, education, and full participation in society. Health care providers in some cases are even turning away such individuals, insurance companies and programs are refusing coverage, and state governments are preventing physicians from using their medical judgement to provide appropriate care.
There are many causes underlying these abuses. One visible cause has been the misinterpretation and lack of explicit guidance in the 2016 CDC Guideline on Opioid Prescribing. The Guideline does not endorse a maximum limit on opioid medicines or involuntary tapering, yet officials have pointed at the Guideline to justify these actions and to put in place arbitrary restrictions that have resulted in tangible harms.
Federal and state governments have a duty to counter these trends and ensure that chronic pain patients have access to appropriate health services to alleviate their suffering and improve their ability to function. Our recommendations fall into four broad categories:
- Limiting the unintended consequences of the response to the overdose crisis for chronic pain patients;
- Ensuring continuity of care for patients of shuttered pain clinics;
- Improving availability, accessibility, and affordability of multimodal pain management, including to non-pharmacological modalities; and
- Improving data collection on the overdose crisis.
The federal government has made some efforts to address inadequate medical care for chronic pain patients. In particular, the National Pain Strategy, developed on instructions from the Department of Health and Human Services after a 2011 Institute of Medicine report revealed major gaps in care for chronic pain patients, attempts to rectify some of these issues.[219] This plan has a number of objectives: it seeks to increase scientific knowledge about chronic pain and pain-related conditions; broaden support for treating chronic pain as a biopsychosocial condition that requires interdisciplinary care; find ways to prevent the onset of chronic pain or injuries that lead to it; enhance payment incentives for insurance companies to cover interdisciplinary care; remove other barriers that lead to disparities in care; minimize the stigmatization of chronic pain patients; and to better educate and train medical professionals about chronic pain. The strategy, the first ever by the federal government, is an important step and should be fully implemented. To date, however, implementation has focused primarily on research rather than removing barriers to pain management for current chronic pain patients. Funding for the strategy’s implementation to date has come from existing budgets of participating government agencies, which means that resources have been insufficient and uncertain. As noted above, the strategy does not address the situation of chronic pain patients who already are on opioid analgesics, a significant omission given the findings of this report.
Limit the Unintended Consequences for Chronic Pain Patients
Any response to a public health crisis may result in unintended, harmful consequences. Governments have a responsibility to limit such consequences and to mitigate negative impacts as much as is possible. As this report documents, there have been unintended consequences of efforts to reduce opioid prescribing for chronic pain patients as a result of, among other things, the inappropriate implementation of the CDC Guideline. The CDC, the Department of Health and Human Services, and other federal and state government agencies should play a leading role in countering these negative impacts. In particular, Human Rights Watch recommends that the Department of Health and Human Services and the CDC:
- Revise the 2016 Guideline for Prescribing Opioids for Chronic Pain to explicitly state that patients should not be involuntarily tapered off opioid medication, and that while higher-dose opioids carry increased overdose risk, there is no maximum dose and some patients may warrant high doses.
- Work with other relevant federal and state government agencies, state medical boards, and professional and civil society groups to ensure that clinicians, including those caring for patients on high doses of opioids, can implement the Guideline’s recommendations without having to fear disruptive legal scrutiny, arbitrary limits, or administrative barriers.
- Work together with the Centers for Medicare and Medicaid Services, the Department of Veterans Affairs, individual states, and private insurance providers to identify and address limits or administrative practices that arbitrarily interfere with the ability of chronic pain patients who need opioid analgesics to access them.
- Develop a system of metrics that measures not just crude reductions in opioid prescribing to chronic pain patients, but also the quality of life, potential adverse consequences, and retention in health services of such patients.
- Develop additional guidance to healthcare workers on procedures to safely reduce the dosage of chronic pain patients on opioids.
- Conduct or commission research on the consequences of involuntary tapering among chronic pain patients, including of reports of suicide, and do so in a manner that is open and available for review by the medical community and people whose lives are being affected.
Ensure Continuity of Care for Chronic Pain Patients
When government agencies close down a pain clinic, dozens, hundreds, or even thousands of chronic pain patients may abruptly lose care and have nowhere to go. This can have serious consequences, including self-medication, illicit drug use or suicidal ideation and behavior. In such cases, the government should take steps to ensure patients’ continuity of care:
- State governments and medical stakeholders should make a coordinated effort to ensure that patients are assisted in transferring to another provider or clinic and are not abruptly cut off their medications.
- State Departments of Health should assist patients affected by clinic closures in finding new providers, and should also refer them to mental health services or opioid substitution therapy if needed. The State Department of Health should help patients answer questions and develop educational materials for patients terminated from care.
Expand Availability, Accessibility, and Affordability for All Treatment Options for Chronic Pain Patients
The 2016 CDC Guideline recommends that healthcare workers use, when possible, non-opioid treatments in managing chronic pain. However, clinicians and chronic pain patients repeatedly told us that many of those modalities are unavailable or unaffordable.
- The Department of Health and Human Services, the Centers for Medicare and Medicaid Services, the Department of Labor, and state insurance commissioners should use their regulatory authority to ensure that public and private insurance plans cover a wide range of treatment modalities for chronic pain, including non-pharmacological interventions such as massage therapy, acupuncture, and mental health services.
- Although the evidence base for chronic pain treatments, including non-pharmacological interventions, is growing, the National Institutes of Health, CDC, and other relevant federal and state agencies should fund and encourage more research into the effectiveness of different modalities for different types of pain.
Improve Quality of Data Available for Analysis in Tackling the Opioid Overdose Crisis
In order to effectively address the opioid overdose crisis, federal and state governments need high-quality data that allows for as full an understanding as is possible of the causes of the crisis as well as steps to counter it. Better data will help clarify the role prescription opioids play in overdose deaths. The flaws in the existing data are detailed at length above. We recommend that the following steps be taken to improve the quality of the data collected:
- Standardize, as much as is possible, reporting of overdose death data across states, and work to include relevant information about substances involved, polypharmacy, and whether the substances included prescription or street opioids in reports;
- Clarify the extent to which prescription fentanyl versus illicit fentanyl contribute to overdose rates; and
- Cross-reference overdose death data with prescription monitoring data and other statistics to obtain detailed information about what percentage of opioid deaths involve recently prescribed opioids, and what percentage involve such opioids in the absence of heroin, fentanyl, or other illicit drugs and alcohol. While some states have performed such analyses, there is no such existing federal data. Furthermore, given that cutbacks in opioid prescribing have clearly affected long-term, high-dose patients, any investigation should explore what the original medical purpose of a given prescription was: whether it was meant to treat acute or post-operative pain or chronic pain.
Acknowledgments
Research for this report was conducted by Laura Mills and Diederik Lohman, respectively researcher and director of the Health and Human Rights division of Human Rights Watch. Laura Mills wrote the report. It was reviewed by Megan McLemore, senior researcher in the Health and Human Rights division of Human Rights Watch; Jasmine Tyler, Advocacy Director of US Programs; Jane Buchanan, Deputy Director of the Disability Rights Division; Christopher Albin-Lackey, senior legal advisor; and Babatunde Olugboji, Deputy Program Director. Matthew Parsons and Cara Schulte, associates with the Health and Human Rights Division, provided invaluable assistance, as did Nour Audi and Russell Simons, summer 2018 interns with Human Rights Watch.
We are deeply grateful to the many chronic pain patients who, despite being afflicted by medical conditions that made it difficult for them to participate in lengthy interviews, nonetheless agreed to be interviewed for this report, in some cases more than once. Without them and their relatives, this report would not have been possible. We are also thankful to the medical professionals who, despite their packed schedules, found time to discuss with us their concerns about prescribing and the challenges they face. Finally, we are grateful to chronic pain and harm reduction advocates whose input was invaluable for this report.
Human Rights Watch received funding for this investigation from the US Cancer Pain Relief Committee, an organization that supports research, education, and advocacy related to pain and palliative care.