In Harm’s Way
State Response to Sex Workers, Drug Users and HIV in New Orleans
Summary
What do I exchange sex for? Food, housing, everything.
—Donald, 40-year-old African-American man, New Orleans, March 2013
More than 1.1 million people in the United States are living with HIV and an estimated 56,000 people become newly infected each year. Some of the highest HIV-infection and death rates in the US are found in southern states such as Louisiana, where deep poverty combines with harmful laws and policies that increase the risk of acquiring, transmitting and dying of HIV. In the city of New Orleans, many people struggle for survival by exchanging sex for money, drugs, or life necessities while trying to protect themselves from HIV. This report presents the voices of sex workers, drug users, transgender women and others neglected, punished, and stigmatized by state laws and policies that endanger their safety, health and lives.
Eight years after Hurricane Katrina struck in 2005, many in New Orleans continue to feel its devastation. More than half of New Orleans’ 350,000 residents live in or near poverty and the city has the second-highest rate of homelessness in the nation. One quarter of the city’s housing stock is blighted or vacant. Yet the Louisiana state government does little to invest in housing, health care or support services for people unable to meet their basic needs. At the same time, state criminal laws block rather than facilitate a public health approach to sex work and injection drug use, which contributes to a death rate from AIDS in Louisiana that is more than double the national average.
Louisiana Governor Bobby Jindal steadfastly opposes expanding the Medicaid program, an option now being offered to states under federal healthcare reform. Instead of seizing an opportunity that would extend insurance benefits to an estimated 400,000 Louisiana residents, the state is moving in the opposite direction by planning to remove thousands of disabled persons from Medicaid eligibility in the coming year. State officials point to the quality of their public hospital system that serves more than 500,000 patients a year, most of whom are uninsured. But even a strong safety net is not a substitute for comprehensive prevention and primary care services, particularly when at least 90 percent of the cost will be borne by the federal government.
For many, safety nets remain out of reach. Louisiana has utterly failed to implement harm reduction methods proven to reduce HIV infections among people who inject drugs. Emphasizing public health and human rights, harm reduction programs provide essential health information and services while respecting individual dignity and autonomy. For drug users, access to clean syringes and equipment have been shown to lower HIV risk and hepatitis transmission, prevent overdose and provide a gateway for drug treatment programs and other important health information. Endorsed by public health authorities worldwide and an important part of the US National HIV/AIDS Strategy, syringe access programs and other effective harm reduction measures have made injection drug use the only mode of HIV transmission that has been in consistent decline since the epidemic began in the US.
Yet Louisiana prohibits sale and distribution of syringes not intended for medical use, categorizes syringes as illegal drug paraphernalia, and criminalizes even trace amounts of illegal drugs that may be found in a syringe. These laws combine to drive most syringe distribution programs underground, keeping clean needles out of the hands of those who need them the most. In New Orleans, the work of the public health authorities is done by activists like Nancy, a 28-year-old woman who delivers clean syringes and health information to drug users on her bicycle. Not surprisingly, neither Louisiana nor New Orleans has been able to reduce its rate of HIV infection among injection drug users in the last five years.
In Louisiana, drug users are also among those most likely to develop AIDS after testing positive for HIV and least likely to be receiving medical care. But the response of state and city officials to the urgent health needs of people who use drugs has been a failure, both in effort and result. Law reform is imperative to ease restrictions on syringe access, but there are many steps the state can take to increase drug users’ access to essential care and services. Health and harm reduction education is not illegal in Louisiana, even for people who inject drugs.
Louisiana also needs to reform its laws related to prostitution. Its “crimes against nature” statutes are insidious vehicles for state-sponsored discrimination against the lesbian, gay, bisexual and transgender (LGBT) communities and women of color and should be repealed without delay. The New Orleans municipal code also criminalizes “loitering for prostitution,” an offense so vague and broadly drawn that it permits police to consider a wide range of behavior to be grounds for arrest, including where people are, what they are wearing, and what they may have done in the past. Loitering statutes interfere with the right to be free from arbitrary arrest and invite discriminatory application, particularly on the basis of gender, race and ethnicity. In New Orleans, Human Rights Watch found that enforcement of these laws targeted transgender individuals, who described a community under siege from the police, subject to constant harassment, verbal abuse, stops for suspicion of prostitution, and demands for sex in exchange for leniency.
Sex workers and people suspected by police of engaging in sex work also reported that police use condoms as evidence of prostitution. In stops and searches related to possible prostitution, officers frequently commented on, confiscated, or threatened arrest on the basis of how many condoms someone was carrying. There is no indication that condoms have been used in prosecutions for prostitution; nonetheless, this practice has an alarming consequence for public health. Sex workers, transgender women and others at high risk of HIV infection told us that they were afraid to carry condoms and that they sometimes had to engage in sex without protection out of fear of police harassment. The New Orleans Police Department should immediately end this practice.
Louisiana has chosen punishment over public health for sex workers and people who use drugs. The United States has the highest incarceration rate in the world, and Louisiana’s incarceration rate is double the national average, giving it the unfortunate distinction of the world’s incarceration capital. In New Orleans, the NO/AIDS Task Force visits every prisoner who tests positive for HIV at the Orleans Parish Prison and arranges a medical appointment upon release. However, their clients are often arrested again before they can make it in to see the doctor; one transgender woman was arrested for prostitution 10 times in three years, and has yet to keep her appointment with the clinic. Jail inevitably interrupts the ability to take one’s HIV medications on a regular basis. Reports from the Orleans Parish Prison indicated delays ranging from two weeks to three months in commencing or resuming HIV treatment.
People who exchange sex for money, drugs, and life necessities have difficult and often dangerous lives. The challenge to public agencies of reaching a population whose primary concern is daily survival is not an easy one, and in New Orleans there is an active network of community organizations, medical providers and officials in the health department who are working to ensure access to care and services. In recent years, state and local health officials have significantly increased the number of people with HIV who are in treatment. Unfortunately, their work is undermined by state and local laws and policies, as well as police practices, that not only fail to reduce the risk of harm but exacerbate a high-risk environment where it is difficult for people to avoid HIV infection and to access life-saving treatment and support.
To effectively address the HIV epidemic and protect the human rights of people who exchange sex for money, drugs, or life necessities, the Louisiana state legislature should reform laws and policies on possession of syringes. Consensual, adult sex work should be decriminalized, and the city of New Orleans should expand community-based HIV prevention and treatment programs and engage individuals from high-risk communities in an effective response to their needs. The New Orleans Police Department is currently under federal oversight for constitutional violations and it should remain so until it has met its obligation to respect the human rights of the LGBT community. Until Louisiana substitutes a public health approach for punitive and discriminatory policies and invests in housing, health care and other basic human needs, HIV will continue to endanger the lives of the state’s most vulnerable residents.
Recommendations
To the City of New Orleans Health Department
- Expand health services to people who inject drugs by increasing harm reduction and health education and promoting HIV testing and linkage to care, hepatitis C testing and care, and the availability of evidence-based drug dependence services.
- Convene a citywide Working Group on the Health of Injection Drug Users with representation of people who use drugs and their advocates, medical providers and law enforcement to develop and coordinate strategies for improving health services to injection drug users.
To the New Orleans Police Department
- Immediately cease using the possession of condoms as evidence to question, arrest, or detain persons suspected of sex work. Issue a directive to all officers emphasizing the importance of condoms for HIV prevention and sexual and reproductive health. Ensure that all officers are regularly trained on this protocol and accountable for all transgressions. Inform the community that such action has been taken and that the New Orleans Police Department will not interfere with the right of any resident to possess condoms.
- Ensure compliance with federal court orders and New Orleans Police Department regulations for interaction with LGBT persons and enforce regulations prohibiting profiling transgender persons as sex workers, verbal abuse and sexual misconduct.
To the Orleans Parish Prison
- Ensure compliance with federal court orders and international standards relating to increased safety in confinement for all prisoners; adopt and enforce procedures required under the Prison Rape Elimination Act for all prisoners, particularly LGBT individuals.
- Take steps to reduce delay in access to HIV medications for incoming and newly diagnosed prisoners.
To the New Orleans City Council
- Repeal “loitering for prostitution” laws, which invite discrimination and punishment based on identity or status rather than criminal behavior.
To the Louisiana State Legislature
- Support expansion of Medicaid under the federal Patient Protection and Affordable Care Act of 2010 to increase access to medical services for residents of Louisiana.
- Address the lack of low-income housing in Louisiana, such as by increasing the Louisiana State Housing Trust Fund and allocating funds for low-income housing from the state’s portion of the Mortgage Settlement Fund.
- Decriminalize voluntary, consensual adult sex work as criminalization impedes the right to health and contributes to other human rights abuses of sex workers and those perceived to be engaged in sex work.
- Decriminalize the possession and distribution of sterile syringes as criminalization impedes the right to health. Repeal provisions of the laws criminalizing trace amounts of illegal substances in syringes and promote syringe access programs in the interest of public health and safety.
- Repeal the Crimes Against Nature statutes in their entirety.
To the Louisiana Department of Health and Hospitals
- Expand health services to people who inject drugs by providing state support for existing syringe access programs, increasing harm reduction and health education, and promoting HIV testing and linkage to care, hepatitis C testing and care, and the availability of evidence-based drug dependence services.
- Convene a statewide Working Group on the Health of Injection Drug Users with representation of people who use drugs and their advocates, medical providers and law enforcement to develop and coordinate strategies for improving health services to injection drug users.
- Support expansion of Medicaid under the federal Patient Protection and Affordable Care Act of 2010 to increase access to medical services for residents of Louisiana.
To the Governor of Louisiana
- Support expansion of Medicaid under the federal Patient Protection and Affordable care Act of 1010 to increase access to medical services for residents of Louisiana.
To the United States Government
- The Office of National AIDS Policy and the federal agencies charged with implementing the National HIV/AIDS Strategy should:
- Call upon states to prohibit the possession of condoms as evidence of prostitution and related offenses; develop a plan, led by the Department of Justice and the Centers for Disease Control, to provide guidance, technical assistance and model legislation to accomplish this objective;
- Ensure that HIV research and surveillance data adequately reflects the impact of HIV on people who exchange sex for money, drugs, or life necessities; and
- Increase efforts to ensure access to health care and harm reduction for people who inject drugs including, but not limited to, supporting the repeal of the federal ban on funding state and local syringe access programs and convening a national Working Group on the Health of Injection Drug Users with representation of people who use drugs and their advocates, medical providers, public health officials, and law enforcement to develop and coordinate strategies for improving health services to injection drug users.
- The US Congress should repeal the ban on federal funding for state and local syringe access programs.
- The US Congress should ensure that persons in Louisiana, and other states that do not expand Medicaid, have access to adequate healthcare services.
- The Department of Justice should continue oversight of the New Orleans Police Department until it demonstrates compliance with civil and human rights obligations in relation to the LGBT community.
To the United Nations
To the United Nations Committees on Human Rights and Racial Discrimination and the Human Rights Council:
- Call upon the United States to ensure that police and prosecutors cease using condoms as evidence of prostitution and related offenses.
- Call upon the United States to repeal broad loitering statutes that invite discrimination and punishment based on identity or status rather than criminal behavior.
- Call upon the United States to promote federal and state legislation supporting syringe access and other harm reduction programs as key elements of the rights to life and to health.
Methodology
This report is based on research conducted between February and September 2013, in the city of New Orleans, in the US state of Louisiana. Human Rights Watch researchers utilized a mixed-method approach that combined quantitative and qualitative interviews with key informant interviews and legal and policy analysis. The focus of the research was on the experiences and needs of individuals who self-identified as having had sex for money, drugs, or life necessities in the past year. In addition to basic demographic information, questions emphasized access to HIV prevention, medical care, and barriers to sustaining HIV treatment; interaction with the police and incarceration experience; and housing status.
The population of individuals who have exchanged sex for money, drugs, or life necessities is a difficult one to identify and randomly sample. We therefore sought to identify a diverse, if not fully representative, population and recruited participants through two methods.
For the quantitative component of the research, Human Rights Watch trained 13 peer interviewers in the administration of the survey and research ethics, including the importance of informed consent and confidentiality. Peer interviewers were diverse in age, gender, sexual orientation and ethnicity, and were selected upon the recommendation of advocates for sex workers, LGBT youth, persons living with HIV, and by city and state HIV officials and administrators. Not all peer interviewers exchanged sex for money, drugs, or life necessities but all had familiarity with individuals and networks of people who did so. Peer interviewers identified and administered the survey to a total of 143 individuals. An additional 26 individuals were identified by flyers left at targeted locations such as NO/AIDS Task Force offices, the syringe exchange site and other HIV service provider venues. Human Rights Watch researchers administered the survey to these participants directly.
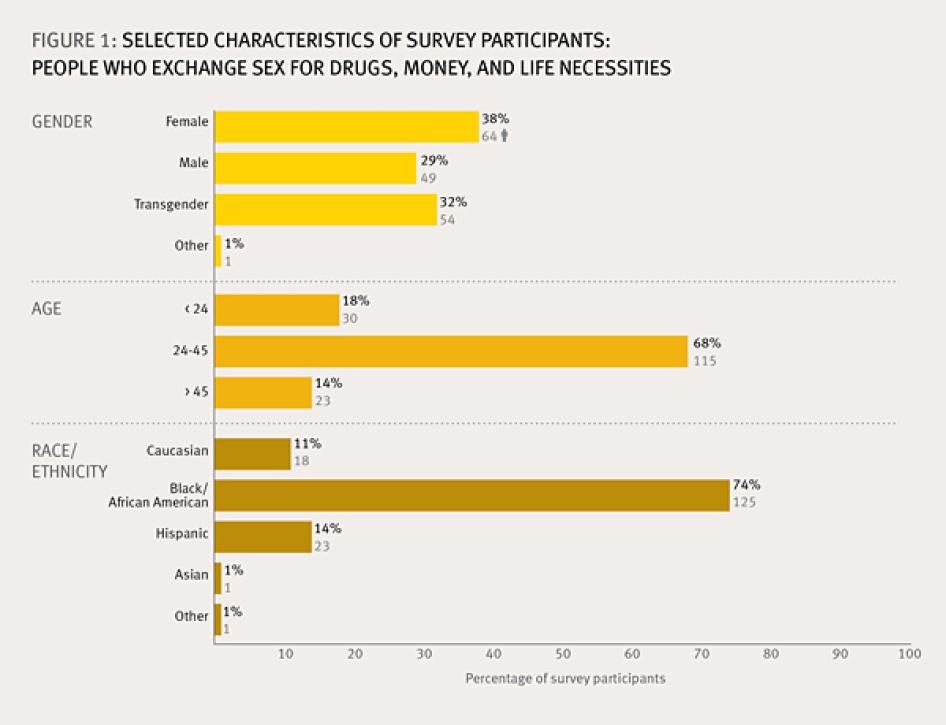
Individuals agreeing to participate in the survey were predominantly African-American (74 percent) and between the ages of 24 and 45 (68 percent); somewhat more female participants (38 percent) were included than male (29 percent) or transgender (32 percent). Peer interviewers were paid a small stipend which covered their training and administration of the survey. Gift cards were provided to interviewees in order to reimburse them for travel and related expenses. (See Figure 1)[1]
All participants were informed of the purpose of the survey, its voluntary nature, and the ways in which the information would be used. All participants provided oral consent to be interviewed and consent was noted on the survey form. Individuals were assured Human Rights Watch would not publish their names and all names reported are pseudonyms. Survey results were tabulated and analyzed with the assistance of the Louisiana Public Health Institute in New Orleans, a non-profit, non-governmental organization conducting research and providing technical assistance on public health and policy.
Human Rights Watch also interviewed more than 50 advocates, healthcare providers, public defenders, police, jail and prison officials, city and state HIV program administrators, and other public health officials in New Orleans and in the city of Baton Rouge. Among government officials, Human Rights Watch interviewed representatives of the Louisiana State Department of Health and Hospitals, the New Orleans City Council, the City’s Office of Health Policy and AIDS Funding, the New Orleans Police Department, and the Orleans Parish Prison.
Documents were obtained through public records requests and shared with Human Rights Watch from multiple sources including the NO/ AIDS Task Force, Orleans Parish Prison and the Municipal Court of New Orleans. Document requests to the New Orleans Police Department were not answered. All documents cited in the report are publicly available or on file with Human Rights Watch. Pseudonyms are used for anyone not interviewed in their official capacity in order to protect privacy and confidentiality.
Background
Sex Exchange and HIV
People in New Orleans who exchange sex for money, drugs, and life necessities are a diverse population. Some exchange sex for food, housing and other fundamental elements of survival while others exercise greater autonomy and may identify themselves as sex workers. Most share an environment in which the risk of acquiring, transmitting and dying of HIV and AIDS is higher than those not engaged in sex exchange.[2] For some, this environment of risk is shaped by poverty, discrimination, and drug dependence, factors that are independently associated with higher risk of HIV infection and poor treatment outcomes.[3] As stated in the National HIV/AIDS Strategy for the United States:
HIV is often only one of many conditions that plague communities at greater risk of HIV infection. In many cases, it is not possible to effectively address HIV transmission or care without also addressing substance use, poverty, homelessness and other issues.[4]
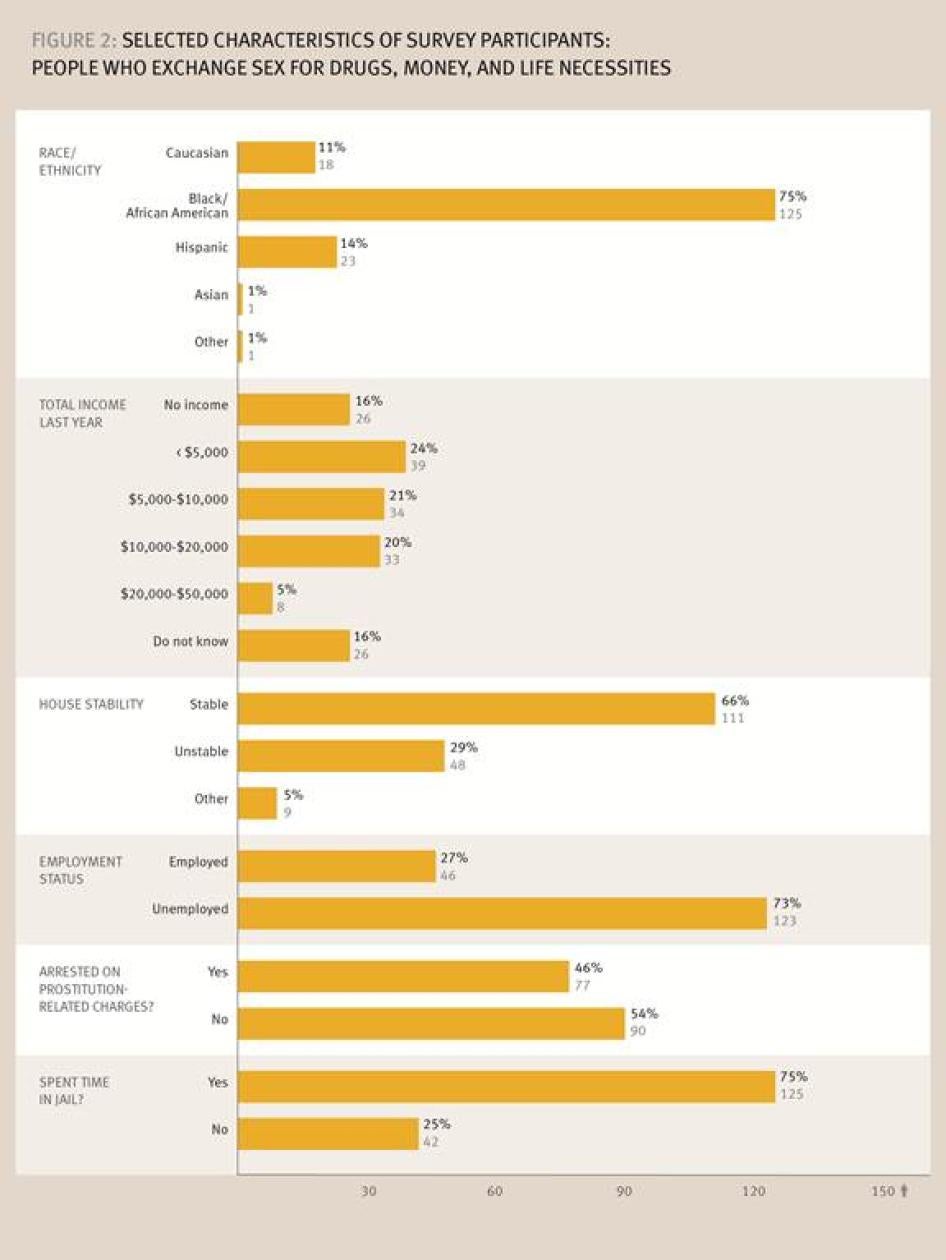
This report presents a snapshot of people who exchange sex for money, drugs, and life necessities in New Orleans, but in many ways its participants reflect the profile of the HIV epidemic in the US South. Of the 169 people interviewed for the survey, 74 percent were African-American; the majority reported income of less than $5,000 per year; nearly one of three reported an “unstable” housing situation; and only one out of every three was employed. (Figure 2)
The criminalization of sex workers and drug possession is increasingly being identified as a barrier to HIV prevention and access to care. The United Nations AIDS organization (UNAIDS) and the Global Commission on HIV and the Law have recommended consideration of decriminalization of sex work as a public health rather than criminal approach to drug use.[5] For participants in the Human Rights Watch survey, interaction with the criminal justice system was common. Seventy-five percent of people surveyed reported having spent some time in jail. Nearly half had been arrested on prostitution-related charges, with 60 percent of transgender women reporting arrest for prostitution (Figure 2).
Human Rights Watch has documented how anti-prostitution enforcement and harsh penalties for low-level drug possession impede the right to health and contribute to conditions where discrimination, violence and other human rights abuses are tolerated, in the United States and globally.[6] As in these previous reports, Louisiana’s drug and anti-prostitution laws represent key barriers to HIV prevention, access to care and the ability to sustain treatment in New Orleans.
HIV in New Orleans
The state of Louisiana, along with the rest of the US South, lies at the center of the nation’s HIV epidemic. Louisiana has the second highest rate of HIV infection in the United States and the fourth highest rate of AIDS among adults and adolescents.[7] As of 2012 there were nearly 19,000 people living with HIV in Louisiana, over half of whom have been diagnosed with AIDS.[8] Many are diagnosed in late stages of illness, and 36 percent of people diagnosed with HIV are not receiving HIV-related medical care.[9] Late diagnosis and lack of medical care contributes to a rate of deaths from AIDS in Louisiana that is nearly double the national average.[10]
Racial disparities among those affected by HIV are dramatic in the state. African-Americans are 32 percent of the state population, but they comprise 73 percent of newly diagnosed HIV cases and 76 percent of new AIDS cases.[11] Rates of newly diagnosed HIV cases among African-American women are 16 times higher than the rate among white women.[12] Male-to-male sexual contact is the predominant mode of transmission for both those living with HIV and newly diagnosed infections, followed by “high-risk heterosexual contact” and injection drug use.[13] Among women, the primary modes of transmission are high-risk heterosexual contact and injection drug use.[14]
Most people living with HIV in Louisiana reside in the state’s two largest cities, New Orleans and Baton Rouge, and the epidemic continues to spread in these cities at rates that lead the nation. The eight-parish region known to the US Centers for Disease Control (CDC) as the New Orleans Eligible Metropolitan Area (NOEMA) for HIV surveillance and data purposes is comprised of the parishes of Orleans, Jefferson, Plaquemines, St. Bernard, St. Charles, St. James, St. John the Baptist, and St. Tammany. This metropolitan area has the second-highest rate of new HIV infections in the United States, and the Baton Rouge metropolitan area has the third-highest rate of new HIV infections in the country.[15] Baton Rouge also ranks first in AIDS case rates and New Orleans ranks fourth among major metropolitan areas in the United States.[16]
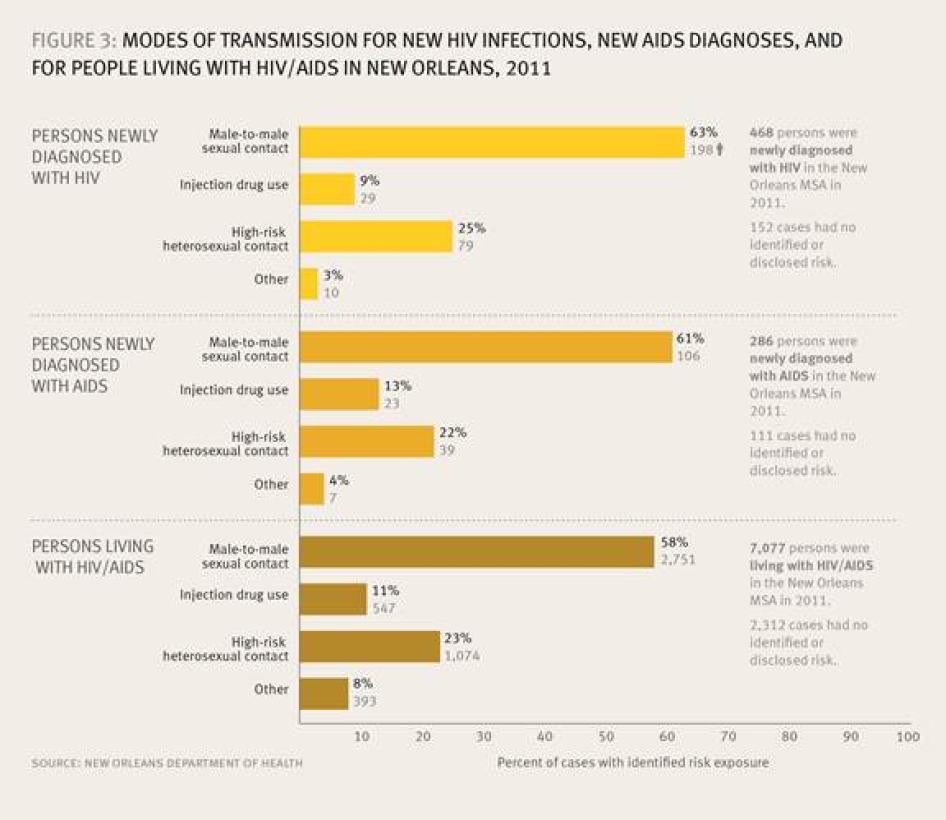
In the New Orleans metropolitan area, there are an estimated 7,200 people living with HIV, more than half of whom are living with AIDS.[17] Three-quarters of those living with HIV are men, although transgender persons have been categorized as men due to inaccurate data collection methods.[18] Modes of transmission for new HIV infections, new AIDS diagnoses, and for people living with HIV in New Orleans are illustrated in Figure 3.
In New Orleans, 41 percent of people with HIV are not receiving HIV-related medical care.[19] Those most likely to be out of medical care in New Orleans are males, Hispanics, Asians and American Indians, and persons 65 and older. Notably, injection drug users are the least likely to be receiving medical care of those in all exposure categories, and also among those most likely to develop AIDS within six months of their HIV diagnosis. These factors point to low utilization of health services by injection drug users as they are being tested for HIV at a very late stage in the disease.[20]
To understand why so many people in Louisiana and New Orleans specifically are not receiving HIV care, one must look to two primary factors: poverty and Hurricane Katrina. Louisiana is one of the poorest states in the nation, with nearly one in three residents, and one in three children, living under the federal poverty level ($11,170 per year for individuals in 2012).[21] About 45 percent of African-Americans in Louisiana live in poverty, as do 40 percent of Hispanic residents.[22] An estimated 20 percent of Louisiana residents have no health insurance coverage, compared to a national average of 16 percent.[23]
In New Orleans, the picture is even bleaker. A 2012 study showed that the poverty rate in New Orleans was nearly double the national average. One out of four New Orleans residents had a zero or negative net worth, 10 percent had no access to a vehicle, and 13 percent had no checking or savings account.[24] The New Orleans Regional AIDS Planning Council has identified the primary barrier for individuals to access HIV services in New Orleans as “severe poverty” and “accessing survival services such as food and housing” that for many, makes HIV a low priority in their lives.[25]
In many respects New Orleans is still seeking a full recovery from the impact of Hurricane Katrina. In August 2005, the city endured Hurricanes Katrina and Rita and the collapse of the levee system that flooded 80 percent of the city. Eight years later, however, the toll of the storm on the housing market, job opportunities and the lives of many individuals remains palpable. The 2010 census showed nearly a 10 percent decline in population since 2000.[26] One out of four houses in New Orleans is blighted or vacant.[27] New Orleans has the second-highest rate of homelessness in the nation.[28]
New Orleans was a predominantly African-American city with a high rate of poverty before Katrina, and significant racial disparities continue to characterize the city’s economic recovery. In 2011, black households earned 50 percent less than white households in New Orleans. Though New Orleans’ overall unemployment rate is only slightly higher than the national average, 53 percent of black men of working age are unemployed, compared to 25 percent of white men locally. In New Orleans, there has been no increase in the percentage of black men attaining bachelor’s degrees in the last 10 years. [29] Black men over 18 are 53 percent of the city’s population but 84 percent of those incarcerated in the Orleans Parish Prison.[30] Though poverty rates actually declined for African-American women after Katrina, longitudinal studies indicate that this does not necessarily reflect an increase in income for this population. Rather, evidence suggests that many of the city’s poorest women did not return to their homes after the storm.[31]
Louisiana Law and Policy Analysis
Syringe Access
The sharing of needles during injection drug use (IDU) is a major risk factor for the transmission of HIV, hepatitis C and other blood-borne diseases. Nationally, injection drug users represent 12 percent of new HIV infections and 19 percent of people living with HIV/AIDS.[32] For drug users, the availability of drug dependence treatment and harm reduction services, including access to sterile syringes, is a key component of the right to health.[33] Syringe exchange programs (SEP), like other harm reduction measures, “meet people where they are” by exchanging clean syringes for used ones, and can be an important opportunity to link people who use drugs to health care and social services.
The effectiveness of syringe exchange in reducing HIV transmission is well documented, globally and in the United States.[34] The federal Centers for Disease Control and Prevention (CDC) endorse syringe exchange programs as part of comprehensive harm reduction for drug users that includes testing for HIV, hepatitis C and STDs and linkage to drug dependence treatment.[35] SEPs have been associated with a reduction in HIV risk behaviors and HIV prevalence, and the ancillary services provided by these programs improve health by providing information about disease prevention and wound care, promoting access to drug treatment, HIV testing, and referrals to non-judgmental sites for overall health care.[36] In providing safe disposal of injection equipment, harm reduction programs reduce the number of contaminated syringes circulating in a community. Thus, SEPs also protect law enforcement officers from needle stick injuries- accidental pricks to the skin from handling hypodermic needles.[37] Syringe exchange and other effective harm reduction measures have made injection drug use the only mode of HIV transmission that has shown long-term consistent decline in adults and adolescents since the epidemic began.[38]
In states with syringe access programs such as New York, the percent of new HIV infections attributable to injection drug use declined from 12 percent in 2002 to 4 percent in 2010.[39] In New York City, operation of a comprehensive syringe access program has brought the rate of new HIV infection among injection drug users to “near zero” according to scientists gathered at the International AIDS Conference in 2012.[40] New Orleans has been unable to reduce new HIV infections among injection drug users as this figure was the same in 2011 as it was in 2008, with infections increasing in the intervening years.[41]
Approximately 45,000 people who inject drugs live in Louisiana, and more than a quarter of them reside in New Orleans.[42] State health authorities estimate that 6 percent of people who inject drugs are living with HIV.[43] Injection drug users tend to have poor health outcomes as a result of later HIV testing and less linkage to medical care than those in other transmission categories. In Louisiana, nearly half of injection drug users newly diagnosed with HIV developed AIDS within six months, indicating that they were tested at a late stage in the disease. Indeed, in Louisiana, injection drug users (IDU) were significantly more likely to be newly diagnosed with AIDS than with HIV.[44] In New Orleans, 48 percent of injection drug users living with HIV are not receiving HIV-related medical care.[45]
Clearly, the need is great for HIV prevention and treatment services for people who inject drugs both statewide and in New Orleans. The State HIV/AIDS Plan for 2012-2015 identifies injection drug users as a “priority population” in need of targeted services and increased resources. Yet the report states “there is currently no IDU-specific programming provided in the state of Louisiana.”[46] This alarming lack of services is explained in the report’s discussion of the array of state criminal laws and policies that appear to block the implementation of syringe exchange by state public health officials. There is no explicit authorization for syringe exchange operation in Louisiana statutes or public health regulations. Criminal laws make distribution of needles without a prescription a felony offense and needles are classified as illegal drug paraphernalia.[47] State drug laws also criminalize even trace amounts of residue of heroin and other illicit substances that might be found in a syringe.[48]
Louisiana law does, however, create an important exception to the prohibition on distribution of syringes. Under Louisiana Revised Statute 40:1024, the prohibition on distribution of syringes “shall not apply to the manufacture, sale, distribution or advertisement of any product or object designed and sold primarily… for bona fide medical or clinical use.” The state administrative code identifies the prevention of transmission of communicable diseases as a legitimate medical need.[49] This exception provides legal protection for the one public syringe exchange program operating in Louisiana.
The Syringe Access Program began operating in New Orleans in May 2006 as part of the Tulane University School of Medicine’s Drop-In Center. The center offered a variety of services for homeless youth, including counseling, referrals and a food bank. In August 2012, the syringe access program transferred to a site at the NO/AIDS Task Force and NO/AIDS now operates the program. The Syringe Access Program office is located in the French Quarter of the city and is open for two hours on Friday afternoons each week. Approximately 80 clients a week receive a supply of clean needles as well as information about HIV, hepatitis, harm reduction and drug dependence treatment resources.[50]
Criminalization of syringe possession remains a serious concern. Elizabeth Jones, who directed the Drop-In Center’s syringe exchange before it transferred to NO/AIDS, told Human Rights Watch that, “As a medical facility, the law protects us but not our clients. They can still be charged with possession of a syringe.”[51]
In addition to the public program operated by NO/AIDS, several “underground” syringe exchanges operate in New Orleans. These small informal exchanges are volunteer-driven and offer clean needles, disposal containers for dirty needles, harm reduction information and other resources to drug users familiar with these providers. The scale of these grassroots efforts is small: for example, one group delivers clean needles by bicycle to an estimated 100 regular clients. The reach of these programs is limited not only by the size of the organization, but by fear of the criminal law. One informal syringe provider explained:
Nobody really knows what the law is for giving out the needles, it might be ok and it might not. But we do know the clients can be arrested for possession so we keep it very quiet and low profile, for everyone’s sake.[52]
Data on city arrests for drug paraphernalia indicate that fear of arrest is not misplaced. From January 2011 through August 2013, 658 charges for illegal possession of drug paraphernalia were brought in New Orleans Municipal Court.[53] These records did not specify which arrests were for syringe possession, but interviews with drug users, their advocates and public defenders indicated that in New Orleans, police made arrests for syringe possession on a regular basis. Virginia Ryan, client services coordinator for the New Orleans Public Defender, said that, “NOPD will definitely arrest for syringe possession. Often it is combined with prostitution or other charges. Yes, we see it all the time.”[54]
The cloud of criminality and legal uncertainty surrounding drug paraphernalia results in an enormous unmet need for clean syringes among drug users in New Orleans. According to the World Health Organization, a syringe exchange program should reach at least 60 percent of an injection drug user population in order to effectively control HIV.[55] A recent study of injection drug users in New Orleans conducted for the CDC found that the syringe access program was utilized by only 18 percent of those surveyed. [56] Dr. MarkAlain Déry, medical director of the Syringe Access Program in New Orleans, told Human Rights Watch:
The syringe exchange available in New Orleans is not coming close to making a dent in what is an urgent need. This is unfortunate because a syringe costs about 10 cents, and treatment for HIV or hepatitis costs hundreds of thousands of dollars.[57]
In 2012, the Louisiana Office of Public Health conducted a CDC National HIV Behavioral Surveillance survey of injection drug users in New Orleans for the CDC. The research involved 495 participants, providing an in-depth exploration of the lives of people who inject drugs, and who exchange sex for life necessities, in the New Orleans metropolitan area. Many of the findings from Human Rights Watch’s investigation are similar to those revealed by the broader research results.
The majority of injection drug users surveyed in New Orleans were African-American, though more than 35 percent were white. Most were poor, with 75 percent reporting an income of $12,500 or less, and 43 percent were unemployed. Nearly 40 percent had not completed high school. Some 91 percent had been in jail or prison, with half reporting incarceration within the last 12 months.[58]
Of the participants in the CDC survey, one of four had exchanged sex for money or drugs. Of the men who answered the survey, 25 percent had exchanged sex for money or drugs, and 31 percent of the women had done so. Exchange sex increased as income levels decreased, with the highest percentage (29 percent) of exchange sex reported from those with incomes below $12,500 per year.[59]
As noted above, 82 percent had never accessed the local syringe exchange, and 65 percent reported having shared a syringe in the last 12 months.[60] Of the 490 participants who answered this question, 46, or 9 percent, reported being HIV positive. Fifty-four percent reported having hepatitis C, though the researchers noted that hepatitis C prevalence was likely to be significantly higher, as even the $79 cost of taking a test for hepatitis C in New Orleans was prohibitive for most respondents.[61]
Harsh criminal laws have created an environment hostile to the public funding of syringe exchange, for even the one formal syringe access program that does exist receives no federal, state or city funding. The NO/AIDS Task Force Syringe Access Program is funded solely from private donations and experiences occasional shortages and interruptions in its supply. The federal ban on syringe exchange funding to state programs was reinstated by Congress in 2012, eliminating a potential source of support and imposing staff restrictions, as no personnel whose position is federally funded may work at the Syringe Access Program. Yet the NO/AIDS Task Force is committed to the Syringe Access Program and is ready and willing to expand it if they receive the funds.[62] Jean Redmann, director of Prevention, said:
It is a hard program to run in Louisiana, believe me. We’re on a shoestring now. But we know how important it is and we work around the federal red tape and the lack of money. But would we scale up if we got some funding from the state? Oh good Lord, yes![63]
But funding and law reform are not the only steps the state can take to address the lack of access to health services for injection drug users. It is not illegal to provide health information in Louisiana, even to drug users, who need targeted information that goes beyond basic HIV prevention. Many US states operate clinics, centers, mobile vans and other outreach services to drug users and other populations that find it difficult to access traditional health settings. Washington, DC has convened a Working Group for Drug User Health that brings together many stakeholders from medical providers to outreach workers and drug users themselves to discuss ways to improve access to health care.[64]
The New Orleans-based organization Women with A Vision has for 22 years advocated for the most marginalized communities in New Orleans—very poor, mostly African-American women, many of whom exchange sex for money, drugs, and life necessities. Women With A Vision has attempted to fill the void left by the public health department for decades by providing comprehensive harm reduction services, including syringes, wound-care kits and HIV and hepatitis C prevention information to people who have no other resource in the city, and in the region. Women With A Vision’s nearly 100 regular harm reduction clients include white men who come from as far as Mississippi and rural Louisiana to receive essential disease prevention services. Deon Haywood, executive director of Women with A Vision, said that Louisiana’s health department could be doing much more to assist a population at high risk for HIV and hepatitis C:
It would not be difficult to hang a poster in a health clinic or hospital that says “If you use injection drugs, here are ways you can protect your health.” That would send the message that the public health department cares if you live or die.[65]
Anti-Prostitution Enforcement
Louisiana state law prohibits prostitution, an offense defined as “the practice by a person of indiscriminate sexual intercourse with others for compensation.”[66] Also prohibited is prostitution by solicitation and penalties begin at a fine of $500 and imprisonment for six months for the first offense.[67] The criminal code for the City of New Orleans prohibits prostitution and solicitation for prostitution with the same penalties as under state law, but the city code adds the offense of “prostitution loitering.” As under similar statutes in other states, some of which have been found unconstitutionally vague, the loitering statute permits arrest based on a wide range of behaviors and factors that include flagging down motorists, gesturing to passers-by, and being known to police as having been convicted for prostitution in the past.[68]
Louisiana law also criminalizes “crimes against nature.” The crimes against nature statute defines this offense as:
The unnatural carnal copulation by a human being with another of the same sex or opposite sex or with an animal, except that anal sexual intercourse with another human being shall not be deemed to be a crime against nature when done in any of the circumstances described in Revised Statutes 14:41 [rape]. …Emission is not necessary, and when committed by a human being with another, the use of the genital organ of one of the offenders of whatever sex is sufficient to constitute same.[69]
A separate section of the law criminalizes “crimes against nature by solicitation,” defined as “the solicitation of a human being by another with the intent to engage in any unnatural carnal copulation for compensation.”[70] “Unnatural carnal copulation” was interpreted by Louisiana courts to mean “oral or anal sexual intercourse.”[71] In 2003 the US Supreme Court ruled in Lawrence v. Texas that state anti-sodomy laws were unconstitutional.[72] Louisiana courts subsequently upheld the portion of the statute that criminalized soliciting a crime against nature for compensation, ruling that “public, commercial sexual conduct” was not protected by the Supreme Court’s holding in Lawrence.[73] Therefore, one can still be arrested for soliciting a crime against nature (including oral and anal sex) for compensation.[74]
Moreover, until 2011, persons arrested for solicitation under the crimes against nature statutes were subject to felony charges while persons arrested for solicitation under the non-crimes against nature statutes were charged with misdemeanors. Persons convicted under the crimes against nature by solicitation statutes were required to register as sex offenders on the state registry, while those convicted of prostitution were not. This sentencing disparity was addressed in part by the legislature, which in 2011 equalized penalties for crimes against nature by solicitation and prostitution offenses for persons convicted after August 15, 2011, by lowering crimes against nature offenses to misdemeanors and eliminating the sex offender registry requirement. People convicted of crimes against nature by solicitation and their advocates then successfully brought suit to attain equalization of penalties for convictions occurring prior to August 15, 2011.[75] A subsequent class action resulted in the removal of more than 800 people from the sex offender registry and more than 500 in Orleans Parish alone.[76]
The crimes against nature statute, however, continues to create inequities and promote discrimination against LGBT people and poor women of color through discriminatory enforcement and the stigma associated with the charge. Inequitable penalties persist in some aspects of the law. For example, a conviction for soliciting “crimes against nature” with a minor requires sex offender registration while identical conduct under the prostitution statute does not.[77] Louisiana human rights advocates object to the very existence of the statute as an invitation to discrimination and abuse. Despite the holding of the US Supreme Court in the Lawrence case, the statute continues to provide a vehicle for criminalization of consensual oral and anal sex among adults in private. As recently as July 2013, Baton Rouge police were continuing to enforce the crimes against nature statute by engaging in a pattern of arresting gay men under the original crimes against nature statute despite consistent dismissal of the charges by prosecutors. When challenged, police department officials responded that the constitutionality of the laws was not their concern; rather, their duty was to enforce any law that was still “on the books.”[78]
In New Orleans, police continue to arrest people for solicitation of a crime against nature. A review of municipal court records indicated that 82 people were charged with this crime in the last two years, and local activists confirm that arrests for crimes against nature remain a part of the New Orleans’ Police Department’s (NOPD) anti-prostitution enforcement.[79] Women With A Vision has led the challenge to the crimes against nature laws in Louisiana. Deon Haywood explained that LGBT persons and poor women of color are most often targets of these arrests, and convictions can carry serious repercussions:
Getting a charge for a crime against nature on your record is worse than a regular prostitution charge. It brands you as a deviant, a freak of some kind.[80]
In New Orleans, anti-prostitution enforcement has been just one aspect of a troubled history of abuse and misconduct by the New Orleans Police Department. The NOPD is currently under federal oversight after the US Department of Justice issued a report in March 2011 finding a pattern and practice of constitutional violations in the areas of excessive use of force, arbitrary stops, searches and arrests, and discriminatory policing on the basis of race and ethnicity as well as sexual orientation and gender.[81] The report stated that LGBT individuals were subject to “harassment and disrespectful treatment” by the NOPD, and that black transgender women were improperly profiled as sex workers. The Justice Department stated:
We also found reasonable cause to believe that NOPD practices lead to discriminatory treatment of LGBT individuals. In particular, transgender women complained that NOPD improperly target and arrest them for prostitution, sometimes fabricating evidence of solicitation for compensation. … Indeed, community members told us they believe some officers equate being African American and transgender with being a prostitute.[82]
A lawsuit followed publication of the Justice Department report and in July 2012 the City of New Orleans entered into a Consent Decree Regarding the New Orleans Police Department.[83] The Consent Decree requires comprehensive changes to practices, procedures, training and discipline within the police department and mandates the development of a policy for non-discriminatory engagement with the LGBT community. Following a year of intense advocacy by activists led by LGBT youth of color in New Orleans, a policy was adopted by the NOPD in June 2013 intended to “ensure that the employees of the New Orleans Police Department do not engage in discriminatory policing and/or racial/bias-based policing or violate any related laws while serving the community.”[84] The policy prohibits the use of demeaning, derogatory or harassing language toward LGBT people; prohibits sexual harassment of members of the public; and states that “officers shall not use an individual’s actual or perceived gender identity or sexual orientation as probable cause that an individual has or is engaged in any crime.” [85]
Lack of Access to Health Care
Louisiana is not a healthy state. The United Health Foundation ranked Louisiana 49th out of 50 states in overall health in 2012, an evaluation taking into account a variety of factors including low health literacy, lack of access to medical care, high levels of obesity, high rates of infant mortality and infectious disease.[86] In Louisiana, 20 percent of the population has no health insurance, but that generalized figure hides significant racial disparities in access to insurance. Minorities are much more likely to be uninsured, as 30 percent of African-Americans and 51 percent of Hispanics are without insurance, compared to 18 percent of whites.[87]
The political environment in Louisiana is problematic for low-income people seeking access to health care. In 2008 Governor Bobby Jindal took office with a $1 billion budget surplus.[88] By fiscal year 2009, however, the state faced an enormous budget shortfall, primarily the result of the largest income tax cut in the state’s history at $1.1 billion over five years.[89] The health care and education budgets are the only categories left unprotected from the state constitution’s balanced budget requirement, and every year of the Jindal administration, Louisiana has seen deep cuts in both of these areas.[90]
The state healthcare budget was thrown into further crisis in July 2012 when the federal government reduced its matching funds for Medicaid and Medicare reimbursement due to a previous overpayment to the state. This action produced an $860 million gap in the state’s $25 billion budget and triggered a cascade of drastic program cuts and reorganization to state healthcare services, including privatization of both the Medicaid program and the hospital system for providing medical care to the uninsured.[91] In the past three years, $2.5 million has been eliminated from the state HIV prevention budget, resulting in staff layoffs and what state health authorities called “a reduction of services and resources that are available to the community.”[92]
Indeed, both state and city HIV administrators cited the challenges of maintaining services to an HIV population that is increasing amid chronic budget shortfalls on the federal, state and local levels. The Comprehensive HIV Plan for New Orleans states that “regardless of whether the funding cuts are at local, state or federal levels the complications are numerous…when local and state cuts occur they often occur with little warning and even less input from impacted offices.”[93] A recent report from the Harvard Law School’s State Healthcare Access Research Project commends Louisiana’s HIV program for significant accomplishments in the face of adverse conditions.[94] Both state and local health officials actively seek additional federal funds in the form of competitive grants and use these funds effectively in many respects. Despite constant budget crises, for example, the percentage of people living with HIV who are not in care has decreased from 58 percent in 2009 to 36 percent in 2012.[95]
Yet despite the chronic shortfall of state healthcare funds, the Jindal administration remains steadfastly opposed to the infusion of federal support that would result from implementation of the Affordable Care Act (ACA).[96] Louisiana was one of 26 states that brought suit to challenge the ACA on constitutional grounds. The June 2012 decision by the Supreme Court upheld most of the ACA but left the issue of Medicaid expansion to the states to decide.[97] Under the formula established by the ACA, states may choose to expand Medicaid eligibility in 2014 to most persons with incomes 133 percent of the federal poverty level (about $15,000 per year for individuals and $30,000 per year for a family of four.) With a 5 percent income disregard, the effective income level for Medicaid eligibility will be 138 percent of poverty level. People with qualifying incomes will be eligible whether or not they have children or are disabled. States that do so will receive federal funds to cover most of the cost of this expansion until the year 2020. Specifically, the federal government will pay 100 percent of the expansion costs from 2014-16 and 90 percent of the costs until the year 2020 and thereafter.[98]
In 2013 the Louisiana legislature voted not to expand Medicaid under the Affordable Care Act.[99] The Jindal administration has called Medicaid expansion under “Obamacare” too expensive, too uncertain, and too intrusive to states’ ability to control their insurance plans for low income residents.[100] However, reports from the Louisiana Budget Project, the Center for Budget and Policy Priorities and other analysts indicate that the expansion would improve the state budget and overall economy. Louisiana’s Medicaid spending would increase by only 1.7 to 2.8 percent from 2014-2019 while the state is likely to see substantial savings through reductions in uncompensated care—visits to hospital emergency rooms—and the benefits of a healthier population.[101] Even the Louisiana Department of Health and Hospitals has conceded potential fiscal benefits to the state if expansion were implemented.[102]
Most importantly, Medicaid expansion would provide health insurance to approximately 400,000 low-income residents of Louisiana who currently have little or no insurance.[103] In Louisiana, an estimated 60 percent of HIV-positive individuals receive healthcare coverage through Medicaid, and more would be covered under the ACA as disability would no longer be required for eligibility.[104] Although Louisiana Medicaid currently provides comprehensive coverage for 95 percent of the state’s poorest children, strict eligibility requirements exclude most poor and working adults. Nationally, the typical income limit for adults to qualify for Medicaid is $12,200 for a family of three. But in Louisiana, parents making more than $2,860 a year for a family of three are making too much to be eligible for Medicaid. Adults without children are not eligible at all unless they are disabled.[105] The state is actually moving to further shrink its Medicaid rolls as it plans substantial cuts to a program that permits disabled recipients of Social Security Insurance to work and still be eligible for Medicaid.[106] The Louisiana Budget Project urged the state to expand Medicaid, noting that “at a time when Louisiana’s health care safety-net is under severe financial strain, a decision to forego expansion will leave the uninsured with few other options.”[107]
In an interview with Human Rights Watch, Secretary of the Louisiana Department of Health and Hospitals Kathy Kliebert emphasized what she said was the unique strength of the state’s “safety net” for uninsured residents.[108] Since the late 1990s, the 10 hospitals and dozens of clinics of Louisiana State University (LSU) have provided free or subsidized care for uninsured, indigent and underserved communities throughout the state. The LSU hospitals also provide training for most of the medical and nursing students in the state. Tight restrictions on Medicaid eligibility create high demand for subsidized care at LSU hospitals, which served 530,000 patients in Fiscal Year 2010-2011, nearly all of whom were uninsured.[109] LSU Hospitals also participate in the Louisiana Public Health Information Exchange, an innovative system for sharing electronic medical records that allows providers to identify people who have fallen out of care for HIV and other infectious diseases. [110]
The LSU hospital system, however, bore the brunt of the budget cuts imposed as a result of the loss of federal healthcare funds in 2012. Indeed, state funding for LSU hospitals has been reduced by 36 percent since Fiscal Year 2008-2009, and the resulting crisis paved the way for approval of plans for private companies to purchase leases from the state and manage the hospitals themselves.[111] To date, five hospitals have been converted to management by private companies and state officials express confidence that this arrangement will permit the state to maintain services to the uninsured. Some health analysts and Louisiana state legislators are not certain, however, that this approach is sustainable when federal dollars for hospitals to serve uninsured persons are set to decline steadily under the Affordable Care Act.[112] Moreover, the package of required services under Medicaid expansion includes preventative, wellness, prescription drug and other services not available from the LSU hospital system.[113]
Kliebert told Human Rights Watch that, “We believe that the hospital system in our state is a strong safety net for the uninsured, providing medical care of at least the same quality and quantity as that provided under Medicaid.”[114]
The quality of the LSU system may be comparable to that of Louisiana Medicaid but neither entity is adequately addressing the needs of the state’s poorest residents. Governor Jindal himself called Medicaid in Louisiana a “system that delivers sub-par results.”[115] Both the LSU hospital system and the state Medicaid system received low marks in a recent independent evaluation of healthcare systems for low income persons. The Commonwealth Fund examined access and affordability, prevention and treatment, avoidable hospital visits and healthy living promotion for persons living at or below 200 percent of the federal poverty level in each of the 50 states. Louisiana ranked 49th out of 50 states overall, and the report concluded:
When looking today at health care access, quality and outcomes, we see two Americas, sharply divided by geography and income. As federal health reforms take hold, state governments and local delivery systems have a historic opportunity to address these inequities.[116]
Housing Policy
Housing is a fundamental human right, critical to dignity, survival and the ability to protect one’s health.[117] It is well established that housing is particularly important for HIV prevention and for the health of people living with HIV and AIDS.[118] Homeless individuals living with HIV die at a rate five times higher than those who are housed. In addition, stable housing supports HIV prevention efforts as it reduces drug use and increases access to mental health care and other social assistance.[119] The crucial role of housing to people living with HIV is emphasized in the National AIDS Strategy for the United States:
Individuals who lack stable housing are more likely to delay HIV care, have poorer access to regular care, are less likely to receive optimal antiretroviral therapy, and are less likely to adhere to therapy.[120]
New Orleans has an acute lack of affordable housing. Hurricanes Katrina, Rita and the subsequent collapse of the levees displaced 455,000 persons, damaged 70 percent of the city’s housing stock, and destroyed 51,000 rental units, including a 75 percent reduction in the number of public housing units as several low-income apartment complexes were bulldozed following the storm.[121] An influx of federal emergency and recovery funding has replaced only 25 percent of the rental housing lost in the aftermath of the hurricane.[122] Though progress has been made, the city continues to feel the impact of Katrina on housing availability. UNITY, a local advocacy organization for the homeless, counted 2,300 homeless people during one night in January 2012. Of these, 60 percent had not been homeless prior to Hurricane Katrina.[123]
In addition to Katrina, the Gulf of Mexico oil spill and chronic state and city budget crises have left thousands of low income people without adequate shelter. Rents have risen 45 percent since 2005, and the cost of an average one-bedroom apartment is currently $800 per month. One in two New Orleans residents pays more than half of their income toward rent, and many homeowners also struggle with mortgage payments that exceed their income, overcrowding and living in substandard conditions.[124]
People living with HIV face additional housing challenges due to discrimination and illness that often leads to unemployment or disability. The CHANGE Coalition recently conducted an assessment of people living with HIV in New Orleans. They found that 6.5 percent of study participants were homeless. Of those who had housing, their situation was often precarious. Nearly 70 percent paid more than a third of their income in rent or mortgage payments, a situation identified by the federal government as living under a “severe cost burden” in relation to housing. One of three people living with HIV responding to CHANGE’s survey stated that an increase of $50 in their monthly housing cost would require them to move. Although federal housing programs such as Housing Opportunities for People with AIDS (HOPWA) provide targeted assistance to people living with HIV, less than one of three survey participants reported receiving a housing subsidy of any type.[125]
Findings
Barriers to HIV Prevention for People Who Exchange Sex
Ninety-five percent of the 169 individuals Human Rights Watch interviewed indicated that they had received HIV prevention information, with one out of four having received such information in the last week, and three out of four having received it in the last year. Participants reported receiving HIV prevention information from their medical providers, outreach services, school, friends, and while in jail.
However, despite high levels of HIV prevention and testing awareness, Human Rights Watch found that for many people who exchange sex for money, drugs, or life necessities in New Orleans, the ability to protect themselves from HIV remains out of reach. Human Rights Watch identified two substantial barriers to HIV prevention in New Orleans: 1) lack of access to clean syringes for injection drug users; and 2) the harassment by police of individuals for carrying condoms—in effect, the criminalization of condom possession.
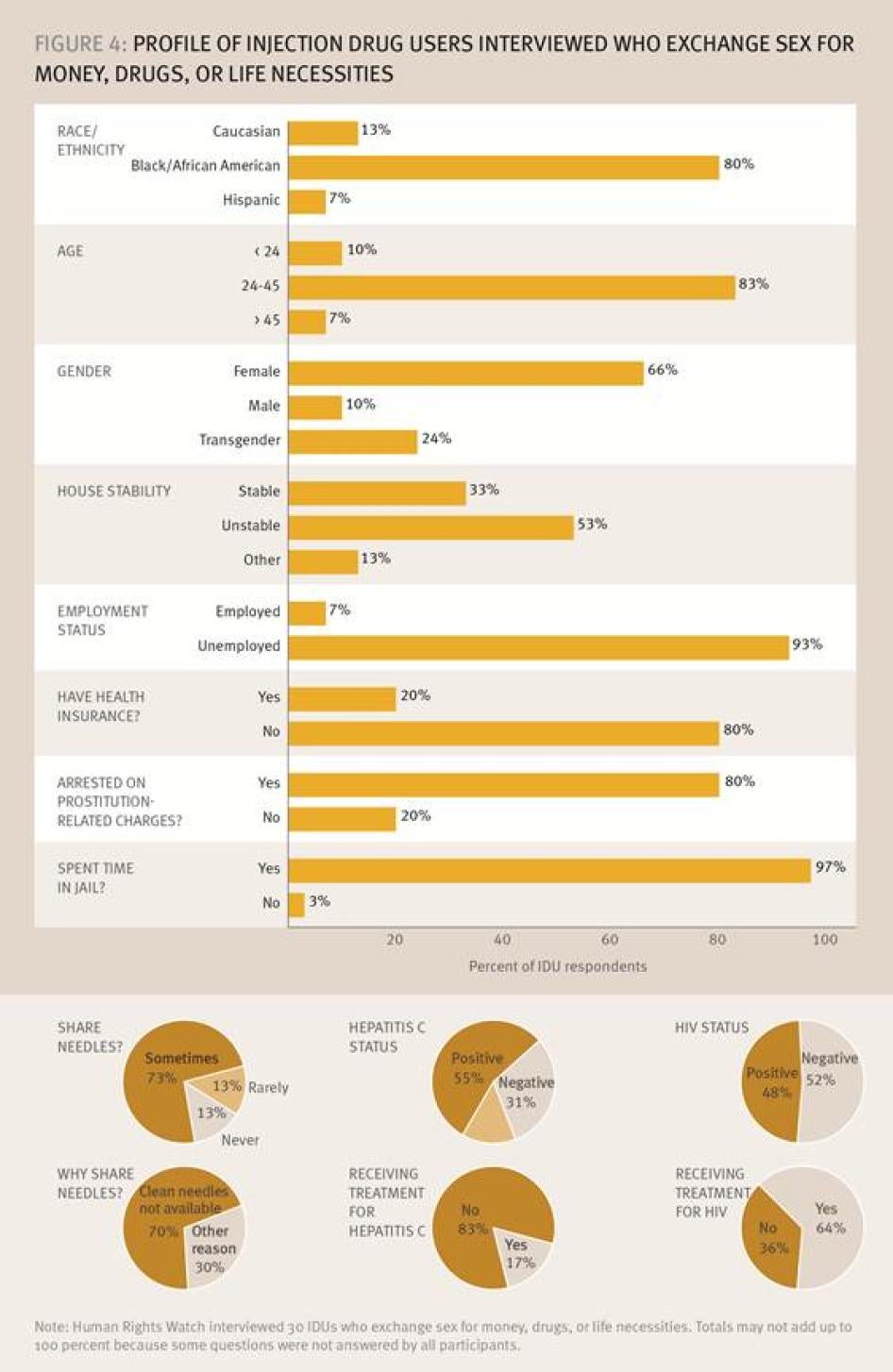
The lack of clean needles in New Orleans has a devastating effect on the ability of people who inject drugs to protect themselves from HIV and hepatitis C. The 30 injection drug users interviewed who exchange sex for money, drugs, or life necessities ranged in age from 19 to 55. Their survey responses reveal that these individuals live a fragile existence: 53 percent live in housing situations that they consider to be “unstable”; 93 percent are unemployed; 80 percent have no health insurance; 80 percent had been arrested for prostitution; and, 96 percent had spent time in jail. Only 13 percent reported “never” sharing needles, and when asked the reason that needles were shared, 70 percent reported that “clean needles were not available.” Some declined to answer, but nearly half of the injection drug users who answered the question reported that they have HIV, and 53 percent reported having hepatitis C.[126]
Of those who reported living with HIV, 64 percent of people injecting drugs were in treatment. In contrast, only 17 percent of individuals who said that they had hepatitis C reported receiving treatment. Figure 4 provides a summary of their answers to selected questions about housing, incarceration and other issues.
The stark reality is that the public health system has utterly failed to protect these individuals from two extremely serious but fully preventable diseases. Camilla, an injection drug user who has lived in New Orleans for 17 years, told Human Rights Watch she has seen people buy dirty needles for five dollars due to shortages in the city. She said that, “I don’t understand why there is no harm reduction here, no clean needles for people. It is such a simple thing. Why should people have to suffer?”[127]
Police Harassment for Possession of Condoms
Municipal court records show approximately 300 misdemeanor arrests a year since January 2011 for prostitution, solicitation of prostitution, prostitution loitering, and crimes against nature for compensation.[128] However, Human Rights Watch found that many complaints about police activity involve street harassment that does not necessarily result in arrest. Specifically, individuals reported that police stops for suspected prostitution frequently included the officer associating an individual’s possession of condoms with criminal activity. Human Rights Watch has documented this practice in other major US cities and found that when police comment on, confiscate or threaten arrest based on condom possession as evidence of prostitution; this reduces condom use among sex workers and those perceived to be sex workers.[129] Both the survey results and individual testimonies indicate that this practice and its harmful consequences are a substantial problem in the streets of New Orleans.
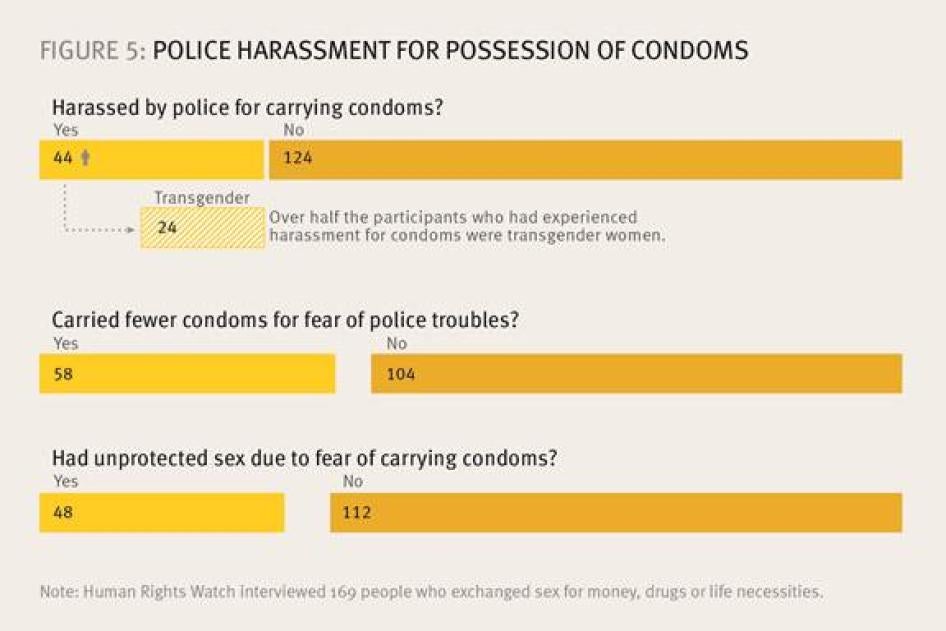
In response to the question “Have you been harassed by police for carrying condoms?”, 44 of 169 participants (26 percent) responded in the affirmative, with 15 reporting that this incident had occurred in the last six months, and one reporting harassment for condoms only two days earlier. Further analysis showed that the practice significantly impacted transgender women, as 24 of the 44 persons who had experienced harassment for condoms were transgender women, 16 were non-transgender women, and three were men (Figure 5).
Juliet, an African-American transgender woman, 31, described the following incident with a police officer, which occurred in August 2011:
He was going through my purse calling me a “thing” and asking me what I needed all those condoms for. He ran my name and luckily that time I didn’t have no attachments so he let me go with a warning. [130]
Anna, a white transgender woman, 35, said that in 2012:
I was driving and I was pulled over and he searched me and found [condoms] and told me I was disgusting and a disgrace to America.
Cleo, a white woman, 36, said that in March 2013:
In the French Quarter I was at [a bar] with a man and the cops asked only the trans women to go outside and they searched us. If we had condoms we got arrested for attempted solicitation.
Barbara, a 26-year-old African-American transgender woman, stated:
I was walking down the street and I was stopped by the police and they searched me for condoms and called me a whore.
According to the Office of the Public Defender, condoms are not used to support prostitution charges in court in Louisiana.[131] But our research found that this police harassment for carrying condoms remains harmful for individuals and for public health. Even one incident can spread quickly by word of mouth and discourage others from carrying condoms for fear of arrest. Fifty-eight of 169 respondents (36 percent) said they have carried fewer condoms than they needed for fear of trouble from the police. One African-American transgender woman said she had not been personally harassed for condom possession but was still fearful because she has “seen the harassment by police happen to others.” Another stated, “I’ve seen other girls being harassed and I learn to be cautious. I hide [condoms] under my wigs.”
In other US cities, some sex workers have reported to Human Rights Watch that their fear of carrying condoms has resulted in unprotected sex with clients. Similarly, in New Orleans, we found that 48 of 169 people surveyed (30 percent) stated that their fear of carrying condoms due to police harassment has resulted in unprotected sex. Selena, a 24-year-old African-American transgender woman, stated:
I’ve seen my friends harassed by police officers while I was on the block trying to earn some money and it made me afraid to carry condoms. … I see them go to jail for it so I know not to do it. Then I try not to let the customer penetrate me without a condom.
Police Profiling, Abuse and Misconduct
Individuals we spoke with indicated that harassment for condoms was often accompanied by other human rights violations including profiling of transgender women for prostitution, verbal abuse, and in some cases sexual misconduct. Sheryl, an African-American transgender woman, 24, said:
I was leaving the drop in clinic when police stopped me, searched my purse and found the condoms I just got from the drop in clinic..asked me was I working because I was arrested for prostitution in the past. They just kept trying to convince me I was working when I was really on my way back to my room.
Frannie, a 26-year-old white transgender woman stated:
In the French Quarter they harassed me and ran my name and found I had sex convictions…. He asked me if I was a transvestite which is crazy because that is very disrespectful. Then he asked to see my purse and he took the condoms from me and said, “What are you doing with all these? Your faggot ass probably got AIDS already. Now get off the streets and don’t let me see you again tonight.”
Nine individuals described specific incidents of alleged sexual misconduct.
Belle, a 17-year-old transgender woman alleged that in April 2013:
In the French Quarter [the police officer] asked what I was doing and I said I was waiting for friends. He got out of his car and asked to see my ID and then he say I looked like a suspect and asked if I had any weapons in my purse. Then he went through my purse and found the condoms then he started asking me how much I charge for a blow job. He said if I wanted to go free I had to give him a blow job because the condoms were reason enough to bring me in so I did it and he let me go.
Jennifer, an 18-year-old African-American transgender woman told Human Rights Watch that in June 2012, “I was made to give oral sex because he figured out I was prostituting. I did it but I felt raped and sad.”
Juanita, a 29-year-old Hispanic woman said:
In December 2012 I was pulled out of a bar by a police officer from New Orleans. He asked me to get into the car. He asked me a lot of questions about me such as how I feel, how I get into this business, if I was interested in quitting with this lifestyle and offered me a payment to practice oral sex on him. I did it and got my money and left.
Individuals were not systematically asked if they had filed a formal complaint in cases of police misconduct. Distrust of the police, however, as well as fear of retaliation was reported by some. Theresa, a 31-year-old transgender woman, told Human Rights Watch:
No I never complained about the police when I was working the street. I have to make a living and see the same cops every night, that would be crazy for me to do that as they be retaliating on me for sure.[132]
Concerns about retaliation by the police were raised in the Consent Decree between the NOPD and the federal government. The decree contains an entire section on new policies and procedures required to ensure that citizen complaints are investigated properly without retaliatory measures.[133]
Human Rights Watch met with Officer Frank Robertson, Public Relations Officer in the New Orleans Police Department and Sgt. Nicole Barbe who acts as a liaison to the LGBT community. Neither said they were aware of any harassment by NOPD officers relating to condom possession, and they expressed concern about the practice from a public health perspective. Sergeant Barbe emphasized the changes that the NOPD were making under new policies for community policing based on non-discrimination and anti-bias. The NOPD now requires a minimum of 40 hours of training per year for both cadets at the police academy and for all officers on new procedures that includes understanding of transgender issues and the consequences of violating the transgender policy, which can include termination. The NOPD has also participated in the city’s Gay Pride parade and other public LGBT festivities in recent years, and according to Barbe the NOPD is “working hard to get on track with the LGBT community.”[134]
Lack of Access to Health Care
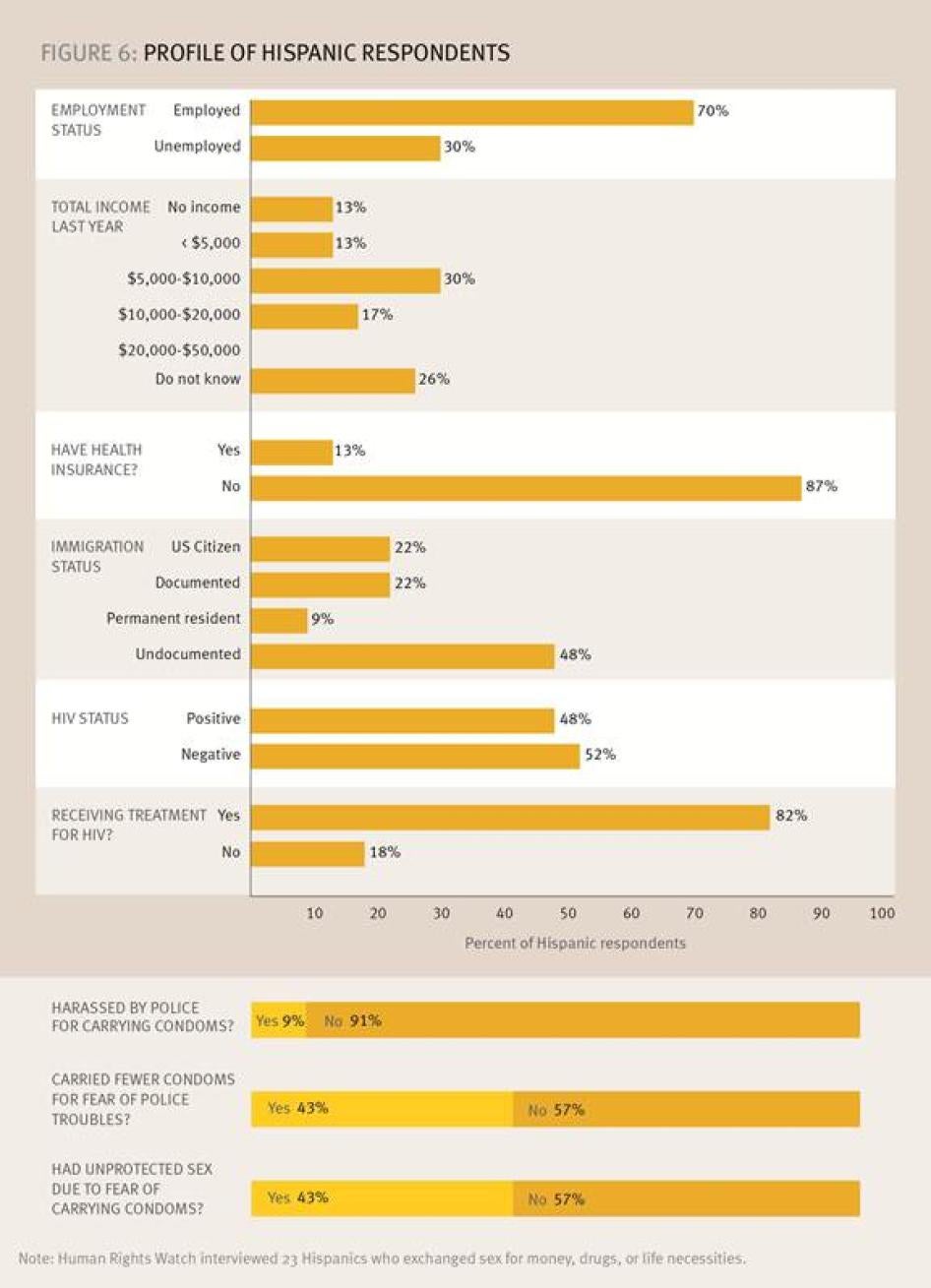
Human Rights Watch found that healthcare coverage for many people who exchange sex for money, drugs, and life necessities in New Orleans was tenuous or non-existent. Fewer than 45 percent of those surveyed reported having health insurance coverage; 85 percent of injection drug users had no health insurance, 48 percent of transgender participants had no coverage, and 87 percent of Hispanic respondents reported no health insurance coverage. Of persons covered by insurance, nearly 30 percent were on Medicaid. Unfortunately, many persons currently covered by health insurance in New Orleans may lose it by the end of 2014, when a special program providing coverage to residents of a four-parish area that includes New Orleans is set to expire.
Under a Medicaid Section 1115 grant waiver program, the Greater New Orleans Community Health Connection expands access to health care for residents of New Orleans by funding community health clinics to serve uninsured individuals who meet income eligibility requirements but are not otherwise eligible for Louisiana Medicaid.[135] After a period of intense advocacy by health officials and advocates, this program has been extended for one year but no commitment has been made to renew this funding after December 31, 2014. If this program had been allowed to expire, an estimated 63,000 people in New Orleans would have lost health insurance coverage.[136] Renewal of the program will depend upon continued commitment and collaboration among city, state and federal health officials.
Barriers to Sustaining HIV Treatment
In recent years, treatment has become the cornerstone of both HIV prevention and care. Public health and HIV experts have increasingly emphasized the importance of early and universal access to anti-retroviral medication not only to improve individual outcomes but to reduce the risk of transmission of the virus to others. The approach characterized as “Treatment as Prevention” has gained traction both in the US and globally based on studies indicating that sufficient suppression of the virus through anti-retroviral therapy can dramatically reduce the possibility of transmission from one person to another and in communities as a whole.[137]
Key to the success of this approach, however, is the ability of the person to sustain a lifetime course of anti-retroviral medication that must be taken on a daily basis. Continuity is particularly important with anti-retroviral drugs as adherence has been strongly associated with suppressing the virus, life expectancy and avoiding resistance to HIV medications.[138] As stated by the US Centers for Disease Control: “The prevention benefit of treatment can only be realized with effective treatment, which requires linkage to and retention in care, and adherence to anti-retroviral therapy.”[139]
Human Rights Watch examined the ability of people who exchange sex for money, drugs, and life necessities in New Orleans to sustain their HIV treatment regimens. Of the 82 participants who were HIV-positive, 70 reported that they were currently receiving treatment for this condition, of which 61 people were taking anti-retroviral drugs. Survey participants were asked, “Have you ever missed a dose of your HIV medication?” Of the 61, 51 (83 percent) reported having missed doses, with 40 (65 percent) stating that they missed doses in the last year. Twenty-five people (40 percent) reported missing doses more than 10 times.
People reported a variety of reasons for missing doses ranging from drug use, jail time, lack of food, lack of housing, and simply forgetting. The responses of the participants when asked why doses were missed provide insight into the multitude of problems people face as they try to adhere to a strict medication regimen on a low income:
“Two months ago in prison didn’t have meds for a month and a week when in jail.”
“Couldn’t think about taking my meds I needed to make some money to live.”
“I got depressed and did not take it. Like 3 doses.”
“I was waiting for Social Security and did not have the money to pay for it. 6 doses.”
“Out of food and money. Food’s expensive.”
“I was unstable. Trying to get money to take care of myself and just didn’t make it to the clinic to get a refill of meds.”
“When I’m smoking or shooting up I don’t take medication.”
“I’m homeless. I leave my meds where I sleep and I can’t remember where I left them.”
“I’d like to be tested again…but I want stable housing before addressing health concerns.”
Two issues emerged from the investigation as primary barriers to maintenance of HIV treatment for people who exchange sex for money, drugs, and life necessities: lack of housing and incarceration.
Lack of Access to Housing as a Barrier to Sustaining HIV Treatment
Human Rights Watch found that people exchanging sex for money, drugs, and life necessities in New Orleans faced severe housing problems, with 30 percent reporting that they were “unstably housed.” Of the 82 HIV-positive participants in the Human Rights Watch survey, 17 (21 percent) were unstably housed. Comments from individuals indicated high levels of concern with housing issues.
Stacy, a 52-year-old African-American woman, said: “I wish the services would get better in NOLA. Especially with housing. You have to wait a long time.”
Alfred, a 36-year-old African-American man, said:
The city doesn’t want to help us. I’ve been homeless since Katrina and it is not until now thanks to UNITY [that I have housing] but that is not even final. …Lack of housing causes many people to hustle out on the street.
The state response to an urgent housing shortage for low-income people has been woefully inadequate. Louisiana has relied almost exclusively on federal aid to address what the director of UNITY calls “the housing crisis for poor people” in New Orleans.[140] The federal government has directed more than $120 billion toward recovery since Katrina, but the majority of the money has gone to emergency relief rather than rebuilding, rental assistance or long-term housing programs.[141]
State support for affordable housing has been meager. The Louisiana State Housing Trust Fund was created by the legislature in 2003 for the purpose of promoting affordable housing for low-income people, but support for the fund has dried up after an initial contribution of $25 million. Other than an additional $31,000 from a state income tax check-off program that expired in 2010, no state funds have been provided to the Trust. The Fund, however, like state housing trusts throughout the country, is well established as an effective mechanism for increasing affordable housing stock. Even with minimal support the Fund has created 35 affordable housing developments with 322 units of new housing.
In dire need of additional financing, the Louisiana Housing Alliance and other advocates in the state have commenced a grass roots campaign to build support for legislative action to “fund the fund.” The many options include a small tax on real estate transactions or allocation of monies received from the Mortgage Settlement Fund. The fund resulted in 2012 from a lawsuit brought by 49 states and the federal government challenging mortgage and foreclosure practices prior to and during the economic recession.[142] Louisiana received approximately $21 million from the mortgage settlement, and the Louisiana Housing Alliance has proposed that some of these dollars be allocated for low-income housing.[143]
Incarceration as a Barrier to Sustaining HIV Treatment
Along with race, gender, poverty and unemployment, the environment of risk for HIV infection and for poorer health outcomes includes a higher likelihood of incarceration. Each year, one in six persons living with HIV spends time in a correctional facility in the United States.[144] In New Orleans, this ratio is likely to be higher, as Louisiana leads the nation in rates of incarceration with a rate 48 percent higher than the national average, while its two major cities lead the nation in rates of new HIV infections.[145] Injection drug users and people who exchange sex are at risk for both HIV and arrest for engaging in these activities. Of the 82 people living with HIV in the Human Rights Watch survey, 62 (75 percent) had spent time in jail or prison. Of injection drug users, 96 percent reported being incarcerated.
Many public health experts characterize correctional settings as places of opportunity to provide HIV testing, counseling, and treatment. The HIV testing program at the Orleans Parish Prison, for example, identified 43 new cases of HIV in 2012, approximately 10 percent of all new cases reported in New Orleans.[146] But the negative impact of incarceration on individual and community health far outweigh any benefit, particularly when one examines the totality of the experience from arrest to release.
For injection drug users, arrest and incarceration has been shown to increase risk of HIV and hepatitis C by interrupting established networks for needle use. Upon release from jail or prison, people who use drugs find new partners, whose HIV status may not be known, for needle-sharing.[147] For this reason, medically supervised safe injection sites in Canada and other countries, where police have agreed to refrain from arrest, have resulted in lower rates of HIV and hepatitis infection among people using drugs at the site.[148] For those who have HIV, arrest can impede access to medical care in multiple ways.
A medical case manager at NO/AIDS Task Force told Human Rights Watch of her client, a transgender woman, who had tested positive for HIV in jail and made an appointment with her to begin treatment:
I have a client now who has been arrested for sex work at least 10 times in the last three years. She has missed 10 appointments with me because she keeps going to jail. I still haven’t met with her and she is still not in care.[149]
As a leading expert on HIV and corrections recently stated, “Of all the life events that knock people out of HIV care, going to jail is one of the biggest disruptors.”[150]
Cycles of arrest for sex work and drug crimes harshly impact communities as well. Human Rights Watch has documented the racial bias underlying drug law enforcement for decades in the United States.[151] In New Orleans, black men over 18 are 53 percent of the city’s population but 84 percent of those incarcerated in the Orleans Parish Prison.[152] The National HIV/AIDS Strategy notes the increased vulnerability of partners, families and minority communities as a whole as a result of relentless incarceration:
High rates of incarceration within certain communities can also be destabilizing. When large numbers of men are incarcerated, the gender imbalance in the communities they leave behind can fuel HIV transmissions by increasing the likelihood that remaining men will have multiple, concurrent relationships with female partners. This in turn increases the likelihood that a single male would transmit HIV to multiple female partners.[153]
Arrest and incarceration frequently causes delay and interruption of HIV treatment. The Orleans Parish Prison is one of the few local jails in the state that has an HIV testing and treatment program.[154] The prison offers HIV tests to every prisoner whose stay is expected to last more than one week. Every prisoner testing positive, regardless of how long their sentence may be, meets with an HIV social worker from NO/AIDS Task Force to facilitate linkage to treatment upon their release. HIV specialists from LSU Medical Center provide treatment services via telemedicine to HIV-positive prisoners.
But delays and treatment interruptions are still a concern. Even in the most efficient law enforcement systems, the period between arrest and official intake at the jail is usually a minimum of 72 hours.[155] At Orleans Parish Prison, inmates expected to “roll out” within days are not offered HIV testing at all, and those already on HIV medication face delays in resuming their regimens. The prison permits family members to bring a prisoner’s medication to the facility, but for those who have no family nearby, the medical team deems it necessary to verify their medications. A fax is sent to local pharmacies to confirm the prisoner’s medication and only upon reply is an order submitted.[156] Newly diagnosed patients must wait to see the HIV specialist before medications are ordered, and reports of how long this process can take varied from two weeks to three months.[157] Dr. Samuel Gore, Medical Director of Orleans Parish Prison, said they try to provide every HIV-positive prisoner with a prescription upon release, but this is not always possible as many releases occur without the knowledge of medical staff. [158]
Transgender Women, Jail and HIV
For transgender women, the cycle of arrest and incarceration can be particularly devastating. Transgender advocates recently released “Injustice at Every Turn,” a survey of nearly 6,500 transgender persons in the United States that depicted a population in crisis.[159] The report documented pervasive discrimination, a poverty level four times higher than the general population, and twice the unemployment rate of non-transgender people, often leaving sex work as the only option for survival. Each of these factors, in addition to vulnerability to HIV and AIDS, was more pronounced in transgender persons of color. Among those surveyed, the self-reported HIV prevalence was four times higher than in the general US population. Rates of HIV among for those who had engaged in sex work were higher than 15 percent. Incarceration rates were seven times higher than the general US population, with one of two African-American transgender persons having spent time in jail or prison.[160]
Human Rights Watch found that many transgender women in New Orleans carried fewer condoms out of fear of arrest. For transgender women, arrest not only threatens already tenuous employment and housing prospects but frequently results in abuse by police and by other prisoners and staff while incarcerated. Human Rights Watch, Amnesty International and others have documented abuse of LGBT people by police and in detention inside the United States.[161] In New Orleans, transgender survey participants reported police profiling them as sex workers and subjecting them to verbal abuse and sexual misconduct. Others cited unsafe conditions while in custody: “In prison the cops don’t give a fuck they see you get your ass kicked and they don’t do anything.”
Rape and other forms of assault remain a major problem in US prisons.[162] The Orleans Parish Prison (OPP) is a dangerous place for anyone and particularly for LGBT individuals. The prison is currently under a Consent Judgment requiring extensive federal oversight of its operations. A federal court in June 2013 found that “OPP fails to adequately protect inmates from harm and serious risk of harm from staff and other inmates.”[163] The court cited the opinions of correctional experts that “OPP is totally dysfunctional in terms of overall security” and that it is “an unsafe facility for both staff and inmates.”[164] Another expert cited by the court stated that Orleans Parish Prison was “likely the worst large city jail in the United States…plagued by suicides and other in-custody deaths, rapes and other sexual assaults, stabbings and severe beatings.”[165]
Since 2011, the organization BreakOUT! has sought to end abuses in the criminal justice system against LGBT youth of color in New Orleans, with a particular emphasis on protecting the rights of transgender women. BreakOUT! was at the forefront of the successful campaign for the New Orleans Police Department policy on interaction between police and members of the transgender community, and is a member of the community advisory board that monitors police behavior. Wesley Ware, the director of Breakout!, told Human Rights Watch that young transgender women working with BreakOUT! were frequently arrested for prostitution, solicitation and “crimes against nature.” Ware submitted testimonies from BreakOUT! members in 2011 to the federal commission for the Prisoner Rape Elimination Act about high levels of violence experienced by LGBT persons at Orleans Parish Prison.[166] The Prison Rape Elimination Act applies to all state and municipal detention facilities in the US, and establishes procedural requirements intended to ensure the protection of LGBT individuals in custody. Among other provisions, the Act requires screening for vulnerability to violence, housing classification decisions to be made on a case-by-case basis, and prohibits segregation of LGBT prisoners unless such action is pursuant to a court order.[167]
Ware told Human Rights Watch:
One transgender woman [in custody] was charged with attempt to escape when she ran from a prisoner who was trying to rape her. Another had bones broken when she refused to give a prisoner oral sex. OPP is a nightmare for them.[168]
HIV and the Hispanic Community in New Orleans
Since Hurricane Katrina, the Hispanic population in Louisiana increased by 44 percent with many Hispanic men moving to New Orleans to seek construction jobs as the city began to rebuild.[169] According to public health officials, HIV case rates are not disproportionate to the size of the population, but the reliability of this data is uncertain due to a small and rapidly fluctuating population.[170] Poor health outcomes following an HIV diagnosis, however, are well documented. Hispanics are one of the groups most likely to develop AIDS within six months of an HIV test, indicating that many are not tested until late in the disease. In New Orleans, 41 percent of Hispanics with HIV are not in treatment.[171]
Access to health care is problematic. Federal law bars undocumented immigrants from being eligible for Medicaid, and imposes a five-year waiting period for legal immigrants to apply for the program.[172] In Louisiana, most Hispanic people rely on hospital emergency rooms for their health care, but some may not qualify for free services. According to advocates, many avoid health care altogether because a bill from the hospital means the government might try to track you, or someone living with you, down.[173]
Human Rights Watch survey participants included 23 Hispanics who exchanged sex for money, drugs, or life necessities. Table 6 illustrates key results, showing that 11 were undocumented; six were employed, with annual income ranging from zero to $20,000 dollars; 20 had no insurance. Of the 23 Hispanic survey participants, 11 reported having HIV, and of these, 9 were receiving treatment.
Human Rights Watch has documented the harsh impact of police interference with condom possession on sex workers who have immigrated to the United States.[174] Immigrants, particularly those who are undocumented, have a heightened fear of arrest because any contact with the police can lead to deportation if they are undocumented. But even those who are documented harbor fear of the police, since prostitution is a deportable offense.[175]Hispanic participants in the Human Rights Watch survey indicated that fear of police activity reduced their willingness to carry condoms. Only two participants reported having been harassed themselves, but nine said they carried fewer condoms for fear of police interference, and all nine said that fear of carrying condoms due to police had resulted in unprotected sex.
Edgar, a 25-year-old Hispanic man, stated in Spanish, “I think it is unfair that cops would arrest someone for carrying condoms, that is why I sometimes have unprotected sex.”[176]
International Human Rights Standards
Right to an Adequate Standard of Living
In the US South, socio-economic conditions combine with harmful state laws and policies that undermine human rights and create an environment in which the risk of acquiring, transmitting, and dying of HIV is higher than any region in the country.[177] This deadly combination takes an especially devastating toll on minority communities, a crisis that federal, state and city governments are obligated under international law to address.[178]
Under principles derived from the Universal Declaration of Human Rights, which is considered broadly reflective of customary international law, everyone has the right to a standard of living adequate for the health and well-being of one’s self and one’s family, including food, clothing, housing, medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond his control.[179] The International Covenant on Economic, Social and Cultural Rights (ICESCR) establishes that medical care, necessary social services and housing are integral components of human dignity, and are part of the claims all people have to their right to an adequate standard of living.[180] The United States has signed, but not ratified, the ICESCR; as a signatory, it must refrain from taking steps that undermine the intent and purpose of the instrument.[181]
An important component of the realization of the right to health for all people is housing.[182] Upholding the right to housing is particularly urgent for people living with HIV, a fact acknowledged by both the US government and the state of Louisiana.[183] Medical care should be accessible, available, and of adequate quality, a goal that remains out of reach for one of three people living with HIV in Louisiana.[184]
Right to Be Free From Racial Discrimination
The federal, state, and local governments in the United States are obligated to address all forms of racial discrimination, including the disparities that characterize the domestic HIV epidemic. This duty is fundamental to upholding international human rights law, including the ICCPR[185] and International Convention on the Elimination of all forms of Racial Discrimination (ICERD).[186] ICERD, to which the United States is a party, requires governments, when the circumstances warrant, to take “special and concrete measures” to ensure the development and protection of racial groups “for the purpose of guaranteeing them the full and equal enjoyment of human rights and fundamental freedoms.”[187]
Under ICERD, the US undertakes to eliminate racial discrimination and guarantee to everyone, without distinction, the right to public health.[188] The treaty obligates governments to address not only intentional racial discrimination but laws, policies and practices that result in disparate racial impact.[189] The UN Committee on Economic, Social and Cultural Rights, the international expert body responsible for interpreting the ICERD, has expressed its concern that the United States lacks appropriate mechanisms for implementation of the treaty at the state level.[190]
Louisiana epitomizes these concerns. The state’s failure to reduce significant socio-economic and health disparities that impact minority communities has placed an unacceptably high burden on the state’s African-American population. In Louisiana, blacks are many times more likely than whites to be homeless, uninsured and living with HIV, disparities that the state has failed to adequately address. Minorities in Louisiana, for example, are much more likely to be uninsured, as 30 percent of African-Americans and 51 percent of Hispanics are without insurance, compared to 18 percent of whites.[191] Blacks are 32 percent of the state population, but they comprise 73 percent of newly diagnosed HIV cases and 76 percent of new AIDS cases.[192] The HIV diagnosis rate among African-American women is 16 times higher than the rate among white women.[193] In New Orleans, blacks are homeless at a rate more than double that of whites.[194] The Louisiana state government’s refusal to expand Medicaid or to continue support for its housing trust fund has disparate impact on minorities and as such is inconsistent with its obligations under international law.
Right to Syringes, Condoms and Other Means of HIV Prevention
HIV is a potentially fatal disease, and other sexually transmitted diseases increase the likelihood of HIV infection. Police interference with the ability to access means of HIV prevention, whether in the form of syringes or condoms, impedes the rights to life and to health and is incompatible with human rights standards. The International Covenant on Civil and Political Rights (ICCPR), to which the United States is a party, guarantees to every person the right to life, a fundamental right that is implicated in any policy that interferes with the prevention of HIV.[195] Indeed, the treaty has been interpreted to require states to take positive steps to curb epidemics and other threats to the public health.[196]
The right to access condoms and related HIV prevention services is also an essential part of the human right to the highest attainable standard of health. The ICESCR obligates state parties to take steps “necessary for… the prevention, treatment and control of epidemic…diseases,” including HIV. The right to health also requires governments to refrain from acts that would harm or interfere with the protection of health. Laws and policies that “are likely to result in bodily harm, unnecessary morbidity and preventable mortality” are considered violations of the right to the highest attainable standard of health.[197]
Both syringe access programs and harm reduction information are essential components of comprehensive HIV prevention, treatment, and care package for people who inject drugs, as defined by the World Health Organization, United Nations Office on Drugs and Crime, and Joint United Nations Programme on HIV/AIDS. [198] State policies that criminalize syringe possession and even trace amounts of illegal substances impede the right to health by forcing harm reduction programs to operate underground and denying individuals the right to disease prevention and medical services.
International law also protects the right of all women to control their reproductive and sexual health. The Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), which the US has signed but not ratified, sets out the right of women to make informed decisions about safe and reliable contraceptive measures, to access family planning information, education and “the means to enable them to exercise these rights.”[199] The International Guidelines on HIV and Human Rights, an authoritative interpretation of human rights law applicable to HIV, address the discrimination and denial of equal access to HIV prevention services faced by marginalized populations, including sex workers and people who inject drugs.[200]
Law enforcement agencies charged with enforcing anti-prostitution laws must act consistently with international human rights obligations. This includes respecting the right to health, an element of public safety that is the province of the police.[201] The United Nations Joint Programme on HIV/AIDS (UNAIDS), noting that sex workers frequently suffer human rights abuses due to the legal status of their work, recommends:
With regard to adult sex work that involves no victimization, criminal law should be reviewed with the aim of decriminalizing, then legally regulating occupational health and safety conditions to protect sex workers and their clients, including support for safe sex during work. Criminal law should not impede provision of HIV prevention and care services to sex workers and their clients.[202]
The UN Guidance Note on HIV and Sex Work refers to the vulnerability to HIV infection among sex workers, which “reflects the failure to adequately respond to their human rights and public health needs.”[203] The UN Guidance Note states:
Condoms, both male and female, are the single most effective available technology to reduce the sexual transmission of HIV and other sexually transmitted diseases. Condoms must be readily available for sex workers and their clients, either free or low cost, and conform to global quality standards. Harassment by law enforcement officers reduces the ability of sex workers to negotiate condom use; governments and service providers should address such factors to maximize the impact of condom programming focused on sex work.[204]
Right to Be Free From Gender Discrimination
In New Orleans, transgender women have been frequent targets of police interference with the right to carry condoms to protect themselves from HIV and other sexually transmitted diseases. Louisiana’s “crimes against nature” laws promote a homophobic and discriminatory environment that invites human rights abuses. Profiling of transgender women as engaging in prostitution is prohibited by internal policy of the New Orleans Police Department, but the policy was recently announced and has yet to have an impact on this pervasive practice on city streets. New Orleans’ broadly worded loitering laws, by permitting police stops based on a person’s past involvement with prostitution, increase the vulnerability of transgender women to a harmful cycle of arrest and detention.
The Yogyakarta Principles, standards endorsed by independent legal experts from 25 countries, apply existing international human rights law to sexual orientation and gender identity. The principles call for an end to laws that promote profiling and other inequality before the law:
States shall take all necessary legislative, administrative and other measures to ensure that sexual orientation or gender identity may under no circumstances be the basis for arrest and detention, including the elimination of vaguely worded criminal law provisions that invite discriminatory application or otherwise provide scope for arrests based on prejudice.[205]
Right to Be Free from Cruel, Inhuman and Degrading Treatment
People who exchange sex for money, drugs, or life necessities, particularly transgender women, described multiple instances of police conduct and abuse in detention that constitutes cruel, inhuman and degrading treatment. These actions contravene both domestic and international law, including the federal orders in effect for both the New Orleans Police Department and the Orleans Parish Prison.[206] The federal Prison Rape Elimination Act also establishes procedural requirements intended to ensure the safety of LGBT individuals in custody.[207] International law to which the US is party, notably the ICCPR and the Convention against Torture and Other Cruel, Inhuman and Degrading Treatment, prohibit a range of mistreatment in police custody and prisons.[208] This includes abusive and corrupt police practices such as verbal harassment, humiliation, and demand of sex in exchange for leniency.
Declarations adopted by the UN General Assembly, such as the UN Code of Conduct for Law Enforcement Officials, the UN Body of Principles for the Protection of Persons Under Detention, and the UN Standard Minimum Rules for the Treatment of Prisoners have also established standards for police behavior. These UN declarations on policing provide that law enforcement officials should treat all persons with compassion and respect for their dignity, and should not inflict, instigate or tolerate any act of cruel, inhuman or degrading treatment or punishment.[209] Effective mechanisms should be established to ensure the internal discipline and supervision of law enforcement officials.[210] Rape and sexual assault in detention perpetrated or permitted by state officials may amount to torture. [211] The UN Special Rapporteur on Torture has specifically condemned discrimination and violence directed against sexual minorities in detention and the lack of police accountability that surrounds these offenses. [212]
In March 2011, as part of its Universal Periodic Review before the UN Human Rights Council, the US accepted a recommendation that the government “ensure access to public services paying attention to the special vulnerability of sexual workers to violence and human rights abuses," stating, “We agree that no one should face discrimination in access to public services or violence based on sexual orientation or their status as a person in prostitution.”[213] This was the first public recognition by the US of its obligation to respect the human rights of sex workers. Unfortunately, the personal accounts of people who exchange sex for money, drugs, or life necessities in New Orleans confirm that there is much work to be done before these rights are realized.
Acknowledgements
This report was written by Megan McLemore, senior researcher in the Health and Human Rights Division. The report was reviewed at Human Rights Watch by Joseph Amon, director of the Health and Human Rights Division, Graeme Reid, director of the LGBT Program, Alison Parker, director of the US Program, and Meghan Rhoad, researcher in the Women’s Rights Division, James Ross, legal and policy director, and Babatunde Olugboji, deputy program director. Research assistance was provided by Margaret Wurth, research assistant with Human Rights Watch; Laura Iris Mattes and Chelsea Edwards, interns in Human RightsWatch’s New York office; and research and logistical assistance was provided by Freddy Gonzales, intern in New Orleans. Production assistance was provided by Jennifer Pierre, associate, Grace Choi, publications director, Kathy Mills, publication specialist, Fitzroy Hepkins, administrative manager, and Amanda Bailly, multimedia producer.
Human Rights Watch gratefully acknowledges the invaluable assistance of individuals and organizations who made this report possible, including Deon Haywood, Zina Mitchell and the staff of Women with a Vision, Wes Ware and the members of BreakOUT!, Tela Love, Fran Lawless, Vatsana Chantala, Brandi Bowen, Noel Twilbeck, Narquis Barak, Megan McIntyre, Megan Coleman-Watkin and many staff members at NO/AIDS Task Force, Virginia Ryan, Stella Cziment, Jee Park, John Flemming and Claire Gutekanst at the Orleans Public Defenders, Oscar Salinas, Jane and Marika from SWOP New Orleans, all of the peer interviewers, and many others. Human Rights Watch extends a special note of thanks to Russell Brewer, Snigdha Mukherjee and Scott Hunter of the Louisiana Public Health Institute for their assistance with data analysis.
Most of all, Human Rights Watch thanks the courageous people who shared their experiences for publication in this report.
[1] All Human Rights Watch survey results are available in the files of Human Rights Watch. Total may not add up to 100 percent because of rounding. Note: only 168 participants responded to the questions set forth in Figure 1.
[2] Joint United Nations Programme on HIV/AIDS (UNAIDS), “Guidance Note on HIV and Sex Work,” 2012, http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2009/JC2306_UNAIDS-guidance-note-HIV-sex-work_en.pdf (accessed September 10, 2013); Samuel M. Jenness et al., “Patterns of Exchange Sex and HIV Infection in High-Risk Heterosexual Men and Women,” Journal of Urban Health, vol. 88, no. 2 (2011), pp.329-341; Stefan Baral et al., “Burden of HIV Among Female Sex Workers in Middle and Low Income Countries: a Systematic Review and Meta-Analysis,” Lancet, vol. 12, issue 7 (2012), pp. 538-49.
[3] US Centers for Disease Control (CDC), “Establishing a Holistic Framework to Reduce Inequities in HIV, Viral Hepatitis, STDs and Tuberculosis in the United States,” 2010, http://www.cdc.gov/socialdeterminants/docs/sdh-white-paper-2010.pdf (accessed September 10, 2013); Irene Doherty et al., “Social Determinants of HIV Infection in the Deep South,” American Journal of Public Health, vol. 97, issue 3 (2007), p. 391; Kevin Fenton and Dean Hazel , “Addressing Social Determinants of Health In The Prevention and Control Of HIV/AIDS, Viral Hepatitis, Sexually Transmitted Infections and Tuberculosis,” Public Health Reports 25(2010), accessed September 10, 2013, http://www.publichealthreports.org/issueopen.cfm?articleID=2475, p.1.
[4] The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf (accessed September 10, 2013), p. 35.
[5] Joint United Nations Programme on HIV/AIDS (UNAIDS), “Guidance Note on HIV and Sex Work,” 2012, http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2009/JC2306_UNAIDS-guidance-note-HIV-sex-work_en.pdf; Global Commission on HIV and the Law, “Risks, Rights and Health,” July 2012, http://www.hivlawcommission.org/resources/report/FinalReport-Risks,Rights&Health-EN.pdf (accessed September 10, 2013); Global Commission on Drug Policy, “War on Drugs: Report of the Global Commission on Drug Policy,” June 2011, http://www.opensocietyfoundations.org/sites/default/files/global-commission-report-english-20110624.pdf (accessed September 10, 2013).
[6] See, e.g. Human Rights Watch, Sex Workers at Risk: Condoms as Evidence of Prostitution in Four US Cities, July 2012 http://www.hrw.org/reports/2012/07/19/sex-workers-risk-0; Human Rights Watch, Off the Streets: Arbitrary Detention and Other Abuses against Sex Workers in Cambodia, July 2010, http://www.hrw.org/reports/2010/07/19/streets; Human Rights Watch, Not Worth a Penny: Human Rights Abuses Against Transgender People in Honduras, May 2009, http://www.hrw.org/reports/2009/05/29/not-worth-penny-0; Human Rights Watch, Targeting Blacks: Drug Law Enforcement and Race in the United States, May 2008, http://www.hrw.org/sites/default/files/reports/us0508_1.pdf; Human Rights Watch, Skin on the Cable: The Illegal Arrest, Arbitrary Detention and Torture of People Who Use Drugs in Cambodia, January 2010, http://www.hrw.org/reports/2010/01/25/skin-cable-0.
[7] CDC, “HIV Surveillance Report: Diagnoses of HIV Infection in the United States and Dependent Areas,” 2011,” vol. 23, February 2013.
[8] Louisiana Department of Health and Hospitals, “Louisiana HIV/AIDS Quarterly Report,” March 2012, http://www.dhh.louisiana.gov/assets/oph/Center-PHCH/LouisianaHIVFirstQuarter2012.pdf (accessed September 10, 2013). This report gave the figure as 18,864 people.
[9] Louisiana Department of Health and Hospitals, “2010 STD/HIV Program Report,” 2010, http://new.dhh.louisiana.gov/assets/oph/HIVSTD/hiv-aids/2010/2010SHPProgramReportFinal.pdf (accessed September 10, 2013). Louisiana has adopted the federal definition of HIV-related medical care as at least one CD4 or viral load test in a twelve month period. State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, June 2012, p. 30. On file with Human Rights Watch.
[10] Kaiser State Health Facts, “Age-Adjusted Death Rate for HIV Disease,” 2010, http://kff.org/hivaids/state-indicator/hiv-death-rate/ (accessed August 15, 2013).
[11] Louisiana Department of Health and Hospitals, “Louisiana HIV/AIDS Quarterly Report,” March 2012, http://www.dhh.louisiana.gov/assets/oph/Center-PHCH/LouisianaHIVFirstQuarter2012.pdf.
[12] State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, June 2012.
[13] High-risk heterosexual contact is defined as sex with persons known to have, or to be at high risk for, HIV infection (e.g. injection drug users). Louisiana Department of Health and Hospitals, “2010 STD/HIV Program Report,” 2010, http://new.dhh.louisiana.gov/assets/oph/HIVSTD/hiv-aids/2010/2010SHPProgramReportFinal.pdf, pp. 17-24.
[14] Ibid., p. 52.
[15] CDC, “HIV Surveillance Report: Diagnoses of HIV Infection in the United States and Dependent Areas, 2011,” February 2013, http://www.cdc.gov/hiv/library/reports/surveillance/2011/surveillance_Report_vol_23.html (accessed September 10, 2013).
[16] Ibid.
[17] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf (accessed September 10, 2013).
[18] Ibid.; State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 56; Human Rights Watch interview with Kira Radtke Friedrich, care and services manager, Louisiana Office of Public Health, STD/HIV Program, New Orleans, March 27, 2013.
[19] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf.
[20] Ibid.
[21] Kaiser Family Foundation, “State Health Facts, Distribution of Total Population by Federal Poverty Level, 2010-2011,” undated, http://quickfacts.census.gov/qfd/states/22000.html (accessed August 16, 2013). The federal poverty level in 2011 as set by the U.S. Department of Health and Human Services (DHHS) was $23, 450 per year for a family of four. See, DHHS “Poverty Guidelines,” undated, http://aspe.hhs.gov/poverty/faq.cfm (accessed August 16, 2013).
[22] Kaiser Family Foundation, “State Health Facts, Poverty Rates by Race/Ethnicity 2010-2011,” undated, http://kff.org/other/state-indicator/poverty-rate-by-raceethnicity/(accessed August 16, 2013).
[23] Kaiser Family Foundation, “State Health Facts, Health Insurance Coverage of the Total Population 2010-2011,” undated, http://kff.org/other/state-indicator/total-population/ (accessed August 16, 2013).
[24] Greater New Orleans Community Data Center, “Assets and Opportunity Profile,” August 2012, https://gnocdc.s3.amazonaws.com/reports/GNOCDC_Assets&OpportunityProfile.pdf (accessed September 10,2013).
[25] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf, p. 55.
[26] US Census Bureau, “State and City Quick Facts New Orleans, Louisiana,” undated, http://quickfacts.census.gov/qfd/states/22000.html (accessed September 10,2013).
[27] US Census Bureau, “American Fact Finder, Selected Housing Characteristics New Orleans, Louisiana 2007-2011.” On file with Human Rights Watch.
[28] National Alliance to End Homelessness, “The State of Homelessness in America 2012,” January 2012, http://www.endhomelessness.org/library/entry/the-state-of-homelessness-in-america-2012 (accessed September 10, 2013).
[29] Greater New Orleans Community Data Center, “New Orleans Index at Eight,” August 2013, https://gnocdc.s3.amazonaws.com/reports/GNOCDC_NewOrleansIndexAtEight.pdf (accessed September 10, 2013), p. 28.
[30] Petrice Sams-Abiodun and Gregory Rattler, Recognizing the Underutilized Economic Potential of Black Men in New Orleans (New Orleans: Lindy Boggs National Center for Community Literacy, 2013).
[31] Institute for Women’s Policy Research, “Women in New Orleans: Race, Poverty and Hurricane Katrina,” August 2010, http://www.iwpr.org/publications/pubs/women-in-new-orleans-race-poverty-and-hurricane-katrina (accessed September 10, 2013).
[32]CDC, “HIV in the United States: at a Glance,” undated, http://www.cdc.gov/hiv/resources/factsheets/us.htm (accessed October 22, 2013.)
[33] UN Committee on Economic, Social and Cultural Rights, “Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights,” General Comment No. 14, The Right to the Highest Attainable Standard of Health. E/C.12/2000/4 (2000); International Harm Reduction Association, “Global State of Harm Reduction 2008: Mapping the Response to Drug-Related HIV and Hepatitis C Epidemics,” 2008, http://www.ihra.net/files/2010/06/16/GSHRFullReport1.pdf (accessed September 10, 2013).
[34] WHO/UNAIDS/UNODC, “Policy Brief: Provision of Sterile Injecting Equipment to Reduce Transmission of HIV,” 2004, http://www.unodc.org/documents/hiv-aids/provision%20of%20sterile%20injecting%20equipment.pdf (accessed September 10, 2013); Susan Hurley et al., “Effectiveness of Needle Exchange Programmes for the Prevention of HIV Infection,” The Lancet, vol. 349 (1997); Scott Burris, “Policy Brief on Needle Exchange,” January 2009, http://www.santacruzhealth.org/pdf/RWJ_SEP%20Policy%20Brief_2010.pdf (accessed September 10, 2013); The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf, p. 6.
[35] CDC, “Syringe Exchange Programs,” December 2005, http://www.cdc.gov/idu/facts/aed_idu_syr.pdf (accessed September 10, 2013).
[36] Amfar Foundation for AIDS Research, “Federal Funding for Syringe Services Programs: Saving Money, Promoting Public Safety and Improving Public Health,” January 2013, http://www.amfar.org/uploadedFiles/_amfarorg/Articles/On_The_Hill/2013/issue-brief-federal-funding-for-syringe-service-programs.pdf (accessed September 10, 2013).
[37] Amfar Foundation for AIDS Research, “Public Safety, Law Enforcement and Syringe Exchange Fact Sheet,” March 2013, http://www.amfar.org/uploadedFiles/_amfarorg/Articles/On_The_Hill/2013/fact%20sheet%20Syringe%20Exchange%20031913.pdf (accessed September 10, 2013); Samuel L. Groseclose et al., “Impact of Increased Access to Needles and Syringes on Practices of Injecting Drug users and Police Officers- Connecticut, 1992-1993,” Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, vol. 10, no. 1 (1995), pp. 82-89; Susan W. McCampbell and Paula N. Rubin, “A Needle Exchange Program: What’s in it for Police?” Police Executive Research Forum, vol. 14, no. 10 (2000). A recent survey of law enforcement officers in North Carolina found that nearly one of ten had experienced needle stick injuries, North Carolina Harm Reduction Coalition, “North Carolina Law Enforcement Attitudes Toward Syringe Decriminalization, 2012,”undated, http://www.nchrc.org/law-enforcement/north-carolina-law-enforcement-attitudes-towards-syringe-decriminalization/ (accessed August 15,2013). In 2013 the North Carolina legislature removed syringes from the state’s drug paraphernalia law. HB 850, signed into law June 19, 2013.
[38]The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf, p. 6.
[39] New York State Department of Health AIDS Institute, “New York State HIV/AIDS Epidemiologic Profile 2012,” May 2013,
http://www.health.ny.gov/diseases/aids/statistics/epi/docs/2012_epidemiologic_profile.pdf (accessed September 10, 2013).
[40] Video interview with Dr. Don Des Jarlais at the International AIDS Conference 2012, Washington, DC, July 18, 2012, http://www.drugabuse.gov/about-nida/organization/offices/office-nida-director-od/aids-research-program-arp/past-meeting-reports-presentations/video-interviews-international-aids-0 (accessed September 10, 2013).
[41] Louisiana Department of Health and Hospitals, “Louisiana HIV/AIDS Surveillance Quarterly Report: Fourth Quarter 2012,” December 31, 2012, http://dhh.louisiana.gov/assets/oph/HIVSTD/hiv-aids/2012/FOURTHQuarter2012.pdf. (accessed September 10, 2013).
[42]State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 21; Sudip Chatterjee et al., “Changes in the Prevalence of Injection Drug Use Among Adolescents and Young Adults in Large US Metropolitan Areas,” AIDS Behavior, vol. 15, no. 7 (2011), pp. 1570-1578.
[43] State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 46.
[44] Ibid, pp. 24 and 26.
[45] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf, p.24.
[46] State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 47.
[47] Louisiana Revised Statutes 40: 1021, 1023, et seq.
[48] Louisiana Revised Statutes 40: 1033.
[49] Louisiana Administrative Code 46: LIII: 2509.
[50]Human Rights Watch email communication with Drew Davenport, SAP Director, NO/AIDS Task Force, August 21. 2013.
[51] Human Rights Watch interview with Elizabeth Jones, Senior Program Coordinator, Tulane Drop-In Center, New Orleans, April 24, 2013.
[52] Human Rights Watch interview with Zoe E., New Orleans, February 27, 2013.
[53] Reports cited include charges under La Rev Stat 40:1023(A) and(C) and New Orleans Municipal Criminal Code 102: 111-113.
[54] Human Rights Watch telephone interview with Virginia Ryan, Client Services Coordinator, Orleans Public Defenders, New Orleans, August 20, 2013.
[55] World Health Organization, “Technical Guide for Countries to Set Targets for Universal Access to HIV Prevention and Care for Injecting Drug Users,” 2009, http://www.who.int/hiv/pub/idu/idu_target_setting_guide.pdf (accessed September 10, 2013).
[56] Data request, Louisiana Office of Public Health STD/HIV Program, National HIV Behavioral Surveillance IDU32012. All NHBS documents cited in this report are on file with Human Rights Watch.
[57] Human Rights Watch telephone interview with Dr. MarkAlain Déry, Assistant Professor of Clinical Medicine, Tulane University, New Orleans, August 16, 2013.
[58] Data request, Louisiana Office of Public Health STD/HIV Program, National HIV Behavioral Surveillance IDU32012.
[59]Ibid.
[60] Ibid.
[61] National HIV Behavioral Surveillance, IDU3 Secondary Data Report, Louisiana 2012, Core Document, p. 20. On file with Human Rights Watch.
[62] Federal Omnibus Appropriations Bill FY 2012, signed into law by President Obama December 23, 2011; Human Rights Watch interview with Jean Redmann, Director of Prevention, NO/AIDS Task Force, New Orleans, July 30, 2013.
[63] Human Rights Watch interview with Jean Redmann, Director of Prevention, NO/AIDS Task Force, New Orleans, July 30, 2013.
[64] Human Rights Watch interview with Cyndee Clay, Executive Director, HIPS, New Orleans, September 9, 2013. HIPS is a Washington DC-based NGO and a member of the Working Group.
[65] Human Rights Watch interview with Deon Haywood, Executive Director of Women with a Vision, New Orleans, September 8, 2013.
[66] Louisiana Revised Statute 14:82(A)(1).
[67] Louisiana Revised Statute 14:82(A)(2).
[68] New Orleans Municipal Criminal Code 54:252. For example, courts have voided loitering for prostitution statutes in Florida, see Wyche v. State of Florida, 619 So.2d 231 (1993).
[69] Louisiana Revised Statutes 14:89(A)(1).
[70] Louisiana Revised Statutes 14:89(A)(2).
[71]Louisiana v. Smith, 766 So. 2d 501, 504 (LA 2000).
[72] Lawrence v. Texas, 539 US 558 (2003).
[73]Louisiana v.Thomas, 891 So. 2d 1233,1237 (LA 2005).
[74] Ibid.
[75]Doe v. Jindal, 851 F. Supp. 2d 995 (E.D. LA 2012).
[76] Human Rights Watch email communication with Andrea J. Ritchie, Esq., co-counsel for the Doe. v. Jindal litigation, November 3, 2013.
[77] Louisiana Revised Statute 14:89 (C) and 14.82.1.
[78] Jim Mustian, “Gays in Baton Rouge Arrested Under Invalid Sodomy Law,” The Advocate, July 28, 2013, http://theadvocate.com/news/police/6580728-123/gays-in-baton-rouge-arrested (accessed September 10, 2013).
[79] New Orleans Municipal Court data, January 2011-June 2013.On file with Human Rights Watch.
[80] Human Rights Watch interview with Deon Haywood, Executive Director, Women with a Vision, February 24, 2013.
[81] United States Department of Justice, “Investigation of the New Orleans Police Department,” March 16, 2011, http://www.justice.gov/crt/about/spl/nopd_report.pdf, pg. v (accessed September 10, 2013).
[82] Ibid.
[83]United States of America v. City of New Orleans, 2:12-CV-01924-SM-JCW (E.D. LA), Consent Decree filed 7/24/12.
[84] New Orleans Police Department “Policy 402: Discriminatory Policing/Bias- Based Profiling,” adopted June 30, 2013, http://www.youthbreakout.org/sites/g/files/g189161/f/201307/FINAL%20ADOPTED%20Policy%20402%20-%20PR402%20-%20Discriminatory%20Policing%20-%20Racial%20Bias-Based%20Profiling.pdf (accessed September 10, 2013).
[85]Ibid, 402-4.
[86] United Health Foundation, “America’s Health Rankings,” 2012, http://www.americashealthrankings.org/Rankings (accessed September 10, 2013).
[87] Kaiser Family Foundation, “State Health Facts, Uninsured Rates by Race/Ethnicity 2010-2011,” undated http://kff.org/uninsured/state-indicator/rate-by-raceethnicity/ (accessed August 23, 2013).
[88] Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, p. 8; Adam Nossiter, “For Louisiana, Bon Temps Proved all too Brief,” New York Times, December 18. 2008.
[89] Ibid.
[90] Louisiana Budget Project, “Education, Not Tax Cuts, is How Your Build A Strong Economy that Helps Everyone,” August 22, 2013, http://www.labudget.org/lbp/2013/08/education-not-tax-cuts-is-how-you-build-a-strong-economy-that-helps-everyone/ (accessed September 10, 2013); Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, p.8.
[91] Louisiana Budget Project, “The 2013 Legislature: A Session of: Missed Opportunities,” June 14, 2013, http://www.labudget.org/lbp/2013/06/the-2013-legislature-a-session-of-missed-opportunities/ (accessed September 10, 2013); Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, p. 8.
[92] State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p 76.
[93] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf, p. 50.
[94] Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, p. 5.
[95] State of Louisiana, “Statewide Coordinated Statement of Need and HIV Comprehensive Plan,” 2009, http://www.hiv411.org/files/File/2011/Louisiana_2009_Statewide_Coordinated_Statement_of_Need_and_HIV_Comprehensive_Plan.pdf (accessed September 10, 2013), p. 44; State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 31.
[96] Patient Protection and Affordable Care Act, signed into law March 23, 2010 (Public Law No. 111-148); Health Care and Education Reconciliation Act, signed into law March 30, 2010 (Public Law 111-152).
[97]National Federation of Independent Business v. Sibelius, 567 U.S. __ 2012.
[98] Affordable Care Act, Title II, Subtitle (A), section 2001.
[99] Michelle Millhollon, “Senate Bats Back Another Effort to Accept Medicaid Expansion,” Baton Rouge Advocate, June 2, 2013.
[100] “Jindal’s Arguments Against Medicaid Expansion”, Health Care Journal of Baton Rouge (2013).
[101] Center for Budget and Policy Priorities, “How Health Reform’s Medicaid Expansion Will Impact State Budgets”, July 25, 2012, http://www.cbpp.org/cms/index.cfm?fa=view&id=3801 (accessed August 26, 2013); Louisiana Budget Project, “Medicaid Expansion: An Opportunity to Invest in Louisiana’s Workforce,” undated, http://www.labudget.org/lbp/wp-content/uploads/2012/09/Medicaid-expansion-an-opportunity-to-invest.pdf (accessed August 26, 2013).
[102] Louisiana Department of Health and Hospitals, “Understanding the Impact of a Medicaid Expansion in Louisiana,” March 13, 2013, http://www.dhh.louisiana.gov/assets/medicaid/docs/MdcdExpntnImpct_Mrch13.pdf (accessed August 26, 2013).
[103] Center for Budget and Policy Priorities, “How Health Reform’s Medicaid Expansion Will Impact State Budgets”, July 25, 2012, http://www.cbpp.org/cms/index.cfm?fa=view&id=3801 (accessed August 26, 2013); Louisiana Budget Project, “Medicaid Expansion: An Opportunity to Invest in Louisiana’s Workforce,” undated, http://www.labudget.org/lbp/wp-content/uploads/2012/09/Medicaid-expansion-an-opportunity-to-invest.pdf (accessed August 26, 2013).
[104] Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2010, http://www.taepusa.org/SHARP/Louisiana.aspx (accessed September 10, 2013), p. 18.
[105] Louisiana Budget Project, “Medicaid Expansion: An Opportunity to Invest in Louisiana’s Workforce,” undated, http://www.labudget.org/lbp/wp-content/uploads/2012/09/Medicaid-expansion-an-opportunity-to-invest.pdf (accessed September 10, 2013).
[106] Louisiana Developmental Disabilities Council, “Louisiana Medicaid Program Changes Will Cause Loss of Services for Many Participants,” July 29, 2013, http://www.hdc.lsuhsc.edu/pdf/LaDDCNews7-29-13.pdf (accessed September 10, 2013).
[107] Louisiana Budget Project, “Medicaid Expansion: An Opportunity to Invest in Louisiana’s Workforce,” undated, http://www.labudget.org/lbp/wp-content/uploads/2012/09/Medicaid-expansion-an-opportunity-to-invest.pdf, p. 2.
[108] Human Rights Watch interview with Kathy Kliebert, Secretary of the Louisiana Department of Health and Hospitals, Baton Rouge, Louisiana, September 10, 2013.
[109] Louisiana Budget Project, “Deep Cuts to LSU Hospitals and Rejection of Medicaid Expansion Would Be a Double Whammy,” July 19, 2012, http://www.labudget.org/lbp/2012/07/deep-cuts-to-lsu-hospitals-and-rejection-of-medicaid-expansion-would-be-a-double-whammy-for-low-income-uninsured-louisianans-and-health-care-providers/ (accessed September 10, 2013).
[110] LSU Health Care Services Division, “The Louisiana Public Health Information Exchange: An Overview, undated. On file with Human Rights Watch.”; Jane Herwehe et al., “Implementation of an Innovative, Integrated, Electronic Medical Record (EMR) and Public Health Information Exchange for HIV/AIDS,” Journal of American Medical Information Association, vol. 19 (2012).
[111] Louisiana Budget Project, “Deep Cuts to LSU Hospitals and Rejection of Medicaid Expansion Would Be a Double Whammy,” July 19, 2012, http://www.labudget.org/lbp/2012/07/deep-cuts-to-lsu-hospitals-and-rejection-of-medicaid-expansion-would-be-a-double-whammy-for-low-income-uninsured-louisianans-and-health-care-providers/; Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, pp. 22-23.
[112] Jeff Adelson, “Louisiana State Representative Calls for Giving Control of Local Hospital System to Local Boards,” New OrleansTimes-Picayune, February 25, 2013; Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, pp.24-25; “The Expansion Question,” Health Care Journal of Baton Rouge (2013).
[113] Center for Health Law and Policy Innovation, Harvard Law School, State Healthcare Access Research Project, Louisiana State Report 2013, p.12.
[114] Human Rights Watch interview with Kathy Kliebert, Secretary of the Louisiana Department of Health and Hospitals, Baton Rouge, Louisiana, September 10, 2013.
[115] Bobby Jindal, “Why I Opposed Medicaid Expansion,” New OrleansTimes-Picayune, July 23, 2013.
[116] The Commonwealth Fund, “Health Care in the Two Americas: Findings from the Scorecard on State Health System Performance For Low Income Populations 2013,” September 18, 2013, p. 15.
[117] Universal Declaration of Human Rights, G.A. Res. 217, UN GAOR, 3rd Sess., pt. 1, UN Doc. A/810 (1948), art. 25(1); International Covenant on Economic, Social and Cultural Rights (ICESCR), adopted December 16, 1966, GA Res. 2200 (XXI), UN GAOR (no. 16), at 49, UN Doc. A/6316 (1966), 99 UNTS 3, entered into force January 3, 1976, art. 11(1), signed by the US on October 5, 1977; Committee on Economic, Social and Cultural Rights, General Comment No. 14, Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4, adopted August 11, 2000, para. 11 (the right to health is “an inclusive right extending not only to timely and appropriate health care but also to the underlying determinants of health, such as access to safe and potable water and adequate sanitation, an adequate supply of safe food, nutrition and housing, healthy occupational and environmental conditions, and access to health-related education and information, including on sexual and reproductive health”).
[118] See, e.g., Columbia University Mailman School of Health, The CHAIN Study, 1995-2009, undated, http://www.nyhiv.com/data_chain.html#reports (accessed September 10, 2013); David Buchanan et al., “The Health Impact of Supportive Housing for HIV-Positive Homeless Patients: A Randomized Controlled Trial,” American Journal of Public Health, vol. 99 (2009), pp. 675-91.
[119] National AIDS Housing Coalition, “Housing is the Foundation of HIV Prevention and Care,” 2013, http://nationalaidshousing.org/PDF/FactSheet.pdf (accessed September 10, 2013).
[120] The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf, p. 28.
[121] Greater New Orleans Community Data Center, “Facts for Features of Katrina Recovery,” August 28, 2013, http://www.gnocdc.org/Factsforfeatures/HurricaneKatrinaRecovery/ (accessed September 10, 2013). For a comprehensive discussion of the controversial decision to raze public housing units in New Orleans post-Katrina, see Davida Finger, “Public Housing in New Orleans Post-Katrina: The Struggle for Housing as A Human Right,” Review of Black Political Economy, vol. 38 (2011).
[122] Ibid.
[123] Human Rights Watch interview with Martha Kegel, Executive Director of UNITY, New Orleans, July 29, 2013; City of New Orleans, “Office of Community Development, 2012-2016 Consolidated Plan,” August 13, 2012, http://www.nola.gov/community-development/documents/general-reports/2012-2016-consolidated-plan-city-of-new-orleans-w/ (accessed September 10, 2013).
[124] City of New Orleans, “Office of Community Development, 2012-2016 Consolidated Plan,” August 13, 2012, http://www.nola.gov/community-development/documents/general-reports/2012-2016-consolidated-plan-city-of-new-orleans-w/.
[125] New Orleans CHANGE Coalition, 2013 HIV/AIDS Housing Analysis. On file with Human Rights Watch.
[126] Note that not all of the 30 injection drug users answered the questions of whether they are HIV-positive or have hepatitis C, so the percentages reflect only the percentage of those answering those questions, x and y respectively.
[127] Human Rights Watch interview with Camilla A., New Orleans, July 30, 2013.
[128] Municipal Court of New Orleans, Prostitution Cases Filed from 1/1/2011-6/30/13, obtained by public records request and on file with Human Rights Watch.
[129] Human Rights Watch, Sex Workers at Risk: Condoms as Evidence of Prostitution in Four US Cities.
[130] Quotations are from HRW survey forms unless otherwise indicated.
[131] Human Rights Watch telephone interview with Stella Cziment and Jee Park, Office of the Public Defender, Special Litigation Department, New Orleans, June 10, 2013.
[132] Human Rights Watch interview with Theresa L., New Orleans, September 6, 2013.
[133]United States of America v. City of New Orleans, 2:12-CV-01924-SM-JCW (E.D. LA), Consent Decree filed 7/24/12,
P. 95.
[134] Human Rights Watch interview with Sgt. Nicole Barbe, LGBT Community Liaison Officer, New Orleans Police Department, New Orleans, September 8, 2013.
[135] Louisiana Department of Health and Hospitals, “Greater New Orleans Community Health Connection,” undated, http://new.dhh.louisiana.gov/index.cfm/page/679 (accessed November 18, 2013).
[136] Human Rights Watch interview with Max Ciardullo, White House Fellow for Healthy Communities, New Orleans Department of Health, New Orleans, May 23, 2013.
[137] Myron S. Cohen et al., “Prevention of HIV-1 Infection with Early Anti-Retroviral Therapies,” New England Journal of Medicine, vol. 365 (2011), pp. 493-505.
[138] AidsInfo, “Guidelines for the Use of Antiretroviral Agents in HIV-1 Infected Adults and Adolescents: Adherence to Antiretroviral Therapy,” March 27, 2012, http://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf (accessed September 2013).
[139] CDC, “Prevention Benefits of HIV Treatment,” undated, http://www.cdc.gov/hiv/prevention/research/tap/ (accessed August 28, 2013).
[140] Human Rights Watch interview with Martha Kegel, Executive Director of UNITY, New Orleans, July 29, 2013.
[141] Greater New Orleans Community Data Center, “Facts for Features of Katrina Recovery,” August 28, 2013, http://www.gnocdc.org/Factsforfeatures/HurricaneKatrinaRecovery/; Elizabeth Ferris, “Housing and Disasters: Thoughts on Katrina and Haiti,” Brookings Institution, August 21, 2012, http://www.brookings.edu/blogs/up-front/posts/2012/08/21-haiti-katrina-ferris (accessed August 31, 2013).
[142] National Conference of State Legislatures, “National Mortgage Settlement Summary,” undated, http://www.ncsl.org/issues-research/banking/national-mortgage-settlement-summary.aspx (accessed August 31, 2013).
[143] Human Rights Watch interview with Nathan Cataline, Community Engagement Coordinator, Louisiana Housing Alliance, September 4, 2013.
[144] Anne C. Spaulding et al., “HIV/AIDS Among Inmates of and Releasees from US Correctional Facilities, 2006: Declining Share of Epidemic but Persistent Public Health Opportunity,” PLoS One (2009), accessed September 10, 2013 doi:10.1371/journal.pone.0007558.
[145] State of Louisiana, HIV/AIDS Strategy for Prevention Treatment and Care 2012-2013, p. 20.
[146] Data received from Orleans Parish Prison, on file with Human Rights Watch. No data are available for new infections for 2012, but in 2011, 421 persons were newly diagnosed with HIV. Louisiana Department of Health and Hospitals, “Louisiana HIV/AIDS Quarterly Report,” March 2012, http://www.dhh.louisiana.gov/assets/oph/Center-PHCH/LouisianaHIVFirstQuarter2012.pdf, p. 15.
[147] Will Small et al., “Impacts of Intensified Police Activity on Injection Drug Users: Evidence from an Ethnographic Investigation,” International Journal of Drug Policy, vol. 17, issue 2 (2009), pp. 85-95; Thomas Kerr et al., “The Public Health and Social Impacts of Drug Market Enforcement: A Review of the Evidence,” International Journal of Drug Policy, vol. 16, issue 2 (2005), pp.210-220. Scott Burris et al., “Racial Disparities in Injection-Related HIV: A Case Study of Toxic Law,” Temple University Law Review, vol. 82, no. 5 (2011), pp. 1263-1307.
[148] Thomas Kerr et al. “Findings from the Evaluation of Vancouver’s Pilot Medically-Supervised Safe Injecting Facility-Insite,” British Columbia Centre for Excellence in HIV/AIDS, 2009, http://www.cfenet.ubc.ca/sites/default/files/uploads/publications/insite_report-eng.pdf (accessed September 10, 2013).
[149] Human Rights Watch interview with Megan McIntyre, Medical Case Manager, NO/AIDS Task Force, New Orleans, April 23, 2013.
[150] Woodruff Health Sciences Center, Emory News Center, “HIV/AIDS: Studies Shed Light on Benefits of Enhancing Links to Primary Care and Services in Jail Settings and Beyond,” November 27, 2012, http://news.emory.edu/stories/2012/11/jj_spaulding_hiv_jail_studies/ (accessed September 10, 2013).
[151] Human Rights Watch, Targeting Blacks: Drug Law Enforcement and Race in the United States.
[152] Petrice Sams-Abiodun and Gregory Rattler, Recognizing the Underutilized Economic Potential of Black Men in New Orleans.
[153] The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
[154] Human Rights Watch interview with Dr. Samuel Gore, Medical Director, Orleans Parish Prison, New Orleans, July 29, 2013.
[155] Malik Jaffer et al., “Improving Medical Care for Patients with HIV in New York City Jails,” Journal of Correctional Health Care, vol. 18 (2012), pp. 1-5.
[156] Human Rights Watch interview with Dr. Samuel Gore, Medical Director, Orleans Parish Prison, New Orleans, July 29, 2013.
[157] Human Rights Watch interview with Dr. Samuel Gore, Medical Director, Orleans Parish Prison, New Orleans, July 29, 2013; Human Rights Watch telephone interview with Dr. Lynn Besch, LSU Medical Center, New Orleans, June 12, 2013; Human Rights Watch interview with Megan McIntyre, Medical Case Manager, NO/AIDS Task Force, New Orleans, April 23, 2013.
[158] Human Rights Watch interview with Dr. Samuel Gore, Medical Director, Orleans Parish Prison, New Orleans, July 29, 2013.
[159] National Center for Transgender Equality and the National Gay and Lesbian Task Force, “Injustice at Every Turn: A Report of the National Transgender Discrimination Survey,” February 3, 2011, http://www.thetaskforce.org/reports_and_research/ntds (accessed September 10, 2013).
[160] Ibid.
[161] Amnesty International, “Stonewalled: Police Abuse and Misconduct Against Gay, Lesbian, Bisexual and transgender People in the United States,” September 2005, http://www.amnesty.org/en/library/asset/AMR51/122/2005/en/2200113d-d4bd-11dd-8a23-d58a49c0d652/amr511222005en.pdf (accessed September 10,2013); Human Rights Watch, Sex Workers at Risk: Condoms as Evidence of Prostitution in Four US Cities.
[162] Human Rights Watch, No Escape: Male Rape in US Prisons, April 2001, http://www.hrw.org/reports/2001/04/01/no-escape-male-rape-us-prisons; Jamie Fellner, Human Rights Watch, “Stop Prison Rape Now,” The Daily Beast, September 4, 2013, http://www.thedailybeast.com/articles/2013/09/04/stop-prison-rape-now.html (accessed September 10,2013).
[163] Order Approving Consent Judgment and Certifying Plaintiff Class, Jones et al. v. Gusman, Civil Action 12-859, Eastern District of Louisiana, filed June 16, 2013, pp. 18-19.
[164] Ibid.
[165] Ibid.
[166] Breakout! Testimony before Prison Rape Elimination Commission, New Orleans, September 15, 2013. On file with Human Rights Watch.
[167] Prison Rape Elimination Act, 2003, 28 CFR 115.42 et seq.
[168] Human Rights Watch interview with Wesley Ware, Director of BreakOUT! New Orleans, May 21, 2013.
[169] State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015, p. 56.
[170] New Orleans Health Department, “Transmutation: New Orleans Eligible Metropolitan Area Comprehensive Plan 2012-2014,” April 2012, http://norapc.org/downloads/5c7f5565b7f0c96e1ba7f0af69c9a48b/1169e6403c374323cbc946043e9a8d95/Transmutation%20NOEMA%20Comprehensive%20Plan%202012%202014.pdf.
[171] Ibid.
[172] Personal Responsibility and Work Opportunity Reconciliation Act, 1996, PL 104-193, as amended by the Illegal Immigration Reform and Immigrant Responsibility Act, PL 104-208; Kaiser Family Foundation, “Medicaid and SCHIP eligibility for Immigrants,” April 1, 2006, http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7492.pdf (accessed august 16, 2013).
[173] Human Rights Watch interview with Jacinta Gonzales, Executive Director, Workers Center for Racial Justice, New Orleans, February 24, 2013.
[174] Human Rights Watch, Sex Workers at Risk: Condoms as Evidence of Prostitution in Four US Cities.
[175] Immigration and Nationality Act of 1952, as amended, (INA) section 212.
[176] “Me parace injusto que la policia lo lleve preso a uno por tener condones consigo. Pore so algunas veces tengo sexo sin proteccion.”
[177] Human Rights Watch, Southern Exposure: HIV and Human Rights in the US South, November 26, 2010, http://www.hrw.org/news/2010/11/26/southern-exposure.
[178] International human rights law applies to all levels of government within a federal system. See, e.g., International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, GA Res. 2200A (XXI), 21 UN GAOR Supp. (No. 16) at 52, UN Doc. A/6316 (1966), 999 UNTS 171, entered into force March 23, 1976, ratified by the US on June 8, 1992, art. 50 (“The provisions of the present Covenant shall extend to all parts of federal States without any limitations or exceptions.”); International Convention on the Protection and Promotion of the Rights and Dignity of Persons with Disabilities, G.A. Res. 61/106, Annex I, U.N. GAOR, 61st Sess., Supp. No. 49, at 65, U.N. Doc. A/61/49 (2006), entered into force May 3, 2008, art. 4(5).
[179] Universal Declaration of Human Rights, G.A. Res. 217, UN GAOR, 3rd Sess., pt. 1, UN Doc. A/810 (1948), art. 25(1).
[180] International Covenant on Economic, Social and Cultural Rights (ICESCR) adopted December 16, 1966, GA Res. 2200A (XXI), UN GAOR (no. 16) at 49, UN Doc. A/6316 (1966), 99 UNTS 3, entered into force January 3, 1976, signed by the US on October 5, 1977.
[181] Vienna Convention on the Law of Treaties, adopted may 23, 1969, entered into force January 27, 1980, article 18.
[182]ICESCR, art. 11(1); Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Do. E/C.12/2000/4, adopted August 11, 2000, para. 11.
[183] The White House “National HIV/AIDS Strategy for the United States,” July 2010, http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf; State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015.
[184] Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, para. 12.
[185] ICCPR, art. 26.
[186] International Convention on the Elimination of All Forms of Racial Discrimination (ICERD), adopted December 21, 1965, GA Res. 2106 (XX), annex, 20 UN GAOR Supp. (No. 14) at 47, UN Doc. A/6014 (1966), 660 UNTS 195, entered into force January 4, 1969, ratified by the United States on November 20, 1994, art. 5.
[187] ICERD, art. 2(2).
[188] ICERD, art. 5(e)(iv).
[189] ICERD, art. 1(1).
[190] Committee on the Elimination of Racial Discrimination, Concluding Observations of the Committee on the Elimination of Racial Discrimination on the United States, Geneva, May 8, 2008, UN Doc. CERD/C/USA/CO 6, paras. 16, 32.
[191] Kaiser Family Foundation, “State Health Facts, Uninsured Rates by Race/Ethnicity 2010-2011,” undated, http://kff.org/uninsured/state-indicator/rate-by-raceethnicity/.
[192] Louisiana Department of Health and Hospitals, “Louisiana HIV/AIDS Quarterly Report,” March 2012, http://www.dhh.louisiana.gov/assets/oph/Center-PHCH/LouisianaHIVFirstQuarter2012.pdf.
[193] Louisiana Office of Public Health, “STD/HIV Program,” undated, http://new.dhh.louisiana.gov/index.cfm/page/919 (accessed September 10, 2013). State of Louisiana, HIV/AIDS Strategy for Prevention, Treatment and Care Services, 2012-2015.
[194] UNITY of Greater New Orleans, “Homeless in New Orleans: A report on Progress in Ending Homelessness,” May 2012, http://unitygno.org/wp-content/uploads/2011/11/Homeless-Services-Working-Group_-Ten-Year-Plan-to-End-Homelessness.pdf (accessed September 10, 2013).
[195] ICCPR, art. 6.
[196] UN Human Rights Committee, General Comment No. 6, art. 6, The Right to Life, April 30, 1982, para. 5.
[197] UN Committee on ESC Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, para. 50.
[198] World Health Organization, “Technical Guide for Countries to Set Targets for Universal Access to HIV Prevention and Care for Injecting Drug Users,” 2009, http://www.who.int/hiv/pub/idu/idu_target_setting_guide.pdf, p. 6.
[199] Convention on the Elimination of All Forms of Discrimination against Women, adopted December 18, 1979, GA res. 34/18034 UN GAOR Supp. No. 46 at 193, UN Doc. A/34/46, entered into force September 3, 1981, art. 16 (1) (e).
[200] Office of the United Nations High Commissioner for Human Rights and the Joint United Nations Programme on HIV/AIDS (UNAIDS), “International Guidelines on HIV and Human Rights,” 2006, http://www2.ohchr.org/english/issues/hiv/docs/consolidated_guidelines.pdf (accessed September 10, 2013), p. 5. The guidelines state:
HIV prevalence has grown among groups most marginalized, such as sex workers, drug users, and men having sex with men. Coverage of interventions to educate people about HIV, to provide them with prevention commodities, services and treatment, to protect them from discrimination and sexual violence, and to empower them to participate in the response and live successfully in a world with HIV is unacceptably low in many parts of the world.
[201] UN Code of Conduct for Law Enforcement Officials, adopted December 17, 1979, GA Res. 34/169, annex, 34 UN GAOR Supp. (No. 46) at 186, UN Doc. A/34/46 (1979), art. 1(c).
[202] Office of the United Nations High Commissioner for Human Rights and the Joint United Nations Programme on HIV/AIDS (UNAIDS), “International Guidelines on HIV and Human Rights,” 2006, http://www2.ohchr.org/english/issues/hiv/docs/consolidated_guidelines.pdf, (accessed September 10, 2013), para. 21(c).
[203] Joint United Nations Programme on HIV/AIDS (UNAIDS), “Guidance Note on HIV and Sex Work,” 2012, http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2009/JC2306_UNAIDS-guidance-note-HIV-sex-work_en.pdf, p. 2.
[204] Office of the United Nations High Commissioner for Human Rights and the Joint United Nations Programme on HIV/AIDS (UNAIDS), “International Guidelines on HIV and Human Rights,” 2006, http://www2.ohchr.org/english/issues/hiv/docs/consolidated_guidelines.pdf, p. 12.
[205] Yogyakarta Principles on the Application of International Human Rights Law in relation to Sexual Orientation and Gender Identity, March 2007, principle 7(a).
[206]United States of America v. City of New Orleans, 2:12-CV-01924-SM-JCW (E.D. LA), Consent Decree filed 7/24/12, sections V,VIII,IX,et seq;Consent Judgment, Jones et al. v. Gusman, Civil Action 12-859, Eastern District of Louisiana, filed December 11, 2012, section IV(A)1.
[207] Prison Rape Elimination Act, 2003, 28 CFR 115.42 et seq.
[208] Convention Against Torture and other Cruel Inhuman or Degrading Treatment or Punishment (CAT), adopted December 10, 1984, GA Res. 39/46, annex, 39 UN GAOR Supp. (no. 51) at 197, UN Doc. A/39/51 (1984) entered into force June 26, 1987, ratified by the US on October 15, 1994.
[209] UN Code of Conduct for Law Enforcement Officials, art. 2; UN Body of Principles for the Protection of All Persons Under Any Form of Detention and Imprisonment, GA Res. 43/173, annex, 43 UN GAOR Supp. (no. 49) at 298, UN Doc. A/43/49 (1988), principle 1; UN Standard Minimum Rules for the Treatment of Prisoners, adopted by the First United Nations Congress on the Prevention of Crime and the Treatment of Offenders, held at Geneva in 1955, and approved by the Economic and Social Council by its resolution 663 (XXIV) of July 31, 1957, and 2076 (LXII) of May 13, 1977, para. 26.
[210] See Guidelines for the Effective Implementation of the Code of Conduct for Law Enforcement Officials, General Assembly, UN Doc. A/RES/44/162, December 15, 1989.
[211] The UN Special Rapporteur on Torture has stated that “rape and other forms of sexual assault in detention are a particularly despicable violation of the inherent dignity and right to physical integrity of every human being; and accordingly constitute an act of torture.” UN Special Rapporteur on Torture, Summary Record of the 21st Meeting, UN ESCOR, Commission on Human Rights, 48th Session, paragraph 35, UN Doc. E/CN.4/1992/SR.21 (1992).
[212] In its 2006 recommendations for the United States, the Committee Against Torture expressed concern about reliable reports of sexual assault in detention and “that persons of differing sexual orientation are particularly vulnerable.” Conclusions and Recommendations: United States, CAT/C/USA/CO/2, para. 32, May 18, 2006.
[213] US Department of State, “US Response to UN Human Rights Council Working Group Report,” March 10, 2011, http://www.state.gov/j/drl/upr/157986.htm (accessed September 10, 2013).