Summary
As a patient, you have to struggle with very low self-esteem and also have to fight with negative attitudes from society … it is like a death sentence.
—Doris Appiah, referring to her five years in a Kumasi prayer camp, Accra, November 2011
Doris, 57, has bipolar disorder, a mental disability characterized by serious shifts in mood, energy, thinking, and behavior.
At 22 her father took her to a prayer camp, a Christian religious institution in Kumasi, south central Ghana. For five years she languished at the camp, which was being run by a self-described prophet who claimed to receive instructions from God about how to treat individuals like Doris, whom he said were “possessed by demons.”[1] At some point she was tethered by a rope to a wall for about two months, forced to fast for days at a time, and left to sleep, bathe, and defecate in the open.
Finally, in 1982 at the age of 27, Doris escaped to the streets of Kumasi, where she wandered barefoot, dirty, and disheveled. “People would see me and run off, calling me a ghost,” she said. “They would not share a bucket [of water] with me to bathe. One person gave me food on a plate, and after I ate, they threw the plate away.”
Before and after her time at the prayer camp, she spent time in Accra Psychiatric Hospital. During one such occasion in 2010, she told Human Rights Watch that she witnessed people being injected with medications against their will, and nurses beating patients who failed to respond to instructions. “I used to feel lonely … ashamed … [being in the hospital],” Doris said. “What I needed was a clinical psychologist to talk to and community-based rehabilitation, but these services are not easy to come by.” After 19 years in prayer camps and psychiatric hospitals, Doris was discharged in 1989, and she started receiving support from BasicNeeds, a local organization that serves people with mental disabilities. BasicNeeds introduced her to their other members for peer support, and to community nurses. Gradually her health improved, and in 2005 she started advocating for rights and better living conditions for persons experiencing what she had gone through.
***
An estimated 2.8 million persons in Ghana have mental disabilities. Of these, 650,000 are thought to have severe mental disabilities. In the country mental disability is widely considered—even by persons with mental disabilities themselves—as being caused by evil spirits or demons.
Focusing on the southern parts of the country, this report examines the experiences of persons with mental disabilities in Ghana in the three main environments in which they receive care: the broader community, the country’s three public psychiatric hospitals, and residential prayer camps. Spread throughout the country, prayer camps are privately owned Christian religious institutions with roots in the evangelical or pentecostal denominations established for purposes of prayer, counseling, and spiritual healing, and are involved in various charitable activities. The camps are run by prophets, many of them self-proclaimed. Some of these camps have units where persons with mental disabilities are admitted, and the prophets seek to heal persons with mental disabilities with prayer and traditional methods such as the application of various herbs. The prophets, or pastors, and staff at these camps have virtually no mental health care training. Human Rights Watch has not been able to ascertain the number of prayer camps in Ghana, but there is a general belief in the country that there are several hundred such camps, operating with virtually no government oversight.
However, the primary role of prayer camps, according to those who spoke to Human Rights Watch, is not to treat persons with mental disabilities. While each of the eight camps Human Rights Watch visited has a unit for treating persons with mental disabilities, such treatment was the smallest component of the work being done at the camps. There was considerably greater emphasis on various forms of spiritual and temporal activities like worship and commercial agriculture.
Private psychiatric hospitals also exist but can treat only about 100 inpatients in total at a time and are too expensive for most Ghanaians.
The research for this report is based on visits to eight prayer camps and three psychiatric hospitals, and interviews conducted between November 2011 and June 2012 with nearly 170 persons including persons with mental disabilities in psychiatric hospitals, prayer camps, and in the community, caregivers, government officials, health service providers, representatives of nongovernmental organizations (NGOs), including those working on disability rights and human rights more broadly, and religious leaders. Also interviewed are representatives of United Nations (UN) agencies and those of international groups working in Ghana.
Human Rights Watch found that persons with mental disabilities in Ghana often experience a range of human rights abuses in the prayer camps and hospitals that Human Rights Watch researchers visited. These patients are ostensibly sent to these institutions by their family members, police, or their communities for help. Abuses are taking place despite the fact that Ghana has ratified a number of international human rights treaties, including the Convention on the Rights of Persons with Disabilities (CRPD), which was ratified in July 2012. These abuses include denial of food and medicine, inadequate shelter, involuntary medical treatment, and physical abuse amounting to cruel, inhuman, and degrading treatment.
Human Rights Watch also found that there were few government-supported, community-based mental health services—including housing, healthcare, and medical care—even though health officials in Ghana told Human Rights Watch that they offer the most cost-effective and appropriate care for most Ghanaians with mental disabilities. Most of the people with mental disabilities interviewed by Human Rights Watch in the course of conducting this research said they preferred to receive treatment on an outpatient basis while living with their families.
Those who received daily support and were interviewed by Human Rights Watch said they did so via local NGOs, which lack the means to support the hundreds of thousands of persons who need similar assistance in Ghana.
Lack of such services, combined with pervasive negative community attitudes towards mental disability, makes integration of persons with mental disabilities into community life extremely difficult, and some are abandoned entirely once they enter a mental health care facility. In one extreme case, researchers reviewed the file of a 75-year-old woman who is believed to have lived on the ward at Ankaful Psychiatric Hospital in the Central Region for over three decades because her family never came to collect her.
In recent years the Ghanaian government has taken some steps to improve the care of people with mental disabilities, including reducing overcrowding in state psychiatric hospitals and passing the Mental Health Act in June 2012. The Mental Health Act, for the first time, laid out a clear procedure for persons with mental disabilities to challenge continued detention. Parliament has also tabled the Traditional and Alternative Medicine Bill, which seeks to regulate traditional health practices based on theories, beliefs, and experiences indigenous to different cultures.[2]
These are positive steps. However, even with the passage of the Mental Health Act, there is no system in place in Ghana to effectively and routinely monitor prayer camps, meaning that the hundreds of individuals housed in them may still be subject to the grave human rights abuses documented in this report. In addition, provisions remain in the 2012 Mental Health Act that still allow for forced admission, involuntary treatment, and guardianship. Also, it is not clear if enough resources will be allocated towards the implementation of the act’s provisions: in 2011 less than one percent of the national budget was dedicated to mental health care.
Ghana is obligated to respect the rights of persons with disabilities under international and regional legal instruments, the national constitution, and other domestic legislation. Despite these legal provisions, it has done little to ensure that protections are in place and enforced.
People with mental disabilities in Ghana whom Human Rights Watch interviewed endured a variety of human rights abuses in psychiatric facilities and prayer camps. These include, but are not limited to: involuntary admission and arbitrary detention, prolonged detention, overcrowding and poor hygiene, chaining, forced seclusion, lack of shelter, denial of food, denial of adequate health care, involuntary treatment, stigma and its consequences, physical and verbal abuse, electroconvulsive therapy, and violations against children with disabilities.
Involuntary Admission and Arbitrary Detention
Most people with mental disabilities interviewed by Human Rights Watch who live in prayer camps and hospitals were placed there without their consent by family members or the police because they had exhibited restless, confused, or aggressive behavior. Others said that their families had called (or paid) the police to take them to psychiatric hospitals, or that police had picked them up on the streets where they were living. Some had not known where they were being taken until they got to a camp or hospital.
Prolonged Detention
Interviewees told Human Rights Watch that they wanted to leave the hospital or camp, but that some administrators would not permit this because family members did not come to pick them up or doctors were too busy to approve their discharge. In some prayer camps they were unable to leave because, they were told, the prophet was still awaiting a message from God. Some remained even after discharge because their families had abandoned them, and they could not return to their home communities. Human Rights Watch could not ascertain whether persons with mental disabilities subjected to prolonged detention, both in hospitals and in prayer camps, had been before a judge to review or challenge their detention.
The previous mental health law did not provide a framework through which people who are detained in psychiatric facilities could challenge such detention. While the new Mental Health Act now creates a tribunal mandated to hear complaints of people with mental disabilities detained under the act, it is not clear whether those detained for mental health reasons outside of psychiatric hospitals, including those detained in prayer camps, can seek protection under the new law.
Overcrowding and Poor Hygiene
Overcrowding is a serious problem in public hospitals and prayer camps. Facilities stank of urine and feces, and there was inadequate water for drinking or bathing. Toilets were broken, overflowed, or nonexistent.
Overcrowding in Accra Psychiatric Hospital and in some wards in Pantang Psychiatric Hospital, together with significant staff shortages (there are only 12 practicing psychiatrists and 600 psychiatric nurses nationwide), created terrible living conditions for persons with mental disabilities. In two psychiatric hospitals, urine, flies, and cockroaches competed for space in the toilets, and nurses, lacking cleaning equipment, instructed patients to clean the wards and toilets, including removing other patients’ feces, without gloves. In Mount Horeb Prayer Camp in the Eastern Region and Edumfa Prayer Camp in the Central Region, individuals urinated and defecated in buckets in rooms that residents said were emptied only once a day.
Chaining
In four prayer camps Human Rights Watch found that people were either locked in chains inside fully built and semi-permanent structures, or chained to a tree or concrete floor until the pastor or prophet declared them “healed.” Movement was impossible beyond the length of the constraint—usually about two meters. People had to bathe, defecate, urinate, change sanitary towels, eat, and sleep on the spot where they were chained. Human Rights Watch found that many of the 135 individuals at the Mount Horeb Prayer Camp were chained 24 hours a day; some said they had been restrained for several months. Researchers found an individual chained in exactly the same spot where he had been interviewed three months earlier.
Forced Seclusion
Seclusion is one of many forms of solitary confinement. The special rapporteur on torture regards as torture, any prolonged isolation of an inmate from others (except guards) for at least 22 hours a day. In all three public psychiatric hospitals Human Rights Watch found that people were isolated for up to three days, sometimes for refusing to take medicine. Patients complained that isolation rooms lacked proper sanitation facilities.
Lack of Shelter
Shelter was a major concern in all eight prayer camps and in some wards in the three psychiatric hospitals that Human Rights Watch visited. In Accra Psychiatric Hospital, for example, over one-third of individuals in the ward designated for patients sent to the hospital by the courts or police slept outside. In other wards patients sat in the sun all day or crowded in corners where shade provided temporary relief from the blistering heat. The situation was often no better—and sometimes worse—in prayer camps, including two in eastern Ghana where individuals spoke of living without adequate shelter, such as a roof over their heads or protection from the sun, and with constant exposure to mosquitoes.
Denial of Food
Many interviewees spoke of persistent, gnawing hunger from forced fasting in prayer camps or inadequate food in hospitals, and many looked hungry. Administrators and pastors of seven of the eight prayer camps visited said fasting was a key component of curing mental disability and would help to starve evil spirits, “making it easier for the spirit of God to enter and do the healing.” People interviewed said there was too little food, sometimes only one meal a day. Some individuals in Mount Horeb, Edumfa, and Nyakumasi Prayer Camps had to fast for 36 hours over 3 consecutive days in 12-hour stints from morning until dusk. Others, mainly the elderly, fasted from 6 a.m. until noon. Such fasting regimes ranged from 7 to 40 days, and meant that people could not take prescribed medication in camps that allowed the use of such medication.
Denial of Adequate Health Care
Access to health care, including drugs, for both physical and mental health problems was a major challenge for persons with mental disabilities. In psychiatric hospitals patients were responsible for buying their own drugs, especially to treat illnesses such as malaria, although some had no relatives to send to buy the drugs or money to do so. In some prayer camps, such as Nyakumasi, the prophet and camp staff did not allow persons with mental disabilities to use prescription medicine. “Even when you get malaria,” Elijah, a 25-year-old man who had been chained to a tree at Nyakumasi prayer camp for five months prior to Human Rights Watch’s visit, said, “they give you adwengo (palm oil) because angels here don’t allow taking medication.” Only one out of the eight camps visited allowed any medical care for mental health disabilities and other medical conditions at all.
Involuntary Treatment
Human Rights Watch found that persons living in psychiatric hospitals were subjected to involuntary treatment through the use of force, coercion, and sedation. Some individuals said they were forced to take treatment against their will, even when medicine failed to work or led to serious side effects or complications. “I don’t like the medicine I receive,” Peace, a 55-year-old woman admitted at Pantang Psychiatric Hospital, told Human Rights Watch. “The drugs cause my legs to swell, eye pains, and insomnia.” Some patients reported being beaten if they refused to take medication, and staff at all three public psychiatric hospitals admitted using physical coercion, and in extreme cases, involuntary sedation via injection. In some prayer camps people were forced to take local herbs against their will, sometimes through their noses.
Stigma and Its Consequences
Persons with mental disabilities endure stigma and discrimination in the health sector, at home, and in the community. Some of the religious leaders interviewed by Human Rights Watch described persons with mental disabilities as incapable, hostile, demonic, evil, controlled by spirits, useless, and anti-social. Such stigma in turn causes family members to abandon persons with mental disabilities in psychiatric hospitals and prayer camps, neither visiting them nor picking them up after discharge. Some give a false address so they cannot be traced. Stigma also deters persons with mental disabilities from seeking professional services in psychiatric hospitals.
Psychiatric nurses and doctors also said they experienced stigma due to their work in their home communities and among professional peers.
Physical and Verbal Abuse
Human Rights Watch documented severe cases of physical and verbal abuse against persons with mental disabilities in the family, community, hospitals, and prayer camps.
Interviewees said they faced threats of abuse, and actual physical and verbal abuse, for trying to escape, when they complained about pain, and when they failed to take medication, or for failing to follow hospital rules. Harriet, a pregnant woman at Ankaful Psychiatric Hospital, told Human Rights Watch, “Yesterday they [nurses] were drawing blood from me and I was feeling a lot of pain and I said, ‘You are killing me.’ The nurse said, ‘If you shout again, I will put the needle in your mouth.’” One nurse told Human Rights Watch that nurses beat aggressive patients who attacked them.
Electroconvulsive Therapy
Psychiatrists in Ghana continue to use electroconvulsive therapy (ECT), a method of treatment which involves passing electricity through the brain, to treat persons with severe depression. One doctor explained that no anesthesia was administered due to lack of equipment and personnel. The UN special rapporteur on torture has noted that unmodified ECT (without anesthesia, muscle relaxant, or oxygenation) is an unacceptable medical practice that may constitute torture or ill-treatment.
Violations against Children with Disabilities
Children with mental disabilities experienced similar conditions to adults in psychiatric hospitals and prayer camps. Some individuals in Accra Psychiatric Hospital’s Children’s Ward—where almost half the patients were actually adults—had been there since 1980. Lack of staff was particularly acute, and a nurse said they lacked the resources to provide stimulating activities, such as games and television, or the skills to engage the children and handle those with intellectual disabilities. Researchers saw filthy living conditions: in some cases children and adults were lying down naked next to their feces. The situation was even worse in three of the eight prayer camps Human Rights Watch visited. In these camps children were subjected to restraints and other abuses. Solomon, 9, who lived in Edumfa Prayer Camp and was often chained in the same room with about 20 other males told Human Rights Watch, “I have been fasting for 21 days .… I feel pains in my stomach, my head, and my whole body.”
***
Necessary Steps
Immediate attention is needed to address the human rights abuses outlined in this report, particularly to ensure adequate food, shelter, and health care for persons with mental disabilities and to ensure civil and criminal penalties for abusive practices such as chaining, forced fasting, prolonged seclusion, and other forms of cruel and degrading treatment in the hospitals and prayer camps.
As Ghana has now ratified the CRPD, the government should promptly review its disability and mental health laws and policies to ensure compliance with its international legal obligations. It must also adopt legal measures and mechanisms to regulate non-orthodox service providers including prayer camps. This should involve formal registration with government health authorities, regular monitoring of services, and training prayer camp staff.
The government should also develop community-based mental health and support services so that persons with mental disabilities can more easily live in the community and outside institutions such as psychiatric hospitals and prayer camps. Discharging people from psychiatric facilities back to their communities will likely encourage independent living in a less restricted environment.
Realizing meaningful community living requires better equipped regional, district, and other hospitals, which are closer to persons with mental disabilities, and training and recruiting more mental health professionals, social workers, and volunteers, especially at district and grassroots levels. It will also necessitate a range of non-medical support services, such as housing, food, and community education about mental health.
Ensuring that persons with mental disabilities can enjoy their human rights requires efforts from a range of stakeholders. There is need for international partners working in Ghana, including the World Bank, the United Nations Children's Fund (UNICEF), and the United States Agency for International Development (USAID), to undertake programs which are sensitive to the needs of persons with mental disabilities.
Key Recommendations
To the Government of Ghana
Immediate Actions:
- Immediately improve conditions in public psychiatric hospitals by ensuring adequate food, shelter, and health care and by prohibiting practices of beating patients, prolonged seclusion, and forced admission and treatment without judicial oversight.
- Take immediate steps to ensure that individuals are not held against their will at prayer camps and hospitals, and to ensure that those in prayer camps are not subjected to forced fasting or chaining and are not denied access to appropriate health care.
Intermediate and Long-Term Actions:
- Develop voluntary community-based mental health services in consultation with persons with mental disabilities and their representative organizations.
- Ensure that persons with mental disabilities and their representative organizations participate fully in planning, implementing, and monitoring government programs on mental health and disability.
- Enforce existing criminal laws on assault to target inhumane practices in psychiatric hospitals and prayer camps, such as chaining and prolonged restraint, mandatory fasting, and treatment without free and informed consent.
- Formulate and implement a national policy on non-orthodox mental health service provision, which should regulate prayer camps as centers for the treatment of persons with mental disabilities to ensure that patients are not involuntarily admitted or detained there, are not abused, and are not given treatment without their consent.
- Train and recruit more mental health professionals to improve the doctor/nurse-patient ratio, and increase the number of non-medical staff in psychiatric hospitals to help nurses with cleaning and other non-medical tasks.
Methodology
This report is based on five weeks of field research in Ghana between November 2011 and January 2012, including visits to Ghana’s three public psychiatric institutions and to eight prayer camps. The research was conducted in three regions in Ghana—Greater Accra Region, Central Region, and Eastern Region—chosen both for the presence of public psychiatric hospitals and the high concentration of prayer camps, according to the Christian Council of Ghana, a local organization working with persons with mental disabilities, and the Ghana Pentecostal and Charismatic Council (GPCC), a body that regulates them.
Human Rights Watch has not been able to ascertain the number of prayer camps in Ghana, but there is a general belief in the country that there are hundreds of such camps, mostly in the southern parts of the country. Human Rights Watch did not visit the northern part of Ghana in the course of conducting this research. Organizations working on mental health and other experts told Human Rights Watch that in the north there are no prayer camps being run by Christian religious institutions, as is the case in the three regions visited by Human Rights Watch. The north is predominately Muslim and its residents usually take persons with mental disabilities to Muslim clerics, known as “malams,” for treatment.
A total of 169 interviews were conducted; of those, 93 were with persons with mental disabilities (9 in psychiatric hospitals, 51 in prayer camps, and 33 living in the community). Of the 93 interviewees with mental disabilities, 52 were women, 36 were men, and 5 were children. Human Rights Watch also interviewed five family members and caregivers of persons with mental disabilities.
Human Rights Watch only visited prayer camps where we had prior information that such camps had a unit for persons with mental disabilities or admitted persons with mental disabilities. Of the eight prayer camps visited, five had varying numbers of persons with mental disabilities. The other three did not have persons with mental disabilities when visited, but had previously cared for them.
Human Rights Watch chose to visit specific prayer camps based on recommendations from local partner organizations, religious councils, and psychiatric social workers in Ghana, as well as independent background research into the camps. Local partners helped in identifying and introducing Human Rights Watch to some of the camps visited.
Among the 21 health service providers interviewed, 2 were psychiatrists, 17 were nurses, and 2 were psychiatric social workers. Interviews were also held with seventeen religious personnel including those who directed and worked within all eight prayer camps visited, pastors of churches, and members of national religious councils.
Human Rights Watch interviewed staff of 20 local disability and human rights organizations and 15 directors and staff of United Nations (UN) agencies and other international institutions including the United Nations Children’s Fund (UNICEF), the World Health Organization (WHO), the United States Agency for International Development (USAID), and the World Bank. Researchers also spoke with eight government officials, including representatives of the Commission for Human Rights and Administrative Justice (CHRAJ), the Ministry of Employment and Social Welfare, and the Ministry of Health (Ghana Health Service), as well as two members of parliament, including the chair of the Parliamentary Committee on Health and the minority leader.
Interviews were semi-structured and covered a range of topics related to experiences in the mental health system. Before each interview, Human Rights Watch staff informed interviewees of its purpose, the kinds of issues that would be covered, and asked whether they wanted to participate. Interviewees were informed that they could discontinue the interview at any time or decline to answer any specific questions without consequences.
No incentives were offered or provided to persons interviewed. When possible, individuals were interviewed without the presence of staff or administrators. Interviewees were asked if they would like their identity to be kept confidential; individuals who requested anonymity have been given pseudonyms. In certain cases, the names of health care professionals have been withheld to protect their identity.
Interviews were conducted by Human Rights Watch researchers in English, and through translators in Twi, a local language.
Human Rights Watch also consulted with international disability rights experts and mental health experts at various stages of the research and writing and reviewed a number of official documents from the Ghanaian government, as well as relevant reports from multilateral and bilateral donors, UN agencies, and NGOs.
This report does not cover conditions experienced by persons with mental disabilities who are treated by traditional healers, even though these healers take care of a significant number of persons with mental disabilities, especially in the northern part of the country.[3] We chose to concentrate on psychiatric hospitals and prayer camps because they housed higher numbers of people with mental disabilities, and there have been reports in the media and by local and international NGOs about the abuses going on in these institutions. The abuses detailed in this report relate only to the three hospitals and eight prayer camps in the Greater Accra, Central, and Eastern Regions visited by Human Rights Watch. No claims have been made about possible abuses in other prayer camps in these regions or other parts of the country.
Throughout the research, efforts were made to verify claims and information provided by interviewees through direct observations, interviews with staff members at psychiatric hospitals and prayer camps, and review of psychiatric hospital records when available.
In the report, the term resident is used to refer to persons with actual or perceived mental disabilities in prayer camps, including those who did not have or know their diagnosis.
I. Mental Disability in Ghana
Overview
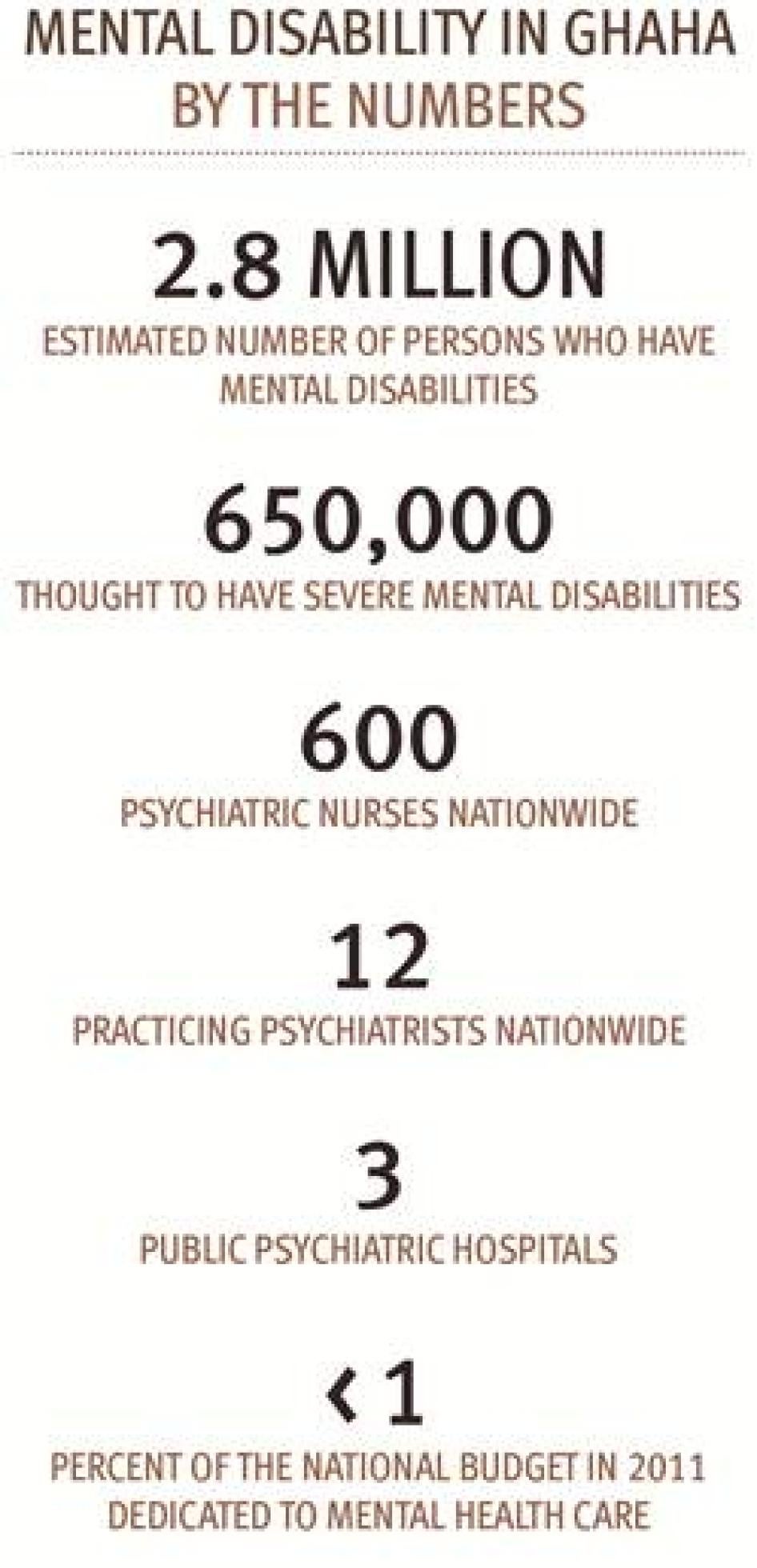
The World Health Organization (WHO) has estimated that there are 2.8 million persons with mental disabilities in Ghana, 650,000 of whom have severe mental disabilities.[4]
There is no specific international consensus on the definition of disability, but the Convention on the Rights of Persons with Disabilities (CRPD), the newest international human rights treaty, describes persons with disabilities as including “those who have long-term physical, mental, intellectual or sensory impairments which in interaction with various barriers may hinder their full and effective participation in society on an equal basis with others.”[5] Ghana signed the CRPD in March 2007 and ratified it on July 31, 2012. The 1992 Constitution of Ghana in article 75 stipulates that parliament must pass an act or a resolution with the votes of more than one-half of all members for the CRPD to enter into force, and parliament passed such a resolution in March 2012, which confirmed the entry into force of the CRPD before it was officially ratified in July 2012.
In this report, mental disability refers to mental health problems such as depression, bipolar disorder, and schizophrenia. Persons with mental health problems also refer to themselves as having psychosocial disabilities, a term that reflects the interaction between psychological differences and social or cultural limits for behavior, as well as the stigma that the society attaches to persons with mental impairments.[6]
The vast majority of patients in Ghana’s psychiatric hospitals are treated for mental health problems. According to Dr. Akwasi Osei, director of Accra Psychiatric Hospital, 20-30 percent of patients are diagnosed with schizophrenia, 20 percent with bipolar disorder, and 15-20 percent with major depression. Drug-related psychosis affects 8-10 percent of patients and epilepsy was found in 5 percent of patients.[7]
According to a senior health official, mental disability in Ghana is widely considered as having a spiritual origin, caused by evil spirits or demons.[8] This view on the causes of disability was held by all camp leaders that Human Rights Watch interviewed, as well as some persons with mental disabilities (mainly in the community and camps) who believed evil spirits caused their mental conditions.
Although Ghana is a middle-income country with per capita gross domestic product (GDP) of around US$1,300,[9] 40 percent of adults live on less than $2 a day.[10] The quality of, and access to, health care are concerns for most Ghanaians, but poor Ghanaians with mental disabilities confront particular challenges, such as high transport fares from their homes to psychiatric hospitals, which are often several kilometers away, and the high cost of health care. While there are no conclusive statistics about the prevalence of poverty among persons with disabilities in Ghana, some studies found that poor households with persons who have disabilities face significant barriers in realizing their right to adequate health care.[11]
Although there is no clear data about Ghana’s mental health care budget, interviews conducted with officials from Ghana Health Service indicate that it is as low as 0.5-6 percent of the total health care budget allocation.[12] Expenditure of the mental health budget is also disputed, with varying figures showing that between 72 percent[13] and 94 percent of the health budget is spent on remunerations of medical professionals.[14] In 2011 less than one percent of the national budget was dedicated to mental health care.[15]
Treatment and Care Options
Individuals with mental disabilities in Ghana who receive treatment generally have three main care options: public mental health services, prayer camps, and traditional healers—people who use ritual and herbal methods of treatment. [16] Community care providers are another, albeit limited, option. Most people utilize more than one option and sometimes more than one at a time.
Public Mental Health Services
Like many developing countries, Ghana faces staff shortages within the public health system. The problem is particularly acute when it comes to mental health: there are only 12 practicing psychiatrists and 600 psychiatric nurses nationwide, serving over 2 million persons with mental disabilities.[17]
Ghana has three public psychiatric hospitals: Accra Psychiatric Hospital, Pantang Psychiatric Hospital, and Ankaful Psychiatric hospital. [18] The capacity of each is 200, 500, and 250 individuals respectively. Accra Psychiatric Hospital is considerably overcrowded, with numbers ranging from 900 to 1200 at any given period between 2010 and 2012. [19]
Staff shortage was identified as a major challenge by all the hospital staff that Human Rights Watch interviewed in the three hospitals. In Accra Psychiatric Hospital’s Special Ward, formerly called the Criminal Ward because patients arrived under police arrest or court order, three nurses were on duty caring for 205 patients at the time Human Rights Watch visited.[20] One ward at Pantang Psychiatric Hospital had four nurses on duty to care for forty patients with visibly critical needs.[21] According to the director of Accra Psychiatric Hospital, to achieve proper care, Ghana needs to increase the number of nurses in the three psychiatric hospitals almost seven-fold, from the current 600 to about 4,000.[22]
Currently, Ghana has 15 psychiatric social workers serving the whole country, which is especially low given that the 2000 Mental Health Training Policy requires the government to train at least 15 psychiatric social workers every 5 years.[23] Ebu Blankson, head of the Social Welfare Department at Ankaful Psychiatric Hospital, told Human Rights Watch, “We have three social welfare staff… taking care of… 500 patients.”[24]
Ghana started a community psychiatric nursing program in 1975, which evolved into a community mental health system. However in 2003, the latest year for which there are reliable statistics, fewer than half of Ghana’s districts—52 out of 110—had community psychiatric nurses.[25] There are also only three clinical psychologists, out of the eighty who are needed.[26]
In 2003 the government established a National Health Insurance Scheme (NHIS), which aimed to make healthcare readily available and more affordable to Ghanaians and eventually replace the user feesystem throughout the country.[27]
Mental health care is not covered by the NHIS, primarily because of the widespread assumption that mental health care in psychiatric hospitals is cost-free.[28] However, patients are often required to buy their own medicines, which are often very expensive.[29]
Persons with mental disabilities in psychiatric hospitals were therefore responsible for buying their own drugs, especially to treat physical illnesses such as malaria, and yet some of them had no relatives and could not buy these medications.[30] Explaining the effects of the shortage, Dr. Akwasi Osei, chief psychiatrist of the Ghana Health Service and director of Accra Psychiatric Hospital, said that the “lack of resources to buy drugs is state-sponsored human rights abuse.”[31]
The Ghana Federation of the Disabled is working with the Parliamentary Subcommittee on Health to improve coverage for persons with disabilities, especially including those with mental disabilities in the NHIS. The NHIS is currently under review,[32] and an amendment bill which would extend coverage to persons with mental disabilities is before parliament and is expected to be enacted before the end of 2012.[33]
Those treated within the public health care system may be inpatients or outpatients within Ghana’s three psychiatric hospitals or in some regional and district hospitals where there are designated psychiatric wards or staff.
Ghana also has four private psychiatric hospitals: two in Kumasi, one in Accra, and one in Tema. Like the three public psychiatric hospitals, the four private hospitals are located in the south of Ghana. [34] The private facilities have an estimated total inpatient capacity of 100 patients, as per their bed capacity. [35] The high cost of care, estimated at about $150 per month per person[36] in such institutions is beyond the reach of most Ghanaians, 40 percent of whom live on less than $2 a day, [37] and 28.5 percent of whom live below the poverty line. [38]
Prayer Camps
Ghana has several hundred prayer camps, which are believed to have emerged in the 1920s, although little is known about their history, numbers, or operations since they are not state-regulated.[39] There are no clear figures on how many prayer camps actually exist in Ghana, and Human Rights Watch was informed by Rev. Opoku Onyinah, chairperson of the Ghana Pentecostal and Charismatic Council (GPCC), that Ghana Evangelism Committee (GEC) is conducting a survey.[40] Most are located in the south of the country: in Ada district alone, one of the ten districts making up the Greater Accra Region, there are an estimated 70 prayer camps.[41]
The camps offer prayer and healing services for persons with mental disabilities and are private Christian religious institutions that are usually managed by prophets, many of them self-professed religious leaders who claim to be able to cure persons having various conditions, including cancer, infertility ,and physical or mental disability, through prayer and other non-medical techniques. The prayer camps which Human Rights Watch visited were like any other Christian place of worship, conducting normal church activities including prayer and counseling, in addition to supporting charitable activities, such as homes for orphans and the elderly. The main difference between prayer camps and the Catholic or protestant churches, according to a Christian leader, is that “prayer camps are more of charismatic and pentecostal churches, and they specifically believe in the power of miracles, consultation with angels, and spiritual healing.”[42]
All of the prayer camps that Human Rights Watch visited said they were Christian institutions, although some, in addition to prayers, also administer traditional herbs. More established prayer camps such as Mount Horeb and Edumfa had special sections referred to as “sanatoria” where persons with mental disabilities were taken for healing.
The camps are mainly intended as retreats for prayer and spiritual healing, and some of them have units for persons with mental disabilities.[43] However, the primary role of prayer camps, according to those who spoke to Human Rights Watch, is not to treat persons with mental disabilities. While each of the eight camps Human Rights Watch visited has a unit for treating persons with mental disabilities, such treatment was the smallest component of the work being done at such camps. There was considerably greater emphasis on various forms of spiritual and temporal activities like worship and commercial agriculture.
According to leaders of camps who administer treatment and are referred to as prophets, persons with mental disabilities are often brought by their families, [44] and may reside in the camps for several days to several years. [45]
Some prayer camps that Human Rights Watch visited were located in open fields or forests; some operated out of structures that were half-built and offered only a rooftop for shelter. Others still were more established and better funded by church networks and looked like small villages. The more established camps included Mount Horeb and Edumfa Prayer camps, both of which occupied large areas of land and had large church halls and retreat facilities for anyone who wanted spiritual services, including prayers, counseling, and consultation on various issues. These camps had several pastors assigned to different ministerial responsibilities, including counseling. Edumfa Prayer Camp management engaged in activities like commercial agriculture and baking, the proceeds of which, according to Prophetess Rebekah Bedford, help fund the day-to-day running of the prayer camp.[46]
In the camps Human Rights Watch visited, we observed that most people brought for healing for mental disabilities, drug use, or epilepsy—unlike those who had come for healing related to illnesses such as cancer—were chained to logs, trees, or other fixed spots and underwent a regime of daily prayer and fasting. Most individuals treated in the prayer camps for mental disability stayed from a few days to more than a year.[47]
In one camp residents were formally registered and received a spiritual healing plan, a form describing an internal code of conduct for prayer camp visitors, responsibilities of visitors, prayer schedules, procedures for discharge from the camp, and regular administrative tasks.[48]
Some prayer camps, like Edumfa, are affiliated with Faith Complementary Health Care Association of Ghana, an association of camps that use natural elements and the bible in healing.[49] The association issued members a booklet with instructions on how to record information of those admitted to the camps, including name, age, occupation, marital status, religion, and nearest relative, as well as individual medical histories, including examination, diagnosis, and treatment.[50] Edumfa Prayer Camp also gave Human Rights Watch a copy of an Indemnity Form, to be signed by the person with mental disability, with entries like “derangement of mind proposed treatment.” Modes of treatment listed on the form include “prayers, fasting, confinement, and such appropriate restraints as circumstances demand.”
Inside a Typical Prayer CampThere are wide variations in the way prayer camps in Ghana operate. Some, like Mount Horeb and Edumfa, are well organized with predictable daily schedules for patients, while most do not follow particular schedules. The prayer camps vary widely in size, some are as big as a small village and include a church building, a special section for persons with mental disabilities, residences for the prophets, and rooms rented to guests and other visitors. Some of these visitors stay within the camp premises for days or weeks. Some camps have big church buildings, while in others, church buildings were under construction. A day at a prayer camp, according to Mount Horeb’s Pastor Christian Hukipoti (the pastor overseeing the section housing persons with mental disabilities) starts with morning devotion (5:00 to 6:00 a.m.) after which patients take their baths. Breakfast, for those who are not fasting, is between 8:00 and 9:00 a.m. This is followed by bible study, which takes place in the church building “for those who are calm,” while those who are not considered calm are kept back in their rooms. Bible study continues until 3:00 p.m., when those who are not fasting take lunch, which lasts until 4:00 p.m. Between 4:00 and 8:00 p.m. is free time, after which those who are calm and are not in chains go for evening prayers, which end at 10:00 p.m. Pastor Hukipoti told Human Rights Watch, Between 11 p.m. and 1 a.m. we do intercession for those who are in chains and can’t go to church, and during this time, the prophet visits the respective rooms, prays for them, and casts demons out of some of them. We also have a nurse who visits our patients from Tetteh Quashi hospital; she comes twice a week (Tuesday and Friday), and we call her during emergencies, for example, when someone reacts [adversely] to medication. At Edumfa and Mount Horeb the prophets would counsel people at different hours of the day, some of whom Human Rights Watch found waiting in tents for a chance to have a one-on-one session with the prophet or prophetess. In addition, the prophets manage and oversee the administration of the camps. The m ajority of people with mental disabilities admitted to prayer camps are often chained around the clock, for several weeks until discharged. Those in chains are unable to join prayers or other activities in the camp. A few of those that Human Rights Watch interviewed who at some point were chained, especially at Mount Horeb and Edumfa prayer camps, were relocated to special wards called the “calm rooms.” Compared to other rooms, “calm rooms” were less crowded and housed the fewest number of people. Such rooms had a few makeshift beds, but some occupants slept on small mattresses, and others slept on the bare floor. A few had been declared by the prophets as healed, but stayed at the camp to provide support to those who were still undergoing treatment. They helped with the cleaning and preparing food, and some were paid a token by the camp. At Mount Horeb Human Rights Watch was told by Pastor Christian Hukipoti that the prophet would go around all the wards at night praying for the people. On Sundays, those deemed healed by the prophet would be unchained, transferred to the calm room, and allowed to attend Sunday service. Family members of camp patients told Human Rights Watch that they made the decision to take their family members to prayer camps usually on the recommendation of people who had been to such camps and had been healed. Some took their relatives to the camps after they could not be cured at psychiatric hospitals and traditional shrines. For others, prayer camps were closer to their communities, which made it easier to bring a family member for admission. While Human Rights Watch could not ascertain whether people actually got healed at the camps, prophets strongly reported that it happened. Our endeavors to ask them for addresses of those who were healed and returned to communities were futile because they said they did not keep records of the people they treated. While some prophets claimed that those healed never came back to the camp after relapses, some people with mental disabilities that Human Rights Watch interviewed said they had been to such camps more than twice. At Mount Horeb, however, two officials working in the “sanatorium,” the section set aside for people with mental disabilities, said they came in as patients, and when they got healed, they chose to serve those who came in for treatment. However, a nurse who visits Mount Horeb Prayer Camp, said she has not seen someone completely healed in the two years she has been visiting the camps, but she said some get better for some time. |
Despite serving as an alternative residential facility for those with mental disabilities, prayer camps operate with little or no state regulation. Many nominally fall under the authority of the Ghana Pentecostal and Charismatic Council (GPCC), an umbrella body for 122 churches and evangelical associations in the country, having been either registered directly as council members or founded by individual members of churches affiliated with the council.[51] The council has an ad hoc committee of elders, which monitors compliance of member churches with the guidelines regulating prayer camps.[52] However, the council’s oversight of the camps is limited, and the camps’ operations are often inconsistent with council guidelines. Prayer camps whose affiliation with the Pentecostal Council has been terminated, or which operate outside its purview, are not subject to any regulation.
The Pentecostal Council has set up structures to govern prayer camps registered with it. These structures include ad hoc committees to monitor their operations and written guidelines for prayer camp operations.[53] According to Rev. Dr. Opoku Onyinah, chairperson of the Ghana Pentecostal and Charismatic Council (GPCC), the guidelines prohibit chaining or fasting of any “sick” person, or restricting which kinds of foods people at the camps could eat. They also require the camps to send persons with mental disabilities to hospitals, and to have vehicles to rush medical cases there if necessary.[54]
The council has sometimes taken disciplinary action based upon these guidelines. For example, in May 2011, the Pentecostal Council disassociated itself and cancelled the membership of Edumfa Prayer Camp—one of the oldest and most prominent prayer camps in Ghana—for failing to meet these standards.[55] Rev. Opoku Onyinah explained that while cancellation of membership does not mean closure of the camp, the public is warned from going to such a camp, until issues that led to cancellation of membership are rectified.[56]
Lack of staff is also a concern in prayer camps. None of the eight camps that Human Rights Watch visited employed a qualified medical or psychiatric practitioner. At Mount Horeb, Edumfa, and Nyakumasi Prayer Camps, where researchers found the largest numbers of persons with mental disabilities, the staff consisted mainly of pastors, prophets, and former patients whose conditions had improved.[57] At Edumfa Prayer Camp, it was largely family members, well-wishers, and a few pastors.
Table 1. Number of Persons with Mental Disabilities Housed at Prayer Camps Visited by Human Rights Watch, November 2011-January 2012
|
Name of Prayer Camp |
Number of people with Mental Disabilities at Time of Visit |
|
Mountains Jesus Divine Temple Mission (Nyakumasi Prayer Camp) |
30 |
|
Mount Horeb International Prayer Ministries (Mount Horeb Prayer Camp) |
135 |
|
Heavenly Ministries Spiritual Revival and Healing Center – Church of Pentecost, (Edumfa Prayer Camp) |
25 |
|
United Bethel Pentecostal Ministry International- Kordiabe |
3 |
|
Charity Prayer Ministry, Kwadoegye |
2 |
Traditional Healers
According to a report by the Commonwealth Human Rights Initiative Africa, an estimated 70-80 percent of Ghanaians utilize traditional medicine.[58] Many seek treatment from the estimated 45,000 traditional healers (people who practice based on theories, beliefs, and experiences indigenous to different cultures including ritual and herbal methods of treatment).[59]
The Community
According to responses from persons with mental disabilities living in the community and their family members who Human Rights Watch interviewed, there were no medical or physical support systems after patients were discharged from psychiatric institutions. [60]
The community support available to persons with mental disabilities was mainly rendered by civil society organizations, including BasicNeeds Ghana (currently working in five out of Ghana’s ten regions), Mindfreedom Ghana, and Mental Health Society of Ghana (primarily working in the southern parts of Ghana). These organizations help community members with mental disabilities, as well as epilepsy and drug-related psychosis, to access services, especially medication. These organizations mainly work with government-trained community psychiatric nurses or volunteers. [61]
II. Abuses
As soon as you get a mental disability, you nearly lose all your rights, even to give your opinion.
—Doris Appiah, national treasurer, Mental Health Society of Ghana, Accra, Greater Accra Region, November 2011
Human Rights Watch found that people with mental disabilities in Ghana suffered a number of human rights abuses, some of which are detailed in this section.
Involuntary Admission, Arbitrary Detention
I was arrested from my home by two men who came with police. They never gave me any reason, and they handcuffed me, took me to police where I spent three days.[62]
—Peace, a 55-year-old woman with schizophrenia, Pantang Psychiatric Hospital, November 2011
Individuals with mental disabilities in psychiatric hospitals and prayer camps in Ghana are routinely institutionalized against their will by family members or police, and denied the opportunity to refuse or appeal their confinement.[63]
It was not clear whether persons with mental disabilities under prolonged detention, both in hospitals and in prayer camps, had been before a judge to review or challenge their detention. Some of the leading local organizations working with persons with mental disabilities that Human Rights Watch interviewed were unaware of any such cases.[64] Dr. Akwasi Osei, chief director of the Ghana Health Service and director of Accra Psychiatric Hospital, told Human Rights that the old mental health law did not make any provision for people who are voluntarily admitted (with consent of relatives) to challenge such admission or any resulting treatment.[65] The new Mental Health Act, however, establishes a tribunal mandated to hear complaints of people with mental disabilities detained under the act, through which persons detained against their will in psychiatric hospitals can challenge such detention. While the new Mental Health Act will allow those detained in institutions to challenge admission and treatment, the law does not expressly cover persons with mental disabilities detained in other settings such as prayer camps.
Some of the individuals who are involuntarily admitted were perceived to be a danger to themselves, property, or others, which according to Dr. Akwasi Osei, chief psychiatrist at Accra Psychiatric Hospital, is determined based on “information given to the doctors of the patient’s conduct at home, his or her level of anxiety, rapport with the hospital staff, and the nature of psychopathology (causes and processes of mental disorder).”[66]
Some have problems of drug abuse and addiction. Others are outcasts in their communities or families, and are perceived as being “different” or “difficult.” According to Dr. Akwasi Osei, if an individual is brought to the hospital by police, psychiatrists determine whether or not to admit the person depending on their symptoms, behavior, and diagnosis, without seeking the patient’s consent, and without an independent judicial review.[67]
Peace, a 55-year-old woman with schizophrenia at Pantang Psychiatric Hospital, told Human Rights Watch, “Hospital is not a place where anyone would like to live … but I have no right to leave the ward.”[68]
Police, working with local government assemblies, also round up persons with actual or perceived mental disabilities when Ghana hosts important visitors.[69] One mental health expert said, “When President [Barack] Obama was coming to Ghana in 2008, police rounded up persons with mental disabilities because they did not want him to see mad men.”[70]
Aisha, an articulate woman in her mid-50s, was taken to Mount Horeb Prayer Camp by her adult children because she was not sleeping at night, and she lived there for two months before Human Rights Watch met her. “I don’t want to be here even for one week,” she said, adding that she would prefer treatment in a psychiatric hospital, but camp administrators would not let her go.[71]
John, who had been living in Mount Horeb Prayer camp for two months, told Human Rights Watch, “I want to go home, but they don’t discharge me, and they don’t give me any reason.”[72]
Richard, an 18-year-old man who was brought to Edumfa Prayer Camp by the police, said that his mother “told police to arrest me as I was sleeping. I was handcuffed at 5 a.m. and brought here. They locked my leg in a chain.”[73]
Under the 2012 Mental Health Act, voluntary patients (people who go to a mental health facility on their own with or without referral) in psychiatric hospitals have a right to seek release by filling out a Discharge against Medical Advice Form (DMAF), a process they should not need to undergo because they had voluntarily admitted themselves for treatment. However, patients who are forcibly “committed” (taken to a facility for treatment without consent, such as by a family member or the police, or without a court order following the commission of a crime) to the hospital do not have such a right under both the prior 1972 Mental Health Law and the new 2012 Mental Health Act.[74] While discharge of voluntary patients against medical advice is allowed in Accra Psychiatric Hospital, a nurse at Pantang Psychiatric Hospital told Human Rights Watch that a doctor’s assessment is required for even voluntary patients to be discharged.[75] There are no such formal discharge procedures in the prayer camps that Human Rights Watch visited; people are allowed to leave only when the prophet considered them ready to be discharged. However, relatives of persons with mental disabilities admitted to prayer camps could ask for their discharge at any time.
The Constitution of Ghana prohibits deprivation of liberty except in circumstances permitted by law.[76] Among these circumstances, a person can be deprived of liberty if he is of “unsound mind … or a vagrant, for the purpose of his care or treatment or the protection of the community.”[77] Furthermore, under the 2012 Mental Health Act, a police officer can arrest a person who leaves a psychiatric facility without being discharged.[78] In cases where the person is not an imminent danger to herself or others, or is not detained because of pending criminal charges, or is not brought before a court, this may result in arbitrary and prolonged detention of persons with mental disabilities, in contravention of the African Charter on Human and Peoples Rights (ACHPR) and the UN Convention on the Rights of Persons with Disabilities (CRPD).
In the three public psychiatric hospitals, the majority of the staff said that involuntary admission, and subsequent continued detention, was not a violation of patients’ rights, and defended a paternalistic approach to psychiatric care that gives deference to health care providers to determine what is in the best interests of the patient.[79] Dr. Osei, head of Accra Psychiatric Hospital, told Human Rights Watch, “Involuntary admission is good because the state is exercising its mandate to protect someone, their family, the public, and property.”[80] This is not a violation of rights, he added. “Sometimes it’s wrong to defend rights without looking at the broader picture.”[81]
Prolonged Detention
I was tricked into coming here by my mother. I would never have accepted, but I have been here for more than one year.
—Raymond, 35-year-old man at Nyakumasi Prayer Camp, Central Region, January 2012
Some individuals, especially those taken to hospitals by police on court order, remained there even after discharge—often because they had been abandoned by families and could not return to their home communities.[82]
Bentil, a 26-year-old woman with schizophrenia, had been in Ankaful Psychiatric Hospital for four months and was cleared for discharge, but she was still there because she had nowhere to go.[83] “No one has come,” she said. “I want to go and stay at home.”[84] In Accra Psychiatric Hospital, Human Rights Watch saw a letter from a clan leader to hospital management requesting that his relative never be discharged, even when his condition improved.
Human Rights Watch learned that doctors in psychiatric hospitals met with patients in general wards every two weeks, in some cases resulting in long delays for discharge and prolonged detention.[85] Sarah, a woman who had voluntarily come to Pantang Psychiatric Hospital and was ready for discharge, said, “The nurses tell me a doctor will come and discharge me, but it is now two weeks and I have not seen any.”[86]
People also remained for long periods in prayer camps, where they told Human Rights Watch they wanted to leave and either go home or go to a psychiatric hospital, but they could not because their families refused or because the prayer camp leaders did not deem them fit to do so. John, for example, a person with a mental disability at Mount Horeb Prayer Camp, said that he was chained for one year without any treatment. He said: “I want to go home, but they don’t discharge me and they don’t give me any reason.”[87]
Most prayer camps that Human Rights Watch visited do not have formal criteria for determining that an individual is ready to leave. Instead, the prophet determines when people can leave, based on his assessment or “a message from God.”[88] According to one prophet, people are allowed to leave when they are “completely okay,” depending on “how someone speaks and what they do.”[89] Another religious leader told Human Rights Watch, “God shows a prophet a patient who has completely healed and he goes to the sanatorium to discharge such a person.”[90]
Conditions of Confinement
Overcrowding and Poor Hygiene
Overcrowding has long been a major problem in Ghana’s psychiatric hospitals and continues to be a problem at its largest hospital, Accra Psychiatric Hospital.[91] Intended to accommodate 600 patients,[92] it has, at times, housed up to 1200 patients, and had 900 patients in November 2011.[93] Lillian, a 41-year-old woman with schizophrenia, told Human Rights Watch, “Most of us don’t have beds. I sleep on a mat and I have no blanket.[94]
The ward for long-term patients at Pantang Psychiatric Hospital had 40 beds for 50 patients.[95] In the Special Ward at Accra Psychiatric Hospital, which houses people brought by police on court order, the situation was even worse. One nurse said, “We currently have 205 patients, and they have to share the 26 functional beds.”[96] As a result of overcrowding, patients sleep on thin mattresses, mats, or on the floor without a bed sheet.[97]
Overcrowding leads to a host of problems, such as supply shortages and health and sanitation hazards such as bed bug infestations and scabies.[98] In some wards in Accra and Pantang Psychiatric Hospitals, Human Rights Watch researchers saw toilets filled with feces and cockroaches.[99] From the gates of these wards, there was a powerful stench of urine and feces. “We experience shortages of basic items like gloves and detergents. Sometimes we don’t have water,” one nurse said.[100]
A nurse at Pantang Psychiatric Hospital told Human Rights Watch, “When we run out of protective gear such as gloves, we ask other patients to clean the ward.”[101] He added that this includes removing feces of other patients and using their bare hands to wash other residents, some of whom have open wounds.
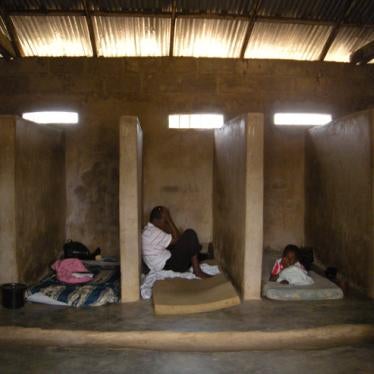
Some prayer camps also had overcrowded living quarters, where most people interviewed did not have mattresses, blankets, or mosquito nets. At Mount Horeb and Edumfa Prayer Camps, small rooms that could reasonably accommodate only about eight people had over twenty.[102] People spent all day and night chained in small, hot rooms of about six by four meters, with little to no ventilation.
Personal hygiene was also a major problem in most of the prayer camps visited by Human Rights Watch. In Mount Horeb and Edumfa Prayer Camps, individuals urinated and defecated in buckets in each room. While prayer camp administrators said they empty the buckets three times a day,[103] residents said that the buckets were emptied once daily, usually early in the morning, leaving a pungent odor in the room for most of the day.[104]
Peter, a 21-year-old man chained to a wall in Mount Horeb Prayer Camp, said, “You can’t have a good bath with a chain. We shit here and they don’t come to clean up.”[105] He added, “It smells a lot inside here. I don’t know when I will leave this place.”[106]
Abigail, a staff member and former resident of Mount Horeb Prayer Camp, said, “People who are aggressive or violent don’t get buckets because they have a tendency to throw the feces at each other.”[107] She added that instead they defecate on the ground near where they are chained.[108]
In Nyakumasi Prayer Camp most persons with mental disabilities were chained to trees in the compound, and they had to urinate in the open and defecate into small plastic bags, which were later thrown into surrounding vegetation. Those who were chained in stalls at Edumfa and Mount Horeb Prayer Camps had to shower in the stalls where they slept and ate. Aisha, a 56-year-old woman at Mount Horeb Prayer Camp, told Human Rights Watch, “I bathe only two times a week, but I want to bathe every day.”[109]
Chaining
I have been chained in one sitting position. I have been here for two years.
—Isaac, a 28-year-old man with schizophrenia, Nyakumasi Prayer Camp, Central Region, January 2012
In the prayer camps visited by Human Rights Watch, many of the patients were chained inside fully built and semi-permanent structures or chained to a tree or concrete floor outside until the pastor or prophet declared them “healed.”[110] There was no movement beyond the length of the chains—usually about two meters. People had to bathe, defecate, urinate, change sanitary towels, eat, and sleep on the spot where they were chained.
Approximately 20 men in Edumfa Prayer Camp were chained and confined in rooms locked with padlocks, even during the day. Kofi, an 18-year-old man, said, “Why do they keep this fasting room locked with padlocks during the day? Even if they treat us like criminals, serving sentences for the worst crimes, we deserve to see some daylight.”[111]
About 120 of the 135 individuals at the Mount Horeb Prayer Camp were chained 24 hours a day (there were only approximately 10 who were not chained during Human Rights Watch’s visit in January 2012). Some told researchers they had been restrained in chains for several months.[112] Human Rights Watch researchers found an individual chained in exactly the same spot where he had been interviewed, three months later.
Elijah was chained to a tree in an open compound at Nyakumasi Prayer Camp for over five months. While describing his experiences, the 25-year-old man said, “This chain is more than a death sentence. At night it gets too cold, when it rains you can’t run to a shade, and we have lots of mosquitoes.”[113]
Aisha, a 56-year-old woman at Mount Horeb Prayer Camp, told Human Rights Watch, “When I defecate in the bucket, it makes everyone in this room uncomfortable. Why chain me when I can walk and go to the toilet?”[114]
Prayer camp personnel consistently told Human Rights Watch they used such restraints because most people in the camp were aggressive or would otherwise try to escape. Prophet Paul Kweku Nii Okia, founder and director of Mount Horeb Prayer Camp, acknowledged that it was illegal to chain an individual, but he attributed the practice to a lack of better means of restraining persons with mental disabilities. He told Human Rights Watch that “if a person comes and he is very wild, there is no way to cool them down, so we have to chain them, with approval of their families.” He added, “The constitution [of Ghana] does not allow us to chain, but we do it with the consent of families.”[115]
Rev. Rebekah Bedford of Edumfa Prayer Camp said the camp’s lawyer advised them to ask family members to sign forms consenting to the chaining of their relatives. “Human rights people don’t agree with people being locked in chains. Because some illnesses are chronic and go on for as many as 15 years without healing, their families give consent.”[116] It should, however, be noted that consent of a relative to chain someone does not render the chaining legal.
The Constitution of Ghana guarantees freedom of movement and only permits restrictions to one’s movement in instances of lawful detention.[117] While it permits a person to enjoy, profess, and practice religion, such enjoyment must be within the limits of the constitution, which prohibits all practices that dehumanize or injure the physical and mental well-being of another person.[118] In the same regard, the 1960 Criminal Code Act makes assault (which includes imprisonment) a crime.[119] A person is considered to have imprisoned another person if,
[I]ntentionally and without a person’s consent, he/she detains another person in a particular place of whatever extent or character, whether enclosed or not, with the use of force or physical obstruction from escape; or compels him or causes him to be moved/carried to another direction.[120]
Forced Seclusion
I am praying to God never to go into seclusion again. There is no toilet, so you have to be there with the shit and urine, yet you eat there as well; they clean [the room] after you have left.
—John (pseudonym), a 37-year-old man with schizophrenia, Pantang Psychiatric Hospital, November 2011
Seclusion is one of the many forms of solitary confinement, which is defined by the United States’ Center for Medicare and Medicaid Services as the involuntary confinement of a patient alone in a room or area from which the patient is physically prevented from leaving.[121] The UN special rapporteur on torture regards any prolonged isolation of an inmate from others (except guards) for at least 22 hours a day as amounting to torture.[122]
In all three public psychiatric hospitals, Human Rights Watch found that people were isolated for varying periods, ranging from 24 hours to three days; some were given sedatives.[123] A nurse at Pantang Psychiatric Hospital said, “We use prolonged seclusion when an individual continuously refuses to take medication, is aggressive, restless, or is a danger to themselves, others, or the environment.”[124] A nurse at Accra Psychiatric Hospital said, “The seclusion rooms are in poor condition, the walls are not padded, and the lighting and ventilation is poor.”[125]
Harriet, a 25-year-old woman who was seven months pregnant, spent six months at Accra Psychiatric Hospital. While there, she was put in a seclusion room for 12 hours. She told us, “The seclusion room … always dirty, very dark and you would not go in without being beaten by nurses.”[126]
Staff in all three public psychiatric hospitals said they had no choice but to put people in seclusion or to administer sedatives to patients who are aggressive and thus a danger to themselves, nurses, and other patients.[127]
The former UN special rapporteur on torture clearly stated that seclusion or solitary confinement in psychiatric hospitals as a form of control or medical treatment “cannot be justified for therapeutic reasons, or as a form of punishment.”[128]
While the 2012 Mental Health Act limits the use of restraints on persons with mental disabilities, it does not abolish restraints completely. An act by one person to restrain another person is generally criminalized, and in such extreme instances where restraint is permitted, specific compliance criteria should be defined, including who has the authority to restrain another person. All acts of restraint that do not meet these criteria, for example assault or unlawful detention, clearly amount to a crime.
Lack of Shelter
In some wards in the three psychiatric hospitals visited by Human Rights Watch, especially Accra Psychiatric Hospital, shelter was inadequate.
At the Accra Psychiatric Hospital, several buildings lacked windows, doors, or shade during the day. Many had old and leaking roofing. Individuals were either crowded in the few spots where there was shade, or baked in the sun. No fewer than 50 individuals in the Special Ward slept outside.[129] A nurse explained, “Patients move in and out of these structures at any time, just as other potential threats like mosquitoes and reptiles move in.”[130]
Some of the rooms in the eight prayer camps that Human Rights Watch visited were only half-built; others had holes in the walls and roofs that would allow in rain, mosquitoes, and cold air at night. A few patients or their families had fashioned bamboo beds and grass-thatched shelters under a tree to get protection from the sun, but many slept on cold, hard concrete floors with no mattress or bedding.[131]
Denial of Food
I’m really, really hungry and they won’t feed me. I don’t understand…. Why can I not eat? They give me porridge at night, but that’s not enough food.[132]
—Afia, 32, Mount Horeb Prayer Camp, January 2012
Administrators and pastors of seven of the eight prayer camps that Human Rights Watch visited said they believed fasting was key to curing mental disability.[133] Doing so, they said, would starve evil spirits and cleanse them.[134] “Fasting helps weaken the demons, making it easier for the spirit of God to enter and do the healing,” one pastor said.[135]
Doris Appiah, national treasurer of the Ghana Mental Health Society and former resident of a prayer camp in Kumasi, told Human Rights Watch that some pastors use fasting as a means to force patients to confess past sinful acts, which are presumed to be responsible for their mental disabilities.[136]She explained that some pastors would beat them to confess that it was their sinful acts that led to their mental disabilities , and those who refused to confess would be forced to fast for up to four days.
When the camp did provide food, people with mental disabilities told Human Rights Watch that it was too meager—at times, just one meal a day.[137] Some pastors reported sharing the little food available on a day among all the patients, especially because some families did not provide food for their relatives, and camps did not have enough money to buy enough food for everyone.[138] Asked why the food was not enough, Prophet Winfred said, “Some people are brought here by police, with no relatives and yet they need to eat; some families are very poor and they can’t feed some people they bring for healing; therefore, we share the little food we have on a given day.[139] The expectation was that families would regularly bring food for relatives at the camps; pastors said this seldom happens. Many interviewees appeared undernourished and complained of hunger.
Prayer camps had different ways of funding their work. Edumfa Prayer Camp, for example, charged a registration fee of 5 Ghana Cedis (US$2.50) to everyone who visited the camp; some had residential facilities which they rented out, and others operated small businesses such as bakeries and shops selling herbal products.
Fasting schedules varied in each camp, depending on why a person was brought into a prayer camp and the prophet’s healing plan.[140] For example, Human Rights Watch found that some individuals in Mount Horeb, Edumfa, and Nyakumasi Prayer Camps were compelled to fast for 36 hours over 3 consecutive days in 12-hour stints from morning until dusk. Others, mainly the elderly, fasted from 6 a.m. until noon.[141] Such fasting regimes lasted from 7 to 40 days.[142]
People in the prayer camps had no choice but to fast as it was considered a mandatory component of the healing process. “I have never fasted in my life because I don’t see any value in it,” said Elijah, who lived in Nyakumasi Prayer Camp, “but here, it is a must.”[143]
Fasting had consequences for people with mental disabilities besides hunger, including being unable to take prescribed medication.[144] One person with bipolar disorder described his experience at the Victory Bible Church Camp: “I had to fast from morning to evening for two years. I wasn’t allowed to take my medication for the entire time.”[145]
In the one prayer camp where fasting was not allowed, the prophetess said, “I don’t let the mad people fast because when I give them medicine, they have to eat well.”[146] As part of her treatment regime, she distributed local herbs and homemade concoctions.
In psychiatric hospitals nurses said that people (especially those on medication) needed some food between 5 p.m. and 9 a.m. (between dinner and breakfast), which hospitals do not provide, and patients are supposed to buy from canteens. One nurse told Human Rights Watch, “Those brought by police usually come with no money and yet they need to eat something between meals; they become so aggressive when they are hungry, and we have nothing to do about it.[147]
Ghana is a state party to a number of international and regional treaties, including the International Covenant on Economic, Social and Cultural Rights (ICESCR), which require Ghana to respect and protect the right to food.[148] The Constitution of Ghana does not expressly recognize the right to food, neither does it provide for the right to health. It does, however, make provisions for the rights to life and adequate livelihood, which imply the right to food.[149]
Denial of Adequate Health Care
Access to health care for both physical and mental health problems was a major challenge for persons with mental disabilities in psychiatric hospitals, prayer camps, and the community.
Drug shortages bedevil all three public psychiatric hospitals in Ghana, mainly because of limited government supply, including medications for conditions such as malaria and skin infections.[150] Some patients in psychiatric hospitals needed alternative means of treatment that were either unavailable, or nurses did not have the proper skills to administer them.[151] Lillian said, “I get Largactil [a psychotropic drug], which I don’t like; doctors tell me I can’t get any other type [of medication], yet I get side effects like loss of sleep when I take it.”[152]
Persons with mental disabilities living within the community after having been discharged from mental health facilities also reported shortages of medications, generally provided to them by local NGOs. Suleiman Ayiku, an elderly man with bipolar disorder living in Greater Accra Region, told Human Rights Watch,
I get my drugs from BasicNeeds [a local mental health organization], but these run short, so I end up taking medications every three or four days as opposed to every day because I can’t afford buying the remainder [from a private pharmacy] to run me on a daily basis.[153]
Prayer camps that Human Rights Watch visited had varying policies and practices regarding the provision of adequate medical care for both mental health problems and other medical conditions. Some camps reportedly coordinate with nearby hospitals to ensure some medical care in the camps, and some take persons in severe mental health crises to the local hospital.[154] However, the frequency of visits by medical professionals is inadequate. For example, a psychiatric nurse who works at Tetteh Quarshie Memorial Hospital only visits Mount Horeb Prayer Camp once a month and must attend to both the physical and psychiatric health issues of the more than 100 individuals in the camp.[155] The nurse said, “We just sacrifice the services. The maximum I spend at Mount Horeb is two hours.”
In Edumfa and Charity prayer camps, management claimed to have a good working relationship with Ankaful Psychiatric Hospital and said it referred persons with serious mental health conditions to the hospital. However, hospital management said that camp officials are not cooperative and do not refer patients.[156] In other prayer camps, there was no arrangement whereby persons in the camps obtained professional psychiatric services.[157] According to Dr. Akwasi Osei, chief psychiatrist at Accra Psychiatric Hospital, “The main challenge is that [prayer camps] want a mutual referral of patients between prayer camp and institutions, which is not possible.”[158] He claimed that no doctors referred patients to prayer camps.[159]
Administrators of three camps said that they mainly give herbal concoctions to people who demonstrated aggressive behavior.[160] Some camp leaders said they had learned of the medicinal value of these herbs through a dream or vision.[161]
In Nyakumasi Prayer Camp, which housed about 30 persons with mental disabilities at the time of Human Rights Watch’s visit, the use of orthodox medicine was not permitted; people only had access to traditional medicines.[162]
Honorable Mubarak Muntaka, chairperson of the Health Committee of Ghana’s Parliament, told Human Rights Watch that parliament was currently reviewing legislation to improve regulations of health care professionals, health facilities, and traditional medicine practitioners.[163] The new Mental Health Service established under the 2012 Mental Health Act is charged with working with both non-orthodox service providers (such as prayer camps and traditional healers) and professional mental health providers to ensure effective monitoring of centers that provide services to persons with mental disabilities.[164]
The 2012 Mental Health Act also makes provision for the establishment of a visiting committee to conduct inspections of facilities and centers that provide services to persons with mental disabilities.[165] However, it is unclear how this committee will address human rights violations in prayer camps or manage a regular schedule for inspection given that there are so many camps, including those that are not registered with the government. Implementation of the Mental Health Act is, however, dependent on the passage of a legislative instrument to guide that implementation, which at the time of writing had not yet been passed.
Involuntary Treatment
I receive medication twice a day, and I only take it because it is the rule. If I don’t take it, they will give me an injection.
—Lillian, a woman with schizophrenia, Accra Psychiatric Hospital, November 2011
Some of those interviewed by Human Rights Watch in psychiatric hospitals said that they were forced to take medication against their will. Sarah, a 25-year-old primary school teacher who voluntarily checked herself into Pantang Psychiatric Hospital, said, “Taking medication is compulsory here. I take it because I wouldn’t want to be coerced again.”[166]
Staff at all three public psychiatric hospitals admitted that they use force in different ways, from physical coercion to, in extreme cases, involuntary sedation via injection.[167] One nurse said, “We request them kindly to take the medication and when they refuse, we hold them and force the drug into their mouth.”[168] Nurses and individuals in the hospitals also said that if someone resisted medication, it was sometimes hidden in food.[169]
In some cases, patients were forced to take medication, even when they said it failed to work or produced serious side effects.[170] Peace told Human Rights Watch, “I don’t like the medicine I receive; the drugs cause my legs to swell, eye pains, and insomnia.”[171]
Persons with mental disabilities in psychiatric institutions and prayer camps, as well as hospital and camp staff, reported that family members or staff routinely decided on a person’s admission to, treatment within, and discharge from mental health facilities even when they voluntarily brought themselves to such facilities, effectively denying them their legal capacity to make their own decisions.[172]
In prayer camps, herbal concoctions are commonly administered to persons with mental disabilities without any explanation or consent.[173] The herbs are mixed with water and either administered in drops through the nose, smeared over the body, or given to them to drink.[174]
Doris Appiah, treasurer of the Mental Health Society of Ghana and former resident at a prayer camp in Kumasi, told Human Rights Watch, “I was given herbs in the nose and forced to drink some. I didn’t like them because they were bitter and had terrible side effects. My tongue swelled and came out [of her mouth].”[175]
The former UN special rapporteur on torture, Manfred Nowak, in his 2008 interim report, observed that forced and non-consensual administration of psychiatric drugs, particularly neuroleptics, for treating a mental condition needs to be closely scrutinized.[176] Depending on the circumstances of the case, the suffering inflicted and the effects upon the individual’s health may constitute a form of torture or ill-treatment.[177]He added that,
[The] suffering inflicted should be assessed with reference to the patient’s subjective experience or display of fear and terror, grief, and disturbing sensations of body and mind produced by the drugs, and long-term consequences such as traumatic reactions and the loss of significant relationships and opportunities.[178]
Nowak further said “protocols for informed consent need to be developed to ensure that accurate and unbiased information is provided to individuals who are considering treatment with psychiatric drugs, including information about less intrusive alternatives.”[179]
In situations where a person cannot give consent to admission or treatment at that moment, and their health is in such a state that if treatment is not given immediately, their life is exposed to imminent danger, immediate medical attention may be given in the same manner it would be given to any other patient with a life threatening condition who is incapable of consenting to treatment at that moment.[180]
It therefore follows that separate standards should not be set for persons with mental disabilities. Special measures should be in place to ensure that a person in such a situation is given the earliest opportunity to consent to treatment as soon as they attain or regain a status capable of doing so.[181] In instances where States P arties employ preventative detention measures to protect a person with a disability or society from imminent danger, the basis for such detention should not hinge upon his or her disability, but rather his or her behavior.[182] Even then, there needs to be clearly defined rules premised on the side of capacity and avoidance of harm, and these rules need to be enforced.[183]
The Criminal Code Act (as amended) permits a guardian of a person with a mental disability to “consent to the use of force against a person for purposes of medical or surgical treatment, or otherwise for his benefit.”[184] This and other relevant laws must be amended in order to comply with the CRPD.
Stigma and Its Consequences
Life negatively changes as soon as people know that you have a mental disability. That’s why we hide it.
—Dora Ashong, 43-year-old woman with a mental disability who is a disability advocate, Accra, Greater Accra Region, January 2012
Persons with mental disabilities in Ghana experience stigma and discrimination in the health sector, at home, and in the community. Religious leaders often described them as incapable, hostile, demonic, evil, controlled by spirits, useless, and anti-social.[185] “It is a real challenge to persuade the public that mental disability is not a spiritual crisis, but a medical condition,” one religious leader said.[186]
Bernard, a 49-year-old man with schizophrenia who has received mental health treatment since 1982, told Human Rights Watch,
The stigma is too much. When you go to Accra Psychiatric Hospital, it is like you are not a human being. Families don’t have anything to do with you anymore; they don’t need you no matter how brilliant you are … my elder brother still insults me; he says my friends are also mad because they go to church with me; and because of this, when I speak, my siblings don’t listen to me.[187]
One significant consequence of such stigma is that relatives abandon persons with mental disabilities in psychiatric hospitals and prayer camps.[188] Many family members do not visit, do not pick up relatives after discharge, and even give a false address so they cannot be traced.[189]
Stigma also deters persons with mental disabilities from seeking professional support in psychiatric hospitals. Bernard told Human Rights Watch, “People look down upon you; those who know you will not want you to speak in society. That’s why I go to Meprobi general clinic and not a psychiatric hospital.”[190]
Nearly all persons with mental disabilities with whom we spoke identified stigma in their families as one of their main worries about being discharged from a psychiatric hospital or prayer camp. Some also expressed fears of hostility when they go back to their respective communities. Peace, a 55-year-old woman with bipolar disorder at Ankaful Psychiatric Hospital, said,
For the two months I have been here, my family has informed people, and I don’t know how harsh they are going to treat me. No matter what you do, they say, ‘After all, you have been at a mental hospital.’ That’s why when I left Ankaful Psychiatric Hospital last time, I went to a hotel and not home.[191]
As a result, some people even opted to live in institutions or prayer camps, where they were not questioned about their mental health status and where their conditions were better understood. Describing the stigma faced after being discharged from a psychiatric hospital, one woman said, “As a patient, you have to struggle with very low self-esteem and also have to fight with negative attitudes from society … it is like a death sentence.”[192]
Some family members also considered mental disability as a disgrace to the family.[193] Even family members face discrimination from community members and fear ostracism. For example, John Kwabena, brother to a woman with a mental disability said, “People don’t want to marry into a family where there is someone with a mental disability.”[194]
Nurses working in psychiatric institutions also reported experiencing stigma in their home communities, where they said people considered nurses to be “mentally ill” since they work with persons with mental disabilities. “They think we are also like our patients,” a nurse at Ankaful Psychiatric Hospital said.[195] Psychiatric nurses and doctors are stigmatized even among their peers. A nurse who works in a psychiatric unit of a general district hospital said that her colleagues at the hospital call her abodamness, which means “craziness.”[196] Indeed, stigma against psychiatrists is so strong that many medical students opt for other specialties.[197] Dr. Anan, head of Ankaful Psychiatric Hospital, said it took him over 15 years to enter the psychiatric field because of the related stigma.[198]
Some religious leaders attributed stigma to the lack of community awareness. Robert Amo, director of programs and advocacy, Christian Council of Ghana (CCG), said, “Citizens are not well informed about mental disability.”[199]
The government of Ghana has done little to minimize the effects of stigma endured by persons with mental disabilities, their caregivers, and the medical staff who treat them. While there is scattered information about mental disabilities on the radio, television, and in newspapers, the government does not have a systematic plan to address this challenge.
Gifty Anti, a senior presenter at Ghana Broadcasting Corporation, explained her experience covering mental health issues. She said,
Media coverage of mental health issues is nothing near good; in fact, on a scale of ten, it is about three if not less. It only comes up when an event surfaces. I try to invite both survivors and service providers, but they fear to come to TV shows because of the stigma. They say that when they appear on TV programs, stigma increases.
Physical and Verbal Abuse
Human Rights Watch documented severe cases of physical and verbal abuse of persons with mental disabilities in the family, community, and hospitals and prayer camps.
Abuse from family members is especially acute. Sarah, a 25-year-old primary teacher who voluntarily checked herself into Pantang Psychiatric Hospital, told Human Rights Watch, “Whenever I get hallucinations, I expect to be beaten. I got this scar when my brother beat me because I had refused to go to the family house.”[200] Aisha, a 57-year-old woman at Mount Horeb Prayer Camp, told Human Rights Watch, “Three months prior to coming to this prayer camp, my brother beat me, and my skin color changed.”[201]
In the three public psychiatric hospitals, three patients reported being beaten by nurses when they did not take their medication or follow hospital rules.[202] Michael, a 38-year-old man with schizophrenia at Pantang Psychiatric Hospital said, “We are beaten by the security men and the male nurses. They beat me when I tried to escape from the ward.”[203] Harriet, the pregnant woman at Ankaful Psychiatric Hospital, told Human Rights Watch that nurses threatened physical abuse. She said, “Yesterday they were drawing blood from me and I was feeling a lot of pain and I said, ‘You are killing me’; the nurse said ‘if you shout again, I will put the needle in your mouth.’”[204]
One nurse explained that some patients are at times aggressive and assault the staff, so nurses beat them in self-defense.[205] One former patient of Accra Psychiatric Hospital told Human Rights Watch, “I saw some people being beaten like animals. Those who failed to follow the instructions of nurses, they would beat them mercilessly. Whenever I saw this, it would frighten me.”[206]
Ghana’s domestic laws, such as the Criminal Code Act of Ghana, criminalize all forms of assault and battery.[207] Human Rights Watch attempted to obtain data from the hospitals, the Attorney General’s Office, the chief psychiatrist for the Ghana Health Service, and the Ministry of Justice about any ongoing or previous allegations, investigations, or prosecutions of staff at hospitals or prayer camps for assault against persons with mental disabilities. However, at the time of writing, we had not yet heard a response from some of the authorities.[208]
In his response, Dr. Akwasi Osei, Chief Psychiatrist, Ghana Health Service, attributed the reported abuses to the fact that the old mental health law did not make provisions for patients to challenge involuntary admission and treatment in psychiatric facilities.[209] He added that this made it difficult for people who were not admitted under court order to challenge such admission especially because the old law required consent of a caregiver or relative.
As noted earlier, the new Mental Health Act now establishes a tribunal and an appeal procedure which seeks to address this. It remains to be seen how structures will be set up to ensure that persons with mental disabilities can challenge both admission and treatment against their will.
Electroconvulsive Therapy
Psychiatrists in Ghana continue to use electroconvulsive therapy (ECT), a method of treatment which involves passing electricity through one’s brain, to treat persons with severe depression.[210] Dr. Akwasi Osei, chief psychiatrist for the Ghana Mental Health Service and head of Accra Psychiatric Hospital, explained the process of administering the electroshocks:
We don’t give anesthesia because we don’t have a machine and personnel. ECT is a little uncomfortable, but it gets better. Some patients get four to six shocks, two or three times a week and not more because it can lead to permanent memory loss.[211]
Former UN special rapporteur on torture, Manfred Nowak, has noted that unmodified ECT (without anesthesia, muscle relaxant, or oxygenation) is an unacceptable medical practice that may constitute torture or ill-treatment, as it may cause adverse effects such as cognitive deficits and loss of memory.[212]
Nowak concludes that, even in its modified form (where seizure is not induced by the maximum dose of electrical charge),[213] “it is of vital importance that ECT be administered only with the free and informed consent of the person concerned, including on the basis of information on the secondary effects and related risks such as heart complications, confusion, loss of memory and even death.”[214] Like those who have undergone unmodified ECT, survivors of the modified form in different parts of the world have found severe and permanent memory loss devastating to personal identity.[215]
Dr. Osei told Human Rights Watch that before treatment is administered, the patient’s consent is sought. In cases where hospital staff deem patients incapable of giving their informed consent, family members (if they are accompanied) consent on their behalf; unaccompanied patients are treated without consent.[216]
The 2012 Mental Health Act offers some protection against involuntary admission and treatment, although it is not absolute. While the act creates a mechanism through which someone who is involuntarily admitted and given treatment can challenge both admission and treatment, some of the circumstances under which such admission and treatment is permitted are susceptible to abuse; for example, the act allows for involuntary admission and treatment where the person’s condition is deemed as expected to deteriorate. While the act empowers a patient or primary caregiver to appeal involuntary admission or treatment, it still remains to be seen how persons with mental disabilities seeking to challenge admission and treatment will be supported by the state to ensure effective implementation of the law, including access to courts, as well as the enjoyment of rights by persons with mental disabilities.
The act makes provision for appointment of a guardian with full powers to make decisions on behalf of an individual, as opposed to a support person, on the basis that a person for whom a guardian is appointed is presumed, by a clinical team of mental health professionals, as lacking capacity. The retention, in the 2012 Mental Health Act, of guardians making decisions rather than moving towards assisted decision-making for persons with disabilities violates the CRPD. Although criminal statutes outlawing assault might, in theory, be used to prosecute instances of forced treatment, it was unclear at the time of writing whether authorities had ever pursued criminal charges against psychiatric hospital staff for use of ECT.[217] Ghana therefore needs to align provisions of the mental health law with the CRPD and create a system through which the laws can be implemented, including access to legal aid.
Violations against Children with Disabilities
Children with mental disabilities experienced similar conditions to adults in psychiatric hospitals and prayer camps. Some children that Human Rights Watch saw in Accra Psychiatric Hospital had multiple disabilities, which exacerbated their vulnerability to human rights violations.
Despite its name, the Children’s Ward at Accra Psychiatric Hospital houses people ranging from 14 to 40 years of age. At the time researchers visited, there were 22 patients; 13 of them were brought by their parents, the majority of whom never visited.[218] Almost half of the patients in the Children’s Ward were actually adults; those younger than 18 ranged in age from 12 to 17. A nurse said that some of the adults had been in the ward since 1980.[219]
Most patients in the ward have been diagnosed with mania, epilepsy, or intellectual disabilities such as Down syndrome. In only a few cases had children had been diagnosed with bipolar disorder or schizophrenia.[220]
The staff shortage was particularly pernicious in the Children’s Ward, given the complex needs of the people kept there. The ward has five morning staff, fewer than five staff in the afternoon, and only two staff at night. A nurse in the ward said, “It is harder at night since most of the children and individuals don’t sleep.”[221] People in the Children’s Ward received medication, but not all who did so needed it. According to one nurse,
While no one on current admission has a psychiatric condition, some of them receive psychotropic drugs because they are so restless. We don’t have access to alternative services that would stimulate these children. In any case, we lack the necessary skills to handle children with intellectual disabilities since we [were] train[ed] to deal with psychotic adult cases.[222]
Dormitories in the ward were dirty, and patients slept on thin mattresses on the floor. At the time of Human Rights Watch’s visit, some children and adults were lying down naked next to their feces. The nurse said they had reacted negatively to their prescribed medicines.[223]
In the prayer camps visited by Human Rights Watch, the situation was even worse for children, who were subjected to restraints and other abuses. Victoria, a 10-year-old girl, shoeless and covered with dirt, had been chained to a tree at Nyakumasi Prayer Camp.[224] She had a serious skin disorder with crusting and bumps on both arms. When asked about this condition, the prophet said it was up to Victoria’s mother to buy medication.[225] Children in prayer camps were subjected to the same regime of fasting as adults and they were chained in the same conditions. These conditions were particularly difficult since some rooms were noisy and some adults would sometimes strip naked.
Ghana’s constitution expressly prohibits subjecting a child to torture or other cruel, inhuman, or degrading treatment or punishment.[226] It also prohibits depriving a child of medical and other benefits on the basis of religious or other beliefs.[227] The constitution empowers parliament to enact laws to ensure that every child, regardless of disability, has a right to the same measures of special care, assistance, and maintenance as is necessary for their development.[228]
The 1998 Children’s Act prohibits discrimination against a child on the grounds of disability or health status, among others,[229] and guarantees the best interest of the child in any matter concerning his or her welfare.[230] The act further prohibits treating a child with a disability in a non-dignified manner and entitles children to a right to special care that can develop their maximum potential and self-reliance.[231]
III. Legal Framework
Ghana is obligated to respect the rights of persons with disabilities under international and regional laws, the national constitution, and other domestic legislation. Despite these legal provisions, it has done little to ensure that protections are in place and enforced.
Key International and Regional Obligations
Ghana is a party to the International Covenant on Civil and Political Rights (ICCPR),[232] the International Covenant on Economic, Social and Cultural Rights (ICESCR),[233] the Convention on the Elimination of Discrimination against Women (CEDAW),[234] Convention against Torture and Other Cruel Inhuman or Degrading Treatment or Punishment (Convention against Torture),[235] and the Convention on the Rights of the Child (CRC).[236] Ghana ratified the Convention on the Rights of Persons with Disabilities (CRPD) and its Optional Protocol.[237] The CRPD makes explicit that the human rights enumerated in other major human rights documents apply with equal force and in particularly important ways to individuals with disabilities.
Ghana is a State Party to several regional instruments, including the African Charter on Human and Peoples’ Rights (ACHPR)[238] and the Protocol to the African Charter on Human and Peoples' Rights on the Rights of Women in Africa (the Maputo Protocol).[239] Ghana has also signed the African Charter on the Rights and Welfare of the Child (ACRWC).[240]
Right to Non-Discrimination
The ICESCR, ICCPR, CEDAW, CRC, CRPD, and the ACHPR expressly prohibit discrimination and require States Parties to take steps to eliminate all forms of discrimination against an individual, including persons with disabilities.[241]
Non-discrimination is one of the cardinal principles upon which the CRPD is grounded.[242] The CRPD sets minimum guiding standards to States Parties on how to realize equality and non-discrimination, including by recognizing that all persons are equal before and under the law and are entitled without discrimination to the equal protection and equal benefit of the law.[243]
Freedom from Torture or Cruel, Inhuman, or Degrading Treatment or Punishment and Right to Protection of Personal, Mental, and Physical Integrity
The ICCPR, CRC, CRPD and African Charter all prohibit subjecting any person to torture or to cruel, inhuman, or degrading treatment or punishment, including non-consensual medical or scientific experimentation.[244]
The Convention against Torture defines torture as “any act by which severe pain or suffering, whether physical or mental, is intentionally inflicted on a person for such purposes as … intimidating or coercing him or a third person, or for any reason based on discrimination of any kind.” Cruel, inhuman, or degrading treatment or punishment is defined as those acts that cause grievous harm but do not amount to torture.[245] In either case, the pain, suffering, or harm must be instigated with the consent or acquiescence of a public official or other person acting in an official capacity.[246]
The prohibition against torture or cruel, inhuman, or degrading treatment “relates not only to public officials, such as law enforcement agents in the strictest sense, but may apply to doctors, health professionals and social workers, including those working in private hospitals, other institutions and detention centers.”[247] Governments are required to “prevent, investigate, prosecute and punish such non-State officials or private actors.”[248]
The African Commission held in Civil Liberties Organization v. Nigeria that “deprivation of light, insufficient food and lack of access to medicine or medical care also constitute violations of article 5 of the African Charter [on respect for inherent dignity and freedom from torture].”[249]Both the CRPD and the African Charter recognize the right to respect for physical and mental integrity.[250]
Right to Liberty and Security of the Person
The right to protection from arbitrary detention is contained in article 9 of the ICCPR, article 6 of the ACHPR, and article 14 of the CRPD. Article 9 of the ICCPR states, “No one shall be subjected to arbitrary arrest or detention” and “no one shall be deprived of his liberty except on such grounds and in accordance with such procedures as are established by law.” [251]
Article 9 also mandates that an individual have the opportunity to challenge his or her detention, such that “[a]nyone who is deprived of his liberty by arrest or detention shall be entitled to take proceedings before a court, in order that that court may decide without delay on the lawfulness of his detention and order his release if the detention is not lawful.” [252]
According to the UN Human Rights Committee, these provisions apply not only to those accused of crimes, but also “to all persons deprived of their liberty by arrest or detention” including those detained because of, “for example, mental health difficulties, vagrancy, drug addiction, immigration control, etc.” [253]
Article 14 of the CPRD, however, provides even greater protections against deprivations of liberty to persons with disabilities. Article 14 not only forbids arbitrary detention but also states that detention cannot be justified on the basis of the existence of a disability. [254] There should therefore be some basis underlying the deprivation of liberty that does not discriminate based on disability.
Article 14 of the CRPD thus goes further than the previous regime of arbitrary detention enumerated in article 9 of the ICCPR. For states that have ratified the CRPD, article 14 sets the higher standard with respect to safeguards against detention than its equivalent provision in the ICCPR and should be applied under the doctrine that the combined effect of any treaties or domestic norms should be interpreted so as to offer the greatest protection to the individual. [255]
According to article 6 of the ACHPR, every individual has the right to liberty and to the security of his person, and state cannot deprive individuals of freedom except for reasons and conditions previously laid down by law; but in any case, no one may be arbitrarily arrested or detained.[256]
While interpreting the foregoing article, the African Commission on Human and Peoples Rights held in the case of Prohit & Moore v. The Gambia that “article 6 does not mean that any domestic law may justify the deprivation of such persons’ freedom and neither can a State party to the African Charter avoid its responsibilities by recourse to the limitations and claw back clauses in the African Charter.”[257] The Commission emphasized that the phrase “every individual” includes a person with a disability.[258]
Manfred Nowak, the former special rapporteur on torture, noted that,
In certain cases, arbitrary or unlawful deprivation of liberty based on the existence of a disability might also inflict severe pain or suffering on the individual, thus falling under the scope of the Convention against Torture. When assessing the pain inflicted by deprivation of liberty, the length of institutionalization, the conditions of detention and the treatment inflicted must be taken into account.[259]
Right to Equal Recognition before the Law
The CRPD obligates States Parties to recognize persons with disabilities as persons before the law who enjoy legal capacity on an equal basis with others.[260] Legal capacity can be described as “a person's power or possibility to act within the framework of the legal system. Legal capacity describes the rights and status of a person and is not connected with cognitive competence.”[261]
According to Gerard Quinn, a prominent disability rights expert and director of the Centre for Disability Law and Policy at the NUI Galway School of Law, legal capacity is “the essence of being human and transcends decision-making.”[262] Legal capacity underpins the principle that medical interventions must be based on free and informed consent.[263] The special rapporteur on torture noted in his report that discriminatory legislative frameworks and practices such as laws that deprive persons with disabilities of their legal capacity enhance violence against persons with disabilities.[264]
The CRPD further obligates States Parties to provide such support as may be needed to exercise one’s legal capacity.[265] Supported decision-making “is a framework within which a person with a disability can be assisted to make valid decisions. The key concepts are empowerment, choice, control and responsibility.”[266] Supported decision-making may take many forms:
Those assisting a person may communicate the individual’s intentions to others or help him/her understand the choices at hand. They may help others to realize that a person with significant disabilities is also a person with a history, interests and aims in life, and is someone capable of exercising his/her legal capacity.[267]
Right to Live in the Community
The CRPD recognizes the equal right of all persons with disabilities to live in the community, with choices equal to others.[268] The CRPD thus requires governments to allow persons with disabilities to choose their place of residence and with whom they live, provide access to a range of in-home, residential, and other community support services, including personal assistance, and ensure that community services and facilities are responsive to their needs.[269]
In this regard, states should facilitate the right to live in the community by offering “a range of in home, residential and other community support services, including personal assistance necessary to support living and inclusion in the community, and to prevent isolation or segregation from the community.”[270] States should also respect an individual’s right to privacy in any type of living situation.[271] While full realization of this right is subject to available resources, a state should nevertheless undertake the steps necessary towards its realization.
According to the Office of the High Commissioner for Human Rights (OHCHR’s) national implementation criteria for the CRPD, parties to the CRPD need to shift social service systems for persons with disabilities away from those focused on institutional care towards a system of community-based support services, including housing.[272]
Freedom from Exploitation, Violence, and Abuse
Both the African Charter and the CRPD prohibit all forms of exploitation, violence, and abuse.[273] Furthermore, the CRPD requires that “all facilities and programs designed to serve persons with disabilities are effectively monitored by independent authorities.”[274]
States Parties to the CRPD are required to take all appropriate measures to promote the physical, cognitive, and psychological recovery, rehabilitation, and social reintegration of persons with disabilities who become victims of any form of exploitation, violence, or abuse.[275]
Right to Health
The highest attainable standard of health is a fundamental human right enshrined in numerous international and regional instruments, including the Universal Declaration of Human Rights (UDHR), the ICESCR, CRC, CEDAW, CRPD, ACHPR, and ACRWC.[276]
According to the Committee on Economic, Social and Cultural Rights, which monitors implementation of the ICESCR, access to health services should be based on non-discrimination, especially for “the most vulnerable or marginalized sections of the population, including individuals with disabilities.”[277] Physical accessibility requires that health facilities, goods, and services be within safe physical reach, mandating equitable distribution of health facilities and personnel within the country, even in rural areas.[278] The CRPD further requires that health information be accessible to persons with disabilities.
The African Charter further calls on States Parties to take special measures to address the needs of older persons and persons with disabilities.[279] In a 2008 landmark case of Purohit and Moore v. The Gambia, the African Commission held that “mental health patients should be accorded special treatment which would enable them to not only attain but also sustain their optimum level of independence.”[280]
Rights of Children with Disabilities
Children with disabilities enjoy all the rights enumerated in the numerous international and regional instruments discussed in this section.[281] Indeed, all children are, “by reason of [their] physical and mental immaturity,” in need of “special safeguards and care, including appropriate legal protection.”[282]
In light of these heightened requirements, the CRC requires States Parties to recognize “that a mentally or physically disabled child should enjoy a full and decent life, in conditions which ensure dignity, promote self-reliance, and facilitate the child’s active participation in the community,” and that appropriate assistance—including education, training, health care services, rehabilitation services, and recreation opportunities—for children with disabilities shall be provided free of charge whenever possible.[283] The CRC also requires institutions, services, and facilities responsible for the care or protection of children to conform to standards in the areas of safety, health, the number and suitability of staff, and competent supervision.[284]
In addition, the African Charter on the Rights and Welfare of the Child (ACRWC)[285] specifically calls for special measures to ensure protection of children with mental or physical disabilities under conditions that respect a child’s dignity, self-reliance, and active participation in the community.[286]
Ghanaian National Laws and Policies
The Constitution of Ghana guarantees fundamental rights to persons with disabilities and prohibits discrimination and exploitation.[287] Specific disability laws have also been adopted, but such laws either do not meet international standards or are not rigorously implemented.
The Constitution of Ghana provides for equality of every person before the law and prohibits all forms of discrimination.[288] The constitution, however, restricts rights of persons considered to be of “unsound mind” in a number of aspects.[289] The constitution also permits limitations on liberty for persons of “unsound mind.”[290] The term “unsound mind,” however, is not defined.
General Disability Laws and Policies
The 2006 Persons with Disability Act No. 715 recognizes a series of rights, including the right to family life, access to public life, education, health, and employment. The act mainly addresses matters relating to physical access to services with no mention of core rights relevant to persons with mental disabilities. The act also creates a National Council on Persons with Disability (NCPD) specifically mandated to monitor and evaluate disability policies and programs, formulate strategies for implementation of the national disability policy, advise the Ministry of Social Welfare on disability issues, and submit to the minister proposals for appropriate legislation on disability.[291]
Ghana’s 2000 National Disability Policy aims to remove barriers related to the employment, education, transportation, and health care of persons with disabilities.[292] The policy requiresthe Ministry of Health to provide “free general and specialist medical care, rehabilitative operation treatment and appropriate assistance for persons with total disability, and also include the study of disability and disability-related issues in the training institutions for health professionals.”[293]
While the policy targets persons with disabilities generally, strategies and projects do not include persons with mental disabilities. A senior official in the Ministry of Employment and Social Welfare told Human Rights Watch that the department does not handle issues of persons with mental disabilities since this falls under the Ministry of Health.[294]
Mental Health Laws and Policies
In March 2012 the parliament of Ghana passed into law a new Mental Health Act (Act 846) which regulates all matters concerning persons with mental disabilities, including women and children.[295] The law introduces a number of initiatives, such as the establishment of a Mental Health Service, whose objective is to “promot[e] mental health and to provide humane care in a least restrictive environment … at primary health care level.”[296] The act also establishes visiting committees at regional and district levels to ensure mental health laws are implemented through periodic inspection and inquiries about patient complaints.[297] It also provides for admission to, treatment within, and discharge from public psychiatric hospitals, and it creates a mental health review tribunal mandated to investigate complaints of persons in psychiatric hospitals, including cases of involuntary admission and treatment, as well as an appeal process against the decisions of the tribunal. [298]
As noted earlier, the 2012 Mental Health Act still conflicts with the CRPD in several aspects. The law, for example, authorizes arbitrary use of intrusive and irreversible treatment. It also permits involuntary admission and treatment, without giving any guidelines on how persons with mental disabilities will access courts of law to challenge such acts. The Mental Health Act also presumes the incapacity of some persons with mental disabilities, limiting their ability to make decisions about where they live and what treatment they receive. The act does not effectively provide a framework for supported decision-making, as envisioned by the CRPD.[299]
Anticipating passage of the Mental Health Act, Ghana’s former President John Evans Atta Mills pledged that the government would adopt a community mental health care strategy and the necessary regulations to implement the act.[300]
There are a few other bills in parliament that may contribute to improving the welfare of persons with mental disabilities, mainly the Health Institutions and Management Bill that seeks to regulate public and private facilities and will regulate prayer camps once enacted into law. It remains to be seen how this bill will be implemented once it passes into law.
IV. International Partners
International partners, including development agencies and international NGOs working in Ghana, are well placed to assist Ghana’s government in respecting, protecting, and fulfilling the rights of persons with mental disabilities. These entities are in a position to engage with the government to develop and fund inclusive policies and programs.
As of 2008, development assistance funded nearly 15 percent of Ghana’s health budget.[301] International development agencies should ensure that their development assistance strategies and policies conform with the principles of non-discrimination, inclusion, and equality articulated in the Convention on the Rights of Persons with Disabilities and other treaties.
International partners including the World Bank, World Health Organization (WHO), the United States Agency for International Development (USAID), United Nations Children Fund (UNICEF), Japanese International Cooperation Agency (JICA), Department for International Development (DFID), Danish International Development Agency (DANIDA), the European Community (EC), and Australian Agency for International Development (AusAID) have broadly contributed to several development projects in Ghana, especially in the health sector, but despite the prevalence of mental disabilities, few of these partners have invested in mental health.
Over the years, WHO has funded the integration of mental health into the public health program, the training of primary care workers, the provision of motorcycles for the community psychiatric program, the support of awareness programs, and funding for training of volunteers and providers at the sub-district level.[302]
In the 2008-2011 Ghana Cooperation Strategy, WHO supported processes leading to the enactment of the 2012 Mental Health Act.[303] The Strategy noted that, “in addition to the lack of access to care, there are issues of serious human rights violations against persons with mental disorders.”[304]
World Bank disability-related projects focus on support for inclusive education and a school for the deaf.[305] Dante Ariel Mossi, senior country officer, explained, “We have not yet done anything in the field of mental health. Ghana is a young country, and there are so many issues which are not yet covered.”[306] He added, “However, vocalizing our action into policy is critical, [including] through support to families with members with mental disabilities and ensuring budgetary allocations.”[307] In the health sector, the World Bank has been involved in discussions aimed at improving the national health insurance scheme to ensure that it expands to cover more vulnerable groups.[308]
DFID funds the Mental Health and Poverty Project, a research consortium with partners in Ghana, South Africa, Zambia, and Uganda.[309] Through this project, a comparative critique of national mental health policy has been carried out with recommendations on areas requiring change and lessons to learn from each country.
UNICEF’s work in Ghana has mainly focused on prevention-related initiatives especially against polio. They do not have a targeted program for children with mental disabilities in Ghana, although they are now planning to support implementation of the Mental Health Act.[310]
From the above, it is clear that there are a number of international partners working in Ghana, but mental health programs seem to be very limited. There is need for Ghana’s international partners to restructure their programs to ensure that disability becomes a critical part of their development initiatives in Ghana.
International partners are also better placed to influence Ghana’s health budget through directly committing resources to mental health care and also encouraging the government to increase allocation of funds to mental health care in its health budget.
V. Conclusion
The Ghanaian government is taking steps to improve the rights of persons with mental disabilities, including by recently passing the 2012 Mental Health Act.
However, the new act continues to violate Ghana’s obligations under the CRPD because it retains provisions on involuntary admission and treatment, including the use of intrusive and irreversible treatment methods, provides for guardianship as opposed to supported decision-making, and does not provide adequate regulation of non-orthodox mental health service providers, including prayer camps.
In addition, much more still needs to be done to ensure dignified living conditions in psychiatric hospitals and prayer camps, to provide access to appropriate mental health care based on principles of free and informed consent, and to end unlawful and inhumane practices such as forced detention, chaining, forced fasting, and denial of access to medical services.
To realize the rights of persons with mental disabilities in Ghana, the government, development agencies, health care providers, and citizens should support their transition from institutions to independent community living, with access to community-based mental health services and support services as and when they may be needed.
It is critical that relevant evidence-based information is gathered to guide the formulation and implementation of a locally feasible and sustainable plan. Providing adequate health care to persons with mental disabilities also requires the inclusion and active participation of individuals in psychiatric hospitals and prayer camps, family members, social workers, health service providers, counselors, and law and order enforcement agencies.
The government should increase available mental health care services across the country, including by opening psychiatric units in regional and district hospitals. In the short term, the government needs to increase and train all staff about the newly ratified CRPD and improve infrastructure and equipment in these facilities.
Religious leaders have a critical role to play in ensuring respect for the rights and dignity of persons with mental disabilities. They can greatly contribute to reducing stigma surrounding mental disability and increasing community acceptance of persons with disabilities. This should include publicly denouncing inhumane practices, like chaining in prayer camps, and monitoring the practices of their members who render services to persons with mental disabilities, mainly in prayer camps.
In the same regard, police and local authorities should continuously visit centers where persons with mental disabilities are detained, including prayer camps, and take action against unlawful acts like chaining, arbitrary detention, torture and other physical or mental abuse, and the act of compelling people with mental disabilities to fast. In addition, other bodies mandated to inspect detention centers and investigate human rights violations such as the Commission on Human Rights and Administrative Justice (CHRAJ) should closely monitor places of detention where persons with mental disabilities are taken.
The CHRAJ in Ghana should take a lead in this process by designing an inspection and complaints framework for persons with mental disabilities, and it should also offer support to other human rights organizations, especially training on monitoring, investigating, and filing complaints on behalf of persons with mental disabilities.
The government of Ghana must establish a mechanism through which the regional and district visiting committees established under the 2012 Mental Health Act are able to periodically and systematically visit all non-orthodox mental health service providers. The government must also ensure that persons with mental disabilities know their rights.
Schools, religious institutions, and other social groups should try harder to accommodate persons with mental disabilities and to respect, protect, and fulfill their rights. Such individuals often need personal assistance, housing, support in finding jobs, and family support. These prevent isolation in the community and ensure that a person’s needs do not compromise his or her full and equal participation and inclusion in society.
Ghana should also ratify the Optional Protocol to the Convention against Torture and all other forms of inhumane treatment, which it signed in 2006. The Optional Protocol requires independent inspection of all detention centers and gives a framework on how this should be done.
Recommendations
To the Ministry of Health
- Immediately improve conditions in psychiatric hospitals and prayer camps by providing adequate food, shelter, and health care, and by prohibiting, inspecting, and taking legal action against the practices of beating patients, forced and prolonged fasting, prolonged seclusion, and chaining of people.
- Formulate and implement a national policy on non-orthodox mental health service provision, which should regulate the use of prayer camps for persons with mental disabilities.
- Set out clearly the right of persons in institutions, including stating that prayer camps have no right to detain, abuse, forcibly treat, or assault inmates or deprive of them of food or drink. Set out what acts will amount to crimes, including unlawful detention, assault, and other abuse.
- Together with other stakeholders, design a mental health plan detailing implementation strategies and activities to realize policies on disability and mental health. The plan should clearly specify the budget and timeframe and the roles of different stakeholders involved in implementing activities or programs.
- Progressively develop voluntary community-based mental health services and other social forms of support to allow persons with mental disabilities to live independently and in the community.
- Train and recruit more mental health professionals to improve the doctor/nurse-patient ratio, and increase the number of non-medical staff in psychiatric hospitals to help nurses with maintenance work.
- Formalize working relationship between prayer camps and psychiatric hospitals; design measures through which persons with mental disabilities in prayer camps can access mental health services, including diagnosis, voluntary treatment, and regular monitoring by professional mental health service providers.
- Conduct a public information campaign to raise awareness about mental disability and disability rights, especially among alternative mental health service providers and the broader community, in partnership with organizations of persons with mental disabilities and media; ensure that all patients are informed of their rights.
- Prohibit admission and treatment of children with mental disabilities in prayer camps, and other practices like locking in rooms with adults, and other forms of inhumane treatment, which would compromise their development and enjoyment of rights as children. Investigate and prosecute those who do not adhere to these principles.
- Include psychotropic drugs on the list of essential drugs provided by the National Health Insurance scheme, in order to enhance the scheme’s access to persons with mental disabilities, especially those living in the community.
To the Ministry of Employment and Social Welfare
- Ensure that persons with mental disabilities and their representative organizations are involved and participate fully in planning, carrying out, and monitoring government programs that promote employment and social welfare.
- Develop a framework through which rights of persons with disabilities generally are monitored. This should be done in conjunction with the Commission for Human Rights and Administrative Justice.
- Train persons with mental disabilities about their rights and the existing mechanisms through which they can challenge violations of such rights.
To the Parliament of Ghana
- Stengthen and monitor the implementation of laws banning inhumane practices in psychiatric hospitals and non-orthodox mental health services, including chaining and prolonged restraint, mandatory fasting, and treatment without free and informed consent.
- Amend or repeal all domestic legislation that is in violation of the CRPD, including the 2012 Mental Health Act, and ensure that persons with mental disabilities are entitled to equal recognition before the law, legal capacity, protection from arbitrary detention based on disability, and supported decision-making as the alternative to guardianship.
To the National Disability Council
- Introduce and/or monitor policies and programs promoting rights of persons with mental disabilities on aspects like deinstitutionalization, community education about mental disability, and provision of support to persons with disabilities and their families.
- Collect and disaggregate data about persons with mental disabilities to guide formulation and implementation of policies. Such information should be harmonized with and disseminated among stakeholders working with persons with mental disabilities to address the barriers faced by persons with mental disabilities in Ghana.
- Coordinate ongoing initiatives around mental health issues among disabled persons organizations (DPOs) and government departments in Ghana to enhance community-based care, including health, social care, housing, education, employment, transport, leisure, criminal justice, and social security.
- Establish an effective monitoring framework, including designating a special body to oversee conditions of persons with mental disabilities whose right to personal liberty is restricted. This body should have a special mandate to monitor compliance by community and alternative mental health services, including prayer camps and traditional healers.
- Maintain a register of prayer camps which house or interact with persons with mental disabilities.
To Management of Psychiatric Institutions
- Immediately improve the infrastructure in psychiatric hospitals, including repairing dilapidated buildings and broken water and electricity supply systems, and increasing supplies of gloves, detergents, and other neccesary equipment needed for adequate maintenance and hygiene.
- Adopt guidelines on exceptional circumstances that must arise to allow for involuntary detention and/or treatment in a psychiatric facility.
- Train staff on human rights-based approaches to psychiatric treatment.
To the Judiciary, Police, and Prison Officials
- Strengthen existing structures to effectively address legal concerns of persons with mental disabilities. This should include continuous training for the officials of the judiciary, police, prisons, and the Commission for Human Rights and Administrative Justice, and improving accessibility to justice centers for persons with mental disabilities.
- Strengthen investigation and prosecution procedures to bring perpetuators of crimes against persons with mental disabilities in psychiatric hospitals, prayer camps, and other facilities to justice. Be clear that detention, assaults, and other abusive attacks, such as chaining or forced fasting, committed on persons within such institutions amount to crimes as they would outside the institutions.
- Set up mechanisms whereby persons within institutions can report crimes and other abuse without fear of reprisal.
To Inter-Religious Council, Ministry of Culture and Chieftaincy, and Faith-Based Organizations
- Design internal guidelines to monitor operations of prayer camps affiliated to religious councils.
- Advocate for the integration of persons with mental disabilities in the community.
- Provide training to broader membership including at grassroots levels about the rights of persons with mental disabilities.
- Provide counseling and other forms of support to persons with mental disabilities and their families.
- Sensitize chiefs, clan leaders, and other traditional leaders about the causes, effects, and manifestations of mental disability, and the rights of persons with mental disabilities.
To Management of Prayer Camps
- Immediately end the use of chaining, fasting, and any form of detention.
- Provide adequate food, shelter, and health care to persons with mental disabilities.
- Enable persons with mental disabilities to freely enter and leave at will, to refuse treatment, and to seek psychiatric or orthodox medical care, and ensure that all persons in the camps are always fully aware of this.
- Ensure coordination between mental health professionals and staff at prayer camps to offer mental health services based on free and informed consent.
To Disabled Persons’ Organizations, Human Rights Organizations, and Media
- Lead awareness-raising campaigns to sensitize the public about mental disability and the rights of persons with mental disabilities, including the right to live in the community.
- Demand continuous improvement in mental health services by the government through legal and policy reforms, establishment of a regulatory framework for non-orthodox service providers, and establishment of community care systems.
To Ghana’s Development Partners, including the World Bank, the World Health Organization, UNICEF, USAID, and DFID
- Support the government of Ghana and disabled persons’ organizations through funding and providing techical assistance as needed to safeguard and raise awareness of the rights of persons with mental disabilities.
- Monitor the implementations of laws, policies, and programs on mental disability and any other laws and policies which are incidental to the enjoyment of human rights by persons with mental disabilities.
- Encourage the government of Ghana to allocate appropriate resources to the mental health sector including funds to support national psychiatric hospitals and the creation or improvement of psychiatric units at regional and district levels to ensure easy access to services for persons with mental disabilities.
- Ensure mainstreaming of disability issues, including mental disability, in development programs and in work with other stakeholders including government and local and international human rights and children‘s rights organizations.
To Families and the Broader Community
- Support persons with mental disabilities by asking them how best to assist them in dealing with a mental health crisis and making decisions about their treatment and recovery.
Acknowledgements
This report was researched and written by Medi Ssengooba, Finberg fellow at Human Rights Watch, with research assistance from Shantha Rau Barriga, senior disability rights researcher and advocate; Corinne Dufka, senior researcher in the Africa Division; and Rona Peligal, deputy director, Africa Division.
The report was edited by Shantha Rau Barriga; Corinne Dufka; Rona Peligal; Joseph Amon, health and human rights director; Amanda McRae, disability rights researcher; Alice Farmer, children’s rights researcher; Clive Baldwin, senior legal advisor; Danielle Haas, senior editor; and Babatunde Olugboji, deputy program director. Layout, design, and production were coordinated by Grace Choi, publications director, Ivy Shen, multimedia associate, Fitzroy Hepkins, mail manager; and Alex Gertner and Margaret Wurth, both coordinators in the Health and Human Rights Division.
Human Rights Watch would like to thank Professor Robert Dinerstein, American University, Washington College of Law; Robinah Alambuya, president of the Pan African Network of People with Psychosocial Disabilities; and Peter Yaro, director of BasicNeeds Ghana, for providing expert review of sections of this report. We are deeply indebted to Dr. Akwasi Osei, chief psychiatrist of the Ghana Health Service and director of Accra Psychiatric Hospital, for providing us with useful information and for giving us access to Ghana’s psychiatric hospitals. We are grateful to Rita Kusi, director of the Ghana Federation for the Disabled, for assisting us in organizing our field research missions. We would also like to thank Dan Taylor, director of Mindfreedom Ghana, for his support before, during, and after our research missions.
Human Rights Watch also appreciates the support of local service and advocacy organizations for persons with disabilities in Ghana that shared their invaluable expertise with our researchers. Most importantly, we wish to thank all those who shared their experiences in psychiatric hospitals, prayer camps, and in the community, all of whom spoke with courage and dignity about their mental disabilities, personal histories, and concerns.
A special thank you to Fondation d'Harcourt for the financial support that made this research and report possible.
[1] Prophets are widely respected in Ghana, where they are visited by a wide cross-section of society, including senior government officials.
[2] People with mental disabilities interviewed by Human Rights Watch who had visited traditional healers said that usually the method of treatment involves use of local herbs and sacrificing animals “to appease the gods.”
[3] People with mental disabilities interviewed by Human Rights Watch who had visited traditional healers said that traditional healers generally operate independently and use methods of treatment involving local herbs and sacrificing animals “to appease the gods.”
[4]World Health Organization (WHO), Mental Health Improvement for National Development (MIND), Country Summary Series: Ghana, 2007, http://www.who.int/mental_health/policy/country/GhanaCoutrySummary_Oct2007.pdf (accessed April 1, 2012). Mental disabilities are classified as severe when someone is undergoing episodes of psychosis, which may, among other symptoms, result in hallucinations. Provisional results from the 2010 population and housing census indicate that 4.8 million Ghanaians have disabilities.
[5]Convention on the Rights of Persons with Disabilities (CRPD), adopted December 13, 2006, G.A. Res. 61/106, Annex I, U.N.GAOR Supp. (No. 49) at 65, U.N. Doc. A/61/49 (2006), entered into force May 3, 2008, ratified by Ghana on July 31, 2012, art. 1.
[6]World Network of Users and Survivors of Psychiatry, Manual on Implementation of the Convention on the Rights of Persons with Disabilities, p. 9, http://www.chrusp.org/home/resources (accessed July 7, 2010).
[7] Human Rights Watch interview with Dr. Akwasi Osei, chief psychiatrist, Ghana Health Service, and director, Accra Psychiatric Hospital, January 17, 2012.
[8] Human Rights Watch interview with Dan Osei, acting director, Policy Planning, Monitoring and Evaluation, Ghana Health Service, January 17, 2012.
[9]Department for International Development (DIFD) Ghana Operational Plan 2011-2015, April 2011, http://www.dfid.gov.uk/Documents/publications1/op/ghana-2011.pdf (accessed May 21, 2012).
[10]Ghana Federation of the Disabled, Disability Situation in Ghana, http://gfdgh.org/disability%20situation%20in%20ghana.html (accessed May 20, 2012).
[11]Sophie Mitra, et al., Special Protection & Labour, the World Bank, “Disability and Poverty in Developing Countries: A Snapshot from the World Health Survey,” April 2011, http://siteresources.worldbank.org/SOCIALPROTECTION/Resources/SP-Discussion-papers/Disability-DP/1109.pdf (accessed September 12, 2012).
[12]World Health Organization Mental Health Atlas 2005, Geneva: WHO, 2005, p. 209, http://www.who.int/mental_health/evidence/mhatlas05/en/index.html (accessed May 30, 2012); The Ghana Chronicle, “Need to Decentralize Mental Health Services,” October 8, 2008, http://www.ghanaweb.com/GhanaHomePage/NewsArchive/artikel.php?ID=151315 (accessed September 12, 2012). The article reports that out of a total budget of GH¢867.2 million, about US$443.8 million, (including the National Health Insurance Fund, NHIF) allocated to the health sector in 2009, only 1.12 percent or GH¢9.7 million or 4.9 million US Dollars, was allocated to the mental health sub-sector; Human Rights Watch interview with Dan Osei, acting director, Policy Planning, Monitoring and Evaluation, Ghana Health Service, January 17, 2012; Human Rights Watch interview with Dr. Akwasi Osei, chief psychiatrist, Ghana Health Service, and director, Accra Psychiatric Hospital, January 16, 2012.
[13] “Budget Trivialises Mental Health,” Peacefmonline.com, January 22, 2010, http://news.peacefmonline.com/health/201001/37060.php (accessed September 11, 2012). Of the total allocation to the mental health sub-sector, GH¢7 million (72 %) was used for emoluments, and GH¢2,686 (28 percent) used for non-wages, such as drugs, medical supplies, and other amenities. Nothing was allocated for capital expenditure, that is to say, expenditure on buildings, medical equipment, vehicles, etc.; Herena Selby, Modern Ghana,Ghanaian Chronicle, “Prayer Camps and Mental Illness,” June 19, 2012, http://www.modernghana.com/news/328243/1/prayer-camps-and-mental-illness.html (accessed September 11, 2012).
[14]Olivia Fournier “The Status of Mental Health Care in Ghana, West Africa and Signs of Progress in the Greater Accra Region” Berkeley Undergraduate Journal, vol. 24, no. 3 (2011), p. 9-34.
[15] The mental health budget mainly focuses on Ghana’s three public psychiatric hospitals, with no commitment to other aspects of support for persons with mental disabilities, such as community-based services.
[16] Human Rights Watch interview with Dan Osei, January 17, 2012.
[17]Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012; Human Rights Watch interview with Dr. Anan Armah Arlob, medical director, Ankaful Psychiatric Hospital, November 24, 2011.
[18]See Accra Psychiatric Hospital, http://accrapsychiatrichospital.org/pages/about-us.php (accessed, April 16, 2012).
[19]Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012.
[20] Human Rights Watch visit to Accra Psychiatric Hospital, November 14, 2011.
[21]Human Rights Watch visit to Pantang Psychiatric Hospital, November 14, 2011.The Chronic Ward housed people who had serious mental health problems. Over half of the total number of individuals on the ward had been diagnosed with schizophrenia.
[22]Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012.
[23] Mental Health Training Policy, Revised Edition, 2000. The policy also requires recruitment or training of at least 10 psychiatrists; 20 one-year diploma in psychiatry; 40 clinical psychologists; 10 occupational therapists and 200 mental health nurses.
[24]Human Rights Watch interview with Ebu Blankson, head, Social Welfare Department, Ankaful Psychiatric Hospital, January 19, 2012.
[25]WHO, Ghana Mental Health Profile 2003, http://www.who.int/mental_health/policy/country/GhanaCoutrySummary_Oct2007.pdf (accessed on April 12, 2012).
[26] Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012.
[27]National Health Insurance Act, 2003, http://www.nhis.gov.gh/_Uploads/dbsAttachedFiles/Act650original2.pdf (accessed March 3, 2012); Joseph Mensah et al. “Global Development Network 1999-2009: An Evaluation of Ghana’s Health Insurance Scheme in the Context of the Health MDGs,” GND Working Paper Series, March 2010, http://depot.gdnet.org/newkb/submissions/Health%20Project_40.pdf (accessed September 12, 2012).
[28]Human Rights Watch email correspondence with Ophelia Abrokwah, administrator, National Health Insurance Scheme, June 20, 2012.
[29]Human Rights Watch interview with Dr. Anan Armah Arlob, director, Ankaful Psychiatric Hospital, November 24, 2011. Human Rights Watch interview with a psychiatric nurse, Accra Psychiatric hospital, November 16, 2011. Human Rights Watch interview with Martin (pseudonym) psychiatric nurse, Pantang Psychiatric hospital, November 19, 2011.
[30] Human Rights Watch interview with a Daniel (Pseudonym), ward in charge at Pantang Psychiatric Hospital, Pantang Psychiatric Hospital, November 16, 2011.
[31] Human Rights Watch interview with Dr. Akwasi Osei, chief psychiatrist, Ghana Health Service, and director, Accra Psychiatric Hospital, Accra, November 16, 2011.
[32] Human Rights Watch interview with Rita Kusi, executive director, Ghana Federation of the Disabled (GFD), Accra, November 15, 2011.
[33] Human Rights Watch, email correspondences with Ellen Kwakoah Asamoah, Client Relations, Strategy and Corporate Affairs Division, National Health Insurance Authority, Accra, August 23, 2012.
[34] Victor Deku, et al., “Mental Health and Poverty Project, Phase.1 Country report: A Situation Analysis of Mental Health Policy Development and Implementation in Ghana,” June 11, 2008, http://www.health.uct.ac.za/usr/health/research/groupings/mhapp/country_reports/Ghana_report.pdf, (accessed October 8, 2012)
[35] Ibid.
[36] Human Rights Watch telephone correspondence with Peter Yaro, director, BasicNeeds Ghana, August, 24, 2012.
[37] Ghana Federation of the Disabled, “Disability Situation in Ghana,” http://gfdgh.org/disability%20situation%20in%20ghana.html (accessed May 20, 2012).
[38] Central Intelligence Agency, the World Factbook, Ghana, https://www.cia.gov/library/publications/the-world-factbook/geos/gh.html (accessed August 11, 2012).
[39]Commonwealth Human Rights Initiative (CHRI), Africa Division, Human Rights Violations in Prayer Camps and Access to Mental Health in Ghana, 2008.
[40] Human Rights Watch email correspondence with Rev. Dr. Opoku Onyinah, chairperson, Ghana Pentecostal and Charismatic Council (GPCC), August 28, 2012. The GEC is a non-denominational organization which serves as a platform to give assistance to churches and Christian organizations in the country to propagate the Gospel.
[41]Helena Selby, “Prayer Camps and Mental Illness,” The Chronicle, undated, http://ghanaian-chronicle.com/prayer-camps-and-mental-illness/ (accessed March 28, 2012).
[42] Human Rights Watch interview with Robert Amo, director of programs and advocacy, Christian Council of Ghana, Accra, November 23, 2011.
[43]Commonwealth Human Rights Initiative (CHRI), Africa Division, “Human Rights Violations in Prayer Camps and Access to Mental Health in Ghana,” 2008. A study by Commonwealth Human Rights Initiative of 16 prayer camps in the Greater Accra Region, Volta Region, and Central Region, found that 80 individuals admitted had mental disabilities. Human Rights Watch interview with Prophet Mama Comfort, Mama Comfort Church, Greater Accra Region, November 17, 2011.
[44] Human Rights Watch interview with Prophet Paul Kweku Nii Okia, founder, Mount Horeb Prayer Camp, Mamfi Mountains, Eastern Region, November 19, 2011;Human Rights Watch interview with Rev. Rebekah Bedford, director, Edumfa Prayer Camp, Central Region, January 19, 2012; Human Rights Watch interview with Prophet Leo Badoo, proprietor, Nyakumasi Prayer Camp, and Elijah (pseudonym), resident, Nyakumasi Prayer Camp, January 19, 2012.
[45] Human Rights Watch interview with Rev. Dr. Opoku Onyinah, chairperson, Ghana Pentecostal and Charismatic Council, Accra, January 25, 2012.
[46] Human Rights Watch interview with Rev. Rebekah Bedford, January 19, 2012, Human Rights Watch observations at Edumfa Prayer Camp.
[47] Human Rights Watch interview with Elijah (pseudonym), resident, Mountains Jesus Divine Temple Mission, Nyakumasi Prayer Camp, Cape Coast, Central Region, January 19, 2012; Human Rights Watch interview with Ali (pseudonym), resident, Nyakumasi Prayer Camp, January 19, 2012; Human Rights Watch interview with Abigail Kruvi, staff, Mount Horeb Prayer Camp, November 19, 2011; Human Rights Watch interview with Doris Appiah, national treasurer, Mental Health Society of Ghana (MEHSOG), Accra, January 15, 2012.
[48]Human Rights Watch interview with Rev. Dr. Opoku Onyinah, January 25, 2012.
[49] Human Rights Watch interview with Rev. Rebekah Bedford, January 19, 2012
[50] Details in a booklet issued by Faith Complementary Health Care Association of Ghana, given to Human Rights Watch by Prophetess Rebekah January 19, 2012.
[51]Human Rights Watch interview with Rev. Dr. Opoku Onyinah, January 25, 2012.
[52] Ibid.
[53] Ghana Pentecostal and Charismatic Council (GPCC), Guidelines for Operation of Prayer Camps, obtained by email from Rev. Dr. Opoku Onyinah, chairperson, GPCC, January 25, 2012. The guidelines further set standards below which a prayer camp should operate on a non-residential basis; otherwise, it should be closed. The guidelines provide that a prayer camp must have: proper accommodation, e.g. use of foam mattresses; good sanitation, cleanliness; good drinking water and food where needed; the counselee must be interviewed and segregated according to type of disease. The management committee should ensure that the center gets these facilities.
[54]Ghana Pentecostal and Charismatic Council (GPCC), Guidelines for Operation of Prayer Camps, obtained by email from Rev. Dr. Opoku Onyinah, GPCC, January 25, 2012.
[55] Human Rights Watch interview with Rev. Dr. Opoku Onyinah, January 25, 2012.
[56] Ibid.
[57] Some former patients of the camps told Human Rights Watch that they felt better since coming to the camp; and others said they felt worse; especially those who were not allowed to take medications. Some had gone to the same camp several times, and there are some we saw in November 2011, but who were still in chains in January 2012.
[58]Commonwealth Human Rights Initiative, “Denying Ghana’s Disabled Their Rights: The Disability Act, 5 years on,” June 23, 2011, http://chriafrica.blogspot.com/2011/06/denying-ghanas-disabled-their-rights.html (accessed April 13, 2012). Commonwealth Human Rights Initiative, is an international human rights nongovernmental organization mandated to ensure practical realization of human rights in the former British colonies,
[59]Traditional and Alternative Medicine Bill, 2010.
[60] Human Rights Watch interview with Doris Appiah, national treasurer, Mental Health Society of Ghana (MEHSOG), Accra, January 15, 2012; Human Rights Watch interview with Ms. Akosua-Amponsah, mother and care taker of an 18-year-old boy with schizophrenia, Greater Accra Region, January 22, 2012; Human Rights Watch interview with Samuel (Pseudonym), Dakuman Community, Greater Accra Region, January 18, 2012.
[61] Human Rights Watch interview with Peter Yaro, executive director, BasicNeeds Ghana, Accra, Ghana, November 13, 2011.
[62]Human Rights Watch interview with Peace (pseudonym), patient, Pantang Psychiatric Hospital, November 19, 2011
[63]Human Rights Watch interview with Prophet Paul Kweku Nii Okia, Mount Horeb Prayer Camp, November 19, 2011; Human Rights Watch interview with Rev. Rebekah Bedford, January 19, 2012; Human Rights Watch interview with Prophet Charity Donkor, January 19, 2012; Human Rights Watch interview with Prophet Appiah Kubi, Mount Horeb, November 19, 2011; Human Rights Watch interview with Prophet Leo Baidoo, Nyakumasi Prayer Camp, January 19, 2012; Human Rights Watch interview with Prophet Charity Donkor, Charity Ministries, January 19, 2012.
[64] Human Rights Watch email correspondence with Dan Taylor, executive director, Mindfreedom Ghana, August 13, 2012.
[65] Ibid.
[66]Human Rights Watch Interview with Dr. Akwasi Osei, January 17, 2012.
[67]Ibid.
[68] Human Rights Watch interview with Peace (pseudonym), November 24, 2011.
[69]Human Rights Watch interview with a Dr. Akwasi Osei, January 19, 2012.
[70]Human Rights Watch interview with Dr. Anan Armah Arlob, medical director, Ankaful Psychiatric Hospital, November 25, 2011.
[71]Human Rights Watch interview with Dr. Anan Armah Arlob, medical director, Ankaful Psychiatric Hospital, November 25, 2011.
[72]Human Rights Watch interview with John (pseudonym), resident, Mount Horeb Prayer Camp, Mamfi, Eastern Region, January 19, 2012.
[73]Human Rights Watch interview with Peter (pseudonym), resident, Edumfa Prayer Camp, Central Region-Cape Coast, January 19, 2012
[74]Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011.
[75]Human Rights Watch interview with psychiatric nurse, Pantang Psychiatric Hospital, November 19, 2011.
[76]Constitution of the Republic of Ghana, 1992, art.14 (1)
[77]Constitution, art.14 (1) (a)
[78] Mental Health Act, No. 846, 2012.
[79]Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 14, 2011; Human Rights Watch interview with Patience Nsatimba, nurse, Pantang Psychiatric Hospital, November 19, 2011; Human Rights Watch interview with a nurse, Ankaful Psychiatric Hospital, November 24, 2011.
[80]Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011.
[81]Ibid.
[82]Human Rights Watch interview with Dr. Anan Armah Arlob, medical director, Ankaful Psychiatric Hospital, November 25, 2011; Human Rights Watch perused the file of Margaret (pseudonym), who could not see and or hear well. Human Rights Watch interview with a nurse, a ward in charge, Ankaful Psychiatric Hospital, November 25, 2011. The nurse said that the woman who had been there for 35 years could have been discharged a few years ago, but she had nowhere to go.
[83]Human Rights Watch interviews with Bentil (pseudonym), patient, and a nurse, a ward in charge, Ankaful Psychiatric Hospital, November 24, 2011. Human Rights Watch also perused the individual’s file.
[84] Human Rights Watch interview with Bentil (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011
[85] Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011.
[86] Human Rights Watch interview with Sarah, (pseudonym), patient, Pantang Psychiatric Hospital, November 19, 2011.
[87] Human Rights Watch interview with John (pseudonym), resident, Mount Horeb Prayer Camp, Eastern Region, November 19, 2011.
[88] Human Rights Watch interview with Elijah (pseudonym), resident, Mountains Jesus Divine Temple Mission, Nyakumasi Prayer Camp, Cape Coast, Central Region, January 19, 2012.
[89] Human Rights Watch interview with Reverend Mary Asamora, Church of the Lord Mission, Senya Breku Prayer Camp, Senya Breku, January 26, 2012.
[90]Human Rights Watch interview with Pastor Francis Bayadam, Good News Evangelicals Mission International, Accra, November 23, 2011. The sanatorium was a section of the prayer camp where persons with mental disabilities resided.
[91]Brandee Burler, “The Treatment of Psychiatric Illness in Ghana,” SIT Graduate Institute, African Diaspora Collection, 1997.
[92]Accra Psychiatric Hospital, http://accrapsychiatrichospital.org/pages/about-us.php (accessed June 29, 2012).
[93]Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011.
[94]Human Rights Watch interview with Lillian (pseudonym), patient, Accra Psychiatric Hospital, Accra Psychiatric Hospital, November 17, 2011. Lillian was in the Open Female Ward, which a Hawa (nurse on duty) said had 55 patients on admission at the time of Human Rights Watch’s visit, but had only 30 beds.
[95]Human Rights Watch interview with nurse, Pantang Psychiatric Hospital, November 19, 2011.
[96]Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 16, 2011.
[97]Ibid.
[98]Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 16, 2011.
[99]Human Rights Watch visit to the Special Ward (former Criminal Ward) and Open Female Ward, Accra Psychiatric Hospital, November 16, 2011. Human Rights Watch visit to the Female Chronic Ward, Pantang Psychiatric Hospital, November 19, 2011.
[100]Human Rights Watch interview with nurse, Pantang Psychiatric Hospital, November 19, 2011; Human Rights Watch interview with three nurses, Accra Psychiatric Hospital, November 16, 2011.
[101] Human Rights Watch interview with nurse, Pantang Psychiatric Hospital, November 19, 2011.
[102]Human Rights Watch visits to Mount Horeb Prayer Camp, Mamfi, Eastern Region, January 20, 2012; Human Rights Watch visits to Edumfa Prayer Camp (Central Region), January 19, 2012. At Edumfa Prayer Camp, patients were housed in open-plan concrete buildings about 23 meters long by 10 yards wide. All residents were chained in concrete stalls adjacent to each other and wide enough to fit a small mat or mattress. The first ward housed over 40 patients with serious mental health problems, and was completely full. Many patients were yelling, singing, shouting, or talking to themselves. About 10 men were housed in a separate closed but quite crowded room. About half the men were chained, and only a few could hold a conversation.
[103]Human Rights Watch interview with Abigail Kruvi, staff, Mount Horeb Prayer Camp. November 19, 2011.
[104]Human Rights Watch interview with Aisha (pseudonym), patient, Mount Horeb Prayer Camp, January 21, 2012.
[105]Human Rights Watch interview with Peter (pseudonym), resident, Mount Horeb Prayer Camp, Eastern Region, January 20, 2012.
[106]Ibid.
[107]Human Rights Watch interview with Abigail Kruvi, staff, Mount Horeb Prayer Camp, November 19, 2011.
[108]Ibid.
[109]Human Rights Watch interview with Aisha (pseudonym), Mount Horeb Prayer Camp, January 21, 2012.
[110]Human Rights Watch visits to Mount Horeb Prayer Camp (Eastern Region), Edumfa Prayer Camp (Central Region) and Nyakumasi Prayer Camp (Central Region-Cape Coast), between November 2011 and January 2012.
[111]Human Rights Watch interview with Kofi (pseudonym), resident, Edumfa Prayer Camp, Central Region-Cape Coast, January 19, 2012.
[112]Human Rights Watch visits to Mount Horeb Prayer Camp, Mamfi, Eastern Region, November 19, 2011 and January 25, 2012.
[113]Human Rights Watch interview with Elijah (pseudonym), resident, Mountains Jesus Divine Temple Mission, Nyakumasi, Cape Coast, Central Region, January 19, 2012.
[114]Human Rights Watch interview with Aisha (pseudonym), resident, Mount Horeb Prayer Camp, January 19, 2012.
[115]Human Rights Watch interview with Prophet Paul Kweku Nii Okia, founder, Mount Horeb Prayer Camp, Mamfi Mountains, Eastern Region, November 19, 2011.
[116]Human Rights Watch interview with Rev. Rebekah Bedford, director, Edumfa Prayer Camp, Central Region, January 19, 2012.
[117]Constitution, art. 21 (2) (g).
[118]Ibid., art. 26 (1) and (2).
[119] Criminal Code Act, 1960 (as amended in 2003), sec. 80.
[120] Ibid., secs. 88 (1) and (2).
[121]Code of Federal Regulations Part 482, Title 42 – Public Health, section 482.13, http://www.gpo.gov/fdsys/pkg/CFR-2011-title42-vol5/pdf/CFR-2011-title42-vol5-sec482-13.pdf.The Centers for Medicare and Medicaid Services (CMS) is an agency within the US Department of Health and Human Services responsible for administering several key federal health care programs, including Medicare, the Children’s Health Insurance Program (CHIP), and Health Insurance Portability and Accountability Act (HIPAA).
[122] Mendez, Juan. Report of the Special Rapporteur on torture and cruel, inhuman or degrading treatment or punishment, A/66/268, August 2011, http://daccess-dds-ny.un.org/doc/UNDOC/GEN/N11/445/70/PDF/N1144570.pdf?OpenElement,p.8http://www.ohchr.org/en/NewsEvents/Pages/DisplayNews.aspx?NewsID=11506&LangID=E June 24, 2012).
[123]Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 16, 2011.
[124] Human Rights Watch interview with Patience Nsatimba, deputy ward in charge, Male Ward, Pantang Psychiatric Hospital, November 19, 2011.
[125] Human Rights Watch interview with Kingston (pseudonym) nurse, Accra Psychiatric Hospital, November 16, 2011.
[126]Human Rights Watch interview with Harriet (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011.
[127]Human Rights Watch interview with Mary (pseudonym), psychiatric nurse, Ankaful Psychiatric Hospital, Female Acute Ward, Ankaful Psychiatric Hospital, November 24, 2011; Human Rights Watch interview with Daniel (pseudonym), psychiatric nurse, Accra Psychiatric Hospital, November 16, 2011; Human Rights Watch interview with Peter Atta, ward in charge, Pantang Psychiatric Hospital, November 21, 2011; Human Rights Watch interview with Jane (pseudonym), nurse, Accra Psychiatric Hospital, November 16, 2011.
[128] Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (SR Torture Interim Report), 28 July 2008, UN Doc A/63/175, para. 56. See Human Rights Committee, concluding observations on the second periodic report of Slovakia (CCPR/CO/78/SVK), para. 13 and on the second periodic report of the Czech Republic (CCPR/C/CZE/CO/2), para. 13, where the committee expressed concern about the persistent use of cage-net beds as a means to restrain psychiatric patients, recalling that this practice is considered inhuman and degrading treatment and amounts to a violation of articles 7, 9 and 10 of the International Covenant on Civil and Political Rights.
[129]Human Rights Watch interview with Daniel (pseudonym), psychiatric nurse, Accra Psychiatric Hospital, November 16, 2011.
[130]Ibid.
[131]Human Rights Watch visit to Nyakumasi Prayer Camp, Central Region- Cape Coast, January 19, 2012.
[132]Human Rights Watch interview with Afia (pseudonym), Mount Horeb Prayer Camp, January 21, 2012.
[133]Human Rights Watch interviewed Prophetess Charity Donkor, director, Charity Prayer Ministry, Central Region, Cape Coast. January 19, 2012; Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Greater Accra Region, November 21, 2011; Human Rights Watch interview with Rev. Rebekah Bedford, Edumfa prayer camp, Central Region, November 19, 2012.
[134]Human Rights Watch interview with Rebecca Norah, community psychiatric nurse, Tetteh Quash Hospital, Akwampim North district, January 25, 2012.
[135]Human Rights Watch interview with Pastor Paul Kweku, director International Christ Miracle Gospel Ministries, Mamfi, Eastern Region, January 21, 2012.
[136]Human Rights Watch interview with Doris Appiah, January 15, 2012.
[137] Human Rights Watch interview with Aisha (pseudonym), resident, Mount Horeb Prayer Camp, Eastern Region, January 19, 2012, Human Rights Watch interview with Joseph (pseudonym), resident, Mount Horeb Prayer Camp, Eastern Region, November 19, 2012,
[138] Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011; Human Rights Watch interview with Rev. Rebekah Bedford, Edumfa prayer camp, Central Region, November 19, 2012; Human Rights Watch interview with Pastor Paul Kweku, director, International Christ Miracle Gospel Ministries, Mamfi, Eastern Region, January 21, 2012.
[139] Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011. Human Rights Watch did not find evidence that police brought people to prayer camps as some administrators said. None of the people interviewed said they had been brought to the prayer camp by police.
[140]Human Rights Watch interview with Pastor Francis Bayadam, Good News Evangelicals Mission International, Accra, November 23, 2011.
[141]Human Rights Watch interview with Pastor Christian Addo, Mount Horeb Prayer Camp, January 21, 2012.
[142]Human Rights Watch interview with Prophetess Charity Donkor, director Charity Prayer Ministry, Central Region, Cape Coast. January 19, 2012; Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011; Human Rights Watch interview with Rev. Rebekah Bedford, November 19, 2012.
[143]Human Rights Watch interview with Elijah (pseudonym), Mountains Jesus Divine Temple Mission, Nyakumasi, Cape Coast, Central Region, January 19, 2012.
[144]Human Rights Watch interview with Linda (pseudonym), community psychiatric nurse, Tetteh Quarshie Memorial Hospital, Akwampim North district, January 25, 2012.
[145]Human Rights Watch interview with Mark Dodoo, member, Nyamg Adom Self Help Group, Dakuman Community, January 18, 2012.
[146]Human Rights Watch interview with Rev. Mary Asamora, Church of Lord Mission, Senya Breku, Central Region, January 26, 2012.
[147] Human Rights Watch interview with Avotri Seyram, nurse, Special Ward, Accra Psychiatric Hospital, November 16, 2011.
[148]ICESCR, art. 11.
[149]Constitution, arts. 13 and 36.
[150]Human Rights Watch interview with Dr. Anan Armah, director, Ankaful Psychiatric Hospital, Ankaful Psychiatric Hospital, November 23, 2011.
[151]Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 14, 2011.
[152]Human Rights Watch interview with Lillian (pseudonym), patient, Accra Psychiatric Hospital, November 17, 2011. Largactil is “used in the management of psychotic conditions. Largactil controls excitement, agitation and other psychomotor disturbances in patients with schizophrenia and reduces the manic phase of manic-depressive conditions. It is also used to control hyperkinetic states and aggression and is sometimes given in other psychiatric conditions for the control of anxiety and tension.” South African Electronic Package inserts, http://home.intekom.com/pharm/aventis/largact.html (accessed April 18, 2012).
[153]Human Rights Watch Interview with Suleiman Ayiku, member, Mental Health Society of Ghana, Accra, January 15, 2012.
[154] Human Rights Watch interview with Prophetess Charity Donkor, director Charity Prayer Ministry, Central Region, Cape Coast. January 19, 2012. Human Rights Watch interview with Rev. Rebekah Bedford, Edumfa prayer camp, Central Region, November 19, 2012. Human Rights Watch interview with Pastor Paul Kweku, director International Christ Miracle Gospel Ministries, Mamfi, Eastern Region, January 21, 2012.
[155] Human Rights Watch was told by Prophet Paul Kweku, that Mount Horeb Prayer Camp had 120 individuals in November 2011; and Pastor Christian said the camp had 135 individuals in January 2012. Tetteh Quarshie Memorial Hospital, Mampong- Akwampim, is a general hospital near Mount Horeb. It has a psychiatric unit, which is served by two psychiatric nurses and has been without a psychiatric doctor attached to it since 2010.
[156]Human Rights Watch interview with Ebu Blankson, psychiatric social worker, Ankaful Psychiatric Hospital, January 18, 2012.
[157]In Nyakumasi, Kordiabe, and Senya Breku Prayer Camps, prophets did not tell Human Rights Watch of any formal relationships with psychiatric hospitals. At Nyakumasi and Edumfa Prayer Camps, psychotropic treatment is not allowed in the camps.
[158]Human Rights Watch interview with Dr. Akwasi Osei, January 16 2012.
[159]Ibid.
[160]Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011; Human Rights Watch interview with Rev. Rebekah Bedford, Edumfa prayer camp, Central Region, November 19, 2012; Human Rights Watch interview with Prophetess Charity Donkor, director Charity Prayer Ministry, Central Region, Cape Coast. January 19, 2012.
[161]Human Rights Watch interview with Prophetess Charity Donkor, director, Charity Prayer Ministry, Central Region, Cape Coast. January 19, 2012; Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011; Human Rights Watch interview with Prophet Rebekah Bedford, Edumfa prayer camp, Central Region, November 19, 2012.
[162]Human Rights Watch interview with Prophet Leo Baidoo, proprietor, Nyakumasi Prayer Camp, and Elijah (pseudonym), resident, Nyakumasi Prayer Camp, January 19, 2012.
[163]Human Rights Watch interview with Hon. Mubarak Muntaka, chairperson, Parliamentary Committee on Health, Parliament of Ghana, Accra, January 21, 2012.
[164]Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012.
[165]Mental Health Bill, 2012, section 34.
[166] Human Rights Watch interview with Sarah (pseudonym), patient, Pantang Psychiatric Hospital, November 19, 2011.
[167]Human Rights Watch interview with psychiatric nurse, Accra Psychiatric hospital, November 16, 2011; Human Rights Watch interview with psychiatric nurse, Pantang Psychiatric hospital, November 19, 2011; Human Rights Watch interview with Dr. Akwasi Osei, chief psychiatrist and director, Accra Psychiatric Hospital, November 16, 2011.
[168]Human Rights Watch interview with Margaret Nartay, ward in charge, Ankaful Psychiatric Hospital, November 24, 2011.
[169]Human Rights Watch interview with Abigail Kruvi, staff Mount Horeb Prayer Camp, Mount Horeb Church, November 19, 2011; Human Rights Watch interview with Bentil (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011.
[170]Human Rights Watch interview with Harriet (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011; Human Rights Watch interview with Peace (pseudonym), patient, Pantang Psychiatric Hospital, November 19, 2011; Human Rights Watch interview with Michael (pseudonym), patient, Pantang Psychiatric Hospital, November 16, 2011; Human Rights Watch interview with Elizabeth, patient, Pantang Psychiatric Hospital, November 19, 2011.
[171]Human Rights Watch interview with Lillian (pseudonym), Accra Psychiatric Hospital, November 16, 2011.
[172]Human Rights Watch interview with two nurses, Accra Psychiatric Hospital, November 16, 2011; Human Rights Watch interview with psychiatric nurse, Ankaful Psychiatric Hospital, November 19, 2011; Human Rights Watch interview with Michael (pseudonym), patient, Accra Psychiatric Hospital, November 16, 2011 and Sarah (pseudonym), patient, Pantang Psychiatric Hospital, November 24, 2011.
[173]Commonwealth Human Rights Initiative, Human Rights Violations in Prayer Camps and access to Mental Health in Ghana, August 2008. Concoctions or local herbs shown to Human Rights Watch included Nyamidea (God has blessed), Orunamu, Eme and Dya tree; Human Rights Watch interview with Prophet Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 21, 2011; Human Rights Watch interview with Rev. Mary Asamora, Church of the Lord Mission, Senya Breku Prayer Camp, Central Region, Ghana, January 26, 2012; Human Rights Watch interview with Prophet Rebekah Bedford, Edumfa Prayer Camp, Central Region, November 19, 2012; Human Rights Watch interview with Ebu Blankson, psychiatric social worker, Ankaful Psychiatric Hospital, January 18, 2012. Blankson conducted a survey of 4 of the 12 districts in Central Region, and registered over 40 prayer camps and found that herbs were widely used to treat patients.
[174] Human Rights Watch interview with Prophetess Winifred Buff, Kasoa Healing Center, Kasoa, Central Region, November 23, 2011.
[175]Human Rights Watch interview with Doris Appiah, January 15, 2012.
[176] Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (SR Torture Interim Report), 28 July 2008, UN Doc A/63/175, at [50].
[177] Ibid.
[178]See P.R. Breggin, Psychiatric Drugs: Hazards to the Brain (New York, Springer, 1983); D. Cohen, ‘A Critique of the Use of Neuroleptic Drugs’ in S Fisher and RP Greenberg (eds.), From Placebo to Panacea: Putting Psychiatric Drugs to the Test (New York, John Wiley, 1997); G.E. Jackson, Rethinking Psychiatric Drugs: A Guide for Informed Consent (Bloomington, Author House, 2005).
[179] Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (SR Torture Interim Report), 28 July 2008, UN Doc A/63/175, at [50], as cited by Tina Minkowitz, Abolishing Mental Health Laws to Comply with the Convention on the Rights of Persons with Disabilities, McSherry PAGE: 1 SESS: 7 OUTPUT: Wed Jul 28 10:48:01 2010. The American Medical Association defines informed consent as “a process of communication between a patient and physician that results in the patient's authorization to undergo a specific medical intervention.” This requires more than simply getting a patient to sign a written consent form; the physician performing the treatment and/or procedure (not a delegated representative) must fully inform the patient and discuss the ramifications of treatment. According to the AMA, the patient should thus know their diagnosis, if known; the nature, risk, benefit and purpose of a proposed treatment or procedure. A patient should be told about existing alternatives (regardless of their cost or the extent to which the treatment options are covered by health insurance); as well as risks associated with such alternative procedures. The patient should know the risks and benefits of not receiving or undergoing a treatment or procedure; and the patient should have an opportunity to ask questions. American Medical Association (AMA), Patient-Physician Relationship Topics, informed consent, accessed from http://www.ama-assn.org/ama/pub/physician-resources/legal-topics/patient-physician-relationship-topics/informed-consent.page, May 19, 2012.
[180] UN OHCHR, From Exclusion to Equality: Realizing the Rights of Persons with Disabilities, 90 (2007), http://www.ohchr.org/Documents/Publications/training14en.pdf, accessed August 12, 2012.
[181] Human Rights Watch phone interview with Professor Robert Dinerstein, director, Disability Law Clinic, American University, Washington College of Law, April 2, 2012.
[182] Office of High Commissioner for Human Rights, Information Note No.4: Persons with Disabilities, “Dignity and Justice for Detainees Week.”
[183] UN OHCHR, From Exclusion to Equality: Realizing the Rights of Persons with Disabilities, 90 (2007), http://www.ohchr.org/Documents/Publications/training14en.pdf (accessed August 12, 2012).
[184] Criminal Procedure Code Act, 1960, Sec. 42.
[185]Human Rights Watch interview with Harriet (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011; Human Rights Watch interview with Jane Quaye, executive director FIDA Ghana, November 23, 2011; Human Rights Watch interview with John Kwabena Arthur, relative and caregiver of a woman with a mental disability, November 20, 2011.
[186]Human Rights Watch interview with Reverend Richard Nii Kumu Ollennu, Ebenezer Presbyterian Church offices, Accra, January 16, 2012.
[187]Human Rights Watch interview with Barnard Akumiah, member Mental Health Society of Ghana (MEHSOG), Accra, November 20, 2011.
[188]Brandee Burler, the Treatment of Psychiatric Illness in Ghana, SIT Graduate Institute, African Diaspora Collection, 1997.
[189]Human Rights Watch interview with Jane (pseudonym), nurse, Accra Psychiatric Hospital, November 16, 2011. Jane told Human Rights Watch that the Open Female Ward had an individual who stayed for 20 years because her family never came to pick her up. At Ankaful Psychiatric Hospital, we examined a file of a 75-year-old woman who was believed to have lived on the ward for over 35 years.
[190]Human Rights Watch interview with Bernard Akumiah, person with a mental disability living in the community, Greater Accra Region, November 14, 2011.
[191]Human Rights Watch interview with Peace (pseudonym), resident, Pantang Psychiatric Hospital, November 19, 2011. Prior to coming to Pantang, Peace was first admitted to Ankaful Psychiatric Hospital.
[192]Human Rights Watch interview with Doris Appiah, November 20, 2011.
[193]Human Rights Watch interview with John Kwabena Arthur, Ministries, Accra, Ghana, November 16, 2011. John has a sister who has a mental disability and he takes care of her.
[194] Human Rights Watch interview with John Kwabena, relative of a person with a mental disability, Greater Accra Region, November 20, 2011
[195]Human Rights Watch interview with Millicent Asirifi, nurse, Ankaful Psychiatric Hospital, November 24, 2011.
[196]Human Rights Watch interview with Rebecca Norah, nurse at Tetteh Quarshie District hospital, who visits Mount Horeb Prayer Camp, January 25, 2012.
[197]Human Rights Watch interview with Dr. Akwasi Osei, January 17, 2012.
[198] Human Rights Watch interview with Dr. Anan Armah, director, Ankaful Psychiatric Hospital, November 23, 2011.
[199]Human Rights Watch interview with Robert Amo, director of programs and advocacy, Christian Council of Ghana (CCG), Accra, November 23, 2011.
[200]Human Rights Watch interview with Sarah (pseudonym), patient, Pantang Psychiatric Hospital, November 19, 2011.
[201]Human Rights Watch interview with Aisha (pseudonym), resident, Mount Horeb Prayer Camp, January 19, 2012.
[202]Human Rights Watch interview with Michael (pseudonym), a 38-year-old man with schizophrenia, Pantang Psychiatric Hospital, November 16, 2011; Human Rights Watch interview with John (pseudonym), patient, Accra Psychiatric Hospital, Accra, November 16, 2011; Human Rights Watch interview with Aisha (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011.
[203]Human Rights Watch interview with Michael (pseudonym), patient, Pantang Psychiatric Hospital, November 16, 2011.
[204]Human Rights Watch interview with Harriet (pseudonym), patient, Ankaful Psychiatric Hospital, November 24, 2011.
[205]Human Rights Watch interview with Daniel Kwame, ward in charge, Pantang Psychiatric Hospital, November 16, 2011.
[206]Human Rights Watch interview with Barnard Akumiah, member, Mental Health Society of Ghana, Accra, November 20, 2011.
[207]Criminal Code Act, 1960 (Act 29), as amended in 2003. Section 84 defines assault as “forceful touching of a person without their consent, and with the intention of causing harm, pain, or fear, or annoyance to that person” and according to section 86, the definition in section 84 provision applies regardless of whether the person is “capable of consenting due to a mental disability.”
[208] Human Rights Watch, letter faxed to Dr. Benjamin Kunbour, Ministry of Justice and Attorney General, Accra, Ghana, August 1, 2012. Human Rights Watch, email sent to Dr. Akwasi Osei, Chief Director, Ghana Health Service and director Accra Psychiatric Hospital, re: request for your opinion, July 29, 2012.
[209] Email communication between Human Rights Watch and Dr. Akwasi Osei, chief psychiatrist, Ghana Health Service, and director, Accra Psychiatric Hospital, in response to the email re: request for your opinion, August 21, 2012.
[210]Electroconvulsive therapy, also known as electroshock or ECT, is a controversial type of psychiatric shock therapy involving the induction of an artificial seizure in a patient by passing electricity through the brain. ECT is used to treat bipolar disorder and severe depression in cases where antidepressant medication, psychotherapy, or both have proven ineffective. See Doctors Lounge, http://www.doctorslounge.com/psychiatry/procedures/ect.htm, accessed on May 7, 2012.
[211]Human Rights Watch interview with Dr. Akwasi Osei, chief psychiatrist, Accra Psychiatric Hospital, November 16, 2011.
[212]Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (SR Torture Interim Report), 28 July 2008, UN Doc A/63/175, at [50].
[213]Hiroaki Inomata et al., Long Brief Pulse for Pulse-wave modified Electro-convulsive Therapy, arXiv:1112.2072v1 [q-bio.NC], December 9, 2011, accessed May 21, 2012). The World Psychiatric Association Position Statement on the Ethics of the Use of Unmodified Electroconvulsive Therapy (2009) explains the process of modified ECT to have emerged with the introduction of anesthesia and muscle relaxation prior to the administration of ECT. For more details, see, http://www.arabpsynet.com/Journals/ajp/ajp20.1-P57.pdf (accessed on June 29, 2012).
[214] Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (Special Rapporteur, Torture Interim Report), 28 July 2008, UN Doc A/63/175, at [50].
[215] Tina Minkowitz, “Abolishing Mental Health Laws to Comply with the Convention on the Rights of Persons with Disabilities,” in B. McSherry and P. Weller (eds), Rethinking Rights-Based Mental Health Laws (Portland: Hart, 2010) ch 7, p. 151.
[216] Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011.
[217] Human Rights Watch letter faxed to the Ministry of Health, Accra, Ghana, August 1, 2012.
[218] Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 16, 2011. The nurse told Human Rights Watch that parents bring children with disabilities because they cannot care for them. Other people in the ward have no parents, and are brought by the public. For example, one girl with an intellectual disability was brought by a nurse because community members threatened to kill her.
[219] Human Rights Watch interview with nurse, Accra Psychiatric Hospital, November 16, 2011.
[220] Human Rights Watch interview with Dr. Akwasi Osei, November 16, 2011. Mania is a mental condition marked by periods of great excitement, delusions, and over activity. See http://oxforddictionaries.com/definition/english/mania (accessed July 7, 2012).
[221]Human Rights Watch interview with a nurse, Accra Psychiatric Hospital, November 16, 2011.
[222]Human Rights Watch interview with a nurse, Accra Psychiatric Hospital, November 16, 2011.
[223]Human Rights Watch interview with Aminah (pseudonym), nurse, Accra Psychiatric Hospital, November 16, 2011.
[224] Human Rights Watch interview with Victoria (pseudonym), resident, Nyakumasi Prayer Camp, Central Region, January 19, 2012.
[225] Human Rights Watch interview with Prophet Leo Baidoo, director, Nyakumasi Prayer Camp, Central Region, January 19, 2012.
[226]Constitution, art. 28 (3).
[227] Ibid., art. 28 (4)
[228]Ibid., art. 28 (1)
[229] Children's Act, 1998 (Act 560), Ghana, December 30, 1998, art. 3, http://www.unhcr.org/refworld/docid/44bf86454.html (accessed September 11, 2012).
[230]Ibid., art. 2.
[231]Ibid., art. 10 (1) and (2)
[232] International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, G.A. Res. 2200A (XX1), 21 U.N. GAOR Supp. (No. 16) at 52, U.N. Doc. A/6316 (1966), 999 U.N.T.S. 171, entered into force March 23, 1976, acceded to by Ghana 07 September 2000.
[233] International Covenant on Economic, Social and Cultural Rights, G.A. res. 2200A (XXI), U.N. Doc. A/6316 (1966), entered into force January 3, 1976, acceded to by Ghana 07 September 2000.
[234] Convention on the Elimination of Discrimination Against Women (CEDAW), adopted 18 December 1979 by G.A. resolution 34/180, entered into force on 3 September 1981, ratified by Ghana 02 January 1986.
[235] Convention against Torture and Other Cruel Inhuman or Degrading Treatment or Punishment (CAT), adopted 10 December, 1984 and entered into force on 26 June 1987, in accordance with article 27(1) by General Assembly resolution 39/46
[236] Convention on the Rights of the Child, G.A. res. 44/25, annex, 44 U.N. GAOR Supp. (No. 49) at 167, U.N. Doc. A/44/49 (1989), entered into force September 2, 1990, ratified by Ghana 5 February 1990.
[237] Convention on the Rights of Persons with Disabilities (CRPD), adopted December 13, 2006 by G.A. Res. 61/106, Annex I, U.N.GAOR, 61st Sess., Supp. No. 49 at 65, U.N. Doc A/61/49 (2006), entered into force May 3, 2008, U.N. Doc. A/61/61, signed by Ghana on March 30, 2007 and ratified by Ghana on July 31, 2012.
[238]African [Banjul] Charter on Human and Peoples’ Rights, adopted June 27, 1981, OAU Doc. CAB/LEG/67/3 rev. 5, 21 I.L.M. 58 (1982), entered into force October 21, 1986, ratified by Ghana, 01/03/1989.
[239] Protocol to the African Charter on Human and Peoples' Rights on the Rights of Women in Africa (the Maputo Protocol), adopted July 11, 2003, entered into force November 2005, signed by Ghana in 2000, ratified by Ghana in 2007.
[240]African Charter on the Rights and Welfare of the Child, adopted (1990), entered into force Nov. 29, 1999OAU Doc. CAB/LEG/24.9/49, signed by Ghana 18/08/1997, but not yet ratified.
[241]ICESCR, art. 2 (1). ICCPR, art. 2(1). CEDAW, art. 5. CRC, art. 2 (1). ACHPR, art. 18 (4) and 28.
[242]CRPD, art. 3(b).
[243]Ibid., art. 5
[244]ICCPR, art. 7; CRC, art. 37; CRPD, art. 15; ACHPR, art.5.
[245]CAT, art. 1(1)
[246]CAT, art. 1(1)
[247]See General Comment No. 2 (2008) of the Committee against Torture on the implementation of article 2 of the Convention (CAT/C/GC/2), para. 17. See also U.N. Commission on Human Rights, Report of the Special Rapporteur on torture and cruel, inhuman or degrading treatment or punishment, Session 7, A/HRC/7/3, para. 31.
[248] U.N. Commission on Human Rights, Report of the Special Rapporteur on torture and cruel, inhuman or degrading treatment or punishment, E/CN.4/1986/15, para. 119.
[249]Civil Liberties Organization v. Nigeria, Communication 151/96: http://www.achpr.org/english/Decison_Communication/Nigeria/Comm.151-96.pdf, accessed on April 23, 2012.
[250]CRPD, art. 17. ACHPR, art. 4.
[251] ICCPR, art 9.
[252] ICCPR, art 9.
[253] UN Human Rights Committee, General Comment 8, art. 9, U.N. Doc HRI/GEN/1/Rev.1 at 8 (1994), para. 1.
[254] CRPD, art. 14.
[255] The so-called “ savings clauses ” of the treaties set out that the standards in the respective treaties cannot be used to undermine a higher standard or protection provided elsewhere in law (either international or domestic), and therefore represent only the minimum standard and may be improved.
[256] ACHPR, art.6.
[257] Prohit & Moore v. The Gambia, Communication No. 241/2001, para, 64.
[258] Ibid.
[259] U.N. Commission on Human Rights, Report of the Special Rapporteur on torture and cruel, inhuman or degrading treatment or punishment, A/63/175, July 2008
[260] CRPD, art. 14.
[261] Barbara Carter, Office of the Public Advocate, Victoria, Australia, ‘Supported Decision Making, Background and Discussion Paper’, November 2009, http://www.publicadvocate.vic.gov.au/file/file/Research/Discussion/2009/0909_Supported_Decision_Making.pdf, (accessed May 10, 2012).
[262] Gerard Quinn, ‘Personhood & Legal Capacity Perspectives on the Paradigm Shift of Article 12 CRPD’, HPOD Conference, Harvard Law School, 20 February 2010.
[263]Commissioner for Human Rights, Council of Europe, ‘Who Gets To Decide? Right to Legal Capacity for Persons with Intellectual and Psychosocial Disabilities’, CommDH/ Issue Paper (2012) 2, Strasbourg, 20 February 2012.
[264]Interim Report of the Special Rapporteur on Torture and other Cruel, Inhuman and Degrading Treatment or Punishment (SR Torture Interim Report), 28 July 2008, UN Doc A/63/175, at [50].
[265]CRPD, art. 12 (3).
[266]Barbara Carter, Office of the Public Advocate, Victoria, Australia, ‘Supported Decision Making, Background and Discussion Paper’, November 2009, http://www.publicadvocate.vic.gov.au/file/file/Research/Discussion/2009/0909_Supported_Decision_Making.pdf, accessed on May 03, 2012.
[267] United Nations enable, Handbook for Parliamentarians, ‘Legal Capacity and Supported Decision Making, http://www.un.org/disabilities/default.asp?id=242
[268] CRPD, art. 19.
[269] Ibid., art. 19.
[270] Ibid. art. 19(b).
[271] CRPD, art. 22.
[272] OHCHR, “Thematic Study,” http://www2.ohchr.org/english/bodies/hrcouncil/docs/10session/A.HRC.10.48.pdf, para. 50
(“The recognition of the right of persons with disabilities to independent living and community inclusion requires the shift of government policies away from institutions and towards in-home, residential and other community support services.”).
[273] CRPD, art. 16. ACHPR, art. 5.
[274] CRPD, art. 16.
[275] Ibid.
[276]UDHR, art. 25, ICESCR, art. 25, CRC, art. 25, CEDAW, art 12, CRPD, art. 25, ICESCR art, 12, CRPD art. 25, ACRWC, art 14.
[277] CESCR, General Comment No. 14, para 12(b)
[278] CRPD, art. 25(c).
[279] Ibid, art. 18 (4).
[280]Purohit and Moore V. The Gambia, para 80-81, A/63/175 July 2008.
[281]CRC, art. 25; CRPD, art. 6; ACRWC, art. 3.
[282] CRC, preamble.
[283] CRC art. 23.
[284]CRC, art. 3 (3).
[285]Organization of African Unity (OAU), African Charter on the Rights and Welfare of the Child (ACRWC), 11 July 1990, CAB/LEG/24.9/49 (1990), entered into force Nov. 29, 1999.
[286]ACRWC, art. 13 (1)
[287]Constitution, art. 29 (4).
[288]Ibid., art. 17 (1).
[289]Ibid., art. 94 (2) (b) (ii).
[290]Ibid., art. 14. (d)
[291]Persons with Disability Act, 2006, sec. 42.
[292]Ghana Country Report on the Implementation of the Madrid International Plan of Action Ageing (MIPAA), August, 2007, http://www.un.org/ageing/documents/review_map/GHANA.pdf (accessed September 10, 2012).
[293]National Disability Policy, Ghana, 2000.
[294]Human Rights Watch interview with Nancy Lucy Dzah, chief director, Department of Social Welfare, Ministry of Employment, and Social Welfare, Accra, January 23, 2012.
[295]The Mental Health Act. No. 846 was passed into law on March 4, 2012, after almost 12 years of negotiation. The new law seeks to regulate mental health issues in Ghana, and to repeal the 1972 Mental Health legislation, which the new law describes as “out of date and does not accord with best practice standards which aim to protect, promote the lives of citizens with mental disabilities,” http://www.graphic.com.gh/news/page.php?news=19294&title=Parliament+Passes+Mental+Health+Bill (accessed March 4, 2012).
[296]Mental Health Act, No. 846, 2012
[297] Ibid.
[298]Ibid.
[299]Mental Health Act, No. 846, 2012
[300]His Excellence John Evans Atta Mills, State of Nations Address, “Raising Ghana to the next level,” February 17, 2011, http://nppyouthuk.files.wordpress.com/2011/02/sona2011_final.pdf (accessed April 23, 2012).
[301]Godson Abekah Nkrumah, et al., “Financing the Health Sector in Ghana: A review of the Budgetary Process,” European Journal of Economics, Finance and Administrative Science, no. 17, 2009, http://www.eurojournals.com/ejefas_17_05.pdf (accessed June 4, 2012). It is reported that donor funding to the health sector was 13.8percent and 14.33 percent in 2006 and 2008 respectively.
[302]WHO, Ghana Mental Health Profile, 2003.
[303]WHO Country Cooperation Strategy 2008-2011, Ghana, WHO Regional Office for Africa, p. 24.
[304] Ibid., p. 5, http://www.afro.who.int/en/ghana/country-cooperation-strategy.html, (accessed May 20, 2012). The Country Cooperation Strategy (CCS) is the medium-term strategy for the WHO at the country level. It describes how the three levels of the Organization work at country level; taking into cognizance, the Common Country Assessment, the United Nations Development Assistance Framework (UNDAF), the WHO Medium Term Strategic Plan (2008 - 2013), and the various country policy and development papers.
[305] Human Rights Watch interview with Eunice Yaa Brimfah, Ackwerh, senior education specialist, World Bank Ghana, Accra, November 19, 2011.
[306] Human Rights Watch interview with Dr. Dante Ariel Mossi, senior country officer, World Bank Ghana, Accra, November 19, 2011.
[307] Ibid.
[308] Human Rights Watch interview with Eunice Yaa Brimfah, senior education specialist, World Bank Ghana, Accra, November 19, 2011.
[309]Department of Psychiatry, University of Ghana Medical School/Ministry of Health Partner, Mental Health Information Systems-Ghana, Mental Health and Poverty Project, Policy Brief, 2010, http://www.health.uct.ac.za/usr/health/research/groupings/mhapp/policy_briefs/MHPB16.pdf (accessed June 11, 2012).
[310]Human Rights Watch interview with Dr. Lyabode Olusanni, country representative, UNICEF Ghana, Accra, January 23, 2012.