Unjust and Unhealthy
HIV, TB, and Abuse in Zambian Prisons
Map of Zambian Prisons Visited
Fact Sheet
Table 1: Basic Statistics for Prisons Visited
|
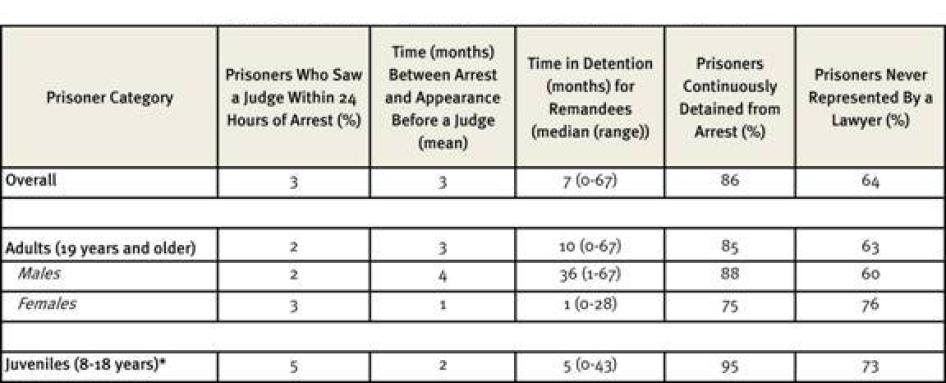
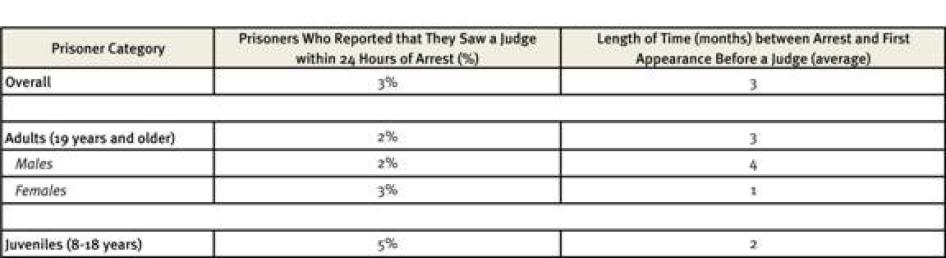
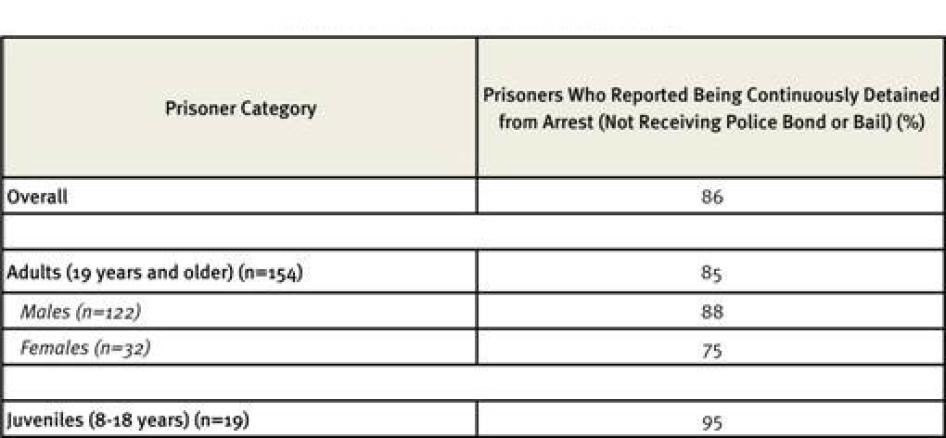
Table 2: Access to Justice for Prisoners Interviewed
*Under Zambian law, a prisoner under the age of nineteen years (the minimum age of criminal responsibility is eight years) is classified as a “juvenile,” despite the fact that under international law, 18 year-olds are adults. |
Categories of Prisoners Held in Zambian Prisons Under Zambian LawConvicted criminal prisoner (convict): A prisoner serving a sentence, having been found guilty of a criminal offense by a court. Unconvicted prisoner (remandee): Any person committed to custody by a court order or order of detention who is not a convicted criminal prisoner. Juvenile: Under Zambian law, a prisoner under the age of nineteen years (the minimum age of criminal responsibility is eight years) is classified as a “juvenile,” despite the fact that under international law, 18 year-olds are adults. Throughout this report, the term “juvenile” will be used to designate the category of prisoners ages eight to 18 held in Zambian prisons when necessary to refer to the classification used by the government. Otherwise, individuals in prison under age 18 will be referred to as “children” in accordance with the Convention on the Rights of the Child. Prohibited Immigrant: A prisoner detained under a broad range of alleged immigration-related violations, including visitors with an expired permit to remain in Zambia, individuals entering Zambia without being able to establish a valid passport, and persons previously deported from Zambia. Throughout this report, individuals detained under the “prohibited immigrant” classification will be referred to as “immigration detainees”. |
Summary
I have seen people die in the night in the cell—there is nothing we can do. We shout for someone, but the guards will say, “he is just playing sick, he wants to escape. Let us wait two or three days, and see how he will be.” And then he dies.
– Nickson, 36, Mukobeko Maximum Security Prison, September 30, 2009
They say, “you’re going to Chimbokaila [Lusaka Central Prison]? It’s a death sentence.” Not because they are afraid you will be given beatings, but because of TB. They know the conditions are bad.
– Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, Lusaka, February 6, 2010
People who break the law should be held accountable. The appropriate punishment may be imprisonment. But for detainees in Zambian prisons—a third of whom have never been convicted of any crime—being held behind bars can have life-threatening consequences. Overcrowding, malnutrition, rampant infectious disease, grossly inadequate medical care, and routine violence at the hands of prison officers and fellow inmates make Zambian prisons death traps.
Zambia’s prison system is in crisis. Built to accommodate 5,500 prisoners before Zambian independence in 1964, the country’s prisons housed 15,300 in 2009. Between September and October 2009, the Prisons Care and Counselling Association (PRISCCA), AIDS and Rights Alliance for Southern Africa (ARASA), and Human Rights Watch visited six facilities, two of which were filled at 573 percent and 622 percent of capacity, respectively. Some inmates are forced to sleep seated, or in shifts.
Inmate health problems are compounded by practices prohibited under international law as inhuman and degrading treatment or as torture, such as corporal punishment and “penal block” isolation practices, where prisoners are stripped naked and left in a small, windowless cell while officers pour water onto the floor to reach ankle or mid-calf height. There is no toilet in the cell, so inmates must stand in water containing their own excrement. Certain inmates—appointed as “cell captains” by officers—are also invested with disciplinary authority and mete out the overwhelming majority of punishments, through night-time “courts” in their cells and beatings. Beatings are particularly harsh when aimed at inmates engaging in same-sex sexual activity, and at prisons with associated farm facilities, where inmates’ hard labor conditions closely resemble slave labor.
Water is unclean or unavailable; soap and razors are not provided by the government. The food provided by the Prisons Service is so insufficient and nutritionally inadequate that food has become a commodity traded for sex or labor in the prisons.
In October 2009, the Zambia Prisons Service employed only 14 health staff—including one physician—to serve its 15,300 prisoners. Of Zambia’s 86 prisons, only 15 had any health clinic or sick bay, many of these with little capacity beyond distributing paracetamol. For those prisons without a clinic—and for more serious medical conditions at those with a clinic—access to care is controlled by medically unqualified and untrained prison officers. Lack of adequate prison staff for the transfer of sick prisoners—as well as lack of transportation and fuel—and security fears also conspire to keep inmates from accessing medical care outside of the prisons, in some cases for days or weeks after they fall ill.
Even while largely unknown and unmeasured, tuberculosis (TB) transmission is a constant and serious threat in the prisons’ cramped, dark, unventilated cells. Suspected prevalence rates are very high, with the Zambia Prisons Service reporting an incidence rate for TB of 5,285 cases per 100,000 inmates per year. Rates in Zambia outside of prison in 2007 were less than one-tenth as high.
Only 23 percent of prisoners we interviewed had been tested for TB. The conditions at each of the prisons we visited—combining overcrowding, minimal ventilation, and a significantly malnourished and weakened population—are ripe for the quick spread of TB. The TB isolation cells designed to house the ill are in such poor condition that even the physician in charge of the prison medical directorate deems them “death traps”—yet, since they are slightly less crowded than standard cells, inmates who completed TB treatment told us that they sometimes chose to remain in the cells with inmates with active TB so as to avoid the worst of the desperate overcrowding elsewhere.
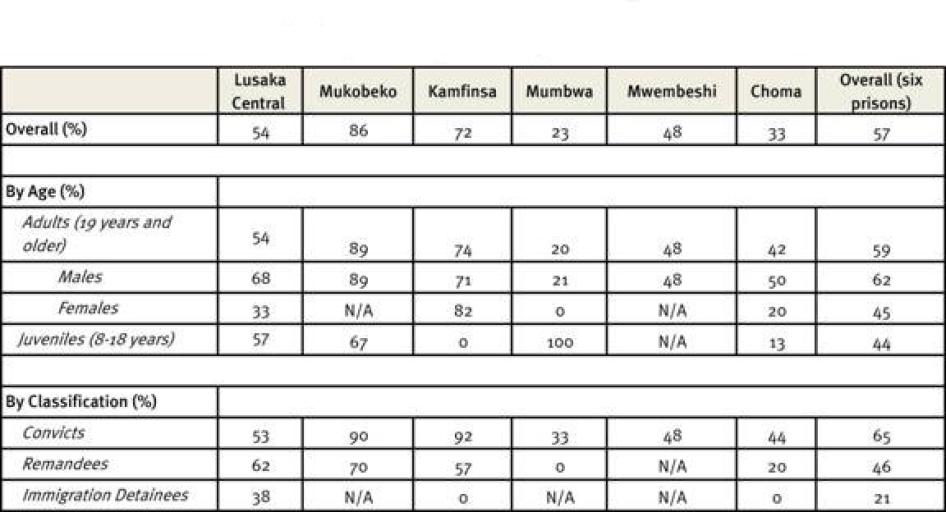
The prevalence of HIV in Zambian prisons was last measured at 27 percent—nearly double that of the general adult population (15 percent). To the credit of Prisons Service officials and non-governmental organization (NGO) partners, in recent years the prisons have expanded HIV testing, so that 57 percent of the prisoners we interviewed across all six facilities we visited had been tested. However, access was uneven: Larger prisons had significantly higher levels of testing than smaller prisons, and men were more likely to be tested than women and juveniles. Access to anti-retroviral therapy (ART) for HIV treatment has also improved among the prison population in recent years, particularly in the larger prisons. However, proper treatment is impossible in the absence of prison-based health services.
According to the prisoners we spoke with, sexual activity between male inmates is common, including both consensual sex between adults, and relationships where sex is traded by the most vulnerable in exchange for food, soap, and other basic necessities not provided by the prison. PRISCCA, ARASA, and Human Rights Watch also documented cases of rape between male prisoners. The total ban on condoms, however, in the context of common sexual activity and rape, creates a serious risk of HIV transmission and presents a major obstacle to HIV prevention.
This report is the first analysis of prison health conditions in Zambia by independent human rights organizations. In preparing this report, PRISCCA, ARASA, and Human Rights Watch interviewed 246 prisoners, eight former prisoners, 30 prison officers, and conducted facility tours at six prisons throughout the central corridor of Zambia. The purpose of this research was to understand health conditions and human rights violations in Zambian prisons, and to provide recommendations for a future which respects the basic rights and minimum standards due to prisoners.
Good prisoner health is good public health. Prisoners come from and mostly return to the community, carrying infectious diseases from one to the other. Prison officers are also daily exposed to the conditions and health risks in prison and can expose their families and contacts outside of prison. While certainly poverty and access to healthcare are issues in the Zambian general population, the government nevertheless has an obligation to ensure basic minimum standards for detainees and medical care at least equivalent to that available in the general population, in order to protect both prisoners’ rights and public health. Resource constraints notwithstanding, the Zambian government has a binding and non-negotiable obligation not to expose people to conditions of torture and cruel, inhuman, or degrading treatment, which it currently violates when sending people to prison.
Contrary to international standards, convicted, unconvicted, and immigration detainees—children and adults—are held together, equally subject to the prisons’ grossly inadequate conditions. Detainees in each of these categories, men as well as women, face particular challenges in their confinement.
Prisoners who have yet to face trial—routinely held at every facility with convicted prisoners in violation of international and Zambian law—are held on remand for extended periods, exacerbating prison overcrowding. Interviews with inmates, prison officials and NGOs found such problems as police investigation failures, lack of bail, and lack of representation for accused persons keep individuals unnecessarily, and often unlawfully, incarcerated for extended periods of pre-trial detention. The large number of remand prisoners is a result of failures in the criminal justice system as a whole, including the Zambian judiciary, Police, and Prisons services. At Mukobeko Maximum Security Prison, one prisoner told us that he spent three years and seven months awaiting even an initial appearance before a magistrate or judge; another prisoner, now convicted and living at Lusaka Central Prison, told us that he had spent 10 years as an unconvicted prisoner awaiting resolution of his case. The incarceration of unconvicted detainees is clearly a major contributing factor to the prisons’ extreme overcrowding: At Lusaka Central Prison, 601 of the 1145 inmates—more than half—are remandees. Overall, 35 percent of the Zambian prison population is composed of remandees. Even given Zambia’s grossly inadequate prison conditions, the current cost to the government of incarcerating remand detainees unnecessarily for extended periods is not insignificant, and savings could likely be generated by increasing the use of bail instead of pre-trial detention.
Immigration detainees—including administrative detainees held pending deportation—are frequently detained and await deportation without due process, mingled with convicted and remandee prisoners. Among the immigration detainees PRISCCA, ARASA, and Human Rights Watch interviewed, only 38 percent had ever seen a magistrate or judge, compared with 97 percent of non-immigration detainees. Many who were detained appeared to have reasonable claims to legal status. Immigration detainees are routinely told to pay for their own deportation and are held until they pay.
Children held in detention are entitled to particular protections under international law. Children should be detained only as a last resort, and for the shortest appropriate time; children who are detained should be separated from adults. However, in Zambia, children are routinely incarcerated for minor offenses, often after criminal processes in which they have not had any legal representation. Held together with adults (including adults incarcerated on charges of defilement of a minor) at some facilities, detained children are exposed to the risk of rape.
Women detainees are entitled to specific protections under regional human rights standards, but incarcerated women in Zambia do not have their unique healthcare needs met. Women’s health services including gynecological care and cervical cancer screening are non-existent. Pre-natal services are absent or inadequate, and there is no HIV Prevention of Mother-to-Child Transmission (PMTCT) program under the prison medical directorate. The already nutritionally inadequate prison food is unchanged for nursing or pregnant women.
Compounding these injustices and overcrowding is injustice within the criminal justice system. The Zambian police and Drug Enforcement Commission (DEC) enjoy broad powers under Zambian law, and police and DEC officers reportedly arrest and hold numerous alleged family members, friends, and innocent by-standards as “co-conspirators” when their primary targets cannot be found. Such arrests, which may or may not comply with Zambian law, are considered arbitrary arrests—and therefore unlawful—for the purpose of international standards on the deprivation of liberty. Lack of non-custodial sentencing, restrictions on the use of parole, and delays in appeals further contribute to overcrowding.
Under international human rights law, prisoners retain their human rights and fundamental freedoms, except for the restrictions on rights necessitated by the fact of incarceration itself. States are required to ensure prisoners a standard of health care equivalent to that available to the general population, a commitment acknowledged by the Zambia Prisons Service.
The Zambian government has repeatedly committed itself to uphold the human rights of prisoners through its assumption of international and regional obligations. As a state party to the International Covenant on Civil and Political Rights, the Convention Against Torture, the International Covenant on Economic, Social and Cultural Rights, the Convention on the Elimination of All Forms of Racial Discrimination, the Convention on the Elimination of All Forms of Discrimination Against Women, the Convention on the Rights of the Child, and the African [Banjul] Charter on Human and Peoples’ Rights and its protocol on the rights of women, Zambia has an obligation to ensure that its criminal justice and penitentiary standards comply with international and regional human rights standards, to ensure that detainees are treated with appropriate dignity and full respect for their human rights, and to prevent all forms of cruel, inhuman, or degrading treatment.
Clearly, resource constraints are a major consideration, but greater priority on prison funding needs to be put at the national level and greater support from international donors needs to be forthcoming if change is to be effected. Some necessary reforms—particularly legal reforms—are resource-neutral; those that aren’t are crucial to the realization of the rights of prisoners and are the responsibility of both the national government and international donors.
To address existing human rights violations in its prisons, the Zambia Prisons Service should immediately reform prison disciplinary systems to discontinue current abusive disciplinary practices, and end the use of cell captains to carry out brutal punishments on behalf of prison officials. Prisoners should not be punished for sexual or other kinds of intimacy, except in cases of rape.The Prisons Service should immediately install a clinical officer at each prison to assess health and review prisoner medical complaints. In the intermediate and longer term, the Prisons Service—in collaboration with the Parliament and international donors—should secure enough funding for the prison budget to ensure conditions consistent with international standards and scale up prison-based medical care.
Furthermore, in order to alleviate the failings in the criminal justice system that exacerbate overcrowding and violate the rights of prisoners, the Zambian Parliament, judiciary, Police Service, and Prisons Service need to work together to decrease arbitrary arrests, increase the use of bail, and reduce judicial delays. Significant effort should be made to scale up the use of parole and non-custodial alternatives to incarceration. Every prisoner, including child detainees, should be able to exercise their right to have a lawyer of their choosing. Only with cooperation between these bodies, and with the assistance of international agencies, donors, and NGOs, will the rights of prisoners and the goal of prisoner rehabilitation be fully realized.
Zambia’s prison system is at a pivotal moment for change to bring the conditions in its prisons in line with its international and national commitments to prisoner health. The Zambia Prisons Service, in conjunction with PRISCCA and other stakeholders, has itself recently completed an audit of Zambia’s 53 standard prisons, research that included detailed information on prison facility conditions and a list of prisoners at each facility in need of special assistance. Having acknowledged the problems in the prison system, conducted an internal audit, appointed a new medical director, and granted access to human rights monitors, the Zambia Prisons Service has shown a desire and openness to improvement. By building on the observations in its own audit, those of outside human rights groups, and collaborating with Parliament, the judiciary, the immigration service, the police, and international agencies, donors, and NGOs, the Zambia Prisons Service has the opportunity to improve the welfare of its prisoners, and to become a regional model in doing so.
Key Recommendations
For Immediate Implementation
- The President of Zambia should issue a public statement identifying prison conditions and health as a national crisis and should establish a high-level inter-ministerial task force to urgently develop a national prison health plan
- The Zambian Parliament should amend the law to limit the powers to carry out sweeping, group arrests in violation of international law currently enjoyed by the police and Drug Enforcement Commission
- The Zambian Parliament should address overcrowding by taking steps to expand parole eligibility by amending the Prisons Act and Prisons Rules
- The Zambia Prisons Service and Ministry of Home Affairs should prohibit the use of penal block practices, and discipline staff and inmates for abuses against prisoners
- The Zambia Prisons Service and Ministry of Home Affairs should establish the presence of a clinical officer at each prison who can judge prisoner health complaints and facilitate access to outside Ministry of Health medical facilities
- The Zambia Prisons Service and Ministry of Home Affairs should provide condoms to all prisoners and prison officers, in conjunction with education on harm reduction to increase condom acceptance
- The Ministry of Justice should issue guidelines for bail administration to encourage increased defendants’ instruction in bail rights and increased granting of bail, considering accurate information about household incomes in Zambia
- International agencies, donors, and NGOs should integrate discussion of prison health into existing technical advisory committees to the Zambian government
For Intermediate-Term Implementation
- The Zambia Prisons Service and Ministry of Home Affairs should consistently separate children and adults, and convicted, remand, and immigration detainees
- The Zambian Parliament should allocate funding for supervision of community-based sentences
- The Zambian Parliament should repeal or amend Sections 155, 156, and 158 of the Penal Code in order to decriminalize consensual sexual conduct among adults, and implement gender-neutral laws to protect adults and children from sexual violence and assault
- International agencies, donors, and NGOs should fund and supplement direct health service programs in prisons including TB testing and treatment; women and children’s health; and nutrition support
- The Zambian judiciary and Ministry of Justice should ensure all detainees, including those under 18, have access to a lawyer of their choice
- The Ministry of Health should develop a detailed plan for the improvement of prison health services and conditions as part of its National Health Plan 2011-2015
For Long-Term Implementation
- The Zambian Parliament should secure and international donors should assist with securing enough funding for the prison budget to ensure conditions consistent with international standards. Funding should be sought for facility renovation, upgrading water and sanitation facilities, adequate food, the provision of basic necessities, and adequate prison-based health services
- The Zambia Prisons Service and Ministry of
Home Affairs should establish clear guidelines on the provision of prison-based
health services, and scale up those services to:
- Conduct health screening of all prisoners upon entry and at regular intervals
- Provide TB screening to all inmates entering prison, and all existing inmates, and ensure prompt initiation on treatment for those with confirmed disease
- Offer voluntary HIV counseling and testing to all inmates entering prison and all existing inmates and prompt initiation on anti-retroviral treatment
- Establish clinics at each prison with a consistent supply of essential medications and a minimum capacity to conduct TB and HIV testing and treatment
- Ensure access to antenatal services, including PMTCT, early infant testing, and ART for infants
Methodology
This report is based on information collected during four weeks of field research conducted by the Prisons Care and Counselling Association (PRISCCA), the AIDS and Rights Alliance for Southern Africa (ARASA), and Human Rights Watch in September-October 2009 and February 2010. The Zambian Ministry of Home Affairs granted permission for access to six prisons and to conduct confidential interviews with inmates and staff, with access provided by the Zambia Prisons Service. Researchers interviewed 246 prisoners, eight former prisoners, 30 prison officers in charge and officers, and conducted facility tours at six prisons throughout the central corridor of Zambia. 232 of the prisoners interviewed completed a survey providing information about the prisoner’s incarceration history, medical care, and HIV/AIDS and TB testing and treatment.
Researchers visited six facilities: Lusaka Central Prison (Lusaka province), Mukobeko Maximum Security Prison (Central province), and Kamfinsa State Prison (Copperbelt province); one rural district prison: Mumbwa Prison (Central province); and two peri-urban prisons: Mwembeshi Commercial Open Air Farm Prison (Central province), and Choma State Prison (Southern province).
Researchers also interviewed 28 representatives from local and international organizations working on prison, HIV/AIDS, and health issues, and donor governments and agencies.
Researchers engaged repeatedly with Zambian government officials throughout the course of this research. The research commenced with a workshop, attended by the commissioner of prisons, officers in charge and officials of the Zambia Prisons Service, to introduce the research and identify key prison health concerns of prison officers and officials. Researchers also conducted 18 interviews with officials from the Ministry of Home Affairs, Ministry of Health, Zambia Prisons Service, police and immigration services, the Drug Enforcement Commission, the National HIV/AIDS/STI/TB Council, and the National Human Rights Commission. Researchers toured Lusaka Central Prison, the prison clinic, and the University Teaching Hospital accompanied by Dr. Chisela Chileshe, the director of prison medical services. PRISCCA, ARASA, and Human Rights Watch lodged a letter with the commissioner of prisons requesting the Prisons Service’s Annual Reports and statistics on prison staffing, deaths in custody, reports of those who are ill in custody, and reports of assaults and disease in prison custody in accordance with Zambian law requirements that such records be kept [see Appendix]. As of this writing, our request had not been answered. PRISCCA, ARASA, and Human Rights Watch also lodged a letter with the Drug Enforcement Commissioner requesting copies of records or reports on the number and charges of individuals arrested, convicted, and incarcerated in Zambia on drug-related charges. As of this writing, that request had also not been answered.
In each prison visited, the research team requested from the officer in charge a private location to conduct interviews with a cross-section of prisoners held in that facility, including female prisoners, immigration detainees, juveniles,[1]and pre-trial detainees. Priority was given to the inclusion of prisoners from each category rather than proportional representation. Officers identified prisoners who were then provided an explanation of the survey, asked if they were willing to participate, and assured of anonymity in the final report.
Table 3: Prisoner Characteristics
Interviews were conducted in English, French, Bemba, Nyanja, and Tonga, with translation provided by PRISCCA members. Individuals participating were assured that they could end the interview at any time or decline to answer any questions without any negative consequence. The names of all prisoners interviewed and quoted in this report have been changed to protect their identity and for their security.
The average length of time prisoners we interviewed had spent in prison varied widely, ranging from an average of less than one month for adult females at Mumbwa Prison, to an average of 44 months for adult men at Mukobeko Maximum Security Prison. The prisoners we interviewed across prisons had an average age between 30 and 40, and most were of Zambian nationality, though non-Zambian nationals were more common at Lusaka Central and Kamfinsa prisons. Male prisoners had more frequently achieved secondary or higher education than female prisoners. The percentage of married prisoners ranged from 41 at Lusaka Central to 70 at Mwembeshi.
Table 4: Prisoner Interviewee Demographics
Background
The Prisons of Zambia
Despite international and national legal commitments to prisoner health, observers have noted in recent years that conditions in Zambia’s prisons are grossly inadequate.[2] Zambia’s prisons were built prior to 1964 to accommodate 5,500 prisoners.[3] In October 2009, they housed 15,300—nearly three times official capacity.[4] In 2005, when the total national prison population was 14,427, nearly 35 percent of those were remand prisoners awaiting trial (including 230 remanded juveniles).[5] Women constitute 2.6 percent of the total convicted prison population in Zambia.[6]
Zambia has a total of 86 prisons throughout the country, 53 of them standard prisons and 33 open air/farm prisons. One of these facilities is dedicated exclusively to juveniles, and one exclusively to women, though juveniles are incarcerated with the adult population at other facilities throughout the country, and women live in separate sections of additional facilities throughout the country.
Zambia’s Prison Population[7]2005 Total Population: 14,427 Adult Convicts: 8,658 Adult Remandees: 4,938 Immigration Detainees: 294 Condemned Prisoners: 273 Remandee Juveniles: 230 Convicted Juveniles: 79 Mentally Ill Prisoners: 25 |
Source: Zambia Human Rights Commission, “Annual Report: 2005”
By law, the Zambia Prisons Service is established for the management and control of prisons and the prisoners they hold.[8] International law requires that penitentiary systems’ “essential aim” is prisoners’ “reformation and social rehabilitation,”[9] and Zambia’s system espouses the goals of both order and reform.[10]
Zambian law establishes minimum standards for medical care, and requires that the officer in charge of each prison maintain a properly secured hospital, clinic, or sick bay within the prison.[11] A serious gap exists between these legal requirements and practice, with little or no medical care available at most of Zambia’s 86 prisons. Only 15 of Zambia’s prisons include health clinics or sick bays, and many of these clinics have little capacity beyond distributing paracetemol.[12] In February 2010, the Zambia Prisons Service employed only 14 trained health staff—one physician, an administrative rather than a clinical role, one health environmental technician, nine nurses, and three clinical officers[13]—with 11 prospective staff still in training.[14] “The ratio is out of this world,” Dr. Chisela Chileshe, the physician in charge of the prison medical directorate, concluded, referring to the ratio of medical staff to the inmates under their care.[15]
While there are some Ministry of Health medical staff seconded to work in the prisons, they are often present there only a few days a week, and there is only one Ministry of Health physician who visits the prisons.[16]Coordination between prison health officials and Ministry of Health officials has been minimal. The National Health Strategic Plan 2006-2010, designed to lay out how to achieve national health priorities through goals for government, health workers, cooperating partners, and other key stakeholders, includes no mention of prisons.[17]
Donors have actively supported health initiatives in Zambia, though relatively little of this assistance has gone to government or NGO-based prison health initiatives thus far. For HIV/AIDS alone, in 2009 the United States contributed over US$262 million and the Global Fund contributed over $137 million to Zambia, with other major HIV/AIDS donors including the European Union, Sweden, Denmark, Norway, the Netherlands, and the United Kingdom.[18] In 2008, the National HIV/AIDS/STI/TB Council analyzed HIV/AIDS spending in Zambia. That assessment listed no amount for aid to prisoners in 2005 and $76,300 in 2006.[19] Some NGOs have received grants for prison-based health work—for example, in 2006 the Prisons Fellowship of Zambia in Lusaka and Ndola each received $10,506 as Global Fund Sub-Recipients,[20] the Go Centre/CHRESO Ministries, which provides HIV testing and treatment at several prisons, is funded by the US President’s Emergency Plan for AIDS Relief,[21] and USAID funds an HIV prevention, treatment, care and support (“SHARe”) program which operates in some prisons.[22] Funding problems for both Prisons Service and Ministry of Health services will be compounded by the fact that, as a result of a corruption scandal at the Ministry of Health, Global Fund funding to Zambia has been halted pending an audit.[23]
Funding to improve the prisons generally is inadequate.[24] In 2010, the Zambian national budget was over 16 trillion Zambian kwacha ($3,376,810,000), 14.5 percent of which was financed through partners.[25] The Zambia Prisons Service 2010 budget was 52 billion Zambian kwacha ($10,974,600).[26] The Prisons Service has never been funded by the Ministry of Finance to its requested amount.[27] NGOs note that every year, the Prisons Service is the least funded of the services under the Ministry of Home Affairs.[28]
Prison medical services particularly suffer from lack of funding. Despite a comprehensive strategic plan on HIV/AIDS/STI/TB, according to the Ministry of Home Affairs HIV/AIDS focal point person Gezepi Chakulunta, “we haven’t done much on the strategic plan because of lack of funding.”[29] Dr. Chileshe explained that plans to expand prison health services were likewise hampered by lack of funding. He has plans for a directorate which will include a head office and prison-based services, a physician in each of the country’s nine regions, a referral hospital for prisoners, and clinics in all the prisons, but funding for such a system remains uncertain.[30]
Prison-based medical care under the medical directorate (aside from seconded Ministry of Health employees and medications) comes out of the prison budget (under the Ministry of Home Affairs), rather than the Ministry of Health budget. In 2009, a budget for prison medical services did not exist.[31] For 2010, Dr. Chileshe reported that “my budget will be 200 million kwacha [$42,210] per year ... about 16.6 million per month [$3,503] excluding salaries....I do not have enough to do all that we want.”[32] By contrast, to have a clinical officer and clinic at each of the 53 standard prisons (still leaving 33 open air prisons without a Prisons Service clinic), he said, would cost about 26 billion kwacha ($5,487,320).[33]
HIV and TB in Zambia and the Prison System
While HIV prevalence among Zambian adults is 15 percent,[34] available evidence suggests that HIV prevalence in Zambian prisons is significantly higher. A study conducted in 1998-99 in three Zambian prisons found a male HIV prevalence of 27 percent, and a prevalence of 33 percent among female inmates.[35] Based on these data, prevalence has until recently been routinely estimated at 27 percent of the overall prison population.[36] HIV/AIDS has had deadly consequences in the prison population, among officers and inmates: Between 1995 and 2000, an estimated 2,397 inmates and 263 prison staff died from AIDS-related illnesses.[37]
In the general population, in 2004, the Zambian government introduced free access to anti-retroviral therapy (ART) in the public health sector. In June 2005, the government declared the ART service package (including counseling, x-rays, and CD4 testing[38]) free of charge.[39] The Zambian National HIV/AIDS Policy includes prisoners and commits to providing HIV prevention information, voluntary counseling and testing upon admission to custody, and detection and treatment programs to prisoners.[40]
Since its commitment to free treatment in the public health sector, Zambia has been making progress in treating its HIV-positive population. Between 2004 and 2007, the number of people on ART jumped from 20,000 to 151,000, an increase from seven percent coverage of those requiring it to 46 percent.[41] The estimated percentage of women living with HIV who received ART to prevent mother-to-child transmission increased from 18 percent in 2004 to 47 percent in 2007.[42] However, Zambian HIV/AIDS NGO representatives report that access to ART in rural areas is significantly more limited than that in urban areas, and there is also a sizable difference between medical infrastructure and personnel availability between urban and rural areas.[43] Access or further expansion is uncertain with the suspension of Global Fund grants, pending corruption investigations.
Such a high HIV prevalence, coupled with poor prison conditions, raises a significant risk of tuberculosis (TB) infection. As well as being the most common opportunistic infection among people living with HIV in Africa, TB is pervasive in southern African prisons because of overcrowding, poor ventilation, and lack of prevention practices such as prompt identification and treatment of persons with active TB.[44]A 2000-2001 study in 13 Zambian prisons for pulmonary TB among inmates concluded that a high rate of pulmonary TB exists in Zambian prisons, speculating that true prevalence rates may approach 15-20 percent, with significant rates of drug resistance and multi-drug resistant TB[45] (MDR-TB).[46]Indeed, with mortality rates as high as 24 percent, tuberculosis is among the main causes of death in prisons in developing countries.[47]Worldwide, TB is the “leading infectious killer for people living with HIV”, responsible for an estimated 13 percent of AIDS deaths.[48]
In the general population, Zambia bears a heavy burden of TB, with a prevalence of 387 cases of all forms of TB per 100,000 members of the population in 2007 and 115 TB-related deaths per 100,000 members of the population in that year.[49] In 2009, there were 50,000 cases of TB throughout the country.[50] MDR-TB comprised 1.8 percent of all new TB cases in 2007. Yet Zambia has also been making progress in treating TB in the general population: Between 2000 and 2006, the coverage of Directly Observed Treatment, Short-course (DOTS) expanded significantly.[51] For new sputum smear-positive cases, between 1999 and 2007, the treatment cure rate rose from 50 percent to 78 percent; the treatment success rate rose from 69 percent to 85 percent.[52] However, difficulties in screening, diagnosing and treating various forms of TB—particularly extra-pulmonary TB—continue to contribute to difficulties in establishing an effective response to the disease nationwide.[53]
In the prison population, suspected prevalence rates are very high, though reliable data do not exist.[54] The physician in charge of the prison medical directorate reported that TB is the leading cause of death in the prisons;[55] he acknowledged that “the prisons are a breeding ground for TB/HIV” and has recognized the impact of prison conditions on the spread of TB.[56] The Zambia Prisons Service has reported a case infection rate for TB of 5,285 cases per 100,000 inmates per year.[57]
At Mumbwa prison, a prison officer reported that with a prison population of 354, only four prisoners had been tested for TB in the previous year—and all four were found to be positive.[58] High HIV prevalence compounds the dangers posed by TB: As the HIV/AIDS coordinator at Lusaka Central prison aptly noted, “People with compromised immune systems are vulnerable to TB. Ventilation is very poor at the prison. People with HIV catch TB easily.”[59]
Zambia’s Obligations Under International, Regional, and Domestic Law
The Zambian government is obliged under national and international law to protect the rights of prisoners and those in its custody.
On the international level, Zambia is a party to core regional and international human rights treaties. These include the International Covenant on Civil and Political Rights (ICCPR), the Convention Against Torture (CAT),[60] the International Covenant on Economic, Social and Cultural Rights (ICESCR),[61] the Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW),[62] the Convention on the Rights of the Child (CRC),[63] the Convention on the Elimination of All Forms of Racial Discrimination (ICERD),[64] the African Charter on Human and Peoples’ Rights,[65] and the Protocol to the African Charter on Human and Peoples’ Rights on the Rights of Women in Africa.[66] These treaties provide for the protection of basic civil and political rights and also ensure specific guarantees relating to the treatment and conditions in custody for those deprived of their liberty. These treaties are supplemented by instruments specific to the treatment of those in detention, discussed below.
On the national level, key protections are laid down in the Constitution and The Prisons Act and Rules of the Laws of Zambia.
Prisoners’ Rights
Under international human rights law, prisoners retain their human rights and fundamental freedoms, except for such restrictions on their rights required by the fact of incarceration; the conditions of detention should not aggravate the suffering inherent in imprisonment,[67] except as necessary for justifiable segregation or the maintenance of discipline.[68]This rule cannot be dependent on the material resources available to the national government in question.[69]
The most fundamental protection for prisoners is the absolute prohibition on torture. As well as being a well-established norm of international law by which Zambia is bound, the prohibition is also reflected in the Zambian Constitution, and in several of the human rights treaties to which Zambia is a party.[70] The ICCPR and the CAT prohibit torture and cruel, inhuman, or degrading treatment or punishment without exception or derogation. Article 10 of the ICCPR further requires that “[a]ll persons deprived of their liberty shall be treated with humanity and with respect for the inherent dignity of the human person.”[71] The African Charter on Human and Peoples’ Rights also protects every individual’s human dignity and prohibits “all forms of exploitation and degradation,” including slavery, torture, and cruel, inhuman or degrading punishment and treatment.[72]
The CAT defines torture and cruel, inhuman or degrading treatment or punishment to include not only acts committed by public officials, but also acts committed with their acquiescence.[73] Thus, prison officials are responsible for all abuses in prison committed by inmates with their acquiescence.
Numerous international instruments provide further guidance on the protection and respect of human rights of persons deprived of their liberty. The most comprehensive such guidelines are the United Nations (UN) Standard Minimum Rules for the Treatment of Prisoners. Other relevant instruments include the Body of Principles for the Protection of All Persons under Any Form of Detention or Imprisonment and the Basic Principles for the Treatment of Prisoners.[74]
International law and standards guarantee imprisoned children special protections. The Convention on the Rights of the Child protects children from torture or other cruel, inhuman or degrading treatment or punishment, and provides that children deprived of their liberty shall be treated with humanity and respect for the inherent dignity of the person.[75] Detention of a child “shall be used only as a measure of last resort and for the shortest appropriate period of time.”[76] For those children who are detained, they are to be separated from adults.[77] The United Nations Standard Minimum Rules for the Administration of Juvenile Justice lays out additional protections for children deprived of their liberty.[78]
Women detainees also benefit from special legal protections. Regional law provides that women in detention should be held in an environment “suitable to their condition” and ensures their right to be treated with dignity.[79] The Southern African Development Community Protocol on Gender and Development, which Zambia has signed, commits states by 2015 to “ensure the provision of hygiene and sanitary facilities and nutritional needs of women, including women in prison.”[80]
The Right to Health
All people have a right to the highest attainable standard of health.[81]The International Covenant on Economic, Social and Cultural Rights requires states parties to take steps individually and through international cooperation to progressively realize this right via the prevention, treatment, and control of epidemic diseases and the creation of conditions to assure medical service and attention to all.[82] African regional law also supports the right to health.[83] “Progressive realization” demands of states parties a “specific and continuing obligation to move as expeditiously and effectively as possible towards the full realization of [the right].”[84]The concept of available resources is intended to include available assistance from international sources.[85]
States have an obligation to ensure medical care for prisoners at least equivalent to that available to the general population.[86] According to the Economic, Social and Cultural Rights Committee, the monitoring body for the Covenant on Economic, Social and Cultural Rights, “States are under the obligation to respect the right to health by, inter alia, refraining from denying or limiting equal access for all persons, including prisoners or detainees, minorities, asylum seekers and illegal immigrants, to preventive, curative and palliative health services.”[87]Furthermore, the ICCPR requires that governments should provide “adequate medical care during detention.”[88] The Committee Against Torture—the monitoring body of the Convention Against Torture—has found that failure to provide adequate medical care can violate the CAT’s prohibition of cruel, inhuman or degrading treatment.[89]
Thus, international human rights law explicitly protects prisoners against discrimination in receiving health care. The Zambia Prisons Service has acknowledged this commitment: “It has been decreed in various Charters, Conventions and International Instruments that all prisoners, irrespective of nationality, race or gender are entitled to the same quality of health care as that available outside jail.”[90]
Prison Conditions and Consequences for Detainees’ Health
These conditions defeat the purpose of rehabilitation. You cannot subject people to this and expect them to reform. It’s so tough and rough that it is survival of the fittest. A person who walks in a good person, before serving one fourth of their sentence, they become a beast. They leave deformed. These conditions destroy us mentally and physically.
– Winston, 35, Mukobeko Maximum Security Prison, September 29, 2009
All prisoners are due respect based on their inherent dignity as human beings.[91] The requirement to take positive steps to ensure minimum guarantees of humane treatment for persons within their care[92] implies an obligation on states “to fulfil and protect the various human rights of detainees, above all their rights to food, water, health, privacy, equal access to justice and an effective remedy against torture and other human rights violations, [which] derives from the simple fact that detainees are powerless.”[93] Current conditions in Zambian prisons violate international law and standards on prisoners’ welfare.
Overcrowding
The way they used to pack slaves in the ship, that is how we sleep.
– Kenneth, 37, Mukobeko Maximum Security Prison, September 30, 2009
Zambian prisons are among the most overcrowded prisons in the world, and were at over 275 percent of capacity in October 2009.[94] The government of Zambia itself has admitted that “Zambian prisons have for a long time experienced enormous problems” including “poor state of infrastructure, congestion, poor diet, poor health care, poor sanitation and water supply and a general lack of rehabilitation facilities,” and that existing prison population levels “cannot be sustained by the current prison infrastructure.”[95] International monitors have also repeatedly recognized that overcrowding in Zambian prisons is unacceptable, as are the health and human rights consequences of this overcrowding.[96]
Overcrowding often leads to or exacerbates other problems, including inadequate food, nutrition, and health care; inadequate living conditions; and poor health and hygiene. International standards establish basic requirements with respect to prisoners’ accommodations, including with regard to ventilation, floor space, bedding, sanitation facilities, personal hygiene, and room temperature.[97] PRISCCA, ARASA, and Human Rights Watch documented serious overcrowding that violated these basic standards, and exacerbated existing human rights violations.
At the time of our visit, Mukobeko Maximum Security Prison, a facility built in 1950 for a capacity of 400, housed 1731 inmates[98]—433 percent of its capacity. Lusaka Central Prison, a facility built in 1923 with a capacity of 200[99] housed 1145[100]—573 percent of capacity. Mwembeshi, a farm prison opened with a capacity of 55 inmates, housed 342—622 percent of its capacity—on the day of our visit.[101] At Mukobeko, 140-150 inmates sleep in cells measuring eight meters by four meters,[102] which inmates reported were designed for 40.[103] At Choma, 76-78 inmates sleep in each eight meter by four meter cell.[104]
International standards require that prisoners be provided with a separate bed, and separate, sufficient, and clean bedding. These requirements were not met in any of the facilities visited by PRISCCA, ARASA, and Human Rights Watch.[105]
At many prisons visited, overcrowding is often so severe that inmates cannot lie down at night. J. Kababa, officer in charge at Lusaka Central, confirmed that at that facility: “they sleep in shifts. Because of the congestion, not all can sleep at once. Some sleep, some sit. They take turns to make sure that others get a chance.”[106] He elaborated: “They are not sleeping, they are just squatting. Instead of resting in the night, they come out tired.”[107] Felix, 43, an HIV-positive remandee at Mukobeko, reported that “we have no space. There is not even enough space to lie down. We must sit, packed in like bags.”[108] Detainees at Mukobeko, Mumbwa, and Mwembeshi reported that they sleep on their sides, up to five on a mattress, unable to turn over.[109]
Officers recognized the pain experienced by inmates held in such overcrowded conditions. The social welfare worker at Lusaka Central Prison noted: “There is terrible suffering when you see them at night.”[110] “I am not happy to keep people in these inhumane facilities,” the offender management officer at Mukobeko, admitted.[111]
Over and over again, inmates reported the horrific overcrowding they face every night in their cells, describing the bodies of inmates in the cell as “squeezed like logs in a pile,”[112] “packed like sacks,”[113] or “like bodies in a mortuary,”[114] “like fish in a refrigerator,”[115] or simply “packed like pigs.”[116] Albert, 30, a remandee at Lusaka Central told PRISCCA, ARASA and Human Rights Watch:
We are not able to lie down. We have to spend the entire night sitting up. We sit back against the wall with others in front of us. Some manage to sleep, but the arrangement is very difficult. We are arranged like firewood.[117]
Such overcrowding leads to terrible, repeated suffering, night after night. As Rodgers, age 42, a remandee at Lusaka Central said, “we are being tormented physically. The way we sleep. If you put more pigs in a room for a night than can fit, in the morning you would find all the pigs are dead. These are the conditions we are in.”[118]
Packed together in their cells from four p.m. to six a.m. nightly, illness spreads rapidly among inmates: The medical officer at Choma reported that the most common health problems are respiratory infections, diarrhea, and skin conditions and rashes.[119] Prisoners across facilities reported frequent rashes as a result of close bodily contact. As immigration detainee Jean Marie, age 28, put it, “we are sweating at night on the floor; we don’t know what illness we have but we pass them back and forth.”[120]
The risk of TB transmission is high. Sick and healthy are routinely mixed together, and multiple inmates reported frequent coughing.[121] International standards require proper ventilation to meet the requirements of health and require that windows be large enough to allow the entrance of fresh air.[122] However, ventilation requirements are not met at Zambian prisons. Several of the prisons we visited lacked adequate ventilation, and had only air vents.[123] “We are all breathing the same confined air, contributing to all airborne diseases,” Hastings, 32, told us.[124] Esther, 47, confirmed:
Ventilation is very poor. I have very small window and cell captains block windows with their shoes, etc. and in this season it is so bad, some people faint in the night. In the last month, five times. When we are full, which is at least once a month, we have to sleep sitting up.[125]
International law requires that accused persons and prisoners held on non-criminal charges be kept separate from the convicted and treated separately; that adults and children, and men and women also be separated.[126] Zambian law on the books is in line with most of these standards. However, in practice, detention practices can be different.[127] Men and women were separated at all of the facilities PRISCCA, ARASA, and Human Rights Watch visited, and women guarded only by female officers. However, our research found that, apart from separation of male and female detainees, all categories of prisoners were packed together, in violation of international standards. Convicted, unconvicted, and immigration detainees were held together at all facilities, including non-criminal immigration detainees (among them asylum seekers) held solely on administrative rather than penal grounds, pending their deportation.
Children were not separated from the adult population at the facilities we visited that included child inmates. Patrick Chilambe, the officer in charge at Choma, confirmed that all prison populations, except for males and females, are routinely mixed;[128] “as a father it pains me,” he told us, that children do not have their own facilities—“we need to build a separate area for juvenile offenders.”[129] Kabinga, 17, reported that we “are not happy to share the same cell with adults and have complained to prison management, but our complaint has been ignored.”[130] Peter, a teenager, reported being threatened by other inmates if he revealed the combined sleeping arrangements: “We sleep with the adults, but they told us to say we sleep in a juvenile cell. If we don’t say we sleep in a separate cell, they will beat us. We are given punishment when we start talking. But we are scared we might die here.”[131]
Food and Nutrition
People are very, very hungry. It is difficult to rehabilitate someone when he is starving.
– Clement, 28, Mukobeko Maximum Security Prison, September 30, 2009
The most universal complaint we heard about prison conditions—from nearly every prisoner at every facility we visited—involved the insufficiency and low quality of the food. The food was described by prisoners as “not fit for human consumption,”[132] “food in name only,”[133] and “fit for pigs.”[134] “They really are not getting enough food,” the chaplain at Mukobeko admitted; in fact, “[they are] starving. They always eat something, but it can be a struggle.”[135]
Particularly harsh conditions of detention, including deprivation of food, constitute inhuman conditions of detention in violation of the ICCPR.[136] International standards require that prisoners be supplied with “food of nutritional value adequate for health and strength, of wholesome quality and well prepared and served.”[137] This standard has been cited with approval by the UN Human Rights Committee when examining the minimum standards that a state must observe for those deprived of their liberty, “regardless of a state party’s level of development.”[138] International standards further protect the rights of children deprived of their liberty to suitable food of sufficient quantity and quality to satisfy dietetic, health, and hygiene requirements.[139] Zambian law prescribes a dietary scale that includes meat or fish, cocoa, sugar, salt, fresh fruits in season, and fresh vegetables.[140] Neither international law and standards nor Zambian law requirements are met by the diet provided to prisoners.
Food consists usually of rice at breakfast, followed by a single meal[141] of maize meal and kapenta (tiny dried fish commonly eaten in Zambia) and/or beans at four p.m.. Despite the fact that farm prisons grow tomatoes and other vegetables, the occasional cabbage was the only government-provided vegetable, and most of the vegetables grown on the farms are sold to generate prison income.[142] Cruelly, inmates must therefore toil to produce vegetables that they virtually never have the opportunity to eat, only to see them sold off and the profits disappear into the prison system. The Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010) has noted that “the practices of diverting food from prisons or selling crops where the proceeds do not revert back to Prisons Service must be stopped.[143] “Vegetables?” asked Winston, 35, “It’s like vegetables don’t even exist. They sell the stuff from the farm; we don’t ever see it.”[144] The quantity of meals was reported by prisoners across facilities and confirmed by the officer in charge at Mumbwa to be approximately 400 to 450 grams of maize meal per day (400 grams of maize meal is equivalent to roughly 1,400 calories[145])—in addition to small quantities of beans and/or kapenta.[146] George Sikaonga, the officer in charge at Mukobeko, though, claimed that the issue, as per the dietary school, was 900 grams of maize meal per day.[147] Meals were widely considered insufficient and many prisoners reported a constant feeling of hunger.[148] “I go to bed hungry,” George, 44, an immigration detainee at Kamfinsa, told us.[149] Frederick, 23, an inmate at Mwembeshi farm prison, said that “we are starving by the time we eat and it is not enough after all day of work.”[150]
Inmates and prison officers at several prisons reported that prisoners were routinely denied food. Inmates at farm prisons said that these facilities often ran out of food, leaving some inmates with nothing to eat. Johnston, 41, a remandee at Mumbwa, told us that remandees only eat after convicts, “so if it is all gone, we don’t eat anything. This happens regularly.”[151] Robbie, 33, an inmate at Mwembeshi farm prison, reported “we have a shortage of food. When we are short, we have to sleep without eating anything until tomorrow. Some nights we eat nothing. When we are short, we just sleep like that. It happens once a week, sometimes twice a week.[152] Furthermore, Adam, 34, a remandee at Mumbwa, reported that because the prison has no electric cookers, “When it rains we can’t use the firewood. We eat nothing on those days. When we can’t cook, we don’t eat.”[153] The officer in charge at Choma said that because of firewood shortages, cooking and serving meals was sometimes done only once a day.[154]
Poor nutrition leads to numerous health problems. Dr. Chileshe confirmed that malnutrition is a serious problem throughout the prison system.[155] The medical officer temporarily stationed at Mukobeko, who has been with Zambia Prisons Service for nine years, noted that food provided to prisoners is inadequate and unvaried, with the result that some prisoners become malnourished; approximately seven of every 20 medical cases he screens point to malnutrition.[156] The medical officer at Choma prison also confirmed that she found inmates to be malnourished.[157] Inmates reported that the poor quality of food and water led to persistent diarrhea[158]; one reported dental problems as a result of the stones mixed in with the food,[159] and another reported that he couldn’t see properly as a result of malnutrition.[160]
The lack of nutritional diversity in prisoners’ diet may be creating serious and life-threatening health conditions: PRISCCA, ARASA, and Human Rights Watch heard repeated reports of swollen legs and feet,[161] symptoms which are consistent with the nutritional deficit disorder “beri beri.”[162] Francis Kasanga, the deputy officer in charge at Mukobeko, reported that in winter (July) 2009, as many as seven inmates had developed swollen legs and died shortly thereafter. An investigation was conducted and “several doctors recommended the introduction of a special diet, including fruit for the affected, and the problem cleared after this intervention.”[163]
There is no special diet for pregnant women[164] or for women who are nursing.[165] Despite international standards calling for special provision for children incarcerated with their parents[166] and the legal provision that, subject to the commissioner’s conditions, “the infant child of a woman prisoner may be received into the prison with its mother and may be supplied with clothing and necessaries at public expense,” and may stay up until age four,[167] there is no food at all allocated to the children under age four who live with their mothers in prison facilities; they are expected to share out of the portion of the mother.[168] In situations where women are unable to breastfeed, the prison does not offer infant formula. Agnes, 25, an inmate living with her nine month-old baby boy, informed us:
My child is not considered for food—I give my share to the baby (beans and kapenta)—we eat once a day. I am not given any extra food, and no special diet for the child. I am simply able to make some porridge for him out of my nshima [a cornmeal porridge]. The baby has started losing weight and has resorted to breast milk because the maize meal is not appetizing.[169]
The officer in charge at Lusaka Central echoed these concerns: “I get no budget for the children’s food, they must eat their mothers’ food. They are hungry a lot.”[170] Tasila, 24, a pregnant inmate, expressed concern about how she would keep her child fed, clothed, and in good health.[171] Annie, 33, an HIV-positive female inmate, told us that the she could not get extra food for her child, even from church donations, because the “cell captains and officers contrive to take donations of food and goods brought by the church. There is nowhere to go and complain.”[172]
As a result of chronic food shortages, food has become a commodity that is traded to the most vulnerable in exchange for sex and labor. As Willard, 25, put it, “Food is used as power. Those who have relatives who bring them food are powerful in prison, those of us without relatives are weak.”[173]
Orbed, 26, described to us how inmates come to trade sex for food:
Food is a major problem. The quantity and quality are both poor. It is not enough to sustain one’s life in here. We lose weight, we are enslaved—all because of food. Those who are able to afford food can enslave others. They say, “I will give you whatever you want for food if you sleep with me,”—it happens a lot.[174]
Lawrence, 33, confirmed this practice:
Those who have been here much longer get more food, and the lion’s share of everything. For those who come late, they must give services in exchange. It is very common, especially for those who do not receive any help from their families. They are the victims. The food we are fed with is not food that someone can live with. So people tend to give in to such practices if they are less privileged.[175]
Prisoners speaking with us recognized that sex can spread HIV:
I have seen [sexual activity] happen all the time where mostly the lifers, who have nothing to lose, will entice new and vulnerable inmates to sodomy with food and cooking oil. Then they get HIV and when they get out they infect their families. Or they die. I have had several friends catch and die of HIV that way.[176]
Access to Potable Water and Basic Hygiene
It tastes foul, but we drink it.
– Annie, HIV-Positive Inmate, Lusaka Central Prison, October 4, 2009
The UN Standard Minimum Rules on the Treatment of Prisoners specify that sanitary facilities shall “enable every prisoner to comply with the needs of nature when necessary and in a clean and decent manner” and furthermore that “[a]dequate bathing and shower installations shall be provided so that every prisoner may be enabled and required to have a bath or shower, at a temperature suitable to the climate, as frequently as necessary for general hygiene according to season and geographical region.”[177] Sanitation and water facilities in Zambia’s prisons do not meet international standards and indeed violate prohibitions on inhuman and degrading treatment. They also pose a major health risk.
Toilets are insufficient in number and are filthy; in some prisons they consist only of a hole in the ground and at others simply a bucket.[178] At Mwembeshi, inmates reported that there were no toilet facilities at all in the cells, and a bucket was used overnight. The lack of a sewer system, the officer in charge concluded, is “dehumanizing.”[179] What outmoded and insufficient sewer systems do exist are constantly backing up—all of the pipes of the Mukobeko sewer system, built in 1957, are constantly blocked.[180] At that prison, 10 outdoor toilets are shared by more than 1,000 inmates. Paul, 33, at Mukobeko, said, “you pray for your friends not to use the loo.”[181] “You have to plan in advance because there is a long queue,” Daniel, 39, a “lifer” at Mukobeko, pointed out. “You can wait for hours,”[182] leading to fights between inmates.[183] In the cells at Mukobeko, with one toilet for 140-150 inmates, “we queue from when we are locked up, straight through until the morning.”[184] Anderson, 35, an inmate at Choma, told us that there were two toilets for 150 inmates on his side of the prison, which overburdened the system to the extent that “the toilets are always overflowing as people have diarrhea all the time.”[185] At Lusaka Central, female inmates reported that the two toilets in each cell are reserved for urination: “If we excrete for any reason...we were told we would be punished by the cell captain,”[186] –“we must get permission from cell captain to poop when necessary.”[187]
Inadequate toilet and bathing facilities pose particular problems for disabled inmates. Chrispine, 46, a remandee on crutches with one leg amputated, told us that it was particularly hard for him to use the hole in the ground for a toilet,[188] a difficulty confirmed by other disabled inmates.[189] “I find it difficult to balance, jumping over my colleagues in the cell to the toilet,” one explained.[190]
Additionally, water sources at some facilities are disturbingly close to sanitation outflows.[191] As Kalunga, 29, reported, “there is one bowl and pump for water, right next to the pit for trash, which is right next to the pit toilets.”[192] At Mwembeshi, the offender management officer told PRISCCA, ARASA, and Human Rights Watch that “the water table is low, close to latrines. The technician told us we need more chlorine which we don’t often have.”[193] Inmates at multiple facilities described drinking water as unclean.[194]
Furthermore, despite international standards dictating that drinking water be available to every prisoner whenever he or she needs it,[195] water availability is subject to shortages at many of the prisons, in some cases because the water bill is not paid,[196] water is rationed[197] or during electrical shortages.[198] At Mukobeko, the offender management officer reported that the water supply is clean but subject to erratic supply.[199] A prison officer at Mukobeko told us that he has seen fighting among the inmates “many times in accessing water.”[200] Water shortages lead to the use of unclean water: “There is tap water but we go to a stream to fetch water when we get none—none of it is treated, it does not look clean.”[201]
Bathing facilities at some prisons are squalid. At Mwembeshi, the bathing area is a muddy grass structure with no drainage[202] and prisoners reported sharing buckets used for bathing.[203] One inmate reported that they even reuse the same containers for bathing which are used as toilet facilities in the cell at night.[204]
A possible consequence of such poor water quality and sanitation, diarrheal disease is common among inmates. At Mwembeshi, the offender management officer informed us that poor hygiene resulting from a lack of toilets with water, and the use of buckets, facilitates diarrhea.[205] Inadequate water quality and sanitation also can have additional, deadly consequences for inmates: Adam, 34, a remandee, told PRISCCA, ARASA, and Human Rights Watch, “the remandees are told to pick up the toilet tissues after the night and clean up the area in the cell. This is without gloves, it spreads diseases. There was a cholera outbreak a while back in cell three, [which made] 15 inmates [sick].”[206] Unclean bathing facilities also lead to illness. In the ablution block, Moono, a teenager at Lusaka Central, told us, “we end up contracting skin diseases, and there is no proper water.”[207]
The Prisons Service does not provide basic necessities to prisoners, and they are left instead to rely on family members, church donations,[208] or an exchange of sex or labor in order to obtain soap, razors, sanitary pads, and items essential to proper hygiene. International standards require that prisoners shall be provided with toilet articles necessary for health and cleanliness, as well as razors.[209] Zambian law provides that, if an unconvicted prisoner does not provide himself with food and clothing, “he shall receive normal prison food, clothing, and other necessaries”[210] and that convicted prisoners receive these essentials. Yet such articles are not provided. As Catherine, 38, described,
The prison does not provide us with soap, toothpaste, or sanitary pads. If others don’t bring them for us, we have nothing. There are lots of people with no relatives here. They have nothing....Some people have no relatives—if you have no food, you are nobody in this place. You can trade a cup of sugar for work.[211]
The unavailability of soap leads to poor hygiene: As the HIV/AIDS coordinator at Lusaka Central reported, “hygiene is a big problem—no toothpaste, soap, clean clothing, and mattresses are not clean. There are not enough blankets, and no sheets—prisoners get cold. They have no spares, so they cannot wash them.”[212] Inmates routinely rely on shared razor blades,[213] or used razor blades,[214] very high risk behavior that promotes transmission of Hepatitis and HIV. Additionally, inmates are not provided with basic cleaning materials such as gloves and disinfectant in order to clean the latrines or toilet buckets.[215]
International standards require that prisoners be issued separate and sufficient bedding that is “clean when issued, kept in good order and changed often enough to ensure its cleanliness.”[216] Yet in Zambia, mattresses and blankets are filthy and go for months without being washed,[217] in violation of international standards. As Jacob, 26, an inmate at Mwembeshi, told us, “the blankets, they are not clean. Since I came, they have not been cleaned. Someone told me they have not been cleaned since 2005. There are lice and dust in all of them.”[218] Vermin, lice, and cockroaches are commonplace. Indeed, at Mwembeshi, another inmate, 26, reported that “one captain does not let people kill the lice—it is just to be mean and mock them.”[219] Mary, 27, who sleeps by the storeroom at Lusaka Central, had insects enter her ear in the night, and she had to be taken to the hospital.[220]
Uniforms are not provided to remandee prisoners, and clothing provided to convicts is grossly inadequate.[221] Female inmates are given uniforms designed for male inmates.[222] Some of the inmates at each prison are entirely without shoes; others wear only a single shoe. Others wear only half a uniform. The officer in charge at Choma confirmed that while convicted prisoners are meant to be provided with one prison uniform, the uniforms have run out, and often uniforms are taken from older convicts to give to the new.[223] Marlon, 17, in rags, noted simply “I have no proper clothes.”[224] “Some people are walking naked, with no uniforms,” Reynard, 35, observed.[225] With only one set of clothing, inmates are forced to wear their uniform at all times, even when wet.[226] Mwape, 47, at Mukobeko, declared, “I have only one torn t-shirt, one old short, and a pair of sandals to survive on the remaining 11 years of my 17 year sentence.”[227] Mwisa, 29, an inmate at Choma, expressed the toll that inadequate clothing takes on the psyches of inmates: “We have no coats in winter, and people fall ill. It’s a matter of health, but also of dignity. How can one be dignified when begging for clothes?”[228]
Mosquito nets are not provided, despite frequent cases of malaria, and only a few personally owned nets were present at some of the prisons we visited. Sylvia, age 70, informed us that in her cell, “we have two major problems: One, plenty of mosquitoes, and two, no nets.”[229]
Rape
Studies have documented the occurrence of sexual activity inside Zambian prisons,[230] and even the former president has acknowledged this fact.[231] Overcrowding in prisons has been shown to contribute to sexual violence.[232] Our findings suggested a high prevalence of sexual activity between male (but not female) inmates, including consensual sex between adults and the adult relationships described above in which sex was traded for food. PRISCCA, ARASA, and Human Rights Watch also heard reports of rape. Sexual activity was reported at Mukobeko, Kamfinsa, and Lusaka Central prisons, and less frequently at Mumbwa, Mwembeshi, and Choma prisons.
Although there is no general definition of rape in international human rights law, rape has been authoritatively defined as “a physical invasion of a sexual nature, committed on a person under circumstances which are coercive.”[233] Under Zambian law, rape is a gendered crime and may only be committed against a woman. Sexual activity with children under age 16 constitutes defilement under Zambian law.[234] In Zambian prisons, children are frequently forced into sexual relationships constituting rape, particularly when they are held with adult prisoners. At the time of our visit to Mukobeko, three juveniles were held in a cell with three adults— two of the adults in the cell were in prison on charges of defilement of a minor.[235]
Chris, 17, reported that:
I have witnessed sexual abuse. One of the older inmates who was put into our cell to sleep at night started showering my cellmate, a juvenile, with gifts. He promised him money in return for sexual favors. My friend wasn’t happy, and neither did he consent. But the other imposed himself by buying him off with gifts, and saying that there was 100,000 kwacha [US$21] waiting for him “at the reception”. When the older inmate finally approached him sexually, my friend was intimidated, but managed to shout and attracted the attention of the other juveniles. Unfortunately we reported it to the officer on duty at night, and he promised to address it the next day, but he didn’t. The cell captain intervened, though, and removed the man, putting him into one of the other cells....Do I feel safe? No, I don’t feel safe.[236]
David, a teenager at Lusaka Central, reported that “I haven’t physically been abused, because I know the system, and avoid enticements. But my more vulnerable friends fall prey. Once you eat the food, they reprimand you, say you have no choice. I have seen it happen. It pains me to see the pain they undergo as juveniles.”[237] Moono, a teenager at Lusaka Central, concluded: “Mainly the juveniles are very vulnerable. As young people coming into prison, we are full of fear. The convicts take advantage of us by providing us with food and security. We enter their dragnet, but by the time we discover this it is too late.”[238]
Sometimes adults become victims of male rape, too. Evans, 43, a remandee at Lusaka Central, concluded:
Sometimes when you are sleeping someone gets under you. He’s already in your anus. Others wake up, and catch that man....They are brought before the authorities. Sometimes they overlook it, or the officer in charge can take you to the courts of law.[239]
We found, however, that significant denial among the officers exists as to the occurrence of sexual activity: the officer in charge at Mukobeko informed us that no prisoners were engaged in sexual activity to his knowledge,[240] but the deputy officer in charge at Mukobeko admitted that he “had learned of fights between inmates of prisoners fighting over sexual and romantic partners.”[241] Furthermore, a prison officer at Mukobeko told us that he received roughly three reports a month of sexual activity and that “captains are empowered to attend to this.”[242] At Kamfinsa, Patrick Mundianawa, the officer in charge, said that there is “almost no sexual activity at the prison,” only attempts.[243] At Lusaka Central, the officer in charge admitted that “there is a small amount of sexual activity in the prison. When it happens, cell leaders report and we investigate. We rush the victim to the hospital for physical exam. If it is confirmed, the aggressor is taken to court. We always punish someone because it can’t be acceptable as if we did that it would get out of hand.”[244] “I don’t know, I haven’t heard any complaints,” the officer in charge at Mumbwa demurred,[245] but the deputy officer in charge, D. Mulenga, told us that he was aware of cases of consensual sex.[246] The officer in charge at Choma reported that there was no sexual activity in the prison currently.[247]
The Availability and Quality of Medical Care
International law dictates that prisoners be provided with health care at least equivalent to that available in the general community.[248] Health care currently provided in Zambian prisons falls far short of international standards. TB and HIV present specific challenges.
Tuberculosis
The isolation cells are death traps.
– Dr. Chileshe, director, Zambia Prisons Service Medical Directorate, October 13, 2009
TB Transmission
The conditions at each prison visited by PRISCCA, ARASA and Human Rights Watch—combining overcrowding, minimal ventilation, and a significant immuno-compromised population—are ripe for the quick spread of TB, confirmed by suspected high prevalence. As noted above, a 2000-2001 study in 13 Zambian prisons for pulmonary TB among inmates concluded that a high rate of pulmonary TB exists in Zambian prisons, speculating that true prevalence rates may approach 15-20 percent;[249]the Zambia Prisons Service has reported a case infection rate for TB of 5,285 cases per 100,000 inmates per year.[250] High turnover exists in the prison population, so spread of TB to the general public by released inmates is also a significant risk.[251] As an officer at Mwembeshi noted, “The cells are meant to accommodate 10 but they hold 135. The men don’t sleep well. If one has TB, four or five have it. Before it is identified, it has already spread.”[252]
Interviews with inmates and prison officers established that there exists a strong awareness of the possibility of transmission, and a deep fear of both contracting TB and spreading it within the community.[253] As one prison officer at Kamfinsa said, “we need to care for and prevent some diseases like TB. If so many people are sick, the officers can be affected. We necessarily worry about getting TB at our work. If I am sick, I can transfer it to my family. It worries us.”[254] According to an inmate, “the ventilation is not good. There is coughing and TB in the cells. It takes time to be detected, but by the time they detect it, the TB will have spread to many of our fellows. It keeps us worried.”[255] Dr. Chileshe confirmed: “They say, ‘you’re going to Chimbokaila [Lusaka Central Prison]? It’s a death sentence.’ Not because they are afraid you will be given beatings, but because of TB. They know the conditions are bad.”[256]
Children incarcerated at Mukobeko have shared living quarters with the TB isolation cell. The children fear TB patients—“I am worried I will catch TB. There is no window, just a small opening with wire over it—not much ventilation,” Phiri, 17, said.[257] Isaac, 17, at Mukobeko, reported that there were “23 TB patients in my living area. There are no vents, no air. I’m worried.”[258] The officer in charge of Lusaka Central prison acknowledged that the lack of ventilation was a severe problem.[259]
TB Testing
Since 1993, the World Health Organization (WHO) has explicitly recognized the need for “vigorous efforts” to detect TB cases through entry and regular screenings in prisons, and the need for effective treatment programs and continuity of treatment upon transfer or release.[260] The Zambian prison system does have the capacity to diagnose some of the prisoners it tests for TB (the diagnosis involves analysis of a sputum sample under a microscope for TB bacilli). PRISCCA, ARASA, and Human Rights Watch’s research found that, of prisoners we spoke with who had tested for TB, 35 percent had been found positive. Nevertheless, our research suggested that only a small segment of the Zambian prison population has testing to diagnose active pulmonary TB, the form of TB that spreads quickly in the overcrowded and confined spaces of Zambian prisons. Dr. Chileshe reported that, in 2009, between 300 and 400 cases of TB were estimated in the prison system based on reports from the clinics, but he was “sure there are those who have TB who may not be [diagnosed].”[261]
Table 5: TB Testing
|
Lusaka Central |
Mukobeko |
Kamfinsa |
Mumbwa |
Mwembeshi |
Choma |
Overall (six prisons) |
Prisoners Who Reported Having Been Tested for TB While Incarcerated (%) |
18 |
49 |
32 |
4 |
0 |
11 |
23 |
TB Testing for PrisonersOur survey data yielded significant differences in TB testing among prisoners we interviewed both between facilities and between inmate groups within each prison. Testing was higher in larger, urban facilities (Lusaka Central, Mukobeko, and Kamfinsa), and lower in smaller, rural facilities (Mumbwa, Mwembeshi, and Choma). Among the smaller facilities, TB testing among prisoners we interviewed ranged from a low of zero percent at Mwembeshi to 11 percent at Choma; it ranged from 18 percent at Lusaka Central to 49 percent at Mukobeko. Within each facility, certain categories of inmates—women, juveniles, remandees, and immigration detainees—were those least likely to be tested. At all prisons where testing was conducted, except for Lusaka Central, convicts were tested at significantly higher rates—overall more than twice that of remandees, and more than four times that of immigration detainees. Such a disparity is likely a result of a combination of the security fears that keep remandees from accessing medical care generally, discussed below; discrimination against immigration detainees in accessing care; and the fact that immigration detainees have, on average, spent less time in detention than convict and remandee detainees. TB testing among juveniles was significantly lower than that for adults at each prison where testing took place, and overall, juveniles had a TB testing rate of only four percent compared to the adult rate of 25 percent. Even at Mukobeko, where juveniles were been forced to sleep with patients in the TB isolation cell, the juvenile testing rate was only 17 percent compared with an adult rate of 53 percent. Women, as well, had lower testing rates at each prison conducting testing, and overall only 11 percent of adult female prisoners we interviewed had been tested for TB, compared with 28 percent of adult male prisoners. Such a disparity is probably attributable to a combination of factors: women and juveniles had, on average, been detained and incarcerated in their current facility for a shorter time than their male counterparts; juveniles (but not women) reported experiencing fewer health problems during incarceration and thus were probably less likely to visit health facilities; and female inmates were less educated than male inmates and perhaps less aware of and able to request testing. |
Table 6: TB Testing by Prisoner Type
Prisoners Who Reported Having Been Tested for TB While Incarcerated
Significant delays exist between when inmates present with symptoms of TB and when they are tested for the illness.[262] TB should be suspected and tested for in individuals with unexplained weight loss, loss of appetite, night sweats, fever, and fatigue. When the disease is in the lungs symptoms may include coughing for three weeks or more.[263] However, we spoke with two inmates at Lusaka Central on treatment for TB who had waited three months for a trip to a clinic where sputum analysis could be completed after reporting a cough to the cell captains or prison officers, and two others who had waited over four weeks.[264] Indeed, medical staff at some prisons informed us that TB is often the last cause of illness tested for when an inmate presents with coughing, and treatment for upper respiratory infections is first exhausted. The medical officer at Mukobeko confirmed that TB testing takes place after the exhaustion of efforts to address respiratory infection.[265]
Testing for preventative purposes, when an inmate has not yet shown symptoms of infection, is almost entirely unknown: as Muntala, 39, an immigration detainee at Lusaka Central, said, “they take you for tests when you are coughing but by then it is too late.”[266] Even inmates who face an elevated risk of TB infection due to their HIV status are not routinely tested: One HIV-positive inmate told us that he had received no TB test, though he had asked for one, because the Go Centre—the NGO that conducts HIV testing at his farm prison, Mwembeshi—did not have the capacity to test for TB. While they could give him a referral to the hospital, “that would be impossible to get transport from here.”[267] Across all six prisons, we found that 53 percent of HIV-positive prisoners had been tested for TB, however, there is a striking difference between prisons. While 94 percent—16 out of 17— of HIV-positive inmates at Mukobeko had received a TB test, not one of the 10 HIV-positive inmates at Mwembeshi had been tested for TB.
TB Treatment
While an initial course of treatment is provided at all prisons for inmates testing positive for TB, with medications usually consistently available at Ministry of Health facilities when inmates were able to access them, we found no testing and treatment for drug resistance. Drug resistance testing and treatment in the Zambian general population is also inconsistent and not widely available.[268] Yet drug-resistant TB is a major public health threat—the WHO estimates that 300,000-600,000 new cases of multi-drug resistant TB (MDR-TB)[269] emerge every year, with global prevalence as high as 1,000,000 cases[270]—which emerged as a result of program failures, such as interruptions in drug supplies and non-adherence to correct treatment and now may be transmitted from patient to patient. The WHO has recognized that “[t]ransmission in prisons is an important source of spread of drug-resistant TB in some countries,”[271] and that “badly managed tuberculosis treatment does not cure patients, prolongs transmission of infection and promotes multidrug-resistant tuberculosis.”[272]
At the prisons PRISCCA, ARASA, and Human Rights Watch visited, there was an almost complete lack of knowledge of issues around drug resistance—at the prisons and apparently at related hospitals—even for inmates who had previously been treated for TB and whose symptoms persisted or who appeared to be treatment failures. While the WHO has noted that appropriate treatment for drug-resistant TB includes the use of second-line drugs,[273] with individual case management including a history of drug use in the country and the individual,[274] such procedures are not routinely followed. A nurse at the clinic serving Lusaka Central prison informed us that “yes, we have encountered MDR-TB. We recommence them on the same TB drugs as on first phase, but for longer. Then if after eight months they are still not responding, we go to the relapse drugs.”[275] A significant problem is that healthcare staff report that
[We] do not know what drugs the prisoners have taken before for TB. Often they tell us they were on TB medication before but they do not recall anything about it. There are two prisoners now, they told us they were on TB drugs before and we told them to come into the clinic, but we haven’t seen them yet. We can’t just give them drugs until we see what they were on.[276]
TB Isolation
Zambian policy dictates that best practice for TB management demands case detection, isolation, supervised treatment and follow-up support, health education, and nutritional supplementation.[277] If a prisoner is found to be suffering from an infectious or contagious disease, under Zambian law, the officer in charge is required to take steps to place the prisoner under treatment and prevent the disease from spreading to other prisoners.[278] The Ministry of Health recommends “isolation for all prisoners with TB.”[279] Yet Dr. Chileshe acknowledged that isolation is rare, and reported that only in two or three prisons is there true isolation. In the rest of the prison system, there is no isolation capability.[280] “Our officers have tried their best to isolate patients, but they can’t,” he said. “There is literally no space.”[281] Two of the six prisons (Mumbwa and Mwembeshi) PRISCCA, ARASA, and Human Rights Watch visited lack TB isolation facilities entirely, leading TB patients to remain in the overcrowded and poorly ventilated general prison population cells and risking spread of the disease.
In correctional settings, persons suspected of having infectious TB should be placed immediately in an appropriate TB isolation room.[282] TB isolation can be discontinued if a diagnosis of TB is excluded or when a patient is no longer infectious.[283] In Zambian prisons, by contrast, where isolation exists, only patients diagnosed with TB are placed in the isolation cell; inmates with suspected TB based on their symptoms remain in the general population until diagnosis,[284] risking continued infection of the general population.
Even when patients are isolated (on the days of PRISCCA, ARASA, and Human Rights Watch’s visits, Mukobeko Maximum Security, Kamfinsa, Lusaka Central, and Choma claimed to isolate TB patients) the conditions of TB isolation facilities are conducive to serious deterioration of health. Indeed, the conditions of TB isolation cells—which at Lusaka Central included nearly nonexistent ventilation and light and cramped, dirty quarters for very ill patients, who sleep on foam pads on the floor—are, in fact, life-threatening. 57 inmates on the day of our visit lived in an isolation cell approximately four meters by eight meters. The medical officer at Mukobeko informed PRISCCA, ARASA, and Human Rights Watch that TB isolation facilities are improvised and that conditions are “pathetic”;[285] “there were none designed, we are doing the best we can within available resources,” another officer at Mukobeko explained.[286] At Choma, former penal block cells are either used for TB isolation or for grain storage.[287]
In fact, TB isolation facilities are likely a key site of TB infection. Actively coughing residents in a dark, unventilated cell can quickly spread TB or drug-resistant TB to uninfected cellmates. Augustine, 37, reported that he was placed in isolation in 2007 but was found not to have TB and moved out; he became ill subsequently and was diagnosed with TB. He believes that he contracted it in isolation.[288] Another inmate, 38, currently in the TB patients’ cell at Lusaka Central, reported that some in the cell did not have TB and were being exposed to a high risk of TB infection, as the cell has no ventilation and “the situation is terrible.”[289]
An important reason why TB isolation cells may serve as a source of infection is the fact that former TB patients are reluctant to leave the cells, because even their squalor is preferable to the more crowded general population cells. Kachinga, a prisoner at Lusaka Central, actually informed us that he chose to remain in the TB isolation cell after completing his TB treatment because the conditions there were slightly better than those in the other cells:
I was tested for TB and put into the [isolation] cell. I tested positive. I finished my course of treatment, tested again, and was negative. I am still in the [TB isolation] cell. I would love to move out, to give room to other patients coming in, but the other cells are congested. It’s my choice to stay.[290]
Dr. Chileshe confirmed: “Where there are TB patients there is more space, and inmates want to sleep there. You find pregnant women in the cell with TB patients. You may say it’s not medically acceptable, but what can you do?”[291] The number of inmates remaining in isolation for periods beyond their time on TB treatment is suggested by the fact that, at Lusaka Central, the prison clinic had 34 patients recorded on TB treatment the day of our visit; the TB isolation cell, by contrast, held 57 inmates.[292]
HIV/AIDS
The WHO has established standards on HIV prevention, care, and treatment in prisons.[293] The UN Office on Drugs and Crime (UNODC) has also established a framework for a national response to HIV/AIDS prevention, care, treatment, and support in prison settings.[294]While education, testing, and treatment for HIV have been drastically scaled up in recent years in Zambia’s prisons—with the help of NGO partners—significant gaps remain in the appropriate implementation of these services, as well as in prevention practices, between international standards and Zambia’s response to HIV/AIDS in prisons.
HIV Testing
To the credit of Prisons Service officials and NGO partners, recent years have seen the scaling up of HIV testing, albeit provided by an NGO. The Go Centre/CHRESO Ministries provides HIV testing and treatment on regular visits to three Lusaka area prisons (including Lusaka Central and Mwembeshi), two prisons in Mukobeko (including Mukobeko Maximum Security Prison), and a prison in Livingstone.[295] Access to testing at several of the facilities was very good as a result of this program; at others it was more limited, suggesting that even more remote facilities, which PRISCCA, ARASA, and Human Rights Watch did not visit and which are not served by the Go Centre, may have negligible access to testing and treatment. Voluntary counseling and testing is also foreseen at the prison clinics at Lusaka, Livingstone, and Mukobeko in the future; they are currently going through an accreditation process with the Ministry of Health.[296]
On the day of researchers’ visits to each facility, survey data across the six facilities confirmed that, while HIV testing is significantly higher than TB testing, it is more consistently practiced at some facilities than others. Larger facilities had higher HIV testing rates among prisoners we interviewed, ranging from 54 percent at Lusaka Central to 86 percent at Mukobeko Maximum Security; smaller facilities’ HIV testing rates ranged from 23 percent at Mumbwa to 48 percent at Mwembeshi (which is visited by the Go Centre).
Table 7: HIV Testing
|
Lusaka Central |
Mukobeko |
Kamfinsa |
Mumbwa |
Mwembeshi |
Choma |
Overall (six prisons) |
Prisoners Who Reported Having Been Tested for HIV While Incarcerated (%) |
54 |
86 |
72 |
23 |
48 |
33 |
57 |
Within facilities, as with TB testing, the prisoners we interviewed reported that certain categories of inmates including women, juveniles, remandees, and immigration detainees tended to be tested for HIV less frequently than their adult, male, convict counterparts, likely for similar reasons as for TB testing. Between all prisons, adult female testing was 45 percent compared to 62 percent for adult males; 44 percent of juveniles were tested compared with 59 percent of adults; and 46 percent and 21 percent of remandees and immigration detainees, respectively, had been tested compared with 65 percent of convicts.
Table 8: HIV Testing by Prisoner Type
Prisoners Who Reported Having Been Tested for HIV While Incarcerated
Aside from inconsistent implementation, other challenges still exist in the implementation of testing. The National HIV/AIDS/STI/TB Policy requires that women considering having a child be encouraged to seek counseling and testing, and ensures that every pregnant woman has access to HIV/STI screening and treatment, but does not mandate mandatory prenatal testing.[297] However, for female inmates, we heard troubling reports that HIV testing for pregnant women may be mandatory.[298] While one prison officer called HIV testing “voluntary”, additional comments suggested that it may actually be mandatory: “For those who are pregnant, they are tested for HIV....Whether you like it or not you are tested to prevent transmission to the baby.”[299]
HIV peer educators had been trained through the NGOs PRISCCA, In But Free, and Treatment Advocacy & Literacy Campaign (TALC)[300] at several of the prisons PRISCCA, ARASA, and Human Rights Watch visited, and throughout the prisons, detainees reported relatively low levels of discrimination and stigma against HIV-positive inmates from either the officers or other inmates. Researchers heard repeatedly that education campaigns have proved successful: Orbed, 26, an HIV-negative inmate concluded that “since the education campaign, there is no discrimination. The campaign has really worked.”[301]
However, some inmate harassment and prison officer breach of confidentiality lingers. Keith, 32, an HIV-positive inmate, told us: “I have never faced any discrimination from the officers because of my HIV status. From my fellow inmates I have faced a lot, though. It’s quite difficult—when I stand in front of my fellow inmates to educate them, some laugh at me.”[302] Allan, age 34—an HIV-negative inmate—confirmed, “the discrimination among inmates takes the form of mocking the person who is positive. You have to hide the drugs if you want secrecy—it’s hard to maintain....Officers will ask for a list of those wanting VCT and call the names out loud. They will tell those who are negative to leave and those who are positive to remain, so everyone knows what the results are.”[303] Additionally, peer education has not been consistently implemented across facilities within the prisons system, or sometimes within facilities themselves. Paul, 33, an inmate in the “condemned section” at Mukobeko—where inmates under sentence of death are held—reported that the condemned don’t receive the HIV education offered to other prisoners: “We feel like they think we will all die anyway so it doesn’t matter.”[304]
HIV Treatment
Table 9: Number and Percent of Prisoners Who Reported Being Started on HIV Treatment after Testing Positive
Access to ART has also improved among the prison population in recent years. For inmates who have tested positive for HIV, ART is often available to HIV-positive inmates at the prison referral hospital or through the Go Centre/CHRESO, for those six prison facilities they serve. Of the prisoners we interviewed who had tested positive for HIV, 60 percent overall were started on treatment including ART, cotrimoxazole, or any other form of treatment, 89 percent of them on ART. Prisoners at the larger prisons, particularly Lusaka Central and Mukobeko Maximum Security (both served by the Go Centre), were more likely to be started on treatment than their counterparts at smaller, rural prisons.[305]
Furthermore, cotrimoxazole—recommended for all individuals testing positive for HIV in order to treat opportunistic infections—is almost entirely unavailable at all prisons, with only one prisoner we interviewed being started on it after testing positive for HIV. In the general population, by contrast, cotrimoxazole prophylaxis is generally available at all Ministry of Health ART clinics, provided by the Ministry of Health with the Center for Infectious Disease Research in Zambia (CIDRZ) providing back-up for stock-outs.[306]
A high level of adherence is crucial for the success of ART. According to the WHO, “adherence to ART is well recognized as an essential component of individual and programmatic treatment success.”[307] Research on drug adherence has shown that “higher levels of drug adherence are associated with improved virological, immunological and clinical outcomes and that adherence rates exceeding 95 percent are necessary in order to maximize the benefits of ART.”[308] Lack of adherence can lead to the development of drug resistance, illness, or death. Zambian policy dictates that the Zambia Prisons Service—with partner support—provide food supplements to HIV-positive prison officers and inmates on ART.[309]The WHO has determined that “improved nutrition may enhance ART acceptability, adherence, and effectiveness.”[310] Food supplements are similarly important for individuals on TB treatment, adherence to which is important both to cure them of TB and to avoid the development of drug resistance.
Such supplements are not currently provided, however. “They used to give extra food for taking medications but no extra food now. It is hard to take these very strong drugs without enough food” said Willard, 25, an HIV-positive inmate at Mukobeko.[311] Even an inmate with a physician’s prescription for special food was unable to receive it because “the prison can’t afford it.”[312] Emmanuel, 35, an HIV-positive inmate at Mukobeko, had asked to be transferred closer to his family so that they could supply him with better food, but was refused: “I think all people on ART should be transferred if they can’t feed us adequately,” he said.[313]
Table 10: Reasons for Missing HIV Treatment
|
For prisoners who are on medication for HIV and TB, the unavailability of food makes taking medication extremely difficult, even frequently leading to missed doses. Among inmates on ART whom we interviewed, more than half of them (55 percent) had missed doses, and lack of food was cited by more than a third (38 percent) of those who had missed doses as the cause. Augustine, 37, an inmate on medication for TB, noted: “I am not getting enough food, now that they are no longer giving food supplements for those on drugs. I feel weak. I suspect that the drugs could be working but they are so strong I need food for them to work.”[314] Francis, 33, an HIV-positive inmate held at Mwembeshi farm prison, reported to us that he takes his ART only once a day, in the evening, because he has no breakfast in the morning to take the medication with: “I should take them in the morning as well, but if I took them in the morning I could not work, as I would be dizzy and weak.”[315]
Prison officers also lamented the health effects of lack of nutritional supplements for HIV and TB patients.[316] A nurse at the clinic serving Lusaka Central prison reported that the food is “not nutritionally adequate” and the clinic does not provide any extra food to people on HIV or TB drugs: “It is affecting whether they get well,” she concluded.[317] The HIV/AIDS coordinator at Lusaka Central has tried to obtain food supplements for those who need them, in accordance with Zambian prison regulations, but the authorities have been “sluggish” in their response. Without sufficient nutrition, she noted, “someone can be on ART but still die, as two have died of AIDS since I have been here [for nine months].”[318] The officer in charge at Choma also confirmed that the prison’s lack of capacity to provide supplementary food to both inmates and prison officers on ART and TB treatment is a major challenge.[319]
HIV treatment to prisoners is highly dependent on the intervention of the Go Centre at the facilities where that NGO operates; Go Centre health professionals dispense the medication, which may be kept on the inmates’ persons in between visits or delivered by a nurse. At Mukobeko Maximum Security Prison, where the Go Centre conducts voluntary counseling and testing (VCT) and provides drugs,[320] the prison administration reported that 142 prison inmates were on ART, 15 of whom were also on treatment for TB.[321] At Lusaka Central, 113 prisoners were on ART, and 19 on both HIV and TB medication[322] through the Go Centre and Hospital.[323] Waiting lists to access ART were reported both through government hospitals and NGOs.[324]
HIV Prevention
Zambian policy acknowledges that “[p]rison confinement can increase vulnerability to HIV due to frequent unprotected sex in the form of rape, non-availability and non-use of condoms, as well as high prevalence of STIs.”[325] Noting that “[p]revention is better than cure,” the Zambia Prisons Service has set for itself the goal of ensuring “the implementation of a comprehensive HIV prevention package.”[326] Yet we found that the total unavailability of condoms and other essential means of prevention in the context of a population with a very high HIV prevalence and widespread sexual activity, consensual and non-consensual, creates a serious risk of HIV transmission and seriously hinders HIV prevention activities.
International organizations—including the WHO, UNODC, and the Joint United Nations Programme on HIV/AIDS (UNAIDS)—all recommend that condoms be provided to prisoners.[327] In 2007, the WHO, UNODC, and UNAIDS noted that studies have found condom provision in prisons to be feasible, acceptable to prisoners, acceptable to prison staff, and did not have negative consequences such as compromising prison safety or security. Furthermore, “[f]ears about the provision of condoms leading to more consensual and non-consensual sex were not realized.”[328] Zambian prison policy has called for inmates to be provided with the means to protect themselves from HIV.[329] Zambian public health advocates have called for condoms to be introduced for years.[330] Dr. Chileshe has espoused the need for harm reduction in prisons because “people are dying.”[331]
Yet condoms are, without exception, not provided to prisoners and in fact are contraband. Indeed, instead of distributing condoms to prisoners, the Zambia Prisons Service reportedly is considering installing closed circuit television in some prisons at great expense, ostensibly as a means of decreasing sexual activity.[332] The unavailability of condoms is linked to the criminalization of same-sex sexual activity between consenting adults (men and women) in the country as a whole.[333] Zambian law declares “carnal knowledge against the order of nature” punishable by 15 years to life in prison[334] and “acts of gross indecency” between same sex couples are punishable by seven to 14 years imprisonment.[335] Though many reports of consensual same-sex sexual conduct in the general population have been taken to the police, there have been no courtroom prosecutions.[336] The Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan 2007-2010 claims that condom distribution to inmates is forbidden by law, and provides only for condom distribution to members of staff, their family members, and inmates upon discharge.[337]
PRISCCA, ARASA, and Human Rights Watch’s findings confirmed a total lack of condoms in prisons; a strong homophobia and resistance to condom distribution within the prisons among the prisoners themselves; and a problematic association in HIV prevention messages between same-sex sexual activity between men and HIV/AIDS, with no mention of harm reduction or condom use. The issue of condom introduction currently evokes strong responses from many inmates: Elijah, 34, an inmate at Mukobeko, said “condoms can never be allowed by inmates because they are not useful. I heard that the government wants to supply condoms in prison, but we wrote a letter complaining to the commissioner. They would be a passport to sexual activity if we had them. We will demonstrate if they bring condoms here.”[338] Inmates’ responses to the idea of the introduction of condoms ranged from describing condoms as “difficult to talk about”[339]to “not necessary”[340]to “a disaster.”[341]
Cross-Cutting Failures in Delivery of All Medical Services
Lack of Prison-Based Services
Here, there is no medicine.
– Mwamba, 26, Mwembeshi Prison, October 6, 2009
The Zambia Prisons Service is in great need of medically trained staff and equipment at the prison level, and medical facilities are virtually non-existent at most prisons. Four of the prisons we visited had no medical care available inside the prison, relying on the community clinic or hospital to provide all medical care, in addition to the TB and HIV/AIDS services discussed above. At Mumbwa, Japhet, 38, told us that, at the prison, “we have no trained, qualified medical personnel. We only have a room, no medical staff.”[342] The officer in charge at Mumbwa agreed: “We don’t have medical personnel to treat prisoners.”[343] A clinical officer used to visit the prison, but had not done so for six months at the time of our visit.[344]At Mwembeshi, Mwamba, 26, reported “here, there is no medicine. The nurse will give you a referral for the clinic, but they don’t take you.”[345]
Those prisons we visited which do have prison clinics often only have paracetemol and lack basic equipment and infrastructure including running water, disinfectant, and gloves. Despite reporting a wide range of ailments, among the prisoners we interviewed, 19 percent of men and 36 percent of women had only received painkillers and no other medicines. The chief medical inspector at Kamfinsa reported that he is not satisfied with the care provided to the inmates, as he needs more staff and better infrastructure and equipment (including a blood pressure monitor, stethoscope, and forceps). He had received no reply to his letter to the Ministry of Health requesting such equipment.[346] Prison clinics suffer from frequent shortages of medication. The chief medical inspector at Kamfinsa confirmed that a “big problem is running out of drugs at the end of each month. We get a three-week supply from the district, so a one-week shortage happens regularly.”[347]
Lack of staff and drugs make medical care inconsistent. According to Howard, 29, an inmate at Mukobeko, “sometimes they help you, other times no one is there. Sometimes there is no medicine. The clinic has no equipment.”[348] Lawrence, 33, reported:
I take drugs for epilepsy. They should be taken daily. When they are not available at the clinic, though, I don’t take. They are not available once or twice in a month, and I miss at least one week a month. I have seizures when I don’t have the drugs ... I have had three seizures in the last year because I didn’t have the drugs. I usually have problems because the medication is not available.[349]
Mumba, 44, confirmed: “Every time I try to go to the clinic there is a shortage of drugs.”[350] “Medicine is the problem; the clinic lacks medicine,” concluded an inmate at Kamfinsa—“by the time you get to the hospital it is too late, you have already been mistreated and the disease is advanced.”[351] Clifford, 41, another inmate at Kamfinsa, described a similar situation—that medical staff are serious but overworked and “they have no equipment, not even a stethoscope.”[352]
Low levels of testing for TB, and prioritization of testing for respiratory infections, may partially be attributed to the fact that capacity for TB testing does not exist within the prison clinics or nearby community clinics, whereas prison clinics (where they exist) may have antibiotics. TB testing is not offered at Mukobeko,[353] and Daniel, 39, a male convict at Mukobeko prison, said that in deciding whom to take for medical treatment, prison officers “wait until you have no strength left and then they will take you. Even with TB, lots of people are coughing and spitting and they will let it go for months before they do an x-ray....it takes a century for TB because they have to take you to the hospital.”[354] According to one officer at Mwembeshi:
Every a.m. I check my prisoners for signs and symptoms of TB. Then I take them to our nurse, who takes them to the community clinic. But they only do a sputum test; there are no further investigations. Our only hope is UTH [University Teaching Hospital in Lusaka, 40 kilometers away].[355]
The unavailability of prison-based services is also a major barrier to proper HIV treatment. CD4 count testing currently happens only inconsistently, partly because CD4 testing machines are not available at any prison. Prison officials at Mukobeko cited the lack of a CD4 count machine, lack of fuel, and lack of transport, as a problem in providing proper HIV treatment.[356] J. Kababa, the officer in charge at Lusaka Central, informed PRISCCA, ARASA, and Human Rights Watch that “There is no CD4 count equipment at the clinic so I have to take prisoners all over the city. Officers don’t want to take dangerous people out as they might escape and [the officers] will be blamed.”[357]
Partly as a result of the lack of prison-based medical personnel and infrastructure, there is a lack of individualized HIV treatment or recognition of the possibility of drug resistance—inmates routinely reported receiving the same dosage of ART as each of their fellows every three months, without any individualized counseling, testing, or discussion, even when their CD4 count showed no improvement over time. Emmanuel, 35, a prisoner at Mukobeko, reported:
I started HIV meds two years ago, I am not doing well...I have side effects of the medication including neuropathy, swelling, diarrhea. It has been one year since I saw a specialist; they told me they have no transport to take me. So they keep bringing me the same drugs every three months.[358]
For many illnesses (aside from HIV and TB), church representatives and well-wishers frequently fill the role of pharmacist, obtaining medications for prisoners:
We visit the clinic by all means each time we are sick. We are not denied access. But the kind of treatment we need is not found there. We are referred, but we face a problem with that because the hospital is far and we need fuel and transport. Normally, when they give us a prescription, our relatives or the church people have to go and buy it.[359]
“When we are escorted [to the clinic], we are given expensive prescriptions, but we can’t afford them,” an inmate at Lusaka Central told us.[360] Inmates reported that medicines are frequently only available through church and well-wisher visitors: “Medication is provided by Father Bohan [an Irish priest who visits the prison] on prescription from the prison clinic. Deaths were so much, mostly amongst those on death row, before Father Bohan came to our assistance.”[361] Douglas, 40, an inmate at Mukobeko, concluded: “Without the priest, we would hardly have any medicine.”[362]
Drug shortages are hardly surprising, given that the Prisons Service provides minimal funding to fill the gaps when Ministry of Health-provided supplies run short. As the officer in charge at Lusaka Central lamented, “there is no prison budget for medical care. All of it is funded through the Ministry of Health, so when funds run out, they say ‘use your own prison budget,’—but there is none.”[363] The officer in charge at Mumbwa agreed: “There is no budget for medical care for inmates.”[364]
Barriers to Accessing Community-Based Medical Services
Access to community-based clinics and hospitals poses a problem for many inmates. According to the nurse at the clinic serving Lusaka Central confirmed, “There are problems with delays in prisoners getting to the hospital. It can become a delay of weeks.”[365]
PRISCCA, ARASA, and Human Rights Watch interviewed inmates who had waited long periods for referrals to outside medical services: Clifford, 41, an inmate who had water on the lung outside of prison, had received no treatment for the two years he had been in prison—he had never been to the hospital, though he had asked many times.[366] Inmates reported requesting treatment multiple times unsuccessfully: “I had tried to seek medical treatment many times but have not received it. They say sometimes they do not have an officer to escort us to the clinic. I have requested to go six times and have been refused. I have many problems. When I fell sick, I asked for attention, but was not able to go to the clinic.”[367]
According to prison officers, lack of personnel, transport, and fuel to take inmates for care are all major barriers. The officer in charge at Mumbwa said, “Sometimes we don’t have officers to take to the clinic—so they cannot go”[368]; at Kamfinsa, the officer in charge informed us that “staff shortage causes medical care problems as I lack staff to take inmates to hospital.”[369] The medical officer at Choma reported that delays in bringing patients to the clinic as a result of shortage of manpower was the primary barrier to patients accessing necessary testing and treatment.[370] Lack of transport and fuel were named as major barriers in accessing medical care by prison officers at Mukobeko,[371] and the lack of transport to take inmates for medical care for specialized care and referrals was also a challenge at Choma.[372] Even for seriously ill prisoners, according to an officer at Mwembeshi, “we just wait and find someone from the Prisons Service who is travelling to and from Lusaka. It may take a week before a sick prisoner makes it to the hospital.”[373]
Felix, 43, an HIV-positive remandee, reported:
I also have breathing problems....I was tested in prison and was on TB treatment in 2007... in April 2009 I started developing the same symptoms again. I went to the clinic and was referred to Kabwe General Hospital for an x-ray, but the machine was not working. I have asked the officer to take me again, but the officer said that I need another referral, and the clinic hasn’t worked for the last two weeks because the clinical officer has been away.[374]
We spoke with inmates currently on TB treatment who had waited between two and three weeks and one month, respectively, to initiate treatment after TB diagnosis.[375] Concluded one, “I think that people in prison want to be tested for TB. The delay to get tested is not at the hospital or the clinic. The delay is here at the prison. For people to take us from here, it is long. Some people die before they can be treated.”[376] The officer in charge of Lusaka Central confirmed that the biggest problem he faces with medical care is transport, and he is not satisfied with the medical care for prisoners: “TB and HIV patients must go to the hospital, and the numbers are so large there are delays.”[377]
Multiple inmates reported delays in proper HIV treatment as a result of lack of prison-based services. Mwape, 47, who had tested positive for TB and HIV, reported that he was on the wrong treatment for two years as his CD4 count plummeted at Lusaka Central, where he was taken for treatment. Now on second line treatment[378], he reported feeling a bit better, but “there were delays in getting me to the hospital—they cite security reasons and I have seen people die from it.”[379] Mutale, 40, at Mukobeko, informed us that “for opportunistic infections it’s hard to get to the hospital. It can take two weeks sometimes. The officers think we are just malingering. I often suffer from symptoms like diarrhea and chest pains without treatment.[380] An inmate at Kamfinsa Prison reported that he had been tested for HIV and found positive, but had been waiting for a CD4 count test for five months.[381] Frederick, 23, similarly informed PRISCCA, ARASA, and Human Rights Watch that he had been waiting for a CD4 test after a referral to the community clinic, in this case “because I look healthy and am new, they won’t let me go.”[382] Another inmate, at Mukobeko told a similar story: “they are taking CD4 counts, but rarely, like every six to seven months. For example myself, I have never had my CD4 count since being here [since July 2008].”[383]
When care is delivered at outside clinics and hospitals, a number of inmates also reported the stigma that they face from the general population by virtue of their easy identifiability as prisoners.[384] Chanda, 36, a convict at Mukobeko, expressed sadness: “They are tied to shackles on both feet/legs and hands as they walk into the hospital outpatient or admission wards, where they are also tied on chains to the bed and are not allowed to go to the toilet but are provided with bowls where they should either urinate or defecate in full view of all other patients and their bedside caretakers or relatives. The majority of those who fall ill avoid being exposed to such conditions and rather prefer to die within their prison cells.”[385] Henry, 34, at Lusaka Central, reported discriminatory treatment:
At hospital the nurses discriminate against you because you are a prisoner. I am shackled, and the nurses ignore us. I think it is because we are inmates that they don’t take care of us. They have to send inmates from the prison to clean up after the prisoners who are patients because the nurses won’t do it. They discharge early, especially if the prisoner can’t get to the bathroom himself. They get rid of them. Someone died a week ago, he was very thin, very ill, and they took him to wash him but it was too late, he died.[386]
A nurse at the University Teaching Hospital, the tertiary referral hospital for the entire prison system, confirmed that when prisoners are admitted, “they cuff them at the bedside” which presents a problem as “sometimes there is no one to unlock them to take them to the bathroom.”[387]
Security Concerns
Sometimes it is difficult getting to the clinic, sometimes you may not get to go. We ask the cell leader—the guards might say no, though. For those who have big cases, they are afraid they may run away. I have seen people turned away....They have no problem taking convicts, but remandees have a problem because they are afraid we will escape.
– Peter, teenager, Choma Prison, October 8, 2009
Security concerns prevent many inmates from accessing medical care in a timely manner. Mumba, 44, an inmate at Mukobeko, reported that the practice of training prison officers in medical care led to a cadre of medical professionals with misaligned priorities:
They used to bring in health personnel who were very good. Now they have decided that they should train [security] officers to be health personnel. But to add security when we are very sick? They may not refer someone because of the fear of escape.[388]
Officers’ security fears in allowing inmates to go to clinic facilities outside of prison grounds undoubtedly prevent prisoners from accessing care, sometimes for extended periods. One “lifer” at Mukobeko reported “I have bronchitis. I have had no treatment yet because of security problems getting me to hospital. I’ve been waiting three years...they won’t take you for treatment until it is too late.”[389] Nickson, 36, an inmate at Mukobeko, reported:
I have been trying to push to ask for care, but it has not been working....The prisoners are being oppressed here, we are suffering....We are denied access to medical care. They do everything for the security of the prisons...Last time I was sick was two weeks ago—I had malaria. I suffered a lot, and everybody knew. I came to the clinic, and was given only panadol [paracetemol]. I asked to go to the hospital, and was denied. They said to me: “You remandees, you are problems—this prison is all about security.”[390]
Chiluba, 32, a prisoner from Lusaka Central, who was injured by a beating in police custody, was able to go to only the hospital upon direct intervention by the prison’s officer in charge:
I was not examined on prison entry, and it took me one month to go to the clinic. I was referred to UTH [University Teaching Hospital]. It took so long because some prisoners would escape on way to hospital. They had almost stopped taking people. I kept pressuring and upon the officer in charge’s intervention was able to get two prison officers to take me to clinic.[391]
Remandees, in particular, suffer from restricted access to medical care. A contentious relationship between the Prisons Service and police on the subject of remandee security and responsibility for remandees[392] escorted out of the prison result in many prisoners across facilities reporting that remandees are less frequently allowed to seek care than their convict counterparts. Officially, Zambian law provides that every prisoner is in the lawful custody of the officer in charge throughout the period of his imprisonment,[393] and according the deputy commissioner of prisons, “it is the responsibility of the Prisons Service when remandees need to go out when it comes to medical attention.”[394] But the officer in charge at Mumbwa described the prison officers’ calculus:
With remandees, we fear to take them [to the hospital] because we are afraid they will run away—the police will say we let them go deliberately. The police are supposed to take them to the clinic, but it’s rare, so normally they don’t go.[395]
Such uncertainty and fears over responsibility for runaway remandees leads to denial of treatment. Semba, 34, a remandee at Mumbwa reported: “I told the officer in charge about my [HIV] status—she says the police will take you to get it because you are a remandee. I’m feeling weak.”[396] A remandee at Lusaka Central informed us:
I have ankle pain. While playing football, I injured myself on the ankle. It gives me some pain even now. I have requested the officers to take me for an x-ray but they refuse. They say I am not yet convicted, and they fear I will run away.[397]
Johnston, 41, a remandee at Mumbwa, reported:
There is no clinic here. We complain but we are not attended to....They don’t take remandees to the doctor. They take the convicts but they say the remandees are going to run away. One or two who have been very sick got taken to the doctor, but most of them just end up complaining.[398]
Cell Captains and Officers as Gatekeepers
I have seen people die in the night in the cell—there is nothing we can do. We shout for someone, but the guards will say, “He is just playing sick, he wants to escape. Let us wait two or three days, and see how he will be.” And then he dies.
– Nickson, 36, Mukobeko Maximum Security Prison, September 30, 2009
Prisoners depend upon the permission of cell captains and officers to go outside the prison to obtain medical care. At farm prisons, prisoners depend on the permission of cell captains and officers to miss work in order to seek medical care. These cell captains and officers have no medical training, but act as gatekeepers to medical treatment, occasionally with the result that a prisoner becomes very ill or dies without being allowed to seek medical care. Some inmates reported specific limits on the number of inmates allowed to receive medical care each day, though PRISCCA, ARASA, and Human Rights Watch were unable to verify what specific limits, if any, exist at each prison aside from Mumbwa, which has a limit of 10 inmates per day. A female inmate at Kamfinsa described the process of accessing care through the officers: “When I feel pain, I give a request to go to the hospital. But there is a limit of five a day to go to hospital so some get priority. Officers choose who gets care on parade in the morning. If you are sick you raise your hand, they choose five to go. There have been moments when more than five raise their hands, but even then only five are designated for the clinic. I don’t know how they choose.”[399] Angela, 23, reported: “Sometimes you can go as long as a month waiting to go to the clinic... it depends on the officers. Some officers are good, some are terrible.”[400]
Prison staff tend to discount prisoner complaints as “malingering” or “tricks” in order to escape. Mwizya, 30, an inmate at Mukobeko, told us:
Convicts and pretrial remandees looking health[y] are not being attended to at the prison clinic or referred to Kabwe General Hospital and are mostly accused of imposing a fake illness upon themselves so that they can find a way to escape once admitted in the hospital ward. Prison officers wait until the inmate’s health condition deteriorates before attending to them.[401]
A remandee at Kamfinsa reported, “They work out their personal vendettas against you by denying you access.”[402]
Other inmates—called cell captains or masters depending on the context—also act as gatekeepers to accessing medical care: “The masters decide who is sick; those who look fit—they are told to go into their [work] groups.”[403] Martin, 39, an asthmatic inmate at Mumbwa, told us, “The cell captains are preventing me from getting treatment.”[404]
Refusals by officers and cell captains to allow inmates access to treatment can lead to devastating consequences, as described by Elijah, 34:
It is a struggle to get a referral; by the time you get it, someone might die. We had three cases in my section who died in the cells before going to the General Hospital or even the clinic. One had TB—but was not tested for it—and the other two had malaria. If you want to go to the clinic, the normal procedure is that the guards are supposed to pass through and ask how we are feeling. But they don’t. So the inmates report sickness to the person manning the gate. What happens depends on the officer—sometimes you are not taken to the clinic, or the clinic officer is not there. The three people who died were critically ill; the officers knew. Three months ago, when one of them died, the officers were informed, but didn’t take him to the clinic.[405]
PRISCCA, ARASA, and Human Rights Watch requested information from the Zambia Prisons Service on the numbers and circumstances of deaths in custody. At this writing, our request has not been answered, and we are thus unable to assess claims of deaths due to officer negligence.
Immigration detainees, in particular, may face discrimination from other inmates and officers in accessing care. As Jean Marie, at Lusaka Central, told us, “I asked the officer to go to the clinic but he said, you just need to wait for deportation. Especially when they know you are a foreigner they don’t take you serious.”[406]
Prison officers confirmed that they—and in some cases the captains—are gatekeepers for medical care, even expressing discomfort with this position. The intelligence/offender management officer at Choma prison reported that “we [assess inmates’ health] every morning, we determine who goes to the clinic and who doesn’t, and screen them thoroughly to prevent escapes.”[407] At Mumbwa, 10 inmates are taken to the clinic each day, regardless of whether more are on the sick line. The officer on duty—who has no medical training—decides.[408] The medical officer stationed at Mukobeko informed us that “there are stages and monitoring by captains who take care of the sick.”[409] The officer in charge at Lusaka Central expressed succinctly the problems inherent in this system: “Leaving [when prisoners receive medical care] up to me is not a good option, as I and my [staff] are not medical people.”[410]
Range of Services Delivered
Between the few prison clinics, and outside clinics and hospitals, we found that inmates routinely do not receive certain types of basic and essential medical care. Despite Zambian law providing for medical examination of each prisoner upon entry,[411] our interviews almost universally found, and the physician who heads the prison medical directorate confirmed,[412] that no medical screening or testing occurs for prisoners upon entry to a facility. “We need monitoring,” said Dr. Chileshe. “It is a mammoth task, the earlier we do the better. I want files for everyone, not just the sick.”[413]
Shortages of all types of medicines (except ART and TB medication) were an element of our findings at each facility we visited, both at the prison clinics and reportedly at outside Ministry of Health hospitals and clinics (therefore also impacting the general population). Lawrence, 33, reported that at the hospital, “most of the good medicines are not available.”[414]
Mental health services are grossly insufficient for prisoners, though they are also entirely insufficient for the general population.[415] Zambian law requires that social workers, psychologists and—when necessary—psychiatrists should be seen as “crucial players in any multidisciplinary response to problems such as HIV and AIDS,”[416] and international standards provide that “the medical services of the institution shall seek to detect and shall treat any physical or mental illnesses or defects which may hamper a prisoner's rehabilitation.”[417] Current mental health facilities for prisoners are essentially non-existent. Prisoners with “complicated” mental illness are sent to the prison wing of Chainama Hospital, a Ministry of Health facility that in February 2010 housed 19 inmates found either not competent to stand trial or criminally insane.[418] However, for those mentally ill inmates in the general prison population, the Prisons Service does not employ any person responsible for mental illness and does not have any psychiatrist or other mental health professional on staff. Dr. Chileshe reported that patients with mental illness may be held at Lusaka Central, and in that case, “as is possible,” they receive medication, though there were no specific medications for mental illness in the medication cabinet of the prison clinic at the time of our visit.[419]
Multiple inmates reported symptoms suggesting mental health issues. As James, 36, a condemned inmate said, “inmates start hallucinating, planning to get out, because of an inability to have appeals, proper food, and progress in our education. As a result you see mental deterioration in the condemned. I can say this is happening to 101 percent of us.”[420] The mentally ill further suffer from the loss of the little medication they are prescribed: “benzodiazepines are stolen from the mentally ill. The government doesn’t care about the mentally ill.”[421] Artane (Trihexyphenidyl), prescribed to the mentally ill, is also frequently stolen or sold for food and other basic necessities and diverted within the prison.[422]
Women’s Health
Women face a distinct set of healthcare needs in detention.[423] Yet women are a minority and often receive little attention.[424] In addition to experiencing the problems accessing care described above, our findings suggested that incarcerated women in Zambia also face distinctive challenges.
International standards dictate that for women in detention, there shall be “special accommodation for all necessary pre-natal and post-natal care and treatment.”[425] Prenatal care is widely available in the general population.[426] However, the incarcerated pregnant women PRISCCA, ARASA, and Human Rights Watch interviewed described inadequate, and in some cases non-existent, pre-natal care. Helen, 27, who reported she was six months pregnant, said:
I have not been to the clinic yet, no antenatal care. I went to the clinic once but was told the nurses were not working. Since then I have not asked. I do not feel well, lots of ups and downs.[427]
Pregnant women face the same challenges in accessing care as other inmates: “It’s hard...they only count few of us for treatment, then tell the rest of us to wait for tomorrow and restrict us from going. I had no initial exam when I came to the facility, even though I am pregnant. No special treatment is given for pregnant women, I take whatever I can.”[428]
In other cases, pre-natal care existed but was inadequate. The WHO protocol for Prevention of Mother to Child Transmission (PMTCT) of HIV notes that even “[a]ll HIV-infected pregnant women who are not in need of ART for their own health require an effective ARV prophylaxis strategy to prevent HIV transmission to the infant. ARV prophylaxis should be started from as early as 14 weeks gestation.”[429] The chief medical inspector at Kamfinsa prison claims that the WHO PMTCT protocols are used—though they change and additional training is not provided.[430] Yet, Tasila, 24, an inmate at Kamfinsa, who was eight months pregnant, reported treatment directly in violation of WHO guidance:
I already knew when I came in that I was pregnant. I have accessed care three times since I have been in here. The first day that I went, they felt my tummy and told me that the fetus was too small. The second time, they took a blood sample and told me that the baby was growing. The third time, I had VCT—they tested my blood again and told me I was HIV-positive. They told me my CD4 court was too high for ART. I wasn’t given any HIV drugs to prevent transmission, only folic acid and vitamins.[431]
Dr. Chileshe noted that there is no PMTCT program in the prison medical directorate,[432] though PMTCT has been scaled up in recent years in the general population: Between 2004 and 2007, the estimated percentage of women living with HIV who received ART for preventing mother-to-child transmission increased from 18 to 47 percent.[433]
Pregnant women also face stigma when accessing maternity care in public hospitals, accompanied by prison officers.[434]
Women also had not received any gynecological, cervical, or breast cancer screening, though the availability of such services is also limited in the general population.[435]
Child Health
Despite provisions in the Convention on the Rights of the Child noted above guaranteeing children’s right to health, PRISCCA, ARASA, and Human Rights Watch also heard reports from mothers held in prison with their children under age four that those children do not consistently receive adequate health care, and face similar medical care challenges as incarcerated adults. We heard a report at Lusaka Central Prison that a baby had died recently of diarrhea, and was sick for three days before going to the clinic.[436] Inonge, 42, informed PRISCCA, ARASA, and Human Rights Watch that “my child had a high temperature and cough. She was taken to the [community] clinic by prison officers but there was no medicine.” Instead, a donation from a religious organization allowed the mother to purchase medicine for her daughter. “Sometimes there are no medicines for my baby,” Inonge concluded.[437]
Children detained as juvenile inmates frequently are confronted by restrictions on their ability to access medical care similar to those faced by adult prisoners, despite international law protections. Isaac, 17, was wheezing when PRISCCA, ARASA, and Human Rights Watch spoke with him. He had asked at the clinic for help with his breathing troubles, and they had said that they would take him to the hospital, but seven months had gone by and he had still not been taken to the hospital.[438]
Continuity of Care
What medical care prisoners do receive suffers from interruptions upon transfer between facilities and upon release from prison. Mulenga, an inmate at Mukobeko, reported,
I was being seen by a specialist in Lusaka [prior to arrest] but here they won’t allow me to keep seeing that doctor. I get some care at Kabwe General but there is a conflict in treatment. My medical records are still in Lusaka, and I am trying to convince my relatives to retrieve them and bring them here, because Kabwe General said that it is too tedious to request them.[439]
In Zambia, inmates face interruptions in medical treatment upon release from prison, when no provision is made for continuity of care. The Zambia Prisons Service does not have a policy on coordinating medical care on entry to, between, or upon exit from custodial settings. Inmate files are lost, inmates have difficulty knowing where to go to receive care, and inmates returning to rural areas may find themselves entirely unable to continue treatment upon release.[440] The Prison Fellowship of Zambia operates one halfway house in Lusaka, which can accommodate up to 20 inmates; but they are the only prison reintegration program operating in Zambia. “The prisons don’t have reentry programs,” they reported.[441] One former inmate reported that, while having chest problems upon discharge, he received no medical record: “I just came out without a medical record. Who is going to give me a medical record?”[442] The prison clinic at Lusaka Central confirmed that, while they actually keep records for all patients seen, there is no mechanism for patients to obtain their medical record information upon release from prison.[443]
Non-scheduled interruptions in HIV treatment can result in illness, the development or drug resistance, or death. Yet interruptions in HIV treatment result from transfers, discharge, and in the entry process itself, at the police station. Pre-trial detainees in police custody face particular risks. Aaron, 26, informed us that he spent 42 days at the police station: “I was on ART at the time but they would not let me bring my medication from home. Between the delay at the police station and upon entering prison, I missed three months of HIV medication.”[444] Misheck, 32, reported, “I did miss doses [of ART] for a while right after I was arrested when I was in the police station for four months. They don’t give you any medicine there, or food. My family brought my drugs but the police hid them.”[445] Police Service officials acknowledge that interruptions in medical treatment may take place when individuals are taken into custody and then are taken to prison and admitted a need for a single medical directorate to coordinate care for inmates in police and prison custody. Medical records don’t transfer with an inmate, and medical services for the Police and Prisons Services are coordinated separately.[446]
Record-Keeping Problems
Accurate statistics on disease and death within prisons are important both for public health purposes—to address current morbidity and mortality, and plan for prevention and treatment—as well as to establish grounds for recourse for prisoners whose illness or death may be due to government action or inaction. However, it is currently difficult to establish the actual number of people who become ill or die in Zambian custody. Dr. Chileshe specifically warned PRISCCA, ARASA, and Human Rights Watch not to trust any of the numbers currently reported by the Prisons Service, as statistics are not compiled reliably either by the Prisons Service or the different clinics and hospitals prisoners attend.[447]
Inmate reports of illness and death were widely divergent from officer reports. At Mukobeko, one inmate told us, “people infected with TB are held together with those with HIV, who are not cared for or given supplemental foods. I would say that four to five people a month die. In April it was 15 in one month.[448] The Legal Resources Foundation claimed: “People die in the night and they bring out the corpses. Many die—three a week at Lusaka Central.”[449] At Lusaka Central, however, the officer in charge informed us that there were 20 deaths in all of 2008—14 male convicts and six male remandees, of “TB, HIV and malaria”—in 2009, one death through October 2009.[450] Death reporting is likely to be inaccurate, as inmate deaths are not officially investigated if they take place in the hospital—only if they actually take place in the cells. This contravenes Zambian law that provides for the prison medical officer to record the cause of all deaths and past illness[451] and international standards call for an inquiry into each prisoner death.[452]
Prison officers reported HIV and TB to be the primary causes of inmate deaths, but such claims are impossible to verify as the vast majority of these deaths occurred in the hospital and so were not investigated.[453]
Medical Care Challenges at Farm Prisons
At the prison, we work all day, work all day—no good. I am feeling a pain when I’m talking. I can die. We are working. People are sick here in prison....We are not going to hospital here, please help me to go to hospital. I have told the officers. I want to die. I have no help here now. I don’t know if I can die. I have told them I am sick—I was told to wait.
– Gabriel, 45, Mumbwa Prison, October 5, 2009
Inmates at farm prisons appeared to be particularly restricted in their ability to access medical care, as their attempts to do so were frequently rejected as a ploy to avoid work. Inmates at Mwembeshi reported that they were sometimes not allowed to go to the clinic or hospital when sick, and instead were made to work: “It is not possible here to go to the doctor. At the moment we wake up, we go to the field, then we go to a different field. Even if you complain it is not ok—the officers tell you that you still have to go, and instruct the masters to say no.”[454] Only as a last resort, when inmates are too weak to work, are they taken to the hospital for treatment.[455] The ill are routinely taken to the fields to do hard labor: “At this prison, you tell the cell captain you are sick, they tell the guards you are not. Some of the prison officers are not very good. The one on duty doesn’t listen to complaints, doesn’t write down names. Those who are not very ill are taken to the hospital. I don’t know why—but the very ill are taken to the fields.”[456]
Distant from health facilities—at Mwembeshi, the nearest hospital and ambulance are 40 kilometers away in Lusaka, and even the local community clinic is four kilometers from the prison[457]—inmates are dependent on visiting medical professionals for health care. Rabun, 28, an HIV-positive detainee at Mwembeshi who reported sores on his genitals, described some of the complications attendant on relying on visits from visiting medical staff from University Teaching Hospital (UTH) or the Go Centre:
UTH visitors have monitored me, but I am on no HIV treatment and no treatment for the sores on my genitals. It is difficult because of the lack of medical facilities here—we depend on doctors from UTH. Sometimes when I feel sick the officers don’t take us to the hospital. They rarely take us for medical attention. Sometimes they allow us to remain at the prison, other times we go to work. I have had sores on my genitals for two weeks. I asked to go to the clinic, and they promised they will take me tomorrow, but when the day comes they have changed their shifts and a different officer comes in. They keep on promising, but it does not happen.[458]
Inmates reported that they sometimes had to bribe the inmate “chairman” designated to make the list for the Go Centre in order to obtain a place on the list.[459]
Corporal Punishment and Ill-Treatment
Solitary confinement, naked, in water with limited food; corporal punishment by prison officers; beatings by cell captain inmates to whom disciplinary authority is ceded; and beatings in the fields, constant work, and denials of water for inmates sentenced to hard labor all amount to cruel, inhuman or degrading treatment. Prisoner treatment and discipline—at the hands of both prison officers and the inmates to whom disciplinary power is delegated—often violate international and regional law and standards. Widespread physical abuse, humiliation and ill-treatment also have serious implications for inmates’ mental and physical health.
International law and prison standards, and the Zambian Constitution, prohibit the infliction of (including acquiescence to) torture or cruel, inhuman or degrading treatment or punishment against persons in detention, including corporal punishment.[460] The UN Human Rights Committee has admonished Zambia for reports of torture and ill-treatment of persons deprived of their liberty[461] and for failing to supply information on the system for prosecuting and punishing acts of violence against prisoners.[462] Additionally, international standards forbid prisoners from being employed in any disciplinary capacity, or being punished by placement in a dark cell.[463] In response to a complaint from a disabled child detained in a solitary cell without facilities, no natural light, without a blanket or clothing, and subjected to physical abuse, the UN Human Rights Committee noted that confinement in an isolated cell “without any possibility of communication, combined with his exposure to artificial light for prolonged periods and the removal of his clothes and blanket” constituted a violation of the obligation to treat detainees with dignity.[464] Zambian law clearly lays out disciplinary infractions of varying severity and makes provision for punishment,[465] and some inmate reports suggest that corporal punishment from officers has decreased in recent years following a change to the law.[466] Yet officers and inmates still routinely inflict corporal and other inappropriate punishments, contrary to Zambian law and Zambia’s international human rights law obligations.
In cases of abuse, prisoners should be able to access a remedy. International standards provide that detainees should have access to a confidential complaint mechanism.[467] Yet Zambian prisoners do not consistently have access to such a complaint mechanism.
The Penal Block
Mostly, people come out sick. No one has come out in good health—they change completely in there. They don’t always get taken to the clinic, though, unless the inmates put pressure on [the officers]. We say, “this person will die, as you killed the others.”
– Elijah, 34, Mukobeko Maximum Security Prison, September 30, 2009
Except Mwembeshi, each of the facilities we visited had some form of penal block isolation cell where prisoners could be taken for punishment in response to violations of prison rules ranging from engaging in sexual activity, to using alcohol or drugs, to fighting, to disrespecting officers.[468] We were allowed to view the penal block at only one of the facilities—Mumbwa—and observed it to be a dark, two meter by two meter cell, without ventilation. The room was empty, with a bare, hard floor, but the graffiti on the walls told the tale of the misery that had been experienced within the cramped walls: “hard, no, no,” “fools seek to blame,” “sucuide,” (sic) and “hard men no no,” had been painstakingly etched into them.[469]
Zambian law provides for confinement in a separate cell as punishment for certain prison offenses, with a “penal” or reduced diet, for periods as long as 25 days.[470] Prior to such confinement or reduction in diet, a prisoner must be examined by a medical officer and periodic checks of the prisoner’s condition are required by Zambian law and by international standards in cases of confinement or reduction of diet.[471]
The descriptions from inmates of punishment inflicted in the penal block were consistent across facilities.[472] Prisoners are stripped naked and put in a small, usually windowless cell (one to two meters by one to two meters), with water poured onto the floor to reach ankle or mid-calf height. There is no toilet in the cell, so that inmates are forced to stand or sit in water containing their own excrement. Prisoners sleep in the fetid water on the floor of the cell. Prisoners are held in this manner sometimes for days on end[473], either with no food at all for shorter (daytime) stays or with “penal diet” (food rations only every other day) for longer stays.[474] However, as Henry, 34, noted, even eating this minimal food puts inmates in a terrible bind: “You refuse food because there is no toilet.”[475] Bernard, 40, described the ordeal of the penal block in detail:
I went to the penal block one time, but I only stayed for one night because I was coughing up blood and they were afraid I would die. But others stay for two weeks, 21 days, or 30 days. It’s dirty there, not fit for humans. That’s where they used to keep people to be hung when there were still executions. It’s hell all on its own. They remove your clothes, put you in one of the rooms, and pour two buckets of water in there with you. Then you get a penal diet—it’s the same food but just less. One of our friends was taken there and beaten to death.[476]
In the winter months, especially, naked confinement in fetid water is extremely difficult for inmates to bear and we heard reports that inmates frequently require medical attention and even die after release from the penal block.[477] “Usually when one comes out of there one is weak and sick,” Lawrence, 33, at Mukobeko, observed.[478] Mumba, 44, at Mukobeko, reported that “many have come out sick—you don’t always get ART in there.”[479]
There is little doubt that the use of these cells per se to inflict punishment constitutes prohibited inhuman and degrading treatment. Extended use of these cells when combined with other punishments, such as being stripped naked, food restrictions, denial of access to the toilet, and being made to stand ankle-deep in water, constitutes a form of torture.
Some inmates described officers who relish the pain of the inmates: “They pour water in there and put you in there naked. The water stays on the floor, and you can’t sleep. The guards enjoy it if you commit an offense when it is coldest.”[480] Indeed, Winston, 35, reported that officers sometimes use penal block punishment to settle personal vendettas:
If you make a complaint about an officer, you have started a war that will never end. There is systematic harassment; I know because I have been in the forefront of making such complaints. The commanding officer will come and say, “Those of you who want to act like you are a student union at university, you will stay here. If you want to get out you will shut up. Stop complaining, you have no rights; you are just criminals.” Officers use other inmates to make complaints about you and you end up on the penal block. It happens a lot.[481]
Several officers confirmed inmate descriptions of treatment in the penal block. The deputy officer in charge at Mukobeko said: “We remove clothes to prevent the risk of committing suicide. They are with nothing—no bedding, no clothes. The duty officer can pour water in.... This can be with or without penal diet—we remove portions from every meal. We have two cases or so a week.”[482] At Mumbwa, the officer in charge similarly described the punishment in penal block.[483] Some officers expressed concern about the use of the penal block: The officer in charge at Kamfinsa said that the penal block is available but “we’re discouraged from it...because of human rights awareness we don’t do it,” as the Prisons Act requires frequent checks on those in penal block and he doesn’t have the time; furthermore, the penal diet cannot be used because it is inadequate.[484]
Some inmates reported that prisoners are beaten prior to or during confinement in the penal block.[485] “There is also torture there,” reported Samuel, 50, at Kamfinsa. “People are beaten with sticks. The convicts are whipped when they commit an offense.”[486] Mutale, 40, an inmate at Mukobeko reported that his friend was beaten to death in the Mukobeko penal block in 2006, and while officers investigated after the inmates protested, there was no arrest[487]; another inmate reported that a fellow prisoner died from beatings at the Mukobeko penal block in 2007.[488] The penal block, Patrick, 48—an inmate at Kamfinsa—concluded, is “not a safe place. They do things there the old Zambian prison way.”[489]
While typically, children did not appear to be subjected to penal block punishment, Oscar, a teenager, had been held in the penal block at Lusaka Central three years previously, and described the terror he felt:
I have had the experience of being taken to the penal block. There is a small room, where three people can sit. They pour water. You are isolated, in the room alone with the water. They took me there when I came in as a young person [as punishment for theft]. I was kept in there for four days and nights in the cell. The water was above my ankles. There was no light, no windows. There was no beating—the isolation, the water are the punishment. It being the first time, I was really afraid. It was pitch black. I didn’t know what was coming next. I felt very afraid and insecure.[490]
Additional Officer Punishments
The Zambia Prisons Service has clearly made a significant effort to improve disciplinary practices in recent years. The legal abolition of corporal punishment by officers speaks to a commendable desire for and effort toward change in some quarters, and some inmates informed us that officer-inflicted beatings had decreased.[491] One of the most common forms of punishment by officers, reported by numerous prisoners across all prisons, is the loss of early release (“adding days” to the sentence)[492]—a punishment that is acceptable under international standards. Forms of work are also frequently used by officers as punishment.[493] It must be noted, however, that seemingly acceptable forms of punishment may at times be inflicted in discriminatory or otherwise unacceptable manners.[494] One immigration detainee at Lusaka Central reported that when any one of the immigration detainees violates a rule, all of the immigration detainees are made to clean the toilets.[495]
Significant challenges remain in eliminating inappropriate officer punishments. Corporal punishment of prisoners is contrary to Zambian law, and prison officers categorically denied that officers inflict corporal punishment. The officer in charge at Mukobeko reported that punishment is never physical,[496] and prison officers from Kamfinsa informed us that there is no beating.[497] At Lusaka Central Prison, the female deputy officer in charge claimed: “This has changed according to the Prisons Act. There is no violence since I came, no violence here. We keep according to the law. There is no physical punishment. We are just friends.”[498]
International monitors have expressed concern that practical implementation of the abolition on corporal punishment may not have taken place,[499] and our interviews with inmates confirmed that corporal punishment by some officers endures, despite a general trend away from such punishment. An inmate at Mukobeko told us that he was badly beaten by a senior prison officer after he asked for a parcel sent to him by an overseas penpal.[500] Ngwila, 67, reported that just the previous week he had been beaten, and that the officers sometimes beat the inmates for no reason.[501] Clifford, 41, an inmate at Kamfinsa, said “someone just got taken to the penal block today. This is where the worst abuses happen—beatings by junior officers. They operate without supervision from the officer in charge.”[502] As noted above, such beatings sometimes precede or take place during penal block confinement. One inmate told us:
When a person becomes unruly, the officers use excessive power, manhandle him, and beat him up. I witnessed one such incident at Lusaka Central prison. The prisoner misbehaved and there was a mini-riot. The officers had to come in and they beat him up and confined him to the penal block.[503]
Female inmates at Kamfinsa prison reported that inmates are slapped on the back by officers as punishment[504] and also receive strokes with a stick.[505] Inmates at Mwembeshi reported slapping and beating by the officers when inmates resist work.[506] David, a teenager, described officer beatings in more detail:
As for physical abuse, some of the officers are harsh and can slap prisoners or call us names. Yes, I have seen injuries after. Some of the inmates, when they are given work, they resist and say they are tired. They attract physical abuse, slapping. They may bleed from the mouth after, or complain of internal pain.[507]
Erick, a teenager, reported that officers beat inmates as punishment without the knowledge of the officer in charge:
When the inmates demand to go to hospital they are prevented from going so that the officer in charge doesn’t know an officer has injured an inmate. The officers tell the lie that the duty officer is not available to keep us from the clinic, saying that the officer in charge has traveled. The cane is two inches thick, two feet long. I have been caned two times personally. Once, I felt sick because of malaria and I was not able to eat. They said it constituted a crime, that if I don’t want to eat, it constituted a crime. They said if I don’t want to eat, I should give to share with a friend. I was given 10 strokes. The second time, I had visitors from the church who wanted to help me with my case. I was ordered to clean the toilets, but my absence led to be being given 25 strokes. I asked to go to the clinic, but was denied. I was swollen.[508]
Additional reports of abuse at the direction of officers include forms of sexual humiliation, particularly of female inmates. On the women’s side of Kamfinsa Prison, for example, female prisoners reported being stripped naked, smeared with mud, and placed in the hot sun of the prison central courtyard to be viewed by all female prisoners for an entire day as punishment at the explicit direction of the officers.[509] One female inmate described this punishment:
If an order is broken, the inmate is stripped naked, mud is applied by other inmates at the direction of the officer, and the inmate is told to sit in the sun until lockup. Mainly this would happen if between inmates we fight or pick a quarrel—the officers come to judge who is wrong and then to punish. Some have fallen sick after that treatment—I have seen it happen three times.
This punishment is aimed at humiliating or insulting our personality. How can they make me strip naked before younger women who could be my daughter, without taking to consideration how I would feel as a woman, as a mother?[510]
Further forms of sexual humiliation and verbal abuse exist, particularly for female inmates. For example, one inmate reported that as punishment, the officers may put the inmate into the center of a circle of the other prisoners at bath time, where each “showers insults at her, calling her the names of private parts.”[511] Agnes, 25, at Kamfinsa told us “truthfully, each officer has her own problems. Some are harsh, some don’t accommodate us. To tell the truth, we were told to say that there are no problems, but each has their own problems....They degrade us, shout, call us names, make reference to the fact that we are criminals.”[512]
A child detained at Choma reported that another child was tied with a rope and taken out into the sun for approximately two hours for screaming at an officer.[513] Adults at Choma also reported a practice whereby a prisoner would be drenched with water and made to roll on the ground.[514]
Strip searching by officers, while not inflicted as punishment, also greatly disturbs inmates. Inmates reported that they were strip searched, both when returning from court, and at regular intervals in the cells themselves. Multiple inmates reported the shame involved. “I feel grieved about it,” a female inmate at Kamfinsa Prison reported, “I even pray to God that I can just die. The pain and shame is too tough to bear.”[515] In one instance, PRISCCA, ARASA, and Human Rights Watch received a report from a prisoner at Lusaka Central that a body cavity search for all inmates was carried out with a single pair of gloves,[516] an unsanitary practice compromising the health of inmates. Officers, however, denied such treatment: “When we suspect a prohibited article, we carry out a search. We look under beds, in hidden places. We don’t undress physically, but we do rub down. We never look inside bodily cavities, it is against human rights.”[517]
Cell Captain “Justice”
The captains are police in the cells—what they do in the cells, I don’t know. Sometimes they do punish their friends in their cells—I don’t know how they do it. They have their own court, without the officers involved.
– Officer in charge, Mumbwa Prison, October 5, 2009
Despite the instances of officer punishment described above, the majority of punishments are in fact meted out by “cell captain” inmates, to whom officers have delegated disciplinary authority, to some extent as a result of overcrowding and unwieldy inmate-to-staff ratios. By Zambian law and international standards, “[n]o prisoner shall be employed in any disciplinary capacity.”[518] The government maintains responsibility for abuses conducted by inmates with government acquiescence. In the cell, however, captains function as the ultimate authority: “Captains are the rule of law in the cell. They tell you when to stand, when to talk. They prohibit fighting or verbal abuse. They set the urination procedure, and make sure people take baths.”[519]
The prisons are currently understaffed. While all officers in charge reported that an ideal staff-to-inmate ratio would be one to five, this ratio was not achieved at any of the prisons we visited.[520] “We have 900 more inmates than we are supposed to have. The prison is six times more crowded than its original design,” said the officer in charge at Lusaka Central. Inmate cell leaders “protect” other inmates and “ensure discipline” by “serving as the officers’ eyes and ears.” He admits that “this is not a preferred correctional method,” but due to overcrowding and “an ever-rising number of inmates,”[521] he is left with little choice. “I have a staff shortage,” the officer in charge at Mumbwa informed us—“it leads to problems.”[522] Throughout the prison system as a whole, prison staffing has remained at 1,800 since 1954, and has not kept pace with corresponding increases in the prison population.[523]
Low staffing numbers have effectively led to the adoption of a parallel system of justice dispensed by inmates. A progressive “stage” system of inmate elevation is established by law, and allows prisoners to receive special privileges based on good behavior or leadership.[524] Cell captains within each cell are drawn from among the “blueband” category; “masters” in the fields are also bluebands.[525]
Officers in charge differed on the extent to which cell captains are accorded the privilege of inmate discipline. The officer in charge at Kamfinsa informed us that, while there are “not enough staff to supervise the inmates,” “inmates are not permitted to punish other inmates.”[526] The officer in charge at Choma agreed that “the cell captains have power to control fellow inmates by reporting offences such as cigarette smoking in the cells, which is forbidden. The cell captains do not have powers to discipline or punish other inmates.”[527] However, the officer in charge at Mukobeko admitted that cell captains could discipline other inmates for minor offences by instructing the offenders to clean toilets or prison surroundings.[528] The officer in charge at Mumbwa was most direct: “The captains are police in the cells—what they do in the cells, I don’t know. Sometimes they do punish their friends in their cells—I don’t know how they do it. They have their own court, without the officers involved.”[529]
Untrained, poorly supervised and invested with immense authority, cell captains wield their power arbitrarily over other inmates, resulting in prisoner exploitation and widespread abuse. As Keith, 32, described, “the cell captain maintains discipline on the inside....There is a division of labor here: in the cells, the captains are the leaders.”[530] There is a set of “unwritten rules” for which captains impose sentences in the cell.[531] Cell captains in some facilities hold night-time “courts” in their cells, with a trial in front of the other inmates,[532] where they administer “justice” in the form of beatings or other punishments. According to Chiluba, 32:
At night we also have judges and police officers in the cells. The prison officers tolerate. Cell captains, they try to beat us using heavy shoes, and tell us that “if you report, we’ll kill you in the night and tell the prison officers that you died.” The court process takes 30 minutes. They can also give cleaning punishments. Offenses include quarrelling and fighting.[533]
According to one detainee, the outcome of these court sessions is never in doubt: “People are always found guilty.”[534]
The forms of punishment administered by cell captains vary. Most common inmate-inflicted punishments include cleaning, fetching water, or sleeping in a less desirable area of the cell.[535] Inmates also routinely reported frequent corporal punishment inflicted by cell captains.[536] Though a few inmates claimed that cell captains do not beat prisoners[537] and one captain at Mwembeshi told us “we don’t punish them, we try to explain to them the importance of cleaning the cell,”[538] the vast majority of inmates reported that cell captains did administer corporal punishment. Kennedy—a remandee—reported that the cell captains use whips, belts, or electric cable to beat other inmates, usually 10-20 times.[539] Another inmate at Lusaka Central said that he had witnessed canings with a pipe meted out by cell captains, in some cases punishing attempted rape.[540] Albert, 30, reported:
In the cell, there are the voiceless and there are the privileged...Special stages would order the beating if there is sodomy inside or someone is found with drugs. They would be beaten with a hosepipe, with shoes. After I have seen inmates bleeding from the skull, who are taken to the clinic to get painkillers.[541]
Showing his scars, Martin, 39, told us: “My fellow inmates, the bluebands, they beat us hard for no reason. We cannot complain to prison officers because they do not allow us to complain. They subject us to beatings in lock up when the guards are not there. It’s dangerous to fight back, they can kill you.”[542] Another inmate at Mumbwa reported that remandees are whipped with a cane by convicts, and that he once was stoned by a captain when he asked to go to the toilet.[543] At Mumbwa, we also heard a report that one inmate tried to escape from the open farm camp and was beaten almost to death by cell captains. Rendered blind by his injuries, he was at the clinic in town.[544]
Often, such beatings are conducted at the instigation of officers, who incite cell captains to do what they cannot, as a way of subverting prohibitions on officer-inflicted corporal punishment. Moses, 24, noted, “the officers don’t beat us except [in cases of] sodomy, just the cell captains do. But they know the captains beat us, and they say, ‘that is my captain.’”[545]
International standards require that “every prisoner shall have the opportunity each week day of making requests or complaints to the director of the institution or the officer authorized to represent him” and shall be able to make requests or complaints to the inspector of prisons and central prison administration.[546] Under Zambian law, officers in charge are required to ensure that prisoners who have complaints are able to make them to the officer in charge personally.[547]
While inmates at some facilities reported that they had been able to make complaints to the commissioner of prisons about various aspects of their treatment, officer complicity in cell captain abuse means that inmates do not have immediate recourse when they are abused. One inmate at Mumbwa, with swollen hands, told us: “I was beaten by the captains for complaining too much. This was recent. I can’t complain to the officers as they will tell the captains and then I will be beaten again.”[548] Another inmate at Mumbwa reported being beaten to a prison officer, “who told us we were thieves and have to experience this torture.”[549]
Officer-sanctioned beatings by inmates are particularly virulent when inmates want to punish cases of “sodomy,” and we heard repeated testimony from both inmates and prison officers about the extremely violent attacks that result when an inmate is discovered to have engaged in sexual activity with another inmate. Indeed, said Chiluba, 32, “the whole cell can beat one for sodomy or masturbating”[550]; reported another, “we just beat them.”[551] Keith, 32, described an incident in which consensual sexual partners in the condemned section were discovered, and inmates began to beat those involved.[552] Mumba, 44, was injured at the time of the interview as a result of intervening in another such beating:
As we speak, I have a broken rib right now because we wanted to excise someone and take him to the officers. The man was from another cell—I was told he had committed sodomy. People wanted justice in their own hands. When we tried to take him to the officers, we were attacked by an angry mob. The man was rescued, and rushed into the clinic, but I was beaten....The other partner was beaten in the night. People fear if such activities happen, and want to take the law into their own hands, to make an example of someone as a deterrent. Why the fear? That is a question of every person’s mind. They think that the punishment is too lenient because they think sodomy is wrong. Also there is the HIV issue—they don’t want it to spread in prison.[553]
In some cases, prisoners expressed what they believed to be religious grounds for hostility against homosexuals. “In my religion,” Luc, 36, an immigration detainee at Lusaka Central, told us, “you have to be killed for that.”[554]
Inmate-inflicted beatings can result in serious health consequences. As Chilufya, 29, reported:
Many have need of medical treatment after a beating and one ended up dying after a beating in Chimbokaila [Lusaka Central Prison]. A cell captain came and gave him a beating and he wanted to retaliate with a hoe. After that, all the other captains came and beat him. He complained of chest pains and they kept him here for four days, then took him to the clinic which then referred him to UTH [the University Teaching Hospital]. I learnt later from one of the officers who’s a driver that he’s died.[555]
Other forms of punishment which were reported as having been inflicted by cell captains were more unusual. Peter, a teenager, reported that at Choma, captains and older inmates—at the instigation of officers—beat younger inmates when they complain about the living conditions to outsiders, and make them shout “yes sir” for hours at a time:
When we complain about the living conditions, we are beaten. The captains and older inmates beat us—slapping or punches....The officers tell the captains to beat us. After people come to visit, they call us to ask if we said the living conditions are bad. If we say yes, they beat us. They will call all five of us to ask what we were asked, and they will beat us. When people come to ask [about prison conditions] and [the interviewers] break confidentiality, the captains get to know who said what. They are paraded in the cell, interrogated, and beaten.
Some people complained to the officer in charge and it rolled back to them. We complained to the commissioner when he passed through, but later on we were beaten for that. I was given the punishment of shouting “inde-e bwana mukubwa,” [yes, sir] for four hours. The guards are the ones with the problems, not the captains. The guards come to talk to the captains, say that we are dirtying our image—we are put “on lecture” [standing on the toilet in the cell for four hours, shouting “yes, sir,” with beatings if you stop]. If you don’t shout, you are beaten. They ask you to bend, and they beat you on your upper back. We were given instructions a long time ago—when visitors come, don’t make a matter of the living conditions....There is nothing good about this place, the only good thing about this place is getting out.[556]
Other unusual punishments also exist: At Mwembeshi, Jonathan, 35, reported that “in winter, the captains will take you to the pump and pour water on you and then beat you in the cold. It is an all day torture because your clothes are cold and wet.”[557] Mangazi, 37, at Mumbwa, said that another punishment consisted of holding a water container over one’s head for two hours, and being beaten if one drops it.[558]
Inmates accused of beatings, especially in cases of suspected same-sex sexual activity, appear to be rarely punished.[559] While some officers in charge seem to fulfill their function as a complaint mechanism, by accepting confidential complaints, investigating and punishing the offender, others do not. The officer in charge at Mumbwa admitted that cell captains do beat other inmates—“it is nature when they provoke each other—that is normal.” However, she claimed that while cell captains may be demoted if they are discovered by the officers, this has happened “not a lot.”[560] The deputy officer in charge at Mumbwa informed us that captains are generally not allowed to beat inmates, but when the prison officer is far away, they can in private; captains are generally not punished.[561]
Hard Labor
At farm, I dig drains with a pick. I get very bad chest and body pains. Sometimes I come to a place where I feel I am dying.
– Aaron, 26, HIV-positive inmate, Choma Prison, October 8, 2009
Inmate and officer abuse of power were particularly evident at the prisons we visited with associated farm facilities, where inmates’ sentences to hard labor resembled a form of slave labor through a total lack of payment, beatings in the fields by the cell captains (referred to by inmates as “masters”) when an inmate was perceived to work too slowly, no water or toilet facilities, and forced labor at officers’ personal farms after completing work at the prison farm.
International standards on work require that “prison labour must not be of an afflictive [internationally causing distress] nature.”[562] International standards further specify that the “maximum daily and weekly working hours of the prisoners shall be fixed by law or by administrative regulation,” and shall leave one rest day a week and sufficient time for education and rehabilitation activities.[563] Zambian law requires that prisoners not be required to do any labor on Sundays.[564] The conditions of the hard labor at farm prisons are detrimental to prisoners’ health and do not meet Zambian and international law and standards.
Prisoners routinely work every day of the week.[565] The officer in charge at Mumbwa confirmed that inmates work eight hours a day, seven days a week.[566] Noah, 32, at Mumbwa described the conditions of such work:
It is a marathon—you are not supposed to stop and stretch. If they see you do that, you are in trouble. You cannot drink water unless it’s time, even if you are very thirsty. The ground is hard and hard to dig. If you take a break, the captains will shout at you. They want to force you to do work, and only at designated times can you rest. Otherwise, they are always on you. At times, some of the captains may shout and yell at you—others may go to the extent to whip you. They tell us, “you criminal, a criminal is not supposed to get tired—continue working.”[567]
Chibesa, 27, at Mwembeshi, described similar hard labor conditions:
We work all day without food. That is why people run away. Recently five tried to escape. There is no opportunity to take a bath after the work day. Sometimes we bathe only two times a week. When you are working in the fields and all hot and dusty and you ask for a drink of water, the officer tells the captain to beat you. This happens repeatedly. Two weeks ago, someone’s feet started swelling and they said he was lying. They took him to the hospital and after two days he died. We are suffering. Even on Sunday they still have to work. They only let us stop for the visiting hour—they let us clean up and our family thinks everything is ok. But we are suffering.[568]
While PRISCCA, ARASA, and Human Rights Watch did not visit a farm prison where women were engaged in hard labor, we heard from a former inmate at Mukobeko that female prisoners incarcerated there face many of the same challenges as men engaged in hard labor: Female prisoners facing hard labor are treated “like slaves” by the officer in charge, being made to clean her house and wash her clothes; and prisoners are forced to work every day, often at the officer in charge’s farm, without ever eating any of the produce that they have “sweated for.”[569]
The complete unavailability of water for inmates doing hard labor in the hot sun all day is an especially serious health concern: The officer in charge at Mwembeshi admitted “we ration water,” but also claimed that “the captains go and draw water for the inmates when they need it from the water pipe.”[570] Repeatedly from inmates, we heard that water was not provided. Reported one, “when we are out in the fields, there are some boreholes, but the captains refuse to fetch water for the prisoners.”[571] “We are not given a chance to drink water unless the officer is kind and you can beg them. Often we work eight straight hours without water,” said Mwelwa, at Choma.[572] An inmate at Mwembeshi reported that: “The only water is put at the end of the field and we can only drink if we finish our work. But then they move it again so by the time you get to the end, it has been moved. One guy fainted last week due to heat and lack of water.[573]
Hard labor poses particular health problems for some HIV-positive prisoners. While by Zambian law, medical officers are ordered—where practicable—to examine every prisoner before the prisoner is made to do work,[574] some HIV-positive inmates are still made to work in the fields despite a weakened health condition.[575] At Mumbwa, Semba, 34—a remandee—reported: “Everyone must work, even those that are sick. The labor may consist of breaking stones for three to four hours a day. There is no payment. Both remandees and convicts must work.”[576]
Inmates serving sentences for hard labor are also taken outside the prison to work at individuals’ farms. Furthermore, inmates at Mumbwa and Mwembeshi repeatedly reported having to work at some of the prison officers’ personal fields:
If there is no urgent work Monday through Saturday or even Sunday, the prison officers take us to their own fields. In the rainy season, we knock off at 13 hours—and in the afternoon, we have to go to work in the officers’ fields, they divide the numbers. The officer in charge is not aware of some of these things. He is a new officer in charge, and seems to be a very good man. But the officers use their hands to beat us.[577]
While the officer in charge at Mwembeshi reported that inmates do not work on Sundays, or on holidays,[578] inmates claim that working (without pay) in the officers’ fields in the afternoons or on Sundays is routine: “In the officers’ fields, you do the same work you normally do. We go normally every day. The officers go with you, say it is time for ‘wenga wenga’—it means after you have finished the work of the government, you have to go for the officers’ work.”[579]
Under Zambian law, prisoners are to be paid their accumulated earnings upon release[580] and are eligible for payment when the commissioner authorizes the introduction of an earnings scheme in any prison.[581] However, the schedule of payment for prisoners under such an earning scheme in Zambian law is between one kwacha (US$0.0002) a day and three kwacha ($0.0006) a day.[582] These derisive sums mean that inmates never receive payment for their work. Frederick Chilukutu, the deputy commissioner of prisons informed us that with a one kwacha per day requirement, “if you get it now, what can you use it for? It’s nothing.” Therefore, he explained, since paying prisoners one kwacha per day became “irrational,” the Prisons Service has halted payment entirely, a situation which the he admits needs to be reviewed in order to better provide released inmates with money to sustain and establish themselves outside of prison.[583] Currently, no prisoner ever receives money for work when they leave.[584] Forcing inmates to work in effect without pay is a form of forced labor that violates international norms.
Compounding the already dangerous environment of the farm prisons, in the fields, inmate “masters” are given a free hand to brutally abuse their fellow inmates. From inmates at these prisons, researchers repeatedly heard the same story: “the captain will beat people if they fall behind” while the officers look on and even tell them to do the beating.[585] Indeed, “it’s a regular, daily event that we are beaten.”[586] From the beginning of the day, when the captains call out for labor, walking through the group with whips,[587] to the fields—when inmates fashion whips out of tree branches—beating is routine. Kaila, 20, reported that at the Mumbwa open farm prison a master beat him “all the time...for no reason” with the officers watching. “It’s just cruelty,” he concluded. Attempts to complain to the officer in charge had not had lasting effect.[588]
These beatings were confirmed by the masters themselves,[589] one of whom reported that “the officers don’t let you beat too much” but went on to admit that he “would beat the inmates badly sometimes”[590] and that “we are permitted to beat people in the fields.”[591] While one captain posited that brutality had improved due to human rights education, he admitted that other captains wanted to “run the prison in the old way, as they did 10 years ago when beating was happening here, there, everywhere.”[592] Festus, 35, an inmate at Mwembeshi, remarked, “I was chosen to supervise but refused because I feel pity.”[593]
Officers are routinely complicit in this abuse, and in fact sometimes order it.[594] Despite the fact that the officer in charge at Mwembeshi had told the captains not to beat their fellow inmates, an inmate reported that “the officer will force the captain to beat [inmates in the fields] if they are too tired to move.”[595] Jacob, 26, another inmate at Mwembeshi, reported:
The officers see—they are the ones who instruct the masters. They say “tunga nyeleti.” That means—how can I say it?—“push the needle.” It means you have to be beaten, that it’s time for a beating now. The masters beat us because they are instructed.[596]
Even when officers don’t explicitly order the beating in the field, captains abusing their fellow inmates are not decisively punished.[597] While complaints to a well intentioned officer in charge do sometimes result in disciplinary measures against captains who have been their fellow inmates,[598] after complaints, “there are retaliations in the field” by the captains.[599]
Criminal Justice System and Its Impact on Prison Health
In 2007, the UN Human Rights Committee noted that “[t]o the extent that the State party [Zambia] is unable to meet the needs of detainees, it should immediately take action to reduce the prison population.”[600] Prisoner overcrowding—and the health consequences of that overcrowding—are inextricably linked to failings in the criminal justice system which engage the responsibility of the Zambian judiciary, police, immigration, and prisons authorities. Interviews with inmates, prison officials and NGOs found such problems as police investigation failures, lack of bail, and lack of representation for accused persons keep individuals unnecessarily, and often unlawfully, incarcerated for extended periods of pre-trial detention. For prisoners who have been tried, failures of the justice system such as lack of alternative non-custodial sentences, and delays in the appeals process, continue to contribute to the overcrowding.
Extended and Arbitrary Pretrial Detention
Justice delayed is justice denied. It is better even to be found guilty. When you come out, you’ve spent 10 years in prison. Remandees are kept here a long time. I have [been detained] four years now, but my case is not disposed of. There is no justice.
– Rodgers, 42, Lusaka Central Prison, October 3, 2009
Delays and failures within the Zambian criminal justice system lead to unnecessary arrests and detainees being held for long periods of time on remand prior to appearance before a judge and prior to trial, contrary to international and Zambian law. This can have disastrous results for the individuals’ health and lives. The incarceration of pre-trial detainees is clearly a major contributing factor in the prisons’ extreme overcrowding, as remandees are held with convicts in violation of international law. On the day PRISCCA, ARASA, and Human Rights Watch visited Lusaka Central Prison, of the 1145 inmates, 601—more than half—were there on remand.[601] Overall, 35 percent of the Zambian prison population is composed of remand prisoners.[602]
International and regional law provide for the individual right to liberty and prohibit arbitrary arrest and detention.[603] Yet prisoner testimony indicates that problems in police investigation result in many unnecessary and wrongful arrests. According to inmates, police arrest and hold alleged co-conspirators or family members when their primary targets cannot be found. Such detentions, irrespective of provisions in Zambian law permitting them, are arbitrary and unlawful under international law. Catherine, 38, a Lusaka Central inmate, recounted, “the police officers and DEC [Drug Enforcement Commission] officers come here, they bring people here who are innocent. They will pick up a whole family and bring them here.”[604] Angela, 23, also at Lusaka Central, concluded: “The reason the prisons are congested is that they arrest entire families when they just are looking for one person. They will arrest six at a time, even old ladies who can’t walk.”[605] Police officials noted to PRISCCA, ARASA, and Human Rights Watch the need for professional education and sensitization so that officers “don’t go beyond their role” and so that, in the future, “if they detain unlawfully, the person is released.”[606] Such wholesale arrests may, in some cases, even be sanctioned by law, as the Zambian police[607] and drug enforcement officials have expansive powers to detain and arrest.[608] They still, however, violate Zambia’s international human rights obligations with respect to the right to liberty.
Upon arrest, international, regional, and Zambian law provide for the right to be brought before a judge, and to be charged or released.[609] Ninety-seven percent of the prisoners PRISCCA, ARASA, and Human Rights Watch interviewed had not seen a magistrate or judge within 24 hours of arrest, even though such review is required under Zambian law.[610] Indeed, far from seeing a magistrate or judge within the first 24 hours after arrest, the prisoners we interviewed had in many cases been detained for months without ever having seen a magistrate or judge to review their detention. On average, male detainees we interviewed in all six prisons spent four months in detention prior to seeing a judge or magistrate for the first time; female detainees spent one month. Yet survey data established that the average length of time at some prisons was even longer: At Kamfinsa, male detainees averaged nine months between arrest and first appearance before a judge; at Mukobeko Maximum Security, male detainees had averaged five months. Additionally, we spoke with inmates whose first appearance before a magistrate or judge was one year and one month after arrest,[611] one year and two months after arrest,[612] two years after arrest,[613] and three years and seven months after arrest.[614]
Table 11: Appearance before a Judge
International law requires that “[p]re-trial detention should be an exception and as short as possible.”[615] The UN Human Rights Committee has made clear that detention before trial should be used only to the extent that it is lawful, reasonable, and necessary. Necessity is defined narrowly: “to prevent flight, interference with evidence or the recurrence of crime” or “where the person concerned constitutes a clear and serious threat to society which cannot be contained in any other manner.”[616] International standards provide that except in special cases, a person detained on a criminal charge shall be entitled to release pending trial subject to certain conditions.[617]
Yet for individuals awaiting trial in Zambia, there is insufficient use of noncustodial pretrial alternatives. Among the prisoners we interviewed, 95 percent of juveniles, 88 percent of adult males, and 75 percent of adult females were continuously detained from arrest (not having been released on police bond or bail).
Table 12: Continuous Detention
|
Inmates frequently reported that they were unaware of the right to request bail.[618] Bail is explicitly prohibited for numerous offenses including treason, murder, aggravated robbery, and narcotics violations.[619] Judges also use their discretion to deny bail, saying “bail is not a right, but a privilege.”[620] When bail was an option, inmates frequently reported that they had not been able to obtain bail.[621] In 2008, the Human Rights Commission of Zambia concluded that “there are incidences of individuals in remand for offences for which bail could have duly been granted either because of their socio-economic circumstances or lack of knowledge that they can apply for bail.”[622]
Following their initial appearance in front of a magistrate or judge, prisoners may then in practice be held for years before they face trial. Under international and Zambian law, those charged with a criminal offense are to be tried “without undue delay.”[623] Yet “the long stay of prisoners without trial,” lamented Chishala, 38, “is unbearable.”[624] Researchers spoke with convicted prisoners who—between arrest and conviction—had been held on remand for six years,[625] and one who had been held 10 full years between arrest and conviction.[626] PRISCCA, ARASA, and Human Rights Watch also spoke with current remandees who, still awaiting judgment, had been held for up to five years seven months.[627] Among the prisoners we interviewed, the median time since being detained for current remandees was a staggering 36 months (three years) for adult males, with a minimum of one month and a maximum of 67 months (five years, seven months). For juveniles, the median was five months, with a range from eight to a high of 43 months (three years, seven months); for adult females the median was one month, with a range from zero to 28 months (two years, four months).
Table 13: Median Time in Detention for Remandees
Remandee Prisoner Category |
Time in Detention (months) Reported by Remandees (median (range)) |
Adults (19 years and older) (n=27) |
10 (0-67) |
Males (n=16) |
36 (1-67) |
Females (n=11) |
1 (0-28) |
| |
Juveniles (8-18 years) (n=14) |
5 (0-43) |
| |
All Remandees (n=41) |
7 (0-67) |
International standards mandate that persons who are charged with a criminal offense be informed of their right to have access to a lawyer.[628] Zambian law provides that individuals sent for trial before the High Court whom the court considers have insufficient means to engage a lawyer, shall be granted legal aid,[629] and individuals in subordinate courts may apply for legal aid.[630] Researchers found, however, that inmates had low levels of knowledge of their right to a lawyer and low levels of representation. Indeed, 60 percent of adult male prisoners and over 70 percent of adult female and juvenile prisoners reported no legal representation whatsoever. Even children appearing before the High Court were rarely represented by counsel. Erick, a teenager, reported:
I had no representation, I stood on my own behalf. It was my first time in a police station or in court. I was just speaking, and I was scared. So I didn’t know what I was saying.... As young people, it is very threatening to see the inside of the court. Even if you are not guilty, you end up pleading guilty.[631]
There is little by way of legal aid capacity, which means only a few defendants benefit from legal assistance, and that assistance may be of poor quality.[632] As the Legal Resources Foundation observed, “the state legal aid is supposed to be providing legal services, but they are not widespread. They are appointed in capital cases and juveniles, but they should be in all criminal cases. The lawyers also do a bad job: they say, ‘just plead guilty.’”[633]
Table 14: Legal Representation
Lack of legal counsel can lead directly to unnecessary incarceration. Anderson, 35, an inmate at Choma, reported that he did not intend to plead guilty, but the magistrate decided he should plead guilty and “checked it on the form”.[634] In another case, an inmate explained:
The victim was willing to forgive me, but friends and family members told me to admit guilt. I had never been in court before, I had no idea how it proceeds.... I plead guilty and was sentenced to one year.[635]
Judicial delays in case transfers between the subordinate and the High Court, turnover between judges (which leads to a trial being restarted), inefficiency among the prosecution service, and sporadic lack of fuel for court transport all conspire to lengthen pre-trial detention. Frequent adjournments delay trials, despite legal provision that in the cases of individuals held in prison, no adjournment shall be for “more than fifteen clear days.”[636] Detainees reported that often when they go to court, the sessions don’t take place, because the court is waiting for the prosecution to proceed,[637] the lawyer or judge is not there,[638] or because witnesses are not present. One inmate reported that he had been appearing in court every three months for two years waiting for a police officer to testify against him, but that the police officer had never shown up.[639] And, sometimes, inmates are unable to go to court because of a lack of fuel or transport from the prison to court.[640] Thus, for myriad reasons, inmates’ cases are frequently not advanced, leaving them bewildered. Banda, age 17, said: “I am here on remand; I came on July 23, 2007. I am done with my trial, just waiting for judgment....The trial didn’t take too long, it is only the judgment that has taken long. It’s been a year and four months since my trial ended. I’ve been back to court four times just for the judgment but it never comes.”[641]
Table 15: Immigration Detainees’ Access to Justice
Prisoner Category |
Prisoners Who Reported Seeing a Judge Since Being Detained (%) |
Immigration Detainees |
38 |
Non-Immigration Detainee Prisoners |
97 |
Immigration detaineesare frequently detained and await deportation without due process, mingled with convicted and remandee prisoners. Zambian immigration law provides that suspected immigration detainees may be detained for up to 14 days while inquires are made.[642] Immigration service officials informed us that detention is the last resort, but that a docket is prepared and put on file with the court if the case involves someone whom they believe intentionally overstayed their visa.[643] Delays may occur in bringing the detainee before the court if the immigration detainee “doesn’t tell the truth...if people are lying, that is the major source of delays, as the process of verification will take long.”[644] Yet, Hope, 23, an immigration detainee at Lusaka Central, told us “immigration just leaves people here. Some in our group have been here six months without going to court, they don’t take you if you don’t speak the language.”[645] Susan, 36, at Lusaka Central, informed us that “one lady from Rwanda, brought here, has been here for four months has never been to court, just staying here....Immigration brings them and dumps them here.”[646] Among prisoners we interviewed, only 38 percent of immigration detainees had ever seen a magistrate or judge, compared with 97 percent of non-immigration detainees.
Many who were indefinitely detained appeared to have reasonable claims to legal status. Among the immigration detainees we interviewed, we spoke to some who claimed to be Zambian citizens and non-citizens with valid visas, but had been unable to challenge their designation as “prohibited immigrants” in court.[647] One 18 year-old immigration detainee, whose mother is Zambian and father Senegalese, but was raised in the Congo, showed immigration officials his birth certificate when they arrested him, but was told, “‘You don’t speak Bemba, you don’t speak English, you are not Zambian.” He never received a charge document or had the opportunity to see a magistrate or judge to contest his detention.[648] Benjamin, 31, born in Zambia but raised in the Congo by his grandmother, never had a birth certificate: “I thought it was ok because I was born in Zambia and my father is a Zambian.”[649] Laurent, a Congolese detainee who reported he had been in possession of a valid visa when detained, reported:
I entered Zambia on September 29. I had a visa, I was given 26 days. I reached Kitwe and was going to the marketplace when a group arrested me. They said, “give us your passport.” I refused and was taken to the immigration office to be interviewed. I paid 2,000 [Zambian kwacha, US$0.42] in immigration custody. I demanded to know why I was arrested and they said, “We took you in for being arrogant.” It was a completely illegal arrest, but I am just waiting here for anything to happen because my passport and visa are at the immigration office.[650]
Alfred, 55, who reported already holding refugee status in Zambia, told a similar story:
I’m a refugee in Solwezi Maheba Refugee Camp.... I was arrested because I left the camp with no exit permit. And my children are still there at the camp....I left the camp to visit my brother who was sick with TB. He wasn’t here as a refugee, he was paying a visit. I was in a hurry, it was an emergency situation, he was almost dead, so I didn’t ask about what papers I needed to leave the camp; I just left. I have been here for eight months. I have had no contact with my family, UNHCR, or anyone else, and no visits. I have tried to write letters but they rip them up and don’t send them. They are asking me for one million eight hundred kwacha [$380] to go back to DRC.[651]
Immigration detainees are told to pay for their own deportation and are held until they pay.[652] Jean Marie, 28, detained at Lusaka Central, reported “I’ve been waiting to be deported to DRC. I even offered to pay; I told the officers to call immigration and arrange it but they haven’t. I’m ready to pay; I have money in reception. My biggest problem is that they don’t help us. Some [immigration detainees] have been here for two years waiting.”[653] A Liberian detainee, whose wife and child were Zambian citizens but who hadn’t applied for legal status, lamented “immigration came and told me I had to pay my own transport, and if I don’t I have to stay here maybe five or six years. I don’t have the money to deport myself and the government says they don’t have the money to deport me. I don’t want to leave my family, but in Liberia it would be better than prison.[654] Immigration officials confirmed that “under normal circumstances, we don’t ask for money to deport, but we do when we don’t have the money ourselves...at times it may happen frequently that the budget for deporting runs out.”[655]
We also spoke with immigration detainees who felt unable to return to their country of origin and yet had not had the opportunity to request asylum. A Somalian detainee reported “I left Somalia on March 1, 2009.... When they caught me I told the [immigration officials] that I want a refugee camp, but no one helped me. UNHCR came once to [the prison]; they wrote down my name but nothing happened.[656] A Rwandan detainee who had been an opposition journalist told us, “I am despairing because I see no way out of prison but can’t return home. I’m looking at spending the rest of my life in prison.”[657] Immigration officials, by contrast, claimed that all immigration detainees have an opportunity to claim asylum, but sometimes fail to do so at the appropriate time.[658]
Unnecessary and extended detention for immigration detainees or remandees may have significant financial costs both for the government and for the individual, in addition to the personal toll that such detention may take. Families in developing countries frequently face financial hardship when an income-producing member is detained, particularly when the period of detention is long, and detainees are unable to earn income, provide food for themselves and their families, and pay taxes.[659] Even given Zambia’s grossly inadequate prison conditions, the current cost to the government of incarcerating immigration and remand detainees unnecessarily for extended periods is not insignificant, and savings could likely be generated by increasing the use of bail instead of pre-trial detention. Furthermore, state money expended on holding pre-trial or immigration detainees unnecessarily represents “a stark opportunity cost,” for the government, as “[e]very bit of state revenue spent on incarceration results in potentially less money for crucial social services, health, housing, and education.”[660]
Non-Custodial Sentences and Parole
The unavailability of non-custodial sentences also contributes to prison overcrowding. Zambian penal law provides for a range of punishments—among which imprisonment is only one option[661]—including the sentence of community service.[662] However, the 2000 law providing for non-custodial sentences has had minimal impact because of the lack of personnel to supervise those on community service orders.[663] Community service orders were placed under the authority of the Prisons Service, but with no additional resources or staff to implement these orders.[664]
The lack of options to complete custodial sentences in the community also exacerbates prison overcrowding. Parole has only recently become practically available. While parole has been “on the books since the inception of the nation, it has been dormant until relatively recently.”[665] The parole system, however, is burdened by the irrational fact that only inmates with longer sentences—those who have been found guilty of more serious crimes—are eligible for parole, whereas inmates with more minor sentences are ineligible. The legal requirement was originally a four-year sentence; in 2001, the deputy commissioner of prisons reported, the Prisons Service took the initiative to lobby for the law to be amended so that those incarcerated for two years and more are eligible for parole. In 2008, parole board members were appointed and prisoners were paroled in 2009[666] and 2010. Yet the number of inmates paroled is low, in some cases because of a lack of resources for follow-up. According to the officer in charge at Mwembeshi:
We submitted a number of names of eligible inmates but only one was chosen. The problem is that offender management can’t do follow up on the parolees because she lacks a motorbike.[667]
Considering the irrationality of the certain sentence limits on parole, to be truly meaningful, the deputy commissioner of prisons reported that the requirement of two or more years needs to be eliminated, so that the only restriction on the availability for parole would be those who are sentenced to death.[668]
Appeals System
Under international law, everyone convicted of a crime has the right to have his conviction and sentence reviewed by a higher tribunal according to law.[669] Yet in Zambia, the appeal process suffers from serious delays, which also results in the unnecessary detention of some inmates. Delays in appeals, as in pre-trial and trial proceedings, can go on for years. One inmate had been informed that his appeal papers had been lost.[670] Howard, 29, an inmate at Mukobeko, told us he had been waiting for eight years for his appeal to be heard—when it comes to the appeals, he said, “We are just hopeless.”[671] Chishala, 38, reported “I have been waiting six years since I put in my appeal, and I have heard nothing in that time.”[672] Paul, 33, a condemned prisoner at Mukobeko, noted that:
My appeal has taken since 2005. I can no longer afford a lawyer to move it through the system. We are 235 in the condemned section. Only 40 have had their appeals heard. 180 are still waiting, some for over 10 years.[673]
Emmanuel, 35, confirmed that people wait over 10 years. Having waited four years already without resolution of his appeal, “I’m doomed,” he concluded.[674]
Conclusion
According to international law, the penitentiary system shall treat prisons with the essential aim of reformation and social rehabilitation.[675] International standards encourage, prior to prisoner release, prisons to take steps to reintegrate the prisoner into society.[676] Yet Zambia currently makes little, if any, provision for reintegration of prisoners, an omission to which inmates attributed a significant recidivism rate. One prisoner at Mwembeshi reported that “there is no planning with us for release. For inmates, when we finish our sentence we face stigma in the community....I used to see it when I was outside—and I am afraid it could happen to me. When we go outside, we don’t have anything to do.”[677] Another at Mumbwa reported, “there are no re-entry services. People are poor when they get out, so they come right back.”[678] One former prisoner reported being “destroyed” when he came out of prison, financially and personally.[679] “When you come out of prison, you are looked at as an outcast, not as a human being,” said another.[680]
The officer in charge at Mwembeshi reported:
We need real rehabilitation. Many of the inmates here are not criminally minded. Many crimes are circumstantial. People commit offenses because they want to make a living. They need economic empowerment. If one shows an interest in farming, we should help with capital so they have a chance at a new life.[681]
The offender management officer at Mwembeshi concurred: “On discharge people have nothing. We don’t have the resources to bring them to their homes and they are stigmatized upon re-entry, causing recidivism.”[682]
Keeping in mind that, typically, all but a small percentage of prisoners return to the community,[683] and that the prison community is inextricably linked to the general population,[684] Zambian prisons need to improve conditions in the prisons and measures to reintegrate their inmates into the general population post-release, as not simply a matter of prisoner health, but a matter of public health.
Improving the conditions in Zambia’s prisons will require significant changes on the part of the Zambia Prisons Service, and will also require the coordinated efforts of actors throughout the Zambian government, civil society, and international agency and donor communities. In addressing general prison conditions, the Zambia Prisons Service will be unable to effect necessary change without improved support from Parliament and the international donor community. To improve the delivery of medical services to prisoners, NGOs, international agencies and donors, and Zambian Parliament will also play a role in improving the availability and accessibility of services. To reduce the drastic overcrowding that now plagues the prisons, the Zambian judiciary, Parliament, police, and immigration officials will be indispensable in ensuring necessary changes to the law, implementation of non-custodial alternatives, and increased efficiency of the judicial process. Clearly, resource constraints are a major consideration, but greater priority on prison funding needs to be put at the national level and greater support from international donors needs to be forthcoming if change is to be effected. Some reforms—particularly the proposed legal reforms—are resource-neutral; those that aren’t are crucial to the realization of the rights of prisoners and are the responsibility of both the national government and international donors.
Recommendations
To the Zambia Prisons Service and Ministry of Home Affairs
- Increase the use of parole, including a priority for ill detainees and pregnant and lactating detainees
- Reform prisoner disciplinary systems by:
- Suspending all use of penal block cells, which currently violate the prohibition on inhuman treatment
- Immediately discontinuing the practice of stripping inmates naked and holding them in water while in penal block confinement
- Consistently punishing officers using corporal or other inappropriate punishments
- Immediately discontinuing a reliance on separate cell captain justice systems, so that only prison officers decide on or inflict punishment, in accordance with the Prison Act and Prison Rules
- Consistently punishing cell captains judged to have inflicted punishment on their fellow inmates, with aggravated punishments for instances of cell captain-inflicted corporal punishment
- Providing prison officers with additional training in appropriate discipline methods and the inappropriateness of corporal punishment, with prison officer-guided education sessions for all inmates on prison rules and disciplinary methods and punishments
- Ensuring detainees are able to send confidential complaints to state bodies and other organizations, and that all prison officials are aware of this right and do not interfere with it
- Investigate all complaints of sexual assault of inmates by other inmates or officers, and take appropriate action against those found responsible
- Investigate all complaints of physical, verbal, and sexual assault and abuse, by inmates and officers, against inmates suspected or charged with same-sex sexual conduct, whether in custody or prior to incarceration, and take appropriate action against those found responsible
- Establish clear guidelines on the provision
of prison-based health services, and scale up these services to:
- Immediately establish the presence of a clinical officer at each prison, who at the morning line-up can judge prisoner health complaints and facilitate access to outside Ministry of Health medical facilities, eliminating the use of cell captains and non-medical prison officers from doing triage and deciding which prisoners are entitled to evaluation and treatment
- Address TB by:
- Providing TB screening to all inmates entering the prison, and all existing inmates through targeted surveys, sputum analysis, and, if needed, chest x-ray evaluation
- Ensuring prompt initiation on treatment for those with confirmed disease
- Conducting a TB prevalence study to understand the true extent of the disease in the prisons
- Establishing capacity for TB testing and treatment at each prison clinic
- Educating prison officers and cell captains in TB symptoms and the necessity of referral for testing upon the appearance of symptoms
- Further educating prison medical officers in the co-management of HIV and TB
- Establishing clear guidelines and protocols for moving patients into and out of TB isolation, with regular checks to ensure that isolation is appropriate
- Establishing guidelines on preventing officer exposure to TB
- Improving immediately the ventilation, sunlight, and cleaning of TB isolation cells in line with international standards
- Prioritizing placing prisoners who are HIV-positive and TST-positive on continuous Isoniazid Preventive Therapy (IPT) for prevention of active TB as IPT becomes available, given the higher risk of TB in the prison population
- As testing and treatment for drug resistance become available in the general population, ensuring full prisoner inclusion in testing and treatment programs
- Address HIV by:
- Offering voluntary HIV counseling and testing to all inmates entering prison and all existing inmates
- Ensuring prompt initiation on treatment for inmates with confirmed disease
- Establishing HIV voluntary counseling and testing and anti-retroviral therapy treatment and monitoring facilities at each prison
- Implementing a system for HIV voluntary counseling and testing for pregnant inmates as part of a comprehensive system of prenatal care, offering PMTCT where appropriate
- Providing condoms and water-based lubricant to all prisoners and prison officers
- Providing HIV prevention, treatment, and care education, including information and sensitization on harm reduction and safer-sex practices in the context of same-sex sexual conduct at each prison to increase condom acceptance
- Systemic improvement:
- Recruiting new prison officers to ensure adequate staffing in all facilities, including security and healthcare staff
- Conduct health screening of all prisoners upon entry and at regular intervals
- Establish clinics at each prison with at minimum a clinical officer on staff, with a consistent supply of essential medications and a minimum capacity to conduct TB testing and treatment and HIV voluntary counseling and testing and anti-retroviral therapy treatment and monitoring
- Accept prison responsibility for remandee and convict custody equally, escort remandees outside prison grounds for medical care on terms equal to convicts
- Improve prenatal care and institute the provision of breast cancer screening and regular pap smears
- Establish a comprehensive monitoring and evaluation system that records prison illness and deaths
- Increase the use of mobile health services to rural prisons and improve transport from rural prisons to health facilities to improve healthcare availability
- Create a system for continuity of care for inmates upon discharge to include a summary of the inmate’s medical record and a temporary supply of TB or HIV medication where necessary
- Develop more comprehensive links and formalized protocols with Ministry of Health clinics that now provide most care to Zambian prisoners.
- Ensure that conditions of confinement meet
international standards, including by taking immediate action to improve basic
prison conditions by:
- Renovating prison facilities, to provide every detainee with a bed of his or her own, and adequate space, light, and ventilation
- Ensuring strict separation of children from adults; males from females; convicted from unconvicted detainees; and immigration detainees from criminal detainees
- Providing food, at a minimum as established by the dietary scale in the Prisons Rules, including separate rations for children living with their mothers, and additional rations for prisoners with HIV, TB, and other health conditions requiring nutritional supplements
- Ensuring adequate supply of clean water, in particular at regular intervals for prisoners engaged in hard labor in the fields
- Constructing a sufficient number of sanitary toilet facilities for the current number of inmates, inside and outside of cells
- Providing prisoners with basic necessities including adequate clothing/uniforms, blankets and mattresses, mosquito nets, soap, and razors, as well as gloves, disinfectant, rodent and insect extermination materials, and other equipment for safely completing their cleaning duties
- Limiting the number of hours worked by inmates under sentence of hard labor
- Ending the practice of inmates working at officer farms and implementing prisoners’ right not to work on Sundays
- Providing inmates with meaningful compensation for prison work upon release
- Protecting officers and prisoners from infectious disease by creating facilities for hand-washing
- Increase the Prisons Service’s focus on prisoner rehabilitation and reintegration through increasing the availability of education programs in prison and improved reentry planning
To the Zambian Parliament
- Amend the Penal Code, Criminal Procedure
Code, and Narcotic Drugs and Psychotropic Substances Act to:
- Repeal or amend Sections 155, 156, and 158 of the Penal Code in order to decriminalize consensual sexual conduct among adults, and implement gender-neutral laws to protect both adults and children from sexual violence and assault
- Raise the minimum age of criminal responsibility from eight to an age in line with international standards. In line with the Committee on the Rights of the Child, Human Rights Watch recommends an age of at least 14 years, with 12 years as the absolute minimum
- Limit police and Drug Enforcement Commission powers to carry out sweeping, group arrests which violate international law
- Amend the Prisons Act and Prisons Rules to:
- Eliminate the exclusion of prisoners with sentences under two years from the parole program
- Revise the guidelines on pay for prisoner work to bring them in line with inflation and make compensation meaningful
- Amend the Immigration Act to:
- Require that any administrative detention for the purposes of deportation be shown on a case-by-case basis to be proportionate and necessary
- Allow that immigrants who are ordered deported by a court be given a time frame to depart the country that does not presume or require their detention
- Include specific limits on the duration of administrative detention for the purposes of deportation
- Secure enough funding for the budget for
Zambian prisons, so that there are enough resources to ensure conditions
consistent with international standards. Funding should be sought for:
- Facility renovation
- Upgrading of water and sanitation facilities to ensure the availability of clean water and sanitary and adequate toilet facilities at all prisons
- Food and cooking facilities, so that food provision meets national and international standards
- The provision of basic necessities to prisoners, including soap and adequate clothing
- The Parole Board
- Take the necessary steps to ensure that the existing legal provision for non-custodial sentences can be invoked, including by identifying an authority responsible to the Prisons Service who would oversee its implementation
To the President of Zambia
- Issue a public statement identifying prison conditions and health as a national crisis and establish a high-level inter-ministerial task force to urgently develop a national prison health plan
- Establish an inter-ministerial commission to increase collaboration, coordination, and cooperation among the prison, police, judiciary, and immigration authorities on reducing prison overcrowding, including the identification of steps necessary to achieve reduction of overcrowding and a timetable for implementation
- Publicly oppose the criminalization of consensual sexual activity, including same-sex sexual activity, and encourage the provision and use of HIV prevention methods including condoms in prisons
To the Zambian Judiciary and Ministry of Justice
- Issue guidelines for bail administration to encourage granting of bail and easing of surety requirements, considering accurate information about household incomes in Zambia
- Ensure that all magistrates and judges know and advise defendants on their rights—particularly bail and representation rights—when they are brought before them to be charged
- Speed proceedings by:
- Streamlining the process of case transfer from subordinate to High Court
- Providing for judicial cooperation so that retirement, absence, or death of a judge does not necessitate the recommencement of a trial
- Strictly limiting adjournments
- Abiding by all statutory requirements for when defendants need to be seen in court
- Ensure all detainees, including those under 18, have access to a lawyer of their choice
- Ensure defendants who do not have legal representation are provided with adequate assistance to ensure that pleadings are completely understood, witnesses are adequately questioned, and the accused understands his rights and options
- Review the position of all offenders currently in pre-trial detention, with a view to releasing them on bail, and ensure effective non-custodial alternatives for defendants awaiting trial
- Ensure that pre-trial detention is for as short a period as possible and subject to regular review
- Ensure that children are subject to pre-trial detention only as a last resort
To the Zambia Police Service and Drug Enforcement Commission
- Cease all arbitrary arrests including the practice of detaining family members and witnesses when the primary investigation target cannot be found
To the Zambia Ministry of Home Affairs/ Immigration Department
- Ensure that each detainee receives a hearing in a timely manner
- Ensure each detainee’s ability to request asylum
- Reform the system for payment of deportation costs
- Minimize the use of detention for immigration offenses
To the Zambia Ministry of Health
- Develop a detailed plan for the improvement of prison health services and conditions in its National Health Plan 2011-2015
To the Zambia National Human Rights Commission
- Investigate and publish reports on violations of the rights of individuals on the grounds of real and perceived sexual orientation and gender identity and expression in Zambia, raising awareness of both legal and extra-legal forms of violence and discrimination
- Continue existing prison and police cell monitoring, reporting, and advocacy
To international agencies, donors, and NGOs
- In the short term, ensure the direct
delivery of health service provision initiatives in prisons including:
- TB testing and treatment programs
- HIV testing and treatment programs
- Women and children’s health
- Nutrition support programs
- In the long term, support the scaling up of the prison medical directorate to provide each of the services detailed above
- Provide technical and financial support for
legal reform programs to improve coordination among police, immigration, drug
enforcement, judiciary, and prison officials including:
- Decreasing the length and use of pre-trial detention
- Implementing non-custodial sentencing alternatives
- Integrate discussion of prison health into existing technical advisory committees on health to the Zambian government
- Provide financial support for scaling up legal assistance programs for prisoners, in order to speed progression of cases through the judicial system
- Develop community reintegration programs, halfway houses, and microfinance initiatives to assist prisoners with reentry and decrease the risk of recidivism
- Ensure regular visits by UNHCR to prisons to ensure that refugees are not held in prisons and that detainees have an opportunity to claim asylum
Acknowledgements
This report was written by Katherine Wiltenburg Todrys, Bernstein fellow in the Health and Human Rights division at Human Rights Watch, based on research by the author and Megan McLemore, researcher, Rebecca Shaeffer, Kroll Family fellow, and Darin Portnoy, consultant, in the Health and Human Rights division at Human Rights Watch; Nyaradzo Chari-Imbayago, advocacy coordinator at ARASA; and Chris Mumba, treatment literacy officer at the Treatment Advocacy and Literacy Campaign.
The report was edited by Joseph Amon, director of the Health and Human Rights Division at Human Rights Watch. It was reviewed by Megan McLemore; Rebecca Schleifer, advocacy director of the Health and Human Rights Division at Human Rights Watch; Janet Walsh, deputy director of the Women’s Rights Division at Human Rights Watch; Bill Frelick, director of the Refugee Policy Program at Human Rights Watch; Rona Peligal, deputy director of the Africa Division at Human Rights Watch; Juliane Kippenberg, senior researcher in the Children’s Rights Division at Human Rights Watch; Dipika Nath, researcher in the LGBT Rights Division at Human Rights Watch; Godfrey Malembeka, executive director of PRISCCA; Michaela Clayton, director of ARASA; Aisling Reidy, senior legal advisor at Human Rights Watch; and Iain Levine, program director at Human Rights Watch.
Kathleen Myer, consultant with the Health and Human Rights Division at Human Rights Watch, assisted with data entry and analysis; research into donor activities in Zambia was conducted by Sarah Pierce, intern with the Women’s Rights Division at Human Rights Watch. Mignon Lamia, associate in the Health and Human Rights Division at Human Rights Watch, provided editing and production assistance. Anna Lopriore, creative manager and photo editor, Kyle Knight, associate in the Children’s Rights Division, Grace Choi, publications director, and Fitzroy Hepkins, mail manager, all of Human Rights Watch, provided production assistance. Human Rights Watch would also like to thank Giulio Frigieri for the creation and design of the map and João Silva for photography.
A number of people provided invaluable assistance in the research and preparation of this report. Special thanks go to Godfrey Malembeka, himself a former prisoner, who provided coordination for the research mission and interpretation, as well as to Kelvin Musonda, Shadreck Lubita, Rodgers Siyingwa, and George Chikoti of PRISCCA, who served as interpreters and provided coordination assistance. PRISCCA, ARASA, and Human Rights Watch also acknowledge the assistance of the Zambia Prisons Service in permitting access to prison facilities, especially the Commissioner Gibbie Nawa, Deputy Commissioner Frederick Chilukutu, and the Ministries of Foreign Affairs and Home Affairs for clearing researchers and granting authority for this research.
PRISCCA, ARASA, and Human Rights Watch thank all of the individuals who agreed to be interviewed for this report. We are particularly grateful to all of the prisoners and prison officers whom we met and interviewed. Their willingness to share information and their experiences with us made this report possible.
Appendix: Request for Information to the Zambia Prisons Service
[1] Under Zambian law, a prisoner under the age of nineteen years (the minimum age of criminal responsibility is eight years) is classified as a “juvenile,” despite the fact that under international law, 18 year-olds are adults. Throughout this report, the term “juvenile” will be used to designate the category of prisoners ages eight to 18 held in Zambian prisons when necessary to refer to the classification used by the government. Otherwise, individuals in prison under age 18 will be referred to as “children” in accordance with the Convention on the Rights of the Child.
[2]In 2003, the Zambia Human Rights Commission reported that its “inspections revealed serious situations of congestion, filth, disease, inadequate food and poor water and sanitation facilities. Generally inmates lacked decent sleeping facilities and uniforms….Health and medical services were almost non-existent or poor in the majority of the prisons. The major diseases included tuberculosis, diarrhea and scabies….Inmates complained of torture, delayed justice, poor living conditions, inadequate food and poor medical attention.” Zambia Human Rights Commission, “Annual Report: 2003,” 2003, pp. 1 and 12. In 2005, the UN Committee on Economic, Social and Cultural Rights expressed concern about the “living conditions of prisoners and detainees, especially with regard to access to health-care facilities, adequate food and safe drinking water.” UN Committee on Economic, Social and Cultural Rights, “Consideration of Reports Submitted by States Parties under Articles 16 and 17 of the Covenant: Concluding Observations of the Committee on Economic, Social and Cultural Rights: Zambia,” Thirty-fourth session, 25 April-13 May 2006, E/C.12/1/Add.106, June 23, 2005, para. 28, http://www.unhchr.ch/tbs/doc.nsf/c12563e7005d936d4125611e00445ea9/04e80cf87aa13784c125700500465779/$FILE/G0542576.pdf (accessed February 22, 2010).
[3] US Department of State Bureau of Democracy, Human Rights, and Labor, “2009 Human Rights Report: Zambia,” March 11, 2010, http://www.state.gov/g/drl/rls/hrrpt/2009/af/135983.htm (accessed March 18, 2010).
[4]PRISCCA, ARASA, and Human Rights Watch telephone interview with Zambia Prisons Service headquarters, November 23, 2009.
[5]Zambia Human Rights Commission, “Annual Report: 2005,” 2005, http://www.hrc.org.zm/media/2005_annual_report.pdf (accessed March 1, 2010).
[6]Lisa Vetten, “The Imprisonment of Women in Africa,” in Jeremy Sarkin, ed., Human Rights in African Prisons, (Cape Town: HSRC Press, 2008), p. 136 (based on data provided by the International Centre for Prison Studies).
[7] While the prison population was significantly higher—15,300—in 2009, 2005 disaggregated statistics for the entire prison system by prisoner type were the most recent available.
[8]Prisons Act, Laws of Zambia, vol. 7, chapter 97, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 8.
[9] International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 59, U.N. Doc. A/6316 (1966), 999 U.N.T.S. 171, entered into force March 23, 1976, acceded to by Zambia on April 10, 1984, art. 10(3).
[10]Zambia Prisons Service, “HIV & AIDS/STI/TB Workplace Policy of the Zambia Prisons Service,” July 2006, p. 14.
[11]The Prisons Rules, Laws of Zambia, vol. 7, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 24(1).
[12]In 2003, the Zambia Human Rights Commission reported that “[h]ealth and medical services were almost non-existent or extremely poor in the majority of the prisons. Prison clinics have either closed down due to lack of personnel, drugs and other basic essentials…or they exist without any personnel or essential drugs.” Zambia Human Rights Commission, “Annual Report 2003,” p. 15.
[13] In Zambia, clinical officers typically have three years of post-secondary school training and the capacity to prescribe medications. PRISCCA, ARASA and Human Rights Watch interview with Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, Lusaka, February 6, 2010.
[14] Ibid.
[15] Ibid.
[16] Ibid.
[17] Republic of Zambia, Ministry of Health, “National Health Strategic Plan 2006-2010,” November 2005, http://www.who.int/nha/country/zmb/Zambia_NH_Strategic_plan,2006-2010%20.pdf (accessed March 2, 2010).
[18] World Bank, "Implementation, Completion and Results Report on a Grant in the Amount of SDR 33.7 million to the Republic of Zambia for the Zambia National Response to HIV/AIDS (Zanara) Project in Support of the Second Phase of the Multi-Country Aids Program for Africa," February 27, 2009, http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2009/04/01/000333038_20090401005842/Rendered/PDF/ICR9220ZM0P00310Disclosed0031301091.pdf (accessed March 1, 2010), pp. 67-68.
[19] Ministry of Health and National HIV/AIDS/STI/TB Council, "Zambia: National AIDS Spending Assessment for 2005 and 2006: Final Draft Technical Report," July 2008, http://data.unaids.org/pub/Report/2008/nasa_zambia_0506_20080721_en.pdf (accessed March 2, 2010), p. 82.
[20] Ibid., p. 112.
[21] PRISCCA, ARASA, and Human Rights Watch interview with Helmut Reutter, Go Centre/CHRESO Ministries, Lusaka, October 14, 2009.
[22] PRISCCA, ARASA, and Human Rights Watch interview with Simon Mutonyi, SHARe, October 16, 2009.
[23]PRISCCA, ARASA, and Human Rights Watch interview with Sharon Nyambe, national coordinator, HIV/AIDS in prison settings, UNODC, Lusaka, October 16, 2009.
[24]PRISCCA, ARASA, and Human Rights Watch interview with Robby Shabwanga, projects officer, Legal Resources Foundation, October 14, 2009. In 2010, a Ministry of Home Affairs official characterized funding as “nothing”. PRISCCA, ARASA and Human Rights Watch interview with Gezepi Chakulunta, HIV/AIDS focal point person, Ministry of Home Affairs, Lusaka, February 4, 2010.
[25] “2010 Budget Address by Dr. Situmbeko Musokotwane, MP, Honourable Minister of Finance and National Planning Delivered to the National Assembly on Friday 9th October, 2009,” http://www.mofnp.gov.zm/ (accessed March 18, 2010), p. 12.
[26] Email communication from Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, March 15, 2010.
[27] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[28]PRISCCA, ARASA, and Human Rights Watch interview with Robby Shabwanga, projects officer, Legal Resources Foundation, October 14, 2009.
[29] PRISCCA, ARASA, and Human Rights Watch interview with Gezepi Chakulunta, HIV/AIDS focal point person, Ministry of Home Affairs, February 4, 2010.
[30]PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, Lusaka, October 13, 2009; PRISCCA, ARASA and Human Rights Watch interview with Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, Lusaka, February 6, 2010.
[31] Email communication from Dr. Chisela Chileshe, director, Zambia Prisons Service Medical Directorate, March 15, 2010.
[32] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[33] Ibid.
[34] World Health Organization, UNAIDS and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: Core Data on Epidemiology and Response: 2008 Update: Zambia,” October 2008, p. 4.
[35] Oscar O. Simooya et al., “‘Behind Walls’: A Study of HIV Risk Behaviors and Seroprevalence in Prisons in Zambia,” AIDS, vol. 15(13), 2001, pp. 1741-44.
[36] US Department of State Bureau of Democracy, Human Rights, and Labor, “2008 Human Rights Report: Zambia,” February 25, 2009, http://www.state.gov/g/drl/rls/hrrpt/2008/af/119031.htm (accessed March 2, 2010); US Department of State, “2009 Human Rights Report: Zambia.”
[37] Zambia Prisons Service, “Draft Operational Plan,” 2008, p. 9.
[38]The number of CD4 cells (T-helper lymphocytes with CD4 cell surface marker) used to assess immune status, susceptibility to opportunistic infections, and a patient’s need for ART; CD4 count is the most important lab result for untreated HIV patients. Joel E. Gallant and Christoper Hoffmann, Johns Hopkins Point-of-Care Information Technology, “HIV Guide: CD4 Cell Count,” March 18, 2009, http://www.hopkins-aids.edu/management/laboratory_testing/cd4_cell_count.html?contentInstanceId=8279 (accessed March 2, 2010).
[39] World Health Organization, UNAIDS and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: Core Data on Epidemiology and Response: 2008 Update: Zambia.”
[40] Republic of Zambia, Ministry of Health, “National HIV/AIDS/STI/TB Policy,” January 2005, p. 34.
[41] World Health Organization, UNAIDS and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: Core Data on Epidemiology and Response: 2008 Update: Zambia,” pp. 12-13.
[42] Ibid., p. 16.
[43] PRISCCA, ARASA, and Human Rights Watch PRISCCA, ARASA, and Human Rights Watch interview with Felix Mwanza, national coordinator, Treatment Advocacy and Literacy Campaign, Lusaka, October 15, 2009.
[44]UNODC, UNAIDS and World Bank, “HIV and Prisons in Sub-Saharan Africa: Opportunities for Action,” p. 2. E. Rutta et al., “Tuberculosis in a Prison Population in Mwanza, Tanzania (1994-1997),” The International Journal of Tuberculosis and Lung Disease, vol. 5(8), 2001, pp. 703-06.
[45] According to the World Health Organization, multi-drug resistant TB is “is a specific form of drug-resistant TB due to a bacillus resistant to at least isoniazid and rifampicin, the two most powerful anti-TB drugs.” Drug resistance “arises due to the improper use of antibiotics in chemotherapy of drug-susceptible TB patients. This improper use is a result of a number of actions, including administration of improper treatment regimens by health care workers and failure to ensure that patients complete the whole course of treatment. Essentially, drug-resistance arises in areas with poor TB control programmes.” World Health Organization, “Drug- and Multi-Drug Resistant Tuberculosis (MDR-TB)—Frequently Asked Questions,” undated, http://www.who.int/tb/challenges/mdr/faqs/en/index.html (accessed March 1, 2010).
[46]C. Habeenzu et al., “Tuberculosis and Multidrug Resistance in Zambian Prisons, 2000-2001,” TheInternational Journal of Tuberculosis and Lung Disease, vol. 11(11), 2007, pp. 1216-1220.
[47]R. Coninx et al., “Tuberculosis in Prisons,” The Lancet, vol. 346, November 1995, pp. 1238-39. Studies have found a high rate of pulmonary tuberculosis in prisons, which suggests active transmission. See, e.g., D.S. Nyangulu et al., “Tuberculosis in a Prison Population in Malawi,” The Lancet, vol. 350(9087), November 1997, pp. 1284-87.
[48] UNAIDS, “Tuberculosis and HIV,” undated, http://www.unaids.org/en/PolicyAndPractice/HIVTreatment/Coinfection/TB/default.asp (accessed February 12, 2010).
[49] World Health Organization, “Zambia: TB Country Profile: Surveillance and Epidemiology,” 2007, http://apps.who.int/globalatlas/predefinedReports/TB/PDF_Files/zmb.pdf (accessed March 2, 2010).
[50] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Nathan Kapata, director of the national tuberculosis program, Ministry of Health, Lusaka, February 8, 2010.
[51] World Health Organization, “Zambia: TB Country Profile.”
[52] World Health Organization, “Treatment Outcomes, New Smear Positive Cases, 1995-2007,” 2009, http://www.who.int/tb/publications/global_report/2009/update/a-5_afr.pdf (accessed March 2, 2010), p. 8.
[53] PRISCCA, ARASA, and Human Rights Watch interview with Felix Mwanza, national coordinator, TALC, October 15, 2009.
[54] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Helen Ayles, project coordinator, ZAMBART, Lusaka, February 9, 2010.
[55] PRISCCA, ARASA, and Human Rights Watch telephone interview with Chisela Chileshe, October 13, 2009.
[56] Chisela Chileshe, “The Role of a Prison Manager in TB/HIV/AIDS Prevention and Management,” powerpoint presentation, undated, presentation on file with Human Rights Watch.
[57] Zambia Prisons Service, “Draft Operational Plan,” 2008, p. 9.
[58] PRISCCA, ARASA, and Human Rights Watch interview with Sergeant Kabukabu, prison officer, Mumbwa Prison, October 5, 2009.
[59] PRISCCA, ARASA, and Human Rights interview with Annie Sabuni, HIV/AIDS coordinator, Lusaka Central Prison, October 3, 2009.
[60]Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (Convention against Torture), adopted December 10, 2984, G.A. res. 39/46, annex, 39 U.N. GAOR Supp. (No. 51) at 197, U.N. Doc. A/39/51 (1984), entered into force June 26, 1987), acceded to by Zambia on October 7, 1998.
[61]International Covenant on Economic, Social and Cultural Rights (ICESCR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 49, U.N. Doc. A/6316 (1966), 993 U.N.T.S. 3, entered into force January 3, 1976, acceded to by Zambia on April 10, 1984.
[62]Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), adopted December 18, 1979, G.A. res. 34/180, 34 U.N. GAOR Supp. (No. 46) at 193, U.N. Doc. A/34/46, entered into force September 3, 1981, acceded to by Zambia on June 21, 1985.
[63] Convention on the Rights of the Child (CRC), adopted November 20, 1989, G.A. Res. 44/25, annex, 44 U.N. GAOR Supp. (No. 49) at 167, U.N. Doc. A/44/49 (1989), entered into force September 2, 1990, acceded to by Zambia on December 6, 1991.
[64]International Convention on the Elimination of All Forms of Racial Discrimination (ICERD), adopted December 21, 1965, G.A. Res. 2106 (XX), annex, 20 U.N. GAOR Supp. (No. 14) at 47, U.N. Doc. A/6014 (1966), 660 U.N.T.S. 195, entered into force January 5, 1969, ratified by Zambia on February 4, 1972.
[65] African [Banjul] Charter on Human and Peoples' Rights, adopted June 27, 1981, OAU Doc. CAB/LEG/67/3 rev. 5, 21 I.L.M. 58 (1982), entered into force Oct. 21, 1986, ratified on January 10, 1984.
[66]Protocol to the African Charter on Human and Peoples' Rights on the Rights of Women in Africa, adopted by the 2nd Ordinary Session of the Assembly of the Union, Maputo, CAB/LEG/66.6 (Sept. 13, 2000); entered into force Nov. 25, 2005.
[67]United Nations (UN) Standard Minimum Rules for the Treatment of Prisoners (Standard Minimum Rules), adopted by the First United Nations Congress on the Prevention of Crime and the Treatment of Offenders, held at Geneva in 1955, and approved by the Economic and Social Council by its resolution 663 C (XXIV) of July 31, 1957, and 2076 (LXII) of May 13, 1977, paras. 57-58; United Nations (UN) Human Rights Committee, General Comment 21, Article 10, Humane Treatment of Persons Deprived of Liberty (Forty-fourth session, 1992), Compilation of General Comments and General Recommendations Adopted by Human Rights Treaty Bodies, UN Doc. HRI/GEN/1/Rev.7 (1994), paras. 3-4; Basic Principles for the Treatment of Prisoners, adopted December 14, 1990, G.A. Res. 45/111, annex, 45 U.N. GAOR Supp. (No. 49A) at 200, U.N. Doc. A/45/49 (1990), principle 5.
[68] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 57-58.
[69]UN Human Rights Committee, General Comment 21, paras. 3-4.
[70] The Constitution of Zambia Act, The Laws of Zambia, 1996, http://www.parliament.gov.zm/downloads/VOLUME%201.pdf (accessed March 2, 2010), art. 15.
[71]ICCPR, art. 10.
[72]African [Banjul] Charter on Human and Peoples’ Rights, art. 5.
[73] Convention Against Torture, art. 1.
[74] UN Standard Minimum Rules for the Treatment of Prisoners; Body of Principles for the Protection of All Persons under Any Form of Detention of Imprisonment (Body of Princniples), adopted December 9, 1988, G.A. Res. 43/173, annex, 43 U.N. GAOR Supp. (No. 49) at 298, U.N. Doc. A/43/49 (1988); Basic Principles for the Treatment of Prisoners.
[75] Convention on the Rights of the Child (CRC), art. 37(a) and (c).
[76] Ibid., art. 37(b).
[77] Ibid., art. 37(c).
[78] UN Standard Minimum Rules for the Administration of Juvenile Justice (“The Beijing Rules”), adopted November 29, 2985, G.A. Res. 40/33, annex, 40 U.N. GAOR Supp. (No. 53) at 207, U.N. Doc. A/40/53 (1985), art. 26.
[79] Protocol to the African Charter on Human and Peoples’ Rights on the Rights of Women in Africa, art. 24. Zambia is a party to this Protocol.
[80]Southern African Development Community (SADC) Protocol on Gender and Development, http://www.sadc.int/index/browse/page/465 (accessed February 22, 2010), art. 26.
[81]Universal Declaration of Human Rights (UDHR), adopted December 10, 1948, G.A. Res. 217A(III), U.N. Doc. A/810 at 71 (1948), art. 25(1); International Covenant on Economic, Social and Cultural Rights (ICESCR), art. 12. The right to health is also guaranteed by a number of other international human rights treaties and commitments that bind Zambia. The Convention on the Rights of the Child obligates states to “recognize the right of the child to the enjoyment of the highest attainable standard of health and to facilities for the treatment of illness and rehabilitation of health. States Parties shall strive to ensure that no child is deprived of his or her right of access to such health care services.” Convention on the Rights of the Child, art. 24. The right to the health is recognized by the International Convention on the Elimination of All Forms of Racial Discrimination and in 11.1(f), 12 and 14(2)(b) of the Convention on the Elimination of Discrimination Against Women. The right to health has been proclaimed by the Commission on Human Rights, the Vienna Declaration and Programme of Action of 1993 and other international instruments. UN Committee on Economic, Social and Cultural Rights, “Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights,” General Comment No. 14, the Right to the Highest Attainable Standard of Health, E/C.12/2000/4 (2000), http://www.unhchr.ch/tbs/doc.nsf/0/40d009901358b0e2c1256915005090be?Opendocument (accessed February 22, 2010), para. 2.
[82]ICESCR, art. 12.
[83]The African Charter on Human and Peoples’ Rights guarantees the right to health and requires states parties to “take the necessary measures to protect the health of their people and to ensure that they receive medical attention when they are sick.” African [Banjul] Charter on Human and Peoples’ Rights, art. 16. See also, Southern African Development Community (SADC) Protocol on Gender and Development, art. 26.
[84] ICESCR, General Comment No. 14, paras. 30-31.
[85]Ryszard Cholewinski, “Economic and Social Rights of Refugees and Asylum Seekers in Europe,” Georgetown Immigration Law Journal, vol. 14, Spring 2000, pp. 709-55, pp. 714-19.
[86] See, e.g., ICESCR, arts. 12(1) and 2.2; ICCPR, arts. 6, 7 and 10(1); Convention against Torture, art. 16. For a comprehensive discussion of the international legal instruments, international resolutions, and model standards related to detainee health, see Rick Lines, “The Right to Health of Prisoners in International Human Rights Law,” International Journal of Prisoner Mental Health, vol. 4(1), 2008, pp. 3-53; Rick Lines, “From Equivalence of Standards to Equivalence of Objectives: The Entitlement of Prisoners to Health Care Standards Higher than Those Outside Prisons,” International Journal of Prisoner Health, vol. 2(4), 2006, pp. 1-12.
[87]ICESCR, General Comment No. 14, para. 34.
[88]Pinto v. Trinidad and Tobago (Communication No. 232/1987), Report of the Human Rights Committee, vol. 2, UN Doc A/45/40, p. 69.
[89]United Nations (UN) Committee against Torture (CAT), “Concluding Observations: New Zealand,” (1998) UN Doc. A/53/44, para. 175.
[90]Zambia Prisons Service, “HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 2. Indeed, “[a]ll inmates have the right to receive health care, including preventive measures and treatment equivalent to that available in the community.” Zambia Prisons Service, “HIV & AIDS/STI/TB Workplace Policy of the Zambia Prisons Service,” July 2006, p. 17.
[91] ICCPR, art. 10; Convention on the Rights of the Child, art. 37; Basic Principles for the Treatment of Prisoners, prin. 1.
[92]See UN Human Rights Committee, General Comment No. 21, para. 3. See also Manfred Nowak, United Nations Covenant on Civil and Political Rights: CCPR Commentary, 2nd rev. ed. (Kehl/Strasbourg/Arlington, N.P. Engel Verlag, 2005), p. 241 et seq; Manfred Nowak, Interim Report of the Special Rapporteur on Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment, U.N. Doc. A/64/215 (2009), http://www2.ohchr.org/english/issues/torture/rapporteur/docs/A-64-215.pdf (accessed March 2, 2010).
[93]Nowak, Interim Report of the Special Rapporteur on Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment. See also notes 71 and 72 and related text.
[94] US Department of State, “2009 Human Rights Report: Zambia”; PRISCCA, ARASA, and Human Rights Watch telephone interview with Zambia Prisons Service headquarters, November 23, 2009.
[95] Government of Zambia, “National Report Submitted in Accordance with Paragraph 15(A) of the Annex to Human Rights Council Resolution 5/1: Zambia,” U.N. Doc. A/HRC/WG.6/2/ZMB/1 (2008), para. 61.
[96]The US State Department report from 2009 acknowledged rates of overcrowding to the extent that some inmates were forced to sleep sitting upright, and noted that “[p]oor sanitation, dilapidated infrastructure, inadequate and deficient medical facilities, meager food supplies, and lack of potable water resulted in serious outbreaks of dysentery, cholera, and tuberculosis, which the overcrowding exacerbated.” US Department of State, “2009 Human Rights Report: Zambia.” In 2007, the Human Rights Committee “expresse[d] concern at the intolerable rate of prison overcrowding and the very poor conditions in places of detention” and called on Zambia to develop alternatives to imprisonment. Indeed, it recommended that “To the extent that the State party is unable to meet the needs of detainees, it should immediately take action to reduce the prison population.” UN Human Rights Committee, “Consideration of Reports Submitted by States Parties under Article 40 of the Covenant: Concluding Observations of the Human Rights Committee: Zambia,” U.N. Doc. CCPR/C/ZMB/CP/3 (2007), pp. 6-7. In 2008, the Committee Against Torture expressed concern regarding “the severe overcrowding in detention facilities.” Committee Against Torture, “Consideration of Reports Submitted by States Parties Under Article 19 of the Convention: Concluding Observations of the Committee Against Torture: Zambia,” U.N. Doc. CAT/C/ZMB/CO/2 (2008), http://daccess-dds-ny.un.org/doc/UNDOC/GEN/G08/421/29/PDF/G0842129.pdf?OpenElement (accessed March 2, 2010), para. 15
[97] UN Standard Minimum Rules for the Treatment of Prisoners, arts. 9-19.
[98] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[99]PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[100] Ibid. In fact, each of the six prisons we visited far exceeded its design capacity: Kamfinsa Prison, built with a design capacity of 1000, housed 1494 inmates. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009. At Mumbwa Prison, a facility built to hold 150 inmates held 354 on the day of our visit—sometimes the facility holds as many as 460. PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009. Choma prison holds 251, though it was built with a capacity of 120. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[101] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[102] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison. September 29, 2009.
[103] Prisoners PRISCCA, ARASA, and Human Rights Watch interviewed will be cited by unique pseudonym or by a unique code assigned to each prisoner interviewed by researchers, indicating the initials of the interviewer, the date of the interview, and assigning each prisoner interviewed a number. PRISCCA, ARASA, and Human Rights Watch interview with Hastings, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-29-05, Mukobeko Maximum Security Prison, September 29, 2009.
[104] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[105] UN Standard Minimum Rules for the Treatment of Prisoners, para. 19.
[106] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[107] Ibid.
[108] PRISCCA, ARASA, and Human Rights Watch interview with Felix, Mukobeko Maximum Security Prison, September 29, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with KT-03-06, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Evans, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Chiluba, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mukobeko Maximum Security Prison, September 30, 2009.
[109] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Noah, Mumbwa Prison, October 5, 2009. Two women and two children sleep per mattress on the women’s side of Lusaka Central. PRISCCA, ARASA, and Human Rights Watch interview with Inonge, Lusaka Central Prison, October 3, 2009.
[110] PRISCCA, ARASA, and Human Rights Watch interview with social welfare worker, Lusaka Central Prison, October 3, 2009.
[111] PRISCCA, ARASA, and Human Rights Watch interview with Liberty Halanga Hangoma, offender management officer, Mukobeko Maximum Security Prison, September 29, 2009.
[112] PRISCCA, ARASA, and Human Rights Watch interview with Winston, Mukobeko Maximum Security Prison, September 29, 2009.
[113] PRISCCA, ARASA, and Human Rights Watch interview with Allan, Mukobeko Maximum Security Prison, September 29, 2009.
[114] PRISCCA, ARASA, and Human Rights Watch interview with Semba, Mumbwa Prison, October 5, 2009.
[115] PRISCCA, ARASA, and Human Rights Watch interview with Gerald, Mukobeko Maximum Security Prison, September 30, 2009.
[116] PRISCCA, ARASA, and Human Rights Watch interview with Chrispine, Kamfinsa Prison, October 1, 2009.
[117] PRISCCA, ARASA, and Human Rights Watch interview with Albert, Lusaka Central Prison, October 3, 2009.
[118] PRISCCA, ARASA, and Human Rights Watch interview with Rodgers, Lusaka Central Prison, October 3, 2009.
[119] PRISCCA, ARASA, and Human Rights Watch interview with B.M. Hambwalou, medical officer, Choma prison, October 8, 2009.
[120] PRISCCA, ARASA, and Human Rights Watch interview with Jean Marie, Lusaka Central Prison, October 3, 2009.
[121] See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Inonge, Lusaka Central Prison, October 3, 2009.
[122] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 10 and 11(a).
[123] PRISCCA, ARASA, and Human Rights Watch interview with KT-04-06, Lusaka Central Prison, October 4, 2009.
[124] PRISCCA, ARASA, and Human Rights Watch interview with Hastings, Mukobeko Maximum Security Prison, September 29, 2009.
[125] PRISCCA, ARASA, and Human Rights Watch interview with Esther, Lusaka Central Prison, October 4, 2009.
[126] ICCPR, art. 10; UN Standard Minimum Rules for the Treatment of Prisoners, paras. 9-11; Body of Principles, prin. 8. Human Rights Committee, General Comment 21, paras. 9 and 13; United Nations High Commissioner for Refugees, “Detention of Refugees and Asylum Seekers,” October 13, 1986, http://www.unhcr.org/refworld/docid/3ae68c43c0.html%20[accessed%201%20March%202010],%20art.%20f (accessed March 2, 2010), art. f.
[127] Prisons Rules, sec. 162(1); Prisons Act, sec. 60.
[128] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[129] Ibid.
[130] PRISCCA, ARASA, and Human Rights Watch interview with Kabinga, Mukobeko Maximum Security Prison, September 29, 2009.
[131] PRISCCA, ARASA, and Human Rights Watch interview with Peter, Choma Prison, October 8, 2009.
[132] PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Elijah, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Andrew, Mumbwa Prison, October 5, 2009.
[133] PRISCCA, ARASA, and Human Rights Watch interview with Clifford, Kamfinsa Prison, October 1, 2009.
[134] PRISCCA, ARASA, and Human Rights Watch interview with Febian, Mumbwa Prison, October 5, 2009.
[135] PRISCCA, ARASA, and Human Rights Watch interview with chaplain, Mukobeko Prison, September 29, 2009.
[136] Manfred Nowak, “U.N. Covenant on Civil and Political Rights, CCPR Commentary,” (2nd edition) (Khel: N.P. Engel, 2005), pp. 165, 172-75, 244-29. See, for example, cases against Uruguay such as Buffo Carball v. Uruguay, No. 33/1978, Massiotti v. Uruguay, No. 25/1978; Madagascar: Marais v. Madagascar, No. 49/1979, Wight v. Madagascar, No. 115/1982; Jamaica: Robinson v. Jamaica, No. 731/1996, Pennant v. Jamaica, No. 647/1995; Russia: Lantsova v. Russian Federation, No. 763/1997.
[137] UN Standard Minimum Rules for the Treatment of Prisoners, para. 20(1).
[138] See Mukong v. Cameroon, No. 458/1991, para. 9.3.
[139] United Nations Rules for the Protection of Juveniles Deprived of their Liberty, adopted December 14, 1990, G.A. Res. 45/113, annex, 45 U.N. GAOR Supp. (No. 49A) at 205, U.N. Doc. A/45/49 (1990), para. 37.
[140] Prisons Rules, “Prison Rations: Part I.”
[141] According to prisoners at Mukobeko and Lusaka, sometimes the same portion of 450g is divided into two pieces so as make it appear to be two meals.
[142] PRISCCA, ARASA, and Human Rights Watch interview with Noah, Mumbwa Prison, October 5, 2009. The revenues from prison farm labor reportedly are placed into a fund called the Prison Industry Revolving Fund (PIRF). This scheme was created with the understanding that “the government is not managing to feed [prisoners] well because of other demands on the treasury.” Reportedly, the yearly food budget for 2009 was 10 billion kwacha (US$2,110,510), but the Prisons Service would ask for 65 billion kwacha ($13,718,300) if it were not for the existence of the PIRF. The “excess” produced at the farms is sold to generate income. PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[143] Zambia Prisons Service, “HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 10.
[144] PRISCCA, ARASA, and Human Rights Watch interview with Winston, Mukobeko Maximum Security Prison, September 29, 2009.
[145] Email communication from Dr. Jessica Fanzo, director of nutrition, Center for Global Health and Economic Development, Earth Institute at Columbia University, to PRISCCA, ARASA, and Human Rights Watch, April 7, 2010. Most men consume 2,500 calories daily to maintain body weight. Ibid.
[146] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[147] PRISCCA, ARASA, and Human Rights Watch interview with George Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[148] PRISCCA, ARASA, and Human Rights Watch interview with Kayombo, Mukobeko Maximum Security Prison, September 30, 2009.
[149] PRISCCA, ARASA, and Human Rights Watch interview with George, Kamfinsa Prison, October 1, 2009.
[150] PRISCCA, ARASA, and Human Rights Watch interview with Frederick, Mwembeshi Prison, October 6, 2009.
[151] PRISCCA, ARASA, and Human Rights Watch interview with Johnston, Mumbwa Prison, October 5, 2009.
[152] PRISCCA, ARASA, and Human Rights Watch interview with Robbie, Mwembeshi Prison, October 6, 2009.
[153] PRISCCA, ARASA, and Human Rights Watch interview with Adam, Mumbwa Prison, October 5, 2009.
[154] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[155] PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[156] PRISCCA, ARASA, and Human Rights Watch interview with Mutabale Henry, medical officer, Mukobeko Maximum Security Prison, September 29, 2009.
[157] PRISCCA, ARASA, and Human Rights Watch interview with B.M. Hambwalou, medical officer, Choma Prison, October 8, 2009.
[158] PRISCCA, ARASA, and Human Rights Watch interview with George, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Andrew, Mumbwa Prison, October 5, 2009.
[159] PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009.
[160] PRISCCA, ARASA, and Human Rights Watch interview with RS-29-04, Mukobeko Maximum Security Prison, September 29, 2009.
[161] PRISCCA, ARASA, and Human Rights Watch interview with Peter, Choma Prison, October 8, 2009.
[162] Dr. Chileshe confirmed that beri beri is seen in the prisons system. PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[163] PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[164] PRISCCA, ARASA, and Human Rights Watch interview with Tasila, Kamfinsa Prison, October 1, 2009.
[165] PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-01, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Joyce Simukali, prison officer, Kamfinsa Prison (Women’s Side), October 2, 2009.
[166] Body of Principles, prin. 31.
[167] Prisons Act, sec. 56. Zambian policy also provides that these children shall be provided with food. See Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 7 (“Similarly, there are some infants and young children who are imprisoned along with their mothers. By definition these children are under the care of the State—in this case Prisons Service. It is important to recognise these children’s rights and their needs, i.e. necessary facilities and actions to promote the health and wellness of these children and reduce their vulnerability to HIV and AIDS, STIs and TB.”); Zambia Prisons Service, “HIV & AIDS/STI/TB Workplace Policy,” p. 25 (“Children born with HIV should receive appropriate treatment and nutrition through linkages with public health systems and other cooperating partners.”).
[168] PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-04, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-04-05, Lusaka Central Prison, October 4, 2009.
[169] PRISCCA, ARASA, and Human Rights Watch interview with Agnes, Kamfinsa Prison, October 1, 2009.
[170] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[171] PRISCCA, ARASA, and Human Rights Watch interview with Tasila, Kamfinsa Prison, October 1, 2009.
[172] PRISCCA, ARASA, and Human Rights Watch interview with Annie, Lusaka Central Prison, October 4, 2009.
[173] PRISCCA, ARASA, and Human Rights Watch interview with Willard, Mukobeko Maximum Security Prison, September 29, 2009.
[174] PRISCCA, ARASA, and Human Rights Watch interview with Orbed, Mukobeko Maximum Security Prison, September 30, 2009.
[175]PRISCCA, ARASA, and Human Rights Watch interview with Lawrence, Mukobeko Maximum Security Prison, September 30, 2009.
[176] PRISCCA, ARASA, and Human Rights Watch interview with Kayombo, Mukobeko Maximum Security Prison, September 30, 2009.
[177] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 12-14.
[178] The Zambia Human Rights Commission in 2005 corroborated that “[t]oilet and sanitation facilities were either broken down or nonexistent in most cases. Sewer and sanitation infrastructure were dilapidated and posed a serious health hazard.” Zambia Human Rights Commission, “Annual Report: 2005.”
[179] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[180] PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009.
[181] PRISCCA, ARASA, and Human Rights Watch interview with Paul, Mukobeko Maximum Security Prison, September 30, 2009.
[182] PRISCCA, ARASA, and Human Rights Watch interview with Daniel, Mukobeko Maximum Security Prison, September 30, 2009.
[183] PRISCCA, ARASA, and Human Rights Watch interview with Nickson, Mukobeko Maximum Security Prison, September 30, 2009.
[184] PRISCCA, ARASA, and Human Rights Watch interview with KT-29-05, Mukobeko Maximum Security Prison, September 29, 2009.
[185] PRISCCA, ARASA, and Human Rights Watch interview with Anderson, Choma Prison, October 8, 2009.
[186] PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-05, Lusaka Central Prison, October 3, 2009.
[187] PRISCCA, ARASA, and Human Rights Watch interview with Esther, Lusaka Central Prison, October 4, 2009.
[188] PRISCCA, ARASA, and Human Rights Watch interview with Chrispine, Kamfinsa Prison, October 1, 2009.
[189] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-04, Lusaka Central Prison, February 6, 2010. The Lusaka Central Prison social welfare worker confirmed that at that facility, “the physically challenged—there are 5—have problems using the toilet. They need wheelchairs.” PRISCCA, ARASA, and Human Rights Watch interview with social welfare worker, Lusaka Central Prison, October 3, 2009.
[190] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Lusaka Central Prison, February 6, 2010.
[191] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[192] PRISCCA, ARASA, and Human Rights Watch PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mukobeko Maximum Security Prison, September 30, 2009.
[193] PRISCCA, ARASA, and Human Rights Watch interview with Ms. Kaluba, offender management officer, Mwembeshi Prison, October 6, 2009.
[194]PRISCCA, ARASA, and Human Rights Watch interview with Douglas, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-03, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-01, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-05-01, Mumbwa Prison, October 5, 2009.
[195] UN Standard Minimum Rules for the Treatment of Prisoners, para. 20(2).
[196] PRISCCA, ARASA, and Human Rights Watch interview with Ngwila, Choma Prison, October 8, 2009.
[197] PRISCCA, ARASA, and Human Rights Watch interview with Norah, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Annie, Lusaka Central Prison, October 4, 2009.
[198] PRISCCA, ARASA, and Human Rights Watch interview with CM-01-06, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-05-01, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-09, Mwembeshi Prison, October 6, 2009.
[199] PRISCCA, ARASA, and Human Rights Watch interview with Liberty Halanga Hangoma, offender management officer, Mukobeko Maximum Security Prison, September 29, 2009.
[200] PRISCCA, ARASA, and Human Rights Watch interview with Albert Sakala, prison officer, Mukobeko Maximum Security Prison, September 29, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with RS-29-01, Mukobeko Maximum Security Prison, September 29, 2009.
[201] PRISCCA, ARASA, and Human Rights Watch interview with NCI-02-01, Kamfinsa Prison, October 2, 2009.
[202] PRISCCA, ARASA, and Human Rights Watch interview with Festus, Mwembeshi Prison, October 6, 2009.
[203] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-09, Mwembeshi Prison, October 6, 2009.
[204] PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009.
[205] PRISCCA, ARASA, and Human Rights Watch interview with Ms. Kaluba, offender management officer, Mwembeshi Prison, October 6, 2009.
[206] PRISCCA, ARASA, and Human Rights Watch interview with Adam, Mumbwa Prison, October 5, 2009.
[207] PRISCCA, ARASA, and Human Rights Watch interview with Moono, Lusaka Central Prison, October 3, 2009.
[208]Some officers in charge have been particularly proactive in engaging the church and NGO communities and soliciting such support. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[209] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 15-19.
[210] Prisons Act, sec. 89; Prisons Rules, sec. 163(1).
[211] PRISCCA, ARASA, and Human Rights Watch interview with Catherine, Lusaka Central Prison, October 4, 2009.
[212] PRISCCA, ARASA, and Human Rights Watch interview with Annie Sabuni, HIV/AIDS Coordinator, Lusaka Central Prison, October 3, 2009.
[213] PRISCCA, ARASA, and Human Rights Watch interview with Mwape, Mukobeko Maximum Security Prison, September 29, 2009.
[214] PRISCCA, ARASA, and Human Rights Watch interview with Chris, Mukobeko Maximum Security Prison, September 29, 2009.
[215] PRISCCA, ARASA, and Human Rights Watch interview with Douglas, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009.
[216] UN Standard Minimum Rules for the Treatment of Prisoners, para. 19.
[217] PRISCCA, ARASA, and Human Rights Watch interview with MM-06-08, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009.
[218] PRISCCA, ARASA, and Human Rights Watch interview with Jacob, Mwembeshi Prison, October 6, 2009.
[219] PRISCCA, ARASA, and Human Rights Watch interview with MM-06-08, Mwembeshi Prison, October 6, 2009.
[220] PRISCCA, ARASA, and Human Rights Watch interview with Mary, Lusaka Central Prison, October 4, 2009.
[221] Since 2003, the Zambia Human Rights Commission has confirmed that “prisoners’ uniforms…were in a terrible state….Even where ‘uniforms’ were available, they were often in tatters and left the inmates bare.” Zambia Human Rights Commission, “Annual Report: 2003,” p. 15.
[222] PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-01, Kamfinsa Prison, October 1, 2009.
[223] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[224] PRISCCA, ARASA, and Human Rights Watch interview with Marlon, Mukobeko Maximum Security Prison, September 29, 2009.
[225] PRISCCA, ARASA, and Human Rights Watch interview with Reynard, Mwembeshi Prison, October 6, 2009.
[226] PRISCCA, ARASA, and Human Rights Watch interview with Bwalya, Mwembeshi Prison, October 6, 2009.
[227] PRISCCA, ARASA, and Human Rights Watch interview with Mwape, Mukobeko Maximum Security Prison, September 29, 2009.
[228] PRISCCA, ARASA, and Human Rights Watch interview with Mwisa, Choma Prison, October 8, 2009.
[229] PRISCCA, ARASA, and Human Rights Watch interview with Sylvia, Mumbwa Prison, October 5, 2009.
[230] In December 1994, a study of the impact of HIV/AIDS programs in Zambian prisons found that 8.4 percent of respondents reported same-sex sexual activity, although indirect questioning suggested a much higher percentage. O. Simooya et al., “Sexual Behavior and Issues of HIV/AIDS Prevention in an African Prison,” AIDS, vol. 9(12), 1995, pp. 1388-89. The 1998-99 prevalence study found that “[a]lthough only 3.9 percent of inmates reported having sex with other men, the figures may be much higher. When we invited inmates to indicate how common sex between men was at their prison, over 50 percent replied that many were involved, and 6 percent said that almost all were involved.” Oscar O. Simooya et al., “‘Behind Walls’: A Study of HIV Risk Behaviors and Seroprevalence in Prisons in Zambia,” AIDS, vol. 15(13), 2001, pp. 1741-44. UNODC, UNAIDS, and the World Bank have acknowledged that “[c]ommon high-risk behavior in the prison environment include unprotected sex (mostly anal and between males), rape, sex bartering and “prison marriages.” Additionally, “women in prison are also susceptible to sexual exploitation and may trade or be forced to trade sex for food, goods or drugs with other prisoners or staff.” UNODC, UNAIDS and World Bank, “HIV and Prisons in Sub-Saharan Africa,” p. 1. Additionally, “women in prison are also susceptible to sexual exploitation and may trade or be forced to trade sex for food, goods or drugs with other prisoners or staff.” Ibid., p. 9.
[231] Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 4.
[232] UNAIDS, “Report on the Global AIDS Epidemic,” 2006, http://www.unaids.org/en/KnowledgeCentre/HIVData/GlobalReport/2006/default.asp (accessed March 3, 2010), p. 120.
[233] Judgment, International Criminal Tribunal for Rwanda (ICTR), Prosecutor v. Jean-Paul Akayesu, Case No. ICTR-96-4-T (1998), para. 38.
[234] See Penal Code Act, sec. 132 and sec. 138 respectively.
[235] PRISCCA, ARASA, and Human Rights Watch interview with Kabinga, Mukobeko Maximum Security Prison, September 29, 2009.
[236]PRISCCA, ARASA, and Human Rights Watch interview with Chris, Mukobeko Maximum Security Prison, September 29, 2009.
[237]PRISCCA, ARASA, and Human Rights Watch interview with David, Lusaka Central Prison, October 3, 2009.
[238]PRISCCA, ARASA, and Human Rights Watch interview with Moono, Lusaka Central Prison, October 3, 2009.
[239] PRISCCA, ARASA, and Human Rights Watch interview with Evans, Lusaka Central Prison, October 4, 2009. See also, “we have had experiences where the older inmates become physical and abuse us, even sexually. They will offer me food mixed with drugs, and when I take it in the night I sleep without being conscious. Or cigarettes dipped in some drugs. If it works, I sleep and they abuse me in the night, even sexually.” PRISCCA, ARASA, and Human Rights Watch interview with David, Lusaka Central Prison, October 3, 2009.
[240] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[241] PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[242] PRISCCA, ARASA, and Human Rights Watch interview with Albert Sakala, prison officer, Mukobeko Maximum Security Prison, September 29, 2009.
[243] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009.
[244] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009. PRISCCA, ARASA, and Human Rights Watch were unable to verify what these exams consist of, and whether they are conducted with consent, as none of the prisoners we interviewed reported having had such an exam. If conducted without genuine consent, however, physical exams under these conditions could constitute torture.
[245] PRISCCA, ARSA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[246] PRISCCA, ARASA, and Human Rights Watch interview with D. Mulenga, deputy officer in charge, Mumbwa Prison, October 5, 2009.
[247] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[248] Furthermore, international standards provide that “the medical services of the institution shall seek to detect and shall treat any physical or mental illnesses or defects which may hamper a prisoner's rehabilitation. All necessary medical, surgical and psychiatric services shall be provided to that end.” UN Standard Minimum rules for the Treatment of Prisoners, para. 62. Every institution must have at least one qualified medical officer, access to dentistry services, and transfer of sick prisoners requiring specialist treatment to specialized institutions or civil hospitals. Ibid., para. 22. See also Basic Principles for the Treatment of Prisoners, prin. 9.
[249]C. Habeenzu et al., “Tuberculosis and Multidrug Resistance in Zambian Prisons, 2000-2001,” TheInternational Journal of Tuberculosis and Lung Disease, pp. 1216-1220.
[250] Zambia Prisons Service, “Draft Operational Plan,” 2008, p. 9.
[251] Mukobeko had 118 new inmates in August-September 2009. PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009. Lusaka Central receives 20-40 new inmates each day (with two to three leaving each day). PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009. Choma Prison received 104 new inmates in September 2009 (out of 251 total). PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[252] PRISCCA, ARASA, and Human Rights Watch interview with Grief Chisenga, prison officer, Mwembeshi Prison, October 6, 2009.
[253] PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Albert Sakala, prison officer, Mukobeko Maximum Security Prison, September 29, 2009.
[254] PRISCCA, ARASA, and Human Rights Watch interview with Joyce Simukali, prison officer, Kamfinsa Prison, October 2, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Karen Chibwe, prison officer, Lusaka Central Prison, October 4, 2009.
[255] PRISCCA, ARASA, and Human Rights Watch interview with KT-29-05, Mukobeko Maximum Security Prison, September 29, 2009.
[256] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[257]PRISCCA, ARASA, and Human Rights Watch interview with Phiri, Mukobeko Maximum Security Prison, September 29, 2009.
[258]PRISCCA, ARASA, and Human Rights Watch interview with Isaac, Mukobeko Maximum Security Prison, September 29, 2009.
[259] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[260] Joint United Nations Programme on HIV/AIDS (UNAIDS), “WHO Guidelines on HIV Infection and AIDS in Prisons,” UNAIDS Best Practice Collection, 1993, http://data.unaids.org/Publications/IRC-pub01/JC277-WHO-Guidel-Prisons_en.pdf (accessed March 3, 2010), pp. 7-8.
[261] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[262] PRISCCA, ARASA, and Human Rights Watch interview with DP-06-01, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-02, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-03, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-04, Lusaka Central Prison, February 6, 2010.
[263] Centers for Disease Control and Prevention, “Tuberculosis (TB): Testing & Diagnosis,” undated, http://www.cdc.gov/tb/topic/testing/default.htm (accessed March 1, 2010); Centers for Disease Control and Prevention, “Tuberculosis (TB): Diagnosis of Tuberculosis Disease,” undated, http://www.cdc.gov/tb/publications/factsheets/testing/diagnosis.htm (accessed March 1, 2010).
[264] PRISCCA, ARASA, and Human Rights Watch interview with DP-06-01, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-02, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-03, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-04, Lusaka Central Prison, February 6, 2010.
[265] PRISCCA, ARASA, and Human Rights Watch interview with Henry Mutabala, medical officer, Mukobeko Maximum Security Prison, September 29, 2009.
[266]PRISCCA, ARASA, and Human Rights Watch interview with Muntala, Lusaka Central Prison, October 4, 2009.
[267]PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi Prison, October 6, 2009.
[268] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Helen Ayles, ZAMBART, February 9, 2010; PRISCCA, ARASA, and Human Rights Watch interview with Dr. Nathan Kapata, Ministry of Health, February 8, 2010.
[269]Multidrug-resistant TB is defined as tuberculosis caused by Mycobacterium tuberculosis resistant in vitro to the effects of isoniazid and rifampicin, the two most powerful anti-TB drugs, with or without resistance to any other drugs. World Health Organization, “Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis,” 2006, http://whqlibdoc.who.int/publications/2006/9241546956_eng.pdf (accessed March 3, 2010), p.1.
[270]Ibid., p. ix
[271]Ibid., p.16.
[272] World Health Organization and International Committee for the Red Cross, “Tuberculosis Control in Prisons: A Manual for Programme Managers,” 2002, http://whqlibdoc.who.int/hq/2000/WHO_CDS_TB_2000.281.pdf (accessed March 3, 2010), p. 15.
[273] One of six classes of drugs not used in the standard regimen of treatment for TB, to which resistance may have developed.
[274]World Health Organization, “Guidelines for the Programmatic Management of Drug-Resistant Tuberculosis,” p. 9.
[275] PRISCCA, ARASA, and Human Rights Watch interview with nurse, Lusaka Central Prison, October 3, 2009.
[276] Ibid.
[277] Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 18.
[278] Prisons Rules, sec. 108.
[279] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Nathan Kapata, Ministry of Health, February 8, 2010.
[280] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[281] Ibid.
[282] Advisory Council for the Elimination of Tuberculosis, “Prevention and Control of Tuberculosis in Correctional Facilities Recommendations of the Advisory Council for the Elimination of Tuberculosis,” MMWR, vol. 45(RR-8), June 7, 1996, pp. 1-27.
[283] Ibid.
[284] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[285] PRISCCA, ARASA, and Human Rights Watch interview with Henry Mutabale, medical officer, Mukobeko Maximum Security Prison, September 29, 2009.
[286] PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[287] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[288]PRISCCA, ARASA, and Human Rights Watch interview with Augustine, Mukobeko Maximum Security Prison, September 29, 2009.
[289] PRISCCA, ARASA, and Human Rights Watch interview with CM-03-05, Lusaka Central Prison, October 3, 2009.
[290] PRISCCA, ARASA, and Human Rights Watch interview with Kachinga, Lusaka Central Prison, February 6, 2010.
[291] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[292] PRISCCA, ARASA, and Human Rights Watch interview with clinical officer, Lusaka Prison Clinic, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, February 6, 2010.
[293] World Health Organization, “WHO Guidelines on HIV Infection and AIDS in Prisons,” UNAIDS Best Practice Collection, September 1999, http://www.who.int/hiv/idu/WHO-Guidel-Prisons_en.pdf (accessed March 1, 2010).
[294] United Nations Office on Drugs and Crime (UNODC), World Health Organization and the Joint United Nations Programme on HIV/AIDS (UNAIDS), “HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings: A Framework for an Effective National Response,” 2006, http://data.unaids.org/pub/Report/2006/20060701_hiv-aids_prisons_en.pdf (accessed March 1, 2010).
[295] Email communication from Fredrick Mulenga Chitangala, director of programs, Chreso Ministries ART/VCT Clinic, to PRISCCA, ARASA, and Human Rights Watch, February 17, 2010.
[296] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[297] Republic of Zambia, Ministry of Health, “National HIV/AIDS/STI/TB Policy,” January 2005, pp. 29-30.
[298] PRISCCA, ARASA, and Human Rights Watch interview with Grace Mubanga, female officer in charge, Kamfinsa Prison, October 2, 2009.
[299] PRISCCA, ARASA, and Human Rights Watch interview with Joyce Simukali, prison officer, Kamfinsa Prison (Women’s), October 2, 2009.
[300] PRISCCA, ARASA, and Human Rights Watch interview with Felix Mwanza, TALC, October 15, 2009. Since 2000, PRISCCA has been operating at Lusaka Central, and has conducted HIV education and sensitization in each of the six prisons we visited. PRISCCA, ARASA, and Human Rights Watch interview with Godfrey Malembeka, executive director, PRISCCA, Johannesburg, November 23, 2009.
[301]PRISCCA, ARASA, and Human Rights Watch interview with Orbed, Mukobeko Maximum Security Prison, September 30, 2009.
[302]PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009.
[303] PRISCCA, ARASA, and Human Rights Watch interview with Allan, Mukobeko Maximum Security Prison, September 29, 2009.
[304]PRISCCA, ARASA, and Human Rights Watch interview with Paul, Mukobeko Maximum Security Prison, September 29, 2009.
[305] PRISCCA, ARASA, and Human Rights Watch interview with Godfrey Malembeka, executive director, PRISCCA, November 23, 2009.
[306] Email communication from Dr. Stewart Reid, CIDRZ, to PRISCCA, ARASA, and Human Rights Watch, March 1, 2010.
[307] World Health Organization, “Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach,” 2006, http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf (accessed March 4, 2010), p. 70.
[308] Ibid.
[309] Zambia Prisons Service, “HIV & AIDS/STI/TB Workplace Policy,” p. 23.
[310] World Health Organization, “Nutrient Requirements of People Living with HIV/AIDS: Report of a Technical Consultation, Geneva, Switzerland, 13-15 May 2003,” 2003, http://whqlibdoc.who.int/publications/2003/9241591196.pdf (accessed March 1, 2010).
[311] PRISCCA, ARASA, and Human Rights Watch interview with Willard, Mukobeko Maximum Security Prison, September 29, 2009.
[312] PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009.
[313] PRISCCA, ARASA, and Human Rights Watch interview with Emmanuel, Mukobeko Maximum Security Prison, September 30, 2009.
[314] PRISCCA, ARASA, and Human Rights Watch interview with Augustine, Mukobeko Maximum Security Prison, September 29, 2009.
[315]PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi prison, October 6, 2009.
[316] PRISCCA, ARASA, and Human Rights Watch interview with Joyce Simukali, prison officer, Kamfinsa Prison (Women’s Side), October 2, 2009.
[317] PRISCCA, ARASA, and Human Rights Watch interview with nurse, Lusaka Central Prison clinic, October 3, 2009.
[318] PRISCCA, ARASA, and Human Rights Watch interview with Annie Sabuni, HIV/AIDS coordinator, Lusaka Central Prison, October 3, 2009.
[319] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Choma Prison, October 8, 2009.
[320] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[321] Ibid.
[322] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Lusaka Central Prison, October 3, 2009.
[323] PRISCCA, ARASA, and Human Rights Watch interview with nurse, Lusaka Central Prison clinic, October 3, 2009.
[324] PRISCCA, ARASA, and Human Rights Watch interview with social welfare worker, Lusaka Central Prison, October 3, 2009.
[325] Zambia Ministry of Health and National AIDS Council, “Zambia Country Report: Multi-Sectoral AIDS Response Monitoring and Evaluation Biennial Report 2006-2007: Update Version, Submitted to the United Nations General Assembly Special Session on AIDS,” January 31, 2008, p. 4.
[326] Zambia Prisons Service, “Draft Operational Plan,” 2008, p. 16.
[327] UNAIDS, “WHO Guidelines on HIV Infection and AIDS in Prisons,” UNAIDS Best Practice Collection, 1993, http://data.unaids.org/Publications/IRC-pub01/JC277-WHO-Guidel-Prisons_en.pdf (accessed March 3, 2010), p. 5. WHO, UNAIDS, UNODC, “Policy Brief: Reduction of HIV Transmission in Prisons,” Doc. No. WHO/HIV/2004.05 (2004), p. 2.
[328] WHO, UNODC, UNAIDS, “Interventions to Address HIV in Prisons: Prevention of Sexual Transmission,” 2007, p. 13.
[329] “The failure to provide inmates with the means to protect themselves against HIV and AIDS and other infectious diseases is seen to be an infringement of their basic rights. Measures to protect staff and inmates against HIV and other infectious diseases are therefore needed urgently.” Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 2.
[330] Oscar O. Simooya, “Acceptability of Condoms for HIV/AIDS Prevention in an African Jail,” BMJ, June 6, 2000. O. Simooya et al., “Sexual Behavior and Issues of HIV/AIDS Prevention in an African Prison,” AIDS, pp. 1388-89.
[331] Statement made by Chisela Chileshe at NAC National HIV Prevention Conference, November 3-5, 2009.
[332] PRISCCA, ARASA, and Human Rights Watch interview with LGBT rights organization, Lusaka, October 14, 2009.
[333] As Human Rights Watch has reported, Zambian “sodomy laws” are a result of nineteenth-century British colonial legislative impulse towards social and sexual control of their subject populations in Asia and Africa. See the Human Rights Watch report “This Alien Legacy: The Origins of ‘Sodomy Laws’ in British Colonialism” for an exploration of the imposition of sexual and social regulation laws on former British colonies, http://www.hrw.org/en/reports/2008/12/17/alien-legacy.
[334]Penal Code Act, Laws of Zambia, vol. 7, chapter 87, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 155.
[335] Ibid., art. 158.
[336] PRISCCA, ARASA, and Human Rights Watch interview with LGBT rights organization, October 14, 2009.
[337] Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 16.
[338]PRISCCA, ARASA, and Human Rights Watch interview with Elijah, Mukobeko Maximum Security Prison, September 30, 2009.
[339]PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009.
[340]PRISCCA, ARASA, and Human Rights Watch interview with KT-08-01, Choma Prison, October 8, 2009.
[341]PRISCCA, ARASA, and Human Rights Watch interview with Albert, Lusaka Central Prison, October 3, 2009.
[342]PRISCCA, ARASA, and Human Rights Watch interview with Japhet, Mumbwa Prison, October 5, 2009.
[343] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[344] PRISCCA, ARASA, and Human Rights Watch interview with Sergeant Kabukabu, prison officer, Mumbwa Prison, October 5, 2009.
[345] PRISCCA, ARASA, and Human Rights Watch interview with Mwamba, Mwembeshi Prison, October 6, 2009.
[346] PRISCCA, ARASA, and Human Rights Watch interview with Yutamu Lungu, chief medical inspector, Kamfinsa Prison, October 1, 2009.
[347] Ibid.
[348]PRISCCA, ARASA, and Human Rights Watch interview with Howard, Mukobeko Maximum Security Prison, September 30, 2009.
[349]PRISCCA, ARASA, and Human Rights Watch interview with Lawrence, Mukobeko Maximum Security Prison, September 30, 2009.
[350]PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009.
[351] PRISCCA, ARASA, and Human Rights Watch interview with RS-01-13, Kamfinsa Prison, October 1, 2009.
[352] PRISCCA, ARASA, and Human Rights Watch interview with Clifford, Kamfinsa Prison, October 1, 2009.
[353] PRISCCA, ARASA, and Human Rights Watch interview with Henry Mutabala, medical officer, Mukobeko Maximum Security Prison, September 29, 2009.
[354] PRISCCA, ARASA, and Human Rights Watch interview with Daniel, Mukobeko Maximum Security Prison, September 30, 2009.
[355] PRISCCA, ARASA, and Human Rights Watch interview with Grief Chisenga, prison officer, Mwembeshi Prison, October 6, 2009.
[356] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[357] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[358]PRISCCA, ARASA, and Human Rights Watch interview with Emmanuel, Mukobeko Maximum Security Prison, September 30, 2009.
[359]PRISCCA, ARASA, and Human Rights Watch Watch interview with Norah, Kamfinsa Prison, October 1, 2009.
[360] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Lusaka Central Prison, February 6, 2010.
[361]PRISCCA, ARASA, and Human Rights Watch interview with Chanda, Mukobeko Maximum Security Prison, September 30, 2009.
[362]PRISCCA, ARASA, and Human Rights Watch interview with Douglas, Mukobeko Maximum Security Prison, September 29, 2009.
[363] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[364] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[365] PRISCCA, ARASA, and Human Rights Watch interview with nurse, Lusaka Central Prison, October 3, 2009.
[366]PRISCCA, ARASA, and Human Rights Watch interview with Clifford, Kamfinsa Prison, October 1, 2009.
[367]PRISCCA, ARASA, and Human Rights Watch interview with Rodgers, Lusaka Central Prison, October 3, 2009.
[368] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[369] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009.
[370] PRISCCA, ARASA, and Human Rights Watch interview with B.M. Hambwalou, medical officer, Choma prison, October 8, 2009.
[371] PRISCCA, ARASA, and Human Rights Watch interview with Henry Mutabale, medical officer, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[372] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[373] PRISCCA, ARASA, and Human Rights Watch interview with Ms. Kaluba, offender management officer, Mwembeshi Prison, October 6, 2009.
[374]PRISCCA, ARASA, and Human Rights Watch interview with Felix, Mukobeko Maximum Security Prison, September 29, 2009.
[375] PRISCCA, ARASA, and Human Rights Watch interview with DP-06-01, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-02, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-03, Lusaka Central Prison, February 6, 2010; PRISCCA, ARASA, and Human Rights Watch interview with DP-06-04, Lusaka Central Prison, February 6, 2010.
[376] PRISCCA, ARASA, and Human Rights Watch interview with DP-06-03, Lusaka Central Prison, February 6, 2010.
[377] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[378] According to Médecins Sans Frontières, “ As people on antiretroviral treatment (ART) develop intolerable side effects or start to develop resistance to their first set of antiretroviral medicines (ARVs), they need to switch to a different drug combination. Compliance to treatment is important to prevent viral resistance, which will allow the HIV virus to replicate and mutate. In one of MSF’s long-standing HIV/AIDS projects, in Khayelitsha, South Africa, 16 percent of patients need to be switched to ‘second-line’ therapy after five years of treatment. Indeed, in wealthy countries, many people living with AIDS have changed their treatment lines four, five or even six times. With two million people on ARVs across the developing world, the need for access to newer ARV options is growing rapidly.” Médecins Sans Frontières, “Need for Newer Drugs,” July 2009, http://www.msfaccess.org/main/hiv-aids/introduction-to-hivaids/need-for-newer-drugs/ (accessed March 2, 2010).
[379]PRISCCA, ARASA, and Human Rights Watch interview with Mwape, Mukobeko Maximum Security Prison, September 29, 2009.
[380] PRISCCA, ARASA, and Human Rights Watch interview with Mutale, Mukobeko Maximum Security Prison, September 30, 2009.
[381]PRISCCA, ARASA, and Human Rights Watch interview with Chrispine, Kamfinsa Prison, October 1, 2009.
[382]PRISCCA, ARASA, and Human Rights Watch interview with Frederick, Mwembeshi Prison, October 6, 2009.
[383] PRISCCA, ARASA, and Human Rights Watch interview with Misheck, Mukobeko Maximum Security Prison, September 30, 2009.
[384] Dr. Chileshe confirmed that when remandees are referred to the hospital, they are handcuffed to the bed. PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[385] PRISCCA, ARASA, and Human Rights Watch interview with Chanda, Mukobeko Maximum Security Prison, September 30, 2009.
[386] PRISCCA, ARASA, and Human Rights Watch interview with Henry, Lusaka Central Prison, October 4, 2009.
[387] PRISCCA, ARASA, and Human Rights Watch interview with emergency nurse, University Teaching Hospital, Lusaka, February 7, 2010.
[388]PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009.
[389]PRISCCA, ARASA, and Human Rights Watch interview with MM-29-08, Mukobeko Maximum Security Prison, September 29, 2009.
[390]PRISCCA, ARASA, and Human Rights Watch interview with Nickson, Mukobeko Maximum Security Prison, September 30, 2009.
[391]PRISCCA, ARASA, and Human Rights Watch interview with Chiluba, Lusaka Central Prison, October 4, 2009.
[392] PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[393] Prisons Act, sec. 61(1).
[394] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[395] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[396] PRISCCA, ARASA, and Human Rights Watch interview with Semba, Mumbwa Prison, October 5, 2009.
[397]PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009.
[398]PRISCCA, ARASA, and Human Rights Watch interview with Johnston, Mumbwa Prison, October 5, 2009.
[399]PRISCCA, ARASA, and Human Rights Watch interview with Ngosa, Kamfinsa Prison, October 1, 2009.
[400]PRISCCA, ARASA, and Human Rights Watch interview with Angela, Lusaka Central Prison, October 4, 2009.
[401] PRISCCA, ARASA, and Human Rights Watch interview with Mwizya, Mukobeko Maximum Security Prison, September 30, 2009.
[402] PRISCCA, ARASA, and Human Rights Watch interview with RS-01-09, Kamfinsa Prison, October 1, 2009.
[403]PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Mwembeshi Prison, October 6, 2009.
[404]PRISCCA, ARASA, and Human Rights Watch interview with Martin, Mumbwa Prison, October 5, 2009.
[405]PRISCCA, ARASA, and Human Rights Watch interview with Elijah, Mukobeko Maximum Security Prison, September 30, 2009.
[406] PRISCCA, ARASA, and Human Rights Watch interview with Jean Marie, Lusaka Central Prison, October 3, 2009.
[407] PRISCCA, ARASA, and Human Rights Watch interview with Tweedman Hamunyanga, intelligence/offender management officer, Choma prison, October 8, 2009.
[408] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[409] PRISCCA, ARASA, and Human Rights Watch interview with Henry Mutabale, medical officer, Mukobeko Maximum Security Prison, September 29, 2009.
[410] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[411] Prisons Act, sec. 18. See also UN Standard Minimum Rules for the Treatment of Prisoners, paras. 24-25; Body of Principles, prin. 24.
[412] PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[413] Ibid.
[414]PRISCCA, ARASA, and Human Rights Watch interview with Lawrence, Mukobeko Maximum Security Prison, September 30, 2009.
[415] See, e.g., John Mayeya et al., “Zambia Mental Health Country Profile,” International Review of Psychiatry, vol. 16, February 2004, pp. 63-72.
[416] Zambia Prisons Service, “Zambia Prisons Service HIV and AIDS/STI/TB Strategic Plan (2007-2010),” p. 7.
[417] UN Standard Minimum Rules for the Treatment of Prisoners, para. 62; see also paras. 82-83.
[418] PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, February 6, 2010.
[419] PRISCCA, ARASA, and Human Rights Watch tour of Lusaka Central Prison clinic, February 6, 2010.
[420] PRISCCA, ARASA, and Human Rights Watch interview with James, Mukobeko Maximum Security Prison, September 30, 2009.
[421] PRISCCA, ARASA, and Human Rights Watch interview with RS-30-03, Mukobeko Maximum Security Prison, September 30, 2009.
[422] See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with RS-30-03, Mukobeko Maximum Security Prison, September 30, 2009.
[423] UNODC and UNAIDS, “Women and HIV in Prison Settings,” September 2008, http://www.unodc.org/documents/hiv-aids/Women%20and%20HIV%20in%20prison%20settings.pdf (accessed March 3, 2010), p. 2. See also Vetten, “The Imprisonment of Women in Africa,” in Sarkin, ed., Human Rights in African Prisons.
[424] Brenda J. van den Bergh, Alex Gatherer and Lars F. Møller, “Women’s Health in Prison: Urgent Need for Improvement in Gender Equity and Social Justice,” Bulletin of the World Health Organization, vol. 87, 2009, p. 406.
[425] UN Standard Minimum Rules for the Treatment of Prisoners, para. 23.
[426] The UN Population Fund has reported that between 72 and 90 percent of women in Zambia’s general population receive prenatal care. UN Population Fund, “Recognizing the Needs in Zambia,” undated, http://www.unfpa.org/fistula/docs/eng_zambia.pdf (accessed March 2, 2010).
[427]PRISCCA, ARASA, and Human Rights Watch interview with Helen, Lusaka Central Prison, October 4, 2009.
[428] PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-01, Lusaka Central Prison, October 3, 2009.
[429] World Health Organization, “Rapid Advice: Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Inmates,” November 2009, http://www.who.int/hiv/pub/mtct/rapid_advice_mtct.pdf (accessed March 3, 2010), p. 13.
[430] PRISCCA, ARASA, and Human Rights Watch interview with Yutamu Lungu, chief medical inspector, Kamfinsa Prison, October 1, 2009.
[431]PRISCCA, ARASA, and Human Rights Watch interview with Tasila, Kamfinsa Prison, October 1, 2009.
[432] PRISCCA, ARASA, and Human Rights Watch interview with Dr. Chisela Chileshe, February 6, 2010.
[433] World Health Organization, UNAIDS, and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: 2008 Update: Zambia.”
[434] PRISCCA, ARASA, and Human Rights Watch interview with Beatrice Munankopa, deputy officer in charge, Lusaka Central Prison (Women’s), October 4, 2009.
[435] Center for Infectious Disease Research in Zambia (CIDRZ), “Cervical Cancer Screening,” undated, http://www.cidrz.org/cervical_cancer_screening (accessed March 3, 2010).
[436] PRISCCA, ARASA, and Human Rights Watch interview with Angela, Lusaka Central Prison, October 4, 2009.
[437] PRISCCA, ARASA, and Human Rights Watch interview with Inonge, Lusaka Central Prison, October 3, 2009.
[438] PRISCCA, ARASA, and Human Rights Watch interview with Isaac, Mukobeko Maximum Security Prison, September 29, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison,
[439] PRISCCA, ARASA, and Human Rights Watch interview with Mulenga, Mukobeko Maximum Security Prison, September 30, 2009.
[440] PRISCCA, ARASA, and Human Rights Watch interview with Paul Swala, Prison Fellowship of Zambia, October 15, 2009.
[441] Ibid.
[442] PRISCCA, ARASA, and Human Rights Watch interview with Gabriel, former prisoner, Lusaka, February 5, 2010.
[443] PRISCCA, ARASA, and Human Rights Watch interview with clinical officer, Lusaka Central prison clinic, February 6, 2010.
[444] PRISCCA, ARASA, and Human Rights Watch interview with Aaron, Choma Prison, October 8, 2009.
[445] PRISCCA, ARASA, and Human Rights Watch interview with Misheck, Mukobeko Maximum Security Prison, September 30, 2009.
[446] PRISCCA, ARASA, and Human Rights Watch interview with Donald Mwandila, Hospital Admin, Zambia Police Service Medical Directorate, Lusaka, February 4, 2010; PRISCCA, ARASA, and Human Rights Watch interview with K.N. Chikwanda, staff officer medical, Zambia Police Service Medical Directorate, Lusaka, February 4, 2010.
[447]PRISCCA, ARASA, and Human Rights Watch telephone interview with Dr. Chisela Chileshe, October 13, 2009.
[448] PRISCCA, ARASA, and Human Rights Watch interview with RS-30-03, Mukobeko Maximum Security Prison, September 30, 2009.
[449] PRISCCA, ARASA, and Human Rights Watch interview with Robby Shabwanga, projects officer, Legal Resources Foundation, October 14, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Angela, Lusaka Central Prison, October 4, 2009 (“They don’t open the door in the cell at night for anything. There are no windows, no air. Someone who was 28 years old died at night in her cell and they didn’t open the door until the morning.”)
[450] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[451] Prisons Act, sec. 22.
[452] Body of Principles, prin. 34.
[453]The officer in charge at Mukobeko reported that there had been four inmate deaths in the previous month and 10 inmate deaths in 2008 at the time of our visit, 40 percent of which were attributable to TB. PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009. At Kamfinsa, the officer in charge said that there had been two deaths in 2009 until October, four in 2008, all from HIV/AIDS. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009. At Mumbwa Prison, the officer in charge reported that three deaths had occurred in 2009, and one in 2008, all from HIV/AIDS and TB. PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009. At Choma prison, the officer in charge reported to us that in 2009 there had been two inmate deaths from TB and HIV/AIDS-related illness and a short illness, respectively. In 2006, HIV/AIDS was the leading cause of death. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[454]PRISCCA, ARASA, and Human Rights Watch interview with Jacob, Mwembeshi Prison, October 6, 2009.
[455]PRISCCA, ARASA, and Human Rights Watch interview with Febian, Mumbwa Prison, October 5, 2009.
[456]PRISCCA, ARASA, and Human Rights Watch interview with Clive, Mwembeshi Prison, October 6, 2009.
[457] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[458]PRISCCA, ARASA, and Human Rights Watch interview with Rabun, Mwembeshi Prison, October 6, 2009.
[459]PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi Prison, October 6, 2009.
[460] UDHR, art. 5; ICCPR, art. 7; Convention on the Rights of the Child, article 37; Convention Against Torture, arts. 11 and 16; Body of Principles, prins. 1 and 6; Code of Conduct for Law Enforcement Officials, para. 5; Constitution of Zambia, art. 15. Juveniles are particularly protected. The Beijing Rules, para. 17.3.
[461] UN Human Rights Committee, “Concluding Observations of the Human Rights Committee: Zambia,” U.N. Doc. CCPR/C/79/Add.62 ( 1996), http://www.unhcr.org/refworld/type,CONCOBSERVATIONS,,ZMB,3ae6b0324,0.html (accessed March 3, 2010), para. 12.
[462] UN Human Rights Committee, “Concluding Observations of the Human Rights Committee: Zambia,” U.N. Doc. CCPR/C/ZMB/CO/3 (2007), http://www.unhcr.org/refworld/country,,,CONCOBSERVATIONS,ZMB,456d621e2,46d277762,0.html (accessed March 3, 2010), para. 20.
[463] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 28-32.
[464] UN Human Rights Committee, Communication No. 1184/2003: Australia 27/04/2006, March 2006, para. 9.4.
[465] Prisons Act, sec. 90-94.
[466] Criminal Procedure Code (Amendment) Act No. 9 of 2003; Penal Code (Amendment) Act No. 10 of 2003; Prisons (Amendment) Act No. 16 of 2004.
[467] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 35-36.
[468] At the time of our visit, the penal block was non-operational at Lusaka Central, Mumbwa and Choma.
[469] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[470] Prisons Act, secs. 95 and 97-98.
[471] Prisons Rules, secs. 40(1)(b) and 170; UN Standard Minimum Rules for the Treatment of Prisoners, para. 32(1).
[472] PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Aaron, Choma Prison, October 8, 2009; PRISCCA, ARASA, and Human Rights Watch interview with MM-05-04, Mumbwa Prison, October 5, 2009.
[473] Inmates at Mukobeko reported that inmates are held in the penal block up to 30 days. PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Elijah, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Mutale, Mukobeko Maximum Security Prison, September 30, 2009. Inmates at other facilities reported shorter maximum periods in the penal block. PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009 (five days); PRISCCA, ARASA, and Human Rights Watch interview with Albert, Lusaka Central Prison, October 3, 2009 (one day); PRISCCA, ARASA, and Human Rights Watch interview with Rodgers, Lusaka Central Prison, October 3, 2009 (one week); PRISCCA, ARASA, and Human Rights Watch interview with Andrew, Mumbwa Prison, October 5, 2009 (one day); PRISCCA, ARASA, and Human Rights Watch interview with Ngwila, Choma Prison, October 8, 2009 (three days); PRISCCA, ARASA, and Human Rights Watch interview with Anderson, Choma Prison, October 8, 2009 (one day); PRISCCA, ARASA, and Human Rights Watch interview with Aaron, Choma Prison, October 8, 2009 (three days); PRISCCA, ARASA, and Human Rights Watch interview with Tasila, Choma Prison, October 8, 2009 (three days); PRISCCA, ARASA, and Human Rights Watch interview with KT-08-04, Choma Prison, October 8, 2009 (one day); PRISCCA, ARASA, and Human Rights Watch interview with Peter, Choma Prison, October 8, 2009 (one week).
[474] PRISCCA, ARASA, and Human Rights Watch interview with Douglas, Mukobeko Maximum Security Prison, September 29, 2009. By contrast, the penal diet prescribed by Zambian law takes quite a different form. Penal diet consists of 454 grams of maize meal, millet meal or bread, salt, and unlimited water. Prisons Rules, “Prison Rations: Part II.” Reduced diet consists of 340 grams of maize meal, millet meal, brad, or porridge, fresh vegetables, beans or cheese, oil, salt, and unlimited water. Prisons Rules, “Prison Rations: Part III.”
[475] PRISCCA, ARASA, and Human Rights Watch interview with Henry, Lusaka Central Prison, October 4, 2009.
[476] PRISCCA, ARASA, and Human Rights Watch interview with Bernard, Mukobeko Maximum Security Prison, September 29, 2009.
[477] See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Douglas, Mukobeko Maximum Security Prison, September 29, 2009.
[478] PRISCCA, ARASA, and Human Rights Watch interview with Lawrence, Mukobeko Maximum Security Prison, September 30, 2009.
[479] PRISCCA, ARASA, and Human Rights Watch interview with Mumbwa, Mukobeko Maximum Security Prison, September 30, 2009.
[480] PRISCCA, ARASA, and Human Rights Watch interview with Orbed, Mukobeko Maximum Security Prison, September 30, 2009.
[481] PRISCCA, ARASA, and Human Rights Watch interview with Winston, Mukobeko Maximum Security Prison, September 29, 2009.
[482] PRISCCA, ARASA, and Human Rights Watch interview with Francis Kasanga, deputy officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[483] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[484] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009.
[485] PRISCCA, ARASA, and Human Rights Watch interview with Chris, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Patrick, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Aaron, Choma Prison, October 8, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with RS-29-04, Mukobeko Maximum Security Prison, September 29, 2009.
[486] PRISCCA, ARASA, and Human Rights Watch interview with Samuel, Kamfinsa Prison, October 1, 2009.
[487] PRISCCA, ARASA, and Human Rights Watch interview with Mutale, Mukobeko Maximum Security Prison, September 30, 2009.
[488] PRISCCA, ARASA, and Human Rights Watch interview with Henry, Lusaka Central Prison, October 4, 2009.
[489] PRISCCA, ARASA, and Human Rights Watch interview with Patrick, Kamfinsa Prison, October 1, 2009.
[490] PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison, October 3, 2009.
[491] PRISCCA, ARASA, and Human Rights Watch interview with KT-04-01, Lusaka Central Prison, October 4, 2009 (“The guards used to ask other inmates to beat people, but we complained to the Human Rights Commission and it stopped. They fear we will tell the outside, so it has stopped.”).
[492] PRISCCA, ARASA, and Human Rights Watch interview with KT-29-03, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Nickson, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Reynard, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-01, Kamfinsa Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-04-07, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-04-06, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-04, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Catherine, Lusaka Central Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Festus, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Clive, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Choma Prison, October 8, 2009.
[493] Juveniles at Mukobeko reported being made to draw water for the TB patients as punishment. PRISCCA, ARASA, and Human Rights Watch interview with Chris, Mukobeko Maximum Security Prison, September 29, 2009. A female prisoner at Kamfinsa reported digging and weeding as punishment for fighting. PRISCCA, ARASA, and Human Rights Watch interview with NCI-02-01, Kamfinsa Prison, October 2, 2009. Men at Lusaka Central reported manual work as punishment including cleaning toilets and sweeping. PRISCCA, ARASA, and Human Rights Watch interview with Rodgers, Lusaka Central Prison, October 3, 2009. Others reported having to dig pit latrines or sweep. Female inmates at Lusaka Central reported having to water the plants and to clean the toilets as punishment for refusing to dance as part of newcomer orientation rituals. PRISCCA, ARASA, and Human Rights Watch interview with KT-04-04, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Annie, Lusaka Central Prison, October 4, 2009.
[494] The UN Standard Minimum Rules for the Treatment of Prisoners specify that “[t]here shall be no discrimination on grounds of race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status.” UN Standard Minimum Rules for the Treatment of Prisoners, para. 6(1). See also Body of Principles, prin. 5 (“These principles shall be applied to all persons within the territory of any given State, without distinction of any kind, such as race, colour, sex, language, religion or religious belief, political or other opinion, national, ethnic or social origin, property, birth or other status.”); Basic Principles for the Treatment of Prisoners, prin. 2 (“There shall be no discrimination on the grounds of race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status.”).
[495] PRISCCA, ARASA, and Human Rights Watch interview with Mary, Lusaka Central Prison, October 4, 2009.
[496] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[497] PRISCCA, ARASA, and Human Rights Watch interview with Joyce Simukali, prison officer, Kamfinsa Prison (Women’s), October 2, 2009.
[498] PRISCCA, ARASA, and Human Rights Watch interview with Beatrice Munankopa, deputy officer in charge, Lusaka Central Prison, October 4, 2009.
[499] In 2007, the UN Human Rights Committee, in its concluding observations in Zambia, welcomed the abolition of corporal punishment through amendments to the Penal Code, Criminal Procedure Code, the Prisons Act, and the Education Act but regretted lack of information on the practical implementation of this abolition. UN Human Rights Committee, “Concluding Observations of the Human Rights Committee: Zambia,” 2007, p.2. The Committee on the Rights of the Child in 2003 remained “concerned that corporal punishment is still practised and accepted in schools, families, and care and juvenile detention institutions.” Committee on the Rights of the Child, “Concluding Observations: Zambia,” U.N. Doc. CRC/C/15/Add.206 (2003), http://www.unhchr.ch/tbs/doc.nsf/898586b1dc7b4043c1256a450044f331/1a481056be1936eac1256da5004d40ea/$FILE/G0342771.pdf (accessed March 3, 2010), para. 56.
[500] PRISCCA, ARASA, and Human Rights Watch interview with Gerald, Mukobeko Maximum Security Prison, September 30, 2009.
[501] PRISCCA, ARASA, and Human Rights Watch interview with Ngwila, Choma Prison, October 8, 2009.
[502] PRISCCA, ARASA, and Human Rights Watch interview with Clifford, Kamfinsa Prison, October 1, 2009.
[503] PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009.
[504] PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-02, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-01-04, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-02-01, Kamfinsa Prison, October 2, 2009.
[505] PRISCCA, ARASA, and Human Rights Watch interview with NCI-02-01, Kamfinsa Prison, October 2, 2009.
[506] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Jacob, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Clive, Mwembeshi Prison, October 6, 2009.
[507] PRISCCA, ARASA, and Human Rights Watch interview with David, Lusaka Central Prison, October 3, 2009.
[508] PRISCCA, ARASA, and Human Rights Watch interview with Erick, Lusaka Central Prison, October 3, 2009.
[509] PRISCCA, ARASA, and Human Rights Watch interview with Ngosa, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Norah, Kamfinsa Prison, October 1, 2009.
[510] PRISCCA, ARASA, and Human Rights Watch interview with Ngosa, Kamfinsa Prison, October 1, 2009.
[511] PRISCCA, ARASA, and Human Rights Watch interview with Annie, Lusaka Central Prison, October 4, 2009.
[512] PRISCCA, ARASA, and Human Rights Watch interview with Agnes, Kamfinsa Prison, October 1, 2009.
[513] PRISCCA, ARASA, and Human Rights Watch interview with KT-08-02, Choma Prison, October 8, 2009.
[514] PRISCCA, ARASA, and Human Rights Watch interview with KT-08-01, Choma Prison, October 8, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-08-03, Choma Prison, October 8, 2009.
[515] PRISCCA, ARASA, and Human Rights Watch interview with Ngosa, Kamfinsa Prison, October 1, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Catherine, Lusaka Central Prison, October 4, 2009 (“it make me feel very bad”).
[516] PRISCCA, ARASA, and Human Rights Watch interview with Tandiwe, Lusaka Central Prison, October 4, 2009.
[517] PRISCCA, ARASA, and Human Rights Watch interview with Beatrice Munankopa, deputy officer in charge, Lusaka Central Prison, October 4, 2009.
[518] Prisons Rules, sec. 155; Prisons Act, sec. 5(2). See also UN Standard Minimum Rules for the Treatment of Prisoners, para. 28(1).
[519] PRISCCA, ARASA, and Human Rights Watch interview with Luc, Lusaka Central Prison, October 4, 2009.
[520] At Mukobeko Maximum Security Prison, 72 officers oversee 1731 prisoners, an officer-to-inmate ratio of one to 24. PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009. At Kamfinsa, the staff-to-inmate ratio is one to 12. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009. At Lusaka Central, the officer in charge reported 116 staff members for a population of 1145, a ratio of one to 10. PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009. At Mumbwa, 36 staff members oversee 354 inmates, a ratio of one to 10. PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009. At Mwembeshi, 51 officers supervise 342 inmates, a ratio of one to 7. PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009. At Choma prison, 39 staff members supervise 251 inmates (a ratio of one to 6), a number considered by the officer in charge to be insufficient. PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[521] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[522] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[523] The Prisons Service has made proposals to increase this number and hopes to increase it to 5,000 in the next three to five years. PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[524] Prisons Rules, secs. 117-127.
[525] PRISCCA, ARASA, and Human Rights Watch interview with Godfrey Malembeka, Executive Director of PRISCCA, November 23, 2009.
[526] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Mundianawa, officer in charge, Kamfinsa Prison, October 1, 2009.
[527] PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[528] PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, Mukobeko Maximum Security Prison, September 29, 2009.
[529] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[530] PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009.
[531] PRISCCA, ARASA, and Human Rights Watch interview with Felix, Mukobeko Maximum Security Prison, September 29, 2009.
[532] PRISCCA, ARASA, and Human Rights Watch interview with Orbed, Mukobeko Maximum Security Prison, September 30, 2009.
[533] PRISCCA, ARASA, and Human Rights Watch interview with Chiluba, Lusaka Central Prison, October 4, 2009.
[534] PRISCCA, ARASA, and Human Rights Watch interview with MM-05-04, Mumbwa Prison, October 5, 2009.
[535] PRISCCA, ARASA, and Human Rights Watch interview with Orbed, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Felix, Mukobeko Maximum Security Prison, September 29, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Esther, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Bwalya, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Festus, Mwembeshi Prison, October 6, 2009.
[536] PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with William, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison, October 3, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with MM-05-04, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Adam, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Johnston, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with RS-01-03, Kamfinsa Prison, October 1, 2009.
[537] See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009.
[538] PRISCCA, ARASA, and Human Rights Watch interview with MM-06-06, Mwembeshi Prison, October 6, 2009.
[539] PRISCCA, ARASA, and Human Rights Watch interview with Kennedy, Lusaka Central Prison, October 3, 2009.
[540] PRISCCA, ARASA, and Human Rights Watch interview with Moono, Lusaka Central Prison, October 3, 2009.
[541] PRISCCA, ARASA, and Human Rights Watch interview with Albert, Lusaka Central Prison, October 3, 2009.
[542] PRISCCA, ARASA, and Human Rights Watch interview with Martin, Mumbwa Prison, October 5, 2009.
[543] PRISCCA, ARASA, and Human Rights Watch interview with RS-05-01, Mumbwa Prison, October 5, 2009.
[544] PRISCCA, ARASA, and Human Rights Watch interview with William, Mumbwa Prison, October 5, 2009.
[545] PRISCCA, ARASA, and Human Rights Watch interview with Moses, Lusaka Central Prison, October 3, 2009.
[546] UN Standard Minimum Rules for the Treatment of Prisoners, para. 36.
[547] Prisons Rules, sec. 15.
[548] PRISCCA, ARASA, and Human Rights Watch interview with Febian, Mumbwa Prison, October 5, 2009.
[549] PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mumbwa Prison, October 5, 2009.
[550]PRISCCA, ARASA, and Human Rights Watch interview with Chilua, Lusaka Central Prison, October 4, 2009.
[551]PRISCCA, ARASA, and Human Rights Watch interview with Albert, Lusaka Central Prison, October 3, 2009.
[552] PRISCCA, ARASA, and Human Rights Watch interview with Keith, Mukobeko Maximum Security Prison, September 29, 2009.
[553]PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009.
[554] PRISCCA, ARASA, and Human Rights Watch interview with Luc, Lusaka Central Prison, October 4, 2009.
[555] PRISCCA, ARASA, and Human Rights Watch interview with Chilufya, Mwembeshi Prison, October 6, 2009.
[556] PRISCCA, ARASA, and Human Rights Watch interview with Peter, Choma Prison, October 8, 2009.
[557] PRISCCA, ARASA, and Human Rights Watch interview with Jonathan, Mwembeshi Prison, October 6, 2009.
[558] PRISCCA, ARASA, and Human Rights Watch interview with Mangazi, Mumbwa Prison, October 5, 2009.
[559] See, for example, PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Mangazi, Mumbwa Prison, October 5, 2009.
[560] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[561] PRISCCA, ARASA, and Human Rights Watch interview with D. Mulenga, deputy officer in charge, Mumbwa Prison, October 5, 2009.
[562] UN Standard Minimum Rules for the Treatment of Prisoners, para. 71(1).
[563] Ibid., para. 75.
[564] Prisons Rules, sec. 156(1).
[565] PRISCCA, ARASA, and Human Rights Watch interview with NCI-06-06, Mwembeshi Prison, October 6, 2009.
[566] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mumbwa Prison, October 5, 2009.
[567] PRISCCA, ARASA, and Human Rights Watch interview with Noah, Mumbwa Prison, October 5, 2009.
[568] PRISCCA, ARASA, and Human Rights Watch interview with Chibesa, Mwembeshi Prison, October 6, 2009.
[569] PRISCCA, ARASA, and Human Rights Watch interview with Catherine, Lusaka Central Prison, October 4, 2009.
[570] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[571] PRISCCA, ARASA, and Human Rights Watch interview with Rabun, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with MM-08-07, Choma Prison, October 8, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Festus, Mwembeshi Prison, October 6, 2009.
[572] PRISCCA, ARASA, and Human Rights Watch interview with Mwelwa, Choma Prison, October 8, 2009.
[573] PRISCCA, ARASA, and Human Rights Watch interview with Frederick, Mwembeshi Prison, October 6, 2009.
[574] Prisons Rules, sec. 40(1)(a).
[575]PRISCCA, ARASA, and Human Rights Watch interview with NCI-06-05, Mwembeshi Prison, October 6, 2009.
[576] PRISCCA, ARASA, and Human Rights Watch interview with Semba, Mumbwa Prison, October 5, 2009.
[577] PRISCCA, ARASA, and Human Rights Watch interview with Rabun, Mwembeshi Prison, October 6, 2009; see also KT-06-04, Mwembeshi Prison, October 6, 2009.
[578] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[579] PRISCCA, ARASA, and Human Rights Watch interview with Jacob, Mwembeshi Prison, October 6, 2009; see also PRISCCA, ARASA, and Human Rights Watch interview with Mwamba, Mwembeshi Prison, October 6, 2009.
[580] Prisons Rules, sec. 113.
[581] Ibid., secs. 142 and 143.
[582] Prison Rules, “Third Schedule.”
[583] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[584] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-09, Mwembeshi Prison, October 6, 2009. Prisoners at non-farm prisons who work in carpentry, tailoring, or other workshops also receive no payment for their work. The officer in charge at Mukobeko told us that “in terms of the Act, they are supposed to be paid, but they are paid nothing now, only in colonial times.” PRISCCA, ARASA, and Human Rights Watch interview with George S. Sikaonga, officer in charge, September 29, 2009. The officer in charge at Choma confirmed: “In terms of prison regulations, these prisoners are entitled to payment, but these regulations have not been revisited since colonial times and the monthly entitlement of 30 Ngwe in payment is virtually worthless.” PRISCCA, ARASA, and Human Rights Watch interview with Patrick Chilambe, officer in charge, Choma Prison, October 8, 2009.
[585] PRISCCA, ARASA, and Human Rights Watch interview with MM-06-06, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Gabriel, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Japhet, Mumbwa Prison, October 5, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Mwamba, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Ezekiel, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Rabun, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-09, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-04, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Chilufya, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Linos, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-06-06, Mwembeshi Prison, October 6, 2009.
[586] PRISCCA, ARASA, and Human Rights Watch interview with Chibesa, Mwembeshi Prison, October 6, 2009.
[587] PRISCCA, ARASA, and Human Rights Watch interview with Clifford, Kamfinsa Prison, October 1, 2009.
[588] PRISCCA, ARASA, and Human Rights Watch interview with Kaila, Mumbwa Prison, October 5, 2009.
[589] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Mwembeshi Prison, October 6, 2009.
[590] PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi Prison, October 6, 2009.
[591] PRISCCA, ARASA, and Human Rights Watch interview with MM-06-08, Mwembeshi Prison, October 6, 2009.
[592] PRISCCA, ARASA, and Human Rights Watch interview with Francis, Mwembeshi Prison, October 6, 2009.
[593]PRISCCA, ARASA, and Human Rights Watch interview with Festus, Mwembeshi Prison, October 6, 2009.
[594] PRISCCA, ARASA, and Human Rights Watch interview with Robbie, Mwembeshi Prison, October 6, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Aaron, Choma Prison, October 8, 2009.
[595] PRISCCA, ARASA, and Human Rights Watch interview with Ezekiel, Mwembeshi Prison, October 6, 2009.
[596] PRISCCA, ARASA, and Human Rights Watch interview with Jacob, Mwembeshi Prison, October 6, 2009.
[597] PRISCCA, ARASA, and Human Rights Watch interview with Gideon, Mwembeshi Prison, October 6, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Rabun, Mwembeshi Prison, October 6, 2009.
[598] PRISCCA, ARASA, and Human Rights Watch interview with Mwisa, Choma Prison, October 8, 2009.
[599] PRISCCA, ARASA, and Human Rights Watch interview with NCI-06-06, Mwembeshi Prison, October 6, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Linos, Mwembeshi Prison, October 6, 2009.
[600] UN Human Rights Committee, “Concluding Observations: Zambia,” 2007, para. 23.
[601] PRISCCA, ARASA, and Human Rights Watch interview with J. Kababa, officer in charge, Lusaka Central Prison, October 3, 2009.
[602] Roy Walmsley, “World Pre-Trial/Remand Imprisonment List: World Pre-Trial/Remand Imprisonment List,” King’s College London International Centre for Prison Studies, http://www.kcl.ac.uk/depsta/law/research/icps/downloads/WPTRIL.pdf (accessed March 3, 2010).
[603] See, e.g., ICCPR, art. 9; African Charter, art. 6.
[604] PRISCCA, ARASA, and Human Rights Watch interview with Catherine, Lusaka Central Prison, October 4, 2009.
[605] PRISCCA, ARASA, and Human Rights Watch interview with Angela, Lusaka Central Prison, October 4, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Susan, Lusaka Central Prison, October 4, 2009. International observers have confirmed these findings. The US State department has found that in practice, police rarely obtained warrants for those offenses for which warrants are required (offenses including treason, sedition, defamation of the president, unlawful assembly, or abuse of office are excluded) and police arbitrarily arrested family members of criminal suspects, as well as arresting criminal suspects on inadequate evidence or as a means of extortion. Additionally, “[a]uthorities sometimes detained, interrogated, and physically abused family members of criminal suspects to obtain their cooperation in identifying or locating suspects.” US Department of State, “2008 Human Rights Report: Zambia.” Furthermore, “[p]olice arbitrarily arrested family members of criminal suspects. Criminal suspects were arrested on the basis of insubstantial evidence, uncorroborated accusations, or as a pretext for extortion.” US Department of State, “2009 Human Rights Report: Zambia.”
[606] PRISCCA, ARASA, and Human Rights Watch interview with Donald Mwandila, Hospital Admin, Zambia Police Service Medical Directorate, Lusaka, February 4, 2010; PRISCCA, ARASA, and Human Rights Watch interview with K.N. Chikwanda, staff officer medical, Zambia Police Service Medical Directorate, Lusaka, February 4, 2010.
[607]Criminal Procedure Code Act, Laws of Zambia, vol. 7, chapter 88, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 26.
[608] Narcotic Drugs and Psychotropic Substances Act, Laws of Zambia, vol. 7, chapter 96, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 24.
[609] ICCPR, art. 9; Convention on the Rights of the Child, art. 37(d); The Beijing Rules, rule 10.2; Body of Principles, prins. 10, 11 and 37. See also, African Charter, art. 7. The African Commission on Human and Peoples’ Rights has determined that detaining two applicants, for, respectively, five months and slightly over one month without being brought before a judge violated Charter’s protections on fair trial. African Commission on Human and Peoples’ Rights, Huri-Laws v. Nigeria, Comm. No. 225/98 (2000), http://www1.umn.edu/humanrts/africa/comcases/225-98.html (accessed March 4, 2010). See also Constitution of Zambia, art. 3(b); Criminal Procedure Code Act, sec. 30.
[610] In addition to a requirement a police officer making an arrest without a warrant shall send the person before a magistrate without unnecessary delay, Zambian law requires that “[w]hen any person has been taken into custody without a warrant for an offence other than an offence punishable with death, the officer in charge of the police station to which such person shall be brought may, in any case, and shall, if it does not appear practicable to bring such person before an appropriate competent court within twenty-four hours after he was so taken into custody, inquire into the case, and, unless the offence appears to the officer to be of a serious nature, release the person, on his executing bond, with or without sureties, for a reasonable amount, to appear before a competent court at a time and place to be named in the bond: but, where any person is retained in custody, he shall be brought before a competent court as soon as practicable.” Criminal Procedure Code Act, sec. 33(1).
[611] PRISCCA, ARASA, and Human Rights Watch interview with Rodgers, Lusaka Central Prison, October 3, 2009.
[612] PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison, October 3, 2009.
[613] PRISCCA, ARASA, and Human Rights Watch interview with CM-03-04, Lusaka Central Prison, October 3, 2009.
[614]PRISCCA, ARASA, and Human Rights Watch interview with Felix, Mukobeko Maximum Security Prison, September 29, 2009.
[615] ICCPR, art. 9. See also UN Human Rights Committee, General Comment No. 8 on the International Covenant on Civil and Political Rights, Article 9, U.N. Doc. A/40/40 (1982).
[616] UN Human Rights Committee, Hugo van Alphen v. the Netherlands, Communication No. 305/1988 (1990), para. 5.8.
[617] Body of Principles, prins 38-39; United Nations Standard Minimum Rules for Non-custodial Measures (“The Tokyo Rules”), adopted December 14, 1990, G.A. Res. 45/110, annex, 45 U.N. GAOR Supp. (No. 49A) at 197, U.N. Doc. A/45/49 (1990), paras. 6.1-6.2 (“Pre-trial detention shall be used as a means of last resort in criminal proceedings.”); Martin Schönteich, “Pre-Trial Detention and Human Rights in Africa,” in Jeremy Sarkin, ed., Human Rights in African Prisons, (Cape Town: HSRC Press, 2008), pp. 93-116 (“International standards require that pre-trial detention be used only if there is a demonstrable risk that the person concerned will abscond, interfere with the course of justice, or commit a serious offence. They also mandate the widest possible use of alternatives to pre-trial detention.”).
[618] See, for example, PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison, October 3, 2009.
[619] US Department of State, “2009 Human Rights Report: Zambia.” All drug offences under the Narcotic Drugs and Psychotropic Substances Act are nonbailable. Narcotic Drug and Psychotropic Substances Act, sec. 43.
[620] PRISCCA, ARASA, and Human Rights Watch interview with Robby Shabwanga, projects officer, Legal Resources Foundation, October 14, 2009.
[621] See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with Japhet, Mumbwa Prison, October 5, 2009.
[622]Zambia Human Rights Commission, “Constitutionalism and Human Rights: State of Human Rights Report in Zambia,” 2008, pp. 18-19.
[623]ICCPR, art. 14; Body of Principles, prin. 38. See also Constitution of Zambia, art. 18 (“(1) If any person is charged with a criminal offence, then, unless the charge is withdrawn, the case shall be afforded a fair hearing within a reasonable time by an independent and impartial court established by law.”)
[624] PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009.
[625] PRISCCA, ARASA, and Human Rights Watch interview with Mumba, Mukobeko Maximum Security Prison, September 30, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Elijah, Mukobeko Maximum Security Prison, September 30, 2009.
[626] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Lusaka Central Prison, February 6, 2010.
[627] PRISCCA, ARASA, and Human Rights Watch interview with RS-03-09, Lusaka Central Prison, October 3, 2009.
[628] ICCPR, art. 14(3)(d); Body of Principles, prin. 17.
[629]Legal Aid Act, Laws of Zambia, vol. 4, chapter 34, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 9(1).
[630] Ibid., sec. 8(1).
[631] PRISCCA, ARASA, and Human Rights Watch interview with Erick, Lusaka Central Prison, October 3, 2009.
[632]Zambia Human Rights Commission, “Strategic Plan 2007-2011,” October 2006, p. 15.
[633] PRISCCA, ARASA, and Human Rights Watch interview with Robby Shabwanga, projects officer, Legal Resources Foundation, October 14, 2009.
[634] PRISCCA, ARASA, and Human Rights Watch interview with Anderson, Choma Prison, October 8, 2009.
[635] PRISCCA, ARASA, and Human Rights Watch interview with Tasila, Kamfinsa Prison, October 1, 2009.
[636] Criminal Procedure Code Act, sec. 202.
[637] PRISCCA, ARASA, and Human Rights Watch interview with Kalunga, Mumbwa Prison, October 5, 2009.
[638] PRISCCA, ARASA, and Human Rights Watch interview with Joshua, Lusaka Central Prison, October 3, 2009.
[639] PRISCCA, ARASA, and Human Rights Watch interview with Oscar, Lusaka Central Prison, October 3, 2009.
[640] See, for example, PRISCCA, ARASA, and Human Rights Watch interview with Samuel, Kamfinsa Prison, October 1, 2009 (“There is no transit to go to court; I miss court hearings.”).
[641] PRISCCA, ARASA, and Human Rights Watch interview with Banda, Mukobeko Maximum Security Prison, September 29, 2009.
[642]Immigration and Deportation Act, Laws of Zambia, vol. 9, chapter 123, 1996, http://www.parliament.gov.zm/index.php?option=com_content&task=view&id=21&Itemid=49 (accessed February 22, 2010), sec. 25(1).
[643] PRISCCA, ARASA, and Human Rights Watch interview with Denny Lungu, deputy chief immigration officer (administration), Ministry of Home Affairs Department of Immigration, February 5, 2010.
[644] Ibid.
[645] PRISCCA, ARASA, and Human Rights Watch interview with Hope, Lusaka Central Prison, October 4, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with KT-04-04, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-05, Lusaka Central Prison, October 3, 2009.
[646] PRISCCA, ARASA, and Human Rights Watch interview with Susan, Lusaka Central Prison, October 4, 2009.
[647] Note that, under international law, non-citizens lawfully within a state territory may only be expelled following a decision reached in accordance with the law. ICCPR, art. 13.
[648] PRISCCA, ARASA, and Human Rights Watch interview with RS-01-08, Kamfinsa Prison, October 1, 2009.
[649] PRISCCA, ARASA, and Human Rights Watch interview with Benjamin, Kamfinsa Prison, October 1, 2009.
[650] PRISCCA, ARASA, and Human Rights Watch interview with Laurent, Kamfinsa Prison, October 1, 2009.
[651] PRISCCA, ARASA, and Human Rights Watch interview with Alfred, Kamfinsa Prison, October 1, 2009.
[652]See, e.g., PRISCCA, ARASA, and Human Rights Watch interview with George, Kamfinsa Prison, October 1, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Mary, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Hope, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with KT-04-04, Lusaka Central Prison, October 4, 2009; PRISCCA, ARASA, and Human Rights Watch interview with NCI-03-05, Lusaka Central Prison, October 3, 2009.
[653] PRISCCA, ARASA, and Human Rights Watch interview with Jean Marie, Lusaka Central Prison, October 3, 2009.
[654] PRISCCA, ARASA, and Human Rights Watch interview with RS-03-03, Lusaka Central Prison, October 3, 2009.
[655] PRISCCA, ARASA, and Human Rights Watch interview with Denny Lungu, deputy chief immigration officer (administration), Ministry of Home Affairs Department of Immigration, February 5, 2010.
[656] PRISCCA, ARASA, and Human Rights Watch interview with RS-03-01, Lusaka Central Prison, October 3, 2009.
[657] PRISCCA, ARASA, and Human Rights Watch interview with Muntala, Lusaka Central Prison, October 4, 2009.
[658] PRISCCA, ARASA, and Human Rights Watch interview with Denny Lungu, deputy chief immigration officer (administration), Ministry of Home Affairs Department of Immigration, February 5, 2010.
[659] Martin Shönteich, “The Scale and Consequences of Pre-Trial Detention Around the World,” Justice Initiatives: Pre-Trial Detention, Spring 2008, http://www.soros.org/initiatives/justice/focus/criminal_justice/articles_publications/publications/pretrial_20080513/Justice_Initiati.pdf (accessed April 6, 2010), pp. 11-43.
[660] Ibid., p. 33.
[661] Penal Code Act, sec. 24.
[662] Criminal Procedure Code Act, sec. 306(A-E).
[663] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009; PRISCCA, ARASA, and Human Rights Watch interview with Chipo Mushota Nkhata, HIV/AIDS and human rights programs officer, Human Rights Commission, Lusaka, October 13, 2009.
[664] Lukas Mutingh, “Alternative Sentencing in Africa,” in Jeremy Sarkin, ed., Human Rights in African Prisons, (Cape Town: HSRC Press, 2008), p. 196.
[665] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[666] Ibid.
[667] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[668] PRISCCA, ARASA, and Human Rights Watch interview with Frederick Chilukutu, deputy commissioner of prisons, Zambia Prisons Service, October 12, 2009.
[669] ICCPR, art. 14.
[670] PRISCCA, ARASA, and Human Rights Watch interview with CM-03-09, Lusaka Central Prison, October 3, 2009.
[671] PRISCCA, ARASA, and Human Rights Watch interview with Howard, Mukobeko Maximum Security Prison, September 30, 2009.
[672] PRISCCA, ARASA, and Human Rights Watch interview with Chishala, Mukobeko Maximum Security Prison, September 30, 2009.
[673] PRISCCA, ARASA, and Human Rights Watch interview with Paul, Mukobeko Maximum Security Prison, September 30, 2009.
[674] PRISCCA, ARASA, and Human Rights Watch interview with Emmanuel, Mukobeko Maximum Security Prison, September 30, 2009.
[675] ICCPR, art. 10; UN Human Rights Committee, General Comment 21, para. 10.
[676] Basic Principles for the Treatment of Prisoners, prin. 10.
[677] PRISCCA, ARASA, and Human Rights Watch interview with KT-06-03, Mwembeshi Prison, October 6, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with KT-06-06, Mwembeshi Prison, October 6, 2009 (“The other problem is, when we are coming out, the government does not give you anything to start with. When someone’s life is destabilized, he needs a ladder. This is a very big problem. It makes some come back here several times, because once he goes out, he has nothing to do. When we go out, the government should give small capital to start a job. There is no planning for our release.”); PRISCCA, ARASA, and Human Rights Watch interview with Agnes, Kamfinsa Prison, October 1, 2009 (“The major problem affected the other inmates here—there is no addressing of post-discharge, how to cope with our life that we left. The prison administration does not address it—they look at the now, not at the future. I have had some education sessions—mainly dealing with acquiring capital to start a small business. But I need practical skills in tailoring. It is hard to stay here for one year doing nothing.”).
[678] PRISCCA, ARASA, and Human Rights Watch interview with Andrew, Mumbwa Prison, October 5, 2009. See also PRISCCA, ARASA, and Human Rights Watch interview with Japhet, Mumbwa Prison, October 5, 2009 (“Our economy cannot sustain that, the prisons need to ensure that people’s skills are improved or used, or one will go back to crime. It needs to change and develop, all jails in Zambia are congested. There needs to be a broader approach to introduce jobs in jail. People come here and leave worse off than when they first arrived.”); PRISCCA, ARASA, and Human Rights Watch interview with Mwisa, Choma Prison, October 8, 2009 (No re-entry programs, that is why people come back to prison.”).
[679] PRISCCA, ARASA, and Human Rights Watch interview with former prisoner, Lusaka, February 5, 2010.
[680] PRISCCA, ARASA, and Human Rights Watch interview with former prisoner, Lusaka, February 5, 2010.
[681] PRISCCA, ARASA, and Human Rights Watch interview with officer in charge, Mwembeshi Prison, October 6, 2009.
[682] PRISCCA, ARASA, and Human Rights Watch interview with Ms. Kaluba, offender management officer, Mwembeshi Prison, October 6, 2009.
[683]K.C. Goyer et al., “HIV/AIDS in Prison: Treatment, Intervention and Reform: A Submission to the Jali Commission,” undated, p. 8. UNODC, UNAIDS and World Bank, “HIV and Prisons in Sub-Saharan Africa,” p. 11.
[684] UNODC, UNAIDS and World Bank, “HIV and Prisons in Sub-Saharan Africa,” p. 2.