“Even Dead Bodies Must Work”
Health, Hard Labor, and Abuse in Ugandan Prisons
Map: Prisons Visited by Human Rights Watch in Uganda
Definitions and Acronyms
ART or ARVs: Antiretroviral therapy for the treatment of HIV, which works to suppress the HIV virus and stop the progression of the HIV disease
CD4 count: The number of CD4 cells (T-helper lymphocytes with CD4 cell surface marker) used to assess immune status, susceptibility to opportunistic infections, and a patient’s need for antiretroviral therapy
Committals or committed prisoners: Prisoners facing serious criminal charges, such as murder or aggravated robbery, whose cases have been sent to the High Court but who have not yet completed their trials
Farm prison: Prison where prisoners work on government-owned fields to produce mainly maize meal and beans consumed by prisoners countrywide, in addition to other labor
Garden: Field where prisoners work, also referred to as a shamba
JLOS: Justice Law and Order Sector, a group of Ugandan government bodies and international donors working collaboratively to improve access to justice
Katikkiro: Prisoner with disciplinary authority, sometimes called RP (short for “Resource Protection”) or ward leader; Luganda word literally meaning “administrative head”
LAP: Local administration prison; until 2006, local governments in Uganda administered over 170 prisons independent of the Uganda Prisons Service; former LAPs are smaller and historically less resourced than the larger prisons which have been continuously under central government administration
MDR-TB: Multi-drug resistant tuberculosis, a form of tuberculosis caused by Mycobacterium tuberculosis resistant in vitro to the effects of isoniazid and rifampicin, the two most powerful anti-TB drugs, with or without resistance to any other drugs
Murchison Bay Prison Hospital: The only prison referral hospital in Uganda administering care to prisoners, based at the Luzira/Murchison Bay Prison complex in Kampala
OC: “Officer in charge,” in this case, of a prison; he or she is the highest ranking officer present at the facility and has near-total discretion in decisions concerning his or her prison
Panadol: Paracetamol, a basic pain reliever also marketed as Tylenol
PMTCT: Prevention of mother-to-child transmission of HIV; PMTCT health interventions aim to reduce the spread of HIV from a mother to her baby during pregnancy, birth, or breastfeeding
Reception center: Prison intended to hold remanded, newly convicted, short-term, or maximum security prisoners who have not been sent to farm prisons
Remands or remanded prisoners: Prisoners awaiting trial or currently on trial
Septrin: Cotrimoxazole, a medication recommended for all individuals testing positive for HIV in order to treat opportunistic infections
Shamba: Swahili word literally meaning “field”
UPS: Uganda Prisons Service
Summary
If you say you’re sick, the warden just kicks you and says, “Even dead bodies must work.”
—Musa, Muduuma Prison, November 12, 2010
The prisoners at Muinaina Farm Prison have been forgotten by the Ugandan criminal justice system. Almost two thirds of the inmates on this rural hilltop have never been convicted of a crime. Some have not set foot in a courtroom in five years. Prisoners plead guilty just to know their date of release. Yet the backlog in the courts allows the prison authorities to profit from these forgotten prisoners because every day the prisoners at Muinaina go to work, farming the lands of the Uganda Prisons Service (UPS), producing the maize meal that feeds inmates at other prisons. Or they dig on the wardens’ personal farms, growing produce that the wardens sell for personal profit. Or they work for private farmers in the area, who pay the prison authorities. On the farms, they are brutally beaten for lagging behind.
They sleep on a cement floor, crowded together in hot cells. There is hardly any medical care available: HIV-positive prisoners are sent to work and are only sometimes excused when they are too weak to keep up; then they may be transferred to Kampala for treatment. Some prisoners cough, violently, night after night, their lungs possibly full of drug-resistant tuberculosis (TB), which is being spread to those around them. “Help us, we’ll die,” pleaded 10 of the prisoners in a note transmitted to Human Rights Watch.
In Uganda, prison conditions at a few, larger, regional prisons have improved in recent years because of the enactment of the new Prisons Act in 2006, partnerships with a few international donors on health, and the work of the Uganda Prisons Service. At these prisons, prisoners can usually access HIV testing and treatment and general healthcare. Overcrowding is less severe and clean water is usually available. But at many of the others, including Muinaina, the conditions and treatment rise to the level of cruel, inhuman or degrading treatment, and even torture.
Between November 2010 and March 2011, Human Rights Watch interviewed 164 prisoners and 30 prison officers at 16 prisons across Uganda, as part of a series of reports on health in prisons in Africa. Human Rights Watch found that poor conditions, forced and corrupt labor practices, routine violence at the hands of prison wardens, infectious disease, and inadequate medical care threaten the lives and health of the 50,000 inmates who pass through Uganda’s 223 prisons each year.
The conditions at some Ugandan prisons are improving but—particularly in rural, former locally administered prisons—are still far below international standards. Overcrowding is endemic, with prisons nationwide at 224 percent of capacity. Of the 16 prisons visited by Human Rights Watch, all but one was significantly over its official capacity, in one case rising to a staggering 3,200 percent of capacity. Prisoners often sleep on one shoulder, packed together so that they can only shift if an entire row agrees to roll at once.
Prison food is nutritionally deficient, leaving inmates vulnerable to infections and in some cases blind; sex is sometimes traded by the most vulnerable for additional food. Water is often unclean or unavailable. At some prisons, boiled water has become a commodity sold by inmates with kitchen privileges. Proper hygiene is difficult with limited government-provided soap, and lice and scabies are rampant. Mosquitoes and malaria are a constant threat, but the prison administration has only sprayed with insecticide at three prisons, and bed nets are forbidden for male inmates because of security fears.
A brutal compulsory labor system operates in rural prisons countrywide. Thousands of prisoners, convicts and remands, are forced to engage in hard labor—cultivating crops, clearing fields—day after day. Compulsory labor is often combined with extreme forms of punishment, such as beatings to punish slowness, and handcuffing, stoning, or burning prisoners who refuse to work. Few prisoners receive proper medical care for their injuries, and prisoners are regularly refused access to medical care because officers will not allow them to miss work. Prisoner productivity translates directly into profit for prison authorities, but prison authorities often do not account for the funds raised through prison labor.
In addition to abuses in the fields, prisoners are beaten and abused within the prison, allegedly as punishment. Inmates are also sometimes confined in isolation cells, often naked, handcuffed, and sometimes denied food; the cells are sometimes flooded with water up to ankle height. Some have had their hands or legs broken, or have become temporarily paralyzed as a result of beatings, and seldom receive medical care. Prisoners with mental disabilities are in some cases targeted for beatings, and even pregnant women are not spared.
The prevention and treatment of disease pose major problems in Uganda’s prisons. TB spreads quickly in the prisons’ dank, overcrowded, and poorly ventilated wards. TB prevalence in the prisons is believed to be at least twice that in the general population, which already is one of the world’s highest. While the prisons service has recently rolled out TB entry screening at 21 prisons, more than 200 still offer none. Prisoners routinely reported having coughed for long periods without having been tested for TB. TB treatment is only available in the prison medical system at Murchison Bay Hospital in Kampala, but even those inmates transferred for treatment may not stay long enough to be cured. TB patients are sometimes sent back to prisons where continued treatment is not possible in order to perform hard labor or ease prison congestion. The result may be drug resistance or death.
HIV prevalence in Ugandan prisons is estimated to be approximately 11 percent, almost twice national estimates. And although sexual activity among male inmates is acknowledged by prison authorities, condoms are universally prohibited because consensual sexual conduct between people of the same sex is a criminal offence. While just over half (55 percent) of the prisoners Human Rights Watch interviewed had been tested for HIV while in prison, rates were much lower at smaller, rural prisons. However, for those who are positive, treatment may be unavailable. Of Uganda’s 223 prisons, prison-based antiretroviral therapy (ART) is only available at Murchison Bay, and even there, ART is sometimes unavailable to those in need of it according to national protocols.
Under Ugandan law, people with mental disabilities should not be detained in prison. But a backlog of prisoners awaiting mental competency determinations, and still more who develop mental health problems once incarcerated, create a significant need for mental health services within the prison system. At upcountry facilities, mental healthcare is nonexistent; even at Murchison Bay, treatment consists only of medication prescribed by a visiting psychiatrist and dispensed by other inmates, with no attempt at psychotherapy or other forms of alternative mental healthcare. Inmates with mental disabilities at some prisons are simply isolated in punishment cells with no treatment.
The health needs of pregnant women are also largely unmet. Pregnant inmates receive little or no prenatal care. Pregnant and nursing women usually receive the same nutritionally deficient food as all other prisoners. And pregnant women are forced to perform hard labor and beaten just like other prisoners, leading to reported miscarriage or injury. Protections for women detainees under regional human rights standards are simply ignored.
The dangerously unhealthy conditions in many of Uganda’s prisons are in part a result of failures of the criminal justice system; prison officers’ inappropriate denials or delays in permitting access to medical treatment; and an under-resourced and inadequate healthcare system that has received limited support from the government and international donors.
Prison overcrowding is a direct result of extended pretrial detention and underuse of the non-custodial alternatives that are available, such as bail and community service. Fifty-six percent of the Ugandan prison population has never been convicted of any crime and is by law presumed innocent. However, remand prisoners often wait for years for their cases to be resolved and are forced into harsh labor conditions alongside convicts. While efforts have been made in recent years to address the case backlog, an insufficient number of judges, judges’ failure to grant bail in accordance with Ugandan law, and inadequate legal representation still conspire to create significant remand times, particularly for prisoners awaiting trial before the High Court. Corruption is reportedly rampant in the criminal justice system, from arrest through trial, so in some cases those remaining in prison are simply those unable to pay the necessary bribe. Children are also sometimes held in adult prisons instead of in juvenile detention facilities, contrary to Ugandan and international law.
Uganda has repeatedly committed itself to upholding the human rights of prisoners through its assumption of international and regional obligations. Under international human rights law, prisoners retain their human rights and fundamental freedoms, except for restrictions on rights necessitated by the fact of incarceration itself. Uganda has an obligation to ensure that its criminal justice and penitentiary standards comply with international and regional human rights standards, to ensure that detainees are treated with appropriate dignity and full respect of their human rights, and to prevent all forms of cruel, inhuman and degrading treatment. Uganda is also required to ensure adequate healthcare for prisoners, at a standard at least equivalent to that available to the general population, a commitment acknowledged by the Uganda Prisons Service. Yet medically unqualified prison officers routinely assess the health needs of prisoners and then deny their right to access care.
In Uganda, ill-health, hunger, and poor access to healthcare are not unique to prisoners. However, Uganda has an obligation to ensure basic minimum conditions and healthcare for detainees, to protect prisoners’ rights and public health. The Ugandan government has a binding and non-negotiable obligation not to expose people to torture and cruel, inhuman or degrading treatment, which it currently violates when sending them to prison.
Reform is critical: of prison oversight and management and of laws and practices that lead to extended pretrial detention. The Ugandan government and international donors need to prioritize prison funding, while ensuring that corrupt labor practices end. By building on the advice of its own medical staff and that of outside human rights monitors, the Uganda Prisons Service has the opportunity to continue to improve its protection of the rights and health of prisoners, by eliminating the abusive practices that lead to poor health.
Key Recommendations
For Immediate Implementation
The Uganda Prisons Service and Ministry of Internal Affairs should:
- Issue direct orders to stop the use of forced prison labor for private landowners or prison staff;
- Declare a zero tolerance policy for the beating of prisoners and warn that staff and inmates will be disciplined and punished for abuses;
- Carry out regular monitoring visits led by headquarters and medical staff to ensure the health and well-being of prisoners throughout the country and a halt to corrupt labor practices;
- Provide condoms to all prisoners and prison staff, in conjunction with HIV/AIDS education on harm reduction;
- Provide TB screening and offer HIV voluntary counseling and testing to all inmates, and ensure prompt initiation and continuation of treatment for those with confirmed disease;
- Establish guidelines for immediate referral of all prisoners with confirmed TB or HIV to facilities where they will receive treatment, and halt the practice of transferring inmates on treatment away from prisons with treatment capacity;
- Issue direct orders to all officers in charge to allow inmates reporting illness or disability to seek healthcare, and to take responsibility for inmate health.
The judiciary should conduct all bail hearings in open court and the Rules Committee should issue a Practice Direction setting conditions for bail and guidelines on appropriate amounts in line with income levels in Uganda.
For Longer-Term Implementation
The Ugandan Parliament and Ministry of Finance should secure, and international donors should assist with securing, enough funding for the prison budget to ensure conditions consistent with international standards, without reliance on income from forced inmate labor for private landowners.
The Uganda Prisons Service and Ministry of Internal Affairs should establish guidelines on prison-based health services and scale up those services to:
- Establish at each prison nationwide at minimum one trained health worker, with a supply of essential medications;
- Conduct health screenings of all prisoners on entry and at regular intervals;
- Ensure access to prenatal, postnatal, and prevention of mother-to-child transmission of HIV (PMTCT) services and address the nutritional needs of pregnant women and breastfeeding mothers;
- Ensure access to mental health services;
- Provide prompt referrals and transfer to higher level facilities in the community or prison system for appropriate treatment.
The Ministry of Justice should devise a functional legal aid system to ensure that defendants have access to a lawyer from the time of arrest.
Methodology
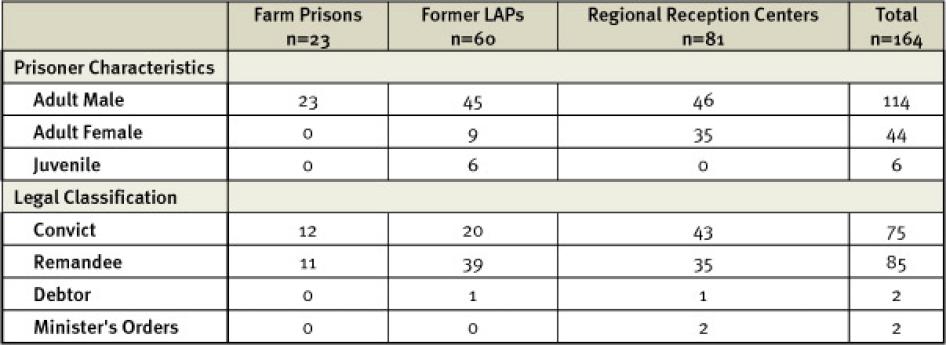
This report is based on 231 interviews, including interviews conducted with 164 prisoners (114 men, 44 women, and 6 children) and 30 prison officers at 16 prisons between November 2010 and March 2011. Prisons were selected to represent a diverse range of facilities based on type, status (formerly locally or centrally administered), size, and level of congestion. Access was granted by the commissioner general of prisons as a part of Human Rights Watch’s routine human rights monitoring in prisons, regularly carried out in Uganda for several years.
Table 1: Prisoner Interviewee Characteristics[1]
In prisons visited, researchers identified prisoners to approach for interviews in two ways: 1) according to a randomized method involving choosing prisoners from the available prisoner registers, and 2) targeted selection of prisoners to ensure representation of certain categories, including those who had been transferred from one prison to another to receive medical care, individuals identified to Human Rights Watch as having undergone specific types of punishment, and women (particularly women who had been pregnant or who had cared for a small child while in prison).
Interviews were conducted in English or in Lubwisi, Luganda, Lukonzo, Luo, Lusoga, Lwamba, Runyoro-Rutoro, Runyankole-Rukiga, Samia, or Swahili, with translation into English. One interview was conducted in French. The purpose of the research was explained to each prisoner, who was asked whether he or she was willing to participate, and offered anonymity. Prisoners were told that they could end the interview at any time or decline to answer any questions without negative consequence. All interviews were conducted privately, with one prisoner at a time. Each prisoner interviewed and quoted in this report has been given a pseudonym to protect the prisoner’s identity and for the prisoner’s security; surnames have been omitted to conceal prisoners’ ethnicities.
Prisoners who were interviewed averaged an age of 31 years. Overall, the most common charges of the prisoners interviewed were theft, murder, and defilement. The time the prisoners interviewed had spent detained ranged considerably between the different types of prisons visited, averaging 22 months, but highest among prisoners at farm prisons (on average 48 months). Prisoners often reported having been moved between prisons, and the time prisoners had spent in the facility in which they were interviewed also varied considerably, but averaged nine months.
Human Rights Watch researchers also conducted facility tours and interviewed 30 prison staff members at the 16 prisons visited, in addition to the Uganda Prisons Service medical authority. In some cases, official titles of individuals are not given for security reasons or at the request of the individual. At the conclusion of field research, Human Rights Watch sent a letter to the Uganda Prisons Service commissioner general of prisons on April 8, 2011, (see Appendix) requesting a response by April 29, 2011 to numerous issues raised in the report; Human Rights Watch did not receive an official response to this letter within the timeframe. Human Rights Watch again requested a response on May 13, 2011, and provided an additional summary of the issues presented in the report on May 16, 2011, at the request of prison authorities. An email response from prison authorities to some of the questions Human Rights Watch had posed was received by email on May 19, 2011, and by letter on June 29, 2011, as this report went to press. That information is reflected throughout the report.
Researchers also interviewed 15 members of the communities surrounding Sentema, Kasangati, and Ntenjeru Prisons (all Central Region), and three prison officers at those prisons, specifically about the practice of hiring out prisoner labor to private landowners.
Finally, researchers interviewed 18 representatives from local and international organizations working on prison, HIV/AIDS, and health issues; health workers within the Ugandan government; and donor governments and agencies.
Caution should be taken in generalizing the results of this research to all prisoners in Uganda. Because Human Rights Watch oversampled prisoners in Kampala-area prisons, which have greater resources than rural prisons, the percentage of prisoners receiving medical testing and care in this report may be greater than the national average. Also, the selection of prisoners within each prison was not perfectly representative. Researchers tried to systematically and randomly select prisoners; however, this was not always possible. Because of the diverse conditions among prisons and because specific groups of prisoners (noted above) were intentionally oversampled, Human Rights Watch has, to the greatest extent feasible, presented disaggregated data according to prison and prisoner type.
This report is part of a series of reports on health in prisons in Africa by Human Rights Watch. The objective of the series of reports is to examine health and human rights issues in prisons in Africa in the context of diverse health and justice policy, reform efforts, and resource availability.
I. Background
The Ugandan Prison System
Uganda has 223 prisons countrywide. Designed to house 13,670, in March 2010 Ugandan prisons were at 224 percent of capacity, with 29,136 male and 1,278 female prisoners in custody.[2] The Uganda Prisons Service employs 6,700 staff, including 6 physicians.[3]
In addition to prisons run by the central government, prior to 2006, local governments administered independent prisons, at which conditions were reportedly grossly inadequate.[4] The Prisons Act of 2006 transferred the functions and administration of these locally administered prisons to UPS,[5] to create one nationwide system. Significant problems remain at the over 170[6] former Local Administration Prisons (LAPs).[7] Although approximately one third of Uganda’s prisoners were housed in former LAPs in March 2010,[8] prisoners in former LAPs constitute the majority of those not served by prison-based health facilities.[9]
Currently, UPS operates two official categories of prisons: reception centers and farm prisons. Although practice varies, in general, remandees and prisoners convicted of petty offences (with sentences less than one year) are kept at reception centers; male prisoners convicted to serve sentences over a few months but less than 10 years, or those with a short period of time remaining on their sentences, are sent to farm prisons. Remand or convicted prisoners facing or serving sentences over 10 years are sent to maximum security reception center prisons.Individual officers in charge (OCs) of prisons are empowered to decide which prisoners, including those undergoing medical treatment, to move to farm prisons; they do so without consultation with medical officials and their decisions are not subject to review.[10]
There is a separate juvenile justice system, with five facilities for children accused or convicted of criminal offences nationwide.[11] Though official statistics indicated no children held in prisons during 2009-2010,[12] in practice children are detained with adults in some.[13]
By law, UPS “shall be provided with adequate resources and facilities.”[14] UPS funding derives from the government of Uganda, donor funding, and “internally generated” revenue.[15] OCs set their budget priorities, which are reviewed and decided upon by prison headquarters in Kampala, with supplies coming almost exclusively in the form of the items requested. The receipt of these items is erratic and undersupply a general problem.[16]
Management of health in prisons is overseen by the Ministry of Internal Affairs, the line ministry for the UPS. UPS has calculated that it spends 17,073 Uganda shillings (US$6.96) per prisoner annually on health when dividing its health budget by the prisoners, staff, and staff dependents who use its services; that figure drops to 4,830 Uganda shillings ($1.98) annually per prisoner when factoring into the calculation the members of the neighboring communities who access prison-supplied health services.[17]
Officially, the total UPS health budget was increased by 55 percent between fiscal year (FY) 2009/10 and FY 2010/11.[18] Yet the overall proportion of the prison budget allocated for health services remained a flat two percent.[19] By comparison, the government provides roughly 9 to 10 percent of its national budget to healthcare.[20] In 2009, the commissioner general of prisons admitted to the media that lack of funding had led to deteriorating infrastructure and health in Ugandan prisons.[21]
Health services for the prisons are headed by a national directorate in Kampala. As of March 2011, 63 of Uganda’s 223 prison units had some level of healthcare worker. At the rest, prisoners were expected to rely on the health facilities in the neighboring communities.[22]
The national referral hospital for prisoners is at Murchison Bay Prison in Kampala. Murchison Bay Hospital treats prisoners temporarily referred from other prisons to receive inpatient or outpatient medical treatment,[23] and is the only medical facility in the prison system accredited to provide TB treatment and antiretroviral therapy for HIV treatment.[24] The UPS has established 10 regional health units intended to oversee delivery of healthcare services.[25] Forty-nine additional health “units” across the UPS have healthcare workers. But, in practice, the capacity of many of the facilities is limited: according to the prison medical authority, “we have no doctors at all in the upcountry units, we have zero.”[26]
The Ugandan Healthcare System
While the UPS often relies on community-based health services for prisoner care, healthcare for Uganda’s general population suffers from numerous problems. Uganda’s healthcare system ranks 186th out of 191 countries according to the World Health Organization (WHO).[27] Life expectancy is among the lowest in the world at 52 years; 1 in every 35 women dies as a result of giving birth.[28]
In national healthcare facilities, only half of all posts are filled.[29] Access to healthcare in poor rural areas is especially difficult. Around half of the population does not have any contact with modern healthcare facilities.[30] Some 70 percent of Ugandan doctors and 40 percent of nurses and midwives are based in urban areas, serving only 12 percent of the population.[31]
Healthcare centers,[32] often in dilapidated condition, frequently house patients together in wards, with no privacy regardless of gender or condition.[33] Medical equipment is lacking and where available, often there is no staff, electricity, or water.[34] The government does not supply sufficient drugs and equipment countrywide, leading to frequent drug stock outs and lack of basic supplies such as gloves or disinfectant.[35]
II. Findings
The engagement of a prisoner in doing work as a principle would be ok, but it has to be closely supervised so that it is not abused.... There seems to be an insensitivity when it comes to the mobilization of labor. If a prisoner is on TB treatment, ARVs—you send him to where there are no services? … If they are on TB treatment, and you take them to a farm, you create drug resistance.
—Prison medical authority, Uganda Prisons Service, November 18, 2010
Prison Conditions
Overcrowding
Overcrowding in Ugandan prisons is endemic and by 2019, the UPS projects the prison population will more than double.[36] Contrary to international and Ugandan law requirements that accused people and convicted prisoners be held separately,[37] at every prison visited, all categories of prisoners (convict, remand, and debtor[38]) were mixed.[39]
Although international standards establish basic requirements with respect to prisoners’ accommodations, including with regard to ventilation, floor space, bedding, and room temperature,[40] 15 of the 16 prisons visited by Human Rights Watch were significantly over their official capacity. Fort Portal Women’s Prison was slightly undercapacity; Muduuma Prison, by contrast, was filled to a staggering 3,200 percent of capacity.[41] Prisoners reported wards routinely sleeping twice or three times their design capacity, and prison officers confirmed that congestion is a major problem.[42] At Luzira Upper, in one ward 124 prisoners packed into a space eight meters square.[43]
Prisoners complained about suffering each night in this limited sleeping space and described being “squeezed like iron sheets,”[44] “like chickens,”[45] or arranged nightly by a designated inmate “like logs,” “firewood,”[46] or “sacks of beans.”[47] Most often, prisoners told Human Rights Watch they were forced to sleep in lines, on one side, so packed together that if one turned to his other side, his entire row was forced to do so.[48] Occasionally, also, prisoners reported being forced to sleep in turns,[49] or seated or standing.[50]
Many prisoners said that they slept without any mattress; prisoners frequently reported being given one blanket to lie on and cover themselves. Sometimes two inmates shared a single blanket or mat. Occasionally, prisoners said they were not allowed to have a mattress, lest the ward become so crowded that its inhabitants would not fit in the room.[51]
Such tightly packed wards allow for little ventilation in contravention of international standards.[52] Inmates repeatedly complained of the heat in the congested cells: “We sweat from the bones.”[53] William said, “When your neighbor sweats, all the sweat will be on you.”[54]
At a few prisons, prisoners are forced to stay in their crowded cells day and night. Ugandan law provides that each prisoner have at least one hour of exercise in the open daily.[55] But at Masaka Ssaza and Butuntumura Prisons, the majority of prisoners spent all day and night locked in the overpacked cells because of security concerns about the prison’s perimeter[56] and were permitted outside for only 20 minutes a day.[57]
Food and Nutrition
Deprivation of food in prison constitutes an inhuman condition of detention in violation of the International Covenant on Civil and Political Rights.[58] International standards require that prisoners be supplied with “food of nutritional value adequate for health and strength, of wholesome quality and well prepared and served.”[59] Under Ugandan law, prisoners are entitled to nutritious food “adequate for health and strength.”[60]
At every prison visited, prisoners reported being given posho (maize meal) and beans once or twice daily, sometimes accompanied by a small portion of porridge for breakfast. Despite a recommended dietary scale including nuts, meat, vegetables, and sugar,[61] prisoners receive only maize meal, beans, and salt.[62] Greens grown by prisoners supplement the rations seasonally at some prisons. However, at others, prisoners reported that the officers confiscated all or a portion of the vegetables grown by prisoners.[63] Mark, at Muinaina Farm Prison, concluded: “We eat greens, but like a goat tied on a rope, the eating is controlled.”[64]
Most prisoners said that the government-provided food was not enough. Prisoners doing hard labor in particular considered food portions insufficient.[65] Julius, at Kitalya Farm Prison, said, “We are eating crumbs. However much energy we use, it is not enough.”[66] Medical personnel and a nutritional assessment conducted by the UPS agreed: “it is not enough for doing hard work.”[67]
Indeed, death records provided by UPS prison authorities to Human Rights Watch indicated that at least one prisoner died in 2010 from malnutrition.[68] The adequacy of the diet in terms of micro-nutrients was also a concern. The prison medical authority noted that:
There is a deficiency in terms of micronutrients, including A and C. Vitamin A is important in the immune system and eyes; vitamin C is important in cellular regeneration when recovering from diseases. These are important because we’re having a population of prisoners vulnerable to infections, and their capacity to recover from and fight off infections is grossly compromised. We see the cases of malnutrition….Especially the long-termers—they develop blindness, and infections like TB.[69]
The lack of adequate nutrition is particularly problematic for pregnant women prisoners and women with small children in prison. Under Ugandan law, “[a] female prisoner, pregnant prisoner or nursing mother may be provided special facilities needed for their conditions.”[70] Some women occasionally reported receiving supplemental milk or eggs during their pregnancy. [71] However, pregnant women typically do not receive extra food rations; they eat exactly the same diet as other prisoners.[72] At Jinja Women’s Prison, those pregnant women who had been exempted from hard labor ate an even less nutritious diet than their non-pregnant colleagues because they did not grow greens which they could eat.[73] Harriet, a new mother at Masaka Main, concluded: “The food we eat doesn’t generate breast milk.... I’m breastfeeding but it’s not enough.”[74] If prisoners choose not to breastfeed, or are unable to breastfeed, they do not consistently have access to formula or safe water with which to prepare it.[75] Despite international standards calling for special provisions for children incarcerated with their parents,[76] and Ugandan law requiring children imprisoned with their mothers to be supplied with “necessities of life,”[77] food is not generally provided for these young children.
Uganda’s own auditor general concluded that the UPS, given its budget and the food grown on farm prisons, would have the capacity to feed prisoners a sufficient diet, but that due to under-declaration and lax oversight of farm production by prison OCs, prisoners’ diets remain inadequate.[78] “[D]ishonest business practices like delivering less quantities of food items,” lack of prioritization (and reallocation of budgeted resources) for food, and the practice of taking prisoners to work on private instead of prison farms led to inadequate food for prisoners.[79]
Water, Sanitation, and Hygiene
There is no permanent water here. The kind of water we use is from the ponds we dig.… When you’re in the gardens, some people who are thirsty, if they come across stagnant water, kneel down and drink it. They drink it without the permission of the warden. But if you’re found drinking like a cow, they beat you.
—Martin, Bubukwanga Prison, November 16, 2010
Prisoners frequently told Human Rights Watch that water was insufficient in quantity and that they were constantly thirsty: “Sometimes we get water, sometimes we don’t. There are times we spend a day without drinking.”[80] At Kitalya Farm Prison, prisoners reported that each received approximately one liter of drinking water a day,[81] but it was not enough after a day of hard labor in the sun.[82] Officers in charge confirmed difficulties in supplying their prisons with sufficient quantity of water.[83]
At Bubukwanga Prison, inmates told Human Rights Watch that water did not consistently run from the tap, and they were forced to drink “stagnant water in the roads,”[84] full of small insects,[85] and green or brown in color.[86] At Muinaina, researchers observed the drinking water to be a cloudy olive green color. The OC at Muinaina described the water as “dirty white” and admitted, “It’s not clean.”[87] Indeed, at some prisons, boiled water has become a commodity sold in the cells by inmates with kitchen privileges, in exchange for soap, sugar, or money to those who can afford it.[88]
Under international standards, prisoners must be provided with adequate bathing installations for general hygiene,[89] yet bathing facilities at many Ugandan prisons fall far short of this standard. At Masafu, five prisoners share one basin of water to bathe each day.[90] At Muduuma, prisoners reported that no bathing water at all was provided.[91]
International standards specify that sanitary facilities shall “enable every prisoner to comply with the needs of nature when necessary and in a clean and decent manner.”[92] Despite efforts to overhaul sewage systems at a few prisons in recent years, prisoners at some prisons reported inadequate toilet facilities including the use of buckets.[93] “The most inhuman thing here is the bucket system” that inmates use at night, the OC at Masafu said.[94] At Muduuma, prisoners complained that they were sometimes refused permission to use the existing toilet facilities because they were located outside of the prison’s perimeter, and received beatings for making the request.[95]
International standards also require that prisoners shall be provided with toilet articles necessary for health and cleanliness[96] and separate and sufficient bedding that is “clean when issued, kept in good order and changed often enough to ensure its cleanliness.”[97] Ugandan law makes provision for prisoners to receive toiletries.[98] Yet, across prisons visited, prisoners and prison officers frequently reported an inadequate supply of such basic necessities. Prison officers admitted that, to give prisoners soap on a regular basis, part of the funding had to come from the proceeds of prisoner labor on private farms.[99]
Physical Abuse
Hard Labor
Thousands of prisoners are forced to engage in hard labor. They cultivate crops, clear fields, or fetch firewood and water. Prisoners, convicted or on remand, work often in oppressive conditions, in heat or rain, sometimes intentionally denied food, water, or bathroom breaks.[100] They are beaten as punishment for being slow or to instill fear upon arrival at prison, handcuffed, stoned, or burned if they refuse to work. Vulnerable prisoners, including children, the sick, elderly, and pregnant women are also beaten and forced to work.[101]
International legal standards place important constraints on how prison labor may be used. Under the United Nations (UN) Standard Minimum Rules for the Treatment of Prisoners, adopted by the United Nations as guidance, prison labor must not be of an afflictive but rather of a vocational nature, and prisoners should be allowed to choose the type of work they wish to perform.[102] The work must not be driven by financial profit motives.[103] No prisoner, whether remand or convict, should be forced to work for private entities, such as private landowners.[104] When working for the government, only convicts and not remands may work, and they must be medically assessed to see if they are fit and healthy for work,[105] they must be treated and remunerated fairly on terms close to what free workers receive, they should be male and between the ages of 18 and 45, and may not work more than 60 days a year.[106] Currently, Ugandan prisons do not comply with any of these international standards.
The practice of compulsory labor is longstanding in Ugandan prisons. In 2003 the government of Uganda wrote in its report to the UN Human Rights Committee that the “illegal and exploitative” practice of hiring prisoner labor to private individuals is a “common feature.” Enforced hard labor of non-convicts was at the time “rampant and therefore tantamount to painful punishment without conviction.”[107] In April 2011 according to the government-owned New Vision newspaper, the Uganda Prisons Service announced a new policy to the parliamentary public accounts committee that all prisoners would be paid 100 to 500 Uganda shillings ($0.04 to $0.21) per day for labor.[108] At time of writing, it was unclear to what extent this new policy had been put into practice.
While according to international standards, the safety and health protections in place for non-prison labor are supposed to be in place for prisoners,[109] prisoners in Uganda face greater risk of injury compared to free laborers because of abusive practices, including being made to work closely together or being beaten so that they will walk quickly through rough terrain without shoes, “like a herd of cattle.”[110] Prisoners spend long hours each day doing forced labor,[111] resulting for many in chest pain, ulcers, and fatigue.[112]
Many prisoners said they had to work while actively ill or injured, particularly if they suffered from illnesses that were not immediately visible. Prisoners often said that “there was no time to go to the hospital” because they were forced to work in the fields and were denied permission to miss work in order to receive care.[113] One prisoner, echoing an expression heard many times by researchers, said that prison authorities “were telling us we didn’t come to a hospital, we came to a prison and should work.”[114]The health consequences of prisoners’ hard labor may be severe: One prisoner died in Mubuku Prison while working in the field in November 2010. The exact cause of his death is unclear, but witnesses who saw the incident recounted that he was beaten and his numerous expressions of thirst and requests for water went ignored by prison authorities.[115]
Abuse in the Fields by Wardens and Other Inmates
They [the wardens] took the sick to work. They would take me to dig. They used to start the digging at 6am, and dig at high speed—but when the sun would rise up and the heat raise, I started feeling dizzy and in most cases I would fall down. I was beaten by the katikkiros [prisoners with disciplinary authority], claiming I was faking illness, until one time when this happened to me, the katikkiros beat me, but the wardens stopped them because I couldn’t move, and they ordered I should be taken back to the prison. I lost consciousness, only to wake up to see I was in the ward.
—Henry, a remand prisoner from Muinaina Farm Prison, interviewed at Murchison Bay Prison, November 20, 2010
At the 11 prisons visited by Human Rights Watch where prisoners were engaged in compulsory labor, prisoners reported routine, brutal beatings in the fields.
Prisoners said they were beaten by both prison officials and other prisoners with disciplinary authority, most commonly with sticks or canes. Beatings occurred for a range of reasons: if prisoners lagged behind others in their work, if they said they were sick, if they made errors in their work, if they straightened up to stretch their backs.[116] At Kitalya Farm Prison, Human Rights Watch researchers observed a prisoner with disciplinary authority hitting prisoners with a stick as they unloaded maize from a truck.[117]
Prisoners at Muduuma and Kitalya Prisons said new arrivals were beaten in order to preemptively instill fear, as work in open fields heightened the opportunity to escape.[118] Some were beaten together in groups as large as 25, each with legs and hands tied behind his back with rope.[119] Wardens and other prisoners then beat them with sticks, batons, or slashers, metal rods with a blade used typically for cutting grass.[120]
At some prisons, prisoners reported unique and especially brutal punishments. Four prisoners from Muinaina Farm Prison independently confirmed that prisoners who worked slowly had dried grass or banana leaves placed on top of them and set afire.[121] One was himself a victim while the remaining three said they observed this practice in at least two incidents in 2009. One from Muinaina Prison said he was forced to sit on an anthill to suffer ant bites.[122] Remand prisoners at Muinaina once refused to go to work in the fields after a new OC initiated a policy of making all prisoners, whether remand or convict, work. They were handcuffed to a tree all day, every day, until they succumbed.[123] Female prisoners from Jinja Women’s Prison recounted working in waist-deep water to cultivate rice for the wardens, as leeches attached to them.[124] The wardens, themselves unwilling to get wet, threw stones at prisoners to punish them.[125]
Despite the prohibition in Ugandan law that “[a] prison officer shall not employ a prisoner in the punishment of a fellow prisoner,”[126] and prohibitions in international standards on prisoners being employed in any disciplinary capacity,[127] some prisoners are given authority to punish other prisoners. One prisoner who was promoted through the ranks said that the prison authorities told him, “Don’t go back to the hoe. Now you have a stick.” He described an intricate hierarchical system in which he oversaw other prisoners, who themselves oversaw squads of 20 prisoners, called a “bicycle.” He said, “I can even beat commanders and say, ‘Your bicycle is not moving.’” If he beat a commander, the commander was then required to beat all 20 prisoners in his bicycle.[128]
The Economic Incentives behind Prison Labor
The money they are receiving for us, where do they put it?
—Ali, a former inmate at a farm prison, interviewed at Murchison Bay Prison, November 20, 2010
Testimony of forced hard labor and abuses was most frequent at farm prisons, or former LAP prisons in rural agricultural communities. Prisoners at those prisons said that they were hired out to work on land for private farmers and on land owned or rented by prison authorities. Because their productivity translated directly into profit for prison authorities, who sold the food harvested from their land or were paid per job by private landowners, they forced prisoners to work for long hours, with little rest, even despite illness or injury.
Prison OCs told Human Rights Watch that they needed the income produced by prison labor to meet the operating costs of the prisons.[129] Four OCs said that they received only 150,000 Uganda shillings (approximately $63) or less per month in addition to in-kind supplies from the prison administration in Kampala, leading to a shortfall which they met by contracting out prison labor.[130] As one OC said, “From the working arrangement, we use the money [the prison receives for private work], if it wasn’t there, then we wouldn’t be surviving, we wouldn’t be running the institution. Because of that, we buy milk for the kids, we buy fuel and repair the vehicle, we put a latrine in the female section.”[131] Another OC explained that, “Labor is not part of their sentence. Labor is just an activity that we subject them to for us to be able to keep them and rehabilitate them somehow.”[132]
OCs said that the prison administration knew of and indeed encouraged the practice of contracting out prison labor, as it was a display of initiative by OCs to ensure that their prisons were well run. One OC reported:
There is a language of initiative in the prisons. But they need to define the limits. The regional command had already told the commissioner, no prison in the region will be using a bucket toilet. He said to us, we should put water-borne toilets in the ward at your cost, don’t ask for any money. By December, all prisons in the Eastern region will be using water-borne toilets. But it is an uphill task….I talked to an engineer, and that will take 12 million shillings [approximately US$5,100].[133]
Prison authorities are not required to account fully to the prison administration in Kampala for the earnings from contracting out prisoner labor, potentially fueling corruption. One OC said that a senior colleague, also in the UPS, had told him when he was promoted, “Eat on the job, but don’t eat the job,” which he took to mean that it would be acceptable to personally gain from prison labor as long as he ensured that the prison could operate.[134] An OC of a farm prison informed Human Rights Watch that he intentionally underreported the amount of food his prisoners produced.[135] Uganda’s auditor general has criticized the “laxity in supervision and accountability for the food grown on the prison farms.”[136]
Generally, three models of prison labor exist. In the first, prisoners work on official farm prisons, farming government-owned land.[137] The produce from this activity is intended to go to Kampala for distribution to prisons nationwide. However, sometimes prison officers keep behind a portion of it to meet prison operating expenses. One OC said:
We declare estimates to Kampala [UPS headquarters]. If we expected 100 bags [of produce], we declare 80. You can’t complain to the boss all the time, or else he will call you a failure. You have to take your initiative. The resources we get from the central government are small, minute. Maybe the government should inject in more funds. The 20 bags sold off don’t make it into the books. The auditors don’t understand.[138]
Second, prisoners are contracted out to private farms at rates ranging from 2,500 to 3,500 Uganda shillings (roughly $1.00 to $1.50) per head per day, significantly lower than what free workers would earn, approximately 7,000 to 10,000 Uganda shillings ($3.00 to $4.25) a day.[139] Private farmers hire prisoners to work on their own land and pay the prison OC directly for the labor. Prison staff takes bookings for prison labor by phone or in person, and payment must be made in advance.[140] Injuries sustained by prisoners while working on private land are the responsibility of the prison and not the private farmer.[141] Private farmers must pay for transportation of the prisoners and may rent additional equipment such as hoes from the prison. They are responsible for providing some food for the prisoners and may also pay the accompanying wardens tips ranging from 5,000 to 15,000 Uganda shillings ($2.00 to $6.25) per day per warden to ensure that prisoners’ productivity is high.[142]
According to prison authorities, hiring labor out to private landowners can be done by the OC “for improvement of administration of his Prison.” It “can only be done as a form of employment in which the inmates will have to earn a statutory fee.”[143] Only prisoners who have been convicted of petty offences are permitted to work on private land.[144] Currently, Ugandan prisons violate their own policy.[145]
Media reports have speculated that wide-ranging police sweeps of people in slum areas of Kampala have been driven by the prison authorities’ desires to have free manpower to contract out to private landowners.[146] Prisoners at Muduuma Prison told Human Rights Watch that police engaged in large-scale street sweeps, accusing them of being “rogue and vagabond,” a vaguely defined crime akin to loitering, releasing those who could pay and taking the remainder for hard labor.[147]
In the third model, prisoners cultivate directly for prison OCs and wardens, who sell the produce at a profit. Officially, prison officers can have prisoners work on officers’ own “small gardens…usually once a week on Saturdays.”[148] One OC stated that he personally earned approximately 1,000,000 Uganda shillings ($425) per season and estimated his wardens each made 500,000 to 600,000 Uganda shillings ($200 to $250) per season, the equivalent of two to three months’ wages, by selling the produce that prisoners cultivated on their land.[149] Prisoners with prior experience in agricultural trade placed estimates of the OC’s stock to be several times the amount he reported to Human Rights Watch.[150] Inmates at the same prison, where remand times were on average five years, believed that their prolonged pretrial detention was in part due to the desire of prison wardens to profit from their labor for a considerable period of time. Human Rights Watch observed storage at the prison of the OC’s private maize and rice stock, which he said he planned to sell.[151] Inmates not only cultivated but also processed the maize from the OC’s private stock, and some prisoners observed private sellers paying the OC within prison grounds.[152] When the prisoners raised the issue of their hard labor with the regional prisons commander, they received no assurances that any of these practices would stop.[153]
Wardens and OCs also benefited personally from prisoners in smaller ways by forcing them to clean their houses or do their laundry, allegedly stealing church-donated goods or food given as payment for labor, and in one instance, having them build the OC a new house.[154]
Prison authorities wrote to Human Rights Watch, saying, “Where prisoners are forced to work without pay, that’s abuse. In my tours, I am yet to meet this. The Officer in Charge of the Prison must keep an inventory of these activities that will have to be checked by the Prisons Inspectorate and the Regional Prisons Commanders.”[155] However, at Kitalya Farm Prison, where Human Rights Watch had to go to the fields to retrieve prisoners from their work for interviews, each of the prisoners interviewed reported that only prisoners with disciplinary authority are ever paid for their work; all others receive nothing.[156] Indeed, the vast majority of prisoners Human Rights Watch interviewed who did hard labor reported being forced to work without pay. At some prisons, prisoners were paid nominal amounts of money, around 200 to 500 Uganda shillings per day ($0.09 to $0.21), or received small amounts of food, soap, or cigarettes as payment, but in most instances, prisoners received nothing.[157]
Punishment
Ugandan law lays out disciplinary procedures for prisons.[158] And some of the punishments currently inflicted are in line with Ugandan and international law: Prisoners may lose the possibility of early release,[159] be given additional cleaning or field work,[160] or denied visitors.[161] For serious unlawful offences committed in prison, a prisoner can be criminally charged, prosecuted, and convicted with an additional sentence.[162] Yet, at almost every prison Human Rights Watch visited, prisoners overwhelmingly reported beatings and the use of isolation cells flooded with water while the prisoner was forced to be naked, beaten, and given limited food as the primary punishments.[163]
Beatings
They hit me so hard, I was crying blood.
—Edmund, Muinaina Farm Prison, March 4, 2011, describing a beating by prison wardens and other inmates
Severe beatings—in the fields as described above but also in the prisons themselves—conducted as punishment either by the wardens or by inmates with disciplinary authority, were reported by prisoners at nearly all prisons visited by Human Rights Watch. Overall, 41 percent of the prisoners interviewed by Human Rights Watch said that they had been beaten; 87 percent of prisoners at farm prisons had experienced a beating.
Corporal punishment is forbidden in Ugandan prisons[164] and international law forbids cruel, inhuman or degrading treatment and torture.[165] Prison officers told Human Rights Watch that they knew corporal punishment was banned and frequently contended that it had been abolished in practice.[166] Yet prison medical staff acknowledged that they had observed injuries inflicted by prison wardens: A health worker at Murchison Bay Hospital reported that most of the injury cases he sees are inflicted either by police or prison staff,[167] and the prison medical authority admitted that he had heard of “instances” where “this has cropped up.”[168] Additional human rights monitors have noted the frequent, continuing, use of beatings, despite its official abolition.[169]
An assistant commissioner of prisons is charged exclusively “to monitor human rights abuses in prisons.” According to prison authorities, four OCs have been removed from their positions due to infractions, and an additional two OCs and two junior officers are currently facing criminal charges for assault of inmates.[170]
At every prison visited but one,[171] prisoners reported that caning still takes place; at most, it is the primary form of punishment. At Bubukwanga Prison, researchers touring the prison were confronted with a prostrate inmate, writhing on the floor and moaning in pain. He said: “I’ve been beaten by the OC, he hit me. He left me very badly off. He said I had stolen, and he beat me with a big cane. He beat me this morning.”[172] He showed researchers the marks the beating had left on his body. Other prisoners confirmed that they had seen the OC beat him that morning, for allegedly stealing some sugar from another inmate.[173]
At some prisons—in particular Luzira Upper, Fort Portal Men’s, and Muinaina Farm—prisoners reported marked decrease in frequency and severity of caning in recent years.However, inmates across facilities still consistently reported routine beatings by wardens: At one prison, several prisoners described being held by each arm and leg as they were beaten on the buttocks and back of the head with a stick.[174] According to one inmate, the OC said, “This is the stubborn part,” as he beat prisoners’ heads.[175] Prisoners reported receiving beatings of varying severity, from five strokes to “so many times I could not count.”[176] The instruments include batons, canes, sticks, whips, electric cable, and wire.
Despite prohibitions in Ugandan law and international standards on prisoners being employed in any disciplinary capacity, prisoners with disciplinary authority also mete out punishments within the prison.[177] At some prisons, prisoners reported having been beaten by prisoners with disciplinary authority in the wards on the orders of wardens or as they watched and tacitly approved.[178]
Several prisoners with mental health problems reported being targeted for beatings by inmates with disciplinary authority because of their mental disabilities.[179] As Ali, one inmate in the “mental health” cell at Murchison Bay, observed, “The cleaner [an inmate with disciplinary authority] will say, ‘Stay in the wards,’ and if you go out—you are beaten. But these people [with mental disabilities] don’t see things in the normal sense. They are punishing people for being mentally sick.”[180]
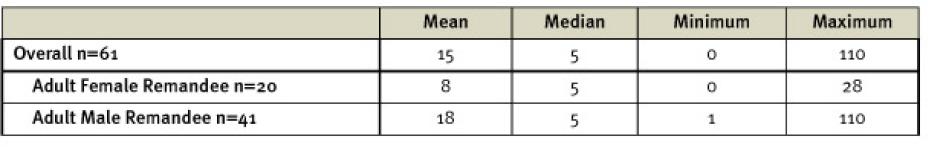
Table 2: Prisoners Reporting Beatings, Health Problems as a Result of Beatings, and Medical Care for Their Injuries
The health effects of beatings may be severe. Prisoners described how beatings in some instances caused loss of consciousness, or partial loss of hearing,[181] while others sustained broken legs as a consequence.[182] One prisoner described how he had been beaten so badly by a warden that he was unable to walk for a month.[183] Another prisoner recalled an incident he had witnessed at a farm prison:
They caned him, and he fell sick. The whole buttocks was rotten. In the ward where I was sleeping, you feel like dying; he lay on the floor crying. This boy received no treatment. But the smell was too much. After some time, we went to the OC’s office, and said, “We are not going anywhere. We need our colleague to get treatment.” The OC reached the door [of the ward], and smelled the stench, and saw the flies. He said the man should get treatment. But even after treatment, he still could not sit. He was totally rotten.[184]
Injuries from beatings at Kitalya Farm Prison were so common that one inmate said, “there was a time from May to October last year when the nurses here were no longer treating us for malaria, they were just treating us for wounds on our buttocks from beating.”[185] But treatment for these injuries is for many an unattainable luxury: only 15 percent of prisoners who told Human Rights Watch they had suffered a health problem as a result of a beating had received treatment, and none of those at former LAPs had received treatment. Matthew, a prisoner at Masafu, experienced a beating so severe that his hand was broken, but the prison warden who beat him would not allow him to go to the hospital.[186]
Isolation Cells
Under Ugandan law, an OC may order a prisoner confined to a separate cell for a period not exceeding 14 days on disciplinary grounds.[187] The law explicitly states that “[s]tripping a prisoner naked, pouring water in a cell of a prisoner, depriving him or her of food and administering corporal punishment and torture is prohibited.”[188]
Yet, at 9 of the 16 prisons visited,[189] Human Rights Watch researchers found that isolation cells were used for punishment, sometimes in conjunction with each of the aggravating factors specifically prohibited by law. Prison officers confirmed the use of isolation cells, but denied the additional deprivations.[190] At four prisons, Human Rights Watch researchers were able to tour the cells used for prisoners’ isolation and found them to be bare cement structures, with a bucket for a toilet, with sizes ranging from one meter by one meter to four meters by five meters. At Luzira Upper Prison, “never forget me” and “broken hands” had been etched into the wall of one of the cells. Prisoners said that isolation can range from a few hours to two weeks, as specified by law, but also noted that it could last in some cases from months to a year[191] depending on the prison and offence.
Despite the explicit legal prohibition, at many prisons a prisoner held in an isolation cell would likely also face a combination of handcuffing, reduced food, water poured on the ground to ankle depth,being stripped naked, and beatings. No toilets are typically available in the cell, so prisoners use a bucket or even a paper bag for their excrement. Esther described the conditions:
They completely undress you, and pour water in there….It’s very cold in there because of the water. I have been there. In the cell, there is something that retains the water and there are so many mosquitoes breeding. The water is very cold, and your body reacts badly. One woman was taken there on her period—she was undressed, and she spent time in blood mixed with water.[192]
Being confined in an isolation cell, compounded with the abuses described above, has a serious effect on inmates’ physical and mental health. Inmates were described as “sick,”[193] “not well,”[194] “swollen,”[195] “yellow and with a rash on their body,”[196] with “burns,”[197] “moving in a zigzag,”[198] or “weak and can’t walk,” [199] after they had been put in isolation and subjected to other abuses including beatings. One prisoner at Luzira Upper said that he had seen three people die there since 2005 as a result of beatings or mistreatment prior to or during incarceration in the isolation cells,[200] but the deaths could not be independently verified. Another prisoner reported one inmate who had been confined to an isolation cell for two months began cutting himself with a razor blade.[201] “When they will take you to the cells, that’s when people change,” concluded Abdul.[202]
The most fundamental protection for prisoners in international and Ugandan[203] law is the absolute prohibition on torture and cruel, inhuman or degrading treatment. There is little doubt that the use of these cells to inflict punishment constitutes prohibited inhuman and degrading treatment. Extended use of these cells when combined with other punishments, such as handcuffing, being stripped naked, food restrictions, and being made to stand ankle-deep in water, constitutes a form of torture.[204]
Prisoners may also be confined in isolation cells (typically without being stripped or forced to stand in water) not strictly as punishment, but as a result of officers’ inability to appropriately handle and offer treatment for their mental health problems. At Jinja Main Prison, researchers found one prisoner with what a warden described as “mental problems” occupying an isolation cell, who informed researchers that he had “not been receiving medicine” and that he had not been seen by a medical professional or offered any treatment.[205] “We have an isolation cell for psychiatric cases or for those who have failed to be disciplined,” admitted the deputy OC at Jinja Main. But, he contended, “We base it on the medical staff to give us the right information.”[206] Tumwesigye described a fellow prisoner at Jinja Main, “not a very stable man,” confined in an isolation cell for a full year.[207]
Prevention and Treatment of Disease
All people have a right to the highest attainable standard of health,[208] and under international law, states have an obligation to ensure medical care for prisoners at least equivalent to that available to the general population.[209] States also have an obligation to meet a certain minimum adequate standard of prison health conditions and care to individuals in detention, regardless of a state’s level of development.[210] The Human Rights Committee, the monitoring body of the International Covenant on Civil and Political Rights, has determined that danger to a detainee’s health and life as a result of the spread of contagious disease and inadequate care constitutes a violation of that treaty.[211]
Under Ugandan law, prisoners are also entitled to “have access to the health services available in the country without discrimination.”[212] The UPS acknowledges its legal responsibility to ensure healthcare services equivalent to those available in the general population.[213] Yet, the prison medical authority admitted that equivalence does not currently exist.[214] HIV and TB, which occur at high rates in the prisons, pose particular challenges. Incomplete and delayed reporting of health conditions from prisons hinders the development of appropriately tailored interventions for these and other health conditions.[215]
Tuberculosis
For TB, the rate is almost two, three, five times the rate in the general community, depending on which region you look at…. The prisoners enter, it makes them worse, it makes those who haven’t come in with diseases acquire them. If we inappropriately handle them—causing drug resistance, as for TB—we act as a petri dish, then they just give it back to the community.
—Prison medical authority, Uganda Prisons Service, November 18, 2010
Transmission
The conditions in Ugandan prisons—combining overcrowding, frequent housing together of the sick and healthy, poor ventilation, and lack of natural light—facilitate the transmission of tuberculosis.[216] “If one prisoner has Tuberculosis (TB) in a room filled with 50 inmates, at the end of a day, everyone will be infected,” the commissioner general of prisons has said, according to media reports.[217]
TB prevalence, already high in Uganda’s general population, is significantly higher in the prison population. Uganda is ranked 16th of the World Health Organization’s 22 high-burden countries for TB worldwide[218] and in 2010 had a prevalence rate of 330 cases per 100,000 members of the population.[219] In 2008, the UPS and UN Office on Drugs and Crime (UNODC) estimated that Ugandan prison TB prevalence was 654 cases per 100,000, almost double national population prevalence.[220]
The Prisons Service acknowledges that TB education programs thus far have been limited.[221] However, the risk of contracting TB through the coughing of their fellow inmates was not lost on many of the prisoners. As Johnson, a prisoner at Bubukwanga who had coughed for the entire five months since he had been detained, said, “I am sure I could be infecting other people. You see, here we sleep in one room—sometimes 70 people, or 80. If you are sick, definitely you will infect others. If they are also sick, they will infect you.”[222]
Testing
We worry a lot when people are coughing that we might catch the disease. No one has ever checked us for TB here. Normally when the nurse comes and people complain about the cough, he says, “I don’t have the gadgets to test you.” He gives you some tablets and says, “Let’s see what will happen next.”
— Owen, Kitalya Farm Prison, February 28, 2011
Regular TB screening is a well-established cornerstone of prison health. Since 1993 the WHO has explicitly recognized the need for “vigorous efforts” to detect TB cases through entry and regular screenings in prisons.[223] On Human Rights Watch’s visits to Ugandan prisons, screening for TB was taking place only at a few of the reception centers located near larger towns.[224] The prison medical authority reported that entry screening had recently been scaled up to 21 prisons from three original pilot sites,[225] and he has plans to scale up entry screening for TB further.[226] But he admitted: “We are wondering why we stayed too long to do that. The findings are shocking.”[227] Outside the major reception centers, TB screening for prisoners upon entry is not taking place.
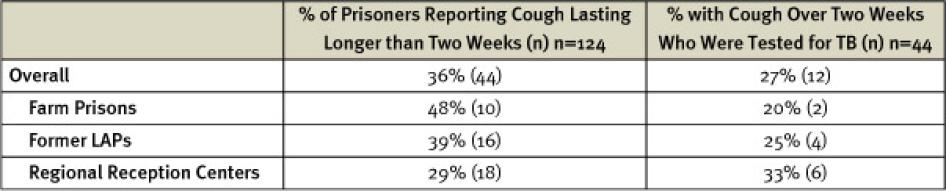
Twenty-eight percent of male prisoners and seven percent of female prisoners interviewed by Human Rights Watch said that they had been tested for TB during the period of their incarceration. Twenty-two percent overall, the percentage of prisoners tested for TB varied between categories of prison and fell to only 11 percent at former LAPs.
Just over one-third (36 percent) of prisoners interviewed said that they had coughed for longer than two weeks since incarceration, but nearly three quarters of these prisoners had not been tested for TB (28 percent had been tested). Some of those prisoners who had been tested had never received the result.[228]
Table 3: Prisoners Interviewed Reporting Cough Longer than Two Weeks Tested for TB
Case detection rates for TB in the UPS are unknown,[229] but it is widely acknowledged that infectious TB patients are not being identified. The director of the national TB program speculated: “TB missed? It must be big. Transmission in prisons may be 10 times higher than in the general population. When you miss one, it is catastrophic.”[230]
Preliminary results from a recent national drug resistance survey suggest that between one and two percent of TB cases are multi-drug resistant (MDR-TB).[231] In the prisons, testing for drug resistance exists only at Murchison Bay Hospital; the prison medical authority acknowledged that drug-resistant cases undoubtedly exist but are not detected.[232]
Treatment
Uganda has been making progress in treating TB in the general population, though significant gaps exist.[233] Among the prison medical facilities, only Murchison Bay Hospital is accredited to manage TB.[234] Elsewhere, the prison medical authority envisions that TB suspects will be transferred to regional prison health units, which will establish contact with nearby public health facilities or, where there is no regional unit, will be referred to the public health system. But as the prison medical authority admitted, “It could be possible there are those not on treatment.”[235]
Inconsistent or incomplete adherence to the eight-month treatment course risks creating drug resistance. Saul was told by medical personnel at the public hospital to stop taking his TB medication after two and a half months but was still coughing at the time of his interview.[236] Prison authorities reported that at least three prisoners died of TB in 2010.[237] Prisoners and prison officers at some prisons reported that there were no medications for TB available at the prisons or at nearby health centers for prisoners with TB.[238] As Gilbert at Kitalya Farm Prison noted, “The nurses tell us there is no medicine, but there are quite a number of them [prisoners] who do cough. I worry about it because those who are suffering from TB, they are here. They are not isolated, and they receive no treatment.”[239]
The development of drug resistance because of transfer to a farm prison, or upon release, is a major concern of prison health officials.[240] The prison medical authority has noted that inappropriate referrals to upcountry prison centers for hard labor of patients on TB treatment risk creating drug-resistant TB.[241] While Ugandan law provides for prisoners under medical treatment to be linked to medical or social services upon discharge,[242] and prison medical officers reported trying to make efforts to link discharged TB patients to appropriate services, they noted that those released from court and others were still released before finishing their course of treatment without being linked to services near their homes.[243]
HIV/AIDS
When I told the prison officer I was HIV-positive, he said, “Fight on, complete the sentence, go home, and get treatment.” It meant he can’t do anything for me. There were wardens I informed. They said prison has nothing to offer me.
—Robert, Masafu Prison, March 8, 2011
In 2009 Uganda had an adult HIV prevalence rate of 6.5 percent.[244] Prevalence in Uganda’s prisons is even higher: a 2008 study found a general prevalence of HIV among prisoners of 11 percent.[245] Yet human rights monitors have continuously found that prisoners have limited access to HIV testing and treatment.[246]
Transmission
Sexual activity occurs in Ugandan prisons. Male prisoners at Murchison Bay, Luzira Upper, Masaka Main, Muinaina Farm, and Kitalya Farm Prison, all larger prisons with longer-term inmates, repeatedly told researchers that they had heard of, witnessed, or participated in sexual relations and same-sex relationships between inmates, particularly involving prisoners in authority positions. Prison wardens and officials confirmed that sexual activity takes place.[247]
Most frequently, prisoners reported that lack of food and other basic necessities led inmates to trade sex for those items.[248] Gilbert concluded: “The cause is the conditions. Some people will receive visitors and be able to have something. They use the power of their resources to entice others with doughnuts or sugar.”[249] As Mukasa, at Luzira Upper, described, “These are the things that happen in a closed environment. There is some homosexuality…. As a young man, they give you tea, and you can end up giving in. They say, ‘You are now a woman,’ once they get you.”[250]
Prisoners also said that rarely they had heard of instances in which individuals were forced into sexual activity.[251] Given the heavy stigma attached to same-sex sexual relations in Uganda, according to Joshua, “Most of them negotiate. It’s very difficult for someone to force. They will catch you and punish you.”[252] Yet sexual coercion does occur. As one prisoner described, “Sometimes, when you are sleeping together in the night, you will feel someone touching you. Sometimes people are forced in the corridors during the day, but at night, if someone touches you, you shout.”[253]
In addition to being subjected to caning or confinement in isolation cells as punishment, prisoners found to be engaging in sexual conduct with others, whether discrete consensual acts or longer-term relationships, are subjected to sexual humiliation in some prisons. According to Jacob:
Sometimes when people are caught having sexual intercourse, they are put out in the field and made to walk around naked. The chiefs in the wards help to identify them. If you are caught red-handed, you are taken to the prison wardens. To try to control the activities, they have undressed those who are caught, and have made them walk around the [area surrounding the prison], to make them ashamed.[254]
International organizations—including WHO, UNODC, and the Joint United Nations Programme on HIV/AIDS (UNAIDS)—all recommend that condoms be provided to prisoners.[255] Homosexual sex is illegal in Uganda.[256] Its criminalization, itself a human rights violation, has the added result of creating stigma and fueling transmission of HIV, particularly as it leads prison authorities to deny condoms to inmates. UPS concludes that “notwithstanding the existence of incontrovertible evidence of MSM [men who have sex with men], the distribution of condoms to prisoners in custody is not possible….Exploring the possibility of introducing condoms within the existing legal regime will continue to be our priority.”[257] According to the prison medical authority, “I know our interventions are not as effective as we wish them to be—we are legally bound.”[258]
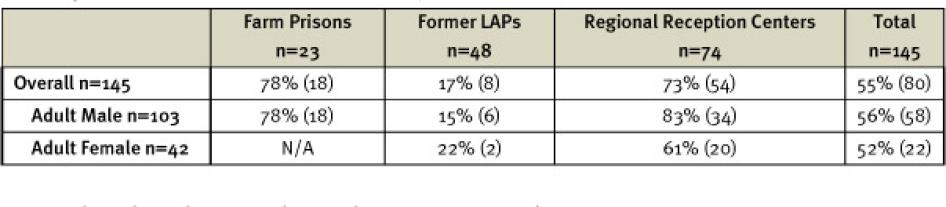
Testing
HIV testing has increased in some prisons in recent years, and overall, 55 percent of prisoners interviewed who did not already know they were HIV-positive when they entered prison reported having been tested for HIV during their incarceration. A prisoner entrusted with medical authority at Luzira Upper claimed that all new entrants are now offered HIV counseling and testing.[259] HIV testing at other prisons is offered in partnership with nongovernmental organizations.[260] Some prisoners also reported receiving diagnostic HIV testing at health centers when allowed to go out to receive healthcare.[261] More rural prisons, however, still lack completely both HIV screening upon entry and diagnostic testing for those who fall ill. At former LAP prisons, only 17 percent of the prisoners interviewed by Human Rights Watch had been tested for HIV during their incarceration. The prisons service acknowledges limited capacity for HIV testing because of inadequate staff, lab infrastructure, and lack of motivation among counselors.[262]
Table 4: Prisoners Interviewed Tested for HIV While Incarcerated, % (n)
Researchers heard reports that at those prisons conducting HIV testing, some prisoners were subject to mandatory testing, as opposed to the voluntary testing required by international best practice.[263] Enid, at Luzira Women’s, said, “Whether, you want it or not, you’re tested here.”[264]
Treatment
I’m positive. All the wardens are aware. Even the OC is aware. I’m not getting medicine. I used to get medicine. I left my medicine out there [outside of prison]. The warden beat me so much, I even fear asking to go to the hospital. Since my arrest up to now, I’ve not been taking my medicine.
- Matthew, Masafu Prison, March 8, 2011
Uganda has in recent years scaled up treatment, though significant challenges remain.[265] Estimates as to the number of prisoners receiving HIV treatment vary significantly.[266]
In 2011 prison-based ART services were only provided at Murchison Bay Hospital to residents of the Luzira/Murchison Bay Prison complex in Kampala. HIV-positive prisoners at other prisons were intended to access services at outside community clinics[267] or to be referred to a regional health facility (where they would access services at public facilities) or to Murchison Bay. The prison medical authority highlighted the HIV treatment gaps: “Upcountry, we don’t have any prison health unit accredited for ARVs. If you are positive and on antiretroviral drugs [when you come into prison], you would be in trouble. There is no mechanism for you to get these supplies….We have those who are positive. But no counselors, no access to public health facilities. What do we do?”[268]
Table 5: HIV Treatment by Prison Type for Prisoners Interviewed
Among prisoners interviewed, 18 (11 percent) self-identified as HIV-positive. Of these, 22 percent were receiving no treatment of any kind, and 50 percent were not receiving ART. The OC at Muduuma Prison confirmed that the prison held HIV-positive prisoners, but they received no ART, as it was not available at the nearby public facility.[269] An HIV-positive prisoner at Muduuma reported:
We, the sick ones, remain in the wards, and the OC comes to inspect. The only thing she does is to say not to go to work….With the OC, I’ve raised the matter [of my HIV-positive status and lack of medication] twice, but she doesn’t come inside the ward, only peeps inside and says, “How are you?”[270]
Prisoners reported deaths of HIV-positive fellow prisoners as a result of inconsistent or denied treatment.[271] Prison authorities indicated that at least three prisoners died of HIV/AIDS in 2010.[272] However Human Rights Watch was unable to verify claims of inmate deaths as a result of denials or lack of medication.
Rural prisons did not always immediately transfer HIV-positive prisoners to Murchison Bay. At Kitalya Farm Prison, seven HIV-positive inmates were receiving only Septrin while awaiting transfer on the day Human Rights Watch visited, but transfer was not immediate. Human Rights Watch researchers saw at Kitalya referral forms of prisoners who had been waiting for over a month to go to Murchison Bay. [273] At Muinaina, the OC reported that HIV-patients “in the early stages” received Septrin and continued to work, while “when it gets complicated, that’s when we have to take them to Murchison Bay,” but acknowledged: “CD4 testing, it’s difficult to monitor.” [274] While some HIV-positive prisoners were transferred to Murchison Bay, they were sometimes returned to their farm prisons, where treatment remained unavailable.
Even at Murchison Bay Hospital, medical staff reported that due to inconsistency in the drug supply[275] (ARVs come from the national medical stores), they are currently only starting patients with a CD4 count less than 250 cells/mm3 on ART, rather than following the national and international standard of less than 350 cells/mm3.[276] The chief physician explained that if national guidelines were followed, “so many would require it, it is not sustainable.”[277]
A high level of adherence is crucial for the success of ART.[278] Lack of adherence can lead to the development of drug resistance, illness, or death. But while many prisoners reported receiving their HIV medications regularly, five HIV-positive prisoners interviewed said they had missed doses. Reasons included drug stock-outs,[279] lack of food,[280] being prevented from going outside to access community-based care,[281] or transfer between prisons.[282] At times, prisoners share drugs to cover the shortfall.[283]
Gerard, an HIV-Positive Patient Sent from a Rural Prison to Murchison Bay Prison HospitalI came in when I knew I was HIV-positive. I had swellings on my elbows and legs, and then I also feel paralyzed once in a while. By the time I was arrested, I was using Septrin, and I didn’t get it. I spent three weeks at Sentema [Prison], and there was no medicine.... They wanted me to go and dig—I told them I was sick… they did not believe me. I showed them my swollen fingers—they said, “We shall step on those fingers so they heal.” I insisted, so they left me. The following day, the swelling continued, and they realized—it was after two weeks when they took us to a clinic outside the prison—they didn’t check me, but they asked me which type of medicine I used. I said Septrin, and they gave me a few tablets. But the following day, there was no medicine. When I stopped taking my medicine, that’s when I felt weak, and my body started shutting down completely. I think they looked at me and thought I was useless at their shambas [fields]; the kind of sickness I had would not allow me to go and work. They decided to get rid of me. The OC at Sentema saw me and I could not walk any more. He said I should be transferred to Murchison Bay, and on that very day I was brought here. When I arrived here, on that very day I was taken to the hospital, and they admitted me. They gave me some tablets—Septrin—they gave me Septrin that very day. The following day, they checked me: They took my blood sample, told me I was HIV-positive, and checked my CD4 count. They said it was very low, 180. They said they were going to put me on a different medicine, but I had to wait, and they kept treating me. This month, they put me on ARVs—it was after two months since they checked me, I don’t know why it was so long. In the beginning, I did not feel very good, but now I’m getting better. I used to move on crutches…but now I can walk on my own, and the body is no longer so weak. I have had difficulty taking my medicine because of lack of food. The problem you get is when you take the medicine, you feel it in your stomach. You would love to eat, but you have to wait. It becomes problematic. Sometimes, I don’t take it because of that. Sometimes, I force myself to because I have no option—I want my life.[284] |
Water- and Insect-Borne Diseases
Malaria
Together with HIV and TB, malaria is one of the leading causes of morbidity and mortality in Uganda’s general population.[285] While national health guidelines call for malaria prevention through use of methods including insecticide-treated nets and indoor residual spraying,[286] such measures have not been adopted in prisons. In the prisons, bed nets are not allowed for male inmates because prison authorities fear they could be used as ropes or nooses,[287] and even among female inmates interviewed by Human Rights Watch, only 29 percent said they had slept under a mosquito net on the preceding night.
Indoor spraying for mosquitoes has only been conducted by the prison administration at three prisons, with help from the International Committee of the Red Cross (ICRC),[288] though even at one of the ICRC’s sites, on the day of Human Rights Watch’s visit, researchers were informed that “the mosquitoes are there because the spray is out of stock.”[289] Prison officers elsewhere expressed a desire to spray for mosquitoes but had not done so because they had not received spray.[290] At some prisons, prison officers had attempted to put screens in the windows, though prisoners sometimes pierced these to relieve the heat in the congested wards.[291] The prison medical authority said that the UPS had allocated 100 million Uganda shillings (approximately $40,000) for FY 2010/2011 to fumigate and was “working out a mechanism,” but distribution of spray had not taken place.[292]
Prevalence is unmeasured but likely very high.[293] Prison officers reported that malaria is common among prisoners[294] and indeed is the most common ailment they observe.[295] “When I came here, half the population was sick with malaria,” one prison OC observed.[296] Between the four-year period of FY 2005/06 to 2008/09, Uganda’s auditor general calculated that 11 percent of deaths reported in Uganda’s prisons were caused by malaria.[297] As with TB, HIV-infected individuals are particularly vulnerable to malaria.[298]
However, treatment is frequently unavailable[299] and capacity hampered by drug stock outs.[300] Reported George, at Mutufu, “There are many who are suffering from malaria. If you don’t have money [to buy your own medicine], you just sleep in the ward and just keep there. The OC will tell you, ‘If you don’t have money, you will die.’ You will not get the medicine.”[301]
Hygiene- and Sanitation-Related Illness
Poor water and sanitation also lead to the spread of disease.[302] Prisoners reported and statistics confirmed that they had seen cholera outbreaks and frequent diarrhea.[303] The UPS has determined that “diarrhea diseases are a major cause of morbidity and mortality among prisoners” as a result of the continued use of the bucket system at the majority of prisons.[304]
Skin diseases are also common. Throughout the prisons, proper hygiene with limited government-provided soap is difficult, and lice and scabies are rampant.[305] Human Rights Watch regularly observed prisoners with significant skin problems, scratching throughout interviews. Jonathan at Masaka Ssaza Prison said, “There are so many lice…they say that the lice are the security guards of the prison.”[306] Prison medical officials accept that skin diseases are common.[307] At Masaka Main Prison alone, which has a population of 630, a medical officer reported seeing between 100 and 150 cases of skin infections a month.[308] However, prisoners frequently reported skin diseases that had gone untreated.[309]
Non-Communicable Health Conditions
Women’s Health
In addition to experiencing the problems accessing care faced by all inmates, women have a distinct set of healthcare needs and challenges in detention.[310] Women detainees benefit from special legal protections. Uganda became a party to the Protocol to the African Charter on Human and Peoples’ Rights on the Rights of Women in Africa (also known as the Maputo Protocol) in July 2010.[311] This provides that women in detention should be held in an environment “suitable to their condition” and ensures their right to be treated with dignity.[312] International standards dictate that women in detention should receive “special accommodation for all necessary prenatal and postnatal care and treatment.”[313] Yet as a minority in prison settings, women often receive little attention.[314]
Female prisoners who were pregnant or had given birth in prison reported that prenatal care was frequently unavailable or inadequate. Christine, six months pregnant at Fort Portal Women’s Prison, reported that she had asked daily to see a doctor for the pain she was experiencing and blood in her urine but had been refused.[315] Lydia, six months pregnant, had received no prenatal care for the month and a half she had been in prison.[316] Women at Luzira Women’s receive prenatal services at the staff clinic, the only prison-based facility offering delivery services (Murchison Bay Hospital is all-male);[317] but even there, female prisoners claimed that care was inadequate.[318] Postnatal care is minimal: Grace said she was forced to return to the prison two hours after giving birth at a hospital.[319] For women who are not pregnant, gynecological care is unheard of.
HIV testing for pregnant women suffered from numerous problems. Pregnant women reported “mandatory” testing in some instances.[320] In others, testing was either not offered[321] or the results were not shared with the woman who had been tested.[322] Prevention of mother-to-child transmission of HIV is available only through prison health services from the Murchison Bay staff clinic; or “if the situation allows, she can access the public health facility.”[323] The WHO protocol for PMTCT notes that even among HIV-infected pregnant women who do not require ART for their own healthcare, “ARV prophylaxis should be started from as early as 14 weeks gestation.”[324] Yet some HIV-positive pregnant inmates described treatment in violation of WHO guidelines. Hellene, a 16 year-old who was six months pregnant, reported: “After the [HIV] testing, they told me I was positive.… I have no ARVs. They give me panadol, Septrin.…PMTCT? They have never discussed with me.”[325]
Pregnant inmates—nearly all of whom said that they were forced to work in the fields—also have their health particularly impacted by hard labor conditions and abusive punishments.[326] At Fort Portal Women’s Prison, two female inmates separately described an incident in which a fellow inmate had a miscarriage at eight months pregnant, a result they believed of her forced hard labor and denial of healthcare.[327] Overall, 30 percent of female inmates interviewed by Human Rights Watch said they had been beaten, including eight pregnant inmates.[328] Hellene, the 16 year-old remandee at Butuntumura Prison who was six months pregnant, described being beaten in the stomach by a warden while digging, necessitating a trip to the hospital.[329] Mary, at Jinja Women’s Prison, reported being beaten and kicked while seven months pregnant, also leading to a hospital visit.[330]
Mental Health
Before coming in [to prison]...I was taken to Butabika dispensary mental health center, some time long ago. I was given a dosage, I was admitted. The doctors were coming to see me. [Now] no one is taking me back. At Butabika, very much good for my body, the drugs.... My spirit tells me to move to Butabika. I should walk to Butabika. That hospital is different from this one here. My spirit is telling me to go.
—Mutebi, Muduuma Prison, November 12, 2010
Ugandan criminal law exempts anyone with “any disease affecting his or her mind incapable of understanding what he or she is doing or of knowing that he or she ought not to do the act or make the omission” from criminal liability.[331] Courts may order accused people to undergo psychiatric assessments to ascertain competency to stand trial,[332] but there is a backlog of prisoners awaiting these determinations.[333] The prison medical authority admitted, “We are mindful we are flouting existing regulations of not having the mentally sick.”[334]
Human Rights Watch found that inmates who could not answer basic questions about their charges, length of incarceration, or age were undergoing criminal prosecution with no legal representation.[335] Additionally researchers found 11 inmates detained indefinitely awaiting action from the Minister of Justice following a ruling of not guilty by reason of insanity.[336]
Nationally, UPS estimates that five percent of prisoners have “mental problems” upon entry.[337] Prisoners and prison officers described that inmates also develop mental health problems following entry into prison.[338] UPS attributes the high burden of mental health problems in prison to a combination of “the association between substance abuse and criminality” and the “high psychological and emotional stress” associated with incarceration.[339] The president of the Uganda Medical Association, a psychiatrist who has previously provided mental health services at Murchison Bay, noted that mental health problems are very prevalent in the prisons, particularly anxiety and depression, as a result of mistreatment upon arrest and the “mental torture” of long remand periods.[340] Prison statistics indicated at least two deaths by suicide in 2010.[341]
At upcountry facilities, mental healthcare is almost nonexistent and, if it exists, is dispensed by the prison OC, a position with no medical training.[342] Prisoners repeatedly described receiving no or inadequate mental healthcare themselves or for their fellow prisoners. “Many get lost. Forget about upcountry, there’s nothing going on up there [in rural facilities],” concluded the president of the medical association.[343]
Prison officers outside of the major regional centers or Kampala by policy are supposed to send serious cases of mental health problems to regional units or Murchison Bay for treatment or analysis of competence to stand trial.[344] Over 140 prisoners at the Luzira prison complex are diagnosed with some form of mental health problem, including those with schizophrenia and severe mental disabilities who “have stayed for years in prison.”[345] But even at Murchison Bay and at regional centers, mental health services were grossly inadequate.[346] Treatment based entirely on provision of medication, without any psychotherapy or alternative mental healthcare, was inferior to that available at the public mental facility, Butabika.[347]
III. Addressing the Causes of Poor Health in Uganda’s Prisons
Criminal Justice Failures
Prolonged Pretrial Detention
Last time I was in court was October 31, 2002, when I was committed…. Can you help me find my way to court?
—Edward, a prisoner awaiting resolution of his case for almost nine years, Muinaina Farm Prison, March 4, 2011
The heavy backlog in the criminal justice system results in overcrowding in prisons,[348] and prolonged periods of time on remand have adverse effects on prisoner health. Despite international legal requirements that pretrial detention be “an exception and as short as possible,”[349] in Uganda, suspects may wait in prison for years for their trials to be resolved. Fifty-six percent of all inmates are on remand, incarcerated awaiting resolution of their case.[350] The average wait is estimated at one year and three months for capital offences, such as defilement,[351] murder, aggravated robbery, rape, and treason.[352] The average wait for lesser offences, such as assault and theft, is three months.[353]
Table 6: Months in Detention for Remand Prisoners Interviewed
As a first step upon arrest, international and regional law provide for the right to be brought before a judge, and to be charged or released.[354] Under Ugandan law, a suspect must be charged by a court within 48 hours of arrest.[355] Yet, 85 percent of prisoners interviewed by Human Rights Watch had not been brought before a court for an initial appearance within 48 hours, and prisoners reported having waited significantly longer.[356]
Table 7: Interviewed Prisoners’ Appearance before a Judge or Magistrate
Human Rights Watch researchers spoke to seven individuals who had been awaiting resolution of their cases for over five years,[357] and seven prisoners who said they had not set foot in a courtroom in over two years.[358] The remand prisoners that Human Rights Watch interviewed had been awaiting resolution of their cases for a median of five months and mean of 15 months. Prisoners find themselves in a position of deciding whether it will be faster to plead guilty and serve a sentence than to plead not guilty and await trial, later to be found innocent. Several described pleading guilty in order to hasten their release.[359]
Long remand times result from several problems within the judicial system, all of which contribute to large prison populations.[360] An insufficient number of judges has led to too few court sessions.[361] In Mubende district, where the High Court sits for only two months a year, the lack of a High Court judge has led to average remand periods of five years at Muinaina Prison.[362] Despite constitutional guarantees of a speedy trial,[363] prisoners languish in detention for long after their cases have been committed to the High Court for trial before any trial begins,[364] and partially heard trials continue indefinitely without complainants or witnesses appearing in court. Prisoners said their trials adjourned repeatedly without any progress.[365] Ekanya said, “I have been to court 16 times…. There is no evidence during trial. The complainant hasn’t come to court. I stand up, then they say go back. Then they say come back on such-and-such a date.”[366] Civilian cases in the military court system trying gun crimes—in itself a violation of international law—progress particularly slowly, given the court’s few sessions.[367]
The Justice Law and Order Sector (JLOS), a group of government bodies including the judiciary, police, prisons, prosecution, Uganda Human Rights Commission, Ministry of Justice and Constitutional Affairs, Ministry of Internal Affairs, and international donors, has been concentrating its efforts through a “Case Backlog Quick Wins” project to reduce the case backlog, particularly by weeding out non-meritorious cases lacking evidence during investigations, appointing more judges, and holding more court sessions, resulting in the clearing of 80,000 cases between March 2010 and March 2011.[368] However, the number of new cases continues to outpace the clearing of old ones, and the backlog continues to grow at 8.5 percent per year.[369]
While the Ugandan constitution provides for a right to bail, few defendants have the opportunity to request bail, increasing the burden on the prison system.[370] In non-capital cases, suspects can represent themselves and orally request bail at magistrate’s court.[371] Suspects in serious cases, meanwhile, can be detained for an indeterminate period of time until their case is sent, or “committed,” to the High Court for trial.[372] During this time, defendants who are unable to afford a private lawyer are effectively prevented from exercising their right to bail because they are brought before a magistrate’s court first, which does not have jurisdiction over the case and therefore cannot hear a bail application. A suspect can apply for bail before the High Court, a complex process often requiring legal help which is prohibitively expensive for most defendants.[373] However, it must be noted that a recent proposal by Ugandan President Museveni, if enacted, would amend the constitution to eliminate bail entirely for suspects accused of crimes including rioting and economic sabotage, in addition to rape and murder.[374]
Only six percent of all prisoners interviewed by Human Rights Watch had ever been released on bail. Seventy-four percent of prisoners interviewed said that they were never offered bail. Eighteen percent said that they were given the option of bail but were unable to afford cash bonds or to post sureties.[375]
Judges also interpret the constitutional provisions on bail as allowing them to impose a mandatory period of detention on remand before bail applications can be heard.[376] Numerous prisoners told Human Rights Watch that magistrates had informed them they were not entitled to apply for bail until they served a minimum period of time on remand.[377] One prisoner who had been on remand for a year and four months was told he had not spent enough time on remand to qualify for bail.[378] Prisoners complained of corruption in the bail system, either through the payment of bail money which did not result in bail or which was never returned to them.[379]
A lack of legal representation also contributes to prison congestion. For serious offences punishable by death or life imprisonment, the state must provide legal representation in courts (referred to as “state brief” lawyers).[380] However, Ugandan law does not specifically stipulate when in the process the right adheres, and in practice suspects rarely meet with their lawyers until the commencement of trial.[381] A handful of nongovernmental organizations provide legal advice in prisons, but their reach is usually constrained to large prisons near larger towns.[382] JLOS’s development partners have found “most disappointing…the continued delays in the development of a legal aid policy.”[383]
Without lawyers, individuals are unable to advocate for bail, request dismissal on the basis of lack of evidence or advocate for a reduced or non-custodial sentence.[384] International standards mandate that people who are charged with a criminal offence be informed of their right to have access to a lawyer.[385] However, only 21 percent of defendants interviewed by Human Rights Watch had been represented by a lawyer. More than three quarters (79 percent) of prisoners who ever had a lawyer had been represented by a government state brief lawyer, and those who did have a state brief lawyer only met the lawyer at trial. Prisoners often said they tried to speak for themselves in court, only to be told by the judge or magistrate they were not allowed to do so.[386]
Corruption in the criminal justice system, particularly bribery and extraction of fees for free services, is reportedly widespread,[387] leading JLOS’s development partners to state they were “disappointed by the lack of meaningful progress in implementing a sector anti-corruption strategy.”[388] Numerous prisoners told stories of rampant corruption throughout the justice system, starting from the time of arrest through trial, eroding their trust in the system to process their cases with good faith or any measure of speed.[389]
Unnecessary and extended pretrial detention imposes significant financial costs on the government, and savings could be generated by increasing the option of bail instead of pretrial detention, freeing up money for crucial social services.[390]
Detention Following Conviction
For defendants who have been convicted of some lesser crimes, community service as a non-custodial option exists, and, in 2010, 11,000 cases were granted community service options.[391] JLOS reported that “[t]he public now support community service as punishment and appreciate its impact in reducing the rates of recidivism.”[392] However, the commissioner of community service stated that the success of his program depended heavily on “the personality of the magistrate” and his or her willingness to use it as a sentencing option.[393] Two prisoners told Human Rights Watch that they were advised by a member of the community service program to plead guilty and ask for the option, only to be later sentenced to prison time instead, when the prosecution and magistrate failed to agree.[394] Hassan said,
After some hundred days, while I was appearing in court, someone came in and advised me that if I accept the case, the sentence will be minimized with a community service agreement. It was a lady from a project related to community service….I admitted, was sentenced, but later realized I had made a mistake because I did not do the crime. That lady talked to all of us, but I was the first to appear. When I was sentenced, the others refused to say they were guilty. She was not a lawyer, but she had assisted others who were being released. She told us she had talked to the magistrate, perused our files, and was conversant with the case and the evidence.[395]
For prisoners who have been convicted and sentenced to a custodial term, there is no parole system in Uganda.[396]
Under international law, everyone convicted of a crime has the right to have his conviction and sentence reviewed by a higher tribunal according to law.[397] However, numerous prisoners described filing an appeal and hearing nothing in response, despite waiting for years.[398] A paralegal working with prisoners said, “No response to appeal?—that’s just a lack of follow up. People with money to get legal representation get justice.”[399]
Detention of Children
Sometimes, children are also detained with adults in Ugandan prisons. Human Rights Watch found six people who said they were children currently being detained with adults in three different prisons, in addition to four young adults who said they had been detained in adult prisons since they were under 18.[400] Detention of children with adults is prohibited under Ugandan and international law[401] and carries severe risks for children, including the potential for violence and sexual abuse.
Determining a child’s age is not a straightforward matter in Uganda. Fewer than four percent of children have a birth certificate despite the state’s obligation to register births.[402] Ascertaining age is an arbitrary process, either based on appearance or inspection of teeth. Because of the logistical difficulties in handling children, police often inflate their ages.[403] Only one of the children interviewed by Human Rights Watch was ever given the opportunity to present evidence of her age.[404] When Human Rights Watch raised concerns about the ages of two prisoners remanded at Bubukwanga Prison with the magistrate, the children were released when they were produced before court, which agreed that they were under age 18.
Prisons Service Failures of Management and Health Services
The Role of Prison Officers in Denying and Delaying Care
When you want to go to the hospital, you tell the wardress. But for the time I have been here, I have never seen any person taken to hospital. It is so close, but the wardress just gives us panadol. When you tell them you want to go to hospital, they just beat you. They say, “Is this a hospital?”
—Nathan, November 12, Muduuma Prison, 2010
Prison wardens and officers in charge play a direct role in denying or delaying prisoners’ access to appropriate medical care.
Ugandan law provides that the OC, on the advice of the medical officer, may order a prisoner to a hospital.[405] As of March 2011, only 63 of Uganda’s 223 prisons had any on-site healthcare worker, covering an estimated 17,741 prisoners at upcountry units and 4,500 at the Luzira complex.[406] But for those at prisons without medical facilities or for those with more serious ailments that could not be dealt with at their prison health unit, prisoners across facilities repeatedly described that prison wardens act as gatekeepers. Wardens denied or delayed inmates’ access to community medical facilities because of suspicions that prisoners were using ill health as an excuse not to engage in forced labor, as a pretext for escape,[407] or for more malicious motivations: Mary, a pregnant inmate at Jinja Women’s Prison, was not allowed to return to the doctor after the doctor told wardens that their beating had “dislocated her pregnancy.”[408]
Delays sometimes last up to a month[409] before wardens will accompany a prisoner to care and at some prisons, access to outside facilities was denied entirely.[410] The prison medical authority acknowledged: “It is so amazing, a health facility which could be 100 meters away from a prison is not accessed by the prisoners. Those things happen. Some of them, it is a lack of responsibility. Why should you deny me to walk 100 meters away?”[411]
In practice, even when medical personnel are present at the prison and do recommend that a prisoner be allowed out to access medical care, a non-medical officer may well override the recommendation of his or her medical colleagues. A medical officer told Human Rights Watch that at the time of the year when Ramadan and Christmas are being celebrated, the escape rate is higher and “they [the wardens] argue with us to reduce the rate of referral.”[412] The prison medical authority admits that there is little integration between medical and non-medical workers and a “lack of sense of ownership of the responsibility and mandate over healthcare issues” exists on the part of OCs.[413]
Prisoners reported that in the time they had waited for medical care, their conditions had deteriorated significantly. Esther said her baby’s fingers had to be amputated because of the delay in allowing her go to the nearby hospital.[414] Prisoners even claimed that deaths occurred as a result of delayed access to outside facilities, claims that could not be independently verified by Human Rights Watch. At Masaka Main Prison, prisoners reported the recent death of an HIV-positive prisoner who had requested care and was taken to the prison-based clinic, only to be refused access to the community hospital and taken back to the ward, where he died.[415] As Peter recounted:
He spent the whole day requesting to go to hospital. He said if he was to die, let him die in hospital. But the guards refused to take him. They knew he was suffering from HIV. Late in the evening, they locked us in the wards. A few minutes later, [he] fell and died. The guards were saying, “You’re afraid of going to court, so you want to go to hospital and escape from there.”[416]
The prison death register confirmed the death in September 2010 from “HIV stage 4 with psychosis” with the cause of death listed as “multiple organ failure.”[417]
Prisoners falling seriously ill in the night are sometimes denied immediate access to care, and have to wait until the following day,[418] including female prisoners experiencing labor pains at night. [419] Inmates reported that, during the nighttime, they had seen their colleagues die,[420] claims Human Rights Watch could not fully verify. Mafabi, at Butuntumura Prison, said: “In September, there was a prisoner who died in full view. He fell sick at night, and we called the wardens, who said ‘wait until tomorrow.’ During morning parade, they carried him out and put him on the ground.”[421] Inmates forced to watch their fellow prisoners suffer in the night said that they tried to treat them with whatever medications they had available.[422]
Prisoners were sometimes not allowed to receive medicines purchased by family and friends on the outside, even when the prison was unable to provide them with appropriate medications.[423] The prison medical authority claims that prisoners are allowed to bring in drugs if the health workers are in contact with their relatives. However, where there are no health workers, “I don’t know what happens there.”[424]
Prisoners with serious ailments also reported they have been denied or delayed access to Murchison Bay or regional prison health referral facilities. Prisoners reported that they or their colleagues waited up to six months[425] for transfer. While admittedly transport unavailability is a challenge,[426] upcountry officers’ incompetence or malice in delaying or denying referrals to prison referral facilities are also to blame for the poor health outcomes.[427] During the time waiting for transfer, a prisoner reported that his head was oozing pus,[428] another that his skin was “peeling off,”[429] another that he was in such terrible pain he was not able to sleep or eat properly,[430] and another that he was unable to walk or move.[431] Medical workers confirmed that in some cases delayed referrals lead to death on arrival at Murchison Bay: “Absolutely we have had delays…and when they occur, they are inappropriate. When he reaches here, and is declared dead, it is not a surprise.”[432]
Once ill prisoners have reached a facility where they can receive treatment, though, they cannot rely on or expect continuous or consistent access to it. It is common practice to transfer sick inmates to upcountry prisons despite there being no healthcare facilities. Coordinating the transfer of prisoners is the mandate of recipient OCs—at Murchison Bay or regional centers—to ease congestion or facilitate work, and is conducted without consultation of trained health workers. The prison medical authority concluded, “You end up having sick people transferred from a facility that offers service to the prisoners for years to an area without. How inhuman can you be?”[433]
Failures in the Delivery of Prison Health Services
To its credit, the UPS has made a marked effort to improve prison medical care in recent years, particularly at the large facilities in regional centers. Yet major gaps remain. At rural, former local administration prisons, often no medical care is available. The deputy OC at Bubukwanga Prison said the prison had no medical staff, no medicines, and no idea who was sick.[434] A medical officer at Masaka Prison noted that, while regional units had supervisory duties over lower units, because of limited funds, “those that are far, we don’t go there. In the faraway units, healthcare is poor.”[435] Only panadol and other basic painkillers, dispensed by the officers, were sometimes available (but quickly exhausted[436]).
Even at prisons with associated medical facilities, obtaining care is far from a sure thing. Health infrastructure at most clinics is “dilapidated” or “make shift” and aside from Murchison Bay, only three of ten regional referral health units even have lab services.[437] X-ray and CD4 count facilities are currently lacking at the regional level,[438] and Murchison Bay lacks an adequate operating theater.[439]
Adequate staffing is a major challenge. At all facility levels, though significant improvements have been made,[440] human resources for health fall far short of the prisons service’s stated needs.[441] UPS employs only six physicians (none of them at upcountry units).[442] Prisoners contend that health staff frequently do not see those who come to them for treatment.[443] Ali, at Murchison Bay Prison, lamented, “The doctors are nowhere to be seen.”[444]
Prisoners at prisons with associated health units told Human Rights Watch that the medicines they needed were frequently unavailable[445] or only partially provided.[446] “You get half-treatment,” Yusuf, at Murchison Bay, concluded.[447] Prison authorities confirmed that problems remain with inadequate access to medications for prisoners, particularly in prisons outside of Kampala.[448] UPS has concluded that the number of health units reporting stock outs of essential medications remains high for reasons including low per capita expenditure.[449] Access to supplies at upcountry medical units from the national drug stores via neighboring Ministry of Health facilities has also “failed.”[450] Uganda’s auditor general has concluded that UPS provision of free medical services to non-prisoners in neighboring communities has a significant negative effect on the resources available for prison health and should be halted.[451]
Funding for referral services is also inadequate.[452] Some prisoners said that, despite the fact that all medical services are to be offered free of charge,[453] when they are taken to Mulago public hospital in Kampala for specialized medical care they are asked for money and denied treatment when unable to pay.[454] The OC at Murchison Bay acknowledged delays in prisoner treatment at Mulago because of the process for funding approval: “By the time they are worked on, it is not even meaningful.”[455]
Donor Funding to Ugandan Health and Prisons
Uganda is a recipient of significant international donor aid, particularly for health. In 2009, Uganda received over US$1.7 billion in bilateral and multilateral donor aid.[456] Health-related, and particularly HIV-related, donor funding to Uganda has been led by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). In FY2010, PEPFAR gave over $280 million to Uganda for AIDS relief,[457] with disbursements from 2004 to July 2010 totaling $1.4 billion.[458] The United States (US) contributes approximately 70 percent of all funding for HIV/AIDS activities in Uganda.[459] In 2007, 93 percent of Uganda’s funding for HIV came from international bilaterals; in 2008 they contributed 83 percent.[460]
However, little funding has been donated to prisons. Total donor funding between FY 2005/06 and FY 2008/09 for UPS fell from 2.11 billion shillings (approximately $875,000) to 0.72 (approximately $300,000), just 1.5 percent of the total prison budget for that year.[461]
While some donor initiatives have been executed or planned for health in Ugandan prisons, their scope is minimal compared to overall health funding to Uganda and given the high rates of HIV and TB infection among the prison population. According to Uganda AIDS Commission estimates, approximately $28 million would have been required to fund comprehensive HIV/AIDS interventions in Uganda Prisons and Police Services from 2007/2008 to 2011/2012; however, actual contributions from external partners totaled only one percent of this amount, and pledges approximately 10 percent.[462] Prison authorities have noted the need for increased funding to fight both HIV and TB.[463]
Officially, UPS’ health division has a number of partners,[464] but undoubtedly the largest monetary contributors are the International Committee of the Red Cross and the U.S. Centers for Disease Control and Prevention (CDC)/PEPFAR. The ICRC has helped to improve water and sanitation and has upgraded HIV, TB, and malaria services at Fort Portal, Luzira Upper, and Gulu Prisons;[465] their support has been extended for two years at $70,000 per year.[466] The CDC has made a five-year commitment to the prisons, between 2009 and 2014, of US$1.6 million, but less than half of the money from the first two years has been absorbed by the UPS because of a delay in the process of creating the prevalence and risk behavior survey on which interventions will be based.[467] Between the ICRC and CDC projects, the UPS should, in theory, receive monetary donor contributions of $390,000 for health over the government-provided budget.[468]
IV. Recommendations
We need resources. But it would be unfair on my part to really stand up and complain we can’t improve the situation because there are no resources. There are many things we can do without resources.
—Prison medical authority, Uganda Prisons Service, March 11, 2011
Improving health in Ugandan prisons will require significant changes on the part of the Uganda Prisons Service, and will also require improved coordinated efforts of the Ugandan government, civil society, and international agencies and donors. Some reforms are resource-neutral; those that are not are crucial to the realization of the rights of prisoners and are the responsibility of both the national government and international donors.
To the President of Uganda
Issue direct orders to the UPS to stop the use of compulsory prison labor by private landowners or prison authorities and to halt the use of abusive punishments
Order an independent inquiry into corruption and use of compulsory labor in the UPS and hold those responsible for the illegal use of forced prison labor accountable
To the Uganda Prisons Service and Ministry of Internal Affairs
Immediately:
- Issue direct orders to stop the use of compulsory prison labor for private landowners and prison authorities
- Investigate and demand accountability for funds raised through prison labor
- Align prison labor practices with
Uganda’s international legal obligations by:
- Halting the use of remand prisoners for labor
- Preventing labor for any private entities, whether by convicts or remands, unless with their consent and with fair remuneration
- Providing male convicts between 18 and 45 engaging in prison labor with terms similar to those free laborers receive in terms of hours worked, conditions of work, and remuneration
- Reform prisoner disciplinary systems by:
- Declaring a zero tolerance policy on the beating of prisoners effective immediately and warning that officers and inmates judged to have inflicted corporal punishment will be prosecuted and punished
- Discontinuing the practice of stripping inmates naked, handcuffing, beating, or holding them in water while in isolation confinement and punish officers found to have engaged in such practices
- Ensuring detainees are able to send confidential complaints to the Uganda Human Rights Commission and other organizations and that all prison officials are aware of this right and do not interfere with it
- Investigating all complaints of abuse against inmates suspected of or charged with same-sex sexual conduct and taking appropriate action against those found responsible for such abuse
- Carry out regular monitoring visits led by headquarters and medical staff, with better defined indicators and targets for prison inspectorate monitors, to ensure the health and well-being of prisoners throughout the country and a halt to corrupt labor practices
- Ensure that conditions of confinement meet
international standards, including by taking immediate action to improve basic
prison conditions by:
- Providing food of improved nutritional content, including rations for children, and additional rations for pregnant prisoners; prisoners with HIV, tuberculosis, and other health conditions requiring nutritional supplements; and inmates engaging in hard labor
- Providing prisoners with basic necessities including adequate uniforms, blankets and mattresses, soap, and toothbrushes
- Providing prisons insecticide to spray regularly for mosquitoes
- Ensuring separation of convicted and unconvicted detainees
- Address prison health by:
- Instructing all OCs to accept primary responsibility for inmate health, including facilitating inmates’ access to community or prison referral health facilities, with disciplinary penalties for failure to do so
- Creating guidelines to ensure that inmates receive health screenings prior to transfer to rural prisons and that ill inmates are not transferred to prisons lacking adequate healthcare facilities
- Scaling up TB screening to all inmates entering prison, and all existing inmates, through targeted surveys, sputum analysis, and, if needed, chest x-ray evaluation
- Offering voluntary HIV counseling and testing to all inmates entering prison and all existing inmates
- Ensuring prompt initiation of treatment at either community- or prison-based facilities for those with confirmed HIV or TB
- Establishing guidelines for referral of all prisoners with confirmed HIV or TB to regional units and ensuring patients on treatment are not transferred away from prisons with treatment capacity
- Establishing clear guidelines for moving patients into and out of TB isolation, with regular checks to ensure that isolation is appropriate
- Ensuring prisoner inclusion in testing and treatment programs for drug-resistant TB
- Providing condoms to all prisoners and prison officers
- Providing HIV prevention, treatment, and care education, including information and sensitization on harm reduction and safer-sex practices in the context of same-sex sexual conduct at each prison to increase condom acceptance
- Creating guidelines on mental health evaluation and care for the prison system, and the transfer of inmates in need of mental health evaluation or treatment to prisons with such capacity
- Making mental health services available on the basis of free and informed consent
- Seek and allocate funding for the prison budget to ensure conditions consistent with international standards, without reliance on income from private landowners
- As more resources become available:
- Address prison health by:
- Establishing the presence of a trained health worker at each prison, with a minimum consistent supply of essential medications and the capacity to conduct TB and HIV testing and who can evaluate prisoner health complaints, including women’s, and facilitate access to prison referral or community hospital facilities
- Conducting health screening of all prisoners upon entry and at regular intervals
- Establishing TB and HIV treatment capacity and accreditation at a minimum at each regional referral unit
- Implementing HIV voluntary counseling and testing for pregnant inmates as part of a comprehensive system of prenatal care, offering prevention of mother-to-child transmission of HIV where appropriate
- Improving prenatal and postnatal care and addressing pregnant women’s nutritional needs
- Developing mental health services for upcountry prisons and expanding those at regional prisons to include psychosocial treatment
- Improving transport from prisons without health units to public health facilities and regional health units
- Developing a comprehensive health information management system with timely and complete reporting by all prisons nationwide
- Improve prison conditions by:
- Renovating prison facilities to provide every detainee with a bed and mattress of his or her own, and adequate space, light, and ventilation
- Ensuring an adequate supply of clean water, and that prisoners are provided with wood or charcoal to boil water free of charge
- Constructing a sufficient number of sanitary toilet and bathing facilities for the current number of inmates
- Increase the UPS’ focus on
rehabilitation and reintegration through:
- Increasing the availability of education programs
- Facilitating consensual paid work of a rehabilitative nature
- Improving community reentry programs
To the Ugandan Parliament and Ministry of Finance
Amend the Penal Code Act to decriminalize consensual sexual conduct among adults
Allot sufficient funding for the budget for Ugandan prisons to ensure conditions consistent with international standards without reliance on the income generated by the forced labor of unconvicted or physically unfit inmates
To the Ugandan Judiciary and Ministry of Justice
Address corruption and bribery in the system by requiring bail hearings to be conducted in open court instead of in camera
The Rules Committee should issue a Practice Direction for bail with conditions and guidelines for reasonable bail amounts, given income levels in Uganda
Instruct judges that the constitution guarantees bail after 60 days for non-capital offences and 180 days for capital offences and that there is no minimum amount of time required for prisoners to remain on remand before they are eligible for bail
Sensitize judges to the benefits of community service options and assure prisoners through agreement with prosecutors and magistrates that their decision to plead guilty on consideration of a promise of community service will actually result in community service sentences
Establish guidelines on time limits within which partially heard trials must be resolved or dismissed due to failure of witnesses or complainants to appear
For defendants who claim to be under 18, request and accept evidence of age and do not order detention of children with adults
Devise a functional legal aid system to ensure that defendants have access to a lawyer, provided by the state if they cannot afford one, from the time of arrest
To the Uganda Ministry of Health
Ensure a consistent supply of essential medications at health clinics countrywide
Ensure prisons receive a reliable supply of medications from the national drug stores
To the Uganda Police Force
Observe the constitutional requirement that all suspects be taken to court and charged within 48 hours of arrest
For suspects who claim to be under 18, request and accept evidence of age and do not order detention with adults
Stop police sweeps to arrest people on spurious charges of “rogue and vagabond”
Stop police brutality against suspects by promptly investigating, charging, and prosecuting instances of unlawful force against suspects
Issue guidelines on police bond and track the implementation of these guidelines
To International Agencies, Donors, and Nongovernmental Organizations
Continue funding efforts to reduce the case backlog, with emphasis placed on appropriate legal assistance, more judges, and more sessions
In the short term, ensure the direct delivery of health service provision in prisons including TB and HIV testing and treatment programs; women’s health; and mental healthcare programs on the basis of free and informed consent
In conjunction with any current or future funding to the UPS, set clear preconditions for funding including that:
- Reliance on income from forced labor as currently implemented is halted, as are beatings and physical abuse
- Prison OCs need to take responsibility for prison health and stop denying prisoners access to care at community- or prison-based medical facilities
- Prisoners with confirmed disease need to be transferred to and kept at facilities where they can receive treatment
In the long term, support the scaling up of the prison medical directorate to provide each of the services detailed above
Develop community reintegration programs, halfway houses, and microfinance initiatives to assist prisoners with reentry and decrease the risk of recidivism
Acknowledgements
This report was researched and written by Katherine Wiltenburg Todrys, researcher in the Health and Human Rights division, and Soo-Ryun Kwon, consultant in the Africa division. Maria Burnett, senior researcher in the Africa division, edited the report and contributed to the research. Joseph Amon, director of the Health and Human Rights division, edited the report and contributed to the research design.
This report was reviewed and edited by Rona Peligal, deputy director of the Africa division; Agnes Odhiambo, researcher in the Women’s Rights division; Darin Portnoy, advisory committee member in the Health and Human Rights division; Shantha Rau Barriga, disabilities researcher/advocate in the Health and Human Rights division; Juliane Kippenberg, senior researcher in the Children’s Rights division; Dipika Nath, researcher in the LGBT Rights division; Aisling Reidy, senior legal advisor; and Babatunde Olugboji, deputy program director.
Mignon Lamia, consultant in the Health and Human Rights division, assisted with data entry and analysis. Alex Gertner, associate in the Health and Human Rights Division, provided editing and production assistance. Grace Choi, publications director, and Fitzroy Hepkins, mail manager, provided production assistance. Giulio Frigieri, consultant, created and designed the map.
Human Rights Watch would like to thank all of the individuals who agreed to be interviewed for this report. Human Rights Watch is particularly grateful to the Uganda Prisons Service for its transparency and to the prisoners and prison officers whom its researchers met and interviewed, without whom this report would not have been possible.
Appendix
April 8, 2011
Dr. J.O.R. Byabashaija Commissioner General of Prisons
Uganda Prisons Service
Plot 13/15 Parliament Avenue
P.O. Box 7182
Kampala, Uganda
Dear Dr. Byabashaija,
I am writing to you to request information related to Uganda’s prisons.
As you know, Human Rights Watch conducts monitoring and reporting on human rights issues globally. The Health and Human Rights Division, which I lead, has, over the past decade, worked in more than two dozen countries globally, examining such issues as HIV/AIDS, TB, drug abuse, mental health, and access to health care for migrants, prisoners, and indigent populations.
With your permission, Human Rights Watch has recently conducted visits to 16 prisons as part of our on-going monitoring of the criminal justice system. We are grateful for your willingness to allow these visits and for the dialogue our Uganda researcher, Maria Burnett, has enjoyed with you in the past on detention issues. We look forward to continuing this dialogue in the future. I write today to seek your response to a number of concerns arising from these visits that relate to the health and human rights of prisoners, so that we can ensure that your views are reflected in an upcoming report on these issues.
Conditions vary greatly from prison to prison, and significant improvements have been made in improving conditions and health care in some prisons in recent years. However, some Ugandan prisons suffer from overcrowding and inadequate food, water, and sanitation. Some prisons lack medical facilities, and prisoners may be prevented from accessing community-based or prison referral facility medical care by the determinations of non-medical officers and because they are forced to work.
Prisoners, and some prison officials, told us that convicted and unconvicted prisoners are forced to work without pay on prison officers’ and private fields; prisoners frequently reported canings, and isolation cell use, sometimes coupled with water on the floor, denials of food, and beatings.
Your response to the following inquiries would be greatly appreciated.
- Please provide us with relevant Uganda Prisons Service (UPS) policies on inmate labor and on disciplinary offenses and appropriate punishment for prisoners.
- Are UPS officers permitted to use prison labor to work on their privately owned land or hire them out to other private landowners? If so, which categories of prisoners are eligible for such work and what oversight is provided by the UPS?
- Please specify how many officers in charge have been disciplined for infractions over the past year, what type of infractions each was charged with, and what disciplinary punishment was imposed.
- Please provide us with information on injuries and deaths of prisoners in custody for the past year, including the cause of injury or death, for each prison.
- Please provide us with data on the number of prisoners punished monthly, disaggregated by type of punishment, for the past year.
- Please provide us with data for the past year on the number of prisoners identified as sick (by type of illness) and number identified as mentally disabled.
- Please provide us with the number of prisoners receiving medical treatment in prison facilities and the number admitted to community facilities, by month, for the past year. Please provide us with data on the number of prisoners tested and treated with antiretroviral drugs for HIV (not including antibiotic (or Septrin) treatment) and tuberculosis for the past year.
- Please provide us with information on donor funding to the UPS, including the amounts contributed to each project by each donor, over the past year.
- Please provide us with a copy of the Fiscal Year 2010-2011 UPS budget.
- Please provide us with a copy of the UPS Standing Orders.
We hope to hear back from you by April 29, 2011. Please email any response to burnetm@hrw.org or fax to +44 (0)20 7713 1800.
We appreciate your attention to these important matters.
Yours sincerely,
Joseph Amon MSPH PhD
Director
Health and Human Rights Division
Human Rights Watch
CC: Dr. Michael Kyomya
[1] For the purposes of this report, the prisons visited are grouped into the following categories: Farm Prisons (Kitalya and Muinaina Farm Prisons); Former Local Administration Prisons (LAPs) (Bubukwanga Prison, Butuntumura Prison, Masafu Prison, Masaka Ssaza Prison, Muduuma Prison, Mutufu Prison); and Regional Reception Center Prisons (Fort Portal Men’s Prison, Fort Portal Women’s Prison, Masaka Main Prison, Murchison Bay Prison, Jinja Main Prison, Jinja Women’s Prison, Luzira Upper Prison, Luzira Women’s Prison). Data in the following tables will represent the responses of adult prisoners interviewed.
[2] Uganda Prisons Service (UPS), “Summary of UPS Prisoners Statistical Returns,” March 2010, http://www.prisons.go.ug/reports/0310.pdf (accessed March 24, 2011).
[3] UPS, “Programme 04: Prisons Medical Services: Work Plan and Budget FY 2010/11,” August 2010, p. 1.
[4] See, e.g., Uganda Human Rights Commission, “Statement from the Uganda Human Rights Commission Presented at the 61st Session of the United Nations Commission on Human Rights by Mrs. Margaret Sekaggya,” April 2005, http://www.nhri.net/pdf/UG18b.pdf (accessed April 12, 2011).
[5] Prisons Act of 2006, sec. 116.
[6] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” March 2010, http://www.oag.go.ug/uploaded_files/1273680950Prisons.pdf (accessed May 5, 2011), p. 1.
[7] Prison authorities wrote to Human Rights Watch, “Our budget is still low compared to the tasks at hand. The transfer of former Local Administration Prisons to the center by the Prisons Act 2006, has increased tasks before us.” Email correspondence from prison authorities to Human Rights Watch, May 19, 2011. See also U.S. Department of State, “2009 Human Rights Report: Uganda,” 2010, http://www.state.gov/g/drl/rls/hrrpt/2009/af/135982.htm (accessed August 10, 2010); Human Rights Watch interviews with prison medical authority, Uganda Prisons Service, Kampala, March 11, 2011; OC, Fort Portal Prison, November 15, 2010; OC, Muduuma Prison, November 12, 2010.
[8] Human Rights Watch estimates that in March 2010, approximately 20,448 prisoners were housed in former centrally administered prisons, and 10,137 in former LAPs. UPS, “Summary of UPS Prisoners Statistical Returns”; UPS and Covenant Word Ministries, “Uganda Government Prisons By District,” undated, http://www.cwm.or.ug/coverage.pdf (accessed May 4, 2011).
[9] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[10] Human Rights Watch interviews with OC, Fort Portal Prison, November 15, 2010; OC, Muduuma Prison, November 12, 2010; prison medical authority, UPS, March 11, 2011; prison medical authority, UPS, Kampala, November 18, 2010.
[11] Remand homes are located at Fort Portal, Gulu, Naguru (in Kampala), and Mbale. Children convicted of crimes are placed in the Kampiringisa National Rehabilitation Centre. In some, non-profit organizations provide educational or other services. Foundation for Human Rights Initiative, “Juvenile Justice in Uganda: Report for the Period January-July 2009,” undated. In accordance with international law, Ugandan law defines children as individuals under the age of 18 and prohibits their detention with adults. Children Act of 1997, sec. 2 & 89(8).
[12] Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010,” September 2010.
[13] Foundation for Human Rights Initiative, “Juvenile Justice in Uganda,” pp. 9-10.
[14] Prisons Act of 2006, sec. 8.
[15] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 4. Between FY 2005/06 and 2008/09, the Ugandan government increased its contribution to UPS from 27.66 (US$11.28 million) to 45.99 billion Uganda shillings ($18.76 million). Donor funding fluctuated from a high of 4.13 billion shillings ($1.68 million) in 2006/07 to a low of 0.72 billion shillings ($0.29 million) in 2008/09. “Internally generated” revenue increased from 1.45 ($0.59 million) in 2005/06 to 1.95 billion shillings ($0.80 million) in 2008/09. Ibid. Overall, the UPS budget was 49.2 billion shillings (approximately $20 million) in FY 2009/10, and 63.48 billion shillings (approximately $26 million) in FY 2010/11.
[16] Human Rights Watch interviews with OC, Masaka Main Prison, November 23, 2010; OC, Masaka Ssaza Prison, November 22, 2010; OC, Fort Portal Prison, November 15, 2010; OC, Kitalya Farm Prison, February 28, 2011; OC, Jinja Women’s Prison, March 2, 2011; OC, Muinaina Farm Prison, March 3, 2011; OC, Mutufu Prison, March 7, 2011; OC, Masafu Prison, March 8, 2011; OC, Murchison Bay Prison, November 10, 2010; OC, Muduuma Prison, November 12, 2010; prison medical authority, UPS, March 11, 2011.
[17] UPS, “Work Plan and Budget,” p. 6.
[18] The health budget increased from 0.87 billion Uganda shillings ($355,139) in FY 2009/10 to 1.35 billion Uganda shillings ($551,727) in FY 2010/11. UPS, “Work Plan and Budget,” p. iv. Prison authorities report that the recurrent non-wage budget of the prison health services increased by 90 percent between FY 2009/10 and FY2010/11 (from 0.39 billion shillings ($149,460) to 0.74 billion shillings ($283,559), and will again be increased by 56 percent in FY 2011/12 (to 1.15 billion shillings ($441,414)).
[19] Human Rights Watch interviews with prison medical authority, UPS, March 11, 2011; UPS, “Work Plan and Budget,” p. 6. Reportedly, prison health services may approach three percent of the overall prison budget in FY 2011/12. Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[20] UPS, “Work Plan and Budget,” p. 28.
[21] Isaac Khisa, “Funding Blamed for Deterioration of Uganda’s Prisons,” East Africa in Focus, October 5, 2009, http://www.eafricainfocus.com/2009/10/04/funding-blamed-for-deterioration-of-uganda%E2%80%99s-prisons/ (accessed August 11, 2010).
[22] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011; Letter to Human Rights Watch from prison authorities, June 29, 2011.
[23] Human Rights Watch interviews with OC, Murchison Bay Prison, November 10, 2010; doctor, Murchison Bay Hospital, November 10, 2010.
[24] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[25] These units are located at Fort Portal, Masindi, Mbarara, Masaka, Jinja (M), Mbale, Gulu, Moroto, Arua and Kigo.
[26] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[27] World Health Organization, “Country Cooperation Strategy Uganda,” WHO/CCS/2, 2000, http://www.who.int/countries/en/cooperation_strategy_uga_en.pdf (accessed April 25, 2011).
[28] WHO, “World Health Statistics,” 2010, http://www.who.int/whosis/whostat/EN_WHS10_Full.pdf (accessed April 25, 2011); WHO et al., “Trends in Maternal mortality 1990-2008: Estimates developed by WHO, UNICEF, UNFPA and The World Bank,” 2010, http://whqlibdoc.who.int/publications/2010/9789241500265_eng.pdf, p. 26 (accessed May 19, 2011). Non-provision of maternal health services and commodities in public healthcare facilities in Uganda remains a major issue. See, e.g., Center for Health, Human Rights and Development et al. vs. The Attorney General, petition to the Constitutional Court of Uganda, 2011.
[29] Uganda Human Rights Commission, “12th Annual Report,” 2009. In 2010, per 10,000 people, there was one physician, less than one dentist, and 13 midwives. WHO, “World Health Statistics.” Foundation for Human Rights Initiative, “The Right to Healthcare in Uganda,” 2010, http://www.fhri.or.ug/executive%20summary%20research%20report.pdf (accessed April 25, 2011) (reporting that as a result of understaffing, patients waited for four to six hours to see a nurse at health centers).
[30] World Health Organization, “Country Cooperation Strategy Uganda”; World Health Organization, “Country Profile: Uganda,” 2009, http://www.who.int/tb/publications/global_report/2009/pdf/uga.pdf (accessed April 25, 2011).
[31]Annie Kelly, “Healthcare a Major Challenge for Uganda,” The Guardian, April 1, 2009.
[32]There are not enough community health centers or hospitals. In theory, there are supposed to be healthcare facilities at the parish, sub-county, and county levels, as well as a hospital at the district level. Richard Kavuma, “Uganda’s Healthcare System Explained,” The Guardian, April 1, 2009. However, at least 26 districts in Uganda do not have a hospital, and patients must walk 12 kilometers in order to reach the nearest community health center. Foundation for Human Rights Initiative, “The Right to Healthcare in Uganda.” On average, rural residents live 5.2 km and urban residents 2.9 km from the nearest health center. Uganda Bureau of Statistics, “National Service Delivery Survey,” 2004, http://openmicrodata.wordpress.com/category/uganda/ (accessed April 25, 2011).
[33] Foundation for Human Rights Initiative, “The Right to Healthcare in Uganda.”
[34] Richard M. Kavuma, “Unhealthy Returns,” The Guardian, February 12, 2010; Foundation for Human Rights Initiative, “The Right to Healthcare in Uganda.”
[35] Foundation for Human Rights Initiative, “The Right to Healthcare in Uganda.”
[36] J.O.R. Byabashaija, “Unclogging Prison Congestion! Whose Responsibility?” presented at the Donor Annual Review, Kampala, undated, http://www.jlos.go.ug/uploads/Unclogging%20Prisons%20Congestion!%20Whose%20Responsibility%20A%20paper%20by%20the%20Commissioner%20General%20of%20Prisons.pdf (accessed April 13, 2011).
[37] International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 52, U.N. Doc. A/6316 (1966), 999 U.N.T.S. 171, entered into force March 23, 1976, acceded to by Uganda on June 21, 1995, art. 10; United Nations (UN) Standard Minimum Rules for the Treatment of Prisoners (Standard Minimum Rules), adopted by the First United Nations Congress on the Prevention of Crime and the Treatment of Offenders, held at Geneva in 1955, and approved by the Economic and Social Council by its resolution 663 C (XXIV) of July 31, 1957, and 2076 (LXII) of May 13, 1977, paras. 9-11; United Nations (UN) Human Rights Committee, General Comment 21, Article 10, Humane Treatment of Persons Deprived of Liberty (Forty-fourth session, 1992), Compilation of General Comments and General Recommendations Adopted by Human Rights Treaty Bodies, UN Doc. HRI/GEN/1/Rev.7 (1994), paras. 9 and 13. See also Prisons Act of 2006, sec. 64(1).
[38] In March 2010, the UPS housed 169 debtors. UPS, “Summary of UPS Prisoners Statistical Returns.” This practice is directly contrary to international law. ICCPR, art. 11.
[39] However, female and male prisoners were separated.
[40] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 9-19. These standards, although non-binding, have been recognized as the minimum standards acceptable to the international community through adoption by the General Assembly.
[41] In March 2010: Luzira Upper was at 366 percent of approved capacity; Luzira Women’s at 357 percent; Murchison Bay at 128 percent; Butuntumura at 893 percent; Muduuma at 3,200 percent; Kitalya at 104 percent; Masaka Main at 333 percent; Masaka Ssaza at 1,611 percent; Muinaina at 269 percent; Jinja Main at 247 percent; Jinja Women’s at 133 percent; Fort Portal Men’s at 213 percent; Fort Portal Women’s at 86 percent; Bubukwanga at 1,343 percent; Masafu at 490 percent; Mutufu at 785 percent. It should be noted that while researchers did seek to visit some prisons on the basis of their overcrowding, researchers did not visit prisons in the Northern region of the country, which in March 2010 was the single most crowded region. UPS, “Summary of UPS Prisoners Statistical Returns.”
[42] Human Rights Watch interviews with OC, Masaka Ssaza Prison, November 22, 2010; doctor, Murchison Bay Hospital, November 10, 2010; OC, Masaka Main Prison, November 23, 2010; deputy OC, Jinja Main Prison, March 1, 2011; OC, Jinja Main Prison, March 1, 2011.
[43] Human Rights Watch facility tour with prison warden, Luzira Upper Prison, November 9, 2010. Diversity exists, however, between the sleeping arrangements at different prisons, and even within prisons. At Murchison Bay, Fort Portal Men’s and Women’s, Jinja Women’s, and Masafu Prisons, prisoners did not consistently complain about sleeping arrangements. At some prisons, some senior inmates or those with resources are given significantly more sleeping space.
[44] Human Rights Watch interview with Asuman, Murchison Bay Prison, November 10, 2010.
[45] Human Rights Watch interview with Ronald, Muduuma Prison, November 12, 2010.
[46] Human Rights Watch interview with Brian, Murchison Bay Prison, November 13, 2010.
[47] Human Rights Watch interview with Phillip, Muduuma Prison, November 12, 2010.
[48] Human Rights Watch interview with Ronald, Muduuma Prison, November 12, 2010.
[49] Human Rights Watch interview with Hellene, 16, Butuntumura Prison, November 11, 2010.
[50] Human Rights Watch interview with Nathan, Muduuma Prison, November 12, 2010.
[51] Human Rights Watch interviews with Dorothy, Butuntumura Prison, November 11, 2010; Owen, Kitalya Farm Prison, February 28, 2011.
[52] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 10 and 11(a).
[53] Human Rights Watch interview with Mutebi, Muduuma Prison, November 12, 2010.
[54] Human Rights Watch interview with William, Muinaina Farm Prison, March 4, 2011.
[55] Prisons Act of 2006, sec. 70.
[56] Human Rights Watch interviews with Hassan, Masaka Ssaza Prison, November 22, 2010; Jonathan, Masaka Ssaza Prison, November 22, 2010; OC, Masaka Ssaza Prison, November 22, 2010; Kakuru, Butuntumura Prison, November 11, 2010 . Prisoners previously held at additional prisons noted that lack of a fence or lack of separate female exercise area had led to them being locked in the ward all day. Human Rights Watch interviews with Charles, Muinaina Farm Prison, March 3, 2011; Harvey, Muinaina Farm Prison, March 3, 2011; Gloria, Jinja Women’s Prison, March 2, 2011.
[57] Human Rights Watch interview with Byamukama, Masaka Ssaza Prison, November 22, 2010.
[58] Manfred Nowak, “U.N. Covenant on Civil and Political Rights, CCPR Commentary,” (2nd edition) (Khel: N.P. Engel, 2005), pp. 165, 172-75, 244-29. See, for example, cases against Uruguay such as Buffo Carball v. Uruguay, No. 33/1978, Massiotti v. Uruguay, No. 25/1978; Madagascar: Marais v. Madagascar, No. 49/1979, Wight v. Madagascar, No. 115/1982; Jamaica: Robinson v. Jamaica, No. 731/1996, Pennant v. Jamaica, No. 647/1995; Russia: Lantsova v. Russian Federation, No. 763/1997.
[59] UN Standard Minimum Rules for the Treatment of Prisoners, para. 20(1). This standard has been cited with approval by the UN Human Rights Committee when examining the minimum standards that a state must observe for those deprived of their liberty, “regardless of a state party’s level of development.” See Mukong v. Cameroon, No. 458/1991, para. 9.3.
[60] The Prisons Act of 2006, sec. 69(1).
[61] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 10.
[62] Prisoners receive 680 grams of maize meal, 148 grams of beans, and 15 grams of salt daily. Human Rights Watch interview with prison medical authority, UPS, November 18, 2010; UPS, “Work Plan and Budget,” p. 5. Prisoners who were fortunate enough to have relatives bring them provisions could have these rations supplemented.
[63] Human Rights Watch interview with Catherine, Jinja Women’s Prison, March 2, 2011; Human Rights Watch interview with Elizabeth, Jinja Women’s Prison, March 2, 2011.
[64] Human Rights Watch interview with Mark, Muinaina Farm Prison, March 4, 2011.
[65] Human Rights Watch interviews with Owen, Kitalya Farm Prison, February 28, 2011; Moses, Kitalya Farm Prison, February 28, 2011; Gilbert, Kitalya Farm Prison, February 28, 2011; Ross, Masafu Prison, March 8, 2011; Matovu, Kitalya Farm Prison, February 28, 2011; Emmanuel, Kitalya Farm Prison, February 28, 2011.
[66] Human Rights Watch interview with Julius, Kitalya Farm Prison, February 28, 2011.
[67] Human Rights Watch interview with enrolled midwife, Kitalya Farm Prison, February 28, 2011. The prison medical authority also reported: “In 2008, we had a nutrition assessment, which observed that the intake was not commensurate to the requirements for prisoners, especially in the farm. We recommended an improvement be made available for the prisoners on the farm. The implementation is not yet there. I don’t know what that situation is.” Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[68] Letter from prison authorities to Human Rights Watch, June 29, 2011.
[69] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010. See also UPS, “Work Plan and Budget,” p. 5 (demonstrating that the diet is deficient in fat and calcium, and consists of no Vitamin A or C whatsoever); Human Rights Watch interview with doctor, Murchison Bay Hospital, November 10, 2010 (noting that eye conditions as a result of lack of Vitamin A are “very common”); The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Uganda Prisons Service,” p. iv (concluding that “[t]he quality of the food served did not meet all the basic food nutrients necessary for a healthy balanced diet”).
[70] The Prisons Act of 2006, sec. 59(3).
[71] Human Rights Watch interviews with Betty, Masaka Ssaza Prison, November 22, 2010; Alice, Masaka Main Prison, November 23, 2010; Harriet, Masaka Main Prison, November 23, 2010.
[72] Human Rights Watch interviews with Christine, Fort Portal Women’s Prison, November 15, 2010; Priscilla, Fort Portal Women’s Prison, November 17, 2010; OC, Fort Portal Women’s Prison, November 17, 2010; Mary, Jinja Women’s Prison, March 2, 2011; Stella, Jinja Women’s Prison, March 2, 2011; Beatrice, Jinja Women’s Prison, March 2, 2011; OC, Jinja Women’s Prison, March 2, 2011; Hannah, Luzira Women’s Prison, November 10, 2010; OC, Masaka Main Prison, November 23, 2010.
[73] Human Rights Watch interviews with Gloria, Jinja Women’s Prison, March 2, 2011; Stella, Jinja Women’s Prison, March 2, 2011.
[74] Human Rights Watch interview with Harriet, Masaka Main Prison, November 23, 2010. See also Human Rights Watch interviews with Leah, Luzira Women’s Prison, November 10, 2010; Olivia, Masaka Main Prison, November 23.
[75] The World Health Organization recommends that mothers known to be HIV-infected should only give infant formula as a replacement when safe water and sanitation are assured, sufficient formula can reliably be provided, and it may be prepared cleanly and carry a low risk of diarrhea and malnutrition. WHO, “Guidelines on HIV and Infant Feeding, http://whqlibdoc.who.int/publications/2010/9789241599535_eng.pdf (accessed May 13, 2011), pp. 7-8. In Uganda, national guidelines recommend that HIV-positive mothers opt for replacement feeding if affordable, feasible, acceptable, sustainable and safe, yet acknowledge that most Ugandan mothers cannot meet this standard. Richard Hasunira, Aaron Muhinda, Rosette Mutambi and Beatrice Were, “Uganda,” in Missing the Target: Failing Women, Failing Children: HIV, Vertical Transmission, and Women’s Health, International Treatment Preparedness Coalition, May 2009, p. 62.
[76] Body of Principles, prin. 31.
[77] The Prison Act of 2006, sec. 59(2)-(4).
[78] Food and firewood requirements for 2009/10 should have totaled slightly under 21.73 billion Uganda shillings ($8.67 million); however, as a significant proportion of food is grown on UPS farms (totaling 4.35 billion shillings or $1.74 million), and 17.27 billion shillings ($6.89 million) were allocated from funding from the government of Uganda under that year’s budget, no substantial funding gap should have existed. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” pp. 11-12. In 2011, the prison medical authority reported that 24 billion Uganda shillings ($9.58) were required to provide adequate food for all the prisoners, but the governmental budget available for food that year and the following one would be 14 billion Uganda shillings ($5.59 million), with the gap covered by prison-produced food. Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[79] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” pp. 11-12.
[80] Human Rights Watch interview with Phillip, Muduuma Prison, November 12, 2010. See also Human Rights Watch interview with Paul, Muduuma Prison, November 12, 2010. International standards and Ugandan law dictate that drinking water be available to every prisoner whenever he or she needs it. UN Standard Minimum Rules for the Treatment of Prisoners, para. 20(2); Prisons Act of 2006, sec. 69(2).
[81] Human Rights Watch interviews with David, Kitalya Farm Prison, February 28, 2011; Emmanuel, Kitalya Farm Prison, February 28, 2011; Matovu, Kitalya Farm Prison, February 28, 2011; Moses, Kitalya Farm Prison, February 28, 2011; Joseph, Kitalya Farm Prison, February 28, 2011.
[82] Human Rights Watch interview with Gilbert, Kitalya Farm Prison, February 28, 2011.
[83] Human Rights Watch interviews with OC, Muinaina Farm Prison, March 3, 2011; OC, Mutufu Prison, March 7, 2011; OC, Kitalya Farm Prison, February 28, 2011. Ugandan government sources have also noted the inadequate provision of clean drinking water in some prisons. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Uganda Prisons Service,” p. v; UPS, “Work Plan and Budget,” p. 4.
[84] Human Rights Watch interview with Andrew, Bubukwanga Prison, November 16, 2010.
[85] Human Rights Watch interview with Douglas, Bubukwanga Prison, November 16, 2010.
[86] Human Rights Watch interviews with Lubega, 17, Bubukwanga Prison, November 16, 2010; Christopher, 17, Bubukwanga Prison, November 16, 2010.
[87] Human Rights Watch interview with OC, Muinaina Farm Prison, March 3, 2011.
[88] Human Rights Watch interviews with Mukasa, Luzira Upper Prison, November 9, 2010; Fred, Luzira Upper Prison, November 8, 2010; Harvey, Muinaina Farm Prison, March 3, 2011; Ralph, Luzira Upper Prison, November 9, 2010; Jacob, Luzira Upper Prison, November 8, 2010.
[89] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 12-14.
[90] Human Rights Watch interviews with George, Mutufu Prison, March 7, 2011; Odong, Mutufu Prison, March 7, 2011; Thomas, Mutufu Prison, March 7, 2011; Jared, Mutufu Prison, March 7, 2011.
[91] Human Rights Watch interviews with Musa, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010.
[92] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 12-14.
[93] Human Rights Watch interviews with Grace, Masaka Ssaza Prison, November 22, 2010; Ross, Masafu Prison, March 8, 2011. Systems where prisoners are obliged to use buckets in their cells as toilets which they then empty—known as “slopping out”—have been condemned by the European Committee on the Prevention of Torture and the European Court of Human Rights as a violation of the prohibition on inhuman and degrading treatment.
[94] Human Rights Watch interview with OC, Masafu Prison, March 8, 2011.
[95] Human Rights Watch interviews with Timothy, Muduuma Prison, November 12, 2010; Onyango, Muduuma Prison, November 12, 2010.
[96] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 15-19.
[97] Ibid., para. 19.
[98] This includes toilet paper, towels, soap, toothbrushes, and toothpaste. UPS, “Work Plan and Budget,” p. 5.
[99] Human Rights Watch interviews with OC, Masaka Ssaza Prison, November 22, 2010; OC, Muduuma Prison, November 12, 2010; OC, Muinaina Farm Prison, March 3, 2011; OC, Masafu Prison, March 8, 2011; OC, Fort Portal Women’s Prison, November 15, 2010.
[100] Human Rights Watch interviews with Musa, Muduuma Prison, November 12, 2010; Mafabi, Butuntumura, November 11, 2010; Terrence, Fort Portal Men’s, November 17, 2010.
[101] Human Rights Watch interviews with Patrick, Muduuma Prison, November 12, 2010; George, Mutufu Prison, March 7, 2011; Brian, Murchison Bay, November 13, 2010; Esther, Fort Portal Women’s, November 17, 2010.
[102] UN Standard Minimum Rules for the Treatment of Prisoners, para. 71(1).
[103] Ibid., art. 72(2).
[104] The International Labor Organization’s Convention 29 on Forced Labor, which Uganda has ratified, states that only convicts can be compelled to work in prison; such work must at all times be supervised by a public authority; and prisoners may not be “hired to or placed at the disposal of private individuals, companies or associations,” which means that prison labor for private entities may be only by consent of the prisoner, whether convict or remand. International Labor Organization, “Convention 29 on Forced Labor,” ratified by Uganda on June 4, 1963, http://www.ilo.org/ilolex/cgi-lex/convde.pl?C029 (accessed April 11, 2011); Lee Swepston, “Prison Labour and International Human Rights,” Industrial Relations Research Association, June 2001, http://www.leeswepston.net/prison.htm (accessed April 11, 2011). UN Standard Minimum Rules for the Treatment of Prisoners, para. 73(1).
[105] International Labor Organization, “Convention 29 on Forced Labor,” art. 11. See also UN Standard Minimum Rules for the Treatment of Prisoners, para. 71(2) (stating that prison labor is subject to the “physical and mental fitness” of prisoners as determined by a medical officer).
[106] International Labor Organization, “Convention 29 on Forced Labor,” arts. 12-14. UN Standard Minimum Rules for the Treatment of Prisoners, para. 73(2). Both the UN Standard Minimum Rules and Uganda’s Prisons Act provide for prisoners’ rights to remuneration for their work. Standard Minimum Rules for the Treatment of Prisoners, paras. 76(1), (2), and (3). Prisons Act of 2006, sec. 57.
[107] Initial Report to the Human Rights Committee: Uganda, U.N. Doc. CCPR/C/UGA/2003/1, 2003, http://www.unhchr.ch/tbs/doc.nsf/898586b1dc7b4043c1256a450044f331/341b0ac3c7807592c1256db0002d4858/$FILE/G0340506.pdf (accessed August 11, 2010).
[108] Mary Karugaba, “Prisoners to be Paid for Work,” New Vision, April 14, 2011.
[109] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 74(1) and (2).
[110] Human Rights Watch interview with Matovu, Kitalya Farm Prison, February 28, 2011.
[111] JLOS stated that one of its major achievements in reducing labor was the mechanization of farm prisons, reducing the number of hours worked per day from eight hours to seven hours in 2009-2010. Justice Law and Order Sector, “Annual Performance Report,” September 2010. Private landowners who had previously hired prison labor reported that prisoners worked as many as nine hours a day on their land, sometimes seven days a week. Human Rights Watch interviews with farmers, near Sentema Prison and Kasangati Prison, January 20, 2011; farmers near Ntenjeru Prison, January 21, 2011.
[112] Human Rights Watch interviews with Phillip, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010; Milton, Fort Portal Men’s, November 17, 2010; Terrence, Fort Portal Men’s, November 17, 2010.
[113] Human Rights Watch interview with Ronald, Muduuma Prison, November 12, 2010; Musa, Muduuma Prison, November 12, 2010.
[114] Human Rights Watch interview with Musa, Muduuma Prison, November 12, 2010.
[115] Human Rights Watch interviews with Milton, Fort Portal Men’s Prison, November 17, 2010; Hussein, Fort Portal Men’s Prison, November 17, 2010
[116] Human Rights Watch interviews with William, Muinaina Prison, March 3, 2011; Musa, Muduuma Prison, November 12, 2010; Onyango, Muduuma Prison, November 12, 2010; Busingye, Bubukwanga Prison, November 16, 2010; Ross, Muinaina Prison, March 8, 2011.
[117] Human Rights Watch field observation, Kitalya Farm Prison, February 28, 2011.
[118] Human Rights Watch interviews with Musa, Muduuma Prison, November 12, 2010; Ronald, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010; Onyango, Muduuma Prison, November 12, 2010; Joseph, Kitalya Farm Prison, February 28, 2011.
[119] Human Rights Watch interviews with Ronald, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010.
[120] Human Rights Watch interviews with Ronald, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010; Onyango, Muduuma Prison, November 12, 2010. These initiation rituals were called “Black Mamba” or “cane crosses,” because when two prisoners beat the newcomer, the lashes made an “X” mark on his back. Human Rights Watch interviews with Timothy, Muduuma Prison, November 12, 2010; Joseph, Kitalya Farm Prison, February 28, 2011.
[121] Human Rights Watch interviews with Edgar, Murchison Bay, November 13, 2010; Pius, Muinaina Prison, March 3, 2011; Kevin, Muinaina Prison, March 3, 2011; Edmund, March 4, 2011.
[122] Human Rights Watch interview with Edgar, Murchison Bay, November 13, 2010.
[123] Human Rights Watch interview with Duncan, Muinaina Prison, March 4, 2011.
[124] Human Rights Watch interviews with Emma, Jinja Women’s Prison, March 2, 2011; Catherine, Jinja Women’s Prison, March 2, 2011.
[125] Human Rights Watch interview with Catherine, Jinja Women’s Prison, March 2, 2011.
[126] Prisons Act of 2006, sec. 97.
[127] UN Standard Minimum Rules for the Treatment of Prisoners, paras. 28-32.
[128] Human Rights Watch interview with Joseph, Kitalya Farm Prison, February 28, 2011.
[129] Human Rights Watch interview with OC, Muduuma Prison, November 12, 2010; OC, Masaka Ssaza Prison, November 22, 2010; OC, Jinja Women’s Prison, March 2, 2011; OC, Muinaina Prison, March 4, 2011; OC, Mutufu Prison, March 7, 2011; OC, Masafu Prison, March 8, 2011. UPS relies on “internally generated” revenue in its budget, and internally generated revenue climbed from 1.45 billion shillings (approximately $600,000) in FY 2005/06 to 1.95 billion shillings (approximately $800,000) in FY 2008/09, with the exception of FY2007/08. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 4.
[130] Human Rights Watch interview with OC, Masaka Ssaza Prison, November 22, 2010; OC, Muinaina Prison, March 4, 2011; OC, Mutufu Prison, March 7, 2011; OC, Masafu Prison, March 8, 2011.
[131] Human Rights Watch interview with OC, Masaka Ssaza Prison, November 22, 2010.
[132] Human Rights Watch interview with OC, Masafu Prison, March 8, 2011.
[133] Ibid.
[134] Human Rights Watch interview with OC, prison and date withheld.
[135] Human Rights Watch interview with OC, Muinaina Farm Prison, March 4, 2011.
[136] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. iv. The auditor general further declared that lack of documentation and accountability led to under-declaration and under-supply of food, compounding food shortages in prisons. Ibid., p. 12.
[137] At Muinana Farm Prison, Human Rights Watch researchers found remanded and committed prisoners working. Prison escape records also indicated that a remanded prisoner from Muinaina Farm Prison was reported by prison authorities to have escaped from the “M/Shamba,” indicating the “main” government-owned field, in 2010. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[138] Human Rights Watch interview with OC, Muinaina Prison, March 4, 2011.
[139] Human Rights Watch interviews with farmers, near Sentema and Kasangati Prisons, January 20, 2011; farmers, near Ntenjeru Prison, January 21, 2011. An OC with 100 prisoners working six days a week could earn around 7,200,000 Uganda shillings a month (approximately $3,060). Prisoners had various colloquial terms for work for private contractors such as, “ekigaali,” “kibawula,” “parties,”and “bed shamba two.” By contrast, going to work on prison land is called “federo” or “main shamba.”
[140] Human Rights Watch interviews with personnel, Sentema Prison, January 20, 2011; OC, Kasangati Prison, January 20, 2011; orderly sergeant, Ntenjeru Prison, January 21, 2011; farmers, near Sentema Prison and Kasangati prisons, January 20, 2011; farmers, near Ntenjeru Prison, January 21, 2011.
[141] Ibid.
[142] Ibid.
[143] Email communication from prison authorities to Human Rights Watch, May 19, 2011.
[144] Ibid.
[145] Data provided to Human Rights Watch by prison authorities on prisoner escapes in 2010 indicated that remanded prisoners escaped from “labour party,” “outside party,” “building party,” and “bricks party.” These categories were distinct from categories (such as “M/shamba” or “staff shamba”) indicating that prisoners had escaped during labor on prison-owned land or staff farms. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[146] Anthony Wesaka and Angelo Izama, “Police, Prisons on the Spot over Inmates Forced Labour,” The Monitor, June 27, 2010.
[147] Penal Code Act of 1950, sec. 168. Human Rights Watch interviews with Washington, Muduuma Prison, November 12, 2010; Nathan, Muduuma Prison, November 12, 2010; Patrick, Muduuma Prison, November 12, 2010; Phillip, Muduuma Prison, November 12, 2010; Paul, Muduuma Prison, November 12, 2010; Ronald, Muduuma Prison, November 12, 2010; Timothy, Muduuma Prison, November 12, 2010; Onyango, Muduuma Prison, November 12, 2010.
[148] Email communication from prison authorities to Human Rights Watch, May 19, 2011. Information provided by prison authorities to Human Rights Watch on prisoner escapes in 2010 indicated that remanded and convicted prisoners were reported to have escaped from “staff shamba [field].” Letter from prison authorities to Human Rights Watch, June 29, 2011.
[149] Human Rights Watch interview with OC, Muinaina Prison, March 4, 2011. Wardens make roughly between 250,000 Uganda shillings and 375,000 shillings (approximately $100 to $160) per month in salary. Housing in barracks for wardens and their families is also usually provided. Human Rights Watch interview with OC, Mutufu Prison, March 7, 2011.
[150] Human Rights Watch interviews with Harvey, Muinaina Prison, March 3, 2011; Eric, Muinaina Prison, March 3, 2011; Edward, Muinaina Prison, March 4, 2011; Duncan, Muinaina Prison, March 4, 2011.
[151] Human Rights Watch interview with OC, Muinaina Prison, March 4, 2011.
[152] Human Rights Watch interviews with Harvey, Muinaina Prison, March 3, 2011; Eric, Muinaina Prison, March 3, 2011; Edward, Muinaina Prison, March 4, 2011; Duncan, Muinaina Prison, March 4, 2011.
[153] Human Rights Watch interview with Eric, Muinaina Prison, March 3, 2011; Duncan, Muinaina Prison, March 4, 2011.
[154] Human Rights Watch interviews with Rosemary, Butuntumura Prison, November 11, 2010; Sylvia, Fort Portal Women’s, November 15, 2010; Christine, Fort Portal Women’s, November 15, 2010; Emma, Jinja Women’s, March 2, 2011; Catherine, Jinja Women’s, March 2, 2011; OC, Masafu Prison, March 8, 2011.
[155] Email communication from prison authorities to Human Rights Watch, May 19, 2011.
[156] Human Rights Watch interviews with Owen, Kitalya Farm Prison, February 28, 2011; David, Kitalya Farm Prison, February 28, 2011; Emmanuel, Kitalya Farm Prison, February 28, 2011; Gilbert, Kitalya Farm Prison, February 28, 2011; Julius, Kitalya Farm Prison, February 28, 2011; Moses, Kitalya Farm Prison, February 28, 2011; Joseph, Kitalya Farm Prison, February 28, 2011.
[157] For example, some prisoners at Masaka Ssaza, Masaka, Jinja Main, Muinaina, and Masafu stated that they were paid 200 to 500 Uganda shillings for work on private farms. Prisoners with authority to supervise other prisoners were sometimes given 500 Uganda shillings ($0.25) out of the warden’s tips while others were not, and in many cases, no prisoner received any remuneration. Human Rights Watch interviews with Ali, Murchison Bay, November 20, 2010; Mafabi, Butuntumura Prison, November 11, 2010; Musa, Muduuma Prison, November 12, 2010.
[158] Under Ugandan law, prisoners upon admission to prison are to be provided with written information on regulations related to the treatment of prisoners in that category; disciplinary requirements of the institution; and the complaints procedure. Prisons Act of 2006, sec. 58(5)(a)-(c). Furthermore, “A prisoner shall not be punished for a prison offence until the prisoner has had an opportunity of hearing the charge against him or her and making a defence and where necessary and practicable, the prisoner shall be allowed the services of an interpreter.” Prisons Act of 2006, sec. 96.
[159] Prisons Act of 2006, sec. 85.
[160] See, e.g., Human Rights Watch interviews with Okello, Luzira Upper Prison, November 8, 2010; Samuel, Fort Portal Men’s Prison, November 15, 2010; Kakuru, Butuntumura Prison, November 11, 2010; Akello, Luzira Women’s Prison, November 10, 2010; Agatha, Luzira Women’s Prison, November 9, 2010; Abigail, Fort Portal Women’s Prison, November 15, 2010; Isaac, Jinja Main Prison, March 1, 2011; OC, Fort Portal Prison, November 15, 2010.
[161] Human Rights Watch interviews with OC, Fort Portal Prison, November 15, 2010; OC, Masaka Ssaza Prison, November 22, 2010; OC, Muinaina Farm Prison, March 3, 2011; OC, Masafu Prison, March 8, 2011.
[162] Prisons Act of 2006, sec. 95; Human Rights Watch interviews with OC, Masaka Ssaza Prison, November 22, 2010; deputy OC, Jinja Main Prison, March 1, 2011; OC, Fort Portal Prison, November 15, 2010.
[163] Prisoners consistently said that smoking (cigarettes or marijuana), engaging in same-sex sexual conduct, refusing or delaying to work, trying to escape, fighting with other prisoners, or stealing would entail either a beating, incarceration in an isolation cell, or both. In some cases, minor disciplinary offences also were considered to merit these punishments, such as dirtying the shower area leading to a beating or use of a mobile phone to a week in an isolation cell. Frequently, prisoners expressed to researchers their fear that speaking with outsiders about the problems in prison would earn them a beating. Prisoners also said that they were beaten at some prisons when they requested medical care. Punishment for sexual conduct was particularly severe.
[164] According to prison authorities, “There is … one punishment that is currently outlawed and that’s Corporal Punishment. This is now treated as assault and purely a Police case [case to be investigated by police].” Email communication from prison authorities to Human Rights Watch, May 19, 2011.
[165] ICCPR, art. 7; Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (Convention against Torture), adopted December 10, 2984, G.A. res. 39/46, annex, 39 U.N. GAOR Supp. (No. 51) at 197, U.N. Doc. A/39/51 (1984), entered into force June 26, 1987), acceded to by Uganda on November 3, 1986.
[166] Human Rights Watch interviews with OC, Muinaina Farm Prison, March 3, 2011; OC, Mutufu Prison, March 7, 2011; OC, Masafu Prison, March 8, 2011; OC, Masaka Ssaza Prison, November 22, 2010.
[167] Human Rights Watch interview with health worker, Murchison Bay Hospital, November 10, 2010.
[168] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[169] Foundation for Human Rights Initiative, “The Human Rights Status Report,” pp. 20-21; Uganda Human Rights Commission, “12th Annual Report,” 2009, p. 44.; The African Centre for Treatment and Rehabilitation of Torture Victims, “The Nature of Torture in Uganda: A Study Conducted in Luwero; Wakiso; Gulu; Arua; Soroti; Jinja; Bushenyi and Kasese Districts,” November 2010.
[170] Email correspondence from prison authorities to Human Rights Watch, May 19, 2011.
[171] Prisoners at Jinja Main Prison reported that since the arrival of a new OC, inmates are no longer beaten.
[172] Human Rights Watch facility assessment of Bubukwanga Prison, November 16, 2010.
[173] Human Rights Watch interviews with Martin, Bubukwanga Prison, November 16, 2010; Christopher, 17, Bubukwanga Prison, November 16, 2010; Johnson, Bubukwanga Prison, November 16, 2010; Otto, Bubukwanga Prison, November 16, 2010; Gideon, 15, Bubukwanga Prison, November 16, 2010.
[174] Human Rights Watch interviews with Gideon, 15, Bubukwanga Prison, November 16, 2010; Christopher, 17, Bubukwanga Prison, November 16, 2010.
[175] Human Rights Watch interview with Martin, Bubukwanga Prison, November 16, 2010.
[176] Human Rights Watch interviews with Logan, Butuntumura Prison, November 11, 2010 (5 strokes); Alice, Masaka Main Prison, November 23, 2010 (5 strokes); Saul, Masaka Ssaza Prison, November 22, 2010 (5 strokes); Betty, Masaka Ssaza Prison, November 22, 2010 (7 strokes); Akello, Luzira Women’s Prison, November 10, 2010 (10 strokes); Alex, Murchison Bay Prison, November 10, 2010 (10 strokes); Mukasa, Luzira Upper Prison, November 9, 2010 (10 strokes); Christopher, 17, Bubukwanga Prison, November 16, 2010 (10 strokes); Mary, Jinja Women’s Prison, March 2, 2011 (10 strokes); Mafabi, Butuntumura Prison, November 11, 2010 (15 strokes); Kenneth, Masafu Prison, March 8, 2011 (15 or 20 strokes); Ross, Masafu Prison, March 8, 2011 (20 strokes); Odong, Mutufu Prison, March 7, 2011 (20 strokes); Ali, Murchison Bay Prison, November 20, 2010 (20 strokes); Matovu, Kitalya Farm Prison, February 28, 2011 (24 strokes); Noah, Fort Portal Men’s Prison, November 15, 2010 (30 strokes); Human Rights Watch interview with Emmanuel, Kitalya Farm Prison, February 28, 2011 (40 strokes); Owen, Kitalya, February 28, 2011 (40 strokes); Peter, Masaka Main Prison, November 23, 2010 (50 strokes); Joseph, Kitalya Farm Prison, February 28, 2011 (50 strokes); Human Rights Watch interview with Gilbert, Kitalya Farm Prison, February 28, 2011 (80 strokes); Daudi, Murchison Bay Prison, November 20, 2010 (almost 100 strokes); Evan, Masaka Main Prison, November 23, 2010 (countless); Priscilla, Fort Portal Women’s Prison, November 17, 2010 (countless).
[177] Human Rights Watch facility tour with prison warden, Luzira Upper Prison, November 9, 2010 (“That [punishment system] is theirs, we are not concerned.”); Human Rights Watch interview with OC, Muduuma Prison, November 12, 2010 (“The prisoners do help in running the prison.”).
[178] Human Rights Watch interviews with Owen, Kitalya Farm Prison, February 28, 2011; William, Muinaina Farm Prison, March 4, 2011; George, Mutufu Prison, March 7, 2011; Kevin, Muinaina Farm Prison, March 3, 2011; Walter, Mutufu Prison, March 7, 2011; Matthew, Masafu Prison, March 8, 2011; Eric, Muinaina Farm Prison, March 3, 2011; Moses, Kitalya Farm Prison, February 28, 2011; Mark, Muinaina Farm Prison, March 4, 2011; Matovu, Kitalya Farm Prison, February 28, 2011; Odong, Mutufu Prison, March 7, 2011.
[179] Mental disabilities, as discussed in this report, include diagnosable mental, behavioral, or emotional conditions that substantially interfere with or limit one or more major life activity. Persons with mental health problems also refer to themselves as having psychosocial disabilities, a term that reflects the interaction between psychological differences and social/cultural limits for behavior as well as the stigma that the society attaches to persons with mental impairments.
[180] Human Rights Watch interview with Ali, Murchison Bay Prison, November 20, 2010.
[181] Human Rights Watch interviews with Elizabeth, Jinja Women’s Prison, March 2, 2011; Pius, Muinaina Prison, March 3, 2011.
[182] Human Rights Watch interviews with Elizabeth, Jinja Women’s Prison, March 2, 2011; Tumwesigye, Jinja Main Prison, March 1, 2011.
[183] Human Rights Watch interview with Daudi, Murchison Bay Prison, November 20, 2010 (describing an incident that took place at a farm prison).
[184] Human Rights Watch interview with Ali, Murchison Bay Prison, November 20, 2010 (describing an incident at a farm prison).
[185] Human Rights Watch interview with Owen, Kitalya Farm Prison, February 28, 2011.
[186] Human Rights Watch interview with Matthew, Masafu Prison, March 8, 2011. The prisoner with authority in Matthew’s ward confirmed, “He has had no medical treatment.” Human Rights Watch interview with Stephen, Masafu Prison, March 8, 2011.
[187] Prisons Act of 2006, sec. 81(1).
[188] Prisons Act of 2006, sec. 81(2). Furthermore, punishment by confinement should only take place after an examination and certification of fitness by a medical officer. Prisons Act of 2006, sec. 94.
[189] Prisoners confirmed the use of isolation cell punishment at: Luzira Upper, Luzira Women’s, Murchison Bay, Butuntumura, Fort Portal Women’s, Masaka Ssaza, Masaka Main, Jinja Main, and Muinaina Farm Prisons.
[190] Human Rights Watch interviews with OC, Fort Portal Women’s Prison, November 15, 2010; OC, Masaka Ssaza Prison, November 22, 2010; OC, Masaka Main Prison, November 23, 2010; OC, Jinja Main Prison, March 1, 2011.
[191] Human Rights Watch interviews with Tess, Masaka Ssaza Prison, November 22, 2010 (one month); Asuman, Murchison Bay Prison, November 10, 2010 (two months at Mbarara and Kitalya); Allan, Masaka Main Prison, November 23, 2010 (two months); Evan, Masaka Main Prison, November 23, 2010 (two months); Adam, Masaka Main Prison, November 23, 2010 (three months); Joshua, Masaka Main Prison, November 23, 2010 (three months); Akello, Luzira Women’s Prison, November 10, 2010 (seven months); Gabriel, Jinja Main Prison, March 1, 2011 (one year); Humphrey, Jinja Main Prison, March 1, 2011 (one year); Tumwesigye, Jinja Main Prison, March 1, 2011 (one year).
[192] Human Rights Watch interview with Esther, Fort Portal Women’s Prison, November 17, 2010.
[193] Human Rights Watch interview with Logan, Butuntumura Prison, November 11, 2010.
[194] Human Rights Watch interview with Gabriel, Jinja Main Prison, March 1, 2011.
[195] Human Rights Watch interview with Betty, Masaka Ssaza Prison, November 22, 2010.
[196] Human Rights Watch interview with Joshua, Masaka Main Prison, November 23, 2010.
[197] Human Rights Watch interview with Elizabeth, Jinja Women’s Prison, March 2, 2011.
[198] Human Rights Watch interview with Owen, Kitalya Farm Prison, February 28, 2011.
[199] Human Rights Watch interview with Allan, Masaka Main Prison, November 23, 2010.
[200] Human Rights Watch interview with Ralph, Luzira Upper Prison, November 9, 2010.
[201] Human Rights Watch interview with Gabriel, Jinja Main Prison, March 1, 2011.
[202] Human Rights Watch interview with Abdul, Luzira Upper Prison, November 8, 2010.
[203] Constitution of 1995, art. 24. The Prisons Act also explicitly states that prisoners are entitled to “be treated with the respect due to his/her inherent dignity and value as a human being.” Prisons Act of 2006, sec. 57(a).
[204] See, e.g., UN Human Rights Committee, Communication No. 1184/2003: Australia 27/04/2006, March 2006, para. 9.4.
[205] Human Rights Watch facility assessment, Jinja Main Prison, March 1, 2011. The prison warden, however, contended that the man was bewitched and so it was not necessary to take him for medical treatment. Ibid. The OC at Masaka Ssaza Prison said that he had isolated “a man with mental problems” in the same cell used for punishment while he was awaiting transport to Murchison Bay Hospital. Human Rights Watch interview with OC, Masaka Ssaza Prison, November 22, 2010.
[206] Human Rights Watch interview with deputy OC, Jinja Main Prison, March 1, 2011.
[207] Human Rights Watch interview with Tumwesigye, Jinja Main Prison, March 1, 2011
[208] See, e.g., Universal Declaration of Human Rights (UDHR), adopted December 10, 1948, G.A. Res. 217A(III), U.N. Doc. A/810 at 71 (1948), art. 25(1); International Covenant on Economic, Social and Cultural Rights (ICESCR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 49, U.N. Doc. A/6316 (1966), 993 U.N.T.S. 3, entered into force January 3, 1976, acceded to by Uganda on January 21, 1987, art. 12; Convention on the Rights of the Child (CRC), adopted November 20, 1989, G.A. Res. 44/25, annex, 44 U.N. GAOR Supp. (No. 49) at 167, U.N. Doc. A/44/49 (1989), entered into force September 2, 1990, ratified by Uganda on August 17, 1990, art. 24; African [Banjul] Charter on Human and Peoples’ Rights, adopted June 27, 1981, OAU Doc. CAB/LEG/67/3 rev. 5, 21 I.L.M. 58 (1982), entered into force October 21, 1986, ratified by Uganda May 10, 1986, art. 16.
[209] See, e.g., ICESCR, arts. 12(1) and 2.2; ICCPR, arts. 6, 7 and 10(1); Convention against Torture, art. 16; ICESCR, General Comment No. 14, para. 34. For a comprehensive discussion of the international legal instruments, international resolutions, and model standards related to detainee health, see Rick Lines, “The Right to Health of Prisoners in International Human Rights Law,” International Journal of Prisoner Health, vol. 4(1), 2008, pp. 3-53; Rick Lines, “From Equivalence of Standards to Equivalence of Objectives: The Entitlement of Prisoners to Health Care Standards Higher than Those Outside Prisons,” International Journal of Prisoner Health, vol. 2(4), 2006, pp. 1-12.
[210] The Human Rights Committee has repeatedly determined that the ICCPR requires governments to provide “adequate medical care during detention.” See, e.g., Pinto v. Trinidad and Tobago (Communication No. 232/1987), Report of the Human Rights Committee, vol. 2, UN Doc A/45/40, p. 69. The Committee Against Torture—the monitoring body of the Convention Against Torture—has also found that failure to provide adequate medical care can violate the CAT’s prohibition of cruel, inhuman or degrading treatment. United Nations (UN) Committee against Torture (CAT), “Concluding Observations: New Zealand,” (1998) UN Doc. A/53/44, para. 175.
[211] Concluding Observations of the Human Rights Committee: Republic of Moldova, CCPR/CO/75/MDA, 2002, http://www.unhchr.ch/tbs/doc.nsf/0/7945fe5e4947c21bc1256c3300339d88?Opendocument (accessed December 20, 2010), para. 9.
[212] Prisons Act 2006, sec. 57(f).
[213] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[214] Ibid.
[215] Prison authorities wrote to Human Rights Watch that “few health units are submitting returns and those submitted are incomplete” and not submitted in a timely manner. Letter to Human Rights Watch from prison authorities, June 29, 2011. Information collected by prison authorities and provided to Human Rights Watch on the number of reported health conditions was not comprehensive or representative of the prison population and is not presented in this report.
[216] UPS, “Work Plan and Budget,” p. 4. See also Human Rights Watch interview with prison medical authority, UPS, November 18, 2010 (“Most of our structures are very poor. They don’t allow in air or sufficient light. What do you expect? The transfer of infections such as TB take advantage of that. And they are overcrowded. You can see the scenario.”). As well as being the most common opportunistic infection among people living with HIV in Africa, TB is pervasive in African prisons because of overcrowding, poor ventilation, and lack of prevention practices. UNODC, UNAIDS and World Bank, “HIV and Prisons in Sub-Saharan Africa: Opportunities for Action,” p. 2; E. Rutta et al., “Tuberculosis in a Prison Population in Mwanza, Tanzania (1994-1997),” The International Journal of Tuberculosis and Lung Disease, vol. 5(8), 2001, pp. 703-06.
[217] Tabu Butagira and Lulu Jemimah, “Prisons Chief—Sodomy Is My Biggest Headache,” The Monitor, June 21, 2009, http://allafrica.com/stories/200811240127.html (accessed April 10, 2011).
[218] Human Rights Watch interview with director, National TB and Leprosy Programme, March 10, 2011; World Health Organization, “Global Tuberculosis Control: A Short Update to the 2009 Report,” 2009, http://whqlibdoc.who.int/publications/2009/9789241598866_eng.pdf (accessed October 6, 2010), p.5. High-burden countries are defined as the countries that rank first to 22nd in the world in terms of absolute numbers of TB cases and which have received particular attention at the global level since 2000. Ibid, p. 4.
[219] Republic of Uganda Ministry of Health, “Manual of the National Tuberculosis and Leprosy Programme,” March 2010, p. 3.
[220] Uganda Prisons Service and United Nations Office on Drugs and Crime (UNODC), “A Rapid Situation Assessment of HIV/STI/TB and Drug Abuse Among Prisoners in Uganda Prisons Service: Final Report,” 2008, http://www.unodc.org/documents/hiv-aids/publications/RSA_Report.pdf (accessed August 11, 2010).
[221] UPS, “Work Plan and Budget,” p. 10.
[222] Human Rights Watch interview with Johnson, Bubukwanga Prison, November 16, 2010.
[223] Joint United Nations Programme on HIV/AIDS (UNAIDS), “WHO Guidelines on HIV Infection and AIDS in Prisons,” UNAIDS Best Practice Collection, 1993, http://data.unaids.org/Publications/IRC-pub01/JC277-WHO-Guidel-Prisons_en.pdf (accessed March 3, 2010), pp. 7-8.
[224] TB screening was reported by officers at Fort Portal Women’s and Men’s Prisons, Masaka Ssaza and Masaka Main Prisons, Murchison Bay and Luzira Upper Prisons.
[225] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[226] UPS, “Work Plan and Budget,” p. 12.
[227] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[228] Human Rights Watch interview with Jonathan, Masaka Ssaza Prison, November 22, 2010; Pius, Muinaina Farm Prison, March 3, 2011; William, Muinaina Farm Prison, March 4, 2011.
[229] UPS, “Work Plan and Budget,” p. 12.
[230] Human Rights Watch interview with director, National TB and Leprosy Programme, March 10, 2011.
[231] Ibid.
[232] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. National TB guidelines in Uganda note that prisoners are a risk group for drug-resistant tuberculosis. Republic of Uganda Ministry of Health, “Manual of the National Tuberculosis and Leprosy Program,” p. 47.
[233] Between 1996 and 2006, the coverage of directly observed treatment, short-course (DOTS) expanded from 0 to 100 percent. The DOTS treatment success rate among new sputum smear positive cases was 73 percent. World Health Organization, “Country Profile: Uganda,” 2008, http://www.who.int/tb/publications/global_report/2008/pdf/uga.pdf (accessed August 10, 2010). DOTS coverage is defined as the percentage of the national population living in areas where health services have adopted DOTS. DOTS treatment success rate is defined as the percentage of new smear-positive patients that are cured (negative on sputum smear examination), plus the percentage that complete a course of treatment, without bacteriological confirmation of a cure.
[234] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[235] Ibid.
[236] Human Rights Watch interview with Saul, Masaka Ssaza Prison, November 22, 2010.
[237] Letter from prison authorities to Human Rights Watch, June 29, 2011. Data on prisoner deaths were incomplete and therefore total mortality from TB in the prison system in 2010 could not be ascertained.
[238] See, e.g., Human Rights Watch interviews with Lubega, 17, Bubukwanga Prison, November 16, 2010; OC, Muduuma Prison, November 12, 2010. Furthermore, serious shortages of TB medications at those facilities which do dispense drugs have occurred in Uganda as a result of delays in supply by the Global Drug Facility. Human Rights Watch interview with director, National TB and Leprosy Programme, March 10, 2011.
[239] Human Rights Watch interview with Gilbert, Kitalya Farm Prison, February 28, 2011.
[240] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[241] Ibid.
[242] Prisons Act of 2006, sec. 83(2).
[243] Human Rights Watch interviews with psychiatric nurse, Masaka Main, November 23, 2010; doctor, Murchison Bay Hospital, November 10, 2010; OC, Masaka Ssaza Prison, November 22, 2010.
[244] UNAIDS, “Report on the Global AIDS Epidemic: Annex 1,” 2010, http://www.unaids.org/documents/20101123_GlobalReport_Annexes1_em.pdf (accessed May 5, 2011), p. 181. This prevalence is down from rates over 10 percent through much of the 1990’s, but an increase from 2007’s 5.4 percent. World Health Organization, UNAIDS, and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: Core Data on Epidemiology and Response: Uganda,” 2008, http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_UG.pdf (accessed August 10, 2010).
[245] UPS and UNODC, “A Rapid Situation Assessment of HIV/STI/TB and Drug Abuse Among Prisoners in Uganda Prisons Service.”
[246] Sinamoakosa Isaac and Mwiruwabo James, Uganda Network of AIDS Support Organizations, “Participatory Action Research Report: Treatment Thematic Area,” November 26, 2009 (on file with Human Rights Watch); Foundation for Human Rights Initiative, “The Human Rights Status Report,” p. 42; Uganda Human Rights Commission, “12th Annual Report,” pp. 38-39.
[247] Human Rights Watch interviews with prison warden, Kitalya Farm Prison, February 28, 2011; OC, Muinaina Farm Prison, March 4, 2011; Tabu Butagira and Lulu Jemimah, “Prisons Chief—Sodomy Is My Biggest Headache,” The Monitor, June 21, 2009, http://allafrica.com/stories/200811240127.html (accessed April 10, 2011). To a far lesser extent than male prisoners, female prisoners also stated that sexual activity occurred and that it was punished. Human Rights Watch interview with Stella, Jinja Women’s Prison, March 2, 2011 (“The wardens had beaten up some people who were engaging in [same-sex sexual activity], but I hadn’t seen. There is a girl here we suspect, the prisoners do isolate her. Even the wardens stopped her from going outside.”); Vivian, Jinja women’s Prison, March 2, 2011 (“I heard about it [same-sex sexual activity] in Kamuli, between two women. The ladies complained about them, and reported that they engaged in lesbian activities.”).
[248] See, e.g., Human Rights Watch interviews with Yusuf, Murchison Bay Prison, November 13, 2010 (“It is common....Food is traded for sex—that’s how it’s done.”); Peter, Masaka Main Prison, November 23, 2010 (“Some people try to befriend the new people here on remand. They give them things like sugar cubes. Then they will take them to the toilet and have sexual activities…. I found two people having sex, many times.”); Adam, Masaka Main Prison, November 23, 2010 (“People who have been here more than two years without visitors are sometimes accepting any offer because they need to survive. Sugar, bread, or anything you can eat is given to these people, and they are enticed to having sex.”); Joshua, Masaka Main Prison, November 23, 2010 (“The rich people [with visitors] give the poor people [those without visitors] things like soap, sugar, or bread in exchange for sex. When they catch them, they take them to the cell.”); Kevin, Muinaina Farm Prison, March 3, 2011 (“It is the prison leaders who engage in homosexuality. They [non-leaders] become their wives. They prepare food for them.”); Tobias, Muinaina Farm Prison, March 4, 2011 (“It is because of greed, of not being able to avail yourself with the essential things you would need. So one who had money would send for things like rice, meat—the other would be attracted to those things and they would ask him to have sex with him so he can give him food. He even gives him money to buy whatever he wanted.”); Gabriel, Jinja Main Prison, March 1, 2011 (“Some also use enticements, like edibles. Someone can use rice meal.”); Ralph, Luzira Upper Prison, November 9, 2010 (“Sex? Yes, they do that. Someone may exchange rice, or food—he gets what he wants.”).
[249] Human Rights Watch interview with Gilbert, Kitalya Farm Prison, February 28, 2011.
[250] Human Rights Watch interview with Mukasa, Luzira Upper Prison, November 9, 2010.
[251] Human Rights Watch interviews with Brian, Murchison Bay Prison, November 13, 2010; Henry, Murchison Bay Prison, November 20, 2010; Allan, Masaka Main Prison, November 23, 2010; Owen, Kitalya Farm Prison, February 28, 2011; Peter, Masaka Main Prison, November 23, 2010.
[252] Human Rights Watch interview with Joshua, Masaka Main Prison, November 23, 2010.
[253] Human Rights Watch interview with Noah, Fort Portal Men’s Prison, November 15, 2010.
[254] Human Rights Watch interview with Jacob, Luzira Upper Prison, November 8, 2011. See also Human Rights Watch interviews with Brian, Murchison Bay Prison, November 13, 2010; Edmund, Muinaina Farm Prison, March 4, 2011.
[255] UNAIDS, “WHO Guidelines on HIV Infection and AIDS in Prisons,” UNAIDS Best Practice Collection, 1993, http://data.unaids.org/Publications/IRC-pub01/JC277-WHO-Guidel-Prisons_en.pdf (accessed March 3, 2010), p. 5. WHO, UNAIDS, UNODC, “Policy Brief: Reduction of HIV Transmission in Prisons,” Doc. No. WHO/HIV/2004.05 (2004), p. 2. In 2007, the WHO, UNODC, and UNAIDS noted that studies have found condom provision in prisons to be feasible, acceptable to prisoners, acceptable to prison staff, and did not have negative consequences such as compromising prison safety or security. Furthermore, “[f]ears about the provision of condoms leading to more consensual and non-consensual sex were not realized.” WHO, UNODC, UNAIDS, “Interventions to Address HIV in Prisons: Prevention of Sexual Transmission,” 2007, p. 13.
[256] Penal Code Act of 1950, cap. 120, sec. 145.
[257] UPS, “Work Plan and Budget,” pp. 10-12.
[258] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010. Prisoners’ reactions to the idea of distributing condoms in the prison ranged from bewilderment (“what is the use of it as a prisoner?”) to disapproval (“they should not be here, those who do it should be arrested”) to fear that the introduction could lead to an increase in a practice of which many inmates strongly disapprove (“it would promote homosexuality”). Human Rights Watch interviews with Edgar, Murchison Bay Prison, November 13, 2010; Peter, Masaka Main Prison, November 23, 2010; Kakooza, Masaka Main Prison, November 23, 2010.
[259] Human Rights Watch interview with Kiyonga, Luzira Upper Prison, November 9, 2010.
[260] These include the AIDS Support Organization (TASO) and the AIDS Information Center. Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[261] Human Rights Watch interviews with Okello, Luzira Upper Prison, November 8, 2010; Saul, Masaka Ssaza Prison, November 22, 2010.
[262] UPS, “Work Plan and Budget,” pp. 10-12.
[263] Informed consent is a well-established element of international guidance on HIV testing. WHO and UNAIDS, “Guidance on Provider-Initiated HIV Testing and Counselling in Health Facilities,” March 2007, http://whqlibdoc.who.int/publications/2007/9789241595568_eng.pdf (accessed June 26, 2011).
[264] Human Rights Watch interviews with Enid, Luzira Women’s Prison, November 9, 2010.
[265] Between 2004 and 2009, the number of people on antiretroviral therapy rose from 44,000 to 200,413. However, a significant gap of people requiring ART who were not receiving it still existed. WHO, UNIDS, and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS: Core Data on Epidemiology and Response: Uganda,” 2008, http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_UG.pdf (accessed August 10, 2010); UNAIDS, “Report on the Global AIDS Epidemic: Annex 2,” 2010, http://www.unaids.org/documents/20101123_GlobalReport_Annexes2_em.pdf (accessed May 5, 2011), p. 252.
[266] UNODC and UPS reported in 2008 that only 100 prisoners on antiretroviral therapy could be documented, but in that same year the Uganda Human Rights Commission suggested that 2,050 prisoners (out of a total population of 28,205) were on ART and cotrimoxazole (Septrin). UPS and UNODC, “A Rapid Situation Assessment of HIV/STI/TB and Drug Abuse Among Prisoners in Uganda Prisons Service.” Uganda Human Rights Commission, “11th Annual Report of the Uganda Human Rights Commission to the Parliament of Uganda,” 2008, p. 45. On the day of researchers’ visits, 345 patients at Luzira Upper were reportedly on some form of HIV treatment; 56 at Murchison Bay were reportedly on ART. Human Rights Watch interview with Kiyonga, Luzira Upper Prison, November 9, 2010; Human Rights Watch interview with doctor, Murchison Bay Hospital, November 10, 2010. Prison authorities reported to Human Rights Watch that, at the 15 prisons providing data during the period of July to December 2010, 1,465 prisoners were on ART. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[267] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[268] Ibid.
[269] Human Rights Watch interview with OC, Muduuma Prison, November 12, 2010.
[270] Human Rights Watch interview with Washington, Muduuma Prison, November 12, 2010.
[271] Human Rights Watch interviews with Logan, Butuntumura Prison, November 11, 2010; Kakura, Butuntumura Prison, November 11, 2010.
[272] Letter from prison authorities to Human Rights Watch, June 29, 2011. Data on prisoner deaths were incomplete and therefore total mortality from HIV/AIDS in the prison system in 2010 could not be ascertained.
[273] Human Rights Watch interview with prison warden, Kitalya Farm Prison, February 28, 2011.
[274] Human Rights Watch interview with OC, Muinaina Farm Prison, March 3, 2011.
[275] Drug shortages or stockouts for ARVs have been reported regularly in Uganda as a result of problems in the supply and distribution system. See, e.g., Government of Uganda, “UNGASS Country Progress Report Uganda: January 2008-December 2009,” March 2010, p. 33; Richard Hasunira, Aaron Muhinda, Rosette Mutambi and Beatrice Were, “Uganda,” in Missing the Target: Failing Women, Failing Children: HIV, Vertical Transmission, and Women’s Health, International Treatment Preparedness Coalition, May 2009, p. 56.
[276] World Health Organization, “Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach: 2010 Revision,” 2010, http://whqlibdoc.who.int/publications/2010/9789241599764_eng.pdf (accessed May 5, 2011), p. 19.
[277] Human Rights Watch interview with doctor, Murchison Bay Hospital, November 10, 2010.
[278] WHO, “Antiretroviral Therapy for HIV Infection in Adults and Adolescents: Recommendations for a Public Health Approach,” 2006, http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf (accessed March 4, 2010), p. 70.
[279] Human Rights Watch interviews with Gerard, Murchison Bay Prison, November 20, 2010; nurse, Luzira Upper Prison, November 9, 2010; Kenneth, Masafu Prison, March 8, 2011.
[280] Human Rights Watch interview with Kenneth, Masafu Prison, March 8, 2011. HIV-positive prisoners do not routinely receive government-provided food supplements outside of the Luzira/Murchison Bay complex.
[281] Human Rights Watch interviews with Matthew, Masafu Prison, March 8, 2011; Washington, Muduuma Prison, November 12, 2010; Gerard, Murchison Bay Prison, November 20, 2010; Kenneth, Masafu Prison, March 8, 2011.
[282] Human Rights Watch interview with Okello, Luzira Upper Prison, November 8, 2010.
[283] Human Rights Watch interview with Rebecca, Luzira Women’s Prison, November 10, 2010.
[284] Human Rights Watch interview with Gerard, Murchison Bay Prison, November 20, 2010.
[285] Government of Uganda Ministry of Health, “National Health Policy: Reducing Poverty Through Promoting People’s Health,” May 2009, http://www.health.go.ug/National_Health.pdf (accessed August 11, 2010), p. 2.
[286] Ibid., p. 14.
[287] Human Rights Watch interview with OC, Muinaina Farm Prison, March 3, 2011. See also Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[288] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[289] Human Rights Watch interview with OC, Fort Portal Prison, November 15, 2010.
[290]Human Rights Watch interviews with OC, Masaka Ssaza Prison, November 22, 2010; OC, Masafu Prison, March 8, 2011; OC, Muinaina Farm Prison, March 4, 2011; warden, Kitalya Farm Prison, February 28, 2011; OC, Masaka Main Prison, November 23, 2010.
[291] Human Rights Watch interviews with OC, Masafu Prison, March 8, 2011; OC, Jinja Main Prison, March 2, 2011.
[292] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[293] UPS, “Work Plan and Budget,” pp. 12-13.
[294] Human Rights Watch interviews with OC, Murchison Bay Prison, November 10, 2010; psychiatric nurse, Masaka Main Prison, November 23, 2010.
[295]Human Rights Watch interviews with OC, Masaka Ssaza Prison, November 22, 2010; OC, Masaka Main Prison, November 23, 2010; OC, Masafu Prison, March 8, 2011.
[296] Human Rights Watch interview with OC, Masafu Prison, March 8, 2011.
[297] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 29. In 2010 prison authorities also reported deaths from malaria. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[298] World Health Organization, “Malaria and HIV Interactions and their Implications for Public Health Policy,” 2005, http://www.who.int/hiv/pub/prev_care/malariahiv.pdf (accessed May 4, 2011).
[299] Human Rights Watch interviews with Simon, 14, Bubukwanga Prison, November 16, 2010; Christopher, 17, Bubukwanga Prison, November 16, 2010; Isaac, Jinja Main Prison, March 1, 2011; Thomas, Mutufu Prison, March 7, 2011. See also, Hudson Apunyo, “10 Inmates Die in Lira Prison,” The Monitor, April 17, 2006, http://allafrica.com/stories/200408170111.html (accessed April 10, 2011).
[300] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011; UPS, “Work Plan and Budget,” pp. 12-13.
[301] Human Rights Watch interview with George, Matufu Prison, March 7, 2011.
[302] UPS, “Work Plan and Budget,” p. 4; Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[303] See, e.g., Human Rights Watch interview with Ralph, Luzira Upper Prison, November 9, 2010. Diarrhea was a cause of death among prisoners in 2007/08 and 2008/09, and cholera in 2005/06. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 28.
[304] UPS, “Work Plan and Budget,” p. 5. Diarrhea and dysentery were both reported among the causes of prisoner deaths in 2010. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[305] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[306] Human Rights Watch interview with Jonathan, Masaka Ssaza Prison, November 22, 2010.
[307] Human Rights Watch interviews with doctor, Murchison Bay Hospital, November 10, 2010; psychiatric nurse, Masaka Main Prison, November 23, 2010; UPS, “Work Plan and Budget,” p. 5.
[308] Human Rights Watch interview with psychiatric nurse, Masaka Main, November 23, 2010.
[309] Human Rights Watch interview with Kaahwa, Bubukwanga Prison, November 16, 2010; Human Rights Watch interview with Ekanya, Bubukwanga Prison, November 16, 2010; Human Rights Watch interview with Otto, Bubukwanga Prison, November 16, 2010; Human Rights Watch interview with Gideon, 15, Bubukwanga Prison, November 16, 2010.
[310] UNODC and UNAIDS, “Women and HIV in Prison Settings,” September 2008, http://www.unodc.org/documents/hiv-aids/Women%20and%20HIV%20in%20prison%20settings.pdf (accessed March 3, 2010), p. 2. See also Vetten, “The Imprisonment of Women in Africa,” in Jeremy Sarkin, ed., Human Rights in African Prisons, (Cape Town: HSRC Press, 2008).
[311] Protocol to the African Charter on Human and Peoples’ Rights on the Rights of Women in Africa (Maputo Protocol), adopted by the 2nd Ordinary Session of the Assembly of the Union, Maputo, CAB/LEG/66.6 (September 13, 2000); entered into force November 25, 2005. Ratified by Uganda on July 22, 2010.
[312] Maputo Protocol, article 24.
[313] UN Standard Minimum Rules for the Treatment of Prisoners, para. 23.
[314] Brenda J. van den Bergh, Alex Gatherer and Lars F. Møller, “Women’s Health in Prison: Urgent Need for Improvement in Gender Equity and Social Justice,” Bulletin of the World Health Organization, vol. 87, 2009, p. 406.
[315] Human Rights Watch interview with Christine, Fort Portal Women’s Prison, November 15, 2010.
[316] Human Rights Watch interview with Lydia, Masafu Prison, March 8, 2011.
[317] Human Rights Watch interview with OC, Murchison Bay Prison, November 10, 2010.
[318] Human Rights Watch interview with Agatha, Luzira Women’s Prison, November 9, 2010; Mercy, Luzira Women’s Prison, November 9, 2010.
[319] Human Rights watch interview with Grace, Masaka Ssaza Prison, November 22, 2010.
[320] Human Rights Watch interview with Mercy, Luzira Women’s Prison, November 9, 2010.
[321] Human Rights Watch interview with Dorothy, Butuntumura Prison, November 11, 2010.
[322] Human Rights Watch interview with Hannah, Luzira Women’s Prison, November 10, 2010.
[323] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[324] World Health Organization, “Rapid Advice: Use of Antiretroviral Drugs for Treating Pregnant Women and Preventing HIV Infection in Inmates,” November 2009, http://www.who.int/hiv/pub/mtct/rapid_advice_mtct.pdf (accessed March 3, 2010), p. 13.
[325] Human Rights Watch interview with Hellene, 16, Butuntumura Prison, November 11, 2010.
[326] Human Rights Watch interviews with Hellene, 16, Butuntumura Prison, November 11, 2010; Christine, Fort Portal Women’s, November 15, 2010; Betty, Masaka Ssaza Prison, November 22, 2010; Mary, Jinja Women’s Prison, March 2, 2011; Vivian, Jinja Women’s Prison, March 2, 20111; Stella, Jinja Women’s Prison, March 2, 2011; Elizabeth, Jinja Women’s Prison, March 2, 2011; Catherine, Jinja Women’s Prison, March 2, 2011.
[327] Human Rights Watch interviews with Esther, Fort Portal Women’s Prison, November 17, 2010; Priscilla, Fort Portal Women’s Prison, November 17, 2010.
[328] See, e.g., Human Rights Watch interviews with Hellene, 16, Butuntumura Prison, November 11, 2010; Betty, Masaka Ssaza Prison, November 22, 2010; Mary, March 2, 2011; Catherine, Jinja Women’s Prison, March 2, 2011.
[329] Human Rights Watch interview with Hellene, 16, Butuntumura Prison, November 11, 2010.
[330] Human Rights Watch interview with Mary, Jinja Women’s Prison, March 2, 2011.
[331] Penal Code Act of 1950, sec. 11.
[332] Trial on Indictments Act, sec. 45.
[333] The lack of a psychiatrist on staff has resulted in reliance on a doctor visiting from Butabika Hospital, Uganda’s sole psychiatric center. However, the doctor’s visit can be as infrequent as once a month. Human Rights Watch interview with OC, Murchison Bay, November 10, 2010. The lack of personnel trained in mental health and therefore able to determine competency to stand trial is an issue not only in the prison system but in the country as a whole, where there are only 32 psychiatrists nationwide. Human Rights Watch interview with president, Uganda Medical Association, March 11, 2011.
[334] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. JLOS has highlighted one of its key challenges as “the absence of medical-legal policy and guidelines [such as] handling of criminal lunatics among others.” Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010,” September 2010.
[335] Human Rights Watch interview with Miriam, Fort Portal Women’s Prison, November 15, 2010; Elliot, Murchison Bay, November 13, 2010; Mutebi, Muduuma Prison, November 12, 2010; Paul, Muduuma Prison, November 12, 2010; Felix, Fort Portal Prison, November 15, 2010; Drani, Fort Portal Prison, November 15, 2010.
[336] Individuals found not guilty “by reason of insanity” (or who are found guilty and sentenced to death as minors) must await orders from the Minister of Justice and Constitutional Affairs for his decision on whether that person will be detained in a prison, a hospital, or other place of custody, or alternatively released. Trial on Indictments Act, secs. 48 and 105. In reality, however, because the Minister of Justice flouts his statutory duty to resolve such cases, these prisoners remain in legal limbo for years without knowing how long they will be detained, where they should be detained, or whether they are entitled to release. Human Rights Watch, “Uganda: Languishing Behind Bars: Resolve Overdue Cases of Prisoners with Mental Disabilities,” April 28, 2011, http://www.hrw.org/en/news/2011/04/28/uganda-languishing-behind-bars.
[337] This statistic was derived using an entry screening process by UPS, still in its very early stages. Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. Uganda has ratified the Convention on the Rights of Persons with Disabilities. Convention on the Rights of Persons with Disabilities (CRPD), adopted December 13, 2006 by G.A. Res. 61/106, Annex I, U.N.GAOR, 61st Sess., Supp. No. 49 at 65, U.N. Doc A/61/49 (2006), entered into force May 3, 2008, U.N. Doc. A/61/61, signed by Uganda on March 30, 2007 and ratified by Uganda on September 25, 2008.
[338] See, e.g., Human Rights Watch facility tour with prison officer, Luzira Upper Prison, November 9, 2010; Kiyonga, Luzira Upper Prison, November 9, 2010; Fred, Luzira Upper Prison, November 8, 2010.
[339] UPS, “Work Plan and Budget,” pp. 12-13.
[340] Human Rights Watch interview with president, Uganda Medical Association, March 11, 2011.
[341] Letter from prison authorities to Human Rights Watch, June 29, 2011.
[342] See, e.g., Human Rights Watch interview with Mutebi, Muduuma Prison, November 12, 2010; Human Rights Watch interview with Paul, Muduuma Prison, November 12, 2010; Human Rights Watch interview with psychiatric nurse, Masaka Main Prison, November 23, 2010.
[343] Human Rights Watch interview with president, Uganda Medical Association, March 11, 2011.
[344] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011; Human Rights Watch interview with psychiatric nurse, Masaka Main Prison, November 23, 2010.
[345] Ibid. Luzira Upper and Murchison Bay each have wards housing 15 to 20 inmates with mental health problems. Human Rights Watch facility tour with prison warden, Luzira Upper Prison, November 9, 2010; interview with OC, Murchison Bay Prison, November 13, 2010.
[346] At Jinja Main, a major regional center, Human Rights Watch researchers found a prisoner with “mental problems” shut away in an isolation cell. He reported that he had received no medication or visits from a health worker. Human Rights Watch facility assessment of Jinja Main Prison, March 2, 2011. A psychiatrist visits Murchison Bay from the Butabika mental hospital, and a clinical psychiatric officer and psychiatric nurse are on staff. But even at Murchison Bay Hospital, prisoners housed in the mental health cell reported simply receiving medication from another inmate. Human Rights Watch interviews with Elliot, Murchison Bay Prison, November 13, 2010; Ali, Murchison Bay Prison, November 20, 2010; Drani, Fort Portal Men’s Prison, November 15, 2010.
[347] Human Rights Watch interview with president, Uganda Medical Association, March 11, 2011.
[348] See, e.g., UPS, “Summary of UPS Prisoners Statistical Returns”; Uganda Human Rights Commission, “12th Annual Report,” p. 24.
[349] ICCPR, art. 9. See also UN Human Rights Committee, General Comment No. 8 on the International Covenant on Civil and Political Rights, Article 9, U.N. Doc. A/40/40 (1982). The UN Human Rights Committee has made clear that detention before trial should be used only to the extent that it is lawful, reasonable, and necessary. Necessity is defined narrowly: “to prevent flight, interference with evidence or the recurrence of crime” or “where the person concerned constitutes a clear and serious threat to society which cannot be contained in any other manner.” UN Human Rights Committee, Hugo van Alphen v. the Netherlands, Communication No. 305/1988 (1990), para. 5.8. International standards provide that except in special cases, a person detained on a criminal charge shall be entitled to release pending trial subject to certain conditions. Body of Principles, prins 38-39; United Nations Standard Minimum Rules for Non-custodial Measures (“The Tokyo Rules”), adopted December 14, 1990, G.A. Res. 45/110, annex, 45 U.N. GAOR Supp. (No. 49A) at 197, U.N. Doc. A/45/49 (1990), paras. 6.1-6.2 (“Pretrial detention shall be used as a means of last resort in criminal proceedings.”); Martin Schönteich, “Pretrial Detention and Human Rights in Africa,” in Jeremy Sarkin, ed., Human Rights in African Prisons, (Cape Town: HSRC Press, 2008), pp. 93-116.
[350] UPS, “Summary of UPS Statistical Returns.”
[351] Defilement, defined as “a sexual act with another person who is below the age of eighteen years,” accounts for roughly a third of all capital cases in prisons. There is a wide literature on the use of the crime as a means of extracting civil redress for families, often in instances of consensual relationships. Penal Code Amendment Act of 2007, sec. 2. UPS, “Census of Prisoners in 48 Central Government Prisons,” September 30, 2007. In 2008, due to the high number of defilement cases, the law was amended to allow magistrate’s courts as well as High Courts to hear such cases.
[352] Chief Justice of Uganda Benjamin Odoki, “Speech at the Case Backlog Review,” March 7, 2011. Capital offences must be heard by a High Court, while lesser offences can be heard by either a magistrate’s court or High Court.
[353] Justice Law and Order Sector, “Annual Performance Report,” September 2010.
[354] ICCPR, art. 9; Body of Principles, prins. 10, 11 and 37. See also, African Charter, art. 7. The African Commission on Human and Peoples’ Rights has determined that detaining two applicants, for, respectively, five months and slightly over one month without being brought before a judge violated Charter’s protections on fair trial. African Commission on Human and Peoples’ Rights, Huri-Laws v. Nigeria, Comm. No. 225/98 (2000), http://www1.umn.edu/humanrts/africa/comcases/225-98.html (accessed March 4, 2010).
[355] Constitution of Uganda, art. 23 (4); Uganda Prisons Service, “Census of Prisoners in 48 Central Government Prisons.”
[356] UPS in 2007 said that of inmates in the central region, where adherence to law is usually best in the country, 70 percent were not taken within this 48-hour period. UPS, “Census of Prisoners in 48 Central Government Prisons.” Only 15 percent prisoners Human Rights Watch surveyed were taken to court within this time period. The vast majority stay in police stations for long periods of times—in some cases up to several months—without understanding the charges against them and in overcrowded cells without water or bathing facilities, in some instances without even being allowed to contact relatives. Human Rights Watch interviews with Roger, Masaka Ssaza Prison, November 22, 2011; Ross, Masafu Prison, March 8, 2011; Kenneth, Masafu Prison, March 8, 2011; Benjamin, Masafu Prison, March 8, 2011; Lucas, 17, Masafu Prison, March 8, 2011; Obua, Masaka Prison, March 23, 2010; Byamukama, Masaka Ssaza Prison, November 22, 2010.
[357] Human Rights Watch interviews with Sebastian, November 8, 2010; Winifred, November 10, 2010; Asuman, Luzira Upper, November 10, 2010; Edward, Muinaina Prison, March 4, 2011; Tobias, Muinaina Prison, March 4, 2011; Michael, Muinaina Prison, March 4, 2011; Bradley, Muinaina Prison, March 3, 2011.
[358] Human Rights Watch interviews with Edgar, Murchison Bay, May 13, 2011; Henry, Murchison Bay, November 20, 2011; Hugh, Jinja Main Prison, March 1, 2011; Edward, Muinaina Prison, March 4, 2011; Edmund, Muinaina Prison, March 4, 2011; Eric, Muinaina Prison, March 3, 2011; Mark, Muinaina Prison, March 4, 2011.
[359] Human Rights Watch interviews Jonathan, Masaka Ssaza Prison, November 22, 2010; Moses, Kitalya Prison, February 28, 2011; Ibrahim, Kitalya Prison, February 28, 2011; Pius, Muinaina Prison, March 03, 2011; Duncan, Muinaina Prison, March 4, 2011; William, Muinaina Prison, March 4, 2011
[360] A recent study of over 2,000 remand detainee records documented that in 32 percent of cases examined, capital detainees had been detained over 180 days prior to committal, and non-capital detainees had been detained for over 60 days before commencement of trial. That study attributed long remand times to issues including unlawful arrests by a multitude of overlapping security forces, a shortage of judges and magistrates, lack of legal representation, poor trial administration, and ineffective investigation practices. Avocats Sans Frontieres and University of Toronto International Human Rights Program, “Presumed Innocent, Behind Bars: The Problem of Lengthy Pretrial Detention in Uganda,” 2011. Furthermore, Uganda’s auditor general has noted that, among almost 40,000 criminal cases handled between July 2006 and June 2010, only 18 percent had been completed within 12 months, the maximum target for completion of capital cases. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Disposing of Cases in the Judiciary,” March 2011, p. 19 (citing the Judiciary Staff Handbook, p. 56).The auditor general attributed long remand times to a combination of problematic court procedures, inadequate infrastructure , low staffing levels, and lack of monitoring and evaluation of the judiciary. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Disposing of Cases in the Judiciary.”
[361] Bruce Kyerere, president of Uganda Law Society, “Review of the Case Backlog Quick Wins Reduction Program,” March 7, 2011 (highlighting Kiboga, Entebbe, Mubende, and Mpigi districts as having infrequent court sessions).
[362] Human Rights Watch interview with OC, Muinaina Prison, Mubende District, March 3, 2011. Mubende, Mityana, Kasanda, Kiboga, and Kyankwanzi are the five districts the court covers. According to prisoners, it sat only once the previous year, and for only two months. Human Rights Watch interviews with Bradley, Muinaina Prison, March 3, 2011; Mohamed, Muinaina Prison, March 4, 2011.
[363] The Ugandan constitution states, “In the determination of…any criminal charge, a person shall be entitled to a fair, speedy and public hearing before an independent and impartial court or tribunal established by law.” Article 28(1).
[364] In one recent study, detainees under the jurisdiction of the High Court spent an average of 488 days on committal from the date of committal to the date of data collection. Avocats Sans Frontieres and University of Toronto International Human Rights Program, “Presumed Innocent, Behind Bars,” p. 34.
[365] Human Rights Watch interviews with Donald, Masaka Main Prison, November 23, 2010; Ekanya, Bubukwanga Prison, November 16, 2010; Christopher, 17, Bubukwanga Prison, November 16, 2010; Sylvia, Fort Portal Women’s Prison, November 15, 2010; Abigail, Fort Portal Women’s Prison, November 15, 2010.
[366] Human Rights Watch interview with Ekanya, Bubukwanga Prison, November 16, 2010.
[367] Human Rights Watch, “Violence Instead of Vigilance: Torture and Illegal Detention by Uganda’s Rapid Response Unit,” March 23, 2011, http://www.hrw.org/en/reports/2011/03/23/violence-instead-vigilance; Avocats Sans Frontieres and University of Toronto International Human Rights Program, “Presumed Innocent, Behind Bars,” 2011; Human Rights Watch interview with OC, Kigo Prison, November 19, 2009. The African Commission, interpreting the African Charter on Human and Peoples’ Rights, has prohibited the trial of civilians in military courts. The African Charter, to which Uganda is a party, guarantees the right to equality before the law and equal protection of the law, fair trial, and judicial independence. The African Charter does not admit any exceptions to the rule against the use of military courts to try civilians, such as emergency situations. The Commission’s Principles and Guidelines on the Right to a Fair Trial and Legal Assistance in Africa also prohibits the trial of civilians in military courts. Law Office of Ghazi Suleiman v. Sudan, Comm. Nos. 222/98 and 229/99, para. 64 (African Commission on Human and Peoples’ Rights 2003); Media Rights Agenda v. Nigeria, Comm. No. 224/98, paras. 60-66 (African Commission on Human and Peoples’ Rights 2000). African (Banjul) Charter on Human and Peoples’ Rights art. 2, June 27, 1981, 21 I.L.M. 58 (entered into force Oct. 21, 1986) [hereinafter African Charter], arts. 2, 3, 7, and 26. African Commission on Human and Peoples’ Rights, Principles and Guidelines on the Right to a Fair Trial and Legal Assistance inAfrica (Nov. 1999)
[368] Chief Justice of Uganda Benjamin Odoki, “Speech at the Case Backlog Review,” March 7, 2011.
[369] Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010,” September 2010. Uganda’s auditor general notes that the case backlog increased from 65,423 in FY 2006/07 to 126, 521 in 2009/10. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Disposing of Cases in the Judiciary,” March 2011, p. 1.
[370] Article 23(6) as amended by the Constitution of the Republic of Uganda (Amendment) Act 11/2005 provides: “(6) where a person is arrested in respect of a criminal offence –(a) the person is entitled to apply to the court to be released on bail and the court may grant that person bail on such conditions as the court considers reasonable; (b) in the case of an offence which is triable by the High Court as well as by a subordinate court, if that person has been remanded in custody in respect of the offence for sixty days before trial, that person shall be released on bail on such conditions as the court considers reasonable; (c) in the case of an offence triable only by the High Court, if that person has been remanded in custody for one hundred and eighty days before the case is committed to the High Court, that person shall be released on bail on such conditions as the court considers reasonable.” Before the constitutional amendment, (b) and (c) stated 120 and 360 respectively as the number of days that must pass before a person is entitled to bail. See alsoUganda v. Besigye, Constitutional Court of Uganda at Kampala, Constitutional Reference No. 20 of 2005, September 22, 2006 in which the Court held that under article 23 (6) (a) of the Constitution the court has a discretion whether to grant bail or not to grant bail and that bail is not automatic. However the Court also observed that “while considering bail the court would need to balance the constitutional rights of the applicant. … and the considerations which flow from people being remanded in prison custody which adversely affects their welfare and that of their families and not least the effect on prison remand conditions if large numbers of unconvicted people are remanded in custody.” In Foundation for Human Rights Initiative vs. the Attorney General, Constitutional Petition No. 20 of 2006, March 26, 2008 the Constitutional Court confirmed that Article 23(6) of the Constitution confers discretion upon court whether to grant bail. Foundation for Human Rights Initiative is appealing the ruling to the Supreme Court. Human Rights Watch Interview with executive director, Foundation for Human Rights Initiative, Kampala, March 9, 2011.
[371] Human Rights Watch interview with paralegal, Kampala, November 19, 2010.
[372] The Magistrates Court Act requires the Director of Public Prosecutions (DPP) to provide the magistrate’s court with an indictment and a summary of the case in order to commit a case to the High Court. Magistrates Court Act of 1971, sec. 168. The Trial on Indictments Act does not allow a person accused of a criminal offence triable by the High Court to be produced in the High Court unless and until such person has been committed for trial by the DPP. Trial on Indictments Act of 1971, sec. 1. Due to the criminal process’s dependency upon the speed of the DPP’s actions, prisoners can continue on remand without any statutorily defined time limitations.
[373] Human Rights Watch interview with paralegal, Kampala, November 19, 2010.
[374] See, e.g., James Sebugenyi, “Bail is a Fundamental Right,” New Vision, May 22, 2011, http://www.newvision.co.ug/D/8/20/755380 (accessed June 21, 2011); Ofwondo Opondo and Wafula Oguttu, “What Does the Proposed Amendment to Scrap Bail Mean for Uganda?” Sunday Vision, May 21, 2011, http://www.sundayvision.co.ug/detail.php?mainNewsCategoryId=7&newsCategoryId=614&newsId=755249 (accessed June 21, 2011). However, eliminating the possibility of bail for nonviolent crimes is inconsistent with human rights standards, under which pretrial restrictions must be consistent with the right to liberty and the presumption of innocence. ICCPR, arts. 9 and 14. Indeed, under international law, the presumption is that “It shall not be the general rule that persons awaiting trial shall be detained in custody, but release may be subject to guarantees to appear for trial.” ICCPR, art. 9(3).
[375] For lesser crimes, the Magistrate’s Court’s Act says that courts consider the nature and gravity of the charge, prior charges, whether the suspect has a fixed abode, and the suspect’s likelihood to “interfere with any of the witnesses” into consideration when adjudging bail applications.” Magistrates Courts Act, Sec. 77(2). For capital crimes, the High Court is to consider whether the suspect has a fixed place of abode, sound securities, prior instances of failure to comply with bail, or other charges. Trial on Indictment Act, sec. 15(4).
[376] Although Article 23 (6) (a) of the Constitution (as amended) has been held to bestow discretion on the courts as to whether to grant bail—where a person is arrested in respect of a criminal offence the person is entitled to apply to the court to be released on bail and the court may grant that person bail—the Constitutional Court also held that is not true of articles 23 (6) (b) and (c). Article 23 (6) (b) provides that for “an offence which is triable by the High Court as well as by a subordinate court” if a person “has been remanded in custody for sixty days before trial, that person shall be released on bail” on conditions set by the court. Under article 23 (6) (c) if the offence is triable only by the High Court, then bail is to be granted if the accused has been in remand for 180 days. The Constitutional Court has said that in the cases of both Article 23 (6) (b) and (c), bail must be granted and there is no discretion. See Uganda v. Besigye, September 22, 2006. In practice, though, this does not happen.
[377] Human Rights Watch interviews with Nyombi, Masaka Ssaza Prison, November 22, 2010; Olivia, Masaka Prison November 23, 2010; Emma, Jinja Women’s, March 2, 2011; Duncan, Muinaina Prison, March 4, 2011; Washington, Muduuma Prison, November 12, 2010.
[378] Human Rights Watch interview with Bradley, Muinaina Prison, March 3, 2011.
[379] Human Rights Watch interviews with Matthew, Masafu Prison, March 8, 2011; Christopher, 17, Bundibuygo Prison, November 16, 2010.
[380] Constitution of Uganda, art. 28(3)(e). The government reportedly spends 38 million Uganda shillings (approximately $19,000) per month on providing state briefs. Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010,” September 2010.
[381] Constitution of Uganda, art. 28(3)(e).
[382] The Uganda Paralegal Advisory Services dispatches its own paralegals and also funds other legal aid organizations, such as AHURIO in Fort Portal, Uganda Christian Lawyers Fraternity in Kampala, and Foundation for the Development of Needy Communities in Mbale, as well as in some instances giving UPS social workers training on paralegal services. Law & Development Partnership, “Evaluation, Paralegal Advisory Services, 2007-2010,” January 7, 2011. For a description of legal aid services available in Uganda, see generally, UN Office on Drugs and Crime, “Handbook on Improving Access to Legal Aid in Africa,” 2011, http://www.unodc.org/documents/justice-and-prison-reform/Webbook_Legal_Aid_in_Africa_lr.pdf (accessed April 25, 2011).
[383] Sarah Callaghan, Chairperson JLOS Development Partners Group ,“JLOS Development Partner Group Response to Annual Progress,” October 4-5, 2010.
[384] Police bond can also be issued by discretion of the police. Human Rights Watch interviews with David, Kitalya Farm Prison, February 28, 2011; Noah, Fort Portal Prison, November 15, 2010; Christine, Fort Portal Women’s Prison, November 15, 2010; Arthur, Mutufu Prison, March 7, 2011; Matovu, Kitalya Farm Prison, February 28, 2011; Kevin, Muinaina Prison, March 3, 2011.
[385] ICCPR, art. 14(3)(d); Body of Principles, prin. 17.
[386] Human Rights Watch interviews with Donald, Masaka Prison, November 23, 2010; Ibrahim, Kitalya, February 28, 2011; Lucas, 17, Masafu, March 8, 2011.
[387]Law & Development Partnership, “Evaluation, Paralegal Advisory Services, 2007-2010,” January 7, 2011; “Leave Bail Money Alone,” New Vision, August 30, 2008; “Billions Lost in Bail Cash Abuse,” Monitor, August 29, 2008; JLOS, “Report of the Joint JLOS/DPG Monitoring Visit, Lango and Acholi Sub-Regions,” June 2010, http://www.jlos.go.ug/uploads/m%20and%20E%20Report%202010.pdf (accessed April 11, 2011). The Inspectorate of Courts received 740 complaints of judicial misbehavior in 2009-2010, though the government purported that it has taken measures to combat corruption by conducting 71 inspections during that period. Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010,” September 2010. According to Transparency International, Ugandans said on a scale of 1-5, with 5 being “extremely corrupt,” they perceived the judiciary to be at 3.9. Transparency International, “Global Corruption Barometer 2010,” 2010, http://www.transparency.org/policy_research/surveys_indices/gcb/2010/results (accessed April 28, 3011).
[388] Sarah Callaghan, Chairperson JLOS Development Partners Group, “JLOS Development Partner Group Response to Annual Progress,” October 4-5, 2010.
[389] Police offered suspects the option of paying to two million Uganda shillings (approximately $840) to dismiss files, magistrates offered to dismiss cases for 50,000 Uganda shillings ($21). Human Rights Watch interviews with Abdul, Luzira Upper, November 8, 2010; Johnson, Bubukwanga Prison, November 16, 2010. Prosecutors could close files for 200,000 Uganda shillings ($100). Human Rights Watch interview with Saul, Masaka Ssaza Prison, November 22, 2010. Court personnel requested money for services that should have been free, such as the transfer of files. Human Rights Watch interview with Catherine, Jinja Women’s Prison, March 2, 2011.
[390] Martin Shönteich, “The Scale and Consequences of Pretrial Detention Around the World,” Justice Initiatives: Pretrial Detention, Spring 2008, http://www.soros.org/initiatives/justice/focus/criminal_justice/articles_publications/publications/pretrial_20080513/Justice_Initiati.pdf (accessed April 25, 2011).
[391] Human Rights Watch interview with commissioner, National Community Service Programme, March 21, 2011.
[392] Justice, Law, and Order Sector, “Annual Performance Report, 2009-2010.”
[393] Human Rights Watch interview with commissioner, National Community Service Programme, March 21, 2011.
[394] Human Rights Watch interview with Hassan, Masaka Ssaza, November 22, 2010; Thomas, Mutufu Prison, March 7, 2011.
[395] Human Rights Watch interview with Hassan, Masaka Ssaza, November 22, 2010.
[396] Human Rights Watch interview with executive director, Foundation for Human Rights Initiative, March 9, 2011.
[397] ICCPR, art. 14.
[398] Human Rights Watch interview with Gabriel, Jinja Main Prison, March 1, 2011; Humphrey, Jinja Main Prison, March 1, 2011.
[399] Human Rights Watch interview with paralegal, Kampala, November 19, 2010.
[400] Prison personnel were unwilling to corroborate their claims of age below 18, but Human Rights Watch observed that several of them looked very young.
[401] Convention on the Rights of the Child, art. 37(c); ICCPR, art. 10(2)(b); Constitution of Uganda, art. 34; Children Act, cap. 59, sec. 91(6).
[402] Foundation for Human Rights Initiative, “Juvenile Justice in Uganda,” September 16, 2009, http://www.fhri.or.ug/pr001.html (accessed April 15, 2011), p. viii.
[403] Ibid.
[404] One of the children interviewed by Human Rights Watch was given the opportunity to present evidence of her age via testimony of her brother, but the police rejected it as false. Human Rights Watch interview with Hellene, 16, Butuntumura Prison, November 11, 2010. All the other children said they told police, court, and prison authorities their age but were ignored or accused of lying. UPS is ostensibly supposed to ascertain that a person is not below 18 years on admission. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Uganda Prisons Service,” p. 8. However, conducting an age assessment requires particular protections for children. According to the UN Committee on the Rights of the Child, children should be informed about the purpose and the implications of an age assessment and be given effective representation by a guardian and lawyer. Such exams should not rely exclusively on physical appearances but should take into account psychological maturity, demeanor, ability to interact with adults, social and educational history, and life experiences. UN Committee on the Rights of the Child, General Comment No. 6, para. 31(i). Jacqueline Bhabha and Nadine Finch, “Seeking Asylum Alone: United Kingdom,” http://www.ilpa.org.uk/seeking%20asylum%20alone.pdf (accessed July 8, 2009), p. 61.
[405] Prisons Act of 2006, sec. 75.
[406] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. Prison authorities noted that “[s]ince the majority of prisoners (nearly 70%) are resident at the 63 units, it implies that only 30% of our prisoners are not having access to a prisons health services run facility as the primary point of contact for health care services.” Letter from prison authorities to Human Rights Watch, June 29, 2011.
[407] Human Rights Watch interviews with Byamukama, Masaka Ssaza, November 22, 2010; Peter, Masaka Main Prison, November 23, 2010; psychiatric nurse, Masaka Main Prison, November 23, 2010; UPS, “Work Plan and Budget,” p. 6.
[408] Human Rights Watch interview with Mary, Jinja Women’s Prison, March 2, 2011.
[409] Human Rights Watch interview with Tess, Masaka Ssaza Prison, November 22, 2010; Ross, Masafu Prison, March 8, 2011.
[410] Human Rights Watch interviews with Phillip, Muduuma Prison, November 12, 2010; Nathan, Muduuma Prison, November 12, 2010; William, Muinaina Farm Prison, March 4, 2011; Matthew, Masafu Prison, March 8, 2011; Walter, Mutufu Prison, March 7, 2011.
[411] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[412] Human Rights Watch interview with psychiatric nurse, Masaka Main Prison, November 23, 2010.
[413] Human Rights Watch interview with prison medical authority, UPS, March 11, 2001.
[414] Human Rights Watch interview with Esther, Fort Portal Women’s Prison, November 17, 2010.
[415] Human Rights Watch interviews with Adam, Masaka Main Prison, November 23, 2010; Joshua, Masaka Main Prison, November 23, 2010.
[416] Human Rights Watch interview with Peter, Masaka Main Prison, November 23, 2010.
[417] Human Rights Watch interview with OC, Masaka Main Prison, November 23, 2010. A medical officer at Masaka, however, claimed that the deceased prisoner had previously been at the outside hospital, but had been incompletely attended to and that his death happened “out of the blue.” Human Rights Watch interview with psychiatric nurse, Masaka Main Prison, November 23, 2010.
[418] Human Rights Watch interviews with Fred, Luzira Upper Prison, November 8, 2010; Kakooza, Masaka Main Prison, November 23, 2010; Kaahwa, Bubukwanga Prison, November 16, 2010; Benjamin, Masafu Prison, March 8, 2011.
[419] Human Rights Watch interviews with Juliana, Jinja Women’s Prison, March 2, 2011; Mary, Jinja Women’s Prison, March 2, 2011; Stella, Jinja Women’s Prison, March 2, 2011.
[420] Human Rights Watch interview with Ralph, Luzira Upper Prison, November 9, 2010.
[421] Human Rights Watch interview with Mafabi, Butuntumura Prison, November 11, 2010. Additional inmates at Butuntumura corroborated the death and that the prisoner had not received treatment. See Human Rights Watch interviews with Kakuru, Butuntumura Prison, November 11, 2010; Logan, Butuntumura Prison, November 11, 2010.
[422] Human Rights Watch interviews with Christopher, 17, Bubukwanga Prison, November 16, 2010; Brian, Murchison Bay Prison, November 13, 2010.
[423] Human Rights Watch interviews with Aaron, Luzira Upper Prison, November 8, 2010; Ralph, Luzira Upper Prison, November 9, 2010; Akello, Luzira Women’s Prison, November 10, 2010.
[424] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[425] Human Rights Watch interviews with Brian, Murchison Bay Prison, November 13, 2010 (two weeks); Samuel, Fort Portal Men’s Prison, November 15, 2010 (two weeks); Bradley, Muinaina Farm Prison, March 3, 2011 (two weeks); Tobias, Muinaina Farm Prison, March 4, 2011 (two weeks); Noah, Fort Portal Men’s Prison, November 15, 2010 (three weeks); Ali, Murchison Bay Prison, November 20, 2010 (one month); Asuman, Murchison Bay Prison, November 10, 2010 (one month); Alex, Murchison Bay Prison, November 10, 2010 (two months); Henry, Murchison Bay Prison, November 20, 2010 (three months); Owen, Kitalya Farm Prison, February 28, 2011 (six months); Gilbert, Kitalya Farm Prison, February 28, 2011 (six months); Edgar, Murchison Bay Prison, November 13, 2010 (six months).
[426] The Prisons Service recently acquired an ambulance for upcountry referrals to Murchison Bay, but more are required to avoid transfer delays. Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[427] The OC at Murchison Bay urged that at least a clinical officer be posted in each health unit to improve timely referrals. Human Rights Watch interview with OC, Murchison Bay Prison, November 10, 2010.
[428] Human Rights Watch interview with Alex, Murchison Bay Prison, November 10, 2010.
[429] Human Rights Watch interview with Brian, Murchison Bay Prison, November 13, 2010.
[430] Human Rights Watch interview with Asuman, Murchison Bay Prison, November 10, 2010.
[431] Human Rights Watch interview with Ali, Murchison Bay Prison, November 20, 2010.
[432] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010. See also Human Rights Watch interview with doctor, Murchison Bay Hospital, November 10, 2010.
[433] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[434] Human Rights Watch interview with deputy OC, Bubukwanga Prison, November 16, 2010.
[435] Human Rights Watch interview with psychiatric nurse, Masaka Main Prison, November 23, 2010.
[436] Human Rights Watch interview with OC, Muinaina Farm Prison, March 3, 2011; Human Rights Watch interview with OC, Jinja Women’s Prison, March 2, 2011.
[437] UPS, “Work Plan and Budget,” pp. 7-8; Human Rights Watch interview with prison medical authority, UPS, November 18, 2010; Letter to Human Rights Watch from prison authorities, June 29, 2011.
[438] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[439] Human Rights Watch interview with OC, Murchison Bay Prison, November 10, 2010.
[440] UPS, “Work Plan and Budget,” p. 14. Prison authorities report that in 2008, only 26 percent of health care posts were filled, and in FY2010/11 this number had increased to 51 percent. Letter from prison authorities to Human Rights Watch, June 29, 2011.
[441] In November 2010, 222 of 436 (51 percent) of health posts established by UPS were filled with professional health workers. In some regions, however, this number fell far lower; in the northeastern region only six percent of established posts had been filled. Human Rights Watch interview with prison medical authority, UPS, November 18, 2010. Uganda’s Auditor General has concluded that “[t]he staffing level in the Health Services Division is too low to deliver adequate medical services in all prisons.” The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 35.
[442] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010.
[443] Human Rights Watch interviews with Sebastian, Luzira Upper Prison, November 8, 2010; Brian, Murchison Bay Prison, November 13, 2010; Evan, Masaka Main Prison, November 23, 2010.
[444] Human Rights Watch interview with Ali, Murchison Bay Prison, November 20, 2010.
[445] Human Rights Watch interviews with Fred, Luzira Upper Prison, November 8, 2010; Brian, Murchison Bay Prison, November 13, 2010; Daudi, Murchison Bay Prison, November 20, 2010; Donald, Masaka Main Prison, November 23, 2010; Mukasa, Luzira Upper Prison, November 9, 2010.
[446] Human Rights Watch interviews with Jonathan, Masaka Ssaza Prison, November 22, 2010; Edgar, Murchison Bay Prison, November 13, 2010; Henry, Murchison Bay Prison, November 20, 2010; Donald, Masaka Main Prison, November 23, 2010.
[447] Human Rights Watch interview with Yusuf, Murchison Bay Prison, November 13, 2010.
[448] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. Prison authorities confirmed in June 2011 that “[s]everal prison health units continue to experience stock out of essential medicines and health supplies.” Letter from prison authorities to Human Rights Watch, June 29, 2011.
[449] Human Rights Watch interview with prison medical authority, UPS, November 18, 2010; UPS, “Work Plan and Budget,” pp. 6-7.
[450] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011.
[451] The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 23.
[452] Not all patients referred from Murchison Bay to Mulago Hospital are actually taken because of limited transportation and human resources for the transfer. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report on Uganda Prisons Service,” p. 21.
[453]Human Rights Watch interviews with doctor, Murchison Bay Hospital, November 10, 2010; OC, Murchison Bay Prison, November 10, 2010.
[454] Human Rights Watch interviews with Ralph, Luzira Upper Prison, November 9, 2010; Asuman, Murchison Bay Prison, November 10, 2010; Mafabi, Butuntumura Prison, November 11, 2010; Alex, Murchison Bay Prison, November 10, 2010.
[455] Human Rights Watch interview with OC, Murchison Bay Prison, November 10, 2010.
[456] OECD, “Creditor Reporting System,” undated, http://stats.oecd.org/Index.aspx?DatasetCode=CRSNEW (accessed April 13, 2011).
[457]The United States President’s Emergency Plan for AIDS Relief, “Uganda: FY 2010 Approved Funding by Program Area, Agency, and Funding Source,” undated, http://www.pepfar.gov/about/2010/africa/150628.htm (accessed April 13, 2011).
[458] Eric Goosby, “PEPFAR Programs in Uganda: An Update,” July 13, 2010, http://blogs.state.gov/index.php/site/entry/update_pepfar_uganda (accessed April 13, 2011).
[459]Ibid.
[460] UNAIDS, “Report on the Global AIDS Epidemic: Annex 2: Country Progress Indicators 2004 to 2010,” 2010, http://www.unaids.org/documents/20101123_GlobalReport_Annexes2_em.pdf (accessed May 5, 2011), p. 238.
[461] In that final year, the amount of donor funding to the UPS was less than half the amount of the “internally generated” revenue from prisoners’ forced labor. The exception was FY 2006/07. The Republic of Uganda Office of the Auditor General, “Value for Money Audit Report of Uganda Prisons Service,” p. 4.
[462] Uganda AIDS Commission, “National HIV & AIDS Strategic Plan 2007/8-2011/12: Moving Toward Universal Access,” undated, http://www.aidsuganda.org/Publications/nsp.pdf (accessed April 13, 2011).
[463] “Uganda: Overcrowded Prisons Heighten TB Risk,” IRIN PlusNews, July 4, 2008, http://www.plusnews.org/report.aspx?ReportId=79104 (accessed April 13, 2011); Andante Okanya and Abou Kisige, AIDS Rocks Local Prisons,” The New Vision, October 1, 2009, http://allafrica.com/stories/200907300248.html (accessed April 11, 2011).
[464] The ICRC, AIDS Information Centre, Northern Uganda Malaria HIV/AIDS and TB Program, the African Prisons Project, U.S. CDC, USAID/SPEAR, National TB Control Assistance Programme, UNODC, and the National Franciscan Prison Ministry are all health partners. UPS, “Work Plan and Budget,” pp. 8-9. There is also an objective for TB in prisons in Uganda Global Fund Round 10. Human Rights Watch interview with director, National TB and Leprosy Programme, March 10, 2011.
[465]Human Rights Watch interview with OC, Fort Portal Prison, November 15, 2010; UPS, “Work Plan and Budget,” pp. 8-9.
[466] Human Rights Watch interview with prison medical authority, UPS, March 11, 2011. The first phase of the project, which is a collaboration under PEPFAR between the CDC, USAID and UPS, will focus on assessing HIV, TB, STI, and malaria epidemiology and service provision, in order to inform the development and implementation of prevention, care and treatment services for staff and prisoners. Ibid.
[467]Ibid.
[468] Ibid.