No Healing Here
Violence, Discrimination and Barriers to Health for Migrants in
South Africa
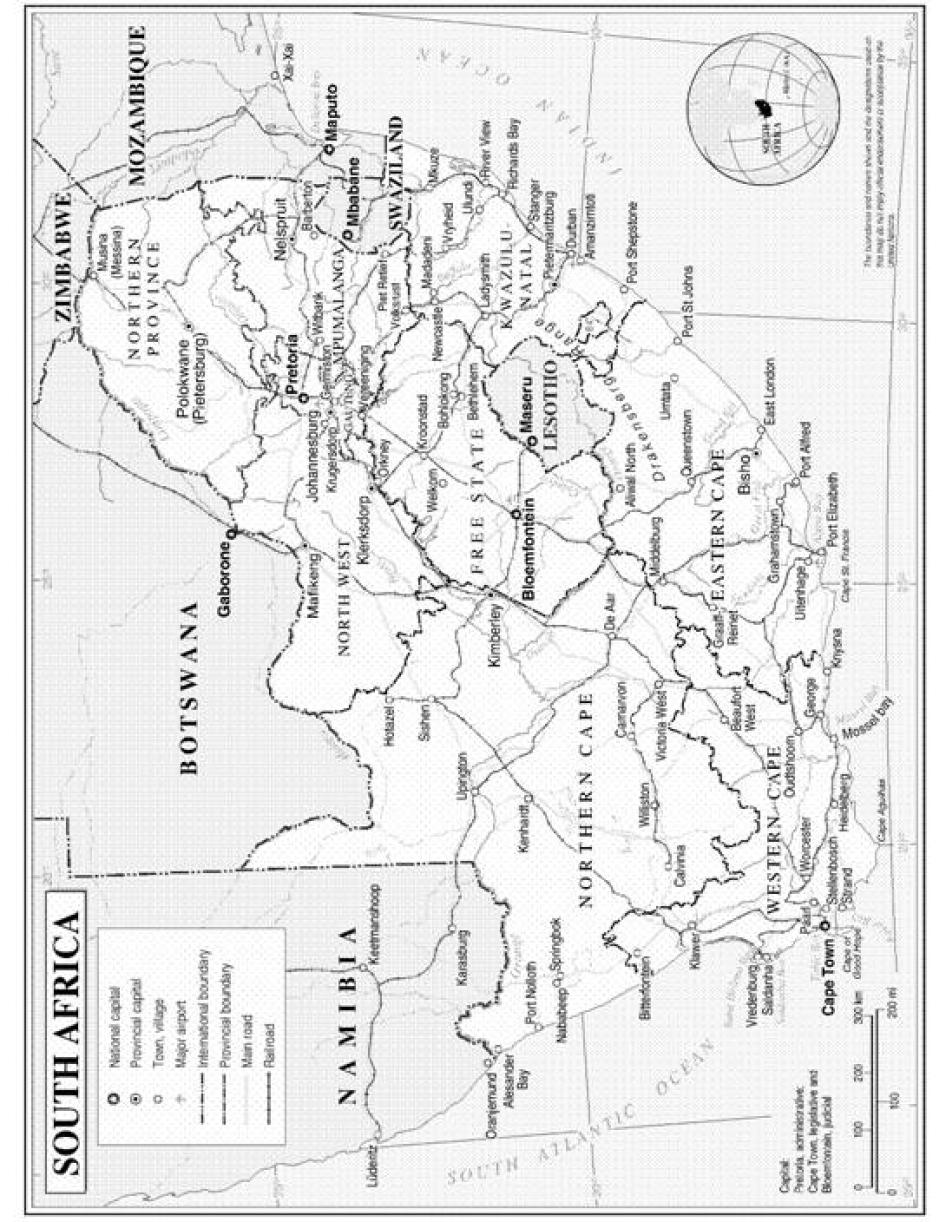
Map of South Africa
©2007 United Nations Department of Peacekeeping Operations.
Executive Summary
“There is no healing here in South Africa. Since I arrived here there is no rest, no recovery.”
— Ndona, Congolese refugee, Johannesburg
Ndona speaks for the many thousands of migrants in South Africa who were made homeless by xenophobic attacks in 2008, forced to take shelter in unsafe and unsanitary camps, abandoned buildings, churches, and on open ground, where they are vulnerable to disease and further violence. Refugees like Ndona fleeing war in places like the Democratic Republic of the Congo (DRC) and Somalia and economic and political crises in places like Zimbabwe, have found themselves without the most basic human rights fundamental to life: food, shelter, physical security, and access to basic health care. As shocking as the severity of the xenophobic violence is the fact that such widespread abuses are tolerated in South Africa, a country with some of the most expansive rights in the world for refugees and other migrants. The widespread violence and displacement leading to homelessness and unsafe living conditions, along with systemic government failures to protect migrants from arrest and deportation, has created a massive health crisis for migrants—and their hosts—in South Africa. Xenophobia, violence, and discrimination create both environments that promote risks to migrants’ health as well as barriers to obtaining basic health care.
South Africa's Constitution provides for the right to health for “everyone” within the country. In recent years, this provision has been tested as regional crises created unprecedented numbers of asylum seekers and undocumented migrants entering there. Since 2007 the Department of Health (DOH) has repeatedly affirmed the rights of asylum seekers and refugees to access the same public health care to which citizens have access. However during this same period, documented and undocumented migrants alike have been denied access to health care. Even when seeking emergency care after xenophobic attacks or rapes, migrants are often turned away by medical personnel who may discharge them prematurely, harass them, charge them excessive user fees, and call the police to deport them.
But the risks to health and barriers to care that migrants experience in South Africa are not the responsibility of the DOH alone. The South African asylum system has failed for years to provide protection to asylum seekers and recognized refugees due to systematic problems. Restrictive immigration provisions leave many labor migrants, long an important part of South Africa's economy, undocumented and unprotected from deportation, discrimination and ill treatment. Up to a million undocumented Zimbabweans may be eligible for asylum or for a still-unimplemented special dispensation program, but remain without protection and documentation that would facilitate their access to health care. The perpetrators of xenophobic violence have gone largely unpunished. Wherever asylum seekers, refugees, and undocumented migrants gather to find shelter in South Africa–in the remnants of closed camps, outside of government offices in cities and near the border, in abandoned garages and in the sanctuary of churches–they are subject to health-threatening conditions, eviction, and arrest. These abuses work against the aims of the inclusive right to health professed by the South African Constitution.
Meanwhile, the collapse of the public health system in Zimbabwe has created a regional health crisis that requires ongoing regional humanitarian coordination. Communicable diseases like HIV/AIDS and tuberculosis are prevalent within South Africa and throughout southern Africa, with relatively low rates of treatment success and relatively high rates of drug resistance. In one example of the inevitability of cross-border health crises, in 2008 Zimbabwe experienced a serious cholera epidemic that eventually affected South Africa, which suffered more than 12,000 infections and more than 60 deaths. Cross-border migrants, particularly those travelling informally without documents, face conditions that increase their susceptibility to infection and decrease their ability to access or adhere to treatment. Despite the risk they face, and the risks that communicable disease poses to the entire community, South Africa has largely failed to design public health initiatives that reach vulnerable mobile and migrant populations. Removing barriers to care, conducting active outreach to at-risk migrant communities, and coordinating with civil society and affected communities, are necessary components of South Africa’s campaign to achieve more universal access for HIV and TB treatment. South Africa cannot achieve positive health outcomes for its own citizens while neglecting those of vulnerable migrant communities.
Migrants to South Africa come for varied and complex reasons. This report deals primarily with three groups: asylum seekers, refugees, and undocumented migrants. Asylum seekers are migrants who claim to have been forced to flee their home country because they have a well-founded fear of being persecuted on account of their “race, religion, nationality, membership of a particular social group or political opinion” as defined by the 1951 UN Refugee Convention. Those who express such a fear are protected under international law from deportation to their home countries (refoulement) pending the resolution of their asylum claims. If an asylum seeker’s claim is proved to the satisfaction of the Department of Home Affairs (DHA), the asylum seeker is recognized as a refugee, a status that carries many of the same rights as permanent residency and citizenship.
Any migrant who enters the country without a visa could be termed an “undocumented migrant,” but in this report the term refers to those (largely Zimbabwean) undocumented migrants to South Africa who do not lodge asylum claims. The term is used to allow for the complex nature of recent migration from Zimbabwe, and the possibility that at least some undocumented migrants should be, or shortly will be, protected by either the asylum system or the special dispensation permit.
In its November 2005 report, “Living on the Margins: Inadequate Protection for Refugees and Asylum Seekers in Johannesburg,” Human Rights Watch reported on the systemic inadequacies in the Department of Home Affairs' (DHA) registration and status determination systems that have left many asylum seekers without documentation, and many legitimate asylum claims unrecognized. The asylum system has been stretched past its capacity by the sharp influx of asylum seekers from Zimbabwe fleeing political oppression, violence, economic collapse, and breakdown in public health, sanitation, and other services. Despite the extraordinary nature of the political crisis in Zimbabwe, the severity of the deprivation there and the long-documented persecution experienced by many of its émigrés, South Africa has recognized only a small minority of Zimbabwean asylum claims approximately 20 percent through 2007. Asylum seekers from all countries continue to be left to navigate a byzantine bureaucracy to gain recognition as refugees, languishing for months and years without resolution and subject to detention and deportation as well as discrimination.
In addition to widespread violence, migrants are also especially vulnerable to communicable disease because of substandard living environments, limited sanitation, and cultural and social dislocation, making them vital targets for public health surveillance and intervention. According to Department of Health policies, everyone in South Africa should have access to treatment for communicable disease without cost. Any barrier to prevention and treatment of communicable disease for vulnerable mobile and migrant populations is unwise from a public health perspective, but also a violation of South African and international law. South Africa has recognized the importance of access to health care for vulnerable and migrant populations in its laws and policy documents, yet continues to allow unlawful discrimination by health care staff, undermining efforts to contain disease and improve treatment outcomes.
In over 100 interviews with migrants, advocates, health care and other service providers in both urban and border communities, Human Rights Watch found that South Africa’s failure to protect asylum seekers and refugees from deportation and violence leads both to increased disease and injury, and increased barriers to treatment for those conditions.
Human Rights Watch documented two broad sets of abuses affecting migrants’ health in South Africa:
- abuses leading to health vulnerability, and
- barriers to access to health care.
Human Rights Watch’s researchers found asylum seekers, refugees and undocumented migrants living in harrowing and life-threatening conditions, constantly under threat of assault, rape, disease, and discrimination. Unable to find secure accommodation, migrants were often displaced from one dangerous informal shelter to another, facing harassment and attacks by their neighbors, evictions by local governments, and police raids. Refugees and asylum seekers, even those who were documented, told Human Rights Watch that in many cases when they seek health care, clinics and hospitals either refuse to treat them, terminate their care prematurely, charge them excessive fees, or verbally harass and mistreat them for being foreign. This amounts to a failure by the South African state to protect the basic rights and safety of migrants. South Africa’s failure to ensure that migrants have access to the health care services to which they are entitled compounds their medical conditions. When discrimination or other factors impede care, migrant patients tend to be diagnosed later and only treated well into the development of illness; and when they are sicker, care is more expensive and treatment tends to be less effective.
South African citizens reliant on the public health system may experience similar health vulnerabilities and access problems to those described here. Certainly, many South Africans also face resource and capacity constraints in public sector care, long wait times, abusive attitudes by staff, poor living conditions, and vulnerability to violence. However, the evidence shows that migrants, including refugees and asylum seekers, experience specific abuses in addition to the systemic failures that affect all patients, compounding the vulnerability they already face. They are actively discriminated against and they are targets of violence specifically and exclusively because they are non-nationals. Furthermore, South Africa’s failures to detect and treat illness and prevent injury in vulnerable populations carry costs of their own. Illness advances, spreads, becomes resistant to first line drugs, and becomes costlier to treat, and short and long-term disabilities create economic dependency in migrants who would otherwise be independent and productive. For a health system that struggles to meet the needs even of its own citizens, the consequences of failing to adequately treat migrants, both to the public health and to the cohesiveness of a multiethnic South African society strained by xenophobia, cannot be ignored.
Abuses Leading to Health Vulnerability
Violence
Even in the context of a high crime rate in South Africa, migrants are particular targets for violence. The xenophobic attacks of 2008 were the most dramatic, but not the only acts of xenophobic violence, which continue to occur frequently all over the country. Non-citizens are also targets for opportunistic crimes like robbery; a migrant advocate told Human Rights Watch that foreigners are sometimes called “ATMs” because “it is so easy to get cash out of them.” Undocumented migrants crossing the Zimbabwean border are targeted for attacks by bandits called magumaguma, who rob and assault vulnerable border crossers, sometimes in league with corrupt malayshas (border guides).
South Africa suffers very high levels of rape and other sexual violence, and migrant women are at intense risk throughout their journey and their residence there, especially those living in unsafe, informal group shelters. Female cross-border traders, vendors, asylum seekers and other migrants are subject to rape by truck drivers offering rides, by fellow travelers, by malayshas paid to bring them across the border, or by magumaguma. Every recently arrived female migrant who spoke to Human Rights Watch, reported being raped, witnessing rape, or fearing rape, and few felt safe enough to report their crimes or to seek health care.
Living Conditions
South Africa does not confine refugees and asylum seekers to camps, a generally progressive policy embraced by most refugee advocates because of the abuses, lack of free movement and inability to pursue livelihoods often associated with refugee camps. The policy requires refugees to locally integrate into South African communities; however many asylum seekers, refugees, and undocumented migrants in South Africa are left homeless, or living in conditions that threaten their health and safety. Non-citizens are excluded from government-subsidized housing, and no formal shelters for asylum seekers or other migrants exist.
Left completely without shelter and at risk of deportation, recently arrived asylum seekers in Musina on the Zimbabwe-South Africa border were in 2008 forced to stay in a fenced in open ground, called “the showgrounds,” rented by the DHA to register asylum seekers. Because of the backlog in registering cases, thousands of undocumented asylum seekers were forced to sleep outside the DHA office, risking arrest and deportation if they left the grounds, and occasional eviction of those within it. For days or even weeks, asylum seekers were confined and exposed to the elements, with limited access to water and sanitation, conditions which facilitated the spread of cholera and other communicable disease. Human Rights Watch also interviewed both documented and undocumented asylum seekers sleeping for months at a time on a rocky hill in the bush outside Musina, vulnerable to weather, illness, and criminal attacks, and unable to raise enough money to move on to safer ground.
Migrants who are able to move on and settle in urban areas live in cramped and poorly ventilated conditions. Refugees displaced in the xenophobic violence told Human Rights Watch how they were pushed out of the affordable townships where they lived, and forced into more expensive neighborhoods they hope will be safer. However, the higher rents in the new neighborhoods necessitate more roommates, heightening the risk of disease and conflict. Other migrants, unable to pay rent, spend nights in informal shelters like the Central Methodist Mission Church in downtown Johannesburg, in an abandoned tire garage in Pretoria, or in a borrowed room in a community center in Cape Town. These shelters are overwhelmingly provided by volunteers and small, local community organizations, with little or no cooperation with, or support from, local government. In fact, the Methodist Church has been threatened with eviction actions by local government and neighboring businesses for allowing between one and three thousand Zimbabweans to take shelter in and around its floors each night. Police have raided it twice in the last two years, and hundreds of homeless asylum seekers were arrested and threatened with deportation. Wherever they take shelter, migrants in South Africa frequently live in hazardous conditions, vulnerable to illness, violence, arrest, eviction, food insecurity, and lack of basic services.
Barriers to Accessing Healthcare
As a result of the violence and dangerous living conditions they suffered, many of the migrants Human Rights Watch interviewed reported seeking basic health care, but were unable to access it. Human Rights Watch documented four major barriers to migrant access to health care: discrimination; inadequate, inaccurate and misleading information; barriers to emergency care for rape survivors; and extralegal user fees.
Discrimination
The most serious barrier to health care access for asylum seekers, refugees and undocumented migrants is discrimination by individual health care providers. Documented and undocumented asylum seekers alike told Human Rights Watch of being refused care even for basic and emergency treatment, including patients with acute tuberculosis and women in labor, because they lacked South African identity documents or simply for being foreign. Turned away from the clinic or hospital nearest to them, some migrants are forced to find care in the non-profit or charity sector; others go without treatment at all or visit multiple public facilities hoping to find better access. Repeated unsuccessful attempts at accessing health care result in late diagnosis and treatment and poorer overall health in migrant communities. Human Rights Watch interviewed women with high risk pregnancies, children with diabetes, and young men with acute TB whose conditions worsened because health care was so difficult to access.
The health rights afforded to migrants on paper are belied by the harassment and denial they face in hospitals and clinics, while their ability to survive and remain in good health is undermined by violence, displacement, and threat of deportation. It is not only the lives and livelihoods of migrants who suffer the consequences of these abuses. The regional nature of communicable disease epidemics makes it in the interests of everyone in South Africa and the southern Africa region to increase health surveillance, screening, testing, and treatment among mobile and migrant communities, and to develop treatment mechanisms that address the unique vulnerabilities of people on the move.
Maintaining health and ability are also vital to the livelihoods of migrants, many of whom bring valuable skills and resources to South African communities. Restricting the ability of migrants to work, find stable housing, and build livelihoods, whether through rights violations or through illness, injury and disability, only makes the migrant and refugee community more likely to be dependent on the state and on humanitarian aid to survive. All sectors of government should coordinate on policy toward non-nationals, so that the goals of one are not canceled out by the actions of another. National, provincial and local municipalities should each individually and together assume responsibility for protecting migrants' rights, including the right to health. South Africa’s obligations to implement the right to health for both citizens and non-citizens within its borders present serious challenges in resources, administration, and service delivery that will require collaboration and planning in multiple sectors of government. Though South Africa may fear that it cannot afford to meet the health needs of everyone in its borders, in reality it cannot afford not to.
Inadequate and Inaccurate Information
Although the DOH has affirmed the rights of asylum seekers and refugees to obtain basic health care and antiretroviral treatment (ART), it has done almost nothing to implement that right. It has initiated no reporting, accountability, or enforcement activities by health care facilities to ensure implementation of the policy; nor has it conducted even basic outreach and educational initiatives to inform migrants of their right to health. Migrants lack knowledge of the health risks they face, the services available, and the scope of their right to obtain them. Many rely on the intervention of advocates just to obtain access to emergency care. Because health care facilities don't provide interpreters, migrants, such as Somali or Francophone refugees from the Great Lakes region, have an even harder time. South Africa's failure to disseminate health and rights information to migrant communities leads to failure to access treatment, late diagnosis and treatment, and in turn to increased morbidity and mortality in migrant patients.
At the same time, the DOH has failed to fully inform health care providers about the policy of treatment access for asylum seekers, refugees and undocumented migrants. It has not provided training or guidance on the interpretation of common forms of non-citizen identification or the fee schedule used for migrant patients, nor made any attempt to systematically collect health surveillance information on migrant and mobile populations to anticipate and provide for their health needs. Greater transparency is also needed with regard to the DOH's planning and budgeting processes, which has been criticized by the South African Human Rights Commission for opacity, lack of participation from affected communities and stakeholders, and lack of responsiveness to health needs on the ground.
Barriers to Emergency Care for Rape Survivors
Language barriers and lack of information make meaningful counseling and consent (for example for HIV diagnosis, or provision of post-exposure prophylaxis (PEP)) all but impossible. Rape survivors, who frequently lack knowledge of the services available to them and often fear deportation, face barriers in accessing lifesaving post-rape emergency medical care, including emergency contraception and (PEP) within the 72 hour window in which treatment is available after an assault. Some health care facilities erroneously require survivors to report the rape to the police before medical treatment is given. For undocumented asylum seekers and other migrants who fear deportation, such a requirement is frequently prohibitive.
Extra-Legal User Fees
The DOH has a complicated system of user fees in the public health system, including various subsidies, which vary from 20 to 100 percent of the total cost of health care depending on the type of care and the income level of the patient. Documented and undocumented asylum seekers, refugees, and other documented migrants are eligible for partial subsidies for basic health care, and may access ART and prenatal care for free. Undocumented migrants from southern Africa should have access to emergency care and treatment of communicable disease without charge, and should be assessed according to the subsidized fee schedule for other kinds of care. However, reception staff at clinics and hospitals regularly charges asylum seekers, refugees and migrants excessive fees in contravention of established DOH policy, frequently resulting in a failure to access essential treatment.
Key Recommendations
South African law and Department of Health policy already establishes the right to health for asylum seekers and refugees on a level comparable to that of citizens. But multiple government departments must act urgently to ensure that these rights are realized, and that migrants are not subjected to abuses that put their health, and the health and survival of South Africans, at greater risk. There are several important steps that both national and provincial governments must take:
- Conduct research into the volume and nature of international migration, including undocumented migration, and into the health status and needs of mobile and migrant populations so that budgets can be planned based on reliable data.
- Develop targeted programs aimed at the health needs of migrants, including cross border and regional antiretroviral and tuberculosis treatment initiatives in partnership with domestic and international organizations.
- Improve training, reporting and accountability for the enforcement of policy toward non-citizens at the level of individual facilities as well as on a provincial and national level, for example by requiring all incidences of treatment denials and referrals be documented and signed by the worker making the decision.
- Improve access to information in migrant communities about their health rights and grievance processes available, for example by posting a list of patients’ rights, including migrants’ rights, prominently near the front desk at each facility, including contact information and instructions to report grievances, in languages common to migrant communities.
- Implement the special dispensation permit for Zimbabweans announced on April 3, 2009, and ensure that asylum seekers, refugees and Zimbabwean migrants are not subject to arbitrary or extra-legal arrest and deportation.
- Collaborate with civil society and local governments to develop transitional and long term housing options for homeless asylum seekers and refugees.
- Amend the Criminal Law (Sexual Offences and Related Matters) Amendment Act or 2007 to remove section 28 (2) which requires that a rape be reported before PEP services can be provided.
- Protect migrants from opportunistic criminal violence near the Zimbabwean border and from xenophobic violence throughout South Africa.
Methodology
This report is based on research conducted by Human Rights Watch in Johannesburg, Musina, Pretoria, and surrounding municipalities, and Cape Town over five weeks between October and November 2008, and again in Musina and Johannesburg for two weeks in March-April 2009. Human Rights Watch conducted over 100 interviews, including over 75 interviews with refugees, asylum seekers, and undocumented migrants and over 30 with service providers and activists, researchers, lawyers, government workers, and to a limited extent, officials at health facilities and departments. Telephone interviews and emails were conducted with some informants with whom Human Rights Watch could not meet in person, or to update information obtained in the field. Efforts were made to interview refugees, asylum seekers, and migrants of multiple ages, genders, and nationalities. The majority of the migrant subjects were documented and undocumented asylum seekers and refugees; a smaller number were Zimbabwean undocumented migrants who did not identify as asylum seekers and undocumented children.
Interviewees ranged in age from nine years old to approximately seventy years old. Women and men were interviewed. They were guaranteed anonymity and in most cases migrant interviewees chose to use a pseudonym. Migrants from a range of African countries including Zimbabwe, Somalia, Democratic Republic of Congo, Ethiopia, Rwanda, Uganda, and Burundi were represented, with the majority being Zimbabwean. In some cases interpreters were used.
Local service providers arranged a minority of interviews for Human Rights Watch; more frequently Human Rights Watch conducted site visits to camps, shelters, and other areas where asylum seekers and refugees are known to gather or reside and conducted interviews there. These included but were not limited to: Akasia Camp in Tshwane (Pretoria), Malas Camp in Pretoria, Central Methodist Mission Church in Johannesburg, the “Showgrounds” in Musina, I Believe in Jesus Church in Musina, Dutch Reformed Church in Musina, Roman Catholic Church in Musina, and Bluewaters Camps A and B in Strandfontein (Cape Town).
Human Rights Watch also reviewed research and reports by national and international health, human rights, and migration organizations, as well as government policies and statistics, and other public sources with information regarding health care access and migration in South Africa.
Access to DOH officials and even government public health system staff was very limited. Human Rights Watch was instructed to obtain written permission from the CEO of each hospital where interviews would take place, and to the Minister of Health for each Province where interviews with DOH staff were desired. In the cases of some government officials and hospital administrators, unfilled vacancies meant that no one on staff was senior enough to provide Human Rights Watch with permission to interview staff. Requests were made in person, on the phone and in writing to provincial and national DOH and CEOs of health care facilities for Human Rights Watch to conduct interviews with health care staff or government administration. With the exception of a brief phone interview with the Public Information Officer of Limpopo Province and an interview with the Public Information Officer of Musina Hospital, none of these requests received a response, despite Human Rights Watch ensuring receipt of the request and placing follow up calls and emails. Written questions were also submitted to the Director General of the Department of Health through the auspices of the Health Attaché of the South African Embassy in Washington, DC, with no response to date, as of this writing.
Background
Migrants in South Africa
South Africa is home to a large, growing and diverse population of migrants who come to South Africa for many reasons. Migration of laborers from neighboring countries to the agricultural and mining sectors dates back to at least the mid 19th century, in both regulated and unregulated forms. The most recent estimates of legally present, foreign-born people in South Africa indicated that approximately one million foreign migrants lived in South Africa, making up 2.3 percent of the total South African population in 2001.[1] Data from that period also suggests that up to 38 percent of all mine workers in South Africa are foreign born.[2] In 2007-2008, 3,817 permanent residence permits, 32,344 work permits, and 13,005 study permits were authorized.[3]
However, the number of undocumented migrants is much higher.[4] An uncounted number of informal cross -border migrants travel to South Africa. Some may travel for short periods of time to buy and sell goods, visit family, or to perform informal labor, while others, seeking greater economic opportunity, fleeing intolerable conditions in their home countries, intend to stay indefinitely. The majority of migrants do not have the means and access to obtain visas and passports and must enter and remain illegally in South Africa. Under South African immigration law, undocumented migrants are deemed to be “illegal foreigners” and can be arrested and deported at any time.[5]
In addition to cross-border workers and traders, South Africa, during 2008, hosted 256,000 asylum seekers and refugees, including 115,800 Zimbabweans, 33,000 Congolese (from the Democratic Republic of Congo), 27,000 Somalis, 11,000 Ethiopians, and about 15,000 from Bangladesh, Pakistan, and India, of whom 37,000 were recognized refugees.
Zimbabweans
The economic implosion and political oppression in Zimbabwe in recent years has created a large Zimbabwean diaspora of migrants fleeing economic deprivation and political oppression. Whereas traditional Zimbabwean migration patterns tended to be formal (regulated by work contracts and including visas), and circular (repeated border crossings and returns to Zimbabwe), because of recent crises in Zimbabwe, larger numbers of Zimbabweans are now remaining in South Africa without documents, or seeking protection through asylum. By the beginning of 2008 there were probably between one and 1.5 million Zimbabweans in South Africa,[6] most of whom remained in South Africa without visas or documentation of any kind. At the same time, the vast majority of new asylum claims have been from Zimbabweans. In 2008 around 115,800 Zimbabweans applied for asylum, including 25,000 to 30,000 Zimbabweans in the border town of Musina in the last half of the year alone.[7] Current estimates suggest that up to 1.5 million Zimbabweans may be in South Africa, but the number of undocumented among them is not known.[8]
Of those Zimbabweans who have applied for asylum, only 1.5 percent were approved for refugee status in 2006 and 2007.[9] The South African government has portrayed undocumented Zimbabwean migrants, and many formal asylum seekers, as ordinary economic migrants, without valid claims to international protection. Moreover, as Human Rights Watch has documented, South Africa's dysfunctional asylum system fails to adequately examine many applications and unjustly rejects many asylum seekers with legitimate refugee claims.[10] Many Zimbabweans, both undocumented migrants and documented asylum seekers, are fleeing persecution, including rampant political violence and routine arbitrary arrests and detention of political opponents of the then ruling Zimbabwe African National Union-Patriotic Front (ZANU-PF).[11] Others are forced to migrate because inflation has made their salaries worth so little that they cannot provide basic needs for their families, or because the breakdown in public sanitation and health systems has put even basic health care out of reach.
In apparent recognition of the humanitarian and legal needs of the vast majority of Zimbabweans who do not obtain international protection, and in a welcome move, outgoing Home Affairs Minister Nosiviwe Mapisa-Nqakula announced in April 2009 that Zimbabwean migrants would be eligible for a special dispensation permit allowing them to stay legally in South Africa for six months.[12] This announcement was accompanied by the implementation of a free 90 -day visa waiver for Zimbabweans (who have passports) and a moratorium on most deportations of Zimbabweans. However, as of November 2009 the special dispensation permit had not been implemented. Until the dispensation is implemented and protection extended to those without the resources for travel documents, the vast majority of Zimbabweans in South Africa remain undocumented.
Rights of asylum seekers and refugees
Under South African law, immigration officials have the right to arrest, detain, and deport migrants without valid permits as “illegal foreigners.”[13] But no one who has expressed a wish to apply for asylum or who has already applied for asylum can be designated as an “illegal foreigner.” The law guarantees that all individuals expressing a wish to apply for asylum the right to be given time to gain access to one of the six Refugee Reception Offices.[14] It also explicitly protects those who have already applied for asylum from initiation of deportation proceedings.[15]
The Refugees Act requires asylum seekers to report their entry and desire to seek asylum to officials upon entry into South Africa at a border post, or alternatively after apprehension by law enforcement. In turn, the government must assist them in obtaining a travel permit, called a section 23 permit, that gives them (usually) 14 days of legal presence, in which they are to lodge an asylum claim at one of the six RROs, at which time they are to be given a section 22 or asylum seeker permit until a decision is reached on their case.[16] However in practice, most asylum seekers are not readily able to access the documents that prove their legal status in South Africa.
Most asylum seekers enter South Africa without documentation, primarily over the Zimbabwean border.[17] Few declare their wish to seek asylum to DHA officials as they are required to, either out of ignorance of the law or fear of law enforcement officials on both sides of the border.[18] As soon as the South African authorities are made aware that the individual in their charge wants to seek asylum or fears persecution upon return home, DHA must give the asylum seeker a transit permit; straight deportation in such cases is illegal.[19]
Despite these regulations, South Africa regularly deports both documented and undocumented asylum seekers.[20] South Africa has rapidly increased deportations in recent years, reporting an increase of 18 percent over the past five years, with a projected increase from 312,000 in 2007 to 370,000 for 2008.[21] The moratorium on deportations of Zimbabweans since April 2009 is likely to result in a leveling or lessening of deportation, but some abusive practices remain.[22] Human rights advocates working in Musina, near the Zimbabwean border, have reported that, since the moratorium on deportations has been announced, the South African Police Service (SAPS) has begun to detain undocumented migrants overnight at Soutpansberg military grounds (SMG) Detention Center overnight until DHA can assess them.[23] This practice is particularly problematic since the North Gauteng High Court issued a ruling in May 2009 that SMG be closed as a migrant detention facility because it is managed entirely by SAPS and is not designated as a place of detention by the Director General of Home Affairs as required under the South African Immigration Act, and because of abysmal and unsafe conditions of detention.[24]
The danger of arrest, detention and fear of deportation facing those traveling while undocumented is self-evident. Yet asylum seekers with or without a Sec. 23 transit permit must travel to one of the six Refugee Reception Offices (RRO) to obtain the section 22 asylum seeker permit that protects them from deportation and secures their rights to work, study and confirms their right to seek basic health care. Because of backlogs and long waits at RROs, only 41 percent of asylum seekers (19 percent of Zimbabweans) who do get a transit permit are able to obtain a Sec. 22 asylum seeker permit before their transit permit runs out, so that even the relatively small number of asylum seekers who complete the process as proscribed by law are still likely to be undocumented at some point despite actual legal status.[25] After the Sec. 23 permit expires and until Sec. 22 document is obtained, asylum seekers are more vulnerable to abuses, and cannot readily establish their legal status for the purposes of seeking health care.[26]
Human Rights Watch and South African human rights monitoring groups have extensively documented the barriers asylum seekers face in gaining documentation at RROs. Asylum seekers often wait in queues with hundreds or even thousands[27] of other asylum seekers, frequently overnight or over several days or weeks before successfully obtaining legal documentation. The average asylum applicant will have to return to the RRO approximately 3 times, and wait approximately 22 days between first arriving at the office and first entering the office.[28]
During Human Rights Watch's site visit to the Musina RRO in November 2008, DHA had run out of ink and was unable to print permits for several days, increasing the backlog and making for longer waiting times. Asylum seeker Hassan's experience was typical:
I've been here for two weeks. Two weeks without leaving this pen [referring to the fenced-in showgrounds]. Every day I am just waiting for my chance to come. Every day they take somebody else–just Ethiopians today, just women today. It's always tomorrow, tomorrow. If you can pay them something, maybe they will see you today. Those with asylum papers can go and work, but I have to stay here until that time. The problem is that you run out of money while you are waiting, and surviving becomes tough. [29]
Nationally, the evidence shows that only 35 percent of asylum seekers are able to gain access to an RRO on their first visit, and nearly half were unable to gain documentation on the first try even once gaining access to the office.[30]
Even after successfully obtaining a permit, an asylum seeker can wait sometimes for years before having a status interview to become recognized as a refugee. A Congolese asylum seeker in Johannesburg told Human Rights Watch,
I applied for asylum in 2007, but I am still waiting for an interview. They keep extending my asylum seeker permit, and each time I must travel to Pretoria and stay waiting from 6 am until 4 pm. It's difficult because I use crutches. If it looks like I am not going to get it in time, I panic.[31]
These wait times are unfortunately typical for asylum seekers in South Africa, where the DHA has come under criticism for years for its backlog of unadjudicated cases. Human Rights Watch has reported over 100,000 unresolved asylum cases from 2008 alone,[32]on top of a pre-existing backlog of 100,000.[33] The average asylum seeker in South Africa will not yet have had a status interview even after a year and three months of waiting.[34]
Once an asylum seeker gets a status interview, the struggle for secure legal status is not over. Human Rights Watch has documented the poor quality of refugee status determination (RSD) by South African Home Affairs officials.[35] Lack of qualified interpreters and insufficient numbers of properly trained Refugee Status Determination Officers (RSDO) lead to decisions “taken hastily with written reasons for rejection of the claim using irrelevant, arbitrary, and pro-forma language or reasoning with no basis in law.”[36] The low quality of RSDO decisions then leads to a high number of legitimate appellate asylum claims. However, very few asylum seekers can afford legal advice and to successfully pursue such a claim.[37]
Inadequate access to legal representation in appeals proceedings heightens the risk that potentially legitimate claims are being denied.[38] And even asylum seekers who do lodge appeals, with or without the benefit of legal counsel, retain the status of “asylum seeker” throughout the process, and must continue to return to the RRO periodically to renew papers, each time encountering the same barriers, and facing the possibility of papers expiring. The bureaucratic hurdles asylum seekers face place thousands in a kind of extended limbo, as the robust legal protection offered to recognized refugees under South African and International law is continually delayed.
Internally Displaced Non-Citizens
In May and June 2008, coordinated, sustained attacks on communities of foreigners by South Africans, frequently neighbors to the victims, in multiple locations country-wide, left at least 62 people dead, including over 20 South African citizens, and displaced at least 60,000 people (estimates go as high as 150,000). Among the victims were people from Bangladesh, Burundi, DRC, Kenya, Malawi, Mozambique, Nigeria, Pakistan, Somalia, and Zimbabwe as well as XiTsonga and TshiVenda-speaking South Africans.[39] Some victims were recognized refugees, citizens, or legal permanent residents; others were undocumented asylum seekers, migrant workers or other undocumented migrants.
After victims initially took shelter in police stations, churches, and community halls, South Africa was forced to set up camps to house those displaced by the violence.These so-called “safety camps” became a flashpoint for ongoing tension between the South African government, displaced foreign nationals and the citizens in the communities from which they fled. Government and camp management have been accused of multiple abuses against camp residents, including arbitrary withdrawal of government services (health care, food and shelter), coercive deportation and documentation practices, eviction and forced relocations.[40] At the time of Human Rights Watch’s visits in November 2008 and March 2009, though all the camps had been officially closed, hundreds of internally displaced refugees continued to reside in the remains of a few camps near Cape Town and Pretoria.
Actions taken by the Department of Home Affairs in the response to the xenophobic attacks of May and June 2008 further complicated and disrupted the legal status and documentation of many of the victims. In July 2008 the government announced a six-month exemption under section 31(3)(B) of the Immigration Act, which was intended to ensure any victim of the xenophobic violence protection from deportation. However, DHA failed to communicate the exemption clearly to the displaced communities, and Amnesty International reported that the process of registering individuals for the exemption was coercive and even violent in some circumstances.[41]
Human Rights Watch spoke with a representative from Jesuit Refugee Services (JRS), an implementing partner of UNHCR with a contract to provide transitional support to displaced
people trying to move out of safety camps, who explained the confusion caused by this system:
A lot of the people who were displaced were asylum seekers; they carried a Sec. 22 form. But they couldn't renew their cards at the camp, so DHA provided this card that allowed for six months of legal status for those who were displaced. Then the cards expired, and people did not know what their status was. It was meant as a protective measure, but it had the effect that many of them lost their original status. So they were actually in a more insecure position legally, and we have seen treatment and rights deteriorate along with it.[42]
DHA also deployed Refugee Status Determination Officers to the safety camps to conduct Rapid Status Determination procedures for displaced asylum seekers. Exceptionally, DHA issued thousands of decisions within a period of weeks, but with a 98 percent rejection rate.[43] Rights monitoring groups reported numerous, serious violations during the rapid status determination process, including no notice of timing of interview, no access to legal counsel, and limited access to appeals processes.[44] Reasons given for rejection were frequently perfunctory or got basic details of the applicant’s narrative wrong.[45]
Stephen, a Burundian asylum seeker displaced in the xenophobic violence, went through the Rapid Status Determination process and, like several other camp residents Human Rights Watch interviewed, experienced a typically insufficient review of his case:
I came here five years ago as an asylum seeker. I’ve been here for 5 years with no decision on my case, until at Harmony Park, all of the sudden I was told I was rejected. But the explanation of rejection did not reflect what I said in the interview. I explained that my family was being threatened by my community, by my neighbors. But in the rejection letter they said I am not a refugee because my persecutors were family members. I never said anything like that. I don't know what my status is now. The letter said I had to leave the country. What about my family? Are they still refugees or do they also have to leave?[46]
Health Rights of Migrants in South Africa
South Africa's Constitution and domestic legislation provide for the rights of everyone to access health care and the basic determinants of health. Furthermore, the Constitutional Court is required to consider international law in its construction of Bill of Rights provisions,[47] including both binding and non-binding law.[48]
Domestic legislation and policies indicate that asylum seekers and refugees are not only included in the right to health care, but are of particular concern to the South African government in progressively realizing the right to health. Section 27(b) of the South African Refugee Act seeks to give effect to the rights in Section 27(1)(a) of the South African Constitution, stating that "A refugee...enjoys full legal protection, which includes the rights set out in Chapter 2 of the Constitution...” and provides specifically for refugees to be treated equally to citizens in terms of health and education. Refugees and asylum seekers are to be assessed for user fees according to the same fee schedule as South African citizens, including fee waivers for indigent patients.[49]
Despite these clear provisions in law and policy, however, refugees, asylum seekers and other migrants are not reliably able to access essential health services, including ART. Research from the Forced Migration Studies Program at the University of the Witswatersrand (Wits) from 2008 has documented persistent, widespread barriers to ART for HIV positive asylum seekers and refugees in Johannesburg.[50] Foreign patients reported being illegally denied ART, most frequently for not having South African identity documents (available only to South African citizens); being charged extralegal and prohibitive user fees; being verbally abused by health care workers; and having communication problems due to language difference.
In response to such concerns, the National Department of Health (DOH) released a memo in 2007 affirming that, "patients should not be denied ART because they don't have an ID."[51] The DOH explained that decreasing identity document-based barriers to ART would benefit South African citizens as well as non-citizens, stating, "this improves access for foreign migrants but also for South African citizens who may not have access to identity documentation." The following year, the DOH issued a directive reaffirming that for basic health care, refugees and asylum seekers "with or without a permit...shall be assessed according to the current means test."[52] It further clarified that in the case of ART, refugees and asylum seekers should be provided services without charge "irrespective of the site or level where these services are rendered." On the provincial level, the Gauteng Department of Health issued another letter in April 2008 reminding provincial DOH facilities, "No patient should be denied access to any area care service, including access to antiretrovirals irrespective of whether they have a South African identification document or not."
Though the DOH is to be commended for establishing a progressive policy on access to treatment, according to advocates the memo was disseminated without any increase in funding, training, or specific regulations to guide facilities in complying with it, and the DOH conducted no oversight activities to ensure its implementation. As a result, individual hospital compliance has been irregular and ad hoc. On 4 March, 2008 health advocacy organizations made a joint submission to the South African National AIDS Council (SANAC) on the health situation of vulnerable groups in South Africa. It found that "(South Africa’s) protective legal framework is not being applied uniformly. Public hospitals, clinics and other institutions appear to be unilaterally creating policies which deny refugees access to health care services, violate existing legal and human rights obligations, and undermine the objectives of the NSP,”[53] Despite affirmations at both national and provincial levels of the DOH's policy of equality of service for asylum seekers and refugees, the policy remains unrealized, existing on paper but without a systematic, coordinated government implementation, and without any urgent action to end discriminatory practices against non citizens.
Health Vulnerabilities of Migrants to South Africa
Among the many migration myths that help fuel xenophobic attitudes is the idea that a sizeable portion of South Africa's migrants are drawn to the country to take advantage of its health system.[54] These fears were fuelled by a cholera outbreak in Zimbabwe in 2008 that leapt the border to South Africa, leading to more than 12,500 cases and 64 known deaths between November 2008 and March 2009.[55] Similarly, the growing awareness of drug resistant strains of TB and the ongoing HIV epidemic have led some South Africans to stigmatize foreigners, despite clear evidence that all three diseases are endemic within South Africa.
Human Rights Watch’s research and other evidence also suggests that, while the health status of new migrants to South Africa is complex and in flux, the picture of a large number of sick migrants acting as health tourists to take advantage of South Africa's public health services is false.
Research on HIV positive migrants from 2008 found that fewer than half of surveyed migrants reported ever needing health care while in South Africa, that an overwhelming majority of them did not become ill or test positive for HIV until sometime after their arrival in South Africa, and that they migrated to South Africa for reasons other than health care.[56] A more recent study of new migrants from Zimbabwe, perhaps those logically the most likely to be motivated by the prospect of access to the basic health services now absent from in their own public health system, found that "motivations such as accessing medical assistance...were not frequently cited."[57] Indeed, the Public Information Officer for the DOH of Limpopo Province told Human Rights Watch that the biggest problem the province faced in providing health services to migrants was not that they required too much care, but that they waited too long until seeking care, when disease had already progressed.[58]
Communicable Diseases
Whatever their motivations, cross-border migrants are vulnerable to a number of communicable diseases in countries of origin, on the migration journey, and in countries of reception. Poor living conditions in South Africa, as described by migrants interviewed by Human Rights Watch, include lack of access to sanitation, water, food, and shelter, or cramped and poorly ventilated spaces. High risk sexual activity, a prevalence of sexual violence and lack of access to health services tend to exacerbate the spread of illness. Health workers told Human Rights Watch that both in border and urban clinics and in safety camps, upper respiratory infection, gastritis, STI, and diarrheal disease were prevalent, and clearly attributable to poor living conditions. [59] The reality is that communicable disease puts whole populations at risk; South African's citizens become more vulnerable when disease is not properly detected and treated in their foreign-born neighbors.
HIV
High rates of HIV regionally, plus the HIV-related risks attendant on migration itself, make HIV prevention, diagnosis and treatment for migrants a major public health concern for South Africa. Though commonly perceived to be "bringing" HIV to South Africa, most migrants in need of ART do not test positive for HIV until after their arrival in South Africa, usually after a time of healthy residence there,[60] suggesting that many may be exposed in South Africa, and that the South African government has a major role to play in reduction of transmission for this population.
After years of mis-management of its HIV epidemic, the South African Department of Health (DOH) has recently made strides toward the goal of universal access to HIV prevention, testing, and treatment. The HIV & AIDS and STI Strategic Plan for South Africa 2007 -2011 (NSP) has a target goal of treating 80 percent of those in need of ART by 2011. As of September 2007, South Africa had achieved a 31 percent rate of coverage of ART to adults and children with advanced HIV.[61] Only 33 percent of pregnant HIV positive women received ART to prevent mother to child transmission.[62] Although ART coverage is still far below the goals expressed in the Strategic Plan, these numbers represent a huge increase in access to treatment, up from approximately 4 percent in 2004, 15 percent in 2005, and 21 percent in 2006.[63] South Africa’s ART program is now the largest in the world, but an even greater roll-out is needed. The national rate of HIV infection from surveillance studies of pre-natal clinics in South Africa has remained around 29 percent since 2006.[64]
In October 2008, then-President Motlanthe replaced Dr. Manto Tshabalala-Msimang with Barbara Hogan, a longtime ANC activist and vocal critic of HIV policy under Mbeki. Within weeks of her appointment, at the HIV Vaccine Research Conference in October 2008, Hogan set a new tone of realism and urgency with regard to HIV in South Africa: “It was imperative to get ahead of the curve of this epidemic 10 years ago," she said. "We have all lost ground."[65]
Hogan also acknowledged the need for targeted programs aimed at cross-border migrants, who are highlighted as a vulnerable population in need of specialized HIV programming in the HIV National Strategic Plan, the blueprint for the HIV treatment program in South Africa. At the South African AIDS Conference in Durban in April 2009, Hogan gave a closing speech that acknowledged migration as a driver of the disease and highlighted the need for sustained, coordinated funding from international donors focused on regional and cross-border care programs. "It would be foolish to think we can scale up in isolation from our neighbors," she said. "Health knows no borders."[66] In May 2009, newly- elected President Jacob Zuma replaced Hogan with Dr. Aaron Motsoaledi. AIDS activists have urged Dr. Motsoaledi to sustain the progress made under Hogan toward fulfillment of the NSP's ambitious goal of 80 percent ART coverage by 2011.
Tuberculosis
Tuberculosis is the leading cause of death in South Africa and for HIV positive people in southern Africa. It is airborne and easily transmitted, thriving in environments with poor ventilation and overcrowding. Normally, TB is easily and cheaply treated. However the prevalence of difficult to treat drug-resistant strains of TB, high incidence of co-infection with HIV, lack of cross-border mechanisms for referral and follow up care and surveillance, and the difficulty of treatment adherence while in transit, make mobile and migrant populations a serious health challenge for South Africa's National TB Control Programme, which already struggles to meet the needs of South African citizens suffering from TB.
When TB treatment is interrupted or mismanaged, whether because of barriers to treatment access, interruption of drug supply chains, or patients' lack of knowledge of where to obtain medication, drug resistance can develop. Drug- resistant TB is much more difficult and expensive to treat than drug-susceptible TB, sometimes requiring extensive hospitalization. It is also associated with much higher rates of treatment failure and mortality. According to South Africa's Medical Research Council, only about half of adults in South Africa with active TB are cured each year.[67]
Mobile populations present special challenges to TB control, largely because of the length of time diagnosis and treatment take. Rates of TB are especially high among migrant mine workers who move in and out of South Africa, for instance from Lesotho and Swaziland, in part because of prolonged exposure to silica in the mines. A recent study of men with TB in Lesotho found that at least 25 percent of them had worked in South African mines.[68] Even where mining companies provide medical care on- site to workers, gaps in treatment have kept success rates low. For example, when HIV and TB are not treated together aggressively or, cross-border referral and follow up is too slow or insufficient, drug sensitivity is not properly detected. South Africa’s insufficient efforts to prevent and treat TB in migrant workers also create a major illness burden for its neighboring countries as well as for its own citizens.[69]
Cholera
Beginning in August 2008, Zimbabwe experienced a major cholera epidemic.[70] The epidemic spread to South Africa in November 2008, through cross-border migration combined with poor living conditions and unsafe water supplies on both sides of the border. It eventually affected tens of thousands of South Africans and killed at least 60 people in South Africa. Thousands died in Zimbabwe. The epidemic brought into sharp relief the public health dangers to South Africans in failing to respond adequately to the health needs of migrants, and the need to anticipate and respond to disease control on a regional basis.
Cholera is an acute intestinal infection caused by bacteria carried in food and water. It has a short incubation period, from less than one day to five days. It produces copious, painless, watery diarrhea and often vomiting that can quickly lead to severe dehydration and death if treatment is not promptly given.[71] However, it is easily and cheaply treated using oral rehydration therapy. Access to latrines, hand washing facilities, clean drinking water and cooked food are a simple means of preventing the spread of cholera.[72]
Undocumented migrants to South Africa frequently crossed the Limpopo River, which tested positive for cholera in December 2008, on foot. Once in Musina, migrants live with limited (if any) access to clean water, toilets, and food. These underlying conditions exacerbated the cross-border spread of cholera.
Then- health minister Barbara Hogan publicly recognized that failures to ensure universal access to water, sanitation and health information in the Musina area helped the cholera spread:
Firstly we need to ensure that communities are provided with basic services like water and sanitation. Secondly, communities need to be informed about communicable diseases, their symptoms and what can be done to treat these diseases. Thirdly, no community is an island – with movement of people and goods through the region and within our country all provinces and health facilities need to be on alert. Fourthly, we must treat anyone with a communicable disease; we cannot say this person is not local and therefore should not be treated.[73]
In response to the pressing need to treat the sick, deportations of Zimbabweans being treated for cholera were temporarily halted. However, some deportations and detentions went on, and thousands of migrants continued to live without shelter or adequate hygiene. Because Health Minister Hogan’s words were not heeded, South Africa’s ability to contain cholera was hindered; and because water and sanitation facilities on both sides of the border have still not improved and forced migrants are still at risk of deportation, South Africa and Zimbabwe should prepare for renewed cholera and other communicable disease outbreaks in the coming year.
Violence
“I came to South Africa for safety. I contributed to their society as a businessman and helped them convict my brother's killer. And what do I get in return? I am left for dead. I have no future.”
— Ali, Johannesburg.
South Africa has one of the highest crime rates in the world, with a rate of homicide second only to Colombia.[74] While criminal violence affects everyone living in South Africa, migrants are far more likely to be the victims of crime and police harassment than South Africans. Data from research conducted before the coordinated xenophobic attacks of 2008 found that 72 percent of migrants reported that they or someone with whom they live has been a victim of crime, compared with 43 percent of South Africans.[75] Non-citizens make up only 3,000 (1.8 percent) of those convicted for a crime in South Africa,[76] but are more likely to be stopped by police, with 71 percent reporting having been stopped by police compared to 30 percent of South Africans.[77] Nonetheless, surveys of South African attitudes have shown that a majority of South Africans believe that crime is increasing due to migration,[78] though most violent crime has dropped or stabilized in South Africa in recent years.[79]
In addition to vulnerability to opportunistic criminal violence, migrants in South Africa are targets for xenophobic violence, as evidenced in the coordinated xenophobic attacks of 2008. However, these were neither the first nor the last examples of xenophobic violence against non-citizens in South Africa.[80] Human Rights Watch interviewed migrants who reported being subject to multiple xenophobic attacks over the course of their residence in South Africa. Said, a Somali businessman with seven years legal residence as a refugee in South Africa, and who was displaced in the 2008 attacks, told Human Rights Watch:
I had a shop. I rented the space from the owner of the building. He has said to me, “if you think the xenophobia is over, you're wrong.” My shop was (then) looted and they beat me. The owner said, I cannot accept foreigners who do business here. Now he is using (the shop) for his own business. Once a business gets going good, it gets looted. I have had to move so many times, before this, for the same reason. In 2004, I had a shop in Port Elizabeth, looted. Then in 2005 in (another town), and then the last time in 2008. Xenophobia didn't just start.[81]
Musa, another Somali businessman victimized during the attacks, explained that violence against foreigners was ongoing:
The thing is that no province is safe. We get reports from those who have tried to leave the camp before us. In the Western Cape, Somalis like us have received warning letters even in the past few weeks. I saw it in the Daily Sun. A whole family was murdered in the Western Cape, in Queenstown. One of our men left the camp, went next door to the township. His name was Mohammad Rage Hussein, born February 1, 1960. He was killed in a wound through his chest in Pretoria three days after leaving this camp on June 27, 2008. They took nothing from him. It wasn't a robbery. It was xenophobia.[82]
The pervasiveness of violence targeted at non-citizens negatively affects their health in a variety of ways. The most obvious is through physical injury and disability. The director of an organization for disabled refugees told Human Rights Watch:
Of course some people have disabilities from birth, but in the refugee community we see that many people become disabled after being physically attacked. One of our members was thrown from a train, and another was burned in his shack. [83]
Human Rights Watch interviewed several victims of xenophobic attacks in South Africa or other violent crime who had lost their livelihood and became permanently disabled as a result. Ali, a 21 year old Somali refugee with a spinal cord injury living in Johannesburg, fled Somalia with two of his brothers and established a small shop in Durban:
We always knew we had to look out for criminals, so we never worked alone. One day, five South Africans came to the store with guns. We thought they just wanted to steal, but they didn't want anything, they didn't take anything. We were hiding behind the counter. I heard the shots and saw that my brother was hit. I didn't know that I was hit too at first. My brother didn't live long, but to watch him die in front of me, it was too long. I survived but I can't walk. I have to use a catheter. I'll never recover. I even went to testify against those guys in court, and they were convicted. But after that I got threats; the friends of those guys came to the shop with guns and told us to stay out of it. The police said they couldn't help me, they couldn't protect me.[84]
Apart from common crime and xenophobic violence, undocumented migrants are uniquely subject to violent attacks and robberies at the hands of corrupt malayshas (border guides) or magumaguma (bandits who prey on migrants in border areas). A survey by the International Organization for Migration (IOM) of over 1,000 border crossers found that roughly a third of migrant respondents reported being victimized by criminals on their journey.[85] Human Rights Watch interviewed a Zimbabwean in Musina who crossed the border multiple times in the last decade. He said: “There are definitely more magumaguma now. It's much more dangerous. Those guys used to help you get across, and now they just want to rob you and beat you.” [86]
Lack of trust between migrant communities and law enforcement officials creates an extra layer of fear and vulnerability for non-citizens. A year after the xenophobic attacks, 70 convictions had been secured, but none of them were for rape or murder, the most serious crimes committed during the violence; instead most of the convicted were charged with theft and assault.[87] The Consortium on Refugees and Migrants in South Africa (CoRMSA) notes in its most recent annual report that “many of the groups and individuals who instigated the attacks are still free and on the streets.”[88]
The use of police to arrest displaced people from “safety” camps, and to disperse crowds of homeless asylum seekers and migrants in downtown Johannesburg, also contributes to poor relationships between police and migrant communities. Musa, the displaced Somali refugee quoted above, explained that he did not trust police to protect him if he left the camp to return to the community. He told a Human Rights Watch researcher: “Two Somalis were killed inside the camps by Metro police guns; three were injured. These are the people we are supposed to call when we are attacked again.”[89]
Newly arrived migrants who do not yet have documents are especially unlikely to report crimes suffered on their illegal border crossing, for fear that the police they report the crime to will deport them. Human Rights Watch interviewed Claudius, a recently arrived undocumented asylum seeker from Zimbabwe who was robbed and beaten when he crossed the border, at a church shelter in Nancefield, a suburb of Musina. Claudius recounted:
I have seen the guy who robbed us; he stays not 100 meters from this church. But what can I do? I can’t even leave this yard, I don’t have my asylum seeker permit and they will just deport me.[90]
Arnold, a documented Zimbabwean asylum seeker who had been sleeping on a rocky bluff for over a month while he waited for his refugee status determination interview, told Human Rights Watch about an encounter with South African police officers:
I went into town to buy some mealie meal. On my way there these guys were harassing me; I told them I didn’t have any money so they took my shoes. On my way back they were waiting for me; they took my mealie meal and the rest of my money. I saw a policeman so I went to him and pointed those guys out; I said those men are thieves, they robbed me. The policeman didn’t bother with them, he just said, do you have your asylum papers? I showed them to him and he said ok, keep moving. They will kick you out before they will help you.[91]
These kinds of failures on the part of law enforcement to investigate and prosecute crimes against foreign nationals in South Africa, from large-scale xenophobic violence to the daily lawlessness of border crossings, help create a culture of impunity in which abuses against migrants go unpunished.
Sexual and Gender Based Violence
“What are we women to do? The men, they can sleep in the bush, but it isn't safe for us. If we weren't raped before we will be raped here.”
– Constance, asylum seeker at the Showgrounds, Musina.
South Africa suffers from the highest prevalence of reported rape in the world.[92] There are around 40,000 reported rapes a year; but the actual incidence of rape is likely to be much higher,[93] due to under-reporting.[94] Moreover, conviction rates are abysmally low, at around 5 percent. Sexual violence is a serious threat to the lives and well being of all women in South Africa, but migrants are particularly vulnerable to certain forms of sexual and gender based violence (SGBV) because of the risks involved in informal cross-border travel, fear of the authorities, lack of knowledge of rights and risks, and barriers to accessing both the justice system and the health system.
The threat of sexual violence is especially intense for undocumented migrant women traveling across the land border into South Africa. Researchers studying sexual activity and violence in Zimbabwe interviewed multiple men who admitted taking advantage of women stranded on the road from the Zimbabwean border town of Beitbridge to Musina in South Africa, offering (sometimes under false pretenses) accommodation or a ride and expecting – or forcing—sex in return.[95] Human Rights Watch spoke with one South African man who said of destitute Zimbabwean women in Musina:
If she is begging for money or a ride and I give it to her, of course I expect something in return. If a man is asking for money, you can give him work and give him the money in exchange. But what can a woman do for me to give her ten rand [around US$1.25]? She must have something to offer in return.[96]
The Government of South Africa has taken up several major initiatives to respond to high rates of sexual violence. It promulgated National Policy Guidelines for Victims of Sexual Offences.[97] The National Prosecuting Authority has a designated Sexual Offences and Community Affairs (SOCA) Unit with specialized prosecutors positioned in dedicated sexual offences courts. SOCA has also helped establish multidisciplinary Thuthuzela Care Centres (TCC), in public hospitals in communities where the incidence of rape is particularly high. TCCs are ‘one-stop’ 24-hour centers which integrate medical, police and legal responses to rape and other sexual offences,[98] currently with sites in five provinces and plans to establish centers in all nine.[99]
However, the availability of these services and initiatives varies greatly between provinces and between urban and rural areas. Many South African women, particularly those in rural areas, still struggle to obtain basic post-rape care.[100] Female migrants are particularly vulnerable to sexual violence during their border crossing, but have few programs directed at their needs especially in the border area, where danger is particularly intense.[101] Human Rights Watch interviewed one such asylum seeker, Theresa in Musina, who explained:
I didn't have any money so I asked a guy at Beitbridge to take me. He said he was taking other people anyway so it wouldn't cost me. During the night, he took me into the bush and said, “Now you can pay for your ride.” There was nothing I could do.[102]
Two traveling companions reported being abducted from the IOM reception center at Beitbridge after being deported from Musina, then being raped repeatedly and robbed by their captors, who brought them forcibly back over the border to South Africa. One of the young women, Julia, described her ordeal to Human Rights Watch:
I heard blood and sounds of cracking. I didn't even know such things could even happen to a person. I was a virgin before that. He really injured me; the blood was all over. I didn't know I could bleed like that. It was 2 am when they made us walk. I hadn't bathed; I had no pads; I started to swell and I was bleeding. I was walking from 2 am until we got to Musina at 2 pm. The only thing I wanted to do was lie down and die.[103]
Nearly every woman migrant Human Rights Watch interviewed at Musina reported having been raped, witnessing rape, or actively fearing rape. One woman waiting to lodge her asylum claim at the showgrounds bemoaned the lack of safe accommodation for female asylum seekers:
What are we women to do? The men, they can sleep in the bush, but it isn't safe for us. If we weren't raped before we will be raped here.[104]
Human Rights Watch interviewed an asylum seeker with an infant child who was raped in the night while sleeping at the showgrounds waiting for her asylum seeker permit at DHA:
Now my asylum seeker permit has expired and I am supposed to go back to renew it, but I don’t want to go back there. There were people all around sleeping but no one helped me.[105]
Medical and legal outreach workers in Musina echoed the sense that rape is prevalent among migrating women:
It's difficult to say how many rapes happen, because there are many hidden cases. If you talk to the men they will tell you that most women are raped while crossing.[106]
Human Rights Watch interviewed Blessing, a recent migrant from Zimbabwe whose traveling companions were raped when they were attacked by magumaguma near the Limpopo River. He recounted:
At one point we were separated; it was dark. There were many of us, so they split up the group. On my side there were two girls and three boys. They only stole from us but the girls they took into the bush nearby. I could hear the girls screaming; they were being raped. I didn't see them again until two days later, at the Showgrounds. I asked those girls if they were ok, if they went to the hospital or the police, and they said no. They didn't want to talk about it to anyone. [107]
Musina-based non-governmental organizations (NGOs) interviewed by Human Rights Watch also reported concerns about the low visibility of young female migrants in the area:
It is difficult for us to know numbers, because the girls do not present themselves. The boys you can see everywhere on the streets—you can't count how many boys there are; they are begging at shops. A lot of them have their own spots and don't rely on elders. But the girls we don't see. We think that maybe girls are coming more with families, or they are coming with predators and traffickers, but it is difficult to prove. We know that a lot of girls and women are raped at the river. There are also rapes even between the showgrounds and this office. But what we don't know is what we don't see.[108]
A Musina-based Zimbabwean activist reported:
On one hand you have commercial sex workers; there are a lot of them in Musina, both Zimbabweans and South Africans. They are vulnerable in one way. Then there are girls who are taken from Zim, kept in a house in Musina and must pay money to the people at the house for as long as they say until they release you. I could tell you fifty or a hundred houses like that. We've talked to SAPS [South Africa Police Service] about it but they say it's not trafficking because the people agreed to pay money to come to Musina.[109]
Musina-area churches and charities have established a shelter for boys, a shelter for men, and a shelter for women (particularly victims of SGBV), but there is no such shelter for young girls.
Shelter/Living Conditions
South Africa does not confine asylum seekers and refugees to camps, but allows them to self-settle into South African communities. However, they are not eligible for housing grants or subsidies, leaving few shelter options for many destitute asylum seekers and refugees. Like many of their South African neighbors, migrants frequently live in substandard, unsanitary and unsafe living conditions and can be subjected to forced evictions and displacement. Many of the asylum seekers and refugees interviewed by Human Rights Watch were living in open fields, cramped churches, overcrowded urban apartments, informal shelters in abandoned buildings, and formal and informal “safety” and other camp settings. Their housing options are limited not only by a lack of available housing but also by forced evictions and being removed by state agents, plus displacement due to xenophobic violence. Many noted that their health had declined as a result of their poor living conditions, and that their experience of violence was specifically tied to the unavailability of adequate housing.
The right to housing is enshrined in the South African Constitution,[110] as well as international law. In the groundbreaking Grootboom case, the Constitutional Court of South Africa in 2000 stated that the government had to provide shelter for those “who have no access to land, no roof over their heads, ... people who are living in intolerable conditions and ... people who are in crisis because of natural disasters such as floods and fires, or because their homes are under threat of demolition.”[111] It specified that at a minimum, people in crisis should be offered the equivalent of “tents, latrines, and a regular supply of water.”
Despite their constitutional right to housing, millions of South Africans, including the community represented in Grootboom, continue to live in informal settlements that do not meet the constitutional minimum standards. Some researchers have suggested that frustration over the state of housing in the townships and informal settlements was one of many triggers for the xenophobic violence in 2008.[112] Because they don't qualify for public housing, migrants have an even more limited number of options for shelter than some citizens, and anecdotal evidence suggests that living conditions for many have deteriorated since the xenophobic attacks of 2008.
Urban Refugees, Asylum Seekers and Undocumented Migrants
“Five people live there altogether. Whatever [illness] one person gets, another gets. It doesn't feel safe with different people going in and out all the time.”
— Patricia, Johannesburg.
The high cost of living in urban areas requires most urban-dwelling migrants to live in extremely cramped conditions, often with poor ventilation and high risk of communicable disease. The escalation of xenophobia has further deteriorated living conditions for many. In Cape Town, refugees displaced by xenophobic violence told Human Rights Watch that they were afraid to move back to their flats in the townships, where they were attacked.
For urban refugees and asylum seekers not fortunate enough even to share a bed, shelter is sometimes found in churches and abandoned buildings. In Pretoria, Human Rights Watch interviewed asylum seekers like Peter, living with over a hundred other (mainly) Zimbabweans in an abandoned tire garage called Malas Camp, who told Human Rights Watch:
It’s hard to survive here. People will fight you over your blanket or your dinner. Especially me because of my leg [Peter's leg was bandaged up and he hobbled from an injury that he claimed wasn't healing well]. You have to be tough to make it.[113]
Maria, staying at Malas Camp with her eight-month-old daughter, said:
When you don't have a place of your own, I think it is worse for women not to have any privacy. Only the people who have been here longer get rooms, or if they just demand them.[114] The rest of us just find any place to lay our heads. It affects you mentally.[115]
Residents in informal shelters also complained about the lack of available sanitary facilities. One said:
We can walk down to the petrol station but they don’t always let us use it. Then we just have to find someplace to go on the ground. There isn’t any place to bathe or wash your hands.[116]
Despite poor conditions and insecurity at shelters, some asylum seekers chose not to return to their homes after the xenophobic violence. A Zimbabwean asylum seeker who was displaced from her Johannesburg flat by the violence told Human Rights Watch: “Since the attacks I just stay at the church. At least here we feel safe.”[117]
Perhaps the best- known shelter for asylum seekers is the Central Methodist Mission Church in Johannesburg, which has housed up to 3,000 mainly Zimbabwean asylum seekers since 2007. The church is ill-equipped to act as a shelter for so many, who fill every open space on the ground of the four-floor church in the evenings; and offers insufficient access to fresh air, water, and sanitary facilities. Arthur, a young Zimbabwean asylum seeker being treated for TB at the church told Human Rights Watch: “I became ill since living here. Many people are attacked by TB at the church. There are too many people, and not enough vents.”[118] The international medical NGO, Médecins Sans Frontières” (MSF), which has a clinic next door, admits that conditions at the church are not always conducive to health:
There is no infection control at the clinic, except for a room on the fourth floor where people acutely ill with TB stay for the start of their treatment. We had an assessment done to see what it would take to install ventilation in the building, but the cost was outrageous. They would have basically had to remake the entire church. We know the current situation at the church isn’t ideal, but it’s the best we can offer right now. [119]
In addition to posing environmental health risks to residents, the Methodist Church, like other informal gathering grounds for refugees in South Africa, has been a target for state violence. A January 2008, a police raid on the church resulted in the arbitrary arrest and detention of 1,500 Zimbabwean asylum seekers. Some were denied food, water and essential medicines during their detention.[120]
More recently, businesses neighboring the church, located in the central business district of Johannesburg, brought an action to evict the refugees from church premises.[121] Starting in February, 2009, when the showgrounds at Musina near the Zimbabwe border were closed, UNHCR has been providing transit for hundreds of asylum seekers evicted from the showgrounds from Musina to the church, far exceeding its capacity. At the time of Human Rights Watch's second visit to the church in April 2009, Bishop Verryn estimated that there were more than 2,000 refugees staying at the church with at least another thousand camped on the streets outside.[122] In July 2009, 344 homeless asylum seekers sleeping outside the church were arrested in the middle of the night and detained for several days. A police spokesman told newspapers that the asylum seekers were arrested for “loitering” following complaints from local businesses.[123]
The process of moving the asylum seekers from Musina to Johannesburg was done without collaboration with and little advance notice to the asylum seeker community, and poor coordination among responsible parties. An asylum seeker who had been moved from Musina to Johannesburg after the closure of the showgrounds described the chaotic experience:
There were thousands of us staying at the showgrounds. Home Affairs told us that they were closing and we had to leave. The police said they would arrest us and take us back to Zimbabwe unless we had asylum papers and left Musina. Many people scattered into the bush, and others like me took the bus to Joburg. Now I am living on the street, just waiting for someone to tell me something.[124]
Formal and Informal Camps
“We are held hostage here. We may die in the camp from illness and hunger, or we may die on the streets from attacks. We are not asking for resettlement to North America or Europe. Just a safe place, where we are accepted by people. So far South Africa has not offered that.”
– Joseph, Akasia Camp, Gauteng.
Although South Africa's official refugee policy does not permit refugee camps under ordinary circumstances,[125] thousands of asylum seekers and refugees in fact live for periods of time in informal camps. These are either formal camps to house victims of xenophobic violence, or informal gathering grounds for asylum seekers with nowhere else to go. All of the government-run safety camps established in Gauteng and Western Cape provinces to provide shelter to people displaced by xenophobic violence had been officially closed when Human Rights Watch conducted site visits.
Research by other reputable international organizations has shown that the South African government sometimes used coercive and violent means to close the camps. One example involved the forcible eviction, arrest and detention of 700 people, including recognized refugees and asylum seekers, at Glendanda Rifle Range Road Camp in Gauteng in 2008.[126] Nonetheless hundreds of displaced people continued to live on the grounds of some of the closed camps as of June 2009, either because of fear of further violence or lack of viable alternatives.
At Akasia camp, near Pretoria, government and UNHCR-issued tents had been removed and burned by the government weeks before Human Rights Watch’s visit, leaving residents to create makeshift shelters using scrap plastic, blankets and wood. These offered scant support during the heavy rains.
One camp resident, struggling to keep her few possessions dry under her shelter, told Human Rights Watch:
God is great for bringing you here today during the rains, so you can see the misery we are living in. In houses made from rubbish. That is what South Africa thinks of us, rubbish people.[127]
Portable toilets had also been removed, leaving residents without regular access to water and sanitation. An evaluation conducted by the Forced Migration Studies Programme at the University of the Witwatersrand on the aftermath of the xenophobic violence found that the authorities withdrew essential services before the formal closure of the camps, contravening South Africa's humanitarian duty to provide basic welfare for internally displaced people.[128]
The right to health care of internally displaced people is set out in the UN Guiding Principles on Internal Displacement. These state that all wounded and sick displaced people shall receive the medical care and attention they require, without discrimination. Additionally, “special attention should also be given to the prevention of contagious and infectious diseases, including AIDS, among internally displaced persons.”[129]
Government provision of medical care at the safety camps in Gauteng was poorly organized, where it existed at all.[130] Volunteer and NGO medical teams provided the vast majority of health care to camp residents.[131]
A Somali refugee living in Akasia camp after its formal closure told Human Rights Watch:
I have asthma; MSF told me and gave me an inhaler. I never had these symptoms before. I also have high blood pressure for the first time, from the stress.[132]
Volunteer health care staff who visited the safety camps until early in 2009 confirmed that camp conditions led to a variety of health conditions:
The most common ailments we are seeing are a result of poor living conditions and stress; we see a lot of upper respiratory infections and gastritis, asthma, diarrheal disease, and then of course more life-threatening issues like tuberculosis.[133]
In addition to new illness, environmental factors have exacerbated some refugees’ pre-existing medical conditions. Abraham, the father of a diabetic child at Akasia, told Human Rights Watch:
We went last week to the hospital. They treated him [his son] there but they also gave me this letter. It says if the boy comes back again we don't know if we can keep up his care, because he can't continue living how we are living. The doctor says a child needs a proper environment to live with diabetes. We don't have a refrigerator for his insulin, or fresh needles to check his blood. He needs to check his blood in the morning and the evening, but we can't do it. The stress is also bad on him, on all of us.[134]
The reality of the unsafe conditions at Akasia had tragic consequences in February 2009, when a 6 year- old Burundian girl at the camp was killed in a fire in her makeshift shelter.[135] The remaining nearly 400 residents at Akasia were finally evicted a few weeks later and their shelters burned and bulldozed, amid ongoing complaints about police force and threats to deport those residents who did not comply.[136]
Authorities in the Western Cape generally organized and implemented their response to the xenophobic violence somewhat more effectively than in Gauteng. But the response was still dominated by civil society organizations and suffered from leadership and coordination deficiencies at the Provincial government level.[137] When Human Rights Watch conducted a site visit to Bluewaters camp near Cape Town, the camp management had closed the gates and informed researchers that the camp was officially closed. They said that no-one was allowed to enter, including the volunteer medical and humanitarian workers who had been coordinating the response to the xenophobic violence.
Camp location also caused unnecessary problems. In the Western Cape, safety camps were placed very close to the ocean, and civil society volunteers reported winter storms that ripped up families' tents and provided insufficient shelter.[138] Remote camp locations also made it difficult for residents to go to work or seek health care outside. According to one report:
Medication (for camp residents) for chronic illnesses, such as anti-tuberculosis (ATB), antiretroviral (ARV) and diabetes drugs, were usually unavailable. There was inadequate information on candidates for chronic medication, in some part due to insensitive procedures for identification.[139]
A DOH-appointed doctor was supposedly present at Bluewaters, but none of the camp residents knew about his presence. Salima, a Burundian refugee, complained to Human Rights Watch, despite great difficulty in speaking, about an acute throat infection she was suffering.
I am coughing; my tonsils are inflamed so I can barely get water down. There’s no doctor here. In a few miles there is a small clinic, but when you are sick you don’t want to walk that far. I went to the camp manager and asked for help but the manager said: “the camp is closed, I can’t help you.” I have no money for transit to the doctors. I am just using some medicines leftover from someone else’s illness. I am not the only one; there is so much illness here.[140]
Conditions are even worse for recently arrived asylum seekers at Musina in Limpopo province. Since Human Rights Watch's June 2009 visit and the closure of the showgrounds[141] some small shelters have opened in local churches for asylum seekers. But the need for good accommodation is much larger than the supply, and it is still provided by community and voluntary groups with insufficient support from UNHCR and the South African government. A South African service provider told Human Rights Watch:
To be honest with you, it looks like our government does not care about asylum seekers. We don't need a permanent refugee camp, but temporary shelter for newcomers.[142]
A local Zimbabwean community activist, who helps arrange much of the available shelter for refugees, told Human Rights Watch:
We rely on the churches to shelter people but we keep looking for something more sustainable. People need not only ground to sleep on but also toilets, showers, and cooked food. The congregations have been very generous with the asylum seekers, but they have to accommodate church services as well.[143]
While service providers in Musina agree that the “closure” of the showgrounds improved immediate conditions outside the DHA office, one told Human Rights Watch:
Really, it just relocates the problem. People don't disappear just because they aren't allowed at the showgrounds; they go into the bush, where we can't reach them. The accommodation crisis is just moved, not resolved. The next time there is a backlog, we will be in the same situation as before, until people can move legally and there is sustainable transitional shelter.[144]
Food insecurity
“The biggest problem here is not medicine, it's hunger. It's been four days (and) I haven't eaten.”
—Moses, Showgrounds, Musina.
The South African Constitution guarantees access to food and water[145] and children's rights to basic nutrition, shelter, basic health care services and social services, without regard to nationality.[146] As well as being key to realizing the right to health, nutrition and food security programs are important components of progressive primary health care strategies for people who are vulnerable and chronically ill. The consequences of chronic food insecurity on the state of health are self-evident: vitamin deficiency leads to increased susceptibility to all kinds of diseases, developmental problems in babies and growing children, or even death. Food security is of particular importance to those suffering from compromised immune systems and chronic diseases (like HIV and TB) and to pregnant women and young children. Despite South Africa’s development of an Integrated Nutrition Programme for the management of nutritional policy toward vulnerable groups, the majority of South African households experience food insecurity.[147] Foreign migrants in South Africa are likewise at risk of food insecurity, and in many cases it is exacerbated by xenophobia and displacement.
A majority of asylum seekers and refugees interviewed by Human Rights Watch described some level of food insecurity. One asylum seeker said:
Besides accommodation, our biggest concern is just eating. I don't know where my next meal is coming from. Yesterday a sister gave me some pap, but today, who knows?[148]
Another explained:
I wasn't expecting this. I saved up money so that I could easily survive on my journey. But I was robbed while I was crossing the border, and now I have nothing. There is food here I could buy, if I had some rand.[149]
Highest levels of food insecurity were reported by newly arrived migrants traveling overland over the South African border with Zimbabwe, and by those living in formal or informal displaced-persons camps. A Somali community leader at Akasia camp told Human Rights Watch:
We just rely on good Samaritans to feed us since the government left. If someone brings a little food, we break it up and share it, because we know that everyone needs it, especially the women and children and the ill. There are many days when we eat only a few slices of bread, or nothing at all.[150]
Food insecurity exacerbates existing health problems. A health care worker in Musina told Human Rights Watch:
Patients will tell us they don't want to take their medicine, like ART, because they don't have any food to take it with.[151]
An asylum seeker at the showgrounds concurred:
I got some antibiotics for this rash I got from sleeping outside. But I haven't taken it today or yesterday because when I don't have a meal they bother my stomach. I don't want to give up the rash only to have stomach problems.[152]
UNHCR, along with civil society groups and local churches, provide some food to refugees on a limited basis to (primarily documented) asylum seekers in Musina. However, the food provided is usually dry and uncooked, forcing recipients to find water, pots, pans, and to make a fire, often a difficult task for destitute migrants living in the bush or on the ground outside the DHA RRO. An asylum seeker, showing Human Rights Watch researchers the open field where he had been staying for two months outside Musina, said:
Look at these cans we have to cook from. They are rusty and there is no place to clean them. Even if I get a little mealie meal, we can't always make a fire. This morning I begged some water from some people in Nancefield; otherwise I would have nothing.[153]
The minority of asylum seekers receiving food aid report other problems:
They don't give it every day, for one thing. They don't give it on the weekends, and it isn't a lot of food. You have to stretch it. You can maybe get one meal a day, and it's just mealie meal.[154]
Cooked food provided to the small number of asylum seekers staying at church- based shelters in Musina are usually provided with papand gravy, beans and sometimes meat, twice a day. A service provider helping unaccompanied minors admitted there were gaps in food provision: “We buy vegetables when we can, but we don't always have them.” [155]
Many Zimbabwean asylum seekers in Musina, particularly unaccompanied minors, reported hunger as a major reason for flight, and several appeared to be malnourished: “I came because of hunger. I think there is no food left in Zim. My family couldn't feed me anymore, so I went out into the streets to beg.”[156]
Physically weakened by the worsening situation in Zimbabwe, migrants' health can therefore deteriorate further after their arrival in South Africa due to lack of food, adequate shelter, sanitation and, in some cases, access to health care for fear of being deported.
A health assessment of food security for migrants in safety camps after xenophobic violence found that, while food provision was initially sufficient, food security diminished as the government decided to close the camps in August 2008, and that “many of the supplementary exercises related to food security advocated by the UNHCR such as conducting an initial…needs assessment and arranging community education on the use of food-aid were not undertaken.”[157] Because much of the food aid to displaced-persons camps was provided by voluntary groups, continuity, planning and coordination of food provision was sometimes a problem.[158] A former camp manager from Western Cape reported to Human Rights Watch that food at Bluewaters was never assessed for nutritional completeness:
Before they made me camp manager, I had no experience doing anything like this. I had some experience organizing, but that's it. That alone should tell you the level of professionalism with which the camps were planned. I started to educate myself. I read UNHCR's guidelines for the treatment of displaced people. What we were doing didn't comply with minimum standards. You could see the lack of nutrition take a toll on people's health.[159]
A volunteer doctor who assessed the health situation for children in the camps agreed:
The food they were given is not fit for growing children. It was mostly just tea and white bread. I was shocked that no one was paying attention to this.[160]
Though acute malnutrition was uncommon among displaced people, the nutritional content of the food was a concern, as diarrhea and acute dehydration was common in the safety camps.[161] Finally, in September and October 2008, local government provision of food to camp residents stopped as reintegration plans were being drawn up, made or implemented, leaving hundreds of camp residents stranded with no readily available food source.[162] Displaced people reintegrating into the community also faced food insecurity. The Forced Migration Studies Program’s (FMSP) evaluation of the Government of South Africa's handling of the camps found that “There was no livelihood intervention to protect IDP's food security after they left [the camp].”[163]
Refugees’ nutrition has also been inadequate, especially for those with pre-existing medical conditions. Cecile, a recognized refugee with high blood pressure living in Johannesburg, said: “I can't eat properly. I need more milk, and sometimes I skip medicine if I don't have food or milk to take with it.”
Ndona, Cecile’s roommate, concurred: “I have hyperglycemia, but I can't stay on the diet I am supposed to take, so the problem keeps getting worse.”[164]
Another urban asylum seeker battling several chronic illnesses noted: “[One] problem [with] my medication is food. If I don't have any when I take my medicine, it hurts my stomach. It seems I never have enough food for when I need to take pills.”[165]
Barriers to Obtaining Healthcare
Migrants to South Africa face a range of risks that leave them vulnerable to injury and disease. Left untreated, these health conditions have a negative impact not only on migrant communities, but on South Africans who end up bearing the human and financial costs of increased transmission of communicable disease and, as a result, migrants’ increased dependence on humanitarian and state aid due to disability and illness.
Human rights abuses also increase vulnerability to ill health and impede access to treatment. Despite the clear legal rules and political commitments requiring South African officials to ensure migrant access to health care, Human Rights Watch documented four major, persistent barriers: discrimination; inadequate, inaccurate and misleading information, barriers to emergency care for rape survivors, and extralegal user fees
1) Discrimination;
2) inadequate, inaccurate and misleading information;
3) barriers to emergency care for rape survivors; and
4) extra-legal user fees;
Discrimination
“Xenophobia is still here. Only now it lives at the hospital.”
—Sefu, Johannesburg[166]
Discriminatory attitudes impede access to health care even before migrants arrive at some health centers in South Africa. A refugee health advocate in Cape Town told Human Rights Watch:
[I]t starts as early as when you call for an ambulance. They can hear that you don’t speak the language, so they don’t hurry to send you the ambulance. They think, this foreigner probably cannot pay. Sometimes they don’t even come when you call.[167]
Allegations of discrimination and xenophobic attitudes by health care staff ranked as one of the leading barriers to health care reported by migrants interviewed by Human Rights Watch. Alleged discriminatory behaviors cited by migrants included outright treatment denial, verbal or even physical harassment, and deliberately longer wait times and premature hospital discharges for migrants. A refugee health advocate with over a decade's experience in South Africa told Human Rights Watch:
In general, before May 2008 access to treatment was improving, but xenophobia has created a lot of problems. It's worse now than before the attacks. It’s not the policy that is the problem by now. It is individual discrimination by nurses and others at the hospital. We have lost the ground we won over the last ten years and have to start again from square one.[168]
Xenophobic attitudes on the part of health care staff have been documented by multiple monitoring groups.[169] In a recent submission to the Gauteng DOH on access to health care for migrants, researchers from the Forced Migration Studies Programme (FMSP) at the University of the Witswatersrand concluded that “Impartiality of health care providers is threatened as they find themselves practising within politicised spaces.... Health care provision is not apolitical.”[170] A refugee in Pretoria gave his experience of xenophobia in a health care setting: “At the hospital people are harsh. They don't take us as human beings.”[171]
Another migrant alleged that health care staff used insulting and xenophobic language:
We don’t like to go to the hospital or outside the camp because the people there say to us, “You are Makwerekwere [foreigners]. This was the word they used during xenophobia.[172]
Xenophobic attitudes were also evident in the straightforward denial of treatment on the basis of nationality:
I was robbed. My phone rang, I answered it and I was assaulted. People on the street just watched it happen. I went to the police and they called an ambulance. I went to Hillbrow clinic [Johannesburg]. They had to stitch up my hand. I asked for an x-ray but they said “no, that's not for foreigners. Go back to Zimbabwe if you want x-rays.” I went back four times but it was always, “no my friend, that's for South Africans.” [173]
In some cases, refugees and asylum seekers bore the harassment and still managed to get access to some health care. In others, health care staff quarreled over the proper treatment of refugees and asylum seekers in front of the patient, highlighting different attitudes and approaches of staff within one treatment facility. Said, at Akasia camp, recounted:
I went to the hospital yesterday; I was sick. I called an ambulance but it didn't come, so someone gave me a ride. At the hospital they told me, “this is not your country, we can't treat you,” and sent me away. I left the hospital and went to another clinic. One doctor, a female doctor, was saying, “Just treat him,” but some others were saying, “Don't treat him.” Some of them said I was a human being and deserved treatment, and others fought her right in front of me. Eventually they gave me medicine. I have been in South Africa for 7 years as a recognized refugee. I was a businessman; I had a grocery business. I used to only go to private hospitals where I paid for treatment. I never had a problem there. Only later when I started to go to public hospitals would I be treated like this. [174]
One refugee service provider explained to Human Rights Watch:
The most frequent kind of discrimination I see is put in terms of documents. The provider will ask for documents, and then if you provide an asylum seeker permit they will say “no, not that one.” I think that providers are generally familiar with the law though. It seems to be that they deny someone when they feel they can get away with it, because when we send people with [referral] letters, they are treated. Or it will come out in terms of wait times. Foreigners will be treated, but not until the end of the day; they are left to last.[175]
Whatever the form treatment denial takes, migrants seeking their legally mandated health care are frequently forced to visit multiple providers in order to gain access to treatment as a result of discrimination at certain facilities. One Bluewaters resident told Human Rights Watch:
At the clinic, even if I arrive first, I go last. Before I lived at the camp I used to go to Westbank Hospital; but now they said I couldn’t come there because it was too far away from where I am living. You spend the whole day going there and then no treatment in the end.[176]
Kelvin, an asylum seeker in Johannesburg interviewed by Human Rights Watch, did not successfully obtain treatment for TB until reaching his third health care facility:
I went to Joburg Hospital because I felt like I had TB. I went to be tested. They told me to go to Hillbrow. At Hillbrow they said, “we don't like foreigners, you are thieves.” So I went to Helen Joseph and got tested there. I was coughing, losing weight. At Hillbrow I heard some of the nurses saying “we don't like them here, this hospital is for South Africans.” I was very sick. I had been sick for three weeks.[177]
In a few instances, discriminatory hospital staff behavior described to Human Rights Watch went beyond verbal harassment into physical abuse and medical neglect. Claudia, an asylum seeker from DRC living in Johannesburg, suffered a miscarriage when she was shot during civil conflict in her country. She became pregnant again after fleeing to South Africa with her husband:
I was going to Edenvale Hospital for all my prenatal checkups. Everything was normal and there were no problems with the pregnancy. But when I was in the labor ward to give birth, I wasn't treated well. The doctor was ok; he was a foreigner too. He said I needed a cesarean section and left me with the nurses who he instructed to refer me to surgery. But when he left those sisters [the nurses] refused to do it; they said I was fine and I could give birth without surgery. They said, “you Africans can just give birth outside.” One nurse said, “we were suffering here during apartheid, and no one came to help us. Now we have peace and all foreigners come to grow the population. That one is not my problem.” They left me alone in the dark for hours. Finally in the morning the doctor came back and heard me crying in my language and said, “how can you leave the lady here suffering? Take her to surgery!” They did the c-section but the baby was traumatized. After I came home, the child's head grew large, he was vomiting and losing weight.[178]
Edenvale Hospital referred Claudia and her son to Johannesburg Hospital, where after being diagnosed with hydrocephalus and cerebal palsy, he was repeatedly turned away for surgical interventions on grounds that shifted from appointment to appointment. She was first told that her son was too young to be treated, then that there was nothing the hospital could do for the child, and finally that they had lost the child’s medical file. According to Jesuit Refugee Services (JRS), who advocated for the child's care, Johannesburg Hospital first told them that the surgery would be too costly, later taking the position that the surgery was too dangerous and that there was no specialist trained to do it.[179] The child received some physiotherapy, but as of Human Rights Watch's last interview with the family, his providers had recently stopped giving therapy, telling Claudia that without surgery, nothing could be done, and that surgery had to have been performed earlier in the child’s life.[180] The child is now nearly three years old, and his condition is too advanced to treat. Claudia summed up her situation:
They destroyed my child because I am a foreigner. It would be better to go back to the Congo and die.[181]
Though claims of such egregious abuses in the course of treatment are difficult to prove, many refugees and advocates expressed concern that the lack of accountability in the South African health system creates an atmosphere in which such abuses can easily go unaddressed.
A refugee health care advocate in Cape Town told Human Rights Watch:
It's not something we can prove, but a lot of us foreigners feel we are cut off from care too soon, that our deaths may even be hastened, or else we are pushed from the hospital in the name of cost cutting. Many of us die in the hospital, and nobody knows what happened. A body can sit in the mortuary for three weeks.[182]
Researchers at Witswatersrand University's FMSP have also called attention to a reportedly high but the unknown number of unnatural deaths of foreigners occurring in public hospitals.[183]
Human Rights Watch also learned of some cases of discriminatory treatment immediately following the xenophobic attacks in 2008. Edmund, a Zimbabwean asylum seeker who had earlier worked on a farm in Limpopo Province became disabled after a tractor accident and moved to Johannesburg. But Johannesburg proved to be no safer:
In June this year, in the time of xenophobia, South Africans attacked our building because they knew Zimbabweans lived there. Some Zimbabweans fought back but I couldn't, because of my injuries. They beat me badly and ruptured my intestines. I went to the hospital that first night during the violence; they operated on me in the night and put a pipe inside my stomach. The beds were all full. Later that same evening a South African came and needed a bed, so they discharged me for the South African. My doctor didn't discharge me; I was transferred out by a nurse. The man who got my bed was a friend of the nurse who needed a place to stay. I had a catheter and an oxygen mask when they told me to go. I had to walk from the hospital, but I couldn't go home because of what happened there. They wouldn't give me any money for a taxi or even a walking stick. I found a broom and broke it and used it as a crutch. I never got a discharge letter, even though I asked for one, and no tablets to take with me. I walked about six kilometers that night and stayed at the church. I was having pain the next day. People at the church brought me to the hospital again; I stayed for three weeks this time and they had to do the surgery again.[184]
As these harrowing narratives detail, the discrimination faced by migrants in health care settings cannot be understood outside the context of a pervasive xenophobia throughout South African society.
Inadequate and Inaccurate Information
The right to information is entrenched in section 32 of the South African Constitution. The enabling legislation emphasizes the transparency and accountability of state bodies and integrates oversight into right to information issues.[185] To fulfill its duties in this regard, the South African state, through the Department of Health, the Department of Home Affairs, and any other relevant bodies, must be transparent in its decision-making and policy implementation processes. It must actively solicit the participation of affected communities (migrants themselves) as well as civil society advocates, service providers, and other arms of government.
Human Rights Watch found clear evidence that the South African government routinely fails to ensure migrants’ rights to seek, receive, and obtain health-related information on a number of grounds. First, it fails to ensure that migrants can obtain information about health risks and services to which they are entitled as a matter of law, either by failing to provide it altogether, or failing to ensure it is available in a manner that can be understood. Second, it fails to ensure that health care providers have adequate information about migrants’ rights to health care.
The most direct way in which South Africa has failed to implement migrants' right to health is by failing to educate them about the health risks they face, and their right to obtain care. The DOH at both national and provincial levels has failed to promote its policy of health care access for asylum seekers and refugees beyond two memos from DOH sent to district hospitals clarifying that asylum seekers and refugees with or without had the right to access health care; and no national or provincial government program exists to educate patients about their rights.
Human Rights Watch interviewed a welfare coordinator at a refugee service organization in Cape Town, who had been conducting a survey of her clients' experience with the public health care system:
We've found that people lack awareness that they can access care without asylum documents. It seems to be that only the patients who really know their right to health care and assert it, end up getting treated. I just had a client who was turned away from the hospital; they told her that she needed to go back to Home Affairs and get her asylum seeker permit. And maybe 10-15 percent of people will do nothing if they are turned away for care. People spend all day in queues, and then they finally get to see someone and they say no, go back to Home Affairs...some people will give up.[186]
Lack of information about HIV and TB care means that some asylum seekers and refugees seek diagnosis and treatment late, often without proper counseling.[187] Mr. Seloba Phuti, the Public Information Officer for Limpopo Province Department of Health, told Human Rights Watch that one of the biggest challenges the provincial government faced in providing health care to the many documented and undocumented migrants in Limpopo was migrants' tendency to seek care late, when illness was already very advanced and more difficult and costly to treat.[188]
One of the most obvious barriers to information that migrants face when seeking public health care in South Africa is lack of linguistic and culturally appropriate health communications. DOH does not employ any translators,[189] so it is up to patients to provide their own interpreters. The long waits at health care facilities make interpretation impossible or unaffordable for most migrants, who cannot afford to pay an interpreter to wait in line all day or for multiple days.
Eva, a South African citizen from Cape Town who is married to a Congolese refugee, told Human Rights Watch:
It's true that everyone gets treated badly in the public hospitals, but it’s worse for non-nationals. Foreigners wait even longer than we do. Health care worker attitudes are a problem. They get annoyed with language problems, and they don’t seem willing to assist. Most clinics don’t have interpreters, so the doctors will just ask yes or no questions, and don't get to the bottom of things. They take advantage of foreigners’ lack of knowledge of their rights, so they will tell them go somewhere else. [190]
Foreigners' lack of understanding of the health care system and their inability to communicate with health workers creates inadvertent problems for the health system, such as when they seek care at the wrong health facility. The Public Information Officer for Musina Hospital said:
The doctors complain that they are seeing foreign patients who should be going to the clinic instead.[191]
This kind of confusion also contributes to the negative perception among migrants of the public health care system. Human Rights Watch found several cases of foreign patients who were told by hospital staff to go to a more appropriate facility, but perceived that they were being denied treatment.[192]
Similar problems arise around testing for HIV. For example, rape survivors who seek treatment at a hospital or clinic for post-rape care such as HIV testing and PEP are required by DOH policy to be tested for HIV before a prescription for post-exposure prophylaxis (PEP) can be given. Foreign patients without local language capacity can misunderstand this process, leading to missed opportunities for life saving care:
For non-citizens, it can be challenging to get consent; we see it especially with francophone refugees. You need a translator, but it is the duty of the patient to identify an interpreter because of confidentiality issues. The patient must be very motivated to arrange all of this.[193]
Informational and linguistic barriers also deter refugees and asylum seekers from making official complaints about discrimination, access to health or treatment. None of the asylum seekers and refugees Human Rights Watch interviewed had lodged an official complaint. As mentioned above, the Gauteng DOH Patient Complaint Line also told Human Rights Watch researchers in April 2009 that no migrants had accessed their system, nor were services or literature in non-South African languages offered.[194] Without information on input from migrant patients, health care facilities at the management level are unlikely to hold individual staff accountable for inadequate service or abuses.
Barriers to Care for Rape Survivors
“When a survivor comes to the hospital after a rape, they tell her, 'first you must go to the police, then we will give you treatment, and only after that will we deport you.'” [195]
— Nurse Medical Focal Point, MSF, Musina
Sexual violence has a profound impact on physical and mental health. In addition to physical injury, it is associated with an increased risk of a variety of sexual and reproductive health problems and immediate and long-term consequences, both mental and physical. Women subjected to sexual violence are at higher risk of contracting HIV, because of the higher likelihood of vaginal tearing and internal injury.[196] Even so, after exposure to HIV, infection can be halted through a course of post-exposure prophylaxis (PEP), a 28-day treatment involving ARVs. This treatment is only effective if provided within 72 hours of the rape occurring.
In 2005 the Department of Health released its National Sexual AssaultPolicy (NSAP) and National Management Guidelines for Sexual Assault Care. One of the objectives of this policy was “to establish designated, specialized, accessible, 24 hour health care services for the holistic management of patients to improve health status after sexual assault, PEP and psychosocial support.”
The NSAP makes clear that “no patient should be turned away if they have not reported the assault to police or choose (not to),” that “Patients should be encouraged to make their own informed decision regarding reporting the case to the police and that this decision should be respected,” and “If the patient decides not to report sexual assault to the police at that time, the examination should be completed, documented and evidence preserved if the patient agrees and consents.”[197] However, due to perceived conflict between the wording of the above passage in the Sexual Offences Act and that of the DOH guidelines, some facilities persist in requiring survivors to lodge a police report prior to receiving care.
In contrast to the holistic services offered at Thuthuzela Care Centres, specialized centres for sexual violence, some designated health facilities for rape survivors are held in casualty wards of busy hospitals, such as Musina Hospital, where victims may be kept waiting for hours, sent to make a police report before obtaining care, or not offered access to the full range of essential medicines for post-rape care.
Though many citizen rape victims also lack sufficient, timely access to post-rape care for a variety of reasons, Human Rights watch’s research shows that migrants in particular are likely to lack information about treatment facilities and their rights under the Sexual Offences Act. In addition to the shock and trauma caused by the rape itself, if a migrant patient does not speak the same language as hospital staff, does not have access to transportation, or does not understand the South African health system, they can easily end up missing the 72-hour window in which emergency contraception and PEP are effective. A nurse-advocate for survivors of sexual violence in Musina told Human Rights Watch:
The biggest problem is that most of them don't come for help within the 72 hours, and then there is not much we can do for them. They are traveling, they are traumatized and injured, they are scared and they don't know where to go.[198]
At Bluewaters camp near Cape Town, a Burundian refugee named Clare pulled aside a Human Rights Watch researcher to report that she had been raped the week before in a taxi:
I went to the clinic and I got a pregnancy test and an HIV test, but I didn't tell them exactly about what happened to me. I haven't been able to go back there to find out the results of the test. I don't know when I will be able to go; I don't want to get into a taxi again.”[199] (By then, the 72- hour window had passed).
Furthermore, official policy is unknown, misunderstood, and/or misapplied by many health practitioners, causing serious barriers to care. Several providers told Human Rights Watch of their belief that a police report must be filed either before PEP and emergency contraception is provided, or concurrent with treatment.[200] A nurse working for MSF in Musina spoke to Human Rights Watch about rape survivors' treatment at Musina Hospital:
When a survivor comes to the hospital after a rape, they tell her, “first you must go to the police, then we will give you treatment, and only after that will we deport you.”[201]
The requirement to file a police report presents a barrier that will often be prohibitive for many migrant women seeking access to lifesaving PEP and other post rape health care. Even South African women are frequently unwilling to report their rapes for a variety of reasons, including stigma, fear of or reliance upon their attacker, or fear of being mistreated in court or by police.[202] In practice, for undocumented migrants who risk deportation, who work in informal sectors or in the sex trade, who know or depend upon their attackers for survival, or anyone else who fears or does not want to make a police report regarding their rape, access to post-rape care can be seriously obstructed.
Human Rights Watch spoke with a nurse advocate for migrant survivors of SGBV in Musina who said:
“If I am not there, they will deport the victim if she doesn't have her papers. The victims are too scared to report unless I go with them, they are too scared of police.”[203]
Although the moratorium on deportations of Zimbabweans may have lessened fear of deportation to a certain extent, service providers in Musina have reported that Zimbabwean migrants have been reporting increased numbers of sexual assaults, many of them occurring in Musina.[204] Police are still arresting undocumented migrants, including survivors of sexual assault and other crime, and holding them at least overnight until DHA can attend to them.[205] An assessment of migrant vulnerability on the South African side of the border area with Zimbabwe found that 90 percent of the survivors of violent attacks and 72 percent who had experienced sexual assault said they did not report the case to the authorities.[206]
Human Rights Watch spoke to Musina Hospital spokesman Edward Malema. He disputed the allegation that the hospital sent people away to the police before providing care:
“No, it is not our policy to delay prophylaxis for any reason. The doctors know they are to go ahead with treatment and at the same time to call the police.”[207]
Even if this is true, even the requirement that police be called simultaneously with treatment still presents a major barrier to those who fear arrest or who for any number of reasons do not wish to file a report, and is contrary to the NSAP. Mr. Malema added that rape was one of the main reasons for hospital admissions of Zimbabweans to Musina Hospital.[208]
User Fees
User fees for health care in the South Africa public health system vary according to the category and means of the patient. Patients are divided into Full paying patients, who are charged the full cost of care and Subsidised patients,who are provided a range of subsidies and fee waivers according to a means-based test. In addition, a limited number of services are provided free of charge on a statutory basis for specific groups.
Subsidized patients are broken up into four income groups and charged fees accordingly, with subsidies ranging from 20 percent to 100 percent of the total cost of care. Patients who can prove they lack means, by reliance on a government social care grant (for age, disability, etc.) or by producing an unemployment insurance card, and anyone else so recognized by the head of the health facility, receive free care. Services provided free for everyone include treatment for infectious disease (including HIV, TB, sexually-transmitted diseases [STDs], cholera, malaria, meningitis and malnutrition, pre-natal[209] and early childhood health care.[210]
According to government directives, foreign patients are generally considered full-paying. Exceptions are made in the cases of:
“Non South African citizens excluding the following:
(a) immigrants permanently resident in the RSA but who have not
attained citizenship
(b) non South African citizens with temporary residence or work
permits
(c) persons from SADC states who enter the RSA illegally.”[211]
All of the migrants interviewed by Human Rights Watch fell into one of these three categories, making them eligible for subsidized health care on the same fee schedule used for South African citizens. Asylum seekers and refugees are not specifically mentioned in the regulations, but as legal residents of South Africa, should be considered subsidy-eligible non-citizen patients. A September 2007 directive from the DOH Revenue Directive to all Provincial Health Revenue Managers, affirmed that for basic care, “Refugees/asylum seekers with or without a permit shall be assessed according to the current Means test.”[212] Furthermore, it stated that refugees and asylum seekers with or without a permit are to be provided ART free of charge regardless of the level of care being sought.[213]
Despite these clear regulations, problems arise when an asylum seeker who is legally present in South Africa doesn't have an asylum seeker permit, or when hospital staff fail to accept asylum and refugee documentation as proof that the patient is eligible for subsidized care. Human Rights Watch research has shown that such patients are often misclassified and charged the full cost of service (sometimes referred to as “foreign patient fees”), high charges leviable only on South African citizens with external funding or non-citizens who are not one of the enumerated classes. Furthermore, even undocumented migrants from elsewhere in southern Africa (including non-asylum seeking Zimbabweans) should be assessed according to the Partially Subsidised fee schedule, but are often charged the costlier foreign patient fees instead.
Asylum seekers and refugees Human Rights Watch interviewed reported being charged a multitude of fees, ranging from 20 – 1800 RSA [US$2.50 to $230] for basic consultation fees, to hundreds of thousands of rand for advanced care. Even when these fees are issued consistent with DOH regulations, they are still too expensive for many patients. In other cases, health care facilities levied charges that clearly violated DOH fee policy.
Multiple sources in Musina reported that Musina Hospital illegally charges user fees to women in labor, in some cases resulting in delayed or denied access to medical assistance during labor for women who cannot afford the fees.[214] Victims of this practice included an undocumented Zimbabwean asylum seeker in labor who was charged 500 RSA [around US$60] for delivery services at the hospital.[215]
Even the smaller (20 percent of total cost) fees associated with the lowest end of the subsidized patient fee schedule can still be prohibitively expensive, particularly for impoverished migrants. One asylum seeker in Musina told Human Rights Watch:
I came here with a woman who tried to go to the hospital to give birth; they charged her 60 rand [US$8], so she left and just gave birth in the bush.[216]
Another asylum seeker with a high-risk pregnancy delayed needed care because of an initial charge of 20RSA [US$2.50]. Although prenatal care generally is not guaranteed to be free for undocumented non-asylum seekers, assistance for women in labor that the kind of urgent care is should fall under the constitutional right of everyone in South Africa to have access to emergency health care, and should not be denied either because of immigration status nor ability to pay.[217] Whether a health care worker perceives an undocumented pregnant woman seeking prenatal care to be a “foreign patient,” (full fees), an undocumented regional migrant (partial subsidy), or an undocumented asylum seeker (free prenatal care plus subsidies) can result in serious health consequences for the patient.
For migrants with chronic conditions like HIV, tuberculosis, and diabetes, requiring ongoing and frequent doctor visits, even the subsidized user fees can add up to more than many (especially disabled or ailing) patients can afford. Cecile, a recognized refugee from DRC living in Johannesburg, finds that her medical costs push her over the edge of her limited budget:
I have high blood pressure and glaucoma. Because of this I am losing my eyesight. A doctor prescribed me glasses, so I could try to find work, but they cost 920 rand [US $115], and they say that it is not emergency, I don't need it so if I want the glasses I must pay. But I have to live on 800 rand [US $100] a month. Almost the whole 800 goes to rent, then I have to pay for my medicine and food. I can't send my daughter to school because I don't have the money for school fees. Our whole income goes just to keep me alive. I'm a beggar in the street because I can't get a job; I can barely see without glasses and I have too many health problems. What will South Africa do to me when I am blind?[218]
Phillip, an HIV-positive, unemployed Ugandan asylum seeker in Johannesburg described the medical debt he has accumulated from user fees for the regular hospital visits he makes to manage his multiple concurrent illnesses.
I had been in South Africa for some years when I tested for HIV. I don't have too many problems getting my ART. It's my other appointments that are the problem. Every month I have appointments at Johannesburg Hospital; they charge me 40 rand [US$5] each, plus I have to pay for my prescriptions. Right now I owe Joburg (Johannesburg General Hospital) 240 rand [US$30]. They say they won't give me a scan that I need on my leg [due to Kaposi’s sarcoma, an opportunistic infection associated with HIV infection] until I pay.[219]
If Cecile and Phillip were South African citizens, their medical conditions and unemployment would likely qualify them for one or more forms of social care grants. “Social pensioners” entirely dependent upon the state for their income must provide proof of grant reliance to qualify for totally subsidized (free) care. Because non-citizens, even recognized refugees with legal residency like Cecile, aren't eligible for government grants, qualifying for a full subsidy is nearly impossible.
A non-citizen's only other hope of qualifying for free health care would be under the third category of fully subsidised patients: “Persons re-classified as H0 [the fee category for full subsidies].” If a patient cannot afford health care fees on the basis of his or her original classification then the patient may be re-classified as “H0” by the person in charge of the health care facility.[220] Human Rights Watch was not able to document how this category is currently implemented, if at all, but it seems on paper to imply official acknowledgement that health facilities may be obliged in law to offer fully- subsidized care to needy patients who would not otherwise qualify. But the vagueness of the provision makes it unlikely that health facilities will implement it voluntarily without clear guidance or instructions from provincial or national DOH authorities.
The public health sector in South Africa is under immense financial and resource strain, and asylum seekers and refugees represent a hitherto unaccounted-for population in health budgeting. Hospitals that serve a large migrant community, such as Musina Hospital, are especially stretched, and may informally be under more financial pressure to charge patients user fees or otherwise limit their expenditure on non-citizens. Edward Malema explained:
The provincial government gives us a budget based on estimated population. But with the Zimbabweans, our population is twice as large.[221] We need to expand the number of beds; 80 percent of patients admitted to the hospital are Zimbabwean.
Hospitals with large migrant populations are also likely to have unexpected but costly duties:
We also have a problem with what to do with the terminally ill and dying. Last week we buried 17 unclaimed bodies. We believe they are Zimbabwean but because of (they use) false names and addresses,[222] it's very difficult to trace their families to come and fetch the body. We keep everyone for 3 months, but it depends on the mortuary budget, and cooperation with the Municipality.[223]
Many undocumented asylum seekers and migrants may be forced to use false documents if they do not have access to passports and visas in their own names, as is the case with many Zimbabweans (due to corruption and seriously decreased capacity in government services in Zimbabwe, or because the migrant is fleeing state persecution and fears traveling under their own name). Others may fear being arrested, or having their presence in South Africa reported to authorities in Zimbabwe, or may be motivated by a desire to protect family members back in Zimbabwe.
Special needs also arise around discharge of seriously and/or terminally ill foreign patients:
We will have a patient admitted in the hospital who is very ill, even dying. If there is nothing else we can do for him, we have to discharge him; we need the bed for others. But how can we discharge someone who is ill, with no clothes, no shelter, and no contacts? They don't like us to call the police but sometimes we must call the police to come take them back to Zim.[224]
Apart from the problematic practice of returning ailing migrants to Zimbabwe against their will, Mr. Malema's depiction of some of the problems the small facility faces makes clear that individual hospitals who happen to be placed in migrant-heavy areas cannot shoulder the challenge of equitable access alone. Musina Hospital, like other hospitals with a heavily migrant patient base, needs national and provincial leadership and coordination, expert assistance, and financial resources to treat its high risk, mobile patient population. At the same time, these hospitals should not be obliged—or permitted—to unilaterally pursue a policy of balancing their budgets by overcharging destitute migrants in contravention of DOH policy.
DHA's backlog of asylum cases is also a critical part of the problem. The resulting long wait time for asylum seeker permits, asylum adjudication, and processing of applications for citizenship mean that legally present migrants in South Africa are provided a lower standard of health care than citizens for many years longer than they could be.
The legal basis for refusing advanced care to refugees that would be available to citizens also remains unclear. Section 27 of the South African Constitution provides for refugees to receive “the same basic health care and basic education to which inhabitants of the Republic receive from time to time.” Without clearer safeguards in law and public policy on the limits of the “basic” care which must be provided equally to refugees and citizens, the practice of denying advanced care to refugees may continue to revolve around a purely nationality-based calculus.
In Soobramoney v Minister of Health,[225] the Constitutional Court accepted the cost-benefit calculus that denied Mr. Soobramoney life-saving dialysis because it was based on rational and non-discriminatory principles (i.e., when there are more potential dialysis patients than available machines, prioritize patients who are likeliest to survive their organ failure). In the case of South Africa’s migrant community, there is little transparency and consistency in the decisions about whether to allow refugees affordable secondary and tertiary care. This raises real constitutional questions about how and when health expenditures may be constrained by denying life-saving treatment to non-citizens.
Legal Rights
South Africa's failure to ensure access to health care for non-citizens, including asylum seekers and refugees, violates its duties under international as well as domestic law. As earlier noted, the South African Constitution requires that, whenever reasonable, the Bill of Rights and domestic legislation should be interpreted in consistency with both binding and non-binding international law.
Domestic Law
Section 27 of the South African Constitution provides that,
I. Everyone has the right to have access to:
a. health care services, including reproductive health care;
b. sufficient food and water; and
c. social security, including, if they are unable to support themselves and their dependents, appropriate social assistance.
II. The state must take reasonable legislative and other measures, within its available resources, to achieve the progressive realisation of each of these rights.
III. No one may be refused emergency medical treatment.
The South African Constitutional Court considered the government’s obligation to fulfill the right to health espoused in section 27 in the seminal case Minister of Health and others v. Treatment Action Campaign and others (hereinafter TAC). The Court in TAC ordered the government
1) to make an approved drug for the prevention of mother-to-child transmission of HIV
2) (PMTCT) available in the public health sector, and
3) to set out a timetable for the roll-out of a national program for PMTCT.
The Court in TAC followed the line of reasoning in its earlier judgment, Government of the Republic of South Africa and others v. Grootboom and others (hereinafter Grootboom), finding that the State had failed to comply with its constitutional obligations to fulfill petitioners’ housing rights.
However, the right to health, like other constitutional rights, is sometimes subject to limitation. The first subsection of section 36, “Limitation of Rights,” in the Constitution reads:
(1) The rights in the Bill of Rights may be limited only in terms of law of general
application to the extent that the limitation is reasonable and justifiable in an open and democratic society based on human dignity, equality and freedom, taking into account all relevant factors, including
a. the nature of the right;
b. the importance of the purpose of the limitation;
c. the nature and extent of the limitation;
d. the relation between the limitation and its purpose; and
e. less restrictive means to achieve the purpose.
Resource constraints, in some circumstances, have been accepted as part of a calculus used to ration health care. At least one Constitutional Court case, Soobramoney v. Minister of Health (hereinafter, Soobramoney) determined that a South African plaintiff was not constitutionally guaranteed access to dialysis treatment where he did not fit the eligibility requirements established by his local clinic.[226] The Court found that for non-emergency care, obligations imposed on the state regarding access to health care are dependent upon the resources available, as stated in sections 27(1) and (2). Because of limited resources the hospital had adopted a policy of admitting only those patients who could be cured within a short period and those with chronic renal failure who were eligible for a kidney transplant.[227] Though the Court found the clinic’s rules to be reasonable and non-discriminatory, it implied that there might be grounds for the challenge of executive policies if such policies were unreasonable or if they were not applied fairly and reasonably.
Whether non-citizens’ right to health may be limited on the basis of their nationality has not been directly considered by the Constitutional Court; however it has upheld certain social and economic rights of non-citizens. In two 2004 cases,[228] of the Court found it unconstitutional to deny permanent residents access to social grants for which they otherwise qualified. However, the Court did not consider whether other non-citizens other than permanent residents should be entitled to access social security nor did it consider whether access to public health care services should be treated in the same way as access to social security. Recently, South African human rights organization Lawyers for Human Rights (LHR) challenged the constitutionality of the exclusion of refugees from government-provided social assistance grants. An interim settlement agreement was reached in March 2006 in which the Government agreed to allow disabled refugees to receive disability grants to the same value as social grants received by South African citizens.[229] However, in practice refugees often find it impossible to actually access the assistance they are guaranteed.[230] There is little if any legal guidance from South African courts indicating circumstances in which the health rights of undocumented migrants may be limited, but any such limitation would have to be justified as consistent with “human dignity, equality and freedom,” and consistent with South Africa’s obligations under international law.
The National Department of Health has taken steps to specifically include asylum seekers and refugees in its strategic planning and regulation. The HIV, AIDS and STI National Strategic Plan for South Africa (2007—2011) (NSP) identifies refugees, asylum seekers and foreign migrants as marginalized groups requiring special policy interventions for HIV prevention, treatment and support. The NSP states in relevant portion:
The disruption of services and support systems caused by conflict or unrest in their home countries means that many refugees have limited information about HIV and AIDS, and they are often not familiar with local services or systems in South Africa. In addition, while their legal status guarantees the right to access HIV-related information and services on the same level as South Africans, barriers such as language, cultural traditions and xenophobia often preclude their ability to access these services. Therefore targeted programmes are necessary to ensure that refugees and asylum seekers have access to information and services- including prevention, care, support and treatment- as an integrated component of the national response to HIV and AIDS.[231]
International Law
South Africa is also party to a number of international and regional treaties that guarantee the right to the highest attainable standard of health and to principles of equality and non-discrimination in the enforcement of rights more generally. These include the International Covenant on Civil and Political Rights (ICCPR), the Convention on the Elimination of Racial Discrimination (CERD), the Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), the Convention on the Rights of the Child (CRC), the African Charter on Human and People's Rights, the African Charter on the Rights and Welfare of the Child.[232]
The Right to Health
The United Nations Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, has stated that asylum seekers and even illegal immigrants should enjoy the right to health: “States are under the obligation to respect the right to health by, inter alia, refraining from denying or limiting equal access for all persons, including prisoners or detainees, minorities, asylum seekers and illegal immigrants, to preventive, curative and palliative health services.”[233]
South Africa has signed, but not ratified, the International Covenant on Economic, Social and Cultural Rights (ICESCR). As a signatory South Africa undertakes not to undermine the object and purpose of the treaty.[234] Furthermore, the South African Constitutional Court has explicitly considered the ICESCR in interpreting the scope of social and economic rights guaranteed by South African Constitution.[235] The ICESCR guarantees the right of everyone to the highest attainable standard of health.[236] The UN Committee on Economic, Social and Cultural Rights (which oversees implementation of the ICESCR) has identified certain core obligations under the right to health which should be implemented immediately.[237] These include: ensuring nondiscriminatory access to health facilities, particularly for vulnerable or marginalized groups; providing essential drugs; ensuring equitable distribution of all health facilities, goods and services; adopting and implementing a national public health strategy and plan of action with clear benchmarks and deadlines; and taking measures to prevent, treat and control epidemic and endemic diseases.[238] The core obligation to prove access to health services on a nondiscriminatory basis, includes four overlapping dimensions of access: non-discrimination, physical accessibility, economic accessibility, and information accessibility.[239] It also states that parties “respect the right to health by…refraining from denying or limiting equal access for all persons, including…asylum seekers and illegal immigrants.”[240]
Articles 23 and 24 of the Convention on the Rights of the Child (CRC), to which South Africa is a party, also recognize the right to health for all children and set out several steps for its realization. Similarly, CEDAW obliges signatory states to adopt adequate measures to guarantee nondiscriminatory access for women to health and medical care, including access to family planning services. It also guarantees adequate maternal and child health care.[241]
The African Charter on Human and Peoples' Rights further guarantees a right to "Enjoy the best attainable state of physical and mental health." It provides that "States Parties to the present charter shall take the necessary measures to protect the health of their people and ensure that they receive medical attention when they are sick.”[242]
By not ensuring nondiscriminatory access to basic health services, South Africa is failing to protect migrants’ right to health.
Non-Discrimination
The Universal Declaration of Human Rights proclaims that “[e]veryone is entitled to all the rights and freedoms set forth in this Declaration, without distinction of any kind, such as race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status.” Additionally, under that Declaration, “[a]ll are equal before the law and are entitled without any discrimination to equal protection of the law.”
The International Covenant on Civil and Political Rights (ICCPR) echoes the UDHR’s proclamations against discrimination. It binds states parties to recognize the rights it guarantees without distinction of any kind, including race, color, sex, language, religion, political or other opinion, national or social origin, property, birth or other status. The International Covenant on Economic, Social and Cultural Rights (ICESCR) includes the same anti-discrimination provision, and as the noted, the ESCR Committee has identified non-discrimination as a core obligation, subject to immediate implementation, not progressive realization.
The UN High Commissioner for Human Rights (OHCHR) has noted that laws that treat citizens and non-citizens differently must serve a legitimate state objective and be proportional to the achievement of that objective.[243] Specifically, the ICCPR permits States to draw distinctions between citizens and non-citizens with respect to two categories of rights: political rights explicitly guaranteed to citizens, and freedom of movement. With regard to political rights, article 25 establishes that “every citizen” shall have the right to participate in public affairs, to vote and hold office, and to have access to public service. Regarding freedom of movement, article 12 (1) grants “the right to liberty of movement and freedom to choose [one’s] residence” only to persons who are “lawfully within the territory of a State”—that is, permitting restrictions on undocumented migrants.[244]
Besides the political rights permitted to be reserved for citizens, almost all the rights in the ICCPR apply to both nationals and non-nationals. The Human Rights Committee which oversees the implementation of the ICCPR has noted that “the general rule is that each one of the rights of the Covenant must be guaranteed without discrimination between citizens and aliens. Aliens receive the benefit of the general requirement of non-discrimination in respect of the rights guaranteed in the Covenant, as provided for in article 2 thereof. This guarantee applies to aliens and citizens alike.”[245]
The general principle of non-discrimination against alien nationals has been affirmed by international documents including the Convention on the Rights of the Child, and the Convention on the Elimination of Racial Discrimination (CERD), and the African Charter. Though CERD does not apply generally to non-citizens, the Committee on the Elimination of Racial Discrimination, the oversight body for CERD, reaffirmed to states-party that no distinctions on grounds of citizenship should "detract in any way from the rights and freedoms recognized and enunciated in particular in the Universal Declaration of Human Rights, the International Covenant on Economic, Social and Cultural Rights and the International Covenant on Civil and Political Rights."[246] Like the Human Rights Committee, the CERD Committee distinguishes between rights that may be confined to citizens, "such as the right to participate in elections, to vote and to stand for elections" and "human rights" which "are, in principle, to be enjoyed by all persons." States parties are under an obligation to guarantee equality between citizens and non-citizens in the enjoyment of these rights to the extent recognized under international law.”[247]
The CERD Committee called on party states to adopt measures that would address both negative and positive rights in health, including to "Remove obstacles that prevent the enjoyment of economic, social and cultural rights by non-citizens, notably in the areas of education, housing, employment and health”[248] and by "Ensur[ing] that states respect the right of non-citizens to an adequate standard of physical and mental health, by, inter alia, refraining from denying or limiting their access to preventive, curative and palliative health services."[249] It also calls on parties to “take into consideration that in some cases denial of citizenship for long-term or permanent residents could result in creating disadvantage for them in access to employment and social benefits, in violation of the Convention's anti-discrimination principles.”[250]
The 1951 Convention and its 1967 Protocol Relating to the Status of Refugees (hereinafter, Refugee Convention),[251] to which South Africa is party, states that: "refugees shall be accorded the same treatment" as nationals in relation to maternity, sickness, disability and old age.” Article 20 states that: “Where a rationing system exists, which applies to the population at large and regulates the general distribution of products in short supply, refugees shall be accorded the same treatment as nationals.” This provision covers essential medicines and services, and maintains that discrimination on the basis of national origin is not an acceptable basis for denying basic needs. Article 23 requires contracting states to “accord to refugees lawfully staying in their territory the same treatment with respect to public relief and assistance as is accorded to their nationals.”
The United Nations High Commissioner for Human Rights has opined that “[s]tates must avoid different standards of treatment with regard to citizens and non-citizens that might lead to the unequal enjoyment of economic, social and cultural rights. Governments shall take progressive measures to the extent of their available resources to protect the rights of everyone—regardless of citizenship—to: social security; an adequate standard of living including adequate food, clothing, housing, and the continuous improvement of living conditions; the enjoyment of the highest attainable standard of physical and mental health; and education.”[252]
South Africa is obliged to ensure non-discriminatory access to health care for non-citizens under both the right to health and the principle of non-discrimination in its international treaty obligations, as well as its specific duties under domestic law.
Recommendations
To realize the right to health promised by South Africa’s Constitution and under international law, the government of South Africa needs to take active steps to ensure equal treatment for migrants. Limited resources are a genuine, day-to-day reality for the government as well as many health professionals and policymakers. But they cannot be used to justify prima facie discrimination against non-citizens in the provision of health care. Many of the recommendations below can be executed relatively quickly and at minimal cost.
To the South African Human Rights Commission
- Designate a properly staffed and resourced desk to monitor provincial, district and facility-level compliance with DOH and constitutional mandates on health care access for asylum seekers, refugees and other migrants.
To the South African Department of Health
- End discrimination and enforce migrants’ rights in healthcare settings, by:
- Improving reporting and accountability structures within facilities, districts, and provinces.
- Amending existing literature and public postings regarding patient rights to include the rights of non-citizens. Include contact information and advice on how to report allegations of mistreatment, and translations of literature and public postings.
- Requiring that all denials of treatment in public health facilities are accompanied by a form containing the name of the person taking the decision and the reason why treatment was not provided.
- Ensuring that referrals to appropriate health facilities are provided in writing.
- Conducting mandatory, ongoing training for healthcare staff on migrants’ rights, xenophobia, and working with culturally diverse patients.
- Explicitly guarantee health rights equal to those of asylum seekers and refugees for Zimbabwean migrants eligible for status under the special dispensation program, by:
- Informing all DOH provincial and local departments that Zimbabweans with special dispensation are guaranteed access to health care.
- Providing training for frontline health care staff and managers on special exemption status and its attendant right to health access.
- Monitoring compliance of individual healthcare facilities, especially those with a high volume of Zimbabwean patients, and developing accountability mechanisms for acts of discrimination by health workers.
- Provide basic health information rights in the languages of the main migrant communities. In addition, consider:
- Recruiting foreign national or multilingual healthcare workers to staff facilities in migrant-heavy areas.
- Developing a network of community-based interpreters among members of the main migrant communities
- Designating funding for professional interpreters at high-burden migrant facilities, or a telephonic interpretation service.
- Producing multilingual literature about health risks and rights, distributing it to migrant communities and making it available at all health clinics and hospitals, especially those known to serve non-citizen patients.
- Conduct pro-active health surveillance, testing, and treatment in at-risk communities, including non-citizen and undocumented ones.
- Facilitate access to life-saving care for mobile, migrant, at risk, and other vulnerable communities by:
- Allowing rape victims to access the full range of appropriate post-rape care whether or not they choose to report the assault to police.
- Leaving the return of non-nationals to their home countries to the DHA and agencies charged with protections for asylum seekers and refugees.
- Clarify and promote the health rights of undocumented migrants from southern Africa, by:
- Affirming in public education programs that undocumented migrants from the Southern African Development Community (SADC) are eligible for basic and emergency care according to the “partially- subsidized” means test.
- Affirming to both frontline and management staff that undocumented migrants are eligible for free testing and treatment for communicable diseases including HIV, TB, cholera, and malaria.
- Including modules on the rights of the undocumented migrants when training healthcare staff.
- Create systems to ensure that impoverished refugees and asylum seekers qualify for full subsidies for healthcare. One option would be to widen the range of documents that can be used to demonstrate that someone is impoverished and can receive a full subsidy for their health care. For example, allowing asylum seekers and refugees to produce evidence from UNHCR and its local partners that they were receiving chronic illness or disability stipends or evidence of total reliance on charity or humanitarian assistance.
- Clarify and improve health budget allocations by:
- Making it available to the public so that it can be seen to be calculated based on identified priorities, and flexible enough to respond to emerging needs.
- Building in clear allocations for non-citizen, migrant and mobile populations when planning for health services.
- Promote treatment success for mobile and migrant populations, by:
- Training healthcare staff in the treatment needs of migrant and mobile populations, and formally incorporating guidelines for the treatment of such populations, developed by UNHCR and the Southern African HIV Clinicians Society into National Department of Health ART Guidelines.
- Developing cross-border and regional ART and TB treatment initiatives with other southern African governments.
- Ensuring that deported migrants have access to essential medicines throughout their detention in South Africa and upon deportation.
- Develop operational partnerships with NGOs providing care to migrants; this may help improve (and reduce the cost of) staff training and capacity. The community-based MDR-TB treatment program in Khyelitsha, a joint partnership between the city of Cape Town (sub district of Khayelitsha) and MSF is one example. This program aims eventually to be run entirely by local DOH.
To the South African Department of Home Affairs
- Ensure that asylum seekers, refugees, and Zimbabwean migrants are not subject to arbitrary or illegal arrest, detention and deportation, by:
- Halting the arbitrary deportation of undocumented and documented asylum seekers.
- Implementing the “special dispensation” permit for Zimbabweans without further delay.
- Liaising with border hospitals, health officials and health clinics to ensure that ill or injured asylum seekers and refugees are not refouled.
- Involve asylum seeker and refugee communities in decisions and policy making by:
- Setting up consultative groups in migrant communities on housing planning and responding to emerging crises.
- Actively recruiting migrants to help communicate policies and procedures in migrant languages and in a culturally-relevant manner.
- Improve the efficiency of services and procedures and ensuring rights protection, by:
- Reducing waiting times for asylum seeker permits, interviews, appeals, and citizenship without reducing due process safeguards.
- Promoting information campaigns so that more migrants can understand and benefit from their unambiguous health rights.
- Ensure asylum seekers' safety while queuing at Refugee Reception Offices, by:
- Providing tents and other adequate protection from the elements.
- Providing accessible clean water and toilets.
- Ensuring that those awaiting documentation are protected from arbitrary deportation.
To the South African Department of Social Development
- Facilitate the implementation of a disability grant to refugees.
- Invite civil society groups and municipalities to develop transitional and long term housing options for homeless asylum seekers and refugees.
To the South African Government
- Adopt the SADC Policy Framework for Population Mobility and Communicable Diseases.
- Amend the Criminal Law (Sexual Offences and Related Matters) Amendment Act, 2007 to remove section 28 (2) which requires that a rape be reported before PEP services can be provided.
To the South African Police Service
- Improve policing of the Zimbabwean/South African border to protect border crossers as well as South African border communities.
- Maintain sanitary and legal conditions of confinement at SAPS-run detention centers and ensure that detainees have access to health care.
- Develop programs to support witnesses in lodging police files and cooperating with investigations. Provide waivers of deportation for cooperating witnesses and victims, including rape victims.
- Fully and aggressively investigate crimes targeting citizens and non-citizens alike.
Protect migrant and refugee communities from xenophobic violence.
Acknowledgments
This report was written by Rebecca Shaeffer, Kroll Family Human Rights Fellow at Human Rights Watch. It is based on research by the author, and by Diederik Lohman, senior researcher, and Megan McLemore, researcher, both for the Health and Human Rights division. The report was edited by Joseph Amon, director, and Rebecca Schleifer, advocacy director of the division. Aisling Reidy, senior legal advisor, and Iain Levine, Program director, also reviewed the report. Bill Frelick, director, and Gerry Simpson, researcher and advocate for the Refugees Division; Liesl Gerntholtz, director of the Women’s Rights Division; and Sipho Mthathi, South Africa office director; also provided input and comments on portions of the report. Mignon Lamia, associate in the Health and Human Rights division, and Dahlia El Zein, Program coordinator, provided editing assistance. Production assistance was provided by Mignon Lamia, Dahlia El Zein, Grace Choi, and Fitzroy Hepkins.
We would like to thank the many community-based, national and international organizations, volunteers, advocates, and health workers who assisted with this work. Human Watch is particularly grateful to Medecins Sans Frontiers, Sabelo Sibanda of Lawyers for Human Rights, Mohammad Hassan of the International Organization for Migration, Duncan Breen of the Consortium for Refugees and Migrants in South Africa, Jo Vearey of the Forced Migration Studies Programme of the University of the Witswatersrand, Blaise Nzuzi of Jesuit Refugee Services, and Pastor Kwangwari of Concern Zim, for their expertise and assistance. Above all, thanks are due to the migrants who shared their experiences with us.
Annex 1: Email Correspondence with the Department of Health, Republic of South Africa
[1]The most recent census, from 2001, reported 687,678 migrants from SADC countries; 228,318 from Europe; 41,817 from the rest of Africa and 40,889 from Asia.
[2]Department of Social Development, Republic of South Africa,“Towards a 10-year review of the population policy implementation in south africa (1998-2008),” March 2009.
[3] Migration and Remittances Team, Development Prospects Group, World Bank, “Migration and Remittances Factbook, South Africa," March 2008, http://siteresources.worldbank.org/INTPROSPECTS/Resources/334934-1199807908806/SouthAfrica.pdf (accessed November 23, 2009).
[4]Reliable numbers of undocumented migrants are difficult, if not impossible, to obtain, as a result of their frequently clandestine entry and residence. Estimates have varied wildly; a government-commissioned study by the Human Science Resource Council estimated that there were between 4-8 million undocumented migrants in South Africa. The HSRC has since retracted this number, but highly exaggerated numbers of undocumented migrants in particular and the foreign-born in general, continue to circulate in the press and official statements. According to the 2007 Community Survey, a national representative survey conducted by StatsSA, the total number of foreign-born residents is just over 1.2 million or 2.79 percent of the total population, far more than the number of known foreign born residents with legal status. Sharp increases in the number of deportations, starting in 2005, may indicate rising numbers of undocumented migrants.
[5] Immigration Act, 2002 (Act No. 13 of 2002) S.32(2), http://www.acts.co.za/immigration/immigration,_2002.htm#immigration_act_2002.htm (Accessed November 23 2009).
[6]The number of Zimbabweans in South Africa is unknown and contested, with estimates ranging from 1 million to 3 million or more. In 2008, Human Rights Watch estimated that between 1 and 1.5 million Zimbabweans lived in South Africa. (See Human Rights Watch, Zimbabwe—Neighbors in Need: Zimbabweans Seeking Refuge in South Africa, June 2008, http://www.hrw.org/en/reports/2008/06/18/neighbors-need-0, p. 23; In its most recent annual report from June 2009, the Consortium for Refugees and Migrants in South Africa (CoRMSA) stated that there were at maximum 1.5 million Zimbabweans in South Africa. Consortium on refugees and migrants in South Africa (CoRMSA) 11 June 2009 "Protecting Refugees, Asylum Seekers and Immigrants in South Africa 2009" “Protecting Refugees, Asylum Seekers and Immigrants in South Africa,” June 19, 2008, http://www.cormsa.org.za/wp-content/uploads/Resources/CoRMSA%20Report%202009%20-%20Protecting%20Refugees,%20Asylum%20Seekers%20and%20Immigrants%20in%20South%20Africa.pdf (accessed November 23, 2009).
[7]United States Committee on Refugees and Immigrants (USCRI), “2009 World Refugee Survey, South Africa Country Update,” http://www.refugees.org/countryreports.aspx?id=2343 (accessed November 23, 2009).
[8]Besides asylum seekers and undocumented migrants, other Zimbabweans travel to South Africa legally as students, skilled workers, academics, and agricultural and mining work. Consortium for Refugees and Immigrants in South Africa (CoRMSA), Migration Policy Brief 1, "Regularising Zimbabwean Migration to South Africa," May 2009, http://www.cormsa.org.za/migration-policy-briefs/ (accessed November 23, 2009).
[9]USCRI, “2009 World Refugee Survey.”
[10]See for example Human Rights Watch, Unprotected Migrants: Zimbabweans in South Africa’s Limpopo Province, August 2006, vol. 18, no. 6(A), July 2006, http://hrw.org/reports/2006/southafrica0806/, pp.10-11; and Human Rights Watch, Keep Your Head Down: Unprotected Migrants in South Africa, vol. 19, no. 3(A), February 2007 http://hrw.org/reports/2007/southafrica0207/, and Human Rights Watch, Neighbors in Need.
[11]For more information on political, economic and related crises in Zimbabwe, see, Human Rights Watch reports: All Over Again, Human Rights Abuses and Flawed Electoral Conditions in Zimbabwe’s Coming General Elections, vol. 20, no. 2(A), March 2008, http://www.hrw.org/reports/2008/zimbabwe0308/; A Call to Action: the Crisis in Zimbabwe, August 2007, http://hrw.org/backgrounder/africa/zimbabwe0807/; You Will be Thoroughly Beaten, vol. 18,no. 10(A), November 2006, http://www.hrw.org/reports/2006/zimbabwe1106/; ‘Bullets for Each of You’: State-Sponsored Violence since Zimbabwe’s March 29 Elections, June 9, 2008, http://hrw.org/reports/2008/zimbabwe0608/; Bashing Dissent: Escalating Violence and State Repression in Zimbabwe, vol. 19, no. 6(A), May 2007, http://hrw.org/reports/2007/zimbabwe0507/; and Human Rights Watch Oral Submission to the 41st Ordinary Session of the African Commission on Human and Peoples’ Rights on the Human Rights Situation in Zimbabwe, August 2007, http://hrw.org/english/docs/2007/05/18/zimbab15968.htm.
[12]“Zimbabweans to be given special permit,” The Star, April 3, 2009, http://thestar.co.za/index.php?fArticleId=4919258 (accessed September 4, 2009).
[13]Immigration Act, 2002, S.32(2).
[14] Ibid., S.9(4).
[15]“[N]o proceedings may be instituted or continued against any person in respect of his or her unlawful entry into or presence within the Republic if… such person has applied for asylum… until a decision has been made on the application,” Refugee Act, 1998 (Act No. 130 of 1998), www.info.gov.za/view/DownloadFileAction?id=70666 (Acessed November 23, 2009) S.21(4).
[16]Ibid.
[17]See Forced Migration Studies Program, University of Witswatersrand (FMSP), "National Survey of the refugee reception and status determination system in South Africa," February 2009, http://cormsa.org.za/wpcontent/uploads/Research/Asylum/FMSPMRMPRefugeeReceptionReport.pdf (accessed November 23 2009) p.25.
[18] See Ibid. p.25. Survey showed that only 37% of asylum seekers knew about the possibility of asylum before fleeing to South Africa.
[19]The relevant portion of the Refugee Act states, “any person who entered the Republic and is encountered in violation of the Aliens Control Act, who has not submitted an application [for asylum at one of the Refugee reception Offices], but indicates an intention to apply for asylum shall be issued with a… permit valid for 14 days within which [time] they must approach a Refugee Reception Office to complete an asylum application." This section reflects conformity with Article 31 of the 1951 Refugee Convention, which prohibits states from penalizing refugees for entering their territory without passing through official border points. Refugee Regulations No. R366, reg. 2.2.
[20]See for example Consortium for Refugees and Migrants in South Africa (CoRMSA), “Protecting Refugees, Asylum Seekers, and Immigrants in South Africa,” June 2009, http://www.cormsa.org.za/wp-content/uploads/Resources/CoRMSA%20Report%202009%20-%20Protecting%20Refugees,%20Asylum%20Seekers%20and%20Immigrants%20in%20South%20Africa.pdf (accessed November 23, 2009) p.62; see also Lawyers for Human Rights, “Court Declares Home Affairs Actions in Deporting Asylum Seeker as Unlawful and Unconstitutional” http://www.lhr.org.za/news/2009/court-declares-home-affairs-actions-in-deporting-asylum-seeker-as-unlawful-and-unconstitut.
[21]South Africa Department of Home Affairs, Annual Report 2007-2008, http://www.info.gov.za/view/DownloadFileAction?id=91004 (accessed November 23, 2009).
[22] See for example Lawyers for Human Rights, “Court Declares Home Affairs Actions in Deporting Asylum Seeker as Unlawful and Unconstitutional,” press release from May 2009, http://www.lhr.org.za/news/2009/court-declares-home-affairs-actions-in-deporting-asylum-seeker-as-unlawful-and-unconstitut (accessed September 10, 2009).
[23] Human Rights Watch phone conversation with Sabelo Sibanda, Lawyers for Human Rights, Musina, September 10, 2009.
[24] Lawyers for Human Rights, “LHR Asks Court to Stop Illegal Detentions at Zimbabwe Border,” March 23, 2009, http://www.lhr.org.za/news/2009/lawyers-for-human-rights-asks-court-to-stop-illegal-detentions-at-zimbabwe-border; see also Global Detention Monitoring Project, “South Africa Detention Profile,“ http://www.globaldetentionproject.org/de/countries/africa/south-africa/introduction.html (accessed September 12, 2009).
[25]FMSP, “National Survey of refugee reception,” p.25.
[26]See for example, “Protecting Refugees, Asylum Seekers and Immigrants in South Africa,” p. 63, documenting repeated incidences of arrests of asylum seekers on their way back from queuing to renew their asylum seeker permit, due process violations that fail to permit arrested asylum seekers to produce evidence of their legal status, etc.
[27]In the case of the Musina RRO, advocates estimated that between 4 and 9,000 asylum seekers queued outside the Home Affairs office at the height in December 2008. Crowds of several thousand were common. Human Rights Watch interviews with Mohammad Hassan, IOM, March 31, 2009 and Tonde, nurse, MSF, March 30, 3009; Human Rights Watch phone interview with Sabelo Sibanda, Lawyers for Human Rights, April 1, 2009. Lawyers for Human Rights counted asylum seekers sleeping outside the Marabastad RRO in Pretoria and found nightly crowds of 80-300 people, see Lawyers for Human Rights, “A Foot in the Door: Access to Asylum in South Africa,” August 2008, p.4.
[28] FMSP, “National Survey of refugee reception,” p. 9.
[29] Human Rights Watch interview with Hassan, Musina, November 13, 2008.
[30]FMSP, “National Survey of refugee reception.”
[31]Human Rights Watch interview with Sefu, Johannesburg, November 21, 2008.
[32]Human Rights Watch, “South Africa, End Strain on Asylum System,” News Release, January 2009, http://www.hrw.org/en/news/2009/01/08/south-africa-end-strain-asylum-system-and-protect-zimbabweans.
[33] Human Rights Watch, Neighbors in Need, p. 90.
[34] “FMSP, “National Survey of refugee reception,” p. 7.
[35]Human rights Watch, Neighbors in Need, p. 90.
[36] Ibid., p. 90.
[37] Ibid., p. 91.
[38] Ibid., p. 92.
[39]Iggleston, Vicky, FMSP, “Xenophobic Violence in South Africa in May 2008: Humanitarian Responses in Gauteng and Western Cape: A Narrative Account,” February 2, 2009, http://www.migration.org.za/report/humanitarian-assistance-internally-displaced-persons-south-africa-lessons-learned-following-a (accessed November 23, 2009) p.6.
[40] See for example, Amnesty International, “Talk for Us Please: Limited Options Facing Individuals Displaced by Xenophobic Violence,”September 12, 2008, http://www.amnesty.org/en/library/asset/AFR53/012/2008/en/a710b149-830f-11dd-8e5e-43ea85d15a69/afr530122008en.html (accessed November 21, 2009).
[41] DHA officials told camp residents the process of applying for the exemption was compulsory, and that DHA forms stated that by signing for the exemption, displaced people revoked any other rights. In some instances, IDPS were arrested, detained, and subject to coercive attempts to revoke legal status and deport for failing to register. See Amnesty International, “Talk for Us Please,” pp. 11 and 18-19 for account of the best- known arrest of displaced people, a group of whom were arrested and removed from Glenanda Rifle Range displaced-persons camp. Police later induced them under interrogation to renounce their asylum seeker or refugee status.
[42] Human Rights Watch interview with Pimbi Blaise Nzuzi, Medical Program Coordinator, Jesuit Refugee Services (JRS), Johannesburg, October 2008.
[43] Amnesty International, “Talk for Us Please,” p. 13.
[44]Ibid. p. 14.
[45]Ibid. p. 15.
[46]Human Rights Watch interview with Stephen, Bluewaters Camp, Cape Town, November 17, 2008.
[47] Constitution of the Republic of South Africa, 1996, http://www.info.gov.za/documents/constitution/index.htm (accessed November 23, 2009) section 39.
[48] S v. Makwanyana and Another. para. 35 [1995] CCT 3/94 (S. Afr.) http://www.concourt.gov.za/files/deathsn/makwanyane.pdf.
[49] As is discussed in more detail in the “User Fees” section, undocumented migrants are also eligible for some fee exemptions in the DOH fee schedule policy, suggesting that the right to health care is not limited only to documented asylum seekers and refugees.
[50]Jo Vearey, "Ensuring migrant rights to health, Assessing Non-Citizen Access to ART," presentation at the Witswatersrand School of Public Health Academic Meeting, May 16, 2008, in “Challenges to the successful implementation of policy to protect the right of access to health for all in South Africa," Report to Dr Patrick Maduna, Chief of Services: Gauteng Department of Health, June 3, 2008, http://migration.org.za/uploads/docs/MigrantGautengDoH.pdf (accessed November 23 2009).
[51]Memorandum from Department of Health to Provincial HAST Managers, Provincial CCMT Managers, February 2, 2007, http://migration.org.za/uploads/docs/MigrantGautengDoH.pdf (accessed November 23 2009).
[52]Directive, Department of Health, Republic of South Africa, "Rights and Obligations of Refugees,” September 2007, http://migration.org.za/uploads/docs/MigrantGautengDoH.pdf (accessed November 23 2009).
[53]Treatment Action Campaign (TAC) and AIDS Law Project (ALP) Joint Submission to the South African National AIDS Council (SANAC) Plenary, "Vulnerable groups: Refugees, asylum seekers, and undocumented persons—‘The health situation of vulnerable groups in SAm'" March 4, 2008.
[54] Crush, Jonathon and Wade Pendleton, “Regionalizing Xenophobia? Citizen Attitudes to Immigration and Refugee Policy,”2004, p. 14, Table 9.
[55] United Nations Office for the Coordination of Humanitarian Affairs (OCHA), Regional cholera update No.9, April 19, 2009, http://ochaonline.un.org/rosa/HumanitarianSituations/CholeraUpdate/tabid/5122/language/en-US/Default.aspx.
[56] Jo Vearey, at “Foreign Migrants and the South African Health Care System: Ensuring the Right to Health is Upheld for All,” panel discussion, June 23, 2008, https://www.cormsa.org.za/wp-content/uploads/Research/Access/ForeignMigrants.pdf (accessed November 21, 2009).
[57]International Organization for Migration (IOM), “Migrants’ Needs and Vulnerabilities in the Limpopo Province, Republic of South Africa Report on Phase Two February - March 2009,” April 2009 http://iom.org.za/site/index.php?option=com_docman&task=doc_download&gid=138&Itemid=50 (accessed November 23, 2009) p. 19.
[58]Human Rights Watch interview with Seloba Phuti, Public Information Officer, Limpopo Provincial Department of Health, April 3, 2009.
[59]Human Rights Watch interview with Agnes, MSF Nurse Johannesburg, November 8, 2008; Human Rights Watch interview with Sara Hjalmarsson, MSF medical focal point Musina, November 14, 2008, Human Rights Watch interview with Tonde, MSF Nurse, Musina Aptil 3, 2009.
[60]Jo Veary, Forced Migration Studies Program, University of Witswatersrand, conducted a study in 2008 that found that 76 percent of migrants in Johannesburg on ART found out their status in South Africa, and have been here for a period of time before becoming sick and testing, see Jo Veary, “Foreign Migrants and the South African Health care System,” 2008.
[61]UNAIDS Fact Sheet, South Africa, 2008, http://www.unaids.org/en/CountryResponses/Countries/south_africa.asp (accessed November 23, 2009)..
[62]Ibid.
[63] WHO, UNAIDS, and UNICEF, “Epidemiological Fact Sheet on HIV and AIDS, 2008 Update,” http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_ZA.pdf (accessed August 30, 2009).
[64] South African Department of Health, “2008 National Antenatal Sentinel HIV and Syphilis Prevalence Survey,” September 2009, http://www.doh.gov.za/docs/nassps-f.html (accessed Nov. 21 2009).
[65]Speech by the Minister of Health Ms. Barbara Hogan at the HIV Vaccine Research Conference: Cape Town, October 13, 2008, http://www.tac.org.za/community/node/2421 (accessed November 23 2009).
[66]"Barbara Hogan closes a clear the air Conference" IRIN News, April 3, 2009, http://www.irinnews.org/report.aspx?ReportId=83779 (accessed June 1 2, 2009).
[67]The National Strategic Plan for Tuberculosis Control 2007 –2011 sets a goal of 80 percent treatment success by 2011, see Department of Health, Republic of South Africa, “National Strategic Plan for Tuberculosis Control, 2007-2011,” www.info.gov.za/view/DownloadFileAction?id=72544 (accessed November 23 2009).
[68]AIDS and Rights Alliance of Southern Africa (ARASA), “The mining sector, tuberculosis and migrant labour in southern Africa,” July 2008, (accessed April 30, 2009).
[69]See for example, “Migrants with MDR-TB in southern Africa being dumped off at borders without referrals to care,” AIDSMap, October 31, 2008, .
[70]World Health Organization, “Global, National efforts must be urgently intensified to control Zimbabwe cholera outbreak,” January 30, 2009, http://www.who.int/mediacentre/news/releases/2009/cholera_zim_20090130/en/index.html (accessed May 20, 2009).
[71] World Health Organization website, “About Cholera,” page, (accessed May 20, 2009).
[72]World Health Organization Regional Office for Africa, "Cholera Outbreak Control Measures at Community Level," fact sheet, July 17, 2001, http://afro.who.int/emc/cholera.html (accessed November 23, 2009).
[73] Statement by Minister of Health Barbara Hogan on the outbreak of cholera in Zimbabwe and South Africa, November 26, 2008, http://www.info.gov.za/speeches/2008/08112711451003.htm (accessed November 23 2009).
[74]This is largely based on data from the Seventh National Data Survey of Crime Trends and Operations of Criminal Justice Systems covering the period of 1998-2000. Newer numbers may reflect an overall dropping rate of violent crime in South Africa). See also Centre for the Study of Violence and Reconciliation, “The Violent Nature of Crime in South Africa,” June 25, 2007, p. 54, www.info.gov.za/issues/crime/violent_crime.pdf (accessed November 21, 2009).
[75]Loren B Landau and Karen Johnson, "Refugees in the new Johannesburg," Forced Migration Review, vol.19, p. 44, www.fmreview.org/FMRpdfs/FMR19/FMR1920.pdf (accessed November 22, 2009).
[76]Center for the Study of Violence and Reconciliation, “Diversity and Transformation in the South African Police Service,” March 2006, p. 45m www.csvr.org.za/docs/policing/diversity.pdf (accessed August 3, 2009).
[77] “Refugees in the New Johannesburg,” p. 44.
[78] Human Sciences Research Council and Institute for Security Studies, “Public Attitudes Regarding Undocumented Migration and Policing/Crime,” African Security Review , vol. 6 no. 4, 1997, www.iss.co.za/pubs/asr/6No4/HRSC.html (accessed November 22, 2009).
[79]South African Police Service, “Annual Report 2008/2009,” July 2009, http://www.saps.gov.za/saps_profile/strategic_framework/annual_report/index.htm, (accessed November 23, 2009) p.5.
[80]A partial list of attacks against non citizens suspected to have xenophobic motivations can be found in Consortium for Refugees and Migrants in South Africa (CoRMSA), “Protecting Refugees, Asylum Seekers and Immigrants in South Africa,” June 19, 2008, p. 43, http://www.cormsa.org.za/wp-content/uploads/Resources/CoRMSA%20Report%202009%20-%20Protecting%20Refugees,%20Asylum%20Seekers%20and%20Immigrants%20in%20South%20Africa.pdf (accessed November 23, 2009).
[81] Human Rights Watch interview with Said, Akasia Camp, November 8, 2008.
[82]Human Rights Watch interview with Musa, Akasia Camp, November 8, 2008.
[83]Human Rights Watch interview with Ana Clet, African Disabled Refugees Organization, Cape Town, November 19, 2008.
[84] Human Rights Watch interview with Ali, Johannesburg, November 21, 2008.
[85]IOM, “Migrants’ Needs and Vulnerabilities,” p. 3.
[86]Human Rights Watch interview with John, Showgrounds, Musina, March 30, 2009. See also Rutherford, Blair, "Zimbabweans Living in the South African Border-Zone: Negotiating, Suffering, and Surviving," in Concerned Africa Scholars Bulletin No. 80, Winter 2008, p. 7.
[87] CoRMSA, “Protecting Refugees, Asylum Seekers and Immigrants in South Africa,” p. 42.
[88] Ibid.
[89] Human Rights Watch interview with Musa, Akasia Camp, November 8, 2009.
[90]Human Rights Watch interview with Claudius, Musina, March 28, 2009.
[91]Human Rights Watch interview with Arnold, Nancefield, November 12, 2008.
[92]1.2 per 1,000 people , according to United Nations Office on Drugs and Crime, Centre for International Crime Prevention, “Seventh United Nations Survey of Crime Trends and Operations of Criminal Justice Systems, covering the period 1998 – 2000,” March 2004; South Africa Prison System data for 2007-2008 records over 70,500 total “sexual crimes,” an increase over recent years, see “Crime in the RSA,” September 22 2009, http://www.iss.co.za/index.php?link_id=24&slink_id=2489&link_type=12&slink_type=12&tmpl_id=3 (accessed November 22, 2009).
[93]Official website of the South African Police Service (SAPS), http://www.saps.gov.za/statistics/reports/crimestats/2008/march_april_2001_2008/catagory/rape.pdf (accessed May 21, 2009); SAPS notes that in December, 2007, South Africa implemented the revised Sexual Offenses Act, which among other things widens the definition of rape to cover male victims and non-vaginal penetration, and deals differently with child rape, pornography, human trafficking, and prostitution, so recent numbers (not yet released by SAPS, as of November 2009) may be different. There are indications that actual rates of rape are much higher than those reported.
[94]Rachel Jewkes and Naeema Abrahams, Gender and Health Group, Medical Research Council, “The epidemiology of rape and sexual coercion in South Africa: an overview,” October 2002.
[95] One Love, Action for Life, “Multiple and Concurrent Sexual Partners in Zimbabwe,” September 2008, http://www.onelovesouthernafrica.org/wp-content/uploads/2009/01/zimbabwe-mcp-final.pdf (accessed May 5, 2009), p. 14.
[96]Human Rights Watch interview with Thandu, Musina, March 2009.
[97] Department of Justice and Constitutional Development, Republic of South Africa, “National Policy Guidelines for Victims of Sexual Offences,” 1998, http://www.justice.gov.za/policy/guide_sexoff/sex-guide05.html (accessed November 23, 2009).
[98] Official website of the Government of South Africa, information on the National Prosecuting Authority of South Africa, Sexual Offences and community Affairs Unit, http://www.info.gov.za/aboutgovt/justice/npa.htm (accessed November 23, 2009).
[99]Address by Ms Brigitte Mabandla, MP, Minister for Justice and Constitutional Development, at the National Prosecuting Authority’s Stakeholder Conference, Wednesday, 28 March 2007, at Gallagher Estate, Midrand, www.doj.gov.za/m_speeches/sp2007.htm (accessed November 23, 2009) p.2; Invitation to the Women's Justice and Empowerment Initiative (WJEI) launch, March 28, 2009, http://www.info.gov.za/speeches/2009/09033009451001.htm (accessed November 23, 2009).
[100] See for example, Amnesty International, “I am at the lowest end of all: Rural women living with HIV face human rights abuses in South Africa,” March 2008.
[101] International Organization for Migration and CARE, “Mobility and AIDS in Southern Africa: Mobility and HIV/AIDS in Southern Africa: a field study in South Africa, Zimbabwe and Mozambique,” September 2003, p. 6.
[102]Human Rights Watch interview, Theresa, Musina, November 14, 2008.
[103] Human Rights Watch interview with Julia, Musina, November 14, 2008.
[104] Human Rights Watch interview with Constance, Showgrounds, Musina, November 12, 2008.
[105]Human Rights Watch interview with Mildred, Musina, November 14, 2008.
[106]Human Rights Watch interview with Sara Hjalmarsson, Nurse-Medical Focal Point, MSF, Musina, November 12, 2008.
[107]Human Rights Watch interview with Blessing, Musina, March 30, 2009.
[108]Human Rights Watch interview with Jacob Matakanye, CEO, Musina Legal Advice Center, November 12, 2008.
[109]Human Rights Watch interview with Pastor Kwangwari, founder, Concern Zim, Musina November 13, 2009. See also "South African refugee girls get lost," Associated Press, May 28, 2009, http://washingtontimes.com/news/2009/may/28/refugee-girls-get-lost/ (accessed May 27, 2009).
[110] Constitution of the Republic of South Africa (SA Const.), Act No. 108 (1996), ch. 6 (Bill of Rights), sec. 27(1)(b).
[111]Government of the Republic of South Africa and Others vs. Grootboom, www.lrc.org.za/Docs/Judgments/grootboom_cc.pdf (accessed August 17, 2009).
[112] “Violence & Xenophobia in South Africa,” Briefing to the Portfolio Committee of the Parliamentary monitoring Group, November 19, 2008, http://www.pmg.org.za/report/20081119-violence-xenophobia-south-africa-human-sciences-research-council-brie (accessed November 23, 2009). A quick-response survey conducted in the communities in which xenophobic violence arose in the days following the attacks indicated that housing issues were a major trigger for frustration.
[113] Human Rights Watch interview with Charles, Pretoria, November 8, 2008.
[114] “Rooms” at Malas Camp are quasi-private spaces separated by gathered scrap metal and tires.
[115] Human Rights Watch interview with Maria, Pretoria, November 8, 2008.
[116]Human Rights Watch interview with Peter, Pretoria, November 8, 2008.
[117] Human Rights Watch interview with Edmund, Johannesburg, November 21, 2008.
[118] Human Rights Watch interview with Arthur, Johannesburg, November 11, 2008.
[119] Human Rights Watch interview with Alexis Moens, MSF Project Driector, Johannesburg, October 30, 2008.
[120]See Human Rights Watch statement, “South Africa: Ensure Justice for Police Raid Victims,” February 18, 2008, http://www.hrw.org/en/news/2008/02/18/south-africa-ensure-justice-police-raid-victims.
[121]“Refugees Face Eviction from Johannesburg Church Premises,” ZimOnline, March 10, 2009, http://www.reliefweb.int/rw/rwb.nsf/db900sid/MYAI-7PZ53J?OpenDocument (accessed November 23, 2009).
[122]Human Rights Watch interview with Bishop Paul Verryn, Central Methodist Mission Church, Johannesburg, April 5, 2009.
[123]“SA slams arrest of homeless Zimbabweans,” The Sunday Independent, July 4, 2009, http://www.sundayindependent.co.za/?fSectionId=&fArticleId=nw20090704185320106C509851 (accessed November 23, 2009).
[124] Human Rights Watch interview with Evidence, Johannesburg, April 5, 2009.
[125]“No Camps for Zimbabwean refugees,” BBC News, August 24, 2007, http://news.bbc.co.uk/2/hi/africa/6962609.stm “Home Affairs Minister Mrs. Mapisa-Nqakula says building camps is the wrong approach… Mrs. Mapise Nqakula said the government's current policy of integration remains their preferred strategy.” See also Landau, Lauren, “Regional Integration, Protection and Migration Policy Challenges in Southern Africa,” http://ir.iss.nl/eserv.php?pid=iss:158&dsID=Handmaker_03Landau.pdf (accessed August 23, 2009), p. 2.
[126]See Amnesty International, “Talk for Us Please: Limited Options Facing Individuals Displaced by Xenophobic Violence,” September 2008, |outline (accessed November 23, 2009). In October, 2008, Lawyers for Human Rights secured the release of the remaining 37 detainees. See Lawyers for Human Rights, “LHR Secures the Release of 37 Refugees and Asylum-Seekers,” October 21, 2008, (accessed November 23, 2009).
[127]Human Rights Watch interview with Cecelia, Akasia Camp, November 8, 2008.
[128] Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons: Lessons Learned Following Attacks on Foreign Nationals in May 2008,” January 2009, http://www.migration.org.za/sites/default/files/reports/2009/Disaster_Response_Evaluation_FINAL_02.02.09.pdf (accessed November 23, 2009), p.34. See also, “A Health Impact Assessment of international migrants following the xenophobic attacks in Gauteng and Western Cape,” January 2009, Forced Migration Studies Program, University of Witswatersrand, http://programs.ifpri.org/renewal/pdf/JohannesburgHealthImpact.pdf (accessed November 22, 2009).
[129]The Office of the UN High Commissioner for Human Rights, Guiding Principles on Internal Displacement, E/CN.4/1998/53/Add.2, February 11, 1998, principle 19.
[130] Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 73.
[131]Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 72; Human Rights Watch interview with Alexis Moens, MSF Project Driector, Johannesburg, October 30, 2008; Human Rights Watch interview with Sharon Ekambaram, General Director MSF South Africa, Johannesburg, October 30, 2008.
[132]Human Rights Watch interview with Abdi Mohammad, Akasia Camp, November 2008.
[133] Human Rights Watch interview with Agnes, MSF nurse, November 8, 2008.
[134]Human Rights Watch interview with Abraham, Akasia Camp, November 8, 2008.
[135]Jesuit Refugee Service, “South Africa: Child dies in fire at Klerksoord camp,” News Briefing, February 17, 2009, (accessed November 23, 2009).
[136]Jesuit Refugee Service, “South Africa: Refugees Forcibly Evicted,” News Briefing, March 17, 2009, http://www.jrs.net/news/index.php?lang=en&sid=4279 (accessed November 23, 2009).
[137]Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 40.
[138]Human Rights Watch interview with Tracey Saunders and Joanna Peare, volunteer coordinators, Cape Town, November 18, 2008; see also FMSP, “A health impact assessment of international migrants following the xenophobic attacks in Gauteng and the Western Cape,” January 2009, p. 28.
[139]Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 72. See also FMSP, “A health impact assessment of international migrants,” p. 51.
[140] Human Rights Watch interview with Salima, Bluewaters Camp, Cape Town, November 17, 2008.
[141] Despite its “closure,” the showgrounds are still a gathering place for many asylum seekers. Higher efficiency rates at the Musina DHA, together with the practice of facilitating the movement of asylum seekers from Musina to Johannesburg or other urban centers, has relieved conditions at the showgrounds to a certain extent.
[142]Human Rights Watch interview with Jacob Matakanye, CEO, Musina Legal Advice Center, November 13, 2008.
[143] Human Rights Watch interview with Pastor Kwangwari, Concern Zim, Musina, March 30, 2009.
[144] Human Rights Watch interview with Mohammad Hassan, IOM, Musina, March 29, 2009.
[145] SA Const. Sec. 27 (1).
[146] SA Const. Sec. 28.
[147]FMSP, “A health impact assessment of international migrants,” p.23.
[148]Human Rights Watch interview with Helen, Musina, November 13, 2008.
[149]Human Rights Watch interview with Xavier, Musina, November 2008.
[150]Human Rights Watch interview with Abdullahi, Akasia Camp, November 2008.
[151]Human Rights Watch interview with Sara Hjalmarsson, Nurse Medical Focal Point, MSF, November 12, 2008.
[152]Human Rights Watch interview with Bernard, Musina, November 2008.
[153]Human Rights Watch interview with Arnold, Nancefield, November 12, 2008.
[154] Human Rights Watch interview with Alice, Nancefield, November 12, 2008.
[155]Human Rights Watch interview with Pastor Kwangwari, Concern Zim, March 29, 2009.
[156] Human Rights Watch interview with Munashe, Musina, November 13, 2008.
[157] “Johannesburg Health Impact,” p. 24.
[158]Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 23.
[159]Human Rights Watch interview with ex camp manager of Bluewaters, Cape Town, November 18, 2008.
[160]Human Rights Watch phone with Dr. Louis Reynolds, People's Health Movement, Cape Town, November 17, 2008.
[161] “Johannesburg Health Impact,” p. 26.
[162]Forced Migration Studies Programme, University of the Witwatersrand, “Humanitarian Assistance to Internally Displaced Persons,” p. 34.
[163] Ibid p. 34.
[164]Human Rights Watch interview with Ndona, Johannesburg, November 21, 2008.
[165] Human Rights Watch interview with Phillip, Johannesburg, November 21, 2008.
[166]Human Rights Watch interview with Sefu, asylum seeker. Johannesburg, November 21, 2008.
[167]Human Rights Watch interview with Tshonda, founder, African Bureau of HIV/AIDS, Cape Town November 2008.
[168]Human Rights Watch interview with Blaise Nzuzi, Medical Director, Jesuit Refugee Services, Johannesburg October 30, 2008.
[169]South African Human Rights Commission, Public Inquiry: Access to Health Care Services, April 2009, http://sahrc.org.za/sahrc_cms/downloads/Health%20Report%20Final%202009%20Part1.pdf (accessed November 23 2009); CoRMSA, “Protecting Refugees, Asylum Seekers, and Immigrants in South Africa,” p. 38.
[170]Jo Vearey and Ingrid Palmary, “Assessing non-citizen access to antiretroviral therapy in Johannesburg,” May 2008, Forced Migration Studies Program, University of Witswatersrand, Report Summary.
[171]Human Rights Watch interview with Said, Akasia Camp, Pretoria November 2008.
[172]Human Rights Watch interview with Layla, Akasia Camp, Pretoria November 8, 2008.
[173] Human Rights Watch interview with Trevor, Johannesburg November 10, 2008.
[174]Human Rights Watch interview with Said, Akasia Camp, Pretoria November 8, 2008.
[175]Human Rights Watch interview with Pascal Minani, Information Officer, Reproductive Hhealth Research Unit, Johannesburg April 6, 2009.
[176] Human Rights Watch interview with Nilda, Cape Town, November 17, 2008.
[177]Human Rights Watch interview with Kelvin, Johannesburg November 10, 2008.
[178]Human Rights Watch interview with Claudia, Johannesburg November 21, 2008.
[179]Human Rights Watch interviews with Pimbi Blaise Nzuzi, Medical Director, Jesuit Refugee Services and Marcelline Sangara, Nurse, Jesuit Refugee Service, November 21, 2008.
[180]Human Rights Watch interview with Claudia, Johannesburg, April 7, 2009.
[181]Ibid.
[182]Human Rights Watch interview with Tshonda, African Bureau of HIV/STI (NGO), Cape Town, November 17, 2008.
[183]Lorena Nunez, Forced Migration Studies Program, University of Witswatersrand, "Note on unnatural causes of death among migrants," Appendix N. in "Challenges to the successful implementation of policy to protect the right of access to health for all in South Africa: Report to Dr Patrick Maduna Chief of Services: Gauteng Department of Health," June 3, 2008.
[184]Human Rights Watch interview with Edmund, Johannesburg November 10, 2008.
[185]The Promotion of Access to Information Act, 2000 (Act No. 2 of 2000), http://www.acts.co.za/promotion_of_access_to_information_act_2000.htm (accessed November 23 2009).
[186] Human Rights Watch interview with Barbara Ngodwana, Welfare Coordinator, Scalabrini Center, Cape Town, November 17, 2008.
[187] Ibid.
[188] Human Rights Watch phone interviewwith Seloba Phuti, Public Information Officer, Limpopo Province Department of Health. April 7, 2009.
[189]The only project known to Human Rights Watch researchers was a small pilot program providing volunteer interpreters in Cape Town being organized by the Snoke Gender Justice project.
[190]Human Rights Watch interview with Eva, Cape Town, November 18, 2008.
[191]Human Rights Watch interview with Edward Malema, Public Information Officer, Musina Hospital, March 29, 2009.
[192]Human Rights Watch interview with Jo Vearey, Forced Migration Studies Program, University of the Witswatersrand, April 7, 2009. Human Rights Watch interview with Lauren Jankleowitz, Reproductive Health and HIV Research Unit, University of the Witswatersrand, April 8, 2009, Human Rights Watch interview with Tony, refugee, Johannesburg, April 7, 2009.
[193]Human Rights Watch interview with Blaise Nzuzi, Jesuit Refugee Services Health Director, Johannesburg October 31, 2008.
[194]Phone conversation with Gauteng DOH Patient Complaint Line, April 7, 2009.
[195]Human Rights Watch interview with Sara Hjalmarsson, Nurse Medical Focal Point, MSF, Musina, November 2008.
[196]See Human Rights Watch, "Policy Paralysis: A Call for Action on HIV/AIDS-Related Human rights Abuses Against Women and Girls in Africa,” December 2003, http://www.hrw.org/sites/default/files/reports/africa1203.pdf.
[197] Department of Health, Republic of South Africa, National Sexual Assault Policy, Guiding Principles (2005) p. 15.
[198]Human Rights Watch interview with Peggy, SGBV advocate, Musina Legal Advice Centre, November 14, 2008.
[199] Human Rights Watch interview with Clare, Bluewaters, November 18, 2008.
[200]Discussed multiple times in Human Rights Watch interviews with MSF, IOM, and Musina Legal Advice Office.
[201]Human Rights Watch interview with Sara Hjalmarsson, Medical Focal Point MSF Musina November 12, 2008. MSF has since initiated an SGBV clinic in Musina to help address the unmet needs of rape survivors.
[202] Amnesty International, "I am the Lowest End of All: Rural Women living with HIV Face Human Rights Abuses in South Africa," March 18, 2008, http://www.amnesty.org/en/library/asset/AFR53/001/2008/en/ebc94db1-f123-11dc-b3df-0fe44bc152bc/afr530012008eng.pdf (accessed November 23, 2009) p.25.
[203]Human Rights Watch interview with Peggy, SGBV Focal Point, Musina Legal Advice Office, Musina, November 14, 2008.
[204] Phone conversation with Sabelo Sibanda, Lawyers for Human Rights, Musina, August 31, 2009.
[205] Ibid.
[206]IOM, “Migrants’ Needs and Vulnerabilities,” p. 26.
[207]Human Rights Watch interview with Edward Malema, Musina, March 31, 2009.
[208]Ibid.
[209] Pre-natal care is only free for legally present non-citizens, but should be made available on a fee-subsidized basis for undocumented SADC migrants. See South Africa Department of Health, “Explanation of the Current Policy Regarding the Classification of Patients for the Determination of Fees,” June 14, 2002, Table 5.
[210] Ibid., Table 5.
[211]Ibid., (Appendix H), Table 1.
[212]Directive, Department of Health, Republic of South Africa, "Rights and Obligations of Refugees," September 2007, http://migration.org.za/uploads/docs/MigrantGautengDoH.pdf (accessed November 23 2009), p. 11.
[213] Ibid.
[214]Human Rights Watch interview with Pastor Kwangari, Founder, Concern Zim, Musina, March 30, 2009; Human Rights Watch interview with Tonde, nurse, MSF, Musina, March 30, 2009; Human Rights Watch interview with Sara Hjalmarsson, Nurse Focal Point, MSF, Musina, November 12, 2008.
[215]Human Rights Watch interview with Sara Hjalmarsson, Nurse Focal Point, MSF, Musina, November 12, 2008.
[216]Human Rights Watch interview with Arnold, Nancefield, November 13, 2008.
[217] According to South Africa Department of Health, “Explanation of the Current Policy Regarding the Classification of Patients for the Determination of Fees,” Table 5, free services are guaranteed for “a pregnant women for the period commencing from the time the pregnancy is diagnosed to forty-two days after the pregnancy has terminated, or if a complication has developed as result of the pregnancy, until the patient has been cured or the conditions as result of the complication has stabilised.”
[218] Human Rights Watch interview with Cecile, Johannesburg, November 21, 2008.
[219] Human Rights Watch interview with Phillip, Johannesburg, November 21, 2008.
[220] South Africa Department of Health, “Explanation of the Current Policy Regarding the Classification of Patients for the Determination of Fees,” Table 2.
[221] Human Rights Watch interview with Edward Malema, Public Information Officer, Musina Hospital, March 31, 2009.
[222]Ibid.
[223] Ibid.
[224] Ibid.
[225] Soobramoney v Minister of Health (Kwazulu-Natal) (CCT32/97) [1997] ZACC 17; 1998 (1) SA 765 (CC); 1997 (12) BCLR 1696 (27 November 1997), http://www.saflii.org/za/cases/ZACC/1997/17.html (accessed November 23, 2009).
[226] Soobramoney v Minister of Health.
[227] Ibid.
[228] Khosa & Others v Minister of Social Development & Others, and Mahlaule v. Minister of Social Development and others 2004(6) BCLR 569 (CC) Constitutional Court of South Africa, May 4 2004, http://www.escr-net.org/usr_doc/judgement.pdf (accessed November 23, 2009).
[229]Lawyers for Human Rights, “Disabled Refugees Challenge Unfair Exclusion from Social Assistance,” http://www.lhr.org.za/news/2005/disabled-refugees-challenge-unfair-exclusion-social-assistance (accessed September 1, 2009).
[230] In a November 2008 interview with Human Rights Watch, Barbara, Welfare Coordinator, Scalabrini Center, Cape Town, informed HRW that although she believed the government was very close to implementing the first disability grants, none of her qualifying clients had yet been able to access them. See also, CoRMSA, “Protecting Refugees, Asylum Seekers and Immigrants in South Africa,” p. 103.
[231]Department of Health, Republic of South Africa, “HIV & AIDS and STI Strategic Plan for South Africa, 2007-2011,” March 12, 2007, http://www.info.gov.za/otherdocs/2007/aidsplan2007/index.html (accessed November 23 2009), p. 36.
[232]International Covenant on Civil and Political Rights (ICCPR), adopted December 16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 52, U.N. Doc. A/6316 (1966), 999 U.N.T.S. 171, entered into force March 23, 1976, ratified by South Africa December 10, 1998; International Convention on the Elimination of All Forms of Racial Discrimination (ICERD), adopted December 21, 1965, G.A. Res. 2106 (XX), UN Doc A/6014 (1966), entered into force January 4, 1969, ratified by South Africa on December 10, 1998; Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW), adopted December 18, 1979, G.A. Res. 34/180, U.N. Doc. A/34/46, entered into force September 3, 1981, ratified by South Africa on Dcember 15, 1995, Convention on the Rights of the Child, adopted November 20, 1989, G.A. Res. 44/25, U.N. Doc. A/REX/44/25, entered into force September 2, 1990 ratified by South Africa on June 16, 1995; African Charter on Human and Peoples' Rights, adopted June 27, 1981, OAU Doc. CAB/LEG/67/3 rev. 5, entered into force Oct. 21, 1986, ratified by South Africa on July 9, 1996; the African Charter on the Rights and Welfare of the Child, OAU Doc. CAB/LEG/24.9/49 (1990), entered into force Nov. 29, 1999, ratified by South Africa on January 7, 2000.
[233]Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of health, Fact Sheet No. 31 on the Right to Health, http://www2.ohchr.org/english/issues/health/right/ (accessed November 23, 2009).
[234] Vienna Convention on the Law of Treaties 1969, United Nations, Treaty Series, vol. 1155, p. 331, entered into force on January 27, 1980, art. 18.
[235] In “Government of the Republic of South Africa and Others v. Grooboom and Others,” the Constitutional Court relied on the ICESCR as well as the Committee on Economic, Social and Cultural Rights in its discussion of minimum core requirements, quoting an earlier case stating that “public international law would include non-binding as well as binding law….they may both be used…as tools of interpretation,” (Grootboom para. 26, quoting S. Makwanyane and Another at para 35, 1995 (3) SA 391 (CC) 1995 (6), BCLR 665 (CC).)
[236]International Covenant on Economic, Social and Cultural Rights (ICESCR), adopted December
16, 1966, G.A. Res. 2200A (XXI), 21 U.N. GAOR Supp. (No. 16) at 49, U.N. Doc. A/6316 (1966),
993 U.N.T.S. 3, entered into force January 3, 1976, art. 12.
[237] These include: ensuring nondiscriminatory access to health facilities, particularly for vulnerable or marginalized groups; providing essential drugs; ensuring equitable distribution of all health facilities, goods and services, adopting and implementing a national public health strategy and plan of action with clear benchmarks and deadlines; and taking measures to prevent, treat and control epidemic and endemic diseases. The core obligation to prove access to health services on a non discriminatory basis includes four overlapping dimensions of access: non-discrimination, physical accessibility, economic accessibility, and information accessibility. UN Committee on Economic, Social and Cultural Rights, “Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights,” General Comment No. 14, The Right to the Highest Attainable Standard of Health, E/C.12/2000/4 (2000), http://www.unhchr.ch/tbs/doc.nsf/(Symbol)/40d009901358b0e2c1256915005090be?Opendocument (accessed May 11, 2006).
[238] CESCR, General Comment 14, para. 1.
[239]CESCR, General Comment 14, para. 12.
[240] CESCR, General Comment 14, para. 34.
[241]CEDAW Committee, General Recommendation 24, Women and Health (Article 12), Compilation of General Comments and General Recommendations Adopted by Human Rights Treaty Bodies, U.N. Doc. HRI/GEN/1/Rev.6 at 149 (2003), para 2. Article 24.9 also provides that“Assessment of the health status and needs of women in that country take into account any ethnic, regional or community variation or practices based on religion, tradition or culture."
[242]African Charter on Human and Peoples' Rights (Banjul Charter) adopted June 27, 1981, art. 16, http://www1.umn.edu/humanrts/instree/z1afchar.htm (accessed May 30, 2009).
[243] Office of the United Nations High Commissioner for Human Rights, “The Rights of Non-Citizens,” 2006, http://www.ohchr.org/Documents/Publications/noncitizensen.pdf.
[244]“The Rights of Non-Citizens,” p. 8.
[245] UN Human Rights Committee, General Comment 15, The Position of aliens under the Covenant, Compilation of General Comments and General Recommendations Adopted by Human Rights Treaty Bodies, UN Doc.
HRI\GEN\1\Rev.1 (1994), para 4.
[246]CERD Commitee, General Recommendation 30, Discrimination Against Non-Citizens, http://www.unhchr.ch/tbs/doc.nsf/0/e3980a673769e229c1256f8d0057cd3d?Opendocument, para. 2.
[247] Ibid, para 3.
[248] Ibid. para 29.
[249] Ibid. para. 36.
[250]Ibid. para. 15.
[251]Convention relating to the Status of Refugees, 189 U.N.T.S. 150, entered into force April 22,
1954, acceded to by South Africa on January 12, 1996; Protocol Relating to the Status of Refugees, 606 U.N.T.S. 267, entered into force October 4, 1967, acceded to by South Africa on January 12, 1996.
[252] The Office of the High Commissioner for Human Rights, “The Rights of Non-Citizens,” p. 25.