No Tally of the Anguish
Accountability in Maternal Health Care in India
Abbreviations
ANC Antenatal care
ANM Auxiliary Nurse-Midwife
APH Antepartum hemorrhage
ASHA Accredited Social Health Activist
AWW Anganwadi worker
BPL Below poverty line
CEDAW Convention on the Elimination of All Forms of Discrimination Against Women
CESCR UN Committee on Economic, Social and Cultural Rights
CHC Community health center
CMO Chief medical officer
CRC Convention on the Rights of the Child
CSSM Child Survival and Safe Motherhood forms
DLHS District Level Household and Facility Survey
FIGO International Federation of Gynecology and Obstetrics
FOGSI Federation of Obstetric and Gynecological Societies of India
FRU First referral unit
HMIS Health Management Information System
HSC Health sub-center
ICCPR International Covenant on Civil and Political Rights
ICESCR International Covenant on Economic, Social and Cultural Rights
ICM International Confederation of Midwives
IFA Iron and folic acid
IMA Indian Medical Association
JSYJanani Suraksha Yojana, literally Motherhood Protection Scheme
MAPEDIR Maternal and perinatal death inquiry and response
MCH Maternal and child health
MDGs Millennium Development Goals
MMR Maternal mortality ratio
MMWG Maternal Mortality Working Group
MOIC Medical officer-in charge
NFHS National Family and Health Survey
NRHM National Rural Health Mission
PHC Primary health center
PNC Postnatal care
PPH Post-partum hemorrhage
RCH Reproductive and child health (program)
RKSRogi Kalyan Samitis, or Patient Welfare Committees
SHC Sub-health center
SR Special Rapporteur
SRS Sample Registration System
UN United Nations
UNFPA United Nations Population Fund
UNICEFUnited Nations Children's Fund
UP Uttar Pradesh state
USAID United States Agency for International Development
WHO World Health Organization
Glossary
Accredited Social Health Activist |
A female health worker appointed under the National Rural Health Mission |
Anganwadi |
Government-run early childhood care and education center. Anganwadi workers' duties include providing nutritional supplements to pregnant and lactating mothers |
Antenatal care |
Care during pregnancy (termed "prenatal care" in American English) |
Antepartum hemorrhage |
Bleeding during pregnancy |
Auxiliary Nurse-Midwife |
A field based health worker usually posted in health sub-centers and primary health centers |
Basic obstetric care |
Obstetric care that includes the ability to conduct normal and assisted deliveries, and manage pregnancy complications by intravenously introducing or injecting anticonvulsants, oxytocic drugs (drugs that expand the cervix or vagina to facilitate delivery), and antibiotics |
Block |
Administrative division of a district |
Chief medical officer |
Highest district level health official in Uttar Pradesh; the equivalent in Tamil Nadu is the deputy director of health services |
Community health center |
Thirty-bed government health facilities in rural India providing secondary health care |
Dalit |
So-called "untouchables," traditionally considered outcastes in India |
District |
Administrative division of a state |
District Level Household and Facility Survey |
A periodic all-India survey conducted under the World Bank funded RCH-II program |
Eclampsia |
Pregnancy complication characterized by seizures or coma |
Emergency obstetric care |
Obstetric care that includes the ability to provide life-saving interventions through surgery (cesarean sections) and blood transfusions |
First referral unit |
A government health facility in India that should be equipped with comprehensive emergency obstetric care facilities and serves as the first hospital in the referral chain when health complications arise that cannot be dealt with at lower-level facilities |
Gram Panchayat |
Literally meaning "assembly of five," a term used to refer to the village-level councils of elected government representatives |
Gram Sabhas |
A cluster of villages governed by a village council |
Gram Vikas Adhikari |
Village development officer |
Janani Suraksha Yojana |
Literally Motherhood Protection Scheme, an NRHM scheme that promotes facility-based deliveries through cash incentives for pregnant women and community-based female health volunteers |
Maternal death |
Death during pregnancy or within 42 days of childbirth or abortion, caused directly or indirectly by pregnancy |
Maternal mortality ratio |
Number of maternal deaths per 100,000 live births |
Maternal Mortality Working Group |
Comprised of the WHO, UNICEF, UNFPA, the UN Population Division, and the World Bank, as well as several outside technical experts |
Millennium Development Goals |
Eight goals that 189 countries have pledged to achieve by 2015, including a 75 percent maternal mortality reduction compared to its 1990 levels (MDG 5) |
National Family and Health Survey |
A periodic all-India sample survey funded by the Indian government and international agencies |
National Rural Health Mission |
The Indian government's flagship program on rural health care for the period 2005-2012 |
Obstetric fistula |
Tissue damage between the vagina and bladder or rectum leading to incontinence |
Panchayat Mitras |
Literally, friends of the village council |
Postnatal period |
42 days from termination of pregnancy |
Postnatal care |
Health care for women after termination of pregnancy up to 42 days from date of termination of pregnancy |
Post-partum hemorrhage |
Bleeding immediately after delivery |
Primary health center |
Basic health facility in rural areas catering to a population of 30,000 |
Rogi Kalyan Samitis |
Patient Welfare Committees, committees at government health facilities |
Scheduled caste |
Phrase under Indian law for Dalits |
Scheduled tribes |
Phrase under Indian law for adivasis or tribal communities |
Sepsis |
Severe infection spreading through the bloodstream |
Sub-health center |
Basic health facility in rural areas catering to a population of 5,000 |
Termination of pregnancy |
The end of a pregnancy, whether through delivery, miscarriage, or abortion |
UN guidelines |
1997 United Nations Guidelines for Availability and Utilization of Obstetric Services |
UN process indicators |
UN Process Indicators for Availability and Utilization of Obstetric Services |
Summary
Who asks what happened afterwards? ... If a person dies, she dies. If someone hangs himself then it becomes a police case. But if someone dies in a hospital then no one cares.
- Suresh S., neighbor of deceased pregnant woman, Uttar Pradesh, March 2, 2009.
For an emerging global economic power famous for its medical prowess, India continues to have unacceptably high maternal mortality levels. In 2005, the last year for which international data is available, India's maternal mortality ratio was 16 times that of Russia, 10 times that of China, and 4 times higher than in Brazil.[1] Of every 70 Indian girls who reach reproductive age, one will eventually die because of pregnancy, childbirth, or unsafe abortion, compared to one in 7,300 in the developed world. More will suffer preventable injuries, infections, and disabilities, often serious and lasting a lifetime, due to failures in maternal care.
"Destiny" or "fate" brought this upon them, say many of the families that experience maternal deaths, unaware that as many as three in four might be prevented if all women and girls had access to appropriate health care.
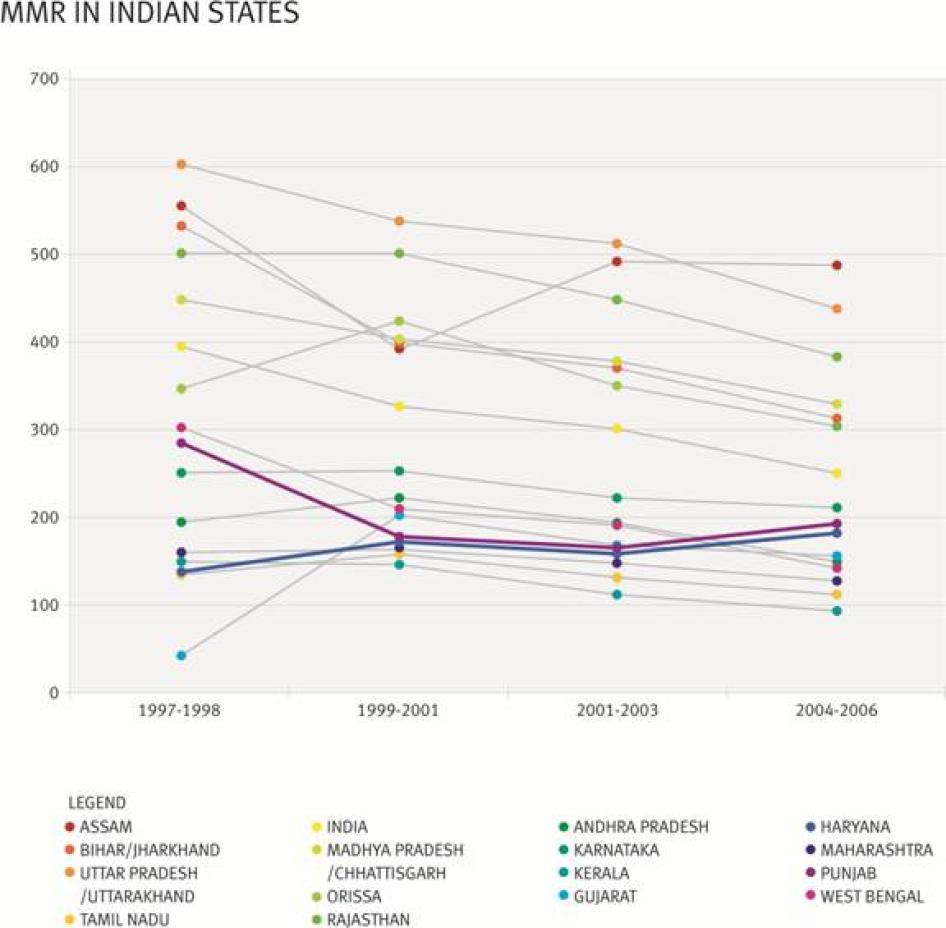
After more than a decade of programming for reproductive and child health with few results, the Indian government acknowledged the problem and in 2005 took steps under its flagship National Rural Health Mission (NRHM) to improve public health systems and reduce maternal mortality in particular. Recent data suggest it is having some success: all-India figures show a decline in maternal deaths between 2003 and 2006.
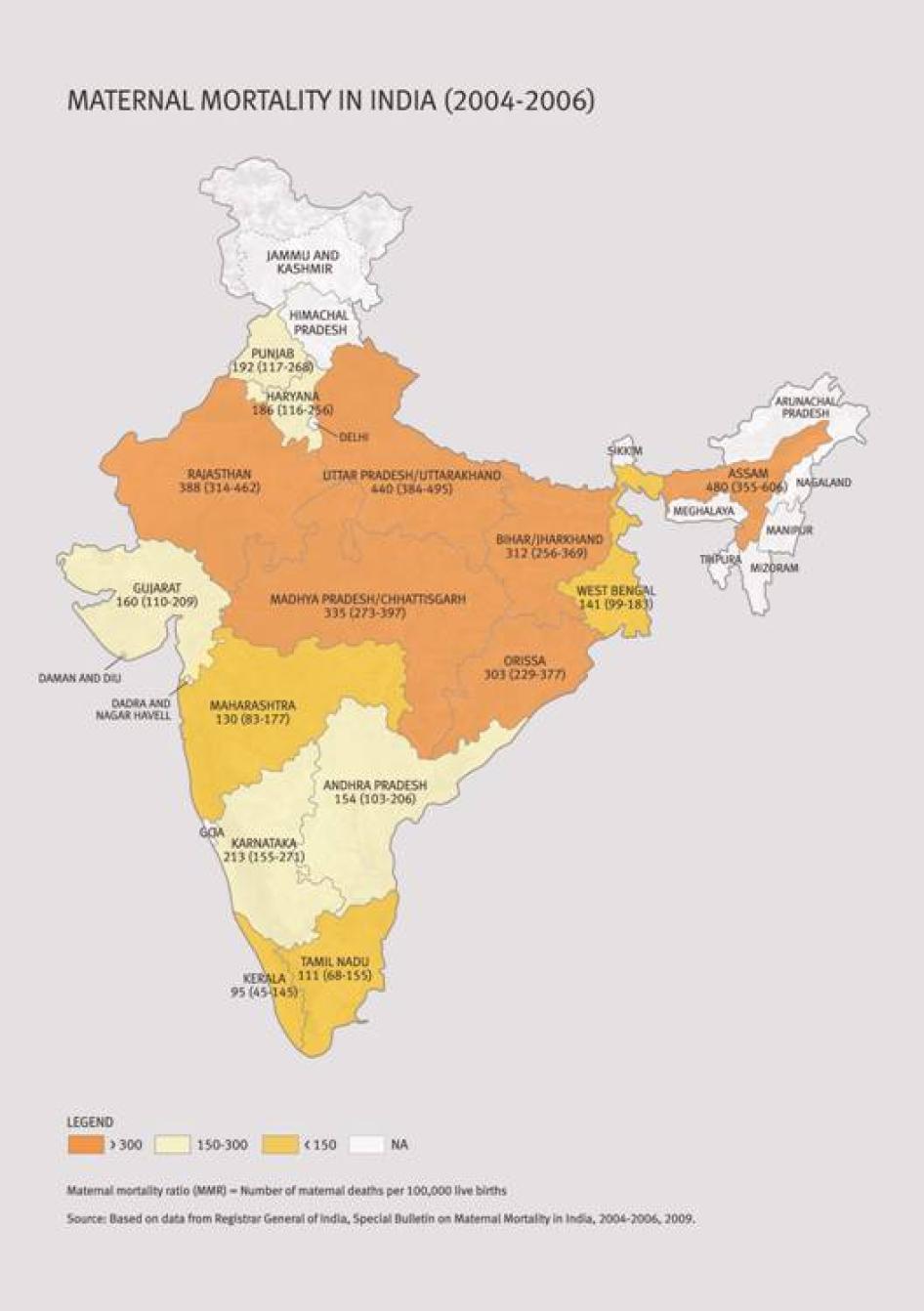
This decline, however, is small in relation to the scope of the problem, and camouflages disparities. Some states like Haryana and Punjab actually showed an increase in maternal mortality. And significant disparities based on income, caste, place of residence, and other arbitrary factors persist even within every state, including those that appear to be improving access to care for pregnant women and mothers. Poor maternal health is far too prevalent in many communities, particularly marginalized Dalit (so-called "untouchable"), other lower caste, and tribal communities.
One step the Indian government has already taken is to increase women's demand for deliveries in health facilities, on the assumption that doing so will promote safe deliveries. National and state officials are also taking steps to upgrade public health facilities to improve the standard of care. They are also making efforts to improve monitoring of health parameters through a new Health Management Information System, and are launching an annual health survey in some key states to boost the levels of health-related information.
These steps are important and, indeed, suggest India has the potential to be a leader among developing countries in attacking maternal mortality and meeting the international commitments spelled out in the "Millennium Development Goal" on maternal mortality. This will be possible, however, only if officials do more to diagnose and steadily improve healthcare systems, programs, and practices by addressing barriers to care and filling health system gaps. And it will be possible only if officials do more to ensure that policies make a difference in the lives of all women and girls, regardless of their background, income level, caste, religion, number of children, place of residence, and other arbitrary factors.
Human Rights Watch believes that a critical issue, one that has received inadequate attention to date, is healthcare system accountability. Accountability, a central human rights principle, is integral to the progressive realization of women's right to sexual and reproductive health and to the realization of the Millennium Development Goal on maternal mortality reduction.
We conducted research in India between November 2008 and August 2009. The work included field investigations with victims and families in Uttar Pradesh and consultations with experts and activists there and in other parts of India. We chose Uttar Pradesh as the locus for field investigation because it has one of the highest maternal mortality ratios and because it is among those states that have introduced an executive order requiring all maternal deaths to be investigated.
Targeted Interventions Generally speaking, maternal mortality is high where womens overall status is low and public health systems are poor. India is no exception and efforts to bolster womens rights and strengthen the healthcare system as a whole must be an important part of efforts to curb maternal mortality. Even so, targeted interventionsbetter access to skilled birth attendance, emergency obstetric care, and improved referral systems, with particular attention to underserved communitieshave been proven to make a significant contribution to reducing maternal deaths, disease, and injury. |
Our research identified four important reasons for the continuing high maternal mortality rate in Uttar Pradesh: barriers to emergency care, poor referral practices, gaps in continuity of care, and improper demands for payment as a condition for delivery of healthcare services.
We also found serious shortcomings in the tools used by authorities to monitor healthcare system performance, identify flaws, and intervene in time to make a difference. While accountability measures may seem dry or abstract, they literally can be a matter of life and death.
As detailed below, we believe that failures in two key areas of accountability are an important reason that many women and girls in states like Uttar Pradesh are needlessly dying or suffering serious harm during pregnancy, childbirth, and the postnatal period:
- Failures to gather the necessary information at the district level on where, when, and why deaths and injuries are occurring so that appropriate remedies can be devised; and
- Failures of grievance and redress mechanisms, including emergency response systems.
Disparities: From Global to Local
Globally, more than half a million women and girls die every year because of pregnancy, childbirth, and unsafe abortions (maternal deaths). Nearly 80 percent of these deaths are directly linked to obstetric complications such as hemorrhage, obstructed labor, or eclampsia (pregnancy-related seizures). Many women die during pregnancy or after childbirth due to indirect causes such as tuberculosis, hepatitis, and malaria. Thousands more-about 20-30 times the numbers who die-are still left with infections, or suffer injuries or disabilities such as obstetric fistula due to pregnancy-related complications. Many others suffer pregnancies ridden with health problems such as anemia and night blindness.
The direct medical cause of any particular death explains just part of the story. Typically, a maternal death marks the tragic ending of an already complex story with different elements-socio-economic, cultural, and medical-operating at different levels- individual, household, community, and so on. Factors contributing to maternal death include early marriage, women's poor control over access to and use of contraceptives, husbands or mothers-in-law dictating women's care-seeking behavior, overall poor health including poor nutrition, poverty, lack of health education and awareness, domestic violence, and poor access to quality health care, including obstetric services.
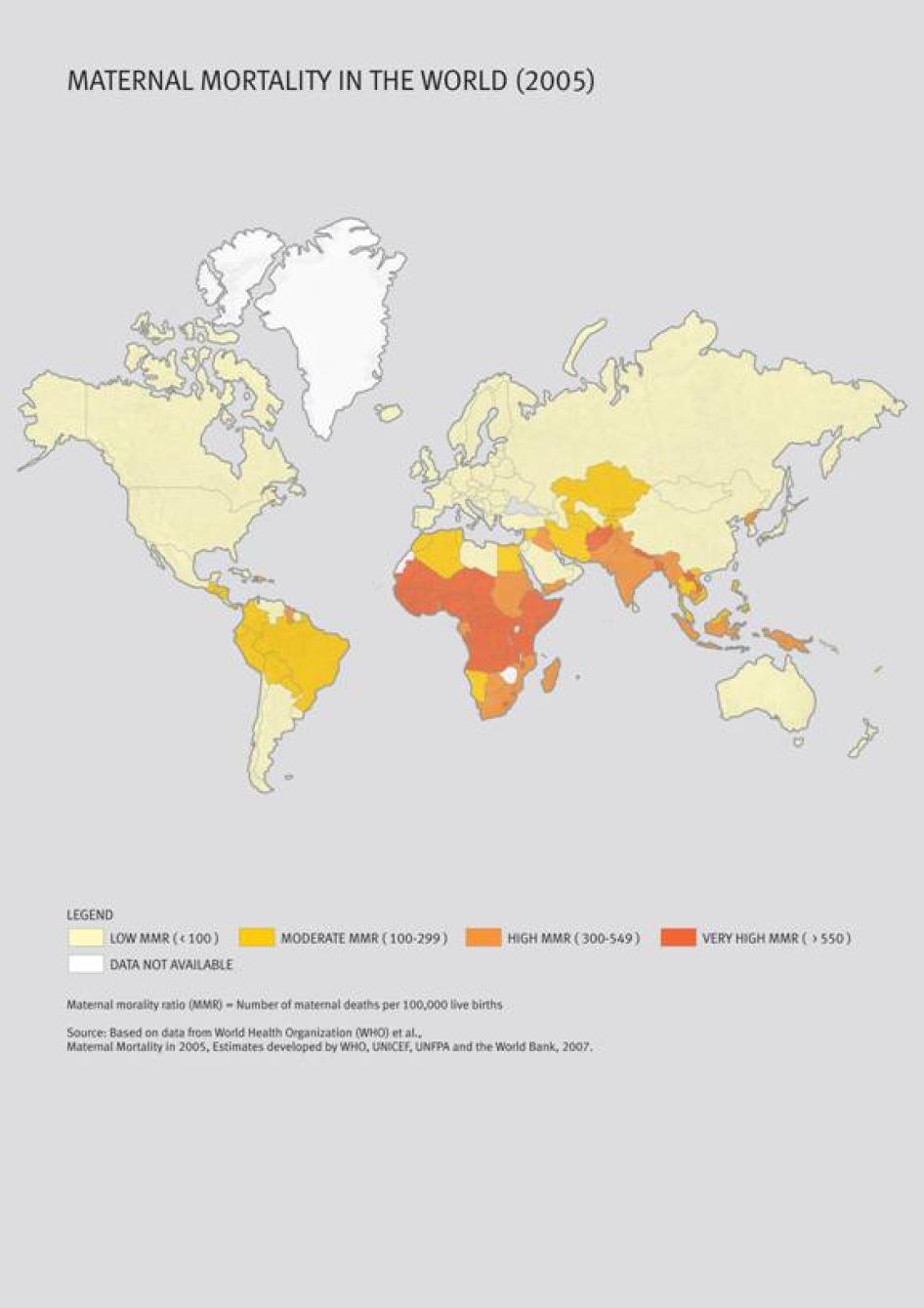
Measures of maternal deaths and morbidities illustrate the vast disparities in global health and access to health care worldwide. Developing countries, including India, bear 99 percent of global maternal mortality. Latest available international figures from 2005 show that India alone contributes to a little under a fourth of the world's maternal mortality, with a maternal mortality ratio (MMR) of 450 maternal deaths per 100,000 live births (compared with Ireland's MMR of 1 and Sierra Leone's 5,400).[2]
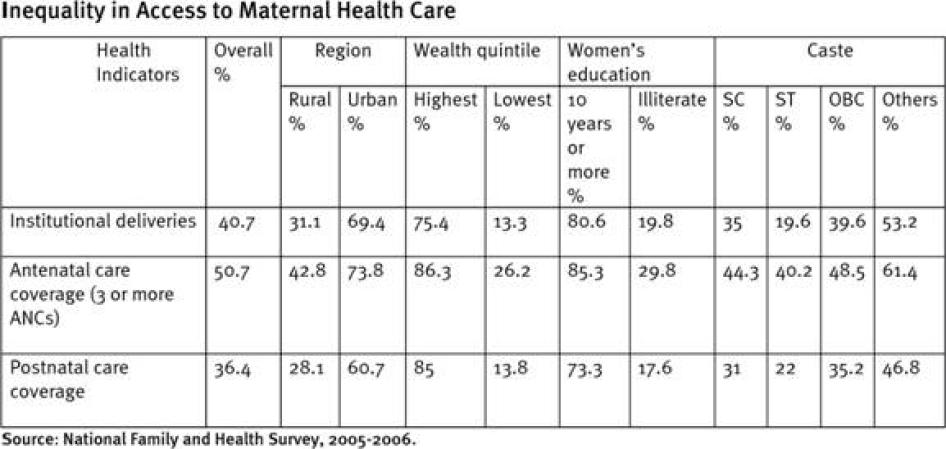
In-country disparities in maternal mortality are huge, with Uttar Pradesh state in north India having one of the highest MMRs, with nearly three times as much as southern Tamil Nadu state. Even within a state, the access to and utilization of maternal health care varies based on region (rural or urban), caste, religion, income, and education. For instance, a 2007 UNICEF study in six northern states in India revealed that 61 percent of the maternal deaths documented in the study occurred in Dalit (so-called "untouchables") and tribal communities.
Recurrent Healthcare System Failures
Indian government policies and programs aim to provide poor rural women with free access to comprehensive emergency obstetric care to save them from life-threatening complications during childbirth. Despite this, thousands of women continue to die because of complications including hemorrhage, obstructed labor, or hypertensive disorders.
The Indian central government's seven-year flagship rural healthcare program, the National Rural Health Mission (NRHM), has ushered in many changes in rural health care, especially maternal health care. It provides for a range of "concrete service guarantees" for the rural poor, including free care before and during childbirth, in-patient hospital services, comprehensive emergency obstetric care, referral in case of complication, and postnatal care. But, critically, it fails to monitor whether these standards are actually being met on the ground and ensure that women are aware of them. The result is recurring health system or program gaps that are not being effectively addressed in practice.
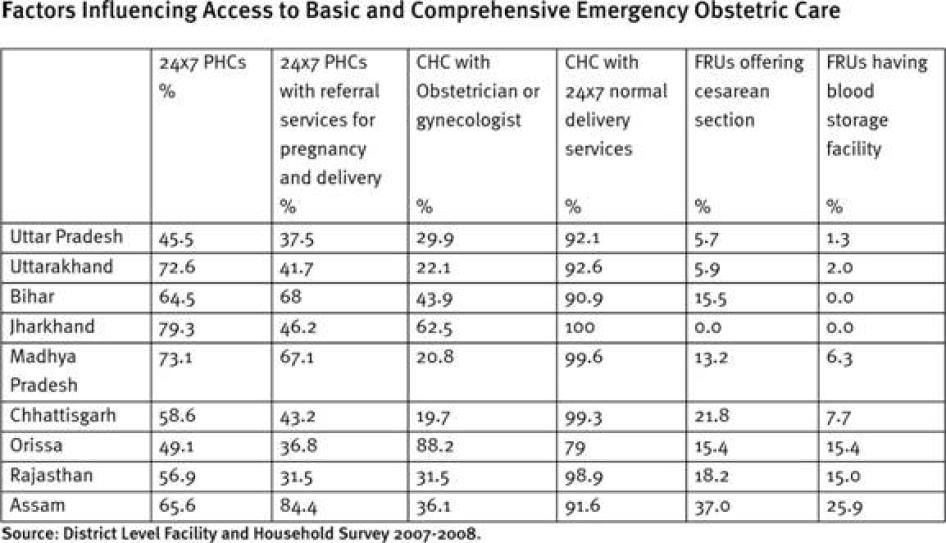
Our research in Uttar Pradesh shows that while health authorities are upgrading public health facilities, they have a long way to go. Currently, a majority of public health facilities that are supposed to provide basic and comprehensive emergency obstetric care have yet to do so. A health worker trained in midwifery can do very little to save the life of a pregnant woman unless she is supported by a functioning health system including an adequate supply of drugs for obstetric first aid, emergency obstetric care, and referral systems for complications such as hemorrhage, obstructed labor, and hypertensive disorders.
For example, most health staff in community health centers of Uttar Pradesh said that they conducted only "normal deliveries." Women with complications were referred to another facility, with little or no referral support. Uttar Pradesh has 583 fewer community health centers than Indian public health standards require. Less than a third of existing community health centers have an obstetrician or gynecologist and about 45 percent do not have funds to operate even the one ambulance they have. In practice, roughly 1 in 20 first referral units (comprehensive emergency obstetric care facilities) in Uttar Pradesh offer caesarean sections and only 1 in 100 have a blood storage facility.
Staff at community health centers and district hospitals visited by Human Rights Watch in Uttar Pradesh reported referring women with pregnancy complications to facilities at times more than 100 kilometers (60 miles) away for a blood transfusion or cesarean section.
We do not have a gynecologist now. No blood facility. So if there is any case that needs blood we refer the case to Allahabad hospital-Sadguru Sewa Trust [more than 100 kilometers away] ... Only normal cases are taken here. We do not take critical cases. In my time [more than two years], we have had only one cesar case [caesarean] performed. - Health staff member at Chitrakoot district hospital, Uttar Pradesh, March 7, 2009. The hospital is supposed to be equipped with comprehensive emergency obstetric care facilities to address all pregnancy-related complications. |
Women are often referred from one health facility to another before reaching a clinic or hospital that is equipped to provide the emergency care they need. In the words of Trishna T. from rural Uttar Pradesh, who recalled her neighbor's frustrating experience of being sent away from a government health facility at the time of delivery: "What's the point of sending us away? If the doctor cannot deal with the case here, then why should we go to the doctor? For the 1400 rupees [US$28, the cash incentive given to women who deliver babies in hospitals or clinics]? Are we going all the way to kill ourselves?" Often such referrals are made without any support for emergency transport and information about whether the higher facility actually has the ability to deal with the complication.
From Bachrawan [comprehensive emergency obstetric care facility] they sent the case to the Rae Bareli hospital and from there they were asked to go to Lucknow hospital. They [the family] could not afford to go there [Lucknow] so they came back here [community health center]....But they [family] started falling at the doctor's [superintendent] feet and holding his hand and leg. So out of mercy he took her and got her admitted. Not into our ward [female ward]. We said no. So he took her into the male ward. She died. He did not want her to die on the road. There is nothing we could have done in that case. We do not have the facilities here. - Nirmala N., health staff member at a community health center, Uttar Pradesh, February 27, 2009, explaining a failed referral from their center. We took her [Kavita K.] to the community health center and they said, "We cannot look at this here." So we took her to [the hospital in] Hydergad. From Hydergad to Balrampur, and from there to Lucknow-all government hospitals. From Wednesday to Sunday-for five days- we took her from one hospital to another. No one wanted to admit her. In Lucknow they admitted her and started treatment. They treated her for about an hour and then she died. - Suraj S., father of Kavita K., Uttar Pradesh, February 27, 2009, recalling his experience when seeking medical assistance for Kavita after she developed postpartum complications. |
The best institutional delivery cannot save a pregnant woman or new mother unless she is cared for in the immediate postnatal period (24-72 hours) with follow-up care in case of complications thereafter. Poor continuity of care through the antenatal and postnatal periods has remained a persistent problem in states like Uttar Pradesh. A 2008 government survey reveals that there is a significant drop in care even within the immediate postnatal period of 48 hours of delivery in Uttar Pradesh.
Women and girls also face considerable financial barriers to care. Even though government programs guarantee a host of free services including out-patient obstetric services, drugs, and in-patient obstetric services such as comprehensive emergency obstetric care, in practice, the care is seldom free. The most obvious example is government discrimination among women on the basis of age and number of children while providing benefits under healthcare programs like the Mother Protection Scheme (Janani Suraksha Yojana or JSY). In many states, pregnant girls under the age of 19 or women and girls with more than two children are not entitled to benefits under the JSY even though young mothers and mothers with multiple pregnancies are especially in need of such medical attention.
Many health workers in hospitals and clinics make unlawful demands for money or payment as a condition for care. Often this is justified as a customary practice around childbirth where families "volunteer" money or gifts to celebrate childbirth. But such practices should be curbed because they impose a severe burden on poor families. In cases where free care is dependent on whether women belong to families holding cards certifying them as below the poverty line, non-issuance of such cards forms a significant barrier to access.
Nothing is free for anyone. What happens when we take a woman for delivery to the hospital is that she will have to pay for her cord to be cut... for medicines, some more money for the cleaning. The staff nurse will also ask for money. They do not ask the family directly ... We have to take it from the family and give it to them [staff nurses] ... And those of us [ASHAs] who don't listen to the staff nurse or if we threaten to complain, they make a note of us. They remember our faces and then the next time we go they don't treat our [delivery] cases well. They will look at us and say "referral" even if it is a normal case. - Niraja N., female community health worker or ASHA, Uttar Pradesh, February 26, 2009. One man I know had taken his wife for delivery to the CHC. He had sold 10 kilos of wheat that he had bought to get money to bring his wife for delivery. He had some 200-300 rupees [US$4-6]. Now in the CHC they asked him for a minimum of 500 rupees [US$10]. Another 50 [rupees] to cut the cord and 50 [rupees] for the sweeper. So he started begging and saying he did not have more money and that they should help for his wife's delivery. I... asked them why they were demanding money. The nurse started giving us such dirty [verbal] abuses that even I was getting embarrassed and wanted to leave. You imagine how an ordinary person must feel who wants help. - Activist from a local nongovernmental organization in Uttar Pradesh, March 2, 2009. |
Improving Accountability: The Critical Need for Need for Better Monitoring and Timely Investigations
Existing approaches have not done enough to ensure that district health authorities gather information about why existing healthcare programs are not being implemented as they should be. They lack critical information about blockages or gaps in the health system. The key issue here is effective monitoring: using maternal death investigations and appropriate monitoring indicators to obtain the data needed for interventions that save lives and reduce harm.
Central and state authorities often point to the number of facility-based deliveries as an important measure of progress. While this can be a useful measure-facility-based deliveries under some circumstances correlate with reduction in maternal mortality-it does not provide the necessary information on whether a mother actually survived the childbirth and postnatal period without injuries, infections, or disabilities.
"Institutional Deliveries" as a Measure of Progress The Mother Protection Scheme (Janani Suraksha Yojana or JSY) promotes hospital or clinic-based deliveries through cash incentives for pregnant women (1400 rupees, or US$28, in rural areas) and community-health workers with the objective of promoting safe deliveries through improved access to skilled birth attendance. In theory the JSY seeks to integrate the cash assistance with prenatal and postnatal care. Nearly 20 million Indian women delivered in health facilities between mid-2005 and March 2009, a reflection, authorities say, of the JSY incentives. The Indian central and state governments use the number of such institutional deliveries as a key measure of progress on maternal health. While the JSY has improved the demand for institutional deliveries, these statistics alone are not an adequate indicator of progress. While conducting field investigations in Uttar Pradesh, Human Rights Watch found that the number of institutional deliveries at health facilities was counted by keeping track of the number of women who received cash assistance. In several instances, women from rural areas claimed that health workers had approached them saying that they could deliver at home but tell authorities they delivered in the health facility, splitting the cash assistance with the health worker. More fundamentally, counting the number of institutional deliveries alone is misleading unless one monitors the actual outcome of pregnancies through the postnatal period. Currently missing is information on whether pregnant women who develop life-threatening complications such as hemorrhage, obstructed labor, and eclampsia (pregnancy-related seizures) receive timely and free access to emergency obstetric care as guaranteed under the NRHM. Health officials were able to give Human Rights Watch data on the number of institutional deliveries but not on the type of care received. Health experts say that for institutional deliveries to be successfully considered a proxy for safe delivery, the following conditions should be met: A skilled birth attendant should be "trained to proficiency" not only in the skills needed to manage "uncomplicated" cases, but also to identify, manage, and refer complications (WHO, ICM, FIGO Joint statement). Skilled care itself requires that an "accredited and competent" healthcare provider has at her disposal the "necessary equipment and the support of a functioning health system, including transport and referral facilities for emergency obstetric care" (WHO, ICM, FIGO Joint statement). Too often, these conditions are not being met in Uttar Pradesh and many other parts of India. |
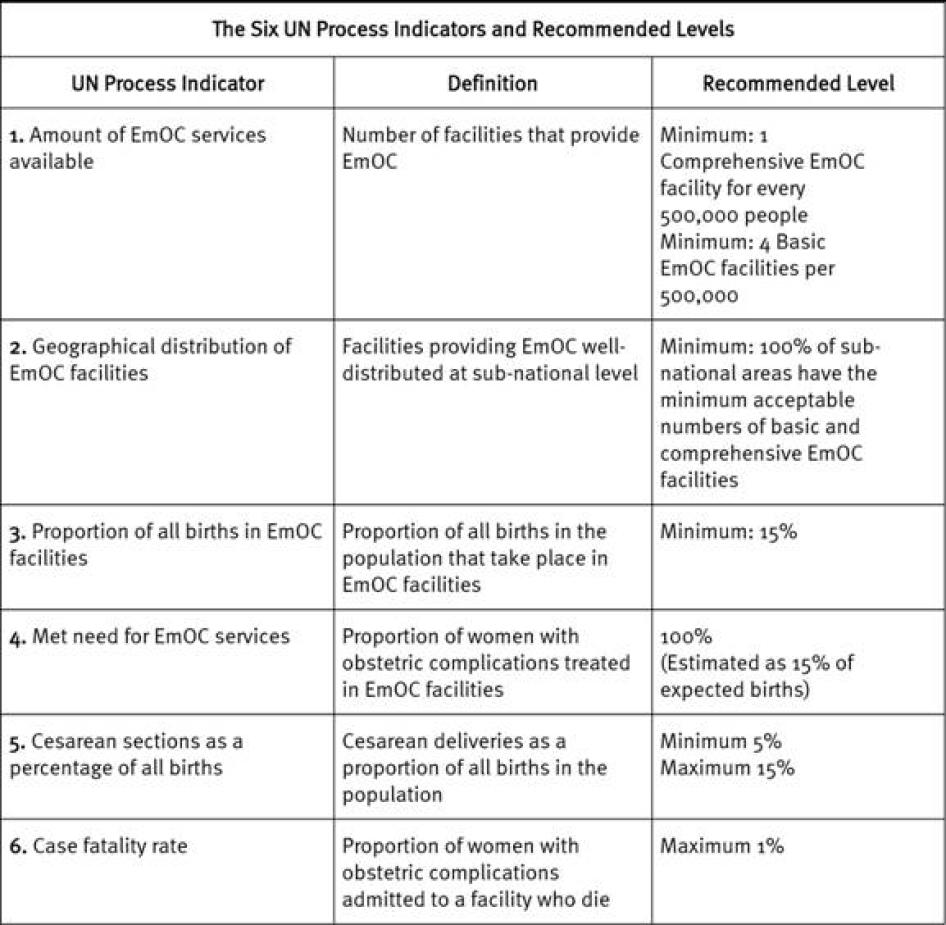
While improving access to basic and comprehensive emergency obstetric care is critical to reducing preventable maternal mortality and morbidity, so far the Indian central government and states like Uttar Pradesh have not monitored the availability and utilization of such services. In 1997 the United Nations Children's Emergency Fund (UNICEF) adopted a set of indicators that monitor key interventions required to reduce maternal mortality, including whether the need for emergency obstetric care has been met and the number of deaths from complications in facilities equipped with emergency obstetric care. These indicators are not being used widely in India. Recently, the Indian government rolled out the Health Management Information System (HMIS) which records whether there is access to first referral units or facilities equipped with comprehensive emergency obstetric care as an indicator, but this is being poorly implemented in Uttar Pradesh.
Maternal death investigations identifying health system shortcomings are a powerful method of monitoring the implementation and effectiveness of healthcare schemes at the district level. Studies in different parts of India have repeatedly illustrated their utility in identifying and plugging gaps in healthcare schemes, particularly in underserved areas, and the Indian government is taking steps to institutionalize such investigations. But for such a system to be implemented successfully, authorities will have to take measures to ensure that maternal deaths are reported accurately.
Human Rights Watch documented several continuing barriers to reporting maternal deaths in Uttar Pradesh, the principal of which are illustrated briefly below:
1)Low priority for the collection and use of data on the frequency and cause of maternal deaths.
This information [maternal deaths] doesn't come to us because we don't get this through the pro forma. We don't have a column for maternal deaths.
- Senior health officials, Directorate of Family Welfare, Uttar Pradesh, March 2009.
When we used to have CSSM forms [Child Survival and Safe Motherhood forms], under "Surveillance" we used to have a maternal deaths column. From last year we have given new forms-called routine immunization now- but most of the data collected in this form is also the same-about deliveries also. But the maternal deaths column in this form is missing-I think it got left out by mistake.
- Officer from Directorate of Family Welfare, Uttar Pradesh, March 2009.
2)Lack of clarity among health workers on what a maternal death is.
In this we note down the name of the person who died, date of the death, age, reasons-we note down if it is a child, but adults also sometimes we note down. If it is a pregnant woman who died then we note it down-we have to report it-any death during delivery or after delivery-within six or eight hours after delivery ... If it is after that then we write the reason-there will be other reasons-fever or something else. Those are not maternal deaths. How can those be maternal deaths?
- Ratna R., health worker, Uttar Pradesh, February 2009.
3)Poor continuity of care, essentially excluding from the records any deaths that happen during the immediate postnatal period or thereafter.
4)Jurisdictional concerns with health workers refusing to provide care or document deaths they do not see as within the purview of their care. Many health workers stated that they were instructed to provide JSY services to only those women who are married and residing in their husband's homes.
"This is Rohini's maikai's [mother's house]village. So her death will not be noted here. We do not register women when they are in their maikai's."
-Ratna R., health worker, Uttar Pradesh, February 2009.
I do not have to note down her name because I did not attend her case.... Only bahus [daughters-in-law] of our village get registered. We are told in the training that we have to motivate only the bahus [for institutional delivery].... We get money if we motivate them for sterilization-150 rupees [US$3] for every case. It does not matter where the woman is [for sterilization]. I learnt all this from the training.
- Pooja P., health worker, Uttar Pradesh, March 2009.
5) Fear of disciplinary actions against health centers and workers that report deaths.
The tracking and monitoring [of maternal deaths] is very poor. How much can you expect one lady [referring to the government-appointed birth attendant, or ANM] to do? .... There is underreporting of [maternal] deaths. My personal experience has been that some ANMs hide deaths. They are busy-out for 10 days doing polio [administering vaccine]-they do not go to all of the villages. If there is a [maternal] casualty in this period, they do not report it.
-G. S. Bajpai, district surveillance officer, Uttar Pradesh, March 2009.
6)Caste-based discrimination by health workers, which excludes many communities from care and therefore reporting.
Even when they [health workers] come they bring someone else who is a Chamar [Dalit community]. He is the one who gives polio [drops]. The nurse is Mishra [so-called upper caste] so she would not touch our children.
-Trishna T., woman who had recently delivered, Uttar Pradesh, March 2009.
7)Poor reporting by private facilities that conduct about 20 percent of all deliveries in India.
In our research, we also visited Tamil Nadu, where authorities have taken measures to improve maternal death reporting and investigations. While the Tamil Nadu system has scope for improvement, certain positive features of the Tamil Nadu approach warrant consideration for possible adoption in other parts of India:
- Awareness campaigns around maternal health.
- Encouraging death reporting from multiple sources, including family members and health workers.
- Encouraging reporting of all deaths of pregnant women irrespective of cause of death.
- Targeted training for health workers on maternal death investigations.
- Focusing on all health facilities, public and private.
- Creating a conducive environment for reporting deaths, including by explaining to health workers the purpose of such reporting.
- Assigning a clear purpose to the inquiry-identifying health system gaps that need to be rectified.
A robust civil registration system that records all births and deaths, including cause of death, is essential for effective long-term monitoring of trends in maternal mortality and enforcing laws against early and enforced marriages that directly influence maternal health. India has a civil registration system put in place by the Registration of Births and Deaths Act of 1969, that mandates recording of maternal deaths, but the system has not yet been implemented consistently. Uttar Pradesh has the worst civil registration system in the country. The latest report by the Office of the Registrar General on vital statistics for the period 1996-2005 has no information on Uttar Pradesh and indicates that no annual reports have been submitted. Since collection of vital statistics is a shared responsibility of the Indian central and state governments according to the Indian Constitution, the Indian central government has direct responsibility for the state of the civil registration system in Uttar Pradesh. For a country famed worldwide for its prowess in research, information technology, and medical sophistication, this shows not a lack of capacity but a lack of political will.
Improving Accountability: Reforming Grievance and Redress Mechanisms and Creating Emergency Response Systems
Our research also found that when women suffer preventable harms or have complaints about their treatment, they have no realistic avenue to raise their concerns and have them resolved. Too often, grievance and redress mechanisms, which should be empowering women and helping to identify gaps in maternal care, do not work. Such systems are vital not simply for holding to account those responsible for past violations but also preventing repetition of the same behavior in the future.
Problems with existing mechanisms for grievance and redress:
1)Women's lack of awareness of their entitlements under the different schemes.
2)Absence of a clear complaints procedure with a time-bound inquiry period.
3)Absence of an early or emergency response mechanism to help families that experience difficulties in seeking appropriate care.
4)Poor access to any complaints procedure, especially for poor women with little or no formal education.
5)Lack of support to pursue complaints. For example, daily wage workers are unable to make repeated appearances before human rights or other commissions to present evidence.
6)Fear of reprisals from doctors and health workers where complaints are pursued.
7)Lack of independence at the time of inquiry.
Where obstacles arise in emergencies-such as when a woman requiring urgent care is refused admission to a facility because of discrimination or because she cannot pay-there should be a mechanism for alerting authorities immediately. Bolstering early response systems will allow people who can make a difference to get the necessary information when they need it.
Even where reforms have reduced maternal death and disease, a good grievance and redress mechanism can serve to warn against possible backsliding and address other concerns of women and girls seeking maternal care, including discrimination and mistreatment.
Appropriate mechanisms for individual redress may include compensation or other appropriate action where there is individual responsibility. Individual responsibility should not be limited to frontline health workers and doctors. Any inquiry into a complaint should also examine possible failures in planning and oversight at the district and sub-district levels.
Seven Concrete Recommendations
The Indian government is already committed to a human rights approach to preventable maternal mortality and morbidity and has shown this commitment in several ways. The Indian central and state governments are poised to play a leadership role among developing countries to strengthen accountability en route to achieving the Millennium Development Goal on maternal mortality reduction. This will go a long way toward recasting India's reputation as a country with the highest number of maternal deaths in the world.
To this end, the Indian central government and Uttar Pradesh and other state governments should:
- Require that all healthcare providers, public and private, "notify" (formally report) all pregnancy-related deaths.
- Institutionalize under the NRHM a system of maternal deaths investigations. Investigations should identify systemic shortcomings and findings should be integrated into the planning and development of district and state-level plans.
- Revise the JSY monitoring indicators through a participatory and transparent process, ensuring that they track adverse pregnancy outcomes. The indicators should be in accordance with "United Nations Process Indicators" for availability and utilization of obstetric services.
- Appoint a full-time special officer to oversee the implementation of the civil registration system in Uttar Pradesh and create a special plan for implementation, including adequate funding.
- Develop, through a participatory and transparent process, a facility-based or regional system of ombudsmen to receive grievances and pursue timely redress. The mechanism should be easily accessible to women with little or no formal education.
- Develop early response systems, including a telephone hotline for health-related emergencies which women facing obstetric emergencies could use.
Donor countries and international agencies should provide technical and financial assistance to promote notification and investigation of maternal deaths. They should also provide technical and financial assistance to ensure that all government health interventions, particularly interventions funded by them, are monitored and evaluated in accordance with UN process indicators.
Methodology
This report is based on Human Rights Watch field investigations and consultations with key stakeholders in India between November 2008 and August 2009. Where available, the accounts gathered through our field investigations have been corroborated by data from government surveys, and reports or studies by nongovernmental organizations, international agencies, and public health experts in India.
Based on our preliminary consultations with 55 public health specialists, lawyers, and representatives from local nongovernmental organizations working on the right to health and women's rights across India, Human Rights Watch chose to focus on Uttar Pradesh state in north India.
Uttar Pradesh was chosen as a case study because, being the most populous state, it accounts for the highest number of maternal deaths in India.[3] It is also one of several states that had issued a 2004 governmental order seeking investigations into maternal deaths.
Human Rights Watch also examined southern Tamil Nadu's relatively stronger system of investigating maternal deaths.
The primary field investigations took place in Rae Bareilly, Unnao, Chitrakoot, Lucknow, and Barabanki districts of Uttar Pradesh in February, March, and June 2009; New Delhi in March 2009; and in Tamil Nadu in April 2009. We supplemented these field investigations with telephone interviews between June and August 2009.
Human Rights Watch researchers interviewed 191 people; 95 in individual interviews and the remainder in group interviews. These included:
In Uttar Pradesh:
- Fifty-six women and men from villages, including individuals from nine families in which maternal deaths had occurred.
- Thirty-four health staff from government health facilities, peripheral field-based health workers including auxiliary nurse-midwives (ANMs), accredited social health activists (ASHAs) or female community health aides, anganwadi workers (female workers tasked with providing early childhood care and education and nutritional supplements for pregnant women), and traditional birth attendants.
- Forty-five officials including heads of village level councils, panchayat mitras (literally, friends of the village council), chief medical officers (highest health authority at the district level), officials from the directorates of family welfare and medical and health services, and members of the district and state project management units of the National Rural Health Mission (NRHM), India's flagship rural healthcare program.
- Seven doctors from the private sector, including representatives from the Uttar Pradesh chapters of the Federation of Obstetric and Gynecological Societies of India and the Indian Medical Association.
- Thirty journalists and representatives from nongovernmental and intergovernmental organizations including Vatsalya, Mamta, SAHAYOG, Healthwatch Forum, Jan Swasthya Abhiyaan-UP chapter, CARE-India, the John Hopkins University project on infant and maternal health, Vanangana, PATH, and UNICEF.
In NewDelhi:
- Eleven officials including officials from the Office of the Registrar General of India, the NRHM directorate, and representatives from the National Health Systems Resource Center, a technical resource center set up under the NRHM.
In Tamil Nadu:
- Four former and four present government officials overseeing maternal mortality reviews.
- Nine activists, including grassroots-level workers and a professor who participates in the maternal mortality review meetings.
Human Rights Watch had hoped to include the perspectives of doctors or health workers who were suspended, dismissed, or arrested following complaints about maternal health care in Uttar Pradesh. Unfortunately, we were able to trace only one such health worker, a hospital staff nurse.
Health workers and nongovernmental organizations providing services to villagers assisted Human Rights Watch in identifying pregnant women and families to interview; we further developed contacts and interview lists through references from interviewees.
Interviews lasted between 20 minutes and three hours and were conducted in English, Hindi, dialects of Hindi such as Awadhi or Bundelkhandi, or Tamil depending on the interviewee's preference. The primary investigator from Human Rights Watch is also fluent in spoken Hindi and Tamil. In cases where the interviewees chose to communicate in Awadhi or Bundelkhandi, the interviews were conducted with the assistance of female interpreters.
All interviews during field investigations in Uttar Pradesh, Tamil Nadu, and New Delhi were conducted after orally obtaining informed consent. Human Rights Watch has respected the choices of all interviewees to be identified, not identified, or have their experiences and views left out of the report entirely, and has assigned pseudonyms or withheld identifiable information accordingly. Pseudonyms have been assigned randomly, and do not correspond to the religion, caste, or tribe of the interviewee.
We supplemented our field investigations with official data provided by the Indian central and Uttar Pradesh state governments in response to several applications filed by Human Rights Watch under the Right to Information Act, 2005.[4]
Human Rights Watch also convened an India advisory group whose purpose was to provide inputs and feedback on methodology, support in reaching out to relevant networks and groups, and review this report.[5]
Scope and Limitations
This report uses a human rights framework to examine maternal health care, setting out several specific steps we believe officials should take to better integrate accountability into maternal healthcare programs and ensure their implementation through the health system. It does not explore all available tools for accountability including external surveys assessing quality of health care, public hearings, social audits of budgets, or community-based monitoring. The NRHM, India's flagship rural healthcare program, sets out a three-pronged accountability framework of external surveys, community-based monitoring, and stringent internal monitoring. This report's focus is on the last of these three prongs, the state's internal monitoring of policies, practices, and performance. While the arguments presented in this report address the specific issue of preventable maternal mortality and morbidity, accountability as a human rights principle is central to the right to the highest obtainable standard of health more generally.
Uttar Pradesh state is one of eight Empowered Action Group (EAG) states with poor socio-economic indicators.[6]The maternal health parameters of the eight states are comparable, and activists and public health experts in India say they exhibit similar recurring health system shortcomings.[7] The concerns raised in this report in chapters III-V have been examined in the context of Uttar Pradesh, but apply to many states, particularly those in the Empowered Action Group. Financial barriers to care are a problem in many states in India including non-Empowered Action Group states.
While interviewing bereaved families, Human Rights Watch's researchers gathered information on the fulfillment of government standards for maternal health care. Detailed identification and analysis of all the socio-economic or medical causes that contributed to each of these maternal deaths is beyond the scope of this report.
Note on Estimates
All data used in this report are estimates. The indicator most often cited in this report is the maternal mortality ratio (MMR) which is an estimate of the number of maternal deaths per 100,000 live births. The Indian government has released maternal mortality estimates based on various measures including MMR. Maternal mortality data for Indian states and for the country as a whole going back to 1997 have been provided by the Indian government in two recent reports. Data for the period 1997-2003 was released in 2006 in a publicly issued special report on maternal mortality and its causes.[8] A second data set, released in mid-2009, provides preliminary information for the period 2004-2006, pending release of the full report.[9] The in-country estimates used in this report are drawn from the interim 2004-2006 data. Information about medical causes of maternal deaths is drawn from the 1997-2003 data.
International data presented in this report are drawn from the latest available international estimates of maternal mortality that date from 2005.[10] The Maternal Mortality Working Group (MMWG) comprised of the WHO, UNICEF, UNFPA, the UN Population Division, and the World Bank, as well as several outside technical experts, developed a methodology to create comparable country, regional, and global estimates of maternal mortality. The MMWG concluded that the data provided by the Indian government's survey is uncertain, containing biases such as ill-defined cause-of-death codes. This group calculated that the Indian survey underestimates the national MMR by 50 percent.
The national MMR figures used in this report should be interpreted with the caveat that they do not fully reflect the changes brought on by the Indian government's flagship healthcare program, the NRHM, which has only been in effect since mid-2005 when the figures were compiled for the period 2004-2006. Furthermore, these figures represent point estimates within a larger range.[11] While the point estimates taken alone suggest a discernible reduction in MMR, the overlap in its ranges makes it difficult to gauge the extent of maternal mortality reduction in many states, particularly the EAG states.[12]
Note on Terminology
"Health workers": We use this phrase to refer to three categories of field-based peripheral workers-ANMs, anganwadi workers, and ASHAs.
"Investigating maternal deaths": We use this phrase to refer to procedures that identify health system shortcomings in addressing the causes, socio-economic as well as medical, of maternal deaths.
The World Health Organization (WHO) has outlined several methods of conducting maternal death reviews including community-based (verbal autopsies) and facility-based reviews, and confidential inquiries.[13] Human Rights Watch does not have the expertise to recommend a particular method of investigating deaths. Confidential inquiries have the merit of covering deaths irrespective of the place of occurrence and of not limiting the inquiry to identifying personal, family, or community factors as is the case with verbal autopsies.
"Lower castes": The phrase "lower castes" has been used to describe two types of castes in India, scheduled castes and so-called "other backward classes." Under Indian law scheduled caste refers to Dalits or so-called "untouchables" who are traditionally considered "outcastes," beneath the lowest caste in the four-caste hierarchy. Indian law uses "other backward classes" to refer to the lowest caste within the four-caste hierarchy, the Shudras. Both groups continue to face historical discrimination and have high rates of poverty.
I. Preventable Maternal Mortality and Morbidity: A Global Public Health Emergency
[Maternal mortality is] a measure of mortality that can be dramatically, rapidly, and consistently decreased-almost to the point of negligibility-if the appropriate actions are taken.
- United Nations Millennium Project Task Force on Child Health and Maternal Health, 2005.
Pregnancy is not a disease or illness. Yet more than half a million women and girls die every year because of pregnancy, childbirth, and unsafe abortions.[14] Health experts determine that about 75 percent of these maternal deaths are preventable. Year after year women die preventable deaths merely because they do not have access to appropriate health interventions.[15]
Pregnancy and childbirth also leave millions of women and girls with short- or long-term injuries, infections, or disabilities (maternal morbidities). For every maternal death there are about 20-30 cases of maternal morbidity.[16]Between 50,000 and 100,000 new incidents of obstetric fistulae (tissue damage between the vagina and the bladder or rectum leading to incontinence) are detected annually.[17] Other long-term morbidities include uterine prolapse (weakened muscles after childbirth leading to displacement of uterus), infertility, and depression; short-term complications include hemorrhage, convulsions, cervical tears, shock, and fever.[18]
This has implications not only for women's reproductive health overall. Differences in levels of preventable maternal mortality and morbidity are strong indicators of other disparities, in particular the unequal access to quality health care, both between women in developed and developing countries and among women in the same country. Nearly 99 percent of all maternal deaths and morbidities occur in developing countries, particularly sub-Saharan Africa and South Asia.[19] The difference between Ireland and Sierra Leone illustrates this disparity: in Ireland 1 death occurs per 100,000 live births compared with Sierra Leone's 5,400 deaths. In Niger, one in every eight 15-year-old girls is expected to eventually die of a maternal cause. In contrast, 1 in 47,600 15-year-olds will die in Ireland.
Causes and the Three Delays
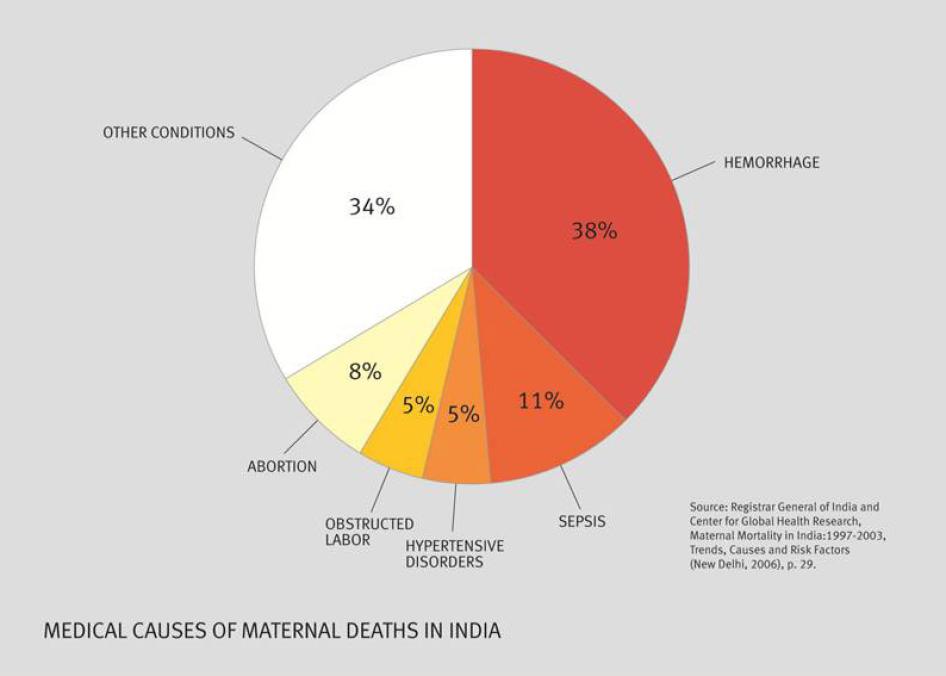
Globally, approximately 80 percent of all maternal deaths are estimated to be caused by direct obstetric causes including hemorrhage, sepsis (severe infection spreading through the bloodstream), eclampsia (pregnancy complication characterized by seizures or coma), unsafe abortions, and prolonged or obstructed labor.[20] Other indirect causes include malaria, tuberculosis, and HIV/AIDS.[21] In countries with high rates of HIV, malaria, or tuberculosis, the proportion of deaths due to such causes may be higher.[22]
Medical causes explain just part of the story. Typically, a maternal death marks the tragic ending of an already complex story with different elements-socio-economic, cultural, and medical-operating at different levels-individual, household, community, and health system-related. Factors contributing to maternal death include early marriage, women's poor control over access to and use of contraceptives of their choice, husbands or mothers-in-law dictating women's care-seeking behavior, overall poor health including poor nutrition, poverty, lack of health education and awareness, domestic violence, and poor access to affordable quality health care, including basic and comprehensive emergency obstetric services.[23]
Health experts typically analyze these myriad circumstances using the "three delays model." In this model the reasons for delay in seeking and utilizing appropriate health care are broken down into three segments-the first being the delay in seeking professional health care, followed by the delay in reaching the appropriate health facility, and lastly, the delay in receiving care.
Some healthcare providers tend to unjustifiably lay all the blame for delay on pregnant women and their families for their uneducated or unresponsive behavior. But the delay in people's decisions to seek care is often due to their perceptions of systemic shortcomings and mistrust in health facilities.[24] Many women and activists from Uttar Pradesh told Human Rights Watch that they did not like going to government healthcare facilities because they are shut, doctors are not present, medicines are not available, or they are too far away.[25] Where a woman's own experiences discourage her from going to a healthcare facility, it is unlikely that information and education programs about facilities or schemes will sustain her motivation to seek care. More nuanced health interventions such as measures to improve the trust in the health system should be taken, for instance, by improving quality of care and creating easily accessible and effective grievance redressal mechanisms.
Reduction Strategies
There is broad global consensus on three critical maternal-mortality-reducing strategies-skilled attendance at birth, access to emergency obstetric care, and access to referral systems. While these three strategies are necessary, they are not sufficient to achieve a 75 percent reduction in maternal mortality.[26]
Available research suggests that access and ability to utilize emergency obstetric care will have maximum impact on maternal mortality. Basic emergency obstetric care includes the ability to conduct assisted vaginal deliveries, remove placenta and retained products, and manage pregnancy complications by intravenously introducing or injecting anticonvulsants, oxytocic drugs (drugs that expand the cervix or vagina to facilitate delivery), and antibiotics.[27] Comprehensive emergency obstetric care includes the ability to provide life-saving interventions including through surgery (cesarean sections) and blood transfusions.[28] Quality basic and emergency obstetric care are dependent on factors such as availability of adequate health personnel trained in midwifery skills, specialists such as anesthetists, gynecologists, and surgeons, adequate infrastructure such as blood banks, blood matching ability, sufficient supply of drugs, and good referral systems.
Skilled birth attendance refers to the presence of health staff trained in midwifery at birth. A skilled birth attendant's ability to save a pregnant woman is limited unless she is supported by a robust health system that includes emergency obstetric care and referral support. Some experts argue that "the skill level of the attendant needed at the peripheral level [sub-district including village level]...depends upon the ready accessibility and acceptance of referral care."[29]
The most skilled attendant cannot save a woman experiencing life-threatening pregnancy-related complications unless she is able to reach the appropriate health facility in time. A strong referral system is not limited to ambulance services. It must at a minimum provide obstetric first aid in case of emergencies and have easily accessible and affordable around-the-clock health care and referral facilities that connect both private and public health facilities.[30]
For all three core interventions to successfully reduce and eliminate preventable maternal mortality and morbidity there has to be a functional public health system. Hence the global priority that is being given to maternal mortality reduction is increasingly hailed as an opportunity to improve public health systems.[31]
International Commitments and Progress on Maternal Mortality Reduction
International and national efforts to reduce maternal mortality span several decades. Concerted global efforts have been made in the last two decades including the 1987 Safe Motherhood Initiative and the 1994 International Convention on Population and Development, which reaffirmed governments' commitment to the issue.[32] And through the Millennium Declaration, 189 countries pledged to achieve eight development goals by 2015, including a 75 percent maternal mortality reduction compared to its 1990 levels.[33] In 2009, in a special session of the Human Rights Council, governments committed to adopting a human rights approach to preventable maternal mortality and morbidity.
But few governments are making adequate progress to achieve a 75 percent reduction in maternal mortality by 2015.[34]There has been less progress in meeting the maternal mortality reduction goal than in meeting any of the other seven MDGs.[35] Even progress in measuring maternal mortality is lacking: a recent international study of 68 countries states that "[t]rends in maternal mortality that would indicate progress towards MDG 5 [maternal mortality reduction] were not available."[36] The authors noted that maternal mortality was high or very high in 56 of the 68 countries. Further, high rates of HIV/AIDS, malaria, and tuberculosis have actually resulted in an increase in maternal mortality in several countries.[37]
II. Maternal Mortality and Morbidity in India
Estimates and Causes
For an emerging global economic power reputed for its medical prowess, India continues to have unacceptably high maternal mortality levels. In 2005, the last year for which international data is available, India's maternal mortality ratios were 16 times that of Russia, 10 times that of China, and 4 times higher than in Brazil.[38] Of every 70 Indian girls who reach reproductive age, one will eventually die because of pregnancy, childbirth, or unsafe abortion, higher than 120 other countries including India's neighbors such as Pakistan, Sri Lanka, the Maldives, and China. More will suffer preventable injuries, infections, and disabilities, often serious and lasting a lifetime, due to failures in maternal care.
While country data on maternal mortality is poor, there is far less government data on maternal morbidity (injuries, infections, and disabilities associated with pregnancy, childbirth, and unsafe abortions). There is some state-wide data on obstetric fistula and infertility. For instance, the District level Facility and Household Survey (DLHS) shows that nearly 1.6 percent of married women in Uttar Pradesh reported obstetric fistula, and 10 percent experienced primary or secondary infertility.[39] The latest nation-wide government-funded survey, the National Family and Health Survey (NFHS), shows that rural women experience many health problems during pregnancy including difficulty with vision during daytime, night blindness, convulsions not from fever, swelling of the legs, body, and face, excessive fatigue, and vaginal bleeding.[40]
National averages camouflage in-country variations in maternal mortality and morbidity, which indicate poor health equity and a lack of equality in access to and utilization of maternal health care. The northern belt in India, comprising the eight Empowered Action Group (EAG) states and Assam, has the highest maternal mortality rates nationally.[41] At 440 maternal deaths per 100,000 live births, Uttar Pradesh reports the second highest maternal mortality in the country, about 1.7 times the estimated national MMR and more than three times that of states like Tamil Nadu in south India.[42]
There are disparities in utilization of maternal health care even within states, districts, and cities. Rural women, the urban poor, and women in geographically remote areas report poorer utilization of maternal healthcare services than those in urban areas.[43] The incidence of morbidity is significantly higher in rural than in urban areas, with rates often two or three times as high.[44] Pregnant women belonging to marginalized communities such as Dalits (so-called untouchables), other backward classes (the so-called lowest caste just above Dalits in the hierarchy), and tribal communities utilize maternal health services far less than women belonging to the uppercastes.[45]A 2007 UNICEF study in six northern states showed that 61 percent of the women who died during pregnancy and childbirth belonged to Dalit or tribal communities.[46]
Roughly 65 percent of all maternal deaths are caused by direct obstetric causes. Hemorrhage is the main cause of death in India, followed by sepsis, and unsafe abortions.[47] At 35 percent, the proportion of maternal deaths due to indirect causes such as tuberculosis, viral hepatitis, malaria, and anemia is also much higher in India than the estimated global average of 20 percent.[48] Poor overall health and nutrition, poor education, women's lack of decision-making power within families, domestic violence, and son-preference coupled with women's poor autonomy in using contraceptives of their choice adversely influence their maternal health.[49]
Maternal mortality remains high in many parts of India despite decades-long initiatives aimed at reducing it.[50] Acknowledging that the number of maternal deaths is "unacceptably high,"[51] the Indian central government itself has identified maternal mortality reduction as a national priority,[52] aiming to bring the MMR below 100 by 2012.[53] The Indian Planning Commission has stated that it will be difficult for India to meet this goal at the present rates at which maternal mortality is declining.[54] Latest all-India estimates show a small decline in maternal mortality from 301 to 254 between 2003 and 2006.[55]
Delivery of Basic and Comprehensive Emergency Obstetric Services
The tiered public health system (see Table 1 on next page) coupled with the services of field-based female health workers including auxiliary nurse-midwives (ANMs) forms the backbone for delivering free basic and comprehensive emergency obstetric care to the rural poor. Norms for providing maternal health care at each of these tiers were recently revised through the Indian government's flagship seven-year rural healthcare program, the National Rural Health Mission (NRHM), read in conjunction with the 2006 Indian Public Health Standards (IPHS).[56]
Table 1: Tiered Public Health System in India[57]
Health facility |
Level |
Population Norm |
|
Health sub-center (HSC) |
Primary |
Plains: One for every 5,000 Hilly or tribal areas: One for every 3,000 |
|
Primary health center (PHC) |
Primary |
Plains: One for every 30,000 |
Community health center (CHC) |
Secondary |
Plains: One for every 1,20,000 |
|
First Referral Unit (FRU) |
Secondary |
One in every 300,000-500,000 (Community health centers are also being upgraded as first referral units) |
District hospital |
Tertiary |
One for every 2-3 million (In some areas district hospitals function as the first referral unit) |
Medical college hospital |
Tertiary |
One for every 5-8 million |
Introduced in mid-2005, the NRHM seeks to "improve access to rural people, especially poor women and children to equitable, affordable, accountable and effective primary health care" with a special focus on maternal mortality reduction.[58] Seeking to achieve goals set under the 2000 National Health Policy and the Millennium Development Goals, it aims to reduce maternal mortality ratios to below-100 levels by 2012,[59] and commits to "report publicly on progress."[60]
The NRHM subsumed the former Reproductive and Child Health Program (RCH-II) program,[61] developing new strategies for maternal mortality reduction. Amongst other things, it seeks to upgrade primary health centers into around-the-clock facilities for basic emergency obstetric care and emergency obstetric first aid.[62] In remote areas where primary healthcare centers are unavailable, the state can accredit sub-centers to conduct normal deliveries. Where sub-centers are also unavailable, the state can accredit private health facilities to provide such care.[63] The NRHM also requires states to upgrade community health centers as "first referral units" equipped to provide comprehensive emergency obstetric care.[64]
The NRHM provides "concrete service guarantees" for many health needs (see Table 2 on next page). These include health education, skilled attendance at all births, free antenatal care, postnatal care, and in-patient facility-based care for delivery and other maternal health conditions at primary and secondary sub-district and district public health facilities, for women below the poverty line.[65] Private healthcare facilities, which are poorly regulated, conduct about 20 percent of the deliveries and also play a significant role in providing abortion services, but these are not governed by the NRHM service guarantees or the IPHS.[66]
Table 2: Service Guarantees under the NRHM
Health sub-center (HSC) |
Primary health center (PHC) |
Community health center (CHC) |
|
Antenatal care ·An ANM with the help of an ASHA should conduct three antenatal check-ups and a fourth visit around 36 weeks. ·Each antenatal check includes examination of weight, blood pressure, anemia, abdominal examination, height and breast examination, minimum laboratory investigations including hemoglobin, urine albumin, and sugar. ·The health staff should identify and promptly refer high-risk pregnancies to the appropriate health facility. Intranatal care ·Sub-centers in remote areas to conduct normal deliveries. ·They should promptly refer cases to an appropriate health facility. Postnatal care ·ANMs with the assistance of ASHAs should conduct a minimum of two home visits (irrespective of place of delivery), the first within 48 hours of delivery and the second within seven or ten days of delivery. |
All norms for antenatal and postnatal care in sub-centers apply to PHCs. They should provide the following services: ·Free out-patient services. · 24-hour delivery services for normal and assisted deliveries (vacuum and forceps delivery) and manual removal of placenta. ·Safe abortions. ·24-hour emergency pre-referral first aid, management of pregnancy induced hypertension. ·Prompt referral of complicated cases to the appropriate health facility. ·All referral services guaranteed free. |
CHCs should provide the following facilities: ·All facilities present in PHCs. ·Surgical and other medical interventions including cesarean sections and safe abortions. ·Blood storage. ·Referral services including transport. |
The NRHM is applicable to all states, but 18 focus states, including Uttar Pradesh, receive additional funding for the stated goal of regional equity.[67]
The Janani Suraksha Yojana
Reforms introduced through the NRHM are coupled with the Janani Suraksha Yojana (JSY, literally, Mother Protection Scheme)-an NRHM scheme replacing the earlier National Maternity Benefit Scheme-that promotes facility-based deliveries through cash incentives for pregnant women and ASHAs.[68] The Indian government promotes facility-based deliveries with the stated objective of improving access to skilled birth attendants for pregnant women, especially those below the poverty line and members of Dalit and tribal communities.[69] Women who deliver in health facilities are given greater cash assistance than women who deliver in their homes. Theoretically, the scheme integrates cash assistance with delivery and post delivery care.[70]
The success of the JSY depends on the ASHAs-rural women appointed as community health aides who are given many tasks including tracking pregnancies, assisting with polio drives, and sharing information about family planning. Under the JSY, ASHAs are tasked with developing a micro birth plan to track the progress of every pregnancy within her area of work.[71] They should identify and register all pregnant women and provide services described as the "four Is." These include "informing" dates for antenatal check-ups, "identifying" a health center for referral, "identifying" the place of delivery, and "informing" pregnant women the expected date of delivery.[72]
ASHAs should facilitate both antenatal and postnatal care, assisting women in getting at least three antenatal check-ups during their pregnancy, and visiting them "within seven or ten days of delivery." During the postnatal care visit, they are responsible for facilitating further access to medical assistance if needed. ASHAs are primarily responsible for arranging transport and escorting the pregnant woman to a pre-identified health facility for delivery.
The cost of the scheme is entirely covered by the Indian central government. The government gives women who choose to deliver in government health facilities or accredited private health facilities 1,400 rupees (US$28) in rural areas.[73] In focus states, such as Uttar Pradesh, the cash assistance to women delivering in public health facilities is not limited by age or number of children.[74] Women who choose to deliver in their homes are given 500 rupees (US$10). But such cash assistance for home deliveries is limited to women above age 18 and with up to two live children.
Critiques of the Government's Approach to Maternal Health
NRHM has resulted in greater attention to maternal health but many government officials and civil society groups have concerns about the government's approach. They argue that poor accountability adversely affects not only planning based on women's health needs but also the implementation of existing maternal healthcare interventions. These gaps in accountability manifest themselves in many ways, notably recurrent health system or programmatic gaps and a lack of government action to ensure that health programs are actually reaching pregnant women from marginalized communities including the poor, Dalit, other backward classes, religious minorities and tribal communities, or women in geographically remote areas. Furthermore, activists say that poor monitoring and attention to the supply-side coupled with the spurt in demand for institutional deliveries has resulted in substandard maternal health care at these facilities.[75]
Moreover, state governments' pattern of unspent NRHM funds buttresses calls for better accountability by activists and doctors.For instance, millions of dollars in government funds for health care in Uttar Pradesh go unspent each year. A study for the Indian Planning Commission shows that roughly 40, 40, and 30 percent of the amount allocated under the NRHM to the Uttar Pradesh government went unspent in fiscal years 2005-06, 2006-07, 2007-08[76]. In February-March 2009, activists in Uttar Pradesh claimed that nearly "700 crore rupees [US$140 million]" remained unspent even though it was almost the end of fiscal year 2008-2009.[77]In a January 2009 letter to 71 district chief medical officers, the Uttar Pradesh NRHM Mission Director urged each of them to spend "30 lakh rupees [US$60,000]" within two months, that is, by the end of March 2009.[78]
Health experts and activists have also expressed concerns about the effectiveness of existing government strategies to improve maternal health. While the JSY has improved access to health care during deliveries, many groups argued that the Indian central and state governments are not taking adequate measures to address unsafe abortions-a significant cause of maternal mortality in India. Even though the NRHM guarantees safe abortion services in public health facilities, and abortions are allowed in accordance with the Medical Termination of Pregnancy Act, in practice, little is being done to promote awareness and access to these services. Furthermore, health care to address maternal morbidities, which affect thousands more women leaving many disabled for life, is not given the attention it requires. What was intended to be a cash assistance integrated with antenatal and postnatal care, in practice, operates as a cash incentive to increase women's demand for facility-based deliveries without information on birth preparedness.[79]
Women's rights and public health experts caution that the government's interventions to improve maternal health are too vertical, ignoring concerns about the overall health of women during their life-cycle, including the underlying determinants of girls' and women's health and their other rights including food, potable water, employment, and access to contraceptives of their choice.[80] The underlying determinants of health influence maternal health care. Dr. Sundari Ravindran, a leading public health expert on the reproductive and sexual health of women, said that in many areas of India, women are likely to experience a far higher rate of pregnancy-related complications requiring emergency obstetric care than the global average of 15 percent.[81] This is because of their overall poor health resulting from poor nutrition and anemia and has implications for the number of facilities that need to be equipped with comprehensive emergency obstetric facilities.
Further, activists repeatedly emphasize that vertically run programs, notably polio eradication, have had negative outcomes, which should not be replicated in maternal healthcare programming.[82] One of the main adverse outcomes of the polio eradication campaign is that field-based health workers spend a large part of their time on it, forcing other health concerns into the backseat. For instance, senior officials from the Uttar Pradesh Directorate of Family Welfare concede that "[p]ulse polio-all focus is on this project and other programs are neglected."[83] A study commissioned by the Uttar Pradesh Health Systems Development Project quotes a USAID study in Uttar Pradesh saying that one of the many challenges to maternal health care is that "National programmes such as Polio eradication [are] consuming half of health functionaries time."[84]
Moreover, many feel that the government mistakenly continues to approach the reproductive and sexual health of women within an overarching framework of "population control or stabilization." The government has not taken measures empowering women to make informed, autonomous, health-related decisions, especially about use of contraceptives or facilitated use of contraceptives that encourage male participation.[85] They point to the government's sterilization program, noting that field-based health workers spend a considerable amount of their time on sterilization without providing information about non-terminal contraceptive methods.[86]
Several women and men from rural Uttar Pradesh reported seeing ASHAs or nurse-midwives only during polio drives or complained that they received prompt assistance only when they wanted to get themselves sterilized.[87] For instance, Vimala V. died after delivering at home and Revati R., a relative who was present at the time of delivery, said she had died without assistance from any health worker. Revati R. explained: "If you tell her [health worker] that it is for sterilization, then they will go to any length to help you-will arrange their own vehicle and take you to the hospital. But if you say that it is for something else, they will not even turn around and look at you."[88]
The "population control" approach has found its way into the JSY as well. In the non-Empowered Action Group states, JSY benefits are restricted to women above age 19 for up to two live births.[89] Likewise, cash assistance for home-based deliveries is restricted to women above age 19 and up to two live births. This shortchanges the medical needs of young mothers and pregnant women with multiple pregnancies.
Finally, the private sector continues to play a significant role in providing healthcare services, including obstetric services. About 64 percent of women go to private healthcare providers for complete antenatal care and about 20 percent of all deliveries occur in private health facilities.[90] Many activists said that the absence of regulation of the private sector posed a significant challenge to ensuring affordable quality maternal health care to all women.[91]
The Importance of Accountability
Accountability is the "raison d'être of a rights-based approach" to health care.[92] Often it is mistakenly equated with blame and punishment of individual medical staff and frontline health workers. While individual responsibility is important in appropriate cases, accountability also includes assessing the performance of district-level planning and decision-making and identifying systemic flaws that need to be rectified. This requires effective monitoring and tracking of progress and obstacles, followed by action holding planners and decision-makers accountable so that policies, programs, and practices are improved.
Several processes enhance health system accountability. First the state should ensure that systemic problems with the provision of health care are identified and fixed instead of being repeated. If despite decades of programming for maternal health, women continue to die because of poor access to emergency obstetric care, inadequate referral systems, or lack of continuity in antenatal and postnatal care, this indicates a failure in planning and implementing maternal healthcare programs. Constructive changes should be made to break the cycle of health system shortcomings by monitoring implementation, replicating successful health interventions, and identifying and rectifying those interventions that do not work.[93] This will enable states to make the most effective use of their resources.
Another thread of accountability is grievance redressal. Ensuring women have access to effective mechanisms to address complaints and concerns about treatment that they have experienced whilst accessing healthcare services improves implementation as well as public trust in health facilities. Such grievance mechanisms should be capable of identifying through a fair and transparent process whether there is culpable behavior on the part of particular individuals, but the mechanisms should also contribute to identifying the full extent of the state's liability for any harm sustained by women when they seek to access maternal health care. This means that the mechanisms must examine not only the decisions of individual front line actors, but also whether the authorities have put into place appropriate systemic measures to minimize, to the greatest extent possible, any risks to life or health of pregnant women. If authorities are found negligent in failing to take such measures, there should be consequences.
Accountability also necessitates that states make progressive improvements in delivery of maternal healthcare services over time in accordance with their international human rights obligations. Governments should monitor progress in maternal health care by gathering data based on appropriate indicators, including pregnancy-related deaths. And such monitoring should occur at all levels-international, national, state, and particularly at the district level where there is power to plan, review, change, and implement schemes within the public health system. Tracking progress in maternal health care over time requires both short-term and long-term monitoring, and should apply to public and private healthcare sectors.
III. Recurrent Health System Gaps Reflect Accountability Deficits
Despite commitments toprovide free antenatal care, basic and comprehensive emergency obstetric care, and postnatal care, Indian authorities have not done enough to review existing schemes to ensure that they address the real health needs of women and girls. In our research, we found recurrent gaps in the provision of maternal health care, gaps that would not exist if policies were being implemented effectively. These include barriers to emergency care, poor referral practices, gaps in continuity of care, and improper demands for payment as a condition for delivery of healthcare services.
As noted at the outset of this report, the analysis that follows draws heavily on Human Rights Watch research in Uttar Pradesh. While not all of our findings will apply uniformly to all parts of India, we believe that they are particularly relevant to the eight Empowered Action Group states.[94] Discussions with public health experts and women's health rights activists have revealed that financial barriers to care are also common to many non-Empowered Action Group states.[95]
Poor Access to Emergency Obstetric Care
The vast majority of women in rural India have poor access to emergency obstetric care that could save their lives, including blood transfusions and cesarean sections.[96] Women with pregnancy complications such as hemorrhage, obstructed labor, and eclampsia are often in need of such life-saving care. First referral units that are supposed to be equipped with such life-saving facilities have existed on paper for years, even before the NRHM was operationalized.[97] Since mid-2005, basic and comprehensive emergency obstetric care are covered by the NRHM service guarantees. Yet, there has been little or no improvement in women's access to and utilization of such care in many parts of India,[98] indicating a serious lapse in accountability.
The Indian government has acknowledged these serious gaps in its surveys and review reports. The latest government District Level Household and Facility Survey paints a dismal picture in Uttar Pradesh. Uttar Pradesh is 583 short of the required number of community health centers;[99] less than a third of those that are in place have an obstetrician or gynecologist. In practice, roughly one in twenty first referral units (FRUs) offer cesarean sections and one in a hundred have blood storage facility.[100]
In its Third Joint Review Mission, a team led by the Indian Ministry of Health and Family Welfare found that none of the first referral units was providing emergency obstetric services as mandated.[101] Similarly, the Second Common Review Mission led by the Indian central government found that "out of 108 functional FRUs in the state ... blood storage facilities are non-existent."[102] These numbers have reportedly improved: in March 2009, one of the officers from the Uttar Pradesh NRHM State Project Management Unit claimed that at the beginning of financial year 2008-2009 (April 2008) only 23 of the 426 community health centers were first referral units, compared to 100 first referral units at the end of the financial year (March 2009). Stating that they had recently placed an order for blood storing facilities for 140 community health centers, the officer asserted that all district hospitals had blood storage and transfusion facilities. When Human Rights Watch specifically enquired whether there were any complaints about the lack of such facilities at district hospitals, the officer said, "No complaints from district hospitals on blood."[103]
Contrary to the official claim, activists, health workers and doctors, and families from two districts neighboring Lucknow city, the capital of Uttar Pradesh, reported that women requiring blood transfusions or cesarean sections were routinely referred to Lucknow city about 100 kilometers away.[104]
A doctor at the Unnao district hospital confirmed that their facilities were inadequate, often necessitating referrals to Kanpur or Lucknow:
[We have] [n]o surgeon in the female ward. This is a combined hospital [for men and women]. So many times a surgeon is not available. Blood is another reason. We have a blood bank. But not enough blood.[105]
In southern Chitrakoot district, the district hospital that is supposed to be equipped with comprehensive emergency obstetric facilities did not have them in March 2009.[106]The staff at the hospital described their predicament:
We do not have a gynecologist now. No blood facility. So if there is any case that needs blood we refer the case to Allahabad hospital-Sadguru Sewa Trust ... Only normal cases [unassisted deliveries and episiotomy cases] are taken here. We do not take critical cases. In my time [more than two years], we have had only one cesar case [cesarean] performed.[107]
As a result, many women who needed such care were referred to the Allahabad medical college hospital, more than 100 kilometers away, without support for referral transport.[108] The journey from Chitrakoot to Allahabad takes between three and four hours. The staff at the Chitrakoot district hospital did not know the outcome of such referred cases but remarked that it was possible that women had died in transit or at the Allahabad hospital.[109]In the last year about 1270 "complicated cases" were referred from the district hospital.[110]Human Rights Watch was able to trace one case in which the family of a pregnant woman who had been referred had taken her all the way from Chitrakoot district to Allahabad for a blood transfusion. The woman, Munira M., died at the Allahabad hospital because of complications.[111]
Munira M.'s death, Chitrakoot district, June 2008 Munira M., belonging to the Chamar caste (a Dalit community), was a mother of two children. Both her deliveries were conducted at home. She started bleeding in the eighth month of her third pregnancy, that is, in June 2008. No ASHA or ANM had visited the village and her relatives believed it was because no one was appointed for the village. Her family rented a tractor and took her to a private hospital nearby, where she was referred to yet another private health facility. Saying that she needed a blood transfusion that they could not provide her in Chitrakoot district, the staff at the second private hospital asked the family to take Munira to Allahabad, more than 100 kilometers away. Both mother and baby died in the Allahabad medical college hospital. |
Manasa M., an ANM, had attended to Renu R.'s delivery in late May 2009 at a primary health center. Renu delivered but started hemorrhaging soon after and needed to be taken more than 30 kilometers away for a blood transfusion. Underscoring the importance of improving the availability of blood transfusion facilities, Manasa said:
There is no facility for blood over here. It is in Barabanki. Barabanki I think has only one blood bank. Sometimes whenever there is an emergency, [there is not enough blood in Barabanki] and the patient has to go to Lucknow, if in a PPH [post partum hemorrhage] case they have to go all the way there....[112]
Even where there are blood transfusion facilities, it appears that affordability is a significant barrier to access.[113] Human Rights Watch spoke with one pregnant woman who was receiving a blood transfusion at a district hospital in Uttar Pradesh, and found that she was not able to afford the six units of blood that she needed. Each bottle of blood cost her family 900 rupees (US$18).[114]
Access to blood transfusion facilities and availability of cesarean sections often means the difference between life and death for women. While the Indian central and Uttar Pradesh state governments have taken some steps to improve women's access to such services, they are yet to continuously monitor implementation and rectify insufficiencies. As a result, women continue to die.
Poor Referral Systems
What's the point of sending us away? If the doctor cannot deal with the case here, then why should we go to the doctor? For the 1400 rupees [US$28]? Are we going all the way to kill ourselves?
- Trishna T., woman who had recently delivered, Chitrakoot district, March 7, 2009.
Poor referral systems leave women running from pillar to post even during emergencies. Of the nine deceased pregnant women's families that Human Rights Watch spoke to, five recounted serious obstacles in even reaching a health facility and being referred from one to another without any support. For women who develop complications during pregnancy and childbirth and in need of life-saving interventions, time is crucial. On paper the NRHM guarantees free referral services at primary, secondary, and tertiary levels.[115] But poor government oversight over referral systems leaves many women without timely appropriate emergency health care. As one UN expert group concluded: "[Even an] elegant model of poor referral from facility to facility could be worse than inefficient. It could be deadly."[116]
Pregnant women use bicycles, motorcycles, theliyas (handcarts), auto-rickshaws (motorcycle taxis), tractors, and jeeps to reach health facilities.[117] Often, families living in interior areas are unable to afford tractors or jeeps or find it difficult to organize such transport from their villages. In such cases the women deliver at home without any referral support.[118]
In January 2008, Vimala V. bled to death on the way to a health facility. She was being rushed to a health facility on a handcart because the family could not arrange for any other mode of transport.[119] She had delivered at home and started hemorrhaging, but had no referral back-up.[120]
Vimala V.'s death, Rae Bareilly district (Story as told by Vimala's relatives and neighbors) Vimala V., in her 20s, was pregnant for the first time. She developed labor pains at home at night. At midnight she delivered at home with the help of neighbors. No health worker was present. According to Vimala's relatives and neighbors, the ANM and ASHA assisted them only for teekakaran (immunization) and nasbandi (sterilization). Vimala was unable to deliver the placenta after her delivery. She started bleeding heavily. It took the family about two hours to arrange for a theliya (handcart) to take Vimala to the government health facility. Vimala died en route. Her husband and relatives now care for her baby. |
ASHAs and ANMs sometimes use their personal motorcycles to transport pregnant women in labor to hospitals. Reena R., an ASHA, described how she often asked her husband to help transport pregnant women in labor to the nearest community health center when they could not arrange better transport. "My husband rides the [motor] bike, the pregnant woman sits in the middle, and I behind her," she said. "Three people on one bike, it is difficult but we have to manage," she explained.[121]
Poor access to affordable transport is exacerbated by repeated referrals from one facility to another. Even when families reach health facilities, it is often not equipped to provide the required care. Several doctors and nurses described how families of pregnant women often fell at their feet, begging to be admitted into the health facility because they could not arrange to go elsewhere for appropriate care.[122]
Nirmala N., a staff nurse at a community health center, described how they referred Kanti K., a pregnant woman, to the nearest first referral unit. But Kanti and her family returned to the community health center later the same day, surprising the health staff. Nirmala explaining why: "From Bachrawan [first referral unit] they sent the case to the Rae Bareli hospital and from there they were asked to go to Lucknow hospital. They could not afford to go there [Lucknow] so they came back here."[123]
Nirmala was there when the family came back, begging to be readmitted. She explained that the staff in the female ward refused readmission because they lacked the requisite expertise and facilities. She said,
But they [family] started falling at the doctor's [superintendent of the community health center] feet and holding his hand and leg. So out of mercy he took her and got her admitted. Not into our ward [female ward]. We said no. So he took her into the male ward. She died. He did not want her to die on the road. There is nothing we could have done in that case. We do not have the facilities here.[124]
In November 2008, Pragya P. died in the community health center. Sita S., her mother-in-law, recalled that that the community health center staff had informed her that they did not have the facilities to conduct Pragya's delivery and demanded money. But Sita asked the thakur (an influential person in the region, literally; landlord) to intervene and plead with them to admit Pragya. "Later on, [the nurse] said she would save the mother but not the child and we agreed," Sita explained. Pragya died in the community health center due to poor access to emergency obstetric care.[125] Angered by the experience, Sita's daughter who had accompanied her, vowed, "I will never go to the hospital. You can take my life but I will not go the hospital."[126]
One of the nurses at the community health center confirmed Sita's story. According to her, the health staff had asked that Pragya be taken to the Rae Bareilly district hospital about 30 kilometers away. The staff nurse claimed that there was an ambulance, but stated that it was left to the families to negotiate the payment with the ambulance driver, in violation of the free referral guarantee.
Eight days after a facility-based delivery, when Kavita K. developed complications at home, her father-in-law took her to the community health center for treatment. He narrated his harrowing experience:
We took her to the community health center and they said, "We cannot look at this here." So we took her to [the hospital in] Hydergad. From Hydergad to Balrampur, and from there to Lucknow-all government hospitals. From Wednesday to Sunday-for five days- we took her from one hospital to another. No one wanted to admit her. In Lucknow they admitted her and started treatment. They treated her for about an hour and then she died.[127]
In June 2009 Human Rights Watch documented another maternal death in Barabanki district. The death occurred due to complications arising from hemorrhage, which apparently could have been averted had there been a better referral system.[128] Within 45 minutes of arriving at the Barabanki district women's hospital on a Monday morning, Latha L. died as the staff was organizing a blood transfusion. Recalling what he told a doctor at the district hospital, Latha's neighbor said, "We had gone to the PHC [primary health center] the previous night in a tractor. The PHC did not send us here [district hospital] on time. The ambulance was standing there [primary health center]-the white vehicle [but it did not bring us]."[129]
The back story was all too familiar and tragic. Latha had just completed eight months of pregnancy. She started bleeding profusely when she went to relieve herself on Sunday evening. "It was flowing, flowing-what can I tell you? There was so much blood. I got scared," whispered Latha's aunt, Warisha W., who went with her to the primary health center in the village tractor. The gates of the PHC were closed. They waited for the health staff to come and look at her. The PHC staff said they could not treat her and instructed them to take Latha to the Barabanki district women's hospital, about 40 kilometers away. The PHC did not provide any first aid to Latha. They did not offer any transport assistance.
According to Warisha, Latha was in too much pain and bleeding too profusely to be jolted along a one hour drive in a tractor to Barabanki district hospital. The family wanted some immediate medical assistance because of her condition. "They did not give her any medicine. Could they not have even given her something to help her until we reached another hospital?" asked Warisha, of the primary healthcare staff. Out of concern for Latha's condition, Warisha explained that they decided to take Latha to a private nursing home close by. They reached the nursing home late Sunday night, where she was kept overnight and discharged because they could not make arrangements for her blood transfusion.
It is unclear how well different public and private facilities are connected in the referral chain or by referral transport in Uttar Pradesh. In the cases we studied, ambulances were present at times, but families were either not aware of the service or could not afford it. A 2008 USAID-funded study in Uttar Pradesh shows that 45 percent of the community health centers surveyed in the study did not have funds to operate even the one ambulance they had.[130] Several district chief medical officers said that the Uttar Pradesh government has piloted referral transport through a network of ambulances in a few areas.[131] We spoke with one such ambulance driver who explained how he was permitted to transport patients only up to the district hospital and if the patients were turned away he was not authorized to drive them to another hospital within or outside the district. He said, "If the patients beg me, out of mercy I take them to a nearby private facility. They have to pay me extra money."[132]
Gaps in Continuity of Care
Women in Uttar Pradesh seldom receive continuous care during and after termination of pregnancy, through the postnatal period (extending 42 days from termination of pregnancy).
Contrary to NRHM standards which require every pregnant woman be registered, provided with antenatal care, and taken to a pre-identified health facility for delivery, many pregnant women and women who had recently delivered told Human Rights Watch that they seldom had regular contact with ASHAs or nurse-midwives in the antenatal period.[133] Others said their contact was limited to receiving iron and folic acid (IFA) tablets and anti-tetanus injections, and there was seldom any birth-preparedness care.[134]
Norms for antenatal care go far beyond distribution of IFA tablets and anti-tetanus injections. However, government surveys show that the entire package is seldom provided.[135] Activists and many doctors and nurses experienced in conducting deliveries repeatedly told us that pregnancy-related morbidity, particularly anemia, is a major concern; ASHAs and ANMs often are not providing or facilitating adequate antenatal care.[136]
A gynecologist who routinely conducts deliveries in Chitrakoot district said that she believed 95 percent of the women she saw were severely anemic. Even a slight delay in treating women with severe anemia reduced the chances of their surviving any crisis, the doctor explained.[137] Another gynecologist working at a government district hospital said,
You want to prevent maternal mortality, yet nobody is bothered about antenatal care ...Even if there is any antenatal check-up, the focus is on injections [immunization] and some iron tablets. ASHA does not give any information about check-ups and physical examinations. What about all the suffering of the pregnant woman during the nine months?[138]
Voicing similar concerns about antenatal care, a staff nurse at a community health center said, "Often we deal with cases where the woman comes for her first check-up when she is nine months pregnant and is in labor. And on top of that many of them are really anemic, only three or four grams blood [referring to hemoglobin levels]."[139]
A staff nurse from a different community health center said,
I see so many cases of APH [antepartum hemorrhage or bleeding during pregnancy], placenta previa [low-lying placenta that can cause bleeding], and malnutrition. Most of the women who come here are those patients who do not have any ANC check- ups. We do not know their [medical] history.[140]
Care in the immediate postnatal period (24-72 hours after childbirth or abortion) is critical to averting maternal deaths; deaths are highest in the postnatal period.[141] Postnatal care also helps women address both short-term and long-term health issues arising out of pregnancy and childbirth.
The NRHM guarantees a minimum of 2 post-partum care visits within 48 hours and another visit within 7-10 days of termination of pregnancy. [142] But government data reveals that such care is seldom provided.[143]
None of the women with whom Human Rights Watch spoke reported any contact with a health worker after delivery, that is, either after they were discharged from a health facility or after they had a delivery assisted at home.[144] Several women who had delivered at primary or community health centers reported being discharged from the health facility within 24 hours. Rohini R., for instance, who had delivered at a primary health center in Barabanki district was discharged within two hours of delivery.[145] Shanta S., who had accompanied her relative, Sunidhi S., to a community health center for delivery said:
[Sunidhi] delivered yesterday. It was a normal delivery in the CHC [community health center] ... ASHA took us there. I was also there. ... We took her to the hospital at 8:30-morning-and she delivered within two hours around 10:30 ... She was discharged in the evening.[146]
Human Rights Watch documented four maternal deaths in the postnatal period. In all cases the families reported that no health worker visited or assisted the mother in this period.[147]
Many factors contribute to the poor state of antenatal and postnatal care, and a discussion of all of them is beyond the scope of this paper.[148] Nevertheless, we were struck by the frequency with which doctors and activists mentioned the amount of healthcare worker time taken up by polio eradication and sterilization programs as cause for concern.[149]
Financial Barriers to Care
The cost of healthcare services, including emergency obstetric care continues to remain a barrier for many poor families. The NRHM framework recognizes "exemption...of below poverty line families from all charges" as an important strategy and guarantees free care to such families.[150] Likewise, in many states JSY benefits depend upon whether the beneficiary is below or above the poverty line.[151] Many activists stated that one of the biggest barriers to benefiting from government healthcare schemes is the non-issuance of government cards certifying poor families as below the poverty line (BPL cards).[152] Explaining how she finds it hard to help poor women, one ASHA said, "The people who are really poor don't have these things [BPL cards] and many others who are better off have BPL cards. So that is a big problem."[153]
Many activists, women from rural areas, and ASHAs in Uttar Pradesh consistently complained to Human Rights Watch that staff in government health facilities demand money for supposedly free services under the NRHM, including out-patient and in-patient care, and drugs.[154]
This was sometimes a bribe. Explaining how the care she received during pregnancy depended upon the money she had, Trishna T. said,
I have never had a check-up [referring to a physical examination during pregnancy] ... Nurse didi [showing respect, literally "elder sister"] has not called us for any check-up. If we have money, then we can go to the doctor and he will look at us. If we don't have money then we can be dying in pain. Just left to be lying in pain. It's like that.[155]
Niraja N., an ASHA explained:
Nothing is free for anyone. What happens when we take a woman for delivery to the hospital is that she will have to pay for her cord to be cut... for medicines, some more money for the cleaning. The staff nurse will also ask for money. They do not ask the family directly ... We have to take it from the family and give it to them [staff nurses] ... And those of us [ASHAs] who don't listen to the staff nurse or if we threaten to complain, they make a note of us. They remember our faces and then the next time we go they don't treat our [delivery] cases well. They will look at us and say "referral" even if it is a normal case.[156]
One activist who unsuccessfully intervened when a staff nurse at a CHC demanded money said,
One man I know had taken his wife for delivery to the CHC. He had sold 10 kilos of wheat that he had bought to get money to bring his wife for delivery. He had some 200-300 rupees [US$4-6]. Now in the CHC they asked him for a minimum of 500 rupees [US$10]. Another 50 [rupees] to cut the cord and 50 [rupees] for the sweeper. So he started begging and saying he did not have more money and that they should help for his wife's delivery. I... asked them why they were demanding money. The nurse started giving us such dirty abuses that even I was getting embarrassed and wanted to leave. You imagine how an ordinary person must feel who wants help.[157]
Several health workers stated that demands for high sums of money were particularly a problem where women came for abortion-related services. Under the NRHM, abortion services in accordance with the law are also guaranteed free of cost to women below the poverty line. For example, one ASHA said of the staff in the government community health center:
Sometimes they charge up to 5000 rupees [US$100] for abortion. Other cases 300 rupees [US$6] after one month, 600 rupees [US$13] after two months... it goes on like that. They do it properly so even though they charge money I convince women to come here. At least they are safe instead of going to a jhola chaap doctor [unqualified doctor].[158]
Many government officials and hospital staff explained to Human Rights Watch that, if money is exchanged, it is because women from rural areas follow nyauchawar, a custom under which they give money when a baby is born. If women in rural areas are happy to follow such a custom, they reasoned, then there is no cause for the state government to intervene to stop the payments. Such an argument to justify service providers demanding payment from vulnerable women without a lawful basis should not be condoned, but it is all the more egregious given that it seeks to justify behavior that leads to women being denied timely medical assistance.
The government has itself guaranteed free basic and comprehensive emergency care to poor rural women under the NRHM, and extralegal demands for monetary contributions should be seen as unlawful whether termed payments or customary shows of gratitude. Any expectation that money must be handed over in order to receive care, or the best attainable care, will disproportionately affect those in no position to pay-women from poor and marginalized communities. The government has a duty to prevent or put an end to such practices which will inevitably intimidate poor women and girls.
IV. Improving Accountability: The Critical Need for Better Monitoring and Timely Investigations
While Indian authorities have taken steps to improve healthcare system accountability, existing approaches have not done enough to ensure that they know where the problems are. The key issue here is effective monitoring: using district-level investigations and appropriate monitoring indicators to obtain the data needed for effective interventions to reduce maternal mortality and morbidity.
Central and state authorities often point to the number of facility-based deliveries as an important measure of progress. While this is a partly useful measure-facility-based deliveries do correlate with reduction in maternal mortality if certain preconditions are met-it is by no means sufficient and officials have relied on it too much.
We believe that more attention must be given to timely district-level investigations into maternal deaths, to use of so-called "UN process indicators" on emergency obstetric care, and to improved reporting of deaths, including through the civil registration system (which records key life cycle events such as births and deaths). This chapter, drawing heavily on Human Rights Watch research in Uttar Pradesh, analyzes shortcomings in these areas.
Poor District-level Monitoring
Monitoring at a level "where there is power to effectuate change"[159] is key to rectifying health system shortcomings. UNICEF has observed that a "national policy requiring specific notification of maternal deaths" would be a powerful tool in reducing maternal mortality.[160] Public health experts and researchers have shown the utility of investigating maternal deaths to get a better understanding of and information about the socio-economic and medical causes of maternal deaths.[161]
Under the NRHM, the Indian central government has recognized that maternal death investigations are a powerful "monitoring tool" at the micro level,[162] reiterating that "reduction of IMR/MMR will also be closely monitored through social audit." The erstwhile RCH-II program now part of the NRHM also requires the collection of information on maternal deaths. In practice, however, such data collection and processes have thus far played little or no role in planning and evaluating maternal healthcare interventions in Uttar Pradesh and many other parts of the country.
The Indian central government and many states have taken concrete steps to improve surveillance of maternal health. Dr. Jorge Caravotta, health specialist from UNICEF India, said,
The Ministry of Health and National Health Systems Resource Center are [working] with UNICEF, UNFPA, WHO to create a maternal surveillance system in the country. Facility and community-based maternal death audits now will be a tangible reality in the field to improve health systems and reduce maternal mortality. The Indian government is taking steps to develop implementation guidelines for this purpose. Ten states have included maternal death audits in the state project implementation plans."[163]
Effective investigations of maternal deaths must be designed to identify systemic issues in healthcare provision which may be causal factors in maternal deaths, particularly among women from marginalized communities.[164] The UN Special Rapporteur on health, after his visit to India in 2007, underlined the utility of such investigations. Urging all states to introduce a system of maternal death audits, he stated that it is of "utmost importance that all the circumstances of maternal deaths be examined in order to find out why the death occurred ... [T]hey can help to identify the structural and systemic failures that are leading to women's preventable deaths."[165]
Barriers to Accurate Reporting of Maternal Deaths
Even though the Uttar Pradesh state government is yet to include maternal death investigations in its state project implementation plans, it has demonstrated its commitment to monitoring adverse pregnancy outcomes through three important initiatives. First-in a pre-NRHM initiative-the government issued a 2004 governmental order requiring maternal death audits, but it was not implemented.[166] Second, in 2007 the state government, through the World Bank funded Uttar Pradesh Health Systems Development Project, undertook a pilot "Maternal Death Notification and Review System."[167] Third, the state government is in the process of launching UNICEF's Maternal and Perinatal Death Enquiry and Response (MAPEDIR) initiative in several districts.[168]
As the Uttar Pradesh government gears up to implement the recently launched the NRHM Health Management Information System (HMIS) and develops initiatives to investigate maternal deaths, it needs to address the gaps in its reporting systems to ensure accurate data collection, particularly on maternal deaths irrespective of place of death-home, en route a health facility, public or private health facility. Health officials should avoid the same pitfalls that plagued the implementation of the 2004 government order. A former senior health official explained that committees to conduct maternal death audits were created and ANMs were supposed to report deaths, "but communities were not involved and no information was given to anyone."[169]
Poor political commitment and priority for such data, a lack of awareness about the objective and importance of such reporting, a lack of adequate training for health workers to implement the maternal death audit system, and underreporting of deaths due to fear of punitive action were cited as reasons that hampered the implementation of the government order.[170] A "lack of a standardized, effective and efficient information system which also includes maternal death tracking for planning, monitoring, and action... is one of the major challenges" for maternal health in Uttar Pradesh.[171]
The Uttar Pradesh state government should immediately address the problem of gross underreporting of maternal deaths. A pilot study conducted by the Uttar Pradesh Health Systems Development Project in a few blocks across four districts identified roughly 380 deaths within six months.[172] While one area registered 100 percent reporting, most areas were found to have average, below average, or poor reporting of maternal deaths.[173] A nongovernmental organization identified 60-70 maternal deaths in one block of a district (administrative area with 100,000 to 300,000 population) between 2006 and 2008.[174] Human Rights Watch spoke with three of the families who had suffered maternal deaths in 2008.[175] The district medical authorities were not aware of any of these deaths. Instead, when pressed, they provided cursory "unofficial" informationaboutfour or five deaths in the whole district (group of blocks) for 2008; the official record reported "zero" maternal deaths.[176]
When asked about the number of maternal deaths in his district in 2008, another district health official said,
Number of maternal deaths-now that is a million dollar question. None reported. But we have heard of 12 or 13 maternal deaths through word of mouth. There was one in the district hospital ... In those other 11 cases, they are afraid to report deaths, they think it will give them a bad name.[177]
Similarly, in Chitrakoot district, the official report showed that there were no maternal deaths for the past year,[178] but Human Rights Watch documented several maternal deaths.[179]
Rae Bareilly district exhibited a better system of reporting deaths. District health records from April 2008 to January 2009 showed 107 maternal deaths, including two deaths in January 2009.[180] The district health official who showed us the records said that the data suffered from underreporting, and was eager to compare the government figures with those generated by PATH, a nongovernmental organization documenting maternal deaths in the region.[181]
Unless deaths are reported, they cannot be investigated and acted upon. The recording and reporting of maternal deaths at so-called sub-health and primary health centers is a "service guarantee" under the NRHM.[182] But to translate guarantees on paper into a "culture of reporting, investigating, and acting on maternal deaths," the government should create an enabling environment, dismantling the barriers against reporting and investigating maternal deaths.[183]
Low Priority for Data on Maternal Deaths
Poor "demand from above" for information on maternal deaths, activists and government officials felt, was a key reason for the poor state of reporting and investigation of such deaths at the field-level.[184] An expert group that conducted a maternal death notification pilot study for the Uttar Pradesh Health Systems Development Project found that "reporting and recording deaths is not a priority for any department,"[185] and that there was "poor initiative from health sector on notification [of maternal deaths] activity."[186]
"There is no data on maternal deaths because no one bothers to collect it," said Dr. Neelam Singh, a Lucknow-based gynecologist and activist experienced in investigating maternal deaths. Health workers on the field responded to what she called "the danda [stick] approach-if the data is demanded from the top, then only the district officers will get into action and put pressure on their juniors to give such data."[187] Many activists and government officials used the polio eradication campaign as a "classic example" illustrative of the top-heaviness of the health system. Cautioning that the coercive element of the polio eradication campaign merits attention and should not be repeated, several health experts and government officials stated that the key lesson from the polio eradication campaign was that it demonstrated that the public health system can be made to work.[188]
The low priority given to data on maternal deaths became evident to Human Rights Watch when senior officials from the directorate of family welfare appeared unaware of their own reporting formats. What directorate officials told us was directly contradicted by workers in the field.
One senior official told us: "This information [maternal deaths] doesn't come to us because we don't get this through the pro forma. We don't have a column for maternal deaths."[189] Describing what he called an error, one health official explained 2008 revisions in their reporting formats. He said,
When we used to have CSSM forms [Child Survival and Safe Motherhood forms], under "Surveillance" we used to have a maternal deaths column. From last year we have given new forms-called routine immunization now- but most of the data collected in this form is also the same-about deliveries also. But the maternal deaths column in this form is missing-I think it got left out by mistake.[190]
Health workers and district-level officials, however, say they are required to provide maternal mortality data to the directorate. One district official showed Human Rights Watch a form titled "Monthly Report to Monitor, Components of M.C.H. Programme."[191] This form contained a column labeled "number of mothers died out of the above," against which district officials are expected to furnish information for the current month, as well as an aggregated total from April of the preceding year. The February 2009 report submitted by one district under this format showed that they had "nil" deaths from April 2008 even though doctors and families shared with Human Rights Watch at least three cases of maternal deaths in this district between April 2008 and February 2009. This indicated that either the district officials were completely unaware of the number of maternal districts in their district or that they were suppressing information about such deaths.[192] ASHAs and ANMs also showed Human Rights Watch their reporting registers that carried a column for recording maternal deaths.[193]
Several health workers reported, however, that they were not asked about maternal deaths during staff meetings. For instance, describing her monthly review meetings, one ASHA said,
[E]very month we [ASHAs] have a meeting in the CHC. All ASHAs are called. At this meeting we discuss nasbandhi [sterilization] and teekakaran [immunization]. Nothing else.[194]
Similarly, explaining how her review meetings were conducted, an ANM said,
[Our] supervisor meets about 20-25 ANMs together. Issues surrounding maternal deaths are not discussed. Last year there was a maternal death in the CHC ... I do not know more details. This case was not discussed in our ANM meeting.[195]
A staff nurse who reported a recent maternal death in her health facility in January 2009 said, "This death case was not shared in any common meeting. We don't have any [such] system."[196]
District health officials stated that they collect information through field-based health workers and generate monthly reports about the number and place of deliveries.[197] The fact that the same district health machinery regularly generates estimates of deliveries and place of delivery, but repeatedly shows near-zero reporting for maternal deaths is indicative of the poor priority and demand for such data.[198]
Several Uttar Pradesh health officials claimed that they struggled to improve their reporting because of their large population. Dr. T. Sundararaman of the National Health System Resource Center, however, felt that population was not a barrier to improving reporting mechanisms. He said that political will and better governance were required to improve data collection.[199] Similarly, Dr. Vishwajeet Kumar, an expert on infant and maternal mortality said that governance, not population, was the issue. He said, "underreporting is a consequence of un-intentioned methodological limitations and seemingly deliberate administrative opaqueness to maternal deaths."[200]
Lack of Definitional Clarity and Inadequate Training
Kavita K. developed complications and died in December 2008 about two weeks after her delivery.[201] Health officials were likely oblivious of her death because of several reasons-one of them as simple as poor awareness of the definition of a maternal death.
Accurate reporting of maternal deaths requires definitional clarity. Many field-based health workers stated that they were the primary sources of information about maternal deaths in villages.[202] Even though ANMs are primarily responsible for the care of pregnant women, many health workers reported relying on each other for information regarding pregnant women and maternal deaths.[203] Almost all of them, including ANMs and anganwadi workers with more than 20 years experience, were unfamiliar with the definition of a maternal death.[204]
Identification of a maternal death hinges on two things: its timing and cause. Depending on when a pregnant woman dies-either during pregnancy or within 42 days after termination of pregnancy (postnatal period)-the death is classified as pregnancy-related.[205] All such deaths are then filtered by medical cause, determining whether the pregnancy had any direct or indirect role in the death.
Maternal deaths are most frequent in the postnatal period, that is, within 42 days of termination of pregnancy.[206] But where health workers are not trained to track and report any pregnancy-related death for the entire period within which they are likely to occur, particularly the postnatal period, deaths will go unreported or misclassified. Health workers from three districts we visited gave varying descriptions of the postnatal period, ranging from a few hours after delivery to a month.[207]
Ratna R. and Kishori K., anganwadi workers who are charged with providing nutritional supplements to children and pregnant women in rural areas, said they kept 15 different registers. In one of them, which they described as the "birth and death register," they said that they were supposed to record details of deaths. One said,
In this we note down the name of the person who died, date of the death, age, reasons-we note down if it is a child, but adults also sometimes we note down. If it is a pregnant woman who died then we note it down-we have to report it-any death during delivery or after delivery-within 6 or 8 hours after delivery ... If it is after that then we write the reason-there will be other reasons-fever or something else. Those are not maternal deaths. How can those be maternal deaths? [208]
Vibha V., an experienced ANM, explained that they were supposed to record maternal deaths. "It is all in the same register, but it has different parts," she said, directing Human Rights Watch's attention to that portion of her register that is titled "Maternal Deaths." "See this," she said, showing the empty pages of the portion of her register for maternal deaths, "this is where we are supposed to record it." She had not recorded any deaths including one documented by Human Rights Watch in the area where she worked. When asked what it means to have a maternal death, she said, "It could be the death of the mother when the child is still inside her and she has not delivered, or during delivery." When Human Rights Watch prodded further asking whether such deaths could occur after the delivery, she nodded in affirmation and said, "It could be after delivery also-that is during the navjoth period [within 28 days of delivery]. If it is within this period we say it is maternal death."[209]
Such a lack of definitional awareness prevailed even though the Uttar Pradesh government had distributed reporting registers to ANMs and ASHAs with clearly printed columns indicating the different periods in which a pregnant woman or mother could die. The reporting format contains a column labeled, "When did the pregnant woman die," that is further subdivided into "before delivery," "during delivery," and "within 6 weeks of the delivery."[210]
Poor translation of textbook definitions into practice is indicative of several things, including lack of understanding of the importance of such definitions and the importance of using registers to report cases. Insufficiently frequent training and refresher courses, several doctors and government officials felt, influenced how health workers functioned, including their ability to track maternal deaths accurately.[211] Emphasizing the importance of such courses, a senior officer pointed out why health workers are likely to forget the definition of maternal death and its reporting procedures: "In real terms ... maternal death in a village may occur once in one year, or sometimes once in two or three years. By the time the death occurs, she [health worker] will have forgotten everything."[212]
The Uttar Pradesh state government gave training a low priority until 2008. Since then health officials have apparently begun reviving training programs for ANMs.[213] The 2007 government Third Joint Review Mission reported that "after a gap of more than a decade" the Uttar Pradesh government is planning to restart training for ANMs.[214] A former senior health official provided an insight into the challenges he faced reviving ANM training programs:
For most of the past 15 years there has been no recruitment of ANMs. In 2004 a few ANMs were recruited under the reserved category. After that again under NRHM some ANMs have been recruited on contract-basis. Because of this the ANM training centers were lying in complete disuse for more than a decade. Many of them were being used as offices or storage. At least 26 of the 40 ANM centers were restarted recently to conduct training sessions for ANMs. Without regular training there can be no skill building.[215]
ASHAs stated that the state government had organized two training programs since January 2007,[216] but one of them said that the time-lag in distributing training manuals and registers adversely affected her data collection in the field:
We had one training in January 2007 and another in March 2008. They give us the training first and then after many months they give us the books [training manuals and registers]. I got the books in September 2008. The same is the case with the survey [of pregnant women] register. They give us the survey register midway through the year so they will not get a proper survey.[217]
Lack of Continuous Care through the Antenatal and Postnatal Periods
Unless there is sufficient emphasis on continuous care, including care during the antenatal and postnatal period, deaths occurring in these periods cannot be prevented, much less reported. Given that ASHAs and ANMs keep all primary information regarding pregnant women, if they are not in regular contact with pregnant women in their areas, then the chances of their providing assistance or documenting deaths accurately are significantly reduced.[218]
For instance, Human Rights Watch documented two cases where women developed complications during the antenatal period. In both cases health workers were not in regular contact with the families during the antenatal period as required by NRHM norms and the women ultimately died. In one case in October 2008, Meena M.'s daughter-in-law, Aditi A., started bleeding in the third month of her pregnancy and was referred from one private health facility to another before her family finally managed to have her admitted at a private health facility in Lucknow city where she died.[219]
In another case in June 2008, Munira M. from Chitrakoot district started bleeding in the eighth month of pregnancy, got referred from one private facility to another, and finally died in a government hospital in Allahabad district.[220] When asked whether families were aware of any initiative to report or register the death, they stated that no one had come to find out details about the death, suggesting that it went unreported. Relevant district medical officers stated that there had been no maternal deaths in 2008.[221]
Similarly, Human Rights Watch documented four maternal deaths in the postnatal period[222] in which families reported that no one had come to note down the details of the death, suggesting that they went unreported.[223] Human Rights Watch can confirm that at least two of the four deaths went unreported.[224]
Death of Aditi A., Unnao district, October 2008 (Story as narrated by her mother-in-law and neighbor) Aditi A., about age 20, was pregnant for the first time. The ASHA and ANM used to come to her village for "iron golis [IFA tablets] and teekakaran [immunization]." According to Niharika N., Aditi's mother-in-law, the ASHA told Aditi to eat vegetables, avoid spicy food, and take the IFA tablets; no other information was provided to Aditi about antenatal care, birth-preparedness, or her entitlements under the NRHM. During her pregnancy, Aditi went to the primary health center nearby for occasional check-ups but was not provided free antenatal care as specified under government norms. In the ninth month of pregnancy Aditi developed labor pain when she was at home. The ASHA came along with a private doctor and the delivery was conducted at home. The family did not receive the 500 rupees (US$10) for home deliveries as specified under the JSY. On the third day after her delivery Aditi complained of severe abdominal pain and fever. The family was not aware of women's entitlements to postnatal care or the requirement for ASHA visits in the postpartum period. No health worker had come to visit Aditi after her delivery. When the pain did not subside, Aditi's relatives arranged for a Marshall (jeep) to take her to the primary health center nearby. She died en route. Her baby died within a year of her death. No health worker had come to inquire about or record Aditi's death. |
The administrative division of work is such that health workers focus their delivery of services to women who are living in their matrimonial or husband's home. Therefore women who do not stay in their matrimonial or husband's homes often do not receive follow-up pregnancy health care. Women often moved between the matrimonial and maternal homes during pregnancy. Nearly 9 percent of all deliveries are said to occur in the maternal home.[225]
Information about pregnant women who moved between their matrimonial and maternal homes during pregnancy was lost within the system. ASHAs and anganwadi workers told Human Rights Watch that they did not normally attend to pregnant women residing in their mother's or relative's houses unless they stayed there permanently.[226] In at least two instances, health workers expressed their inability to record maternal deaths that had occurred within their coverage area because the women concerned died in their maternal homes.[227]
Explaining the reasons why she did not report a maternal death that occurred in her village, ASHA Pooja P. said that Soumya S., the pregnant woman, had come to her aunt's house. When asked how that affected whether she should report the death, Pooja said, "I do not have to note down her name because I did not attend her case." She elaborated saying "Only bahus [daughters-in-law] of our village get registered. We are told in the training that we have to motivate only the bahus." She explained that the government did not provide money to ASHAs who followed-up on pregnant women for the period they lived in their mother's homes. But as she herself pointed out, "We get money if we motivate them for sterilization-150 rupees [US$3] for every case. It does not matter where the woman is [for sterilization]. I learnt all this from the training."[228]
A health official at the district-level told us that ASHAs do not get money for working with women from other villages. She said,
ASHA does not get money for bringing women from other villages. ASHA should take women for ANC [antenatal care], delivery, and PNC [postnatal care]. So if she cannot follow-up fully, then what is the fun in giving her money [incentive to ASHA]?[229]
Ratna R., an anganwadi worker who claimed that it was also her responsibility to record maternal deaths, stated that she had not recorded a maternal death that occurred in her village. According to her, in June 2008, Rohini R. delivered in the village health-subcenter, had convulsions soon after, and died. Ratna said, "This is Rohini's maikai's [mother's house]village. So her death will not be noted here. We do not register women when they are in their maikai's." When asked whether someone else had registered her death she said, "In this case I do not think the ANM registered her death either. But I cannot be sure. But generally in such cases ANMs do not register the death."[230]
One stated rationale for this administrative policy is reduction of duplication of records and payments under the JSY. However, to make recording of a maternal death dependent on whether the pregnant woman chooses to see through a pregnancy in a matrimonial home, maternal home, or elsewhere is an arbitrary distinction and linking access to maternal care based on whether a woman resides in her matrimonial home is discriminatory, not least on the basis of her marital status.
A Hostile Reporting Environment
Health workers are reluctant to report deaths for fear, justifiably or not, of being singled out by government officials for punitive action.[231] Many activists and government officials feel that one of the key reasons for the non-implementation of the 2004 maternal death audit government order is a misunderstanding of the purpose of such an exercise-the fear that the audit seeks to find fault for maternal deaths rather than investigate systemic causes.[232] One district-level health official explained,
For those deaths reported through word of mouth, someone has to complain [for us to record and investigate it]. ASHAs must complain, but they are afraid it gives them a bad name. If we go to do an investigation, no one will come forward [to give us information].[233]
One district level official explained how overworked ANMs sometimes hide maternal deaths where they are not able to provide care as required of them. He said,
The tracking and monitoring [of maternal deaths] is very poor. How much can you expect one lady [referring to the ANM] to do? .... There is underreporting of [maternal] deaths. My personal experience has been that some ANMs hide deaths. They are busy-out for 10 days doing polio [administering vaccine]-they do not go to all of the villages. If there is a [maternal] casualty in this period, they do not report it.[234]
Referring to the fear of reporting maternal deaths within the public and private health sectors, Dr. Narendra Malhotra, the former president of the Federation of Obstetric and Gynecological Societies of India (FOGSI) said,
There is fear of reporting but we have to reassure them that the primary function of such reporting is to find the causes of death and save many more lives. The idea is to report one death and save other lives. That should be the key message.[235]
At the managerial level, the value of reporting and investigating maternal deaths is overshadowed by its perception as a performance indicator, causing officers to give low priority to improve such reporting systems. Sheela Rani Chunkath, formerly the health secretary of Tamil Nadu state, explained that "the attitude of the government generally is that high deaths means poor performance."[236]
Dr. P. Padmanaban, formerly a senior state health official in Tamil Nadu, and advisor to the Indian government on public health, described having raised maternal death reporting in a meeting organized for state health officials in Ahmedabad. He said, "No one was verykeen because it will expose many gaps in the health system. So no one wants to take it up. Performance linked issues-they feel if they report higher number of deaths, then they will be asked questions."[237]
Even though a 2004 government order instituting the maternal death audit system exists on paper, no government officials were able to give us detailed examples of inquiries and their outcomes.[238] One district medical officer cited an example of a maternal death in a primary healthcare center in September or October 2008. In that case an inquiry was held, resulting in the suspension of the concerned medical officer and nurses, but from the official version of the facts it appeared to be a clear-cut case of negligence. According to the official version, the ANM left the premises of the primary health center without informing the medical officer that a pregnant woman had just delivered a stillborn baby. As a result the mother was left unattended, developed post partum hemorrhage, and died within two hours.[239]
Fear of inquiries, disciplinary action, and attacks by patients' relatives also create an environment that threatens free reporting. One staff nurse who had been suspended without an inquiry said, "I am naturally scared of reporting a death. I am only human. Over here if something goes wrong they will first suspend and only then will they find out if we even did anything wrong."[240]
Uncounted Deaths in Private Facilities
While some private facilities that are part of the Federation of Obstetric and Gynecological Societies of India develop registries that record maternal deaths,[241] district health officials do not collect information regarding maternal deaths from private facilities in Uttar Pradesh. Moreover, health officials from the district and state levels give conflicting reports about whether they have the power to collect such information.
A senior health official from the Directorate of Medical and Health Services told Human Rights Watch that district chief medical officers have the power to collect information on maternal deaths from private facilities. He said,
Power to register private clinics and hospitals is with the CMOs office. These clinics report to the CMO. CMO is the nodal officer and collects monthly information. [There is] also High Court ruling on private hospitals that need registration. So there is legal basis to collect information on maternal deaths.[242]
But district chief medical officers contradicted this, saying that they had no powers to collect such information.[243] When asked what information they had about deaths in private health facilities, one district chief medical officer said, "We do not come to know about private clinic deliveries ... Private hospitals do not have to report deaths to the CMO. What can we do? They just have to issue a death certificate."[244]
Acknowledging that "there is missing information [about] deliveries and deaths in private hospitals," an NRHM district program manager confirmed that they "do not have a system for reporting from [other] private hospitals." However, he clarified that the district health officials received some information from the two JSY-accredited private hospitals in every district. He recalled how this issue had been raised in a meeting with state-level officials at least twice recently. But even though state officials were apprised of the problem, they had not taken measures to improve the situation. Instead, state health officials felt that such decisions should be taken by district health officials. No such action was forthcoming from district health officials.[245]
Human Rights Watch visited four private facilities. Doctors from three of them stated that they were not reporting deaths because the district health officials did not ask them for this information.[246]
Uma U.'s death in a private health facility (Story as narrated to by Vignesh V. and Pratap P., husband and father-in-law of deceased mother) Uma U., about age 20, was pregnant for the first time. In June 2008, in the ninth month of pregnancy, her husband, Vignesh V. took her to a government community health center for delivery. According to Vignesh they kept her there for about six or seven hours and when she did not deliver, the staff at the community health center recommended that she be taken to a private hospital. The staff identified the private hospital to which Uma should be taken and went with Uma's husband. In the private health facility, Uma had a surgery. Both mother and baby survived the surgery. She needed a blood transfusion and they arranged for it. But within five or six hours of the surgery, just as Uma began to receive the second bottle of blood, "her color changed and she started getting something like fits." When doctors were alerted they told Vignesh to take her to Kanpur to a bigger hospital. Alternatively, they asked for 25,000 rupees (US$520) for "ICU" facilities. Vignesh agreed to give them the 25,000 rupees. The doctors wheeled her in to another room and when she was brought out, she had passed away. According to Vignesh, all along the baby was kept in an incubator and the doctors had assured him that the "the baby was fine 95 percent." He claimed that as soon the mother died the doctors told Vignesh that the baby would not survive. Subsequently, the baby also died. Vignesh was told to take both the bodies and leave the hospital. |
Several activists stated that poor monitoring and regulation of private facilities and doctors, especially those conducting unsafe abortions, results in unchecked deaths and complications from unsafe abortions. Further, they stated that unregulated unsafe abortion facilities make tracking abortion-related deaths more difficult; getting accurate information about abortion-related deaths is already difficult because these are often hushed up due to social stigma or misinformation that abortions are illegal even though India has a law allowing medical termination of pregnancies.[247] As a result, they are often misclassified as suicides or murders, especially where the death is due to abortion by an unmarried pregnant woman.[248] Unsafe abortions contribute to roughly 10-12 percent of all maternal deaths in India.[249] Unless access to safe abortions is strengthened and abortion clinics are monitored as required under Indian law, the government cannot avert or track maternal deaths due to unsafe abortions.[250]
Discrimination
Caste-based discrimination not only adversely affects access to and utilization of health care but also affects reporting mechanisms. The effectiveness of the reporting mechanism is dependent on field-based health workers being in regular touch with families. If they are not in contact with families because of caste-based reasons, this not only affects the ability of the families to access health care but also adversely affects reporting.
Several surveys and studies have shown that women and girls from lower castes, especially Dalit communities, experience poor maternal health, underlining that the Indian central and state governments have yet to take adequate measures to provide equal access to health care for these communities.[251]
In most villages visited by Human Rights Watch, women were broadly aware of or had at least heard of the cash incentive for facility-based deliveries under the JSY. Many reported seeing health workers at least during immunization drives. In sharp contrast, women from a predominantly Kol (a group considered "untouchable") village in Chitrakoot district were completely unaware of the government health schemes.[252]Chunni C., one of the pregnant women residing in the village, told Human Rights Watch that she had not received any antenatal care, had not regularly seen an ANM or ASHA in her village, and seemed unaware of the JSY.[253] Laali L., another resident of the village, reported seeing the ANM for the first time 15 days prior to her interview with Human Right Watch, not before or after.[254]
Rathrani, an activist from Vanangana, a nongovernmental organization that has worked extensively in Chitrakoot district against caste-based discrimination, stated that there was one anganwadi worker, two ASHAs, and an ANM-all belonging to upper castes-in the vicinity but none of them visited the village because they considered Kols as "achooth [untouchable]."[255]Human Rights Watch spoke to the ASHA from the Biswakarma community, whose responsibility it was to visit the concerned village. She claimed that she was conducting regular visits.[256]
Rajdayya of the Dalit Mahila Samiti (Dalit Women's Society) explained how entrenched caste-based discrimination is in these areas. She said,
Biswakarma and Kol community follow untouchability. And Kol and Nayi community [follow untouchability] between them ... There are many areas where Biswakarma people will not go to the villages of Kol people.[257]
In their effort to dispel myths about caste hierarchies, the Dalit Mahila Samiti tried organizing a joint meal for women from different castes including Kols, Jamadars, and Biswakarmas. Rajdayya explained that she faced considerable resistance:
Kol community women did not want to come for the joint lunch [saying] that they knew their eyes would burst if they came for such a joint lunch. It was like paap [sin] for them. We had to force them to go to show them that it was not true.[258]
The Indian central government has declared the Kol community as a scheduled caste in Uttar Pradesh, acknowledging that this community is traditionally considered untouchable.[259]
In another village visited by Human Rights Watch, women belonging to the Chamar community described how the ANM from the Mishra community visited their village. Trishna T., a resident of the village belonging to the Chamar community said, "The ASHA and nurse [ANM] come only during polio [immunization] time. They come house-to-house then. Otherwise they do not come here. And they do not tell us anything-no meetings organized-nothing."[260]It was unclear whether the ASHA's or ANM's limited visits to the village were part of a larger systemic problem or motivated by caste-based discrimination. But when the women reported that even during the polio eradication drives, the ASHA or ANM came with someone from the Chamar community, they described what appears to be caste-based discrimination. Trishna said,
Even when they come they bring someone else who is a Chamar. He is the one who gives polio [drops]. The nurse is Mishra so she would not touch our children. They only come in the morning to write numbers on our houses and then will record in their registers whether polio [drops] was given.[261]
As is the case with the Kol community, the Indian central government has declared the Chamar community as a scheduled caste, acknowledging that they are also traditionally considered untouchable.[262]
The Tamil Nadu System of Investigating Maternal Deaths
Tamil Nadu has one of the lowest maternal mortality ratios in the country. Government officials and activists say that a number of socio-economic and political factors influence how health measures are implemented, and this in turn influences the maternal health situation in the state.[263] State health officials also have introduced several measures specifically aimed at reducing maternal mortality-"surveillance and audits of maternal deaths" being one of them.[264] In this section, we describe some of the ways in which the Tamil Nadu approach helps create constructive accountability. It documents some positive features of the Tamil Nadu system that can perhaps help inform similar processes elsewhere in the country. It does not advocate that the Tamil Nadu model is the best.[265]
The Tamil Nadu government has been documenting and analyzing maternal deaths for over a decade.[266] Health officials agree that their system has scope for improvement and is not foolproof.[267] Nevertheless, there are several positive lessons to be learned from Tamil Nadu's experiences in Theni and Dharmapuri districts.
First, all levels of the Tamil Nadu government-from the state to the village-recognize maternal mortality reduction as an important health priority and document and investigate maternal deaths as an intervention towards this end. Sheela Rani Chunkath, the former health secretary who is considered one of the pioneers of the Tamil Nadu initiative, said,
Reducing maternal mortality is like a complicated management problem...you need to know how to manage scarce resources-limited number of anesthetists, surgeons, blood banks. For this you have to identify gaps. I have found that conducting maternal death reviews not only sensitizes health staff but also helps in this management process.[268]
Second, investigations in the Tamil Nadu system have a clear purpose: identifying health system gaps that can be improved upon. Almost all state and district health officials that Human Rights Watch spoke to who had participated and overseen the Tamil Nadu system of investigating deaths stated that the initiative was started with clear objectives-to change the idea that maternal deaths are "normal" or "fate," redirect responsibility to the health system instead of blaming families or health workers for maternal deaths, and develop "actionable points to change the health system."[269]
Third, the maternal death reporting system in Tamil Nadu covers all pregnancy-related deaths irrespective of the medical cause of death and place of occurrence.[270] Since the medical cause of death is difficult to ascertain in some cases, relatives and health workers are encouraged to report any pregnancy-related death. Alphonse Mary, the Maternal and Child Health Officer of Dharmapuri district, who conducts inquiries into maternal deaths said, "I get all kinds of cases. Last month I got a case of a pregnant woman who drank poison and died."[271]
The investigation is undertaken at the district level involving officers who have powers to bring about programmatic changes within the health system. District level officials with judicial powers (district collectors) exercise their powers to ensure that private facilities also participate in district-level maternal mortality review meetings. Alphonse Mary said,
Our collector [district level official with judicial powers] has issued summonses to doctors from a private hospital to attend the maternal mortality review meeting because they were not coming. They [doctors from the private facility] have to come .... They had admitted a woman needing a blood transfusion when they knew they did not have the facility. [They] should come and explain why.[272]
Fourth, the Tamil Nadu government has tackled head-on the problem of gross underreporting of maternal deaths. They struggled with underreporting for several years when the system was initially started in the 1990s but there has been incremental improvement in their reporting system annually.[273] Officials stated that a series of awareness programs and training for health workers coupled with a system of multiple reporting of deaths improved their reporting systems.[274] Dr. Kolanda Swamy, who has overseen reporting of maternal deaths for many years in his capacity as deputy director for health services, said,
Encourage multiple reports [of a maternal death]. Anyone should be allowed to report. Not just health workers. For health workers it is mandatory. Appreciate people who are reporting maternal deaths. Censure those who are not reporting. It is much worse for our health workers to not have reported a death at all than to have reported it and come for a maternal death review meeting.[275]
Dr. Iyyannar, deputy director of health services who oversees health concerns in the Dharmapuri district of Tamil Nadu, emphasized the importance of involving relatives to ascertain the actual cause of death. He said,
Sometimes doctors will give positive findings even within the best system. They will rewrite the case sheets. But relatives will tell you exactly what happened and you can get to the bottom of what happened. Simple things like noting time of entry to the hospital and time of referral [can be rewritten]. But attendants coming with the patient will know. And they will give you the exact story.[276]
When asked whether the Tamil Nadu government initiated punitive action against health workers for maternal deaths, government officials stated that in a majority of cases they found that systemic gaps and faults were responsible for the maternal death. "Before blaming doctors and nurses, we have to ensure that the entire system that supports them is working," said Chunkath. Explaining how there was a fine line between negligence, unethical practice, and systemic failure, Dr. Swamy described how they tried to balance these concerns to determine whether to initiate action against individual officers. "After having all the facilities, training and knowing how to handle the case, if a doctor evades responsibility-for example-by refusing to come on time or purposely referring the case to another hospital, then we can say clearly it is unethical practice," said Dr. Swamy.[277] Similarly, Dr. Iyyanar and Alphonse Mary shared examples of cases where they had initiated action against doctors or nurses who they felt had clearly evaded responsibility.[278]
Positive Changes through Maternal Mortality Review Meetings in Theni District
District-level maternal mortality reviews "create a space for innovative schemes that are then replicated all over the state."[279] The former deputy director of health services in Theni district, Dr. Kolanda Swamy, shared three examples of how maternal mortality review meetings led to programmatic changes within Theni district during his tenure. After a series of maternal mortality review meetings, Theni district health officials realized that there were three crucial systemic shortcomings that needed to be addressed to reduce maternal mortality- lack of timely blood transfusions, communication lapses and poor coordination during emergencies, and problems in referrals.
Addressing blood shortage and a lack of capacity to provide blood transfusions
According to Dr. Swamy, there were two reasons why women were not able to get blood transfusions on time: shortages of blood and lack of capacity to conduct blood transfusions. "Very few staff were trained to match blood [type] and give transfusions," said Dr. Swamy. "We took a decision to train as many health staff as possible on these aspects and it helped," he explained. "We had solved a part of the problem. We still needed blood. Where do you go for blood?" He, along with other district health officials, "took a decision saying that every blood storage facility should have minimum five units of all blood groups available around-the-clock." In order to generate self-sufficiency to the maximum extent possible, Theni district officials started organizing blood donation camps in every primary health center at least twice a month. "Our policy was simple-those who want to donate [blood] are welcome. Those who do not want to donate are also welcome," he said. District health officials instructed health staff at primary health centers not to turn away people who did not want to donate blood. Ensuring that the health workers welcomed even those who were not willing to donate blood helped motivate more people to become donors.[280] Dr. Swamy claimed that this initiative has now been scaled up and replicated in many other districts.[281]
Dealing with poor communication during emergencies
"Communication was a big problem for various things," described Dr. Swamy. He explained how through a series of maternal mortality review meetings they found that they needed better coordination to arrange for emergency transport, anesthetists, surgeons, and blood. There were also cases of health workers who would not admit certain women, with different reasons given for rejecting them. To resolve the problem, "Dr. Nandaswamy and I at that time decided to give our mobile numbers to everyone. Our mobile numbers became public property. Any time of the day or night we could be called for anything," said Dr. Swamy. What started as "a small initiative to see how it will work," was then scaled up by the Tamil Nadu state level health officials, and has now grown into the development of a control room in each district which can be called in for emergencies using a toll free number. According to him, the control room deals with all medical emergencies, though most are pregnancy-related.[282]
Referrals
Theni district health officials learned that poor families often became intimidated when referred to another facility or that medical staff at the recipient hospital did not pay adequate attention to poor families seeking emergency assistance. They replaced the referral system with a system of "accompanied transfer." "Poor women from rural areas are already scared to come to health facilities for a variety of reasons-no familiarity, resigned to their fate because they feel they are uneducated and they made a mistake," said Dr. Swamy. "On top of this, if you tell them that the case is referred because it is serious, it scares them some more. So I banned the use of the word 'referral,' and created a system to accompany the family with a health worker-'accompanied transfer' system." Going with a health worker at the time of referral improved the treatment and assistance given to such patients at the recipient hospital at the time of admission.[283] The "accompanied transfer" system has now been institutionalized across Tamil Nadu in public health facilities.[284]
Changes at the State Level
In addition to replicating or scaling up positive interventions that emerged from a few districts, the Tamil Nadu government also has conducted workshops and discussions for district health officials. Government officials say that in these workshops, district officials reflect upon their experiences to see what improvements can be made. One problem that surfaced through these discussions was health workers' use of different protocols to treat emergencies. "Each one would have managed the same complication differently," said Dr. Swamy. When these variations came to light, the Tamil Nadu government officials invited UNICEF to develop a standard protocol to manage obstetric emergencies and conducted trainings for all health workers. Similarly, they realized that there were problems in supplying drugs and addressed this by improving the supply of medicines in health centers.
Several officials felt that positive reinforcement also has been important in improving information exchange. It is not only important to discuss lacunae but also positive experiences and how medical officers and nurses successfully managed complicated cases. To this end, Tamil Nadu government officials have also recently initiated discussions among nurses and medical officers of near-misses (where the pregnant woman almost died) to share positive experiences of how they were able to avert deaths.[285]
Failure to Use Appropriate Indicators
Institutional Deliveries as an Inadequate Indicator of Progress
It is not enough to design and implement apparently worthwhile activities. We have to make sure they work on the ground. Process and output indicators are especially useful in this regard because they provideinformation not only for the final evaluation, but also for ongoing management and improvement of program components.
- Deborah Maine et al., June 1997.
Constant monitoring of the progress of maternal health interventions based on appropriate indicators is critical to evaluating the effectiveness of programs aimed at reducing maternal mortality. After the introduction of the JSY in 2005, both the Indian central and Uttar Pradesh state governments have used increased institutional deliveries (births in healthcare facilities) as a key measure of progress.[286] The Indian central government states that from mid-2005 to March 2009 nearly 20 million women had benefited under the JSY across India.[287] However, using institutional deliveries as a proxy indicator of progress is problematic for several reasons.
The Uttar Pradesh state government monitors the success of the JSY by setting and achieving "targets" for the number of facility-based deliveries, without monitoring or ensuring that such deliveries are in fact safe and include women who develop pregnancy-related complications.[288] The Uttar Pradesh government fixes annual targets for institutional deliveries both at the state and district levels.[289] Several district chief medical officers confirmed that such targets are set while preparing district NRHM plans for the following financial year, and are based on population and birth rate.[290] "There is a target of about 24,000 institutional deliveries under JSY. We are 10 percent over target," said the Unnao district chief medical officer. The Chitrakoot district additional chief medical officer reported that they had achieved 92 percent of their target by March 2009. Saying that these are increased "exponentially each year," the chief medical officer of Allahabad elaborated that, "Last year it was 13,059. This year it is 35,000. Next year it will be 61,000."[291]
The Uttar Pradesh government monitors achievement of targets not through the actual number of safe deliveries, but through the number of beneficiaries.[292] Whenever a JSY cash incentive is paid to a woman who delivers in a health facility, she is counted as a "beneficiary," and her delivery is counted towards meeting the target.[293]
The accuracy of the reported number of facility-based deliveries in Uttar Pradesh is questionable. The pressure to demonstrate increased institutional deliveries has resulted in spurious payment practices in many cases, skewing the JSY data. Several rural women reported that ASHAs or ANMs had approached them to show their deliveries as facility-based even though they were home-based.[294]
Even assuming that the JSY data on the number of facility-based deliveries is accurate, this data alone does not throw light on the extent of impact of the JSY without information and analysis of adverse outcomes such as maternal deaths and severe morbidities. In what appeared to be an extreme case, in March 2009 health workers had paid out the JSY cash incentive to a the family of R., a 26 year-old woman from Azamgarh district, counting her as a beneficiary under the JSY scheme. R. had developed complications during delivery in a health facility and died.[295] "Even though she died, the fact that she was counted as a beneficiary would be reflected in government's records as a successful institutional delivery," said Jashodhara Dasgupta, an expert on maternal health and women's rights from Uttar Pradesh.[296]
While the government can show that a woman delivered in a health facility, they are not tracking whether every registered pregnant woman actually delivered safely, developed complications, or died during the post-partum period.[297] For example, if there are 50 facility-based deliveries and 10 women eventually died due to post-partum complications, the latter fact may never show up in government records.
Neither of the state agencies responsible for family welfare and health collects data on maternal deaths to analyze JSY's impact. A senior official described the JSY as a strategy for reducing maternal mortality, but in the same breath asserted that there was no connection between its monitoring parameters and maternal deaths. She said,
We [the Directorate of Family Welfare] are not collecting any information on maternal deaths. But we want this information ... it is in the pipeline. JSY and maternal deaths are two separate things. Under JSY we only do monitoring of institutional delivery. 'Maternal deaths' is separate and falls under [the] health directorate – this information comes to the CMO [chief medical officer, district-level official].[298]
Contrary to what the official from the family welfare directorate claimed, officials from the Directorate of Medical Services and Health (health directorate) stated that they were not concerned with maternal health-related data including deaths.[299] One officer said, "Maternal health, maternal deaths, anything connected to the mother-all this comes under the family welfare directorate. It does not come under us."[300]
There is also no clear breakdown of the number of institutional deliveries by type of care-basic care or comprehensive emergency care. When sharing the data collated under the JSY, district medical officers showed figures for facility-based deliveries. In some cases, these were broken down by place of delivery-home or health facility (sub-health center, primary health center, community health center, or district women's hospital).[301] But they had no concrete information about the percentage of such deliveries that successfully addressed pregnancy complications.[302] Many health staff in community health centers reported that they largely conducted "normal deliveries."[303]
Former senior state health officials, doctors, and activists say that it is precisely for this reason that the extent of JSY's impact on maternal mortality is unknown.[304] A former senior health official in Uttar Pradesh was doubtful whether the women who actually needed emergency medical care for pregnancy-related complications were in fact benefiting from the JSY scheme.[305] Government NRHM review reports raise similar concerns that remain unaddressed.[306]
Dr. Chandravati, former professor of gynecology at the medical college hospital in Lucknow and an advisor to the Uttar Pradesh state health department, said that the JSY had not yet resulted in "an identifiable decrease in cases of complications and deaths." She felt that it would possibly take more time to show results, and cautioned that gaps in the scheme would need to be addressed to achieve progress. She expressed concern about the scheme, saying that "lots of gaps are there-the facilities are not upgraded and suddenly the load on these institutions has increased."[307]
The UN Special Rapporteur on health expressed similar concerns after his visit to India in 2007. He noted that the Indian authorities have successfully managed to increase the number of women delivering in health facilities, "[b]ut, in many cases, the range and quality of services offered in those facilities has been seriously neglected. In short, the supply-side has received too little attention."[308] He went further to make the important distinction between provision of facility-based care and access to life-saving treatment:
The focus has been on increasing institutional delivery -but institutional delivery does not always provide access to life-saving care, such as emergency obstetric care, and therefore cannot be regarded as a proxy for access to life saving care."[309]
Activists repeatedly pointed out to Human Rights Watch that the JSY's underlying assumption, that institutional deliveries are safe deliveries, is problematic.[310] Institutional deliveries cannot by default be treated as a measure of deliveries by a skilled birth attendant.[311] The presence of a skilled birth attendant at delivery is associated with better delivery outcomes, including reduction in maternal deaths.[312] But such association is considered plausible only where a trained attendant authorized to perform life-saving functions is supported by a performing health system that can provide life-saving interventions in a timely manner.[313] According to a joint statement issued by the World Health Organization (WHO), the International Confederation of Midwives (ICM), and the International Federation of Gynecology and Obstetrics (FIGO), the definition of skilled care itself requires that an "accredited and competent" healthcare provider has at her disposal the "necessary equipment and the support of a functioning health system, including transport and referral facilities for emergency obstetric care."[314] A skilled birth attendant is a healthcare provider who is "trained to proficiency" not only in the skills needed to manage "uncomplicated" cases, but also to identify, manage, and refer complications.[315]
Concerns about the quality of maternal health care, availability of health workers with midwifery skills, and the level of support afforded to such health workers to perform life-saving interventions indicate that the government's assumption that all institutional deliveries are safe is not well supported.[316] Several government officials and doctors in Uttar Pradesh consistently maintained that they did not have the facilities to meet the "demands" for institutional delivery. One senior health official said, "JSY has opened up the gates for institutional deliveries ... Quality is lacking. Once you create the demand, then your facilities have to be ready."[317]
Poor Monitoring of Emergency Obstetric Care Indicators
Measuring maternal mortality ratios is one way of assessing trends and progress in maternal mortality reduction. However, given that such measurement is contingent upon periodic surveys and a strong vital registration system,[318] experts have developed supplementary approaches for measuring progress. The UN process indicators and guidelines, a set of six indicators, are based on the understanding that certain types of obstetric services must be made available and used to reduce maternal mortality.[319] The six indicators address the minimum required number of basic and comprehensive emergency obstetric care facilities for a given population, their geographical distribution, minimum proportion of births that should occur in basic and comprehensive emergency obstetric facilities, whether women with pregnancy complications were in fact treated in emergency obstetric care facilities, acceptable proportion of births through cesarean sections, and the number of deaths among women with pregnancy complications admitted to facilities equipped with emergency obstetric care.
Even though these indicators are neither binding nor adopted by the UN General Assembly, they were initially developed by UNICEF and have thereafter been used by other UN agencies like the UNFPA and the WHO and are commonly referred to as the UN process indicators. Information based on these indicators reveals whether health facilities for basic and comprehensive emergency obstetric care exist, are distributed in a useful fashion, are used by women, and are used by women who develop obstetric complications. They have been issued with detailed guidelines and minimum norms for each indicator.[320]
The Uttar Pradesh government's routine monitoring of maternal healthcare programs does not take into account the UN process indicators.[321]
Even though periodic surveys like the National Family and Health Survey (NFHS) and District Level Household and Facility Survey (DLHS) provide useful information about the status of maternal health in the country, these do not provide information on key indicators such as whether the need for emergency obstetric care was met in all cases and the proportion of maternal deaths among women with obstetric complications admitted to facilities.[322]
The new NRHM Health Management Information System (HMIS) seeks to fill this gap to some extent by including data on obstetric first aid and access to first referral units or health facilities equipped with emergency obstetric care. But the HMIS still does not include information on all the recommended UN process indicators.[323] Further, government advisors from the National Health Systems Resource Center overseeing implementation of the HMIS in different states say that they have experienced considerable difficulty in rolling out the system in Uttar Pradesh, referring to it as a "problem state."[324]
The Indian central government is also conducting a new Annual Health Survey in several states including Uttar Pradesh, tentatively from 2009.[325] The Registrar General's office-the office coordinating the study- did not provide additional information to Human Rights Watch when asked in May 2009, stating that the survey was yet to be finalized.[326] It remains to be seen whether the survey will generate reliable information on maternal health or be in accordance with recommended UN indicators and guidelines.
Poor Long-term Monitoring
Civil Registration and Maternal Mortality
Civil registration is essential for continuous and long-term monitoring of the progressive realization of women's right to health.[327] A strong civil registration system recording vital events such as births and deaths, including the cause of death, has immense implications for good public health policy and decision-making.[328] Almost all developed countries have a reliable national civil registry recording vital events.[329] Reliable civil registration data is almost never available in low or middle income countries.[330]
In the context of maternal health, the Indian government itself has acknowledged that the "absence of reliable estimates" of maternal mortality makes the process of reducing it "both difficult and complex."[331] More recently, the UN Special Rapporteur on health, after his 2007 visit to India, said, "[t]here is no effective, reliable and comprehensive civil registration system for accurately reporting births and deaths in India. There is evidence that women are silently dying in childbirth and during pregnancy."[332]
The UN Millennium Project Task Force on Child and Maternal Health has called for strengthening civil registration as a "critical investment for reaching the [Millennium Development] Goals." The Task Force stated:
While modeling and population-based surveys can augment our understanding of general levels and trends, they are not a substitute for strong, country-owned vital statistics and civil registration systems ... This task force seconds the call for information, starting with a simple accounting of who is born and who dies, as a critical crosscutting investment necessary for reaching the Goals.[333]
In addition to assisting in the long-term monitoring of maternal mortality, civil registration also helps monitor the progressive realization of many other rights. A robust civil registration system with universal birth registration can help monitor early and enforced marriages. Early marriage and child-bearing have a direct impact on the sexual and reproductive health of girls and women.[334] The median age of marriage in India is 17.2 years, below the legal minimum of age 18.[335] 2007-2008 data from rural Uttar Pradesh shows that early child-bearing continues to remain a problem.[336]
Joint Failure of the Indian Central and Uttar Pradesh Governments
Recording vital events such as births and deaths is mandatory under Indian law under the Registration of Births and Deaths Act, 1969.[337] The duty to implement the law rests both with the Indian central and the concerned state government.[338] The 2000 Indian National Population Policy aims to achieve 100 percent registration of all vital events-births, deaths, and marriages by 2010.[339]
Even though registration of births and deaths is mandatory, civil registration in India is poor. The Central Bureau of Health Intelligence reports that an estimated 26 million births and 9 million deaths occur in India every year, of which only 53 percent of births and 48 percent of deaths are registered. Further, about 10 million births, constituting roughly 25 percent of the world's unregistered births and about 4 million deaths go unregistered annually.[340]
Uttar Pradesh has the worst civil registration record in the country. It is the only state to be repeatedly singled out for poor performance in the annual National Conference of Chief Registrars of Births and Deaths.[341] The latest report of the Indian government on civil registration released in March 2009, covering a backlog of nearly ten years between 1996 and 2005, reveals that the Uttar Pradesh state government has not submitted regular and reliable information on births and deaths to the Indian central government since 1996. Despite the prolonged delay in publishing the report, the central government still has no reliable data on civil registration from Uttar Pradesh.[342]
The reasons for such poor implementation of the civil registration system have been well documented and studied through government reports, notably reports issued pursuant to the Birth and Death Registration Act and the Central Bureau of Health Intelligence 2007 report on mortality statistics in India.[343] The Indian central government has noted that "[registration] functionaries at all levels do the work of registration in addition to their other normal duties in an honorary capacity generally, without any incentive," and has concluded that "[this] is why the work of registration, preparation and submission of statistical returns do not get due attention and priority." Such lack of attention and priority manifests itself in many ways including poor budget allocation, and poor training and supervision of staff involved in registering births and deaths.[344]
Officials at Registrar General's office agree that poor priority for such data is the primary problem and gave some examples of how this is reflected in practice. "A lot of lower level officials [for registration] are not appointed," said one official. As of 2006, a mere 9,000 panchayat (local village council) secretaries were overseeing civil registration in 52,000 panchayats in Uttar Pradesh.[345] Local activists say the vacancies have been slowly filled since 2008.[346] Even where registering authorities have been appointed, however, they often have not been able to carry out their duties because they do not have the required forms and stationery for the registration.[347] Further, coordination meetings between block level officials, district level officials, and the state level inter-departmental coordination committee for civil registration are too seldom conducted. "Even if they meet and take even some small decisions-those decisions are not implemented," said an official from the Registrar General's office.[348]
Despite repeated directives issued to the Uttar Pradesh government at the annual conference, and the host of commitments made by the Uttar Pradesh Chief Registrar to improve the situation, many districts of Uttar Pradesh continue to have "zero" birth and death reporting and registration.[349] One official from the Registrar General's Office stated that the Uttar Pradesh government had almost consistently defaulted on providing timely annual proposals for implementing the civil registration system.[350] Even when the Indian central government has released funds for implementing proposals, "[i]t is a perennial problem with UP that they say they cannot give us a consolidated statement of expenses [showing utilization of funds for civil registration]-and then finance here cannot release funds on time. This has been happening almost consistently since 2001," said the official.[351]
Lamenting how things had not changed, one activist described his experience of working with Uttar Pradesh state government officials. "They [Directorate of Medical and Health Services] had their birth and death registration manuals in a big hall. All of them were piled up instead of being distributed to the Gram Vikas Adhikaris [village development officers]," he said. Seeing that the manuals were not being used, they approached the director general seeking permission to distribute the manuals. But this turned out to be an impossible task. "[T]hey raised [a] hundred objections. 'These are issued by Government of India -this and that-we cannot hand it over to you,' said the government" he explained. Eventually "they just went to waste."[352]
In February-March 2009 Human Rights Watch found that in many cases that registrars, including officials and healthcare workers, who are suppose to notify the authorities about births and deaths knew little about their duties under the law. None of the families, staff nurses, ANMs, or ASHAs were even aware that they were supposed to report maternal deaths to the registrar in their village, let alone use a particular format.[353] Activists and families stated that not all gram sabhas (cluster of villages governed by a village council) had a burial or cremation ground maintained by the village council for different religious communities.[354] Where the cost of transporting the dead body to a burial or cremation ground is high, and the family cannot afford it, they dispose of the body in their fields.[355]
Activists say that those who are listed as registrars on paper often exhibit little or no awareness of their appointment as registrars, much less an understanding of their obligations under the law. ANMs and superintendents of community health centers whom Human Rights Watch interviewed were unaware of their appointment as registrars and did not have the prescribed forms and registers to implement the Registration of Births and Deaths Act.[356]
In practice, panchayat mitras (literally, friends of the village council) assist village development officers in discharging their duties as registrars. One such panchayat mitra said,
The gram vikas adhikari finds out about a death if someone from the family comes and makes an application .... If the family does not come then obviously we cannot know about the death. And most families do not come. Out of 100 deaths, about 20 people will come and make an application – only those with bheema [insurance] or other money or property will come and make an application.[357]
Another panchayat mitra said, "We find out about deaths if the pradhan (village head) goes to the villager's house to offer condolence [after the death]. Then this information goes to the gram vikas adhikari."[358]
None of the families with whom Human Rights Watch spoke who had suffered maternal deaths knew they needed to approach the ANM, the village development officer, or the panchayat mitra to register the deaths.[359]
The Uttar Pradesh government has issued an executive order (government notification) making the Medical Cause of Death Certification scheme applicable in many hospitals.[360] However, the scheme is being implemented poorly. One official from the Registrar General's office stated that the "[s]ituation in UP [Uttar Pradesh] is very grim," pointing out that only 0.7 percent of the total registered deaths were medically certified. Until 2004 the Uttar Pradesh government had submitted data under the MCCD scheme only for four hospitals from the entire state even though their government notification covered more hospitals. "From 2005 there is no data at all," he concluded.[361]
As mentioned before, civil registration is the shared responsibility of both the Indian central and the Uttar Pradesh state government under the Indian Constitution.[362]Despite this shared responsibility, national authorities are doing very little to intervene and set right the problem.
V. Improving Accountability: Reforming Grievance and Redress Mechanisms and Creating Emergency Response Systems
Establishing an Emergency Helpline
To protect the health of pregnant women and prevent maternal deaths and injury, it is important that authorities take steps to avert possible maternal deaths once they are alerted that such risks are present.
One such step is establishing an emergency response system which can make prompt interventions when authorities learn that a pregnant woman is facing barriers to care. Where delays in care are due to lack of communication or coordination between health facilities or due to demands for informal monetary payments, discriminatory treatment, or similar factors, the authorities should be notified and be in a position to intervene and take corrective measures.
Newspaper reports from Uttar Pradesh suggest that in the few cases where activists or journalists were able to bring to the attention of district medical authorities cases of denial of health care to pregnant women, authorities intervened to ensure that the women were provided immediate medical attention. The authorities should ensure that this intervention capacity is replicated on a permanent stand-by basis. One format that this could take is the creation of an emergency helpline under the control of district-level authorities who have the power to intervene and make decisions. As a prominent human rights lawyer from Allahabad, K. K. Roy, pointed out, while remedies such as public interest litigation and complaints to state human rights commissions are important, "they are like a fire brigade-they fix the problem after the fire breaks out." Continuing this analogy, he said, "the fire should be prevented."[363]
Role for an Ombudsman's Office
An emergency response system should be supplemented by a facility-level or regional investigative authority such as an ombudsman. The ombudsman would inquire into complaints about the women's treatment or denial of care in health facilities irrespective of whether it results in a death or disability. The reasons may include corruption, discriminatory or abusive treatment, lack of facilities, and so on. For example, a pregnant woman may have complaints about abusive treatment at the time of delivery-beating, pinching, name-calling-even though she delivered safely. Following such a complaint, the ombudsman should look into the facts, and recommend remedies for the patient concerned, including compensation where appropriate, as well as other recommendations to improve delivery of health services.
Absence of accessible, independent, and transparent redress mechanisms contributes to patient frustrations, which at times boil over. One health worker said,
Why do people gherao [surround] the hospital? They have no one who listens to them. If they had someone who could make arrangements for them and understand their problems, then maybe they would not have to come to the streets.[364]
Doctors, staff nurses, and health workers consistently reported to Human Rights Watch that even in cases where they were not able to provide appropriate assistance because of non-availability of drugs, the required expertise, or facilities, "patients did not understand," leading to confrontations between health staff and relatives, or gheraos [protests in which angry family members and others surround the hospital]. This has further exacerbated the problem of access to timely and appropriate care for pregnant women because doctors and nurses have become increasingly reluctant to admit patients presenting what they perceive as "risky cases."[365]
Ruth Daniel, president of the Uttar Pradesh Nurses Association, explained how the lack of a complaints procedure coupled with a poor ratio of staff nurses to patients caused a lot of patient-nurse conflict. She said, "There are a number of cases where our nurses get suspended, dismissed, [have] gone to jail .... I have nurses who are beaten and are scared to work."[366]
Problems with Existing Complaints Mechanisms
Women's Poor Awareness of Entitlements
Poor awareness of services offered under government schemes is the first barrier to making a complaint.[367] On paper, the NRHM provides a host of service guarantees, but these are seldom effectively communicated to pregnant women in rural areas. For example, even though community health centers visited by Human Rights Watch had big painted walls providing some information about the JSY and the duties of the ASHAs in Hindi, most families, especially pregnant women, were unaware of their entitlements under the JSY or the NRHM service guarantees. They only seemed aware of the 1400 rupees (US$28) cash incentive that would be given to them for a facility-based delivery. Almost all poor women reported paying money in government facilities despite being entitled to free antenatal, intra-natal, and postnatal care under the NRHM.[368] Several women including ASHAs reported that staff nurses in government hospitals had demanded money for the delivery, refusing to hand over the delivered baby unless money was paid to them.[369]
The government should consider disseminating information about NRHM entitlements in a manner that can be understood and utilized by women from vulnerable communities with little or no formal education.
Poor Access to Grievance Redressal Procedures
Even women who are aware of their entitlements and feel aggrieved by the treatment meted out to them in health facilities can find they have no way of registering and processing complaints. Government officials gave Human Rights Watch conflicting accounts of procedures for grievance redressal. Some stated that women could make complaints to superintendents or medical officers in charge of hospitals, while others stated that district chief medical officers could receive complaints.[370] One gynecologist in a district hospital claimed that there was a complaints box where women could drop their complaints. But when Human Rights Watch asked her for more details about the types of complaints, processes to deal with them, and their outcomes, she conceded that no one had actually used the complaints box.[371]
A senior official stated that the government had also formed a grievance redressal cell which had received many complaints forwarded by the districts, but was unable to give further details about protocols to deal with such grievances in a timely manner, or the outcomes of grievances filed with the cell. [372]
Under the NRHM, Patient Welfare Committees (Rogi Kalyan Samitis or RKS) at government health facilities are primarily seen as "management" committees that are supposed to function as a "nongovernmental organization."[373] They have been assigned the task of "ensuring accountability of the public health providers," and establishing a system of public grievance redressal at facility level.[374] Medical officers heading the executive bodies of RKS with whom Human Rights Watch spoke were not aware of any of these powers. Women and health workers, including staff nurses and doctors in hospitals, did not know about any grievance redressal powers of the RKS.[375] For instance, one woman in a group said,
We don't know where to go and complain about anything ...We have no information about it [Rogi Kalyan Samiti]. And we will go there and make complaints only if someone goes along with us. How can we go alone and complain there?[376]
Other existing mechanisms such as filing complaints before chief medical officers, state or national human rights commissions, the national Women's Rights Commission, and filing petitions before the High Court or consumer courts are important avenues. But they are not easily accessible to rural women and do not provide timely remedies.Similarly, public interest petitions filed in the Uttar Pradesh High Court in 2006 and early 2009 about maternal health in Uttar Pradesh are still pending. According to K. K. Roy, the lawyer representing the petitioners in the four cases, no substantive orders had been passed providing any relief to the petitioners at this writing.
Many rural women report that they are too scared to complain against doctors or nurses even when they feel that they had experienced some injustice. They fear reprisals by medical officers and health workers. In the few instances that Human Rights Watch was able to document complaints filed by women before the High Court or the State Commission for Scheduled Castes and Scheduled Tribes, activists helping with the complaints said that the doctors or health workers concerned had pressured the women or their families to withdraw the complaint.[377]
Salenta's case is illustrative of the difficulties faced by women from vulnerable communities in pursuing complaints. Salenta, a Dalit woman, delivered in a primary health facility without adequate attention of the health staff in February 2007 and was discharged. After returning home, she complained of severe pain and urinary incontinence. She got no follow-up free postnatal care as guaranteed under the NRHM. Instead, with the help of local activists, she went to different public and private health facilities for treatment and was finally admitted for surgery for obstetric fistula in February 2008. She incurred about 50,000 rupees (US$1000) in medical expenses. During this period, Salenta approached several district, state, and national authorities for redress. Not only did her complaints go unheard but they were also met with threats from at least one district health official. According to SAHAYOG, a prominent Lucknow-based nongovernmental organization that provided her with support to seek redress, a district health official "abused them [Salenta and her family] and accused them of daring to complain to higher authorities. He demanded that they state in writing that they had not gone for an institutional delivery."[378] Salenta's case is now pending before the High Court in Allahabad.[379]
Most women we spoke with, many of whom are illiterate, say that they cannot exercise existing grievance options without support to file and process their complaints.[380] Filing complaints before courts and human rights commissions requires multiple visits by family members to testify before such bodies. Activists from SAHAYOG, who have assisted many pregnant women in seeking justice when they are denied health care, felt that a lack of adequate resources to follow-up complaints is a significant obstacle.[381] "Most of these women come from really poor families living on daily wages," said Shakuntala Joshi of SAHAYOG. "So how do you expect that these people can keep coming before these bodies to tell their story?"
The Need to Follow-Through in Response to Grievances
Even when women successfully lodge their complaints, there is evidence to suggest that no official inquiry or follow-up action ensues or that such steps are significantly delayed. In addition to Salenta's case described above, Human Rights Watch traced a woman who had made a written complaint before the chief medical officer of Chitrakoot district. Saroj, belonging to a Dalit community, filed a complaint in 2008 regarding a failed sterilization surgery. When interviewed by Human Rights Watch in March 2009, she had still not obtained any form of remedy.[382]
Another district official said that about five or six women had made written complaints earlier this year around April to the office of the Unnao district chief medical officer. They claimed that health facility staff had demanded money at the time of delivery or had taken money from their JSY payments. But no inquiry or further action was initiated by the Unnao chief medical officer. One district official who spoke with Human Rights Watch believed that because the complaints lodged were against doctors and would be considered by the Chief Medical Officer, also a medical doctor, the complaints would effectively be ignored. He proposed that a better structure would be to submit complaints to a committee under the district magistrate.[383]
In the relatively few instances in which the Uttar Pradesh health officials initiated action against medical staff, there is evidence to suggest that they did very little beyond suspending or transferring frontline medical staff, primarily auxiliary nurse-midwives, staff nurses, and doctors.[384]
Human Rights Watch requested a senior Uttar Pradesh health official to provide a list of staff nurses who were suspended in order to interview them, but the Uttar Pradesh government would not provide such a list, despite our assurances to respect the confidentiality and privacy of the nurses and patients involved.[385] Human Rights Watch also filed applications under the Right to Information Act, 2005, seeking information about such complaints, their investigation, and outcomes. At the writing of this report the applications are still pending.[386]
In one case in 2008 where a pregnant woman was referred out of a community health center and delivered on the road, a staff nurse at the health facility was suspended. Human Rights Watch was able to trace the nurse. "I was not even on duty when it all happened," she claimed. "In fact I was the one who took her [the mother] back inside after she had delivered on the road, helped her when she was delivering the placenta, and cleaned her," she said.[387]
Reflecting on her experiences after working at the community health center for two years, the staff nurse said that in her community health center, there had been at least two controversial cases where women were referred to a Lucknow hospital in 2009. In one case the pregnant woman delivered on the road. In another, she died. In both cases the media played a critical role in highlighting the problems, forcing the state to respond. According to the staff nurse, the problem was primarily one of referral transport to take women to the Lucknow hospital. The government had conducted inquiries, suspending individual staff nurses, but had not come to any definite conclusions. Expressing her frustration that the problem remained unresolved, she said, "If something goes wrong nurses get into trouble ... Suspending me or another nurse will not solve the transport problem here."[388]
A senior state health official claimed that inquiries were also conducted in five or six cases where staff nurses had sought money from patients in government health facilities and some had been suspended.[389] These inquiries were conducted "mostly to save ourselves [government officials]," she said.
State responsibility for maternal deaths and complaints regarding denial of appropriate health care for reasons such as corruption, non-supply of essential drugs, and discriminatory or abusive treatment, rests primarily with the district health authorities and health facility superintendents who are in charge of planning, oversight, and implementation of maternal healthcare programs. Hence, any inquiry into a complaint should also examine possible failures in planning and oversight at the district and sub-district levels. For instance, where a doctor reports for duty at a primary health center for less than the stipulated duty hours for more than six months, and this comes to light in the context of a maternal death, the serious lapse in regular oversight by district health authorities should also be taken into consideration while apportioning individual responsibility.[390]
VI. International Human Rights and the Indian Legal Framework
International Human Rights Law
International Commitments to Reduce Maternal Mortality
India has participated in several international conferences and United Nations (UN) General Assembly sessions, adopting resolutions that specifically address women's right to sexual and reproductive health, including maternal health. Maternal mortality reduction is an important goal towards achieving this right. Hence along with the international community, India has made some crucial commitments regarding maternal mortality reduction. Key among these are the 1994 International Convention on Population and Development (ICPD), the 1995 Beijing Fourth World Conference of Women, the 1999 UN General Assembly special session reviewing the ICPD resolutions, and the 2000 UN General Assembly session adopting the Millennium Declaration, and the 2008 UN high-level event on the Millennium Development Goals.
Maternal mortality reduction itself should be monitored using two targets-ensuring a 75 percent reduction in MMR levels by 2015 compared with 1990 levels and providing universal access to sexual and reproductive healthcare services to all women.
In-country Obligations of States
India is a party to several international human rights treaties that create binding obligations on the Indian central and state governments. Those with particular relevance to maternal health are the International Covenant on Economic, Social and Cultural Rights (ICESCR),[391] the International Covenant on Civil and Political Rights (ICCPR),[392] the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW),[393] and the Convention on the Rights of the Child (CRC).[394] The obligations on states set out in these treaties to implement human rights guarantees can be divided into obligations to respect, protect, and fulfill the right.[395]
The Indian Supreme Court has held that the implementation of the obligations in these treaties is not conditional upon being incorporated in domestic legislation. Hence district level and state level authorities have the freedom to take measures to directly comply with India's international obligations. Likewise, Indian courts also have the freedom to direct governments to take measures to implement these binding international obligations.[396]
The right to life
Article 6 of the ICCPR sets out that everyone "has the inherent right to life," which shall be protected by law. It guarantees that no one shall be arbitrarily deprived of life. The UN Human Rights Committee which oversees the implementation of the ICCPR has advised states that the right to life should not be considered in a restrictive manner but requires states to adopt a range of positive measures to protect deprivation of life.[397] For example, in its General Comment No. 6 on the right to life, the Human Rights Committee noted that that it would be desirable for states to take positive measures to reduce infant mortality and to increase life expectancy.[398]In light of the states obligation to ensure equality between men and women, governments must take at least equivalent steps to prevent maternal death as to prevent death from disease. The Human Rights Committee has specifically said that when reporting on the right to life protected by article 6, states "ought provide data on birth rates and on pregnancy- and childbirth-related deaths of women... States parties should give information on any measures taken by the State to help women prevent unwanted pregnancies, and to ensure that they do not have to undergo life-threatening clandestine abortions."[399]
In examining states' obligations on the right to life, the Human Rights Committee has often commented on health-related risks to the right to life. It specifically noted that where life expectancy of women is shorter than that of men that this should be addressed;[400] and has on many occasions expressed its concern about the existence of very high levels of maternal mortality which it has identified as often arising as a result of clandestine abortions, early marriage, or practices such as female genital mutilation.[401]The Human Rights Committee has specifically noted that abortions in unsafe conditions, imperil "the life and health of the women concerned, in violation of Articles 6 [right to life] and 7 [freedom from torture and inhuman treatment] of the Covenant."[402] Likewise the Committee has said that where there is a high maternal mortality, that in order to protect the right to life, the state should "[ensure] the accessibility of health services...ensure that its health workers receive adequate training...[and] help women avoid unwanted pregnancies...by strengthening its family planning and sex education programmes."[403]
Another positive obligation is to investigate potential violations of the right to life promptly, thoroughly, and effectively through independent and impartial bodies. As the Human Rights Committee has noted, in certain circumstances the failure to take appropriate measures and exercise due diligence to prevent, investigate, or redress harm caused by acts of private persons or entities, may give rise to a violation of the right to life.[404]
The right to sexual and reproductive health, including maternal health
Article 12 of the ICESCR guarantees the right to the highest attainable standard of health. The UN Committee on Economic, Social and Cultural Rights (CESCR), which oversees implementation of the ICESCR, has affirmed that states are required to take measures to improve child and maternal health, sexual and reproductive health services, including access to family planning, pre- and post-natal care, emergency obstetric services and access to information, as well as to resources necessary to act on that information.[405] It recommends that states remove all barriers to women's access to reproductive health services.[406] Importantly, the committee has said that the obligation to ensure reproductive, maternal, and child health care is of "comparable priority" to the non-derogable core obligations under the Covenant.[407] The UN Special Rapporteur on the right to health has also consistently stated that the right to health includes the right to sexual and reproductive health, including maternal health.[408]
The right to health includes the right to health care and the right to the underlying determinants of health.[409]Underlying determinants of health include food and nutrition, access to safe and potable water, adequate sanitation, sufficient quantity of hospitals, clinics and other health-relatedbuildings, trained medical and professional personnel receiving domestically competitive salaries,and essential drugs.[410]
Under article 12 of the CEDAW, states should take "all appropriate measures" to eliminate discrimination against women in the field of health and ensure equal access to healthcare services. In particular, states should ensure "appropriate services" in connection with "pregnancy, confinement and postnatal period, granting free services where necessary, as well as adequate nutrition during pregnancy and lactation." The CEDAW Committee has called on states parties to take steps under the right to health in particular to "prioritize the prevention of unwanted pregnancy through family planning and sex education and reduce maternal mortality rates through safe motherhood services and prenatal assistance."[411]
According to its obligations under article 24 of the CRC, states have to ensure "appropriate pre-natal and post-natal health care for mothers."
Content of the Obligations
Generally, by undertaking to respect women's right to sexual and reproductive health, including maternal health, states have an obligation not to interfere, either directly or indirectly, with the enjoyment of the right to health.[412] In particular this means that states should abstain from "imposing discriminatory practices relating to women's health status and needs."[413] States should refrain from limiting access to the "means of maintaining sexual and reproductive health,"[414] and "withholding or intentionally misrepresenting health-related information."[415] A state is said to have violated its obligation to respect the said rights when its laws, policies, or actions run contrary to article 12 of the ICESCR, resulting in "bodily harm, unnecessary morbidity, and preventable mortality." Such violations include de jure or de facto discrimination, deliberate withholding of or misrepresentation of information vital to health protection or treatment, failure to take into account its legal obligations while entering into bilateral or multilateral agreements with other states and international organizations.[416]
Protecting the right to sexual and reproductive health obliges states to take measures preventing third parties from interfering with the enjoyment of the right.[417] To this end, states should take measures to ensure that privatization of the health sector does not constitute a threat to the availability, accessibility, acceptability, and qualify of health facilities, goods, and services.[418] This also means that states should take measures to ensure that medical practitioners and other health related professionals meet appropriate standards of education, skill, and ethical codes of conduct.[419] Failure to regulate the private sector, for instance, amounts to a violation of state's obligation to protect the right to health.[420]
The obligation to fulfill, which once again can be broken down as obligations to facilitate, provide, and promote the right to health, requires states to adopt "appropriate" legislative, administrative, budgetary, judicial, promotional, or "other" measures "towards the full realization" of the right to health.[421] The obligation to fulfill gives rise to a bundle of obligations including the sufficient recognition of the right to health in national political and legal systems, provision of health care, equal access to the underlying determinants of health, appropriate training for doctors and medical personnel, sufficient number of hospitals, clinics, and other health-related facilities with regard to equitable distribution within the country.[422] This includes the obligation to provide for sexual and reproductive health services, including safe motherhood, particularly in rural areas.[423]
The CEDAW Committee has advised states that the duty to fulfill rights places an obligation on them to take appropriate legislative, judicial, administrative, budgetary, economic and other measures to the maximum extent of their available resources to ensure that women realize their rights to health care. It notes that high maternal mortality and morbidity "provide an important indication for States parties of possible breaches of their duties to ensure women's access to health care."[424]States party to CEDAW are required to furnish information to the CEDAW Committee on the how measures they have taken "have reduced maternal mortality and morbidity in their countries, in general, and in vulnerable groups, regions and communities, in particular."[425]States party should also include in their reports how they supply free services where necessary to ensure safe pregnancies, childbirth, and post-partum periods for women. The Committee explicitly noted "that it is the duty of States parties to ensure women's right to safe motherhood and emergency obstetric services and they should allocate to these services the maximum extent of available resources."[426]
The obligation to fulfill also requires the state to play the role of a facilitator, whereby it assists individuals and communities to enjoy the rights guaranteed to them.[427] It should perform the function of a "provider" in cases where individuals or a group are "unable, for reasons beyond their control, to realize that right themselves by the means at their disposal." Finally, the state must function as a "promoter" undertaking actions that "create, maintain, and restore" the health of the population-for example-through research and provision of information, ensuring that health staff are trained and respond to the specific needs of vulnerable or marginalized groups, and supporting people in making informed choices about their health.[428] The obligation to "fulfill" the right to health is violated when states fail to monitor the realization of the right to heath at the national level.[429] Further, "failure to reduce ... maternal mortality rates" is a violation of the obligation to fulfill the right to health.[430]
The obligation to fulfill the right to health requires states to undertake actions that create, maintain, and restore the health of the population. Such obligations include fostering recognition of factors favoring positive health results, ensuring that health services are culturally appropriate, and that healthcare staff are trained to recognize and respond to the specific needs of vulnerable or marginalized groups.[431]Adolescent girls who become pregnant should have access to health services that are sensitive to their rights and particular needs.[432]Analyzing pregnancy outcomes through investigations of maternal deaths not only allows the state to recognize factors favoring positive health results, but also allows health workers to respond to the specific needs of vulnerable and marginalized groups.
Accountability as a human rights principle
Accountability is central to a human rights approach to health and helps communities and rights-bearers assess how those with responsibilities are discharging their duties.[433] The UN Special Rapporteur on right to health has stated that "without accountability, human rights can become no more than window-dressing."[434]
Accountability has two components-states should develop redressal mechanisms for mistakes or grievances, and correct systemic failures and replicate programs that work.[435] The latter-constructive accountability-is particularly important in the area of health. It helps governments "identify what works, so that it can be repeated, and what does not, so that it can be revised."[436]
Any system of accountability should be "accessible, transparent, and effective," and cover both public and private health sectors.[437]
Accountability: The obligation to monitor "progressive realization"
Accountability is concerned with "ensuring that health systems are improving, and the right to the highest attainable standard of health is being progressively realized, for all, including disadvantaged individuals, communities, and population."[438] Under the ICESCR, states' obligation to fully realize the right to health is subject to progressive realization.[439]
Progressive realization of the right to health generally and maternal health specifically means that states have a specific and continuing obligation to move as expeditiously and effectively as possible towards the "full realization" of these rights.[440]To this end, states have an obligation "to take steps," individually and through international assistance and co-operation, especially economic and technical, to the maximum of its available resources, through positive measures.[441]
Full realization of the right to health, including maternal health, means progressive realization of both aspects of the right to health, that is, the rights to health care and underlying determinants of health. Investigations of maternal deaths at the district level reveal important information about not only the healthcare system but also socio-economic and cultural factors that contribute to the deaths, including some or all underlying determinants of health. This allows the state to take a host of appropriate public health measures to ensure the progressive realization of the right.
"Appropriateness" of the interventions is a critical element of progressive realization. Almost all international guarantees of health, including pregnancy-related health care, make references to "appropriate" means. The obligation to progressively realize the right to maternal health does not mean that the state can take some measures broadly in the right direction. On the contrary, it is a much more onerous and specific obligation to take the "most appropriate" measure that will progressively realize the right to health. Under article 2 of the ICESCR, states have undertaken to progressively realize the right to health "by all appropriate means."[442]
These repeated calls for "appropriate" means and services should be interpreted in light of the authoritative interpretations issued by the Committee on Economic, Social and Cultural Rights and statements of the UN Special Rapporteur on the right to health. The committee has stated that states should demonstrate in their reports to the committee "not only the measures that have been taken but also the basis on which they are considered to be the most 'appropriate.'"[443] Steps taken by states "must be deliberate, concrete and targeted towards the full realization of the right to health".[444] The UN Special Rapporteur on the right to health has clarified that "progressive realization...does not mean that a State is free to choose whatever measures it wishes to take so long as they reflect some degree of progress. A State has a duty to adopt those measures that are most effective, while taking into account resource availability and other human rights considerations."[445]
In keeping with its international obligations to take the most appropriate measures to progressively realize the right to sexual and reproductive health, including maternal health, the Indian central and Uttar Pradesh state governments should immediately undertake a review of all its policies and programs to determine the appropriateness and effectiveness of its interventions, and revise them to maximize impact.
Another feature of progressive realization is the obligation to maintain the present level of enjoyment of the right to health, that is, the state should not take measures that are retrogressive. Any deliberately retrogressive measure "would require the most careful consideration and would need to be fully justified by reference to the totality of the rights provided...and in the context of the full use of the maximum available resources."[446] In the Indian context, the government's modification of the National Maternity Benefit Scheme, to introduce eligibility criteria in some states for JSY, resulting in the exclusion of many women who were formerly entitled to benefits and not providing them with a reasonable alternative could constitute a retrogressive measure. In some states, the JSY benefits are available to only those women who are above age 18 and up to two live children.[447]
As mentioned before tracking progressive realization through constant monitoring is a key feature of accountability. It involves "monitoring of conduct, performance, and outcomes."[448] In a right-to-health approach to reducing maternal mortality, states should develop "appropriate indicators to monitor progress made, and to highlight where policy adjustments may be needed."[449] The periodic reporting system under the ICESCR aims to ensure that the "state party monitors the actual situation with respect to each of the rights on a regular basis and is thus aware of the extent to which the various rights are, or are not, being enjoyed by all individuals within its territory or under its jurisdiction."[450] Monitoring cannot be achieved merely by gathering aggregate national statistics or estimates, "but also requires that special attention be given to any worse-off regions or areas and to any specific groups or subgroups which appear to be particularly vulnerable or disadvantaged."[451] Such monitoring forms the basis for evaluating the extent to which rights are being progressively realized.[452]
Monitoring should also be based on "appropriate indicators." States have an obligation to adopt and implement a national public health strategy and plan of action, on the basis of "epidemiological evidence."[453] Such a strategy and plan of action should include methods such as right to health indicators and benchmarks, by which progress can be closely monitored.[454] Without such "appropriate indicators and benchmarks...there is no way of knowing whether or not the State is improving its health system and progressively realizing the right to the highest attainable standard of health."[455] Data based on these "appropriate indicators" should be disaggregated on the basis of the prohibited grounds of discrimination to monitor the elimination of discrimination as well as ensure that vulnerable communities are actually benefiting from healthcare schemes.[456]
While monitoring progressive realization, states should identify the factors and difficulties affecting implementation of their obligations.[457]The realization of women's right to health requires the removal of all barriers interfering with access to health services, education and information, including in the area of sexual and reproductive health.[458]Monitoring will help state parties develop a better understanding of the "problems and shortcomings encountered" in realizing rights, providing them with the "framework within which more appropriate policies can be devised."[459]
Finally, monitoring is merely the means to an end-the full realization of the right to health. States should constantly revise and review their laws, policies, programs, and practice based on the information gathered through such monitoring.
The Indian government has a maternal mortality benchmark (MMR should be below 100 by 2010) but does constantly monitor progress based on appropriate indicators, including the recommended UN indicators for monitoring availability and utilization of obstetric services.[460] Merely identifying a time-specific benchmark without gathering information that helps monitor the timely achievement of the goal defeats the very purpose of the benchmark. The Indian central government has an obligation to collect data on processes and outcomes that will enable it to measure progress and revise programs. Further, investigating maternal deaths at the district level will help states to identify socio-economic and cultural causes, and problems that hamper women's access to healthcare services.
"Core obligations" subject to immediate implementation
In order to fully realize the different aspects of the rights to health, states are allowed some leeway by way of time- "full realization...cannot be achieved in a short period of time."[461] However, the obligation to progressively realize is itself an immediate obligation that cannot be postponed. States are under an obligation "to take steps" towards such full realization.[462] States have an obligation to move "as expeditiously and effectively as possible" towards the "full realization" of article 12 of ICESCR.[463]
Moreover, certain "core obligations" are not subject to availability of resources-they should be immediately realized. Non-discrimination, for example, is one such obligation that is not subject to availability of resources.[464] Monitoring progressive realization is another such obligation. The CESCR has emphasized that "the obligation to monitor the extent of realization, or more especially of the non-realization of economic, social and cultural rights, and to devise strategies and programmes for their promotion, are not in any way eliminated as a result of resource constraints."[465] Establishing an accessible, transparent, and effective accountability mechanism, including monitoring, is a core obligation.[466]
The UN Special Rapporteur on the right to health has further observed that states also have a "core obligation" to ensure a "minimum basket of health-related services and facilities," including "sexual and reproductive health services including information, family planning, prenatal and postnatal services, and emergency obstetric care."[467]
Since monitoring progress and creating benchmarks to measure progress are a core obligation, collection of the data necessary to measure such progress should also be treated as such.
Equality and Non-discrimination as a "Core Obligation"
International law obligates governments to ensure basic human rights without discrimination. This obligation is set out in Article 2 of both the ICCPR and the ICESCR.[468] The Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW) explicitly prohibits discrimination against women in all fields including the right to life and health care.
The principle of non-discrimination and equality requires states to develop programs that "promote equitable distribution of health care, including provision in rural or poor areas, or areas with high indigenous or minority populations."[469] The obligation of non-discrimination and equality is an immediate obligation, not subject to availability of resources.[470]
Discrimination in access to health care and underlying determinants of health is prohibited. In addition to those explicitly provided for in the text of the ICESCR, the CESCR has identified other grounds on which discrimination is prohibited. [471] In 2009, the committee adopted a General Comment on the obligation of non-discrimination in which it sets out its understanding of the phrase "other status," enumerating more prohibited grounds of discrimination. This list, though not exhaustive, includes, age, marital and family status including number of children, place of residence, and economic and social situation.[472]
Differential treatment based on prohibited grounds will be viewed as discriminatory unless such treatment can be justified as reasonable and objective.[473] This will include an assessment of the whether the aim and effects of the measures or omissions are legitimate, compatible with the rights enshrined in the ICESCR, and are undertaken solely for the purpose of promoting the general welfare in a democratic society. There should also be a reasonable relationship of proportionality between the aim sought, the measures or omissions, and the effects.
The law, policy, program, or practice of the state does not have to be intentionally discriminatory. Even where it in effect nullifies or impairs the equal enjoyment or exercise of the right to health, it amounts to discrimination.[474]
In some states, the Indian government has limited the JSY scheme only to women above age 18 and for up to two live children. This policy is discriminatory and does not fall within the category of differential treatment. Many activists and public health experts in India state that even though this measure has ostensibly been taken to discourage early marriage and child-bearing, the harm done by excluding young mothers from the JSY scheme is far greater since young mothers are at higher risk of complications due to pregnancy and are in increased need of medical attention at the time of delivery.[475] Likewise, the exclusion of women with more than two live children from JSY benefits is also discriminatory. Activists and experts consistently maintain that women with more than two children are more vulnerable and need better attention.[476] Instead of empowering such women and improving their access to and utilization of contraceptives of their choice, excluding them from the JSY scheme only puts them in harm's way.[477]
The jurisdictional division of health workers in Uttar Pradesh in effect leads to a discriminatory practice-pregnant women living in their mother's homes do not have equal access to sexual and reproductive healthcare services compared with those who live in their husband's homes.[478]
Redress
It is a general principle of human rights law that victims of violations have a right to a remedy. Specifically article 2(3) of the ICCPR requires that individuals have accessible and effective remedies to vindicate their rights. The Human Rights Committee has made explicit that states should also "make reparation to individuals whose rights have been violated. Without reparation ... the obligation to provide an effective remedy, ... is not discharged."[479] Likewise the Committee on economic, social and cultural rights has said that where any person or group is a victim of a violation of the right to health they should have access to effective remedies and should be entitled to adequate reparation. Both committees have emphasized that victims should expect satisfaction and guarantees of non-repetition.[480] The Human Rights Committee has observed that states have an obligation to make changes in relevant laws and practices as necessary and, when there are serious violations, to hold accountable those responsible for human rights violations.[481]
To establish meaningful accountability, an investigation needs to independently identify the extent of the state's liability for maternal deaths or severe morbidities that result from failings in healthcare provision. Therefore effective remedial mechanisms should be designed not only to examine where individual fault or responsibility may lie in a particular case, but need to include an examination of responsibility for planning and oversight at the level of district and sub-health officials. They should examine whether health authorities have taken appropriate systemic measures to minimize, to the greatest extent possible, the risk to life and assess whether the authorities were negligent in failing to take such measures.[482]
Further, the right to health is closely related to and dependent upon the realization of other human rights, such as access to information.[483]Information, particularly information related to sexual and reproductive health is one of the underlying determinants of health.[484]Especially in the context of maternal health, the state is obligated to ensure access to information about sexual and reproductive health services, as well as resources necessary to act on such information.[485] States should also ensure that third parties do not limit people's access to health-related information.[486]As part of its obligation to fulfill the right to health, the state has an obligation to promote information campaigns on sexual and reproductive health.[487]By not providing information about entitlements under existing maternal healthcare schemes and failing to implement grievance redressal procedures, the government is not enabling women to fully claim their rights.
International Assistance and Cooperation for Maternal Mortality Reduction
States have undertaken additional obligations to provide international assistance and cooperation to ensure the realization of economic, social, and cultural rights in low-income countries. In compliance with their international obligations, states should respect the enjoyment of the right to health in other countries and prevent third parties, through political or legal means, from interfering with the enjoyment of the right.[488] In furtherance of this obligation, both the CESCR and the UN Special Rapporteur on the right to health have observed that "States should ensure that their actions as members of international organizations take due account of the right to health."[489] The CESCR has noted that members of international financial institutions such as the World Bank and regional development banks "should pay greater attention to the protection of the right to health in influencing... measures of these institutions."[490] It has reiterated that this would entail "international assistance and cooperation, especially economic and technical...which enable developing countries fulfill their core and other obligations."[491] The UN Special Rapporteur has stated that they should pay particular attention to helping other States give effect to minimum essential levels of health."[492] Following from this obligation to provide international assistance and cooperation, states have an obligation to set up an international mechanism for accountability,[493] including the obligation to design indicators to monitor states obligations at the international level.[494] Moreover, accountability as a human rights principle "extends to international actors working on health-related issues."[495]
The aid given by donor countries and international agencies is governed by the 2005 Paris Declaration on Aid Effectiveness supplemented by the 2008 Accra Agenda for Action. [496] India, along with key funding agencies and donor countries, has adhered to the Paris Declaration and the Accra Agenda for Action, and is committed to implementing them.[497]
Under the Paris Declaration, based on the principle of "mutual accountability" between donor and partner (recipient) countries, donors have committed to aligning their overall support including country strategies, policy dialogues, and development co-operation programs with partners' national development strategies and periodic reviews.[498] Donors have also undertaken to increase aid effectiveness "by strengthening the partner country's sustainable capacity to develop, implement and account for its policies to its citizens and parliament."[499]
In particular, the Declaration recognizes the "shared interest" of donors and partners "in being able to monitor progress," and to this end, both partners and donors have joined hands to "establish mutually agreed frameworks that provide reliable assessments of performance, transparency and accountability of country systems." In keeping with the principle of mutual accountability, donors have also undertaken to "provide timely, transparent and comprehensive information on aid flows."[500]
In 2008, developing countries and donors including bilateral and multilateral development institutions reiterated their commitment to accountability in the use of aid for meeting the Millennium Development Goals in the Accra Agenda for Action. "Achieving development results-and openly accounting for them-must be at the heart of all we do," endorsed ministers of countries and heads of development institutions. Acknowledging that "citizens and taxpayers of all countries expect to see tangible results of development efforts," and restating their commitment to mutual accountability, they committed to being held accountable before their "respective parliaments and governing bodies for these outcomes."[501] Recognizing that "greater transparency and accountability for the use of development resources-domestic as well as external-are powerful drivers of progress," they committed to taking several measures in furtherance of such transparency and accountability.[502] These include developing countries' and donors' commitment to "assess the impact of development policies and adjust them as necessary," through better co-ordination and linking of sources of information, statistical systems, planning, monitoring, and country-led evaluations of performance.[503] To this end, donors committed to supporting and investing in the statistical capacity and information systems of developing countries. [504]
Transparency is another key commitment, both of donors and developing countries. While developing countries will "facilitate parliamentary oversight by implementing greater transparency in public financial management, including public disclosure of revenues, budgets, expenditures, procurement and audits," donors will "publicly disclose regular, detailed and timely information on volume, allocation and, when available, results of development expenditure."[505]
Indian Legal and Policy Framework
India has a strong platform for integrating accountability as a principle into existing programs for preventable maternal mortality and morbidity. The Indian Constitution guarantees the right to life, and has been interpreted by the Supreme Court in a host of judgments as including the right to health.
It is supplemented by the NRHM which recognizes the urgent need to "transform the public health system into an accountable, accessible, and affordable system of quality services," with its vision to "improve access to rural people, especially poor women and children to equitable, affordable, accountable and effective primary health care."[506] The 2009 draft legislation on health codifies the right to health in India, including the rights to emergency treatment and care, which includes emergency obstetric care. It also defines the right to reproductive and sexual health care, which includes the "right to comprehensive obstetric healthcare services with continuum of care, including antenatal and postnatal care," and "right to safe abortion/termination of pregnancy." In addition, the draft legislation creates a detailed complaints mechanism for India.[507]
Constitutional Law and Supreme Court Decisions
Right to Health as a Enforceable Fundamental Right
The right to life is an enforceable fundamental right under article 21 of the Indian Constitution. Fundamental rights impose obligations on the state and are judicially enforceable. The Directive Principles of State Policy, under the Indian Constitution, recognize as part of the "primary duties" of the state the need "to raise the level of nutrition and the standard of living and to improve public health." Reading the "fundamental right to life" under article 21 in conjunction with the Directive Principles of State Policy, the Supreme Court of India has consistently interpreted, in a host of judgments, that the right to life includes the right to health, [508] and stated that "it is a most imperative constitutional goal."[509]
Holding that primary health centers should be one of the state's primary concerns, the court has held that "technical fetters cannot be introduced as subterfuges to cause hindrances in the establishment of health centers."[510]
The Uttar Pradesh High Court has interpreted the right to health to mean the right to adequate and quality medical care.[511]
The Fundamental Right to Admission and Treatment in Emergencies
A detailed analysis of the host of Supreme Court judgments that govern the right to health is beyond the scope of this report. Nevertheless, in the context of preventable maternal mortality and morbidity, it is particularly useful to discuss in some detail the Supreme Court's landmark judgment on the right to admission and treatment in emergencies in Paschim Bangal Khet Mazdoor Samiti v. State of West Bengal.[512] In this case, a patient with serious head injuries received first aid in a primary health center and was subsequently referred from one government hospital to another without being admitted or provided emergency treatment. After doing the rounds in three government hospitals without any success, he was compelled to go to a private hospital. Saying that there was a fundamental right to health, the Supreme Court held that there was a corresponding obligation on the state to provide emergency treatment. Holding that "a patient should not be refused admission when his condition is grave," the Supreme Court held that "the Superintendent [of the hospital] should have given guidelines to respective medical officers for admitting serious cases under any circumstances."[513]
The court issued a set of guidelines for state obligations in emergencies stating "that the guiding principle should be to ensure that no emergency case is denied medical care. All possibilities should be explored to accommodate emergency patients in serious condition."[514] The court issued the following general guidelines:
- Primary health centers should be equipped with adequate facilities to ensure basic treatment to patients, stabilizing their condition before referral.
- Hospitals at the district and sub-division levels should be upgraded so that they can provide care in serious cases.
- Number of facilities available for specialist treatment should be increased to meet the growing need, and such facilities should be available at the district and sub-divisional level hospitals.
- A centralized communication system should be put in place at the state level so that patients can be directed to a hospital which has the required care and free beds for admitting such patients.
- Patients should be transported from primary health centers to higher facilities for care in ambulances. Proper arrangements should be made to ensure that there are a sufficient number of ambulances equipped with facilities and medical personnel.
The Right to Emergency Care as a "Core" Obligation Not Subject to Financial Constraints
In the Pashchim Bangal Khet Mazdoor case, the Supreme Court cited a prior decision imposing a constitutional obligation to provide free legal aid to the poor and drew a parallel between that obligation and the obligation to provide emergency medical care. The court held,
These observations will apply with equal if not greater force in the matter of discharge of constitutional obligation of the State to provide medical aid to preserve human life. In the matter of allocation of funds for medical services the said constitutional obligation of the State has to be kept in view.[515]
The Need for a Policy Requiring Health Officials to Report Maternal Deaths
Many public health experts and human rights activists, including UNICEF, have called for a new national policy requiring all medical professionals, such as doctors, staff nurses, and ANMs, to report maternal deaths.
Public health experts and human rights activists such as Dr. Sundari Ravindran and Dr. Abhijit Das have suggested that there will be great utility to treating maternal deaths on the same platform as communicable diseases.
Prominent human rights lawyers in India such as Dr. Usha Ramanathan and Mihir Desai have noted that such a mandatory notification system is not unknown to Indian legal jurisprudence, including in the area of public health. Dr. Ramanathan said, "Such a mandatory notification system is important particularly because we are talking about deaths in extremely vulnerable communities." Especially when there is such a level of vulnerability, "the state should be pro-active and cannot put the onus on reporting deaths solely on families." Mandatory notification systems have been used in cases where the law recognizes the vulnerability of groups involved, she said, citing examples where certified medical practitioners are required to report cases where they notice the presence of an occupational health problem in workmen on whom they attend. Similarly, she explained, in case of "fatal accident or serious bodily injury" to an interstate workman, the authorities in both the state from which he originates and the state to which he has migrated to work have to be notified by the contractor who employs him, on pain of penalty.[516]
VII. Recommendations
The Indian central government and states with high maternal mortality rates have six years until 2015 to meet global goals on maternal mortality reduction. Countries such as Sri Lanka and Malaysia have shown that maternal mortality can be halved within a period of five or six years. Indian central and state governments, particularly Uttar Pradesh and similarly situated governments have an obligation to take positive measures to ensure the progressive realization of women's right to maternal health-care, and they have very strong local expertise to rely on.
The Indian central and many state governments have taken several positive measures to strengthen accountability, including measures towards institutionalizing a system of maternal death investigations, upgrading health facilities, and improving monitoring by introducing the HMIS. But implementation has lagged due to inadequate political will and failure to apply available resources to strengthen monitoring mechanisms.
To the Indian Central Government and Uttar Pradesh State Government
On Investigating Maternal Deaths
Human Rights Watch recommends that both governments should:
- Require that healthcare providers, public and private, report all pregnancy-related deaths.
- Make maternal death investigation a mandatory component of
the NRHM (as has been done with the ASHA scheme, Village Health and
Sanitation Committees, and Patient Welfare Committees). To this end:
- Allocate available resources for maternal death investigations.
- Constitute a team to develop and issue guidelines through a participatory and transparent process, preferably before the start of financial year 2010-11.
- Ensure that any procedure for investigating
maternal deaths has the following essential minimum features:
- Identifies health system shortcomings in addressing the socio-economic and medical causes of maternal deaths.
- Takes into account the underlying determinants of health such as nutrition.
- Develops remedial measures that should be implemented in a time-bound manner.
- Includes periodic reports of progress made and remedial corrective measures taken after such investigations, respecting patient privacy and confidentiality.
- Ensure that unsafe abortions are reduced by effectively implementing the Medical Termination of Pregnancy Act, 1971.
In the states that have already begun institutionalizing maternal death investigations, Human Rights Watch urges the Indian central government to assess whether the relevant policies and procedures:
- Incorporate the essential features of investigation outlined above.
- Include maternal death investigations in NRHM state annual project implementation plans.
- Integrate findings from maternal death investigations into state policy and planning under the NRHM.
- Call for periodic release of data informing the public of the findings and any remedial actions taken.
On Access to and Utilization of "Skilled Birth Attendance" and Emergency Obstetric Care
Human Rights Watch recommends that the Indian central government invite a group comprising technical experts including representatives from local nongovernmental organizations and international agencies:
- To determine whether health facilities are providing services in accordance with the NRHM concrete service guarantees and are equipped with "skilled birth attendants" as defined by international organizations such as the WHO, ICM, and FIGO. Those that pass should receive certification.
- To revise its monitoring protocols for the JSY through a participatory consultative process in accordance with the 1997 United Nations Process Indicators to Monitor the Availability, Utilization, and Quality of Emergency Obstetric Care (UN process indicators), and the United Nations Guidelines for Monitoring the Availability and Utilization of Obstetric Services (UN guidelines).
In the interim, the Indian central government, the Uttar Pradesh state government and similarly situated state governments should:
- Issue directions to identify, upgrade, and certify on priority basis a minimum number of geographically well-distributed basic and comprehensive obstetric care facilities in every district in accordance with international and national standards.
- Implement the JSY in a manner that all pregnant women, particularly women from marginalized communities and remote areas have access on an equal basis to facilities that are certified as providing "skilled care." Alternative interim arrangements for skilled birth attendance should be made in remote and underserved areas.
On Complaints Mechanisms
Human Rights Watch urges the Indian central government to constitute a high-level body consisting of governmental, nongovernmental, and intergovernmental organizations to:
- Develop, through a participatory and consultative process,
guidelines for the creation of an emergency helpline. Such a helpline
should include the following essential features:
- Be accessible to vulnerable communities, especially rural women with little or no formal education.
- Have the power to take complaints around the clock and provide immediate interventions to avert preventable maternal deaths.
- Develop, through a participatory and consultative process,
guidelines for the creation of grievance redressal mechanism through
independent facility or regional-level ombudsman's office with the
following essential features:
- Be accessible to vulnerable communities, especially rural women with little or no formal education.
- Conduct inquiries in an impartial, transparent, and time-bound manner.
- Assess complaints in keeping with the principle of non-discrimination and equality, by examining the effect of a particular action on vulnerable communities rather than the intent of the actor.
- Examine not only the conduct of frontline health workers but also district and sub-district health officials' failure or negligence in planning or oversight.
- Ensure that remedies are not restricted to taking action against individual healthcare providers in deserving cases, but also include systemic corrective actions to ensure non-recurrence of the same problem.
On the Civil Registration System
The Indian central and Uttar Pradesh state governments should appoint a full-time special officer at the national and state levels to oversee the implementation of the civil registration system, and create a special plan of action allocating funds for its implementation.
On Maternal Morbidities
Acknowledging that existing government surveys and norms address maternal morbidities to some extent, Human Rights Watch calls upon the Indian central government to:
- Ensure continuity of care to reduce not only preventable maternal mortality but also preventable maternal morbidity.
- Develop and design in consultation with governmental, nongovernmental, and intergovernmental organizations a periodic survey to monitor sexual and reproductive morbidity, including severe health conditions such as fistula, uterine prolapse, eclampsia, infertility, and so on.
To Donor Countries and International Agencies
Donor countries and international agencies have a crucial role to play in strengthening international and national accountability in reducing maternal mortality. At the international level, countries should ensure that a system for monitoring progress is put in place. Donor countries and international agencies should also be held accountable for the interventions that they promote in countries such as India.
To this end, donors and international agencies should provide technical and financial assistance for implementation of the recommendations outlined to the Indian central government and Uttar Pradesh state government above, and in particular:
- Provide technical and financial assistance to promote notification and investigation of maternal deaths.
- Provide technical and financial assistance to ensure that all government health interventions, particularly interventions funded by them, are monitored and evaluated in accordance with the UN process indicators and periodically release the results of such monitoring and evaluation to the public.
Acknowledgments
This report was written by Aruna Kashyap, researcher for the Women's Rights Division of Human Rights Watch, based on research by the author, and Nisha Varia, acting deputy director of the Women's Rights Division. The report was edited by Nisha Varia; Marianne Mollmann, advocacy director; and Liesl Gerntholtz, director of the Women's Rights Division. Aisling Reidy, senior legal advisor, and Joseph Saunders, deputy program director, also reviewed the report. Joseph Amon, director of the Health and Human Rights Division; Bede Sheppard, Asia researcher for the Children's Rights Division; and Meenakshi Ganguly, senior researcher for the Asia Division; provided input and comments on portions of the report.
We are particularly indebted to the external reviewers who commented on an early version of the report. These include Dr. Abhijit Das, director of Center for Health and Social Justice, New Delhi; Jashodhara Dasgupta, coordinator of SAHAYOG, Lucknow; Mihir Desai, advocate and human rights activist, Mumbai; Dr. Usha Ramanathan, legal researcher and human rights activist, New Delhi; and Dr. Thelma Narayan, coordinator of the Centre for Public Health and Equity, SOCHARA, Bangalore, who provided methodological and research guidance as well as inputs. Dr. Rakhal Gaitonde and Dr. Subhasri provided research support in Tamil Nadu and reviewed draft sections pertaining to Tamil Nadu. Alicia Yamin, Global Health and Human Rights Fellow at Harvard Law School, also reviewed an early version of this report. Brian Root, statistician and research methodology expert helped analyzed the data presented in this report.
Pooja Sripad and Amy Whiffen, interns in the Women's Rights Division, provided important research support. Alex Horne, former associate in the Women's Rights Division, provided research assistance. Daniela Ramirez and Chloë Fussell,associates in the Women's Rights Division provided editing and production assistance. Anna Lopriore, creative manager, Grace Choi, publications director, and Fitzroy Hepkins, mail manager, provided production assistance.
We are very grateful to the many public health experts, local NGOs, lawyers, and others who assisted our research by sharing their ideas on the subject, in particular, Dr. Abhay Shukla, Chayanika Shah, Prof. Dileep Mavalankar, Dr. Neelam Singh, Kranti, former Registrar General of India P. Padmanabha, Sabala, Dr. Sharad Iyengar, Dr. Sundari Ravindran, and Dr. Vishwajeet Kumar. We also thank members of Saksham, Vanangana, Vatsalya, Action Aid India, CARE India, Healthwatch Forum, and the Uttar Pradesh Jan Swasthya Abhiyan.The views expressed in this report are those of Human Rights Watch and Human Rights Watch takes full responsibility for any errors or omissions.
CEHAT (Mumbai), SAHAYOG (Lucknow), and Vatsalya (Lucknow) provided research support by allowing Human Rights Watch to use their documentation center and library. Healthwatch Forum-Uttar Pradesh provided invaluable assistance with processing the applications filed under the Right to Information Act.
Above all, we thank all families of deceased pregnant women who recounted their experiences. We also acknowledge the government officials, doctors, and health workers who agreed to be interviewed at length for this report.
We acknowledge with gratitude the financial support of Arcadia and the other donors who have supported the work of the Women's Rights Division of Human Rights Watch.
Appendix I
Country |
PMDF (%) |
Number of Maternal Deaths |
Lifetime risk of maternal death: 1 in: |
MMR |
Lower Estimate |
Upper Estimate |
Sierra Leone |
39 |
5400 |
8 |
2100 |
880 |
3700 |
Afghanistan |
41 |
26000 |
8 |
1800 |
730 |
3200 |
Niger |
47 |
14000 |
7 |
1800 |
840 |
2900 |
Chad |
50 |
6900 |
11 |
1500 |
930 |
2000 |
Angola |
34 |
11000 |
12 |
1400 |
560 |
2600 |
Somalia |
33 |
5200 |
12 |
1400 |
550 |
2700 |
Rwanda |
35 |
4700 |
16 |
1300 |
770 |
1800 |
Liberia |
39 |
2100 |
12 |
1200 |
520 |
2100 |
Burundi |
40 |
3900 |
16 |
1100 |
480 |
1900 |
Dem Rep of Congo |
43 |
32000 |
13 |
1100 |
480 |
1900 |
Guinea-Bissau |
44 |
890 |
13 |
1100 |
500 |
1800 |
Malawi |
68 |
6000 |
18 |
1100 |
720 |
1500 |
Nigeria |
34 |
59000 |
18 |
1100 |
440 |
2000 |
Cameroon |
37 |
5700 |
24 |
1000 |
670 |
1400 |
Central African Republic |
31 |
1500 |
25 |
980 |
380 |
1900 |
Senegal |
38 |
4100 |
21 |
980 |
590 |
1400 |
Mali |
33 |
6400 |
15 |
970 |
620 |
1300 |
Lesotho |
39 |
480 |
45 |
960 |
570 |
1400 |
United rep of Tanzania |
28 |
13000 |
24 |
950 |
620 |
1300 |
Guinea |
40 |
3500 |
19 |
910 |
590 |
1200 |
Benin |
34 |
2900 |
20 |
840 |
330 |
1600 |
Nepal |
22 |
6500 |
31 |
830 |
290 |
1900 |
Zambia |
37 |
3900 |
27 |
830 |
520 |
1200 |
Mauritania |
41 |
1000 |
22 |
820 |
480 |
1200 |
Cote D'Ivoire |
29 |
5400 |
27 |
810 |
310 |
1600 |
Congo |
53 |
1300 |
22 |
740 |
450 |
1100 |
Ethiopia |
28 |
22000 |
27 |
720 |
460 |
980 |
Burkina Faso |
25 |
4300 |
22 |
700 |
390 |
1000 |
Gambia |
25 |
360 |
32 |
690 |
250 |
1500 |
Equatorial Guinea |
22 |
150 |
28 |
680 |
210 |
1600 |
Haiti |
24 |
1700 |
44 |
670 |
390 |
960 |
Laos |
20 |
1300 |
33 |
660 |
190 |
1600 |
Djibouti |
25 |
180 |
35 |
650 |
240 |
1400 |
Bangladesh |
21000 |
51 |
570 |
380 |
760 |
|
Ghana |
22 |
3800 |
45 |
560 |
200 |
1300 |
Kenya |
32 |
7700 |
39 |
560 |
340 |
800 |
Uganda |
40 |
8100 |
25 |
550 |
350 |
770 |
Cambodia |
16 |
2300 |
48 |
540 |
370 |
720 |
Gabon |
28 |
220 |
53 |
520 |
290 |
760 |
Mozambique |
25 |
4000 |
45 |
520 |
360 |
680 |
Madagascar |
24 |
3600 |
38 |
510 |
290 |
740 |
Togo |
23 |
1200 |
38 |
510 |
290 |
750 |
Guyana |
10 |
73 |
90 |
470 |
140 |
1600 |
Papua New Guinea |
16 |
820 |
55 |
470 |
130 |
1300 |
Eritrea |
32 |
760 |
450 |
180 |
850 |
|
►INDIA |
117000 |
70 |
450 |
300 |
600 |
|
Sudan |
23 |
5300 |
53 |
450 |
160 |
1000 |
Bhutan |
22 |
280 |
55 |
440 |
160 |
970 |
Yemen |
26 |
3600 |
39 |
430 |
150 |
900 |
Indonesia |
11 |
19000 |
97 |
420 |
240 |
600 |
Comoros |
25 |
110 |
52 |
400 |
150 |
840 |
South Africa |
6 |
4300 |
110 |
400 |
270 |
530 |
Swaziland |
16 |
120 |
120 |
390 |
130 |
980 |
Botswana |
12 |
170 |
130 |
380 |
120 |
1000 |
Myanmar |
3700 |
110 |
380 |
260 |
510 |
|
Timor-Leste |
42 |
190 |
35 |
380 |
150 |
700 |
Dem Rep of Korea |
9 |
1300 |
140 |
370 |
110 |
1200 |
Pakistan |
15 |
15000 |
74 |
320 |
99 |
810 |
Iraq |
20 |
2900 |
72 |
300 |
110 |
600 |
Bolivia |
14 |
760 |
89 |
290 |
160 |
430 |
Guatemala |
22 |
1300 |
71 |
290 |
100 |
650 |
Honduras |
10 |
580 |
93 |
280 |
190 |
380 |
Morocco |
18 |
1700 |
150 |
240 |
140 |
350 |
Peru |
14 |
1500 |
140 |
240 |
170 |
310 |
Philippines |
11 |
4600 |
140 |
230 |
60 |
700 |
Solomon Islands |
18 |
34 |
100 |
220 |
65 |
580 |
Cape Verde |
16 |
32 |
120 |
210 |
68 |
530 |
Ecuador |
12 |
600 |
170 |
210 |
65 |
560 |
Fiji |
9 |
41 |
160 |
210 |
55 |
720 |
Namibia |
22 |
110 |
170 |
210 |
110 |
300 |
Algeria |
10 |
1200 |
220 |
180 |
55 |
520 |
El Salvador |
13 |
290 |
190 |
170 |
55 |
460 |
Jamaica |
11 |
89 |
240 |
170 |
51 |
510 |
Nicaragua |
9 |
270 |
150 |
170 |
120 |
230 |
Tajikistan |
12 |
320 |
160 |
170 |
53 |
460 |
Dominican Republic |
15 |
310 |
230 |
150 |
90 |
210 |
Kyrgyzstan |
8 |
170 |
240 |
150 |
43 |
460 |
Lebanon |
6 |
99 |
290 |
150 |
41 |
500 |
Paraguay |
11 |
260 |
170 |
150 |
99 |
200 |
Viet Nam |
8 |
2500 |
280 |
150 |
40 |
510 |
Iran |
5 |
1900 |
300 |
140 |
95 |
190 |
Kazakhstan |
3 |
340 |
360 |
140 |
40 |
500 |
Colombia |
10 |
1200 |
290 |
130 |
38 |
370 |
Egypt |
2400 |
230 |
130 |
84 |
170 |
|
Panama |
11 |
91 |
270 |
130 |
39 |
410 |
Syria |
11 |
700 |
210 |
130 |
40 |
370 |
Turkmenistan |
6 |
140 |
290 |
130 |
37 |
400 |
Maldives |
20 |
12 |
200 |
120 |
42 |
260 |
Brazil |
4100 |
370 |
110 |
74 |
150 |
|
Thailand |
1100 |
500 |
110 |
70 |
140 |
|
Tunisia |
5 |
170 |
500 |
100 |
27 |
380 |
Libya |
7 |
130 |
350 |
97 |
28 |
300 |
Albania |
5 |
49 |
490 |
92 |
26 |
300 |
Azerbaijan |
4 |
110 |
670 |
82 |
21 |
290 |
Argentina |
530 |
530 |
77 |
51 |
100 |
|
Armenia |
3 |
26 |
980 |
76 |
23 |
250 |
Suriname |
7 |
530 |
72 |
72 |
140 |
|
Georgia |
3 |
32 |
1100 |
66 |
18 |
230 |
Oman |
8 |
41 |
420 |
64 |
18 |
200 |
Jordan |
92 |
450 |
62 |
41 |
82 |
|
Malaysia |
340 |
560 |
62 |
41 |
82 |
|
Mexico |
1300 |
670 |
60 |
60 |
120 |
|
Sri Lanka |
190 |
850 |
58 |
39 |
77 |
|
Venezuela |
340 |
610 |
57 |
57 |
110 |
|
Belize |
4 |
560 |
52 |
52 |
100 |
|
Mongolia |
27 |
840 |
46 |
46 |
93 |
|
China |
7800 |
1300 |
45 |
30 |
60 |
|
Cuba |
6 |
1400 |
45 |
45 |
90 |
|
Trinidad and Tobago |
8 |
1400 |
45 |
45 |
89 |
|
Turkey |
650 |
880 |
44 |
29 |
58 |
|
UAE |
5 |
25 |
1000 |
37 |
10 |
130 |
Bahrain |
4 |
1300 |
32 |
21 |
42 |
|
Costa Rica |
24 |
1400 |
30 |
30 |
60 |
|
Russian Federation |
430 |
2700 |
28 |
28 |
55 |
|
Estonia |
3 |
2900 |
25 |
25 |
50 |
|
Romania |
51 |
3200 |
24 |
24 |
49 |
|
Uzbekistan |
150 |
1400 |
24 |
24 |
49 |
|
Rep of Moldova |
9 |
3700 |
22 |
22 |
44 |
|
Uruguay |
11 |
2100 |
20 |
20 |
40 |
|
Belarus |
16 |
4800 |
18 |
18 |
25 |
|
Puerto Rico |
10 |
2900 |
18 |
18 |
36 |
|
Saudi Arabia |
120 |
1400 |
18 |
12 |
24 |
|
Ukraine |
71 |
5200 |
18 |
18 |
36 |
|
Bahamas |
1 |
2700 |
16 |
16 |
33 |
|
Barbados |
1 |
4400 |
16 |
16 |
31 |
|
Chile |
40 |
3200 |
16 |
16 |
32 |
|
Mauritius |
3 |
3300 |
15 |
15 |
30 |
|
Rep of Korea |
63 |
6100 |
14 |
14 |
27 |
|
Serbia and Montenegro |
16 |
4500 |
14 |
14 |
27 |
|
Singapore |
5 |
6200 |
14 |
14 |
27 |
|
Brunei |
1 |
1 |
2900 |
13 |
3 |
47 |
Luxemburg |
1 |
5000 |
12 |
12 |
23 |
|
Qatar |
2 |
2700 |
12 |
8 |
16 |
|
Bulgaria |
7 |
7400 |
11 |
11 |
22 |
|
Lithuania |
3 |
7800 |
11 |
11 |
22 |
|
Portugal |
12 |
6400 |
11 |
7 |
14 |
|
USA |
440 |
4800 |
11 |
11 |
21 |
|
Cyprus |
1 |
6400 |
10 |
10 |
20 |
|
Latvia |
2 |
8500 |
10 |
10 |
19 |
|
The Former Yugoslav Republic of Macedonia |
2 |
6500 |
10 |
10 |
20 |
|
New Zealand |
5 |
5900 |
9 |
9 |
18 |
|
Belgium |
9 |
7800 |
8 |
8 |
16 |
|
France |
59 |
6900 |
8 |
8 |
16 |
|
Malta |
0 |
8300 |
8 |
8 |
17 |
|
Poland |
27 |
10600 |
8 |
5 |
10 |
|
UK |
51 |
8200 |
8 |
8 |
15 |
|
Canada |
21 |
11000 |
7 |
7 |
13 |
|
Croatia |
3 |
10500 |
7 |
7 |
15 |
|
Finland |
4 |
8500 |
7 |
7 |
15 |
|
Norway |
4 |
7700 |
7 |
7 |
15 |
|
Hungary |
5 |
13300 |
6 |
6 |
11 |
|
Japan |
70 |
11600 |
6 |
6 |
12 |
|
Netherlands |
11 |
10200 |
6 |
6 |
12 |
|
Slovakia |
3 |
13800 |
6 |
6 |
12 |
|
Slovenia |
1 |
14200 |
6 |
6 |
12 |
|
Switzerland |
4 |
13800 |
5 |
5 |
11 |
|
Australia |
11 |
13300 |
4 |
4 |
9 |
|
Austria |
3 |
21500 |
4 |
4 |
7 |
|
Czech Republic |
4 |
18100 |
4 |
4 |
9 |
|
Germany |
29 |
19200 |
4 |
4 |
9 |
|
Iceland |
0 |
12700 |
4 |
4 |
8 |
|
Israel |
6 |
7800 |
4 |
4 |
9 |
|
Kuwait |
2 |
9600 |
4 |
4 |
6 |
|
Spain |
20 |
16400 |
4 |
4 |
9 |
|
Bosnia and Herzegovina |
1 |
29000 |
3 |
3 |
6 |
|
Denmark |
2 |
17800 |
3 |
3 |
6 |
|
Greece |
3 |
25900 |
3 |
2 |
4 |
|
Italy |
15 |
26600 |
3 |
3 |
6 |
|
Sweden |
3 |
17400 |
3 |
3 |
7 |
|
Ireland |
1 |
47600 |
1 |
1 |
2 |
Appendix II
Appendix III
Appendix IV
Note on the Death Registration and Notification System in India
The Registration of Births and Deaths Act, 1969, creates a hierarchical structure of registrars of births and deaths. At the highest end of the spectrum is the Registrar General of India and at the lowest end or local village council level is the sub-registrar or registrar.
Notifiers and registrars are in charge of reporting and registering deaths. The law identifies "notifiers" of births and deaths and obliges them to give information about a death to the nearest registrar. Midwives or health attendants present at death irrespective of its place of occurrence, medical officers in charge of hospitals, and owners or keepers of crematoriums or burial grounds are obliged to give information to registrars about deaths.[517] Doctors, staff nurses, nurse-midwives, ASHAs, and trained traditional birth attendants who are present at the time of delivery are notifiers and should report all deaths to the nearest registrar.[518] In addition, where a death occurs at home, the head of the household should notify the death. And where a death occurs at in any other public place, the person in charge is supposed to notify such deaths.[519]
The Uttar Pradesh government has developed separate notification forms called "death report forms." These forms have a column asking the cause of death. But they also ask whether the death is pregnancy-related, that is, whether the woman died during, at the time of, or six weeks after the termination of pregnancy.[520] So even if notifiers do not know the cause of death, all pregnancy-related deaths can be notified where they have information about the pregnancy.
Registrars should, as soon as the information of a birth or death is given to them, note the details in a register.[521] They should provide an extract of the information (birth or death certificate) recorded by them to the person giving such information. The Uttar Pradesh government has prescribed formats for maintaining and issuing death certificates.[522]
The Uttar Pradesh government has issued government orders asking ANMs, medical officers in charge of primary health centers, and superintendents of community health centers to discharge the functions of birth and death registrars.[523] Village development officers or gram vikas adhikaris are also appointed as registrars.[524] Where a pregnant woman dies in the presence of an ANM during or after delivery, by virtue of being present at the time of delivery, the ANM can automatically register the death and issue a death certificate. Alternatively, if the ANM receives information about a death through the ASHA, she should record it and issue a death certificate. This is also true for medical officers of primary health centers and superintendents of community health centers.
This general registration process is supplemented by a special medical cause of death certification process. The Government of India through the Registrar General's Office has launched the Medical Cause of Death Certification scheme which is implemented in many hospitals of Uttar Pradesh. Under this scheme, the Indian government provides financial and technical support for governments to train and ensure that causes of death are medically certified in hospitals.
Appendix V
[1] Maternal mortality ratio is defined as the number of maternal deaths per 100,000 live births.
[2] World Health Organization (WHO) et al., "Maternal Mortality in 2005, Estimates developed by WHO, UNICEF, UNFPA and the World Bank," 2007, www.who.int/reproductive-health/publications/maternal_mortality_2005/mme_2005.pdf (accessed November 22, 2008. Please refer to "Note on Estimates," in the section below titled "Methodology" for further details about adjustment of country-level data.
[3] WHO defines a maternal death as the death of a woman or girl while pregnant or within 42 days of termination of pregnancy (childbirth or abortion), from any cause related to or aggravated by the pregnancy or its management.
[4] Human Rights Watch filed seven applications in all and received information in two applications. The others are pending at the writing of this report.
[5] The members of this group are Dr. Abhijit Das, director of the Center for Health and Social Justice, New Delhi; Jashodhara Dasgupta, coordinator of SAHAYOG, Lucknow; Mihir Desai, advocate and human rights activist, Mumbai; Dr. Usha Ramanathan, legal researcher and human rights activist, New Delhi; and Dr. Thelma Narayan, coordinator of the Centre for Public Health and Equity, SOCHARA, Bangalore.
[6] The Empowered Action Group is an administrative mechanism established by the Indian central government in 2001 to closely monitor the implementation of family welfare programs and goals set under the National Population Policy, 2000. It comprises of eight states: Uttar Pradesh, Uttaranchal, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Rajasthan, and Orissa.
[7] See Appendix II which presents data drawn from a national survey. Human Rights Watch phone discussions with public health experts and women's health rights activists in India, November 2008 to February 2009; Human Rights Watch discussions with doctors, activists, and lawyers during the National Consultation to Prevent Maternal Mortality in India by Using Public Interest Litigations, Mumbai, December 22-23, 2008.
[8] Registrar General of India and Center for Global Health Research, Maternal Mortality in India: 1997-2003, Trends, Causes and Risk Factors (New Delhi, 2006), p.xvi.
[9] See Registrar General of India, "Special Bulletin on Maternal Mortality in India 2004-2006, Sample Registration System," April 2009, http://www.censusindia.gov.in/Vital_Statistics/SRS_Bulletins/MMR-Bulletin-April-2009.pdf (accessed July 28, 2009) for the latest official Indian government data on maternal mortality in India.
[10] World Health Organization (WHO) et al., "Maternal Mortality in 2005, Estimates developed by WHO, UNICEF, UNFPA and the World Bank," 2007, www.who.int/reproductive-health/publications/maternal_mortality_2005/mme_2005.pdf (accessed November 22, 2008); Hill et al., "Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data," vol. 370, The Lancet (2007), pp. 1311–19.
[11]There is a 95 percent chance that the estimated MMR falls within the margin; a 5 percent chance that it will fall outside of the estimated margin.
[12] Please refer to the graphs depicting MMR reduction over time in India and different states.
[13] WHO, Beyond the Numbers: Reviewing maternal deaths and complications to make pregnancy safer (Geneva: WHO, 2004), p. 4.
[14]WHO et al., Maternal Mortality in 2005, p. 1.
[15] Human Rights Council, Report of the UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, A/61/338, September 13, 2006, para. 7; UN Millennium Project Task Force on Child Health and Maternal Health, Who's Got the Power? Transforming Health Systems for Women and Children (London: Earthscan, 2005), p. 6, figure 2.
[16]The estimates for the number of women who develop pregnancy-related illnesses vary. See Report of the UNSR on health, September 2006, para. 8, where he puts this figure at 30 citing earlier UNICEF data; UNICEF, State of the World's Children, 2009, p. 4, says that 20 times as many women develop complications; the Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 80, estimates that 30-50 times as many women suffer from maternal morbidities.
[17] UNFPA Campaign to End Obstetric Fistula, "Frequently Asked Questions," http://www.endfistula.org/q_a.htm (accessed July 28, 2009). The UNFPA Campaign states that these estimates are too low.
[18] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 80.
[19] WHO et al., Maternal Mortality in 2005, p. 1; UN Inter-Agency and Expert Group on MDG Indicators, The Millennium Development Goals Report (New York: UN Department of Economic and Social Affairs, 2008), p. 24.
[20]WHO, World Health Report 2005, p. 62; Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 79.
[21] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 79.
[22] Ibid., p. 80.
[23] See below, section on "Reduction Strategies" for more details about basic emergency and comprehensive emergency services.
[24] Maine and Larsen 2004, as cited in the Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 85.
[25] Human Rights Watch interview with Premlal P. (pseudonym), Barabanki district, June 1, 2009; group interview with activists (names withheld), Unnao district, March 2, 2009.
[26] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, pp. 81-88. A fourth critical intervention, family planning, is beyond the scope of this report.
[27] UNICEF et al., Guidelines for Monitoring the Availability and Use of Obstetric Services (2nd edn., New York: UNICEF, 1997), p. 26
[28] Ibid.
[29] Koblinsky and Campbell 2003, p. 17 as cited in the Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 85.
[30] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, pp. 84-6.
[31] Ibid.; WHO, Everybody's Business: Strengthening Health Systems to Improve Health Outcomes (WHO: Geneva, 2007), p. v; Department for International Development, "Reducing maternal deaths: Evidence and action, A strategy for DFID," September 2004, p. 19; Lynn Freedman, "Achieving the MDGs: Health systems as core social institutions," Development vol. 48 no. 1 (2005), p. 22.
[32] Report of the International Conference on Population and Development, October 1994, A/CONF.171/13, http://www.un.org/popin/icpd/conference/offeng/poa.html (accessed November 20, 2008).
[33] UN Millennium Declaration, September 18, 2000, G.A. Res. 55/2, U.N. GAOR, 55th Sess., Supp. No. 49, at 4, U.N. Doc. A/55/49 (2000), para. 19.
[34]See for example Sofia Gruskin et al., "Using human rights to improve maternal and neonatal health: history, connections and a proposed practical approach," Bulletin of the World Health Organization, vol. 86 (2008), p. 589. The authors state that between 1990 and 2005, the global levels of maternal mortality have been reducing at less than 1 percent annually, far below the required 5.5 percent annual decline required to meet the MDG; UNICEF, State of the World's Children, 2009, also states that progress on maternal mortality is not adequate to meet the MDG goal.
[35] O. M. R. Campbell and W. J. Graham, "Strategies for reducing maternal mortality: getting on with what works," The Lancet, vol. 368 (2006), at pp. 1284–99; Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 77.
[36]"Countdown to 2015, Maternal, Newborn, and Child Survival: the 2008 report on tracking coverage on interventions," The Lancet, vol. 371 (2008), p. 1247.
[37] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, pp. 27, 80. The report notes that due to high rates of HIV, over a period of ten years, maternal mortality in Zimbabwe and Malawi grew 2.5 and 1.9 times respectively.
[38] WHO et al., Maternal Mortality in 2005, Annex 3; "Countdown to 2015, Maternal, Newborn, and Child Survival: the 2008 report on tracking coverage on interventions," The Lancet, vol. 371 (2008), p. 1247.
[39] Government of India, District Level Facility and Household Survey, 2007-2008 (DLHS-3), http://www.rchiips.org/pdf/rch3/state/Uttar-Pradesh.pdf (accessed May 18, 2009), unpaginated.
[40] Government of India, National Family and Health Survey (NFHS-3), 2005-2006, http://www.nfhsindia.org/NFHS-3%20Data/VOL-1/india_volume_I_chapter_8_corrected_for_website_17oct08.pdf (accessed May 18, 2009), pp. 192-3. Difficulty with vision during the daytime: 7.2 percent (rural), 3.8 percent (urban); night blindness: 10.8 percent (rural), 3.7 percent (urban); convulsions not from fever: 11.3 percent (rural), 7.4 percent (urban); swelling of the legs, body, or face: 24.1 percent (rural), 28.0 percent (urban); excessive fatigue: 48.7 percent (rural), 45.2 percent (urban); vaginal bleeding: 4.1 percent (rural), 5.2 percent (urban).
[41] See above, section titled "Methodology" for a list of the EAG states. Human Rights Watch phone discussion and email communication with Dr. Abhijit Das, member, Advisory Group for Community Action under the NRHM, August 22, 2009. As Dr. Das points out, even though these states have registered an MMR decline in absolute terms, their MMR when expressed in terms of overall India MMR has actually increased. For instance, in 1997, Uttar Pradesh had an MMR that was 1.5 times that of India's, whereas now it is 1.7 times. Similarly, Assam's MMR has increased from 1.4 times to 1.9 times, and Orissa from 0.9 times to 1.2 times.
[42] Registrar General of India, Maternal Mortality in India: 2004-2006, unpaginated.
[43] NFHS-3 2005-2006, p. 222, table 8.23. See Appendix II.
[44] Ibid., pp. 192-3.
[45] Ibid., pp. 209, 214, 194-5, 200. See Appendix II.
[46] UNICEF, Maternal and Perinatal Death Inquiry and Response,Empowering Communities to Avert Maternal Deaths in India (New Delhi: UNICEF, 2008), p. 37.
[47] Registrar General of India, Maternal Mortality in India: 1997-2003, p. 23.
[48] Ibid.
[49] Human Rights Watch phone discussions with public health experts and activists in India, November 2008 to February 2009.
[50] Kranti S. Vora et al., "Maternal Health Situation in India: A Case Study," Journal of Health, Population, and Nutrition, vol. 27, no. 2 (2009), p. 184.
[51]National Population Policy, 2000.
[52]Ibid.; Ministry of Health and Family Welfare, Government of India, "National Rural Health Mission: Meeting people's needs in rural areas, Framework for implementation 2005-2012," http://mohfw.nic.in/NRHM/Documents/NRHM%20-%20Framework%20for%20Implementation.pdf (accessed May 15, 2009), p. 10; Planning Commission of India, Eleventh Five Year Plan 2007-12, (accessed April 24, 2009), p. 59; "Contribution by India, India's development efforts towards the Millennium Development Goals," United Nations High-level Event on the Millennium Development Goals (MDGs), September 2008.
[53] See National Population Policy, 2000; National Health Policy, 2002; NRHM Framework for Implementation, p. 10. There are two different goals-to reduce MMR to below 1o0 by 2010 and 2012.
[54] Planning Commission of India, Eleventh Five Year Plan 2007-12, vol. 2, chap. 3, http://planningcommission.nic.in/plans/planrel/fiveyr/11th/11_v2/11v2_ch3.pdf (accessed April 24, 2009), para. 3.1.12.
[55] Registrar General of India, Maternal Mortality in India: 2004-2006, unpaginated.
[56] NRHM Framework for Implementation, p. 121; See Ministry of Health and Family Welfare, Government of India, "Indian Public Health Standards (IPHS), Guidelines for sub-centers, primary health centers, and community health centers," March 2006, http://mohfw.nic.in/NRHM/Documents/ (accessed November 20, 2008).
[57] See Government of India, "Rural Health Care System in India," Bulletin on Rural Statistics in India, 2008 (updated as on March 2008), July 2009, http://www.mohfw.nic.in/Bulletin%20on%20RHS%20-%20March,%202008%20-%20PDF%20Version/RHS%20Bulletin%20-%20March%202008%20-%20Final%20Tables.pdf (accessed August 17, 2009), p.1; Kranti S. Vora et al., "Maternal Health Situation in India: A Case Study," p. 189. See table below for a description of the NRHM service guarantees. According to these service guarantees, at least in theory, primary health centers should provide basic emergency obstetric care and all facilities from the community health center upwards should provide comprehensive emergency obstetric care.
[58] NRHM Framework for Implementation, p. 8.
[59] Ibid., pp. 9-10.
[60] Ibid., p. 8.
[61] When NRHM was launched the RCH program was in its second phase of implementation and was commonly referred to as RCH-II.
[62] NRHM Framework for Implementation, pp. 14, 121-3. See "Government focuses on Strengthening of primary health infrastructure and improving service delivery," Government of India press release, MV/GK, July 2, 2009, http://pib.nic.in/release/release.asp?relid=49552 (accessed July 15, 2009). 7,212 of the 22,370 primary health centers are supposedly operating as around-the-clock facilities across India.
[63] NRHM Framework for Implementation, p. 79.
[64] Ibid.
[65]Ibid., Annex-II, pp. 37 and 121. A key NRHM strategy to promote equitable access is "exemption…of below poverty line families from all charges." Further the NRHM guarantees "[f]ull coverage for inpatient treatment of maternal diseases/health conditions (free for 50 percent user charges from APL [above poverty line]"; See Government of India, Indian Public Health Standards (IPHS), Guidelines for sub-centers, primary health centers, and community health centers, March 2006. 50 percent of the fee is charged to women above the poverty line.
[66] NFHS-3 2005-2006, p. 209.
[67] Kaveri Gill, "A Primary Evaluation of Service Delivery under the National Rural Health Mission (NRHM): Findings from a Study in Andhra Pradesh, Uttar Pradesh, Bihar, and Rajasthan," Working Paper 1/2009 – PEO, Planning Commission of India, May 2009, http://www.planningcommission.nic.in/reports/wrkpapers/wrkp_1_09.pdf (accessed May 15, 2009), p. 11.
[68] Maternal Health Division of the Ministry of Health and Family Welfare, "Janani Suraksha Yojana (JSY, Mother Protection Scheme): Features and Frequently Asked Questions and Answers," October 2006, http://mohfw.nic.in/dofw%20website/ JSY_features_ FAQ _Nov_2006.htm (accessed May 15, 2009). The JSY replaces the earlier National Maternity Benefit Scheme (NMBS) which provided cash assistance to all pregnant women below the poverty line irrespective of place of delivery. The criteria for eligibility vary according to whether states are classified as "High Performing" or "Low Performing" based on the levels of home-based and health-facility based deliveries. In ten low performing states of Uttar Pradesh, Uttaranchal, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Assam, Rajasthan, Orissa and Jammu and Kashmir, the JSY cash assistance is provided to all women. In the other states, the JSY cash assistance is limited to women below the poverty line, or scheduled caste and scheduled tribe women above age 19 and with fewer than two live children. Some government documents state that where women have a third child they are entitled to benefits on the condition of sterilization.
[69] "Health Care Delivery in Mission Mode," Government of India press release, DS/GK/yearend-420, December 17, 2008, http://pib.nic.in/release/rel_print_page.asp?relid=45769 (accessed June 29, 2009).
[70] JSY Features and Frequently Asked Questions and Answers, paras. 2 and 3.1.
[71] Ibid., paras. 2 and 4.2. See below, section titled "Gaps in Continuity of Care" for more details.
[72] Ibid.
[73] The cash incentive in urban areas differs.
[74] The cash incentive in the non-focus states is limited to women above age 19 for up to two live children. Moreover these women have to be below the poverty line or belong to a scheduled caste or tribe.
[75] Initiative for Health Equity and Society (IHES) and Human Rights Law Network (HRLN), Conference on Using Legal Tools for Preventing Maternal Mortality, Mumbai, December 22-23, 2008; SAHAYOG and Centre for Health and Social Justice (CHSJ), A Civil Society Dialogue Towards a Coalition for the Right to Maternal Health," New Delhi, April 21, 2009.
[76] Kaveri Gill, Table 1.9, p. 65. Gill's study of NRHM allocation and expenditure in the four states of Rajasthan, Uttar Pradesh, Bihar, and Andhra Pradesh showed that money was unspent in all of them through 2005-2008.
See Pathrank N.R.H.M./A.D./Janpadeeya.Inno./08-09/5790-7/Dinank 27.01.2009, Preshak Mission Nirdeshak, Seva Mein Samasth Mukhya Chikitsa Adhikari, Uttar Pradesh (Letter no. N.R.H.M./A.D./Population Innovations/08-09/5790-7/Dated 27.01.2009, From Mission Director to All Chief Medical Officers).
[77] Human Rights Watch interviews with officer-1 and activist (who requested anonymity), Lucknow, February 25, 2009.
[78] Letter from Uttar Pradesh NRHM Mission Director Chanchal Tiwari to All (70) Chief Medical Officers, No. NRHM AD/District Innovation/08-09/5790-07/dated 27.01.2009.
[79] Human Rights Watch phone discussions with public health and women's rights activists, November 2008 to December 2008.
[80] Ibid. See also The Indian Women's Health Charter, 2007.
[81] Human Rights Watch phone discussions with Dr. Sundari Ravindran, August 11, 2009.
[82] See NRHM Framework for Implementation, p. 118. Under the Pulse Polio Immunization program under NRHM, "all out efforts are being made to eradicate all the strains of the polio virus in the country." The pulse polio immunization campaign is also intended to strengthen the immunization coverage of children and pregnant women.
[83] Human Rights Watch group interview with Dr. Khatloiya, Director General (Family Welfare), Dr. C. V Prasad, Director (Family Welfare), and Dr. S. K. Jain, Director (Maternal and Child Health), Lucknow, March 12, 2009.
[84] United States Agency for International Development (USAID)-India, "Report on maternal death audits in Uttar Pradesh," August 2006, as cited inMaternal Death Notification and Review System, Final Report submitted to the Uttar Pradesh Health Systems Development Project, January 2008, p. 15.
[85] Report of the Working Group on Empowerment of Women, Planning Commission of India, p. 100. See also Indian Women's Health Charter, 2007, p. 13, where the Indian women's movement demands "access, irrespective of women's marital status, to safe, effective, reversible, user-controlled contraceptives that encourage male participation." Human Rights Watch discussions with Chayanika, Forum Against Oppression of Women, December 13, 2008.
[86] See Report of the Working Group on Empowerment of Women, Planning Commission of India, http://planningcommission.nic.in/aboutus/committee/wrkgrp11/wg11_rpwoman.pdf (accessed June 12, 2009) p. 100. The working group notes that "The current policy focus on female sterilization should be broadened to providing people with greater reproductive choice. This includes better access to contraception, more information about birth spacing, increasing male responsibility for small families, as well as providing greater education and economic opportunities for women."
[87] Human Rights Watch interviews with 23 rural women including pregnant woman from Chitrakoot, Unnao, and Bae Bareilly districts, February and March 2009. The National Family and Health Survey also supports these women's accounts. See NFHS-3 2005-2006, p. 445, Table 13.16. For matters discussed during contact with health workers, 70 percent of pregnant women and women with children reported "immunization," and 9 percent of them reported that family planning was discussed. In contrast, delivery care, delivery preparedness, and postnatal care are 4.4 percent, 1.0 percent, and 2.3 percent respectively.
[88] Human Rights Watch group interview with Revati R. (pseudonym) and others, relatives and neighbors of deceased mother, village RB-1 (name withheld), Rae Bareilly district,February 26, 2009.
[89] Alternatively, some government documents state that women undergoing a third live birth are eligible to JSY benefits provided they agree to get themselves sterilized. See "Cabinet Committee on Economic Affairs (CCEA) clears Janani Suraksha Yojana," Government of India press release, EK/MK, March 30, 2005,http://pib.nic.in/release/release.asp?relid=8258&kwd= (accessed June 29, 2009). "Women aged 19 years and above, belonging to below poverty line families will be eligible for benefit under the scheme for first two live births. In the 10 Low Performing States viz. Bihar, Chattisgarh, Jharkhand, Madhya Pradesh, Orissa, Rajasthan, Utttar Pradesh, Uttranchal [sic], Assam and Jammu & Kashmir, however, families will be eligible for benefit for third birth also, provided the beneficiary opts for sterlization [sic] immediately after delivery." See also, National Rural Health Mission Training Manual Book One for ASHAs, http://www.mohfw.nic.in/NRHM/Documents/Module1_ASHA.pdf (accessed, August 27, 2009), p. 71. "Women undergoing third live births are also eligible provided they undergo sterilization."
[90] NFHS-3 2005-2006, pp. 197, 209.
[91] Human Rights Watch phone discussions with public health and women's rights activists in India, November 2008 to February 2009.
[92] Office of the High Commissioner for Human Rights, Claiming the Millennium Development Goals: A human rights approach (Geneva: United Nations, 2008), http://www.ohchr.org/Documents/Publications/Claiming_MDGs_en.pdf (accessed June 12, 2009), p. 15.
[93] See below, section titled "International and Indian Human Rights Framework" for accountability as a principle in international human rights law.
See also, Lynn Freedman, "Human rights, constructive accountability and maternal mortality in the Dominican Republic: a commentary," vol. 82 International Journal of Gynecology and Obstetrics (2003) pp. 111; Helen Potts, "Accountability and the Right to the Highest Attainable Standard of Health," Essex Human Rights Center, 2008, http://www2.essex.ac.uk/human_rights_centre/rth/docs/HRC_Accountability_Mar08.pdf (accessed May 15, 2009) where she explains that a crucial function of accountability is to be prospective or forward-looking, correcting failures.
[94] See Appendix II.
[95] Human Rights Watch phone discussions with women's health rights activists from Gujarat, Kerala, Karnataka, and West Bengal, November 2008 to December 2009.
[96] See Bulletin on Rural Statistics, 2008, pp.25, 29, 37, 38, 39. All-India data reveals that there is a shortfall in the required number of community health centers by 36 percent. Roughly 60 percent of community health centers do not have a surgeon, obstetrician, or physician and 50 percent do not have laboratory technicians.
[97] First referral units for emergency obstetric care have been supposedly part of safe motherhood initiatives since at least the 1992 Child Survival and Safe Motherhood (CSSM) Program.
[98] See Appendix II; see also Kranti S. Vora et al., "Maternal Health Situation in India: A Case Study," pp. 189-90.
[99] Bulletin on Rural Statistics in India, 2008, p. 25, Table 12.
[100] DLHS-3, Factsheet, Uttar Pradesh, 2007-2008. See also Kaveri Gill, "A Primary Evaluation of Service Delivery under the National Rural Health Mission (NRHM): Findings from a Study in Andhra Pradesh, Uttar Pradesh, Bihar, and Rajasthan," Working Paper 1/2009 – PEO, Planning Commission of India, May 2009, http://www.planningcommission.nic.in/reports/wrkpapers/wrkp_1_09.pdf (accessed May 15, 2009), p.29: Only 0.6 percent of all community health centers in Uttar Pradesh have anesthetists employed on a regular basis, while only 0.8 percent of such centers have gynecologists.
[101] Third Joint Review Mission, 2007, Appendix 3, RCH process indicators, row 11.
[102] Second Common Review Mission, 2008, unpaginated.
[103] Human Rights Watch interview with officer-3 (name withheld), official from the Uttar Pradesh State Project Management Unit of the NRHM, Lucknow, March 13, 2009.
[104] Human Rights Watch interview with Activist-1 (name and details withheld), Lucknow, February 23, 2009; group interview with Suraj S. (pseudonym) and others, relatives of deceased mother, village RB-2 (name withheld),Rae Bareilly district,February 27, 2009; ambulance driver (who chose to remain anonymous), Unnao district, March 2, 2009; basic health worker (name withheld), community health center-2,March 3, 2009; health staff at government district hospital (name withheld), Unnao district, March 4, 2009; group interview with health staff (who chose to remain anonymous), district women's hospital, Chitrakoot district,March 7, 2009.
[105] Human Rights Watch interview with Anagha A. (psedudonym), health staff, Unnao district women's hospital, March 4, 2009.
[106] Human Rights Watch group interview with health staff (who chose to remain anonymous), district women's hospital, Chitrakoot district,March 7, 2009.
[107] Ibid.
[108] Ibid.
[109] Ibid.
[110] Human Rights Watch interview with a district-level health official (name and designation withheld), Chitrakoot district, March 7, 2009.
[111] Human Rights Watch group interview with the mother-in law (who chose to remain anonymous) and others related to Munira M. (pseudonym), family of deceased pregnant woman, Chitrakoot district, March 8, 2009.
[112] Human Rights Watch interview with Manasa M. (pseudonym), ANM, Barabanki district, June 2, 2009.
[113] Kranti S. Vora et al., "Maternal Health Situation in India: A Case Study," p. 195.
[114] Human Rights Watch interview with Janki J. (pseudonym), pregnant patient at a district women's hospital, location and date withheld.
[115] NRHM Framework for Implementation, p. 121-22. Free referral services include "appropriate and prompt referral for cases needing specialist care … management of pregnancy induced hypertension including referral … pre-referral management (obstetric first aid) in obstetric emergencies that need expert assistance" at the primary health center level. Many community health centers are required to be upgraded as first referral units equipped with emergency obstetric care, in effect being the last stop for a woman seeking emergency care. Alternatively, district women's hospitals, a tier above community health centers, are supposed to be equipped with comprehensive emergency obstetric facilities. Theoretically therefore, no woman should be referred out of a district hospital to another facility for emergency obstetric care.
[116] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 85.
[117] Human Rights Watch interview with activists, women, and health workers, Rae Bareilly, Unnao, Lucknow, Chitrakoot, and Barabanki districts, February, March, and June 2009.
[118] Human Rights Watch interviews with Kranti K. (pseudonym), ASHA, Barabanki district, June 2, 2009.
[119] Human Rights Watch group interview with Revati R. (pseudonym) and others, relatives and neighbors of deceased mother, village RB-1 (name withheld), Rae Bareilly district,February 26, 2009.
[120] Ibid.
[121] Human Rights Watch interview with Reena R. (pseudonym), ASHA, Rae Bareilly district, February 27, 2009.
[122] Human Rights Watch interviews with health staff from community health centers and district hospitals, Rae Bareilly, Unnao, Chitrakoot, Lucknow, and Barabanki districts, February, March, and June 2009.
[123] Human Rights Watch interview with Nirmala N. (pseudonym), health staff, community health center, Rae Bareilly district, February 27, 2009.
[124] Ibid.
[125] Human Rights Watch group interview with Sita S., Anjana A. (pseudonyms), and another (who chose to remain anonymous), village RB-6 (name withheld), Rae Bareilly district, February 27, 2009.
[126] Ibid.
[127] Human Rights Watch group interview with Suraj S. (pseudonym) and others, relatives of deceased mother, village RB-2 (name withheld), Rae Bareilly district,February 27, 2009.
[128] Human Rights Watch group interview with Warisha W. (pseudonym) and others, village-B1 (name withheld), Barabanki district, June 2, 2009.
[129] Ibid.
[130] The Innovations in Family Planning Services (IFPS) II Technical Assistance Project (ITAP), "Rapid Assessment of the Functionality of FRUs and 24x7 PHCs in Uttar Pradesh, Volume 1: Summary and Recommendations, Methodology, Key Findings," May 2008, p. 38.
[131] Human Rights Watch interviews with district health officials of Rae Bareilly district and Unnao district, March 2009.
[132] Human Rights Watch interview with ambulance driver (who chose to remain anonymous), Unnao district,March 2, 2009.
[133] See above, section titled "Delivery of Basic and Comprehensive Emergency Obstetric Services," for NRHM service guarantees. State governments are also encouraged to organize Village Health and Nutrition Days at least once every month in the village anganwadi. The Village Health and Nutrition Day is supposed to facilitate pregnancy-related counseling, antenatal and postnatal care in accordance with guidelines issued by the Indian central government. See Ministry of Health and Family Welfare, "Village Health Nutrition Days, Guidelines for AWWs, ASHAs, ANMs, PRIs," February 2007, http://www.mohfw.nic.in/NRHM/Documents/VHND_Guidelines.pdf (accessed September 15, 2009).
[134] Human Rights Watch interviews with 31 villagers, including pregnant women and women who had recently delivered, in Rae Bareilly, Unnao, and Chitrakoot districts, February 26 to March 9, 2009. Even where women were issued the Mother and Child card and were able to show it to Human Rights Watch, they were not aware of what the card said or what they were entitled to. No one reported being informed about a pre-identified location for delivery. Most women had no information about a Village Health and Nutrition Day, which is supposed to be organized once every month.
[135] DLHS-3, District Fact Sheets for 70 districts of Uttar Pradesh, 2007-2008. A compilation of all district-wise data on percentages of women receiving complete antenatal care, institutional deliveries, assisted home deliveries, and postnatal care shows that antenatal and postnatal coverage are poor. The Village Health and Nutrition Days are also not being organized in many villages across Uttar Pradesh. See NRHM Health Management Information System Portal, "NRHM High-Focus Non NE," 2009-2010, http://nrhm-mis.nic.in/PublicPeriodicNRHMReports.aspx (accessed September 15, 2009). In 2008-2009 only 197,128 Village Health and Nutrition Days were held in villages of Uttar Pradesh compared with 840,000 for 2007-2008. There are 107,452 villages in Uttar Pradesh.
For all-India data see NFHS-3 2005-2006, p. 204. Only 26.6 percent of women reported three or more ANC visits; 14.2 percent received information about pregnancy complications; 8.8 percent of women took IFA for at least 90 days; 2.1 percent of women took an intestinal parasite drug.
[136] Human Rights Watch interviews with 18 individuals including gynecologists, staff nurses at community health centers, activists, and district level health officials from Barabanki, Unnao, Chitrakoot, Rae Bareilly, and Lucknow districts, February-June 2009. See also secondary data from NFHS-3 2005-2006, p. 313, which gives overall information about anemia rates in Uttar Pradesh. Roughly 50 percent of the women in Uttar Pradesh were found to be anemic.
[137] Ibid.
[138] Human Rights Watch interview with a gynecologist (who chose to remain anonymous), district women's hospital, Unnao district, March 4, 2009.
[139] Human Rights Watch interview with Latha L. (pseudonym), staff nurse, community health center, location withheld, March 15, 2009.
[140] Human Rights Watch interview with Kamini K., health staff, community health center-2, Unnao district, March 3, 2009.
[141] UNICEF, MAPEDIR, p. 9. See below, section titled "Lack of Continuous Care through the Antenatal and Postnatal Periods." See also UNICEF et al., Guidelines for Monitoring the Availability and Use of Obstetric Services (2nd edn., New York: UNICEF, 1997), p.20, figure 13. The estimated average interval from onset to death for major obstetric complications are as follows: Post-partum hemorrhage (2 hours), antepartum hemorrhage (12 hours), ruptured uterus (1 day), eclampsia (2 days), obstructed labor (3 days), infection (6 days).
[142] NRHM Framework for Implementation, p. 122-23.
[143] See DLHS-3, district level factsheets for 70 districts in Uttar Pradesh, 2007-2008. The survey shows that postnatal care is poor across Uttar Pradesh. Bahraich district, for instance, with the lowest number of facility-based deliveries at 7 percent reported even lower levels of postnatal care within 48 hours of delivery, at 5.8 percent. Likewise, Jyotiba Phule Nagar district with the highest facility-based deliveries at roughly 58 percent witnessed a significant drop in postnatal care, reporting only 25 percent postnatal care within 48 hours of delivery. For all-India data see NFHS-3 2005-2006, p. 216. Fifty-eight percent of women reported that they did not receive any postnatal care after their most recent delivery. Only 27 percent of women reported receiving care in the first two days after delivery.
[144] Human Rights Watch group interviews with Revati R. (pseudonym) and others, relatives and neighbors of deceased mother, village RB-1 (name withheld), Rae Bareilly district,February 26, 2009; Niharika N. (pseudonym) and others, relatives of deceased mother, village U-1 (name withheld), Unnao district, March 2, 2009; Chunni and others, Chitrakoot district, March 6, 2009; Rupali R. (pseudonym), woman with one-month old baby and Radha R. (pseudonym), anganwadi worker, village C-2 (name withheld), Chitrakoot district, March 7, 2009; Trishna T. (pseudonym) and others, women who had recently delivered, village C-1 (name withheld), Chitrakoot district, March 7, 2009.
[145] Human Rights Watch interview with Rohini R. (pseudonym), mother of newborn baby, village-B1, Barabanki district, June 2, 2009.
[146] Human Rights Watch interview with Shanta S. (pseudonym), relative of woman who had recently delivered, village RB-6 (name withheld), Rae Bareilly district, February 26, 2009.
[147] Human Rights Watch group interview with Revati R. (pseudonym) and others; Suraj S. (pseudonym) and others; Niharika N. (pseudonym) and others; Vikram V. (pseudonym), brother of deceased pregnant woman, village C-1, Chitrakoot district, March 8, 2009.
[148] Human Rights Watch phone discussions and interviews with activists and doctors from November 2008–March 2009. The reasons in Uttar Pradesh include appointment of auxiliary nurse-midwives according to population figures as per the 1990 census as opposed to the 2001 census, poor infrastructure support and training, a lack of transport for mobility of ANMs, and poor human resource policies.
[149] For additional information on the impact of polio eradication and sterilization on other health care needs, see above chapter titled "Maternal Mortality and Morbidity in India."
[150] See, NRHM Framework for Implementation, p. 24; pp. 120-22. The NRHM concrete service guarantees states that women above the poverty line have to bear 50 percent of the cost for in-patient services. It is the duty of the state government to conduct surveys identifying and certifying families as below the poverty line. But this is subject to a quota for number of people who can be certified as below the poverty line, which is fixed by the central government.
[151] Under the JSY, cash assistance for deliveries at home is limited to women below the poverty line. Similarly, JSY cash assistance in the so-called "high performing states" is for women above the poverty line.
[152] Human Rights Watch interviews with activists from local nongovernmental organizations, Uttar Pradesh, August 2009, who stated that they had submitted lists to district level authorities of people who were in fact below the poverty line but had not received BPL cards. Human Rights Watch phone discussions with public health and women's rights activists from India, November 2008 to February 2009; Human Rights Watch email communications from activists in Gujarat, Maharashtra, Chandigarh, Rajasthan, Kerala, and Uttarakhand, August 2009 (on file). See also, Belaku Trust, "Quality of care in rural Karnataka: Women's experiences of institutional deliveries," April 2009, http://www.sahayogindia.org/media/Inst%20Del%20Belaku%20presentation.pdf (accessed August 29, 2009), p. 11;
[153] Human Rights Watch interview with Pooja P. (pseudonym), ASHA, community health center, district name withheld, March 3, 2009.
[154] Human Rights Watch interviews and group interviews with women and ASHAs, Rae Bareilly, Chitrakoot, and Unnao districts, February and March 2009. Families reported spending amounts ranging from 200 rupees (US$5) to 25,000 rupees (US$520). Similar reports have been documented by nongovernmental organizations in other parts of India. See for example, Belaku Trust, Quality of care in rural Karnataka; EKJUT, "Institutional Delivery Study in West Singhbhum district, Jharkhand," 2009, http://www.sahayogindia.org/media/I%20D%20study%20Ekjut.pdf (accessed August 29, 2009), p. 14; Dr. Sebanti Ghosh, "Glimpses of Institutional Maternal Care, West Bengal," 2009, http://www.sahayogindia.org/media/ID%20Study%20West%20Bengal%20report.pdf (accessed August 29, 2009).
[155] Human Rights Watch group interview with Trishna T. (pseudonym) and others, women who had recently delivered, village C-1 (name withheld), Chitrakoot district, March 7, 2009.
[156] Human Rights Watch interview with Niraja N. (pseudonym), ASHA, village RB-5 (name withheld), Rae Bareilly district , February 26, 2009; interviews with about 45 health workers, women from villages, and activists, Rae Bareilly, Unnao, Chitrakoot, and Barabanki districts, February, March and June 2009. Many health workers and women complained that they were either asked for money or contributions in kind.
[157] Human Rights Watch group interview with activists from a local non-governmental organization, location withheld, March 2, 2009.
[158] Human Rights Watch interview with Pooja P. (pseudonym), ASHA, March 3, 2009.
[159] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, pp. 28-9: "Identifying who has the power to change health is a key step in formulating strategies … At the country level, national priorities obviously matter greatly. But priority must also be given to critical decision-making that happens at the district level, where integrated primary health systems are needed to effectively deliver child, maternal, and reproductive health interventions … Invoking notions of "participation" and "accountability" is almost de rigueur in the health literature. A rights-based approach should go beyond the formal mechanisms through which such notions are implemented to ask hard questions about who actually has or shares the power to effectuate change."
[160] United Nations Children's Fund (UNICEF), Tracking progress for maternal newborn and child survival (New York: UNICEF, 2008).
[161] See for example, UNICEF, Maternal and Perinatal Death Inquiry and Response,Empowering Communities to Avert Maternal Deaths in India (New Delhi: UNICEF, 2008); ARTH, "Pregnancy related deaths in southern Rajasthan, India, A community based study of care-seeking using verbal autopsy," March 2008, http://www.arth.in/publications/Pregnancy%20related%20deaths%20in%20southern%20Rajasthan.pdf (accessed December 15, 2009); Human Rights Watch interview with Aditi Iyer, Indian Institute of Management, Bangalore, January 21, 2009; Human Rights Watch phone discussion with Dr. Prakasamma, Academy of Nursing Sciences, January 13, 2009.
[162] NRHM Framework for Implementation, p. 102.
[163] Human Rights Watch phone interview and email communication with Dr. Jorge Caravotta, UNICEF, August 20, 2009.
[164] See UNICEF, Maternal and Perinatal Death Inquiry and Response.
[165] UN Special Rapporteur on health, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Preliminary note on the mission to India, Addendum, A/HRC/7/11/Add.4, February 29, 2008, www2.essex.ac.uk/human_rights_centre/rth/docs/preliminary%20note%20india.doc (accessed on May 17, 2009), paras. 16 and 17.
[166]Uttar Pradesh Shasan, Chikitsa Anubhag 9, Sankhya: 858/5-9-2004-9(15)/2004, Lucknow, Dinank – 12 March 2004, Matrutva Swasthya Par Shaasanaadesh, March 2004. (Uttar Pradesh Government, Medical Section 9, Number: 858/5-9-2004-9 (15)/2004, Lucknow, March 12, 2004, Government Order on Maternal Health, March 2004.
[167] Maternal Death Notification and Review System, Final Report submitted to the Uttar Pradesh Health Systems Development Project, January 2008.
[168] Human Rights Watch interview with Dr. Gaurav Arya, UNICEF, March 14, 2009.
[169] Human Rights Watch interview with L. B. Prasad, former Director General of Health and Family Welfare, Lucknow, March 16, 2009.
[170] Human Rights Watch interviews with L. B. Prasad, former Director General of Health and Family Welfare, Lucknow, March 16, 2009; Officer-1 (who requested anonymity), official involved with the World Bank funded Uttar Pradesh Health Systems Development Project (UPHSDP), Lucknow, February 25, 2009; Jashodhara Dasgupta, Coordinator of SAHAYOG, Lucknow, December 12, 2008.
[171] United States Agency for International Development (USAID)-India, "Report on maternal death audits in Uttar Pradesh," August 2006, as cited in Maternal Death Notification and Review System, Final Report submitted to the Uttar Pradesh Health Systems Development Project, January 2008, p. 15.
[172] This is a World Bank funded project. Human Rights Watch interview with officer-1, February 25, 2009.
[173] Maternal Death Notification and Review System, January 2008, pp. 30
[174] Human Rights Watch group interview with activists from a local non-governmental organization, location withheld, March 2009.
[175] Ibid.
[176] Human Rights Watch group interview with chief medical officer and deputy chief medical officer, district name and details withheld.
[177] Human Rights Watch interview with district medical officers, March 2009 (all other details withheld).
[178] Human Rights Watch group interview with Dr. Adi Ram and Dr. Ram Bahadur Patel, Additional Chief Medical Officers, Chitrakoot district, March 7, 2009.
[179] Human Rights Watch interviews with Dr. Manju Singh, Superintendent of Manekpur community health center, March 7, 2009; Vikram V. (pseudonym), brother of deceased pregnant woman, village C-1, Chitrakoot district, March 8, 2009.
[180] Human Rights Watch interview with Dr. G.S. Bajpai, district surveillance officer, Rae Bareilly, March 9, 2009.
[181] Ibid.
[182] NRHM Framework for Implementation, pp. 124 and 127.
[183] Human Rights Watch interview with Sheela Rani Chunkath, former health secretary of Tamil Nadu, Chennai, April 3, 2009.
[184] Human Rights Watch interviews with Dr. Neelam Singh, Vatsalya, Lucknow, March 14, 2009; officer-1 (who requested anonymity), official involved with the World Bank funded Uttar Pradesh Health Systems Development Project (UPHSDP), Lucknow, February 25, 2009; L. B. Prasad, former Director General of Health and Family Welfare, Lucknow, March 16, 2009.
[185] Maternal Death Notification and Review System, p. 25.
[186] Ibid., p. 28. According to the study, this poor priority manifested itself in different ways-poor participation of block officials during training and feedback sessions on maternal death notification, using these training sessions for discussions on polio eradication/immunization.
[187] Human Rights Watch interview with Dr. Neelam Singh, Vatsalya, Lucknow, March 14, 2009.
[188] Human Rights Watch interview with Dr. Vishwajeet Kumar, public health expert in infant and maternal mortality, Lucknow, March 15, 2009; Human Rights Watch interview with Dr. L. B. Prasad, former Director General of Health and Family Welfare, Lucknow, March 16, 2009.
[189] Human Rights Watch group interview with senior health officials from the Directorate of Family Welfare (names withheld), Lucknow, March 12, 2009.
[190] Human Rights Watch interview with officer-2 (who requested anonymity), senior official from the Directorate of Family Welfare, Government of Uttar Pradesh, Lucknow, March 12, 2009. The National Child Survival and Safe Motherhood Programme Monthly Report, included under part D titled Surveillance, a column for number of maternal deaths in the district. The new reporting forms titled "Universal Immunization Programme: Monthly District Performance Report," largely reproduces the CSSM forms including data on number of pregnant women registered, number of institutional and domiciliary deliveries, and a section titled "Surveillance." However, it does not contain a column to enter number of maternal deaths.
[191] Human Rights Watch group interview with district health officials (names and details withheld).
[192] Ibid.
[193] Human Rights Watch interviews with ASHAs and ANMs, Rae Bareilly and Barabanki districts, February and June 2009. They stated that the data collected by them was sent to their supervisors, which was complied and forwarded to the district health officials.
[194] Human Rights Watch interview with Pooja P. (pseudonym), ASHA, community health center, district name withheld, March 3, 2009.
[195] Human Rights Watch interview with Nirathi N. (pseudonym), ANM, village C-2 (name withheld), Chitrakoot district, March 7, 2009.
[196] Human Rights Watch interview with Latha L. (pseudonym), staff nurse, community health center, location withheld, March 15, 2009.
[197] Human Rights Watch interviews with Chief Medical Officers from different districts of Uttar Pradesh, March 4, March 7, and March 9, 2009.
[198] Rae Bareilly district was a notable exception that reported 107 maternal deaths.
[199] Human Rights Watch interview with Dr. T. Sundararaman, executive director, National Health Systems Resource Center, New Delhi, March 18, 2009.
[200] Human Rights Watch interview with Dr. Vishwajeet Kumar, public health expert on infant and maternal mortality, Lucknow, March 15, 2009.
[201] Human Rights Watch group interview with Suraj S. (pseudonym) and others, relatives of the deceased mother, village RB-2 (name withheld),Rae Bareilly district,February 27, 2009.
[202] Human Rights Watch interviews with 15 field-based health workers in different parts of Uttar Pradesh, February 26-March 17, 2009.
[203] Ibid.
[204] Human Rights Watch group interviews with Ratna R. and Kishori K. (pseudonyms), anganwadi workers, village RB-3 (name withheld); ANM Vibha V. and ASHA Anjali A. (pseudonyms), village RB-4 (name withheld); interview with Niraja N. (pseudonym), ASHA, village RB-5 (name withheld), Rae Bareilly district, February 26, 2009; interviews with Pooja P. (pseudonym), ASHA; Kanti K. (pseudonym), ASHA, village C-3, Chitrakoot, March 6, 2009; Nirathi N. (pseudonym), ANM, village C-2 (name withheld), Chitrakoot district, March 7, 2009.
[205] See World Health Organization, International Classification of Diseases and Related Health Problems, Tenth Revision, 1992 (ICD-10),
[206] UNICEF, MAPEDIR, p. 9.
[207] Human Rights Watch group interviews with Ratna R. and Kishori K. (pseudonyms), anganwadi workers, village RB-3 (name withheld); ANM Vibha V. and ASHA Anjali A. (pseudonyms), village RB-4 (name withheld); interview with Niraja N. (pseudonym), ASHA, village RB-5 (name withheld), Rae Bareilly district, February 26, 2009; interviews with Pooja P. (pseudonym), ASHA; Kanti K. (pseudonym), ASHA; Nirathi N. (pseudonym), ANM, March 7, 2009.
[208] Human Rights Watch group interview with Ratna R. and Kishori K (pseudonyms), anganwadi workers, February 26, 2009.
[209] Human Rights Watch group interview with ANM Vibha V. and ASHA Anjali A. (pseudonyms), February 26, 2009.
[210] Ibid.
[211] Human Rights Watch interviews with officer-1 (who requested anonymity), official involved with the World Bank funded Uttar Pradesh Health Systems Development Project (UPHSDP), Lucknow, February 25, 2009; medical officer in charge of CHC (name withheld), Unnao district, March 3, 2009; Dr. G. Kumariya, chief medical officer, Rae Bareilly district, March 9, 2009; Dr. L. B. Prasad, former director general of directorates of health and family welfare, Lucknow, March 16, 2009.
[212] Human Rights Watch interview with officer-1, February 25, 2009.
[213] Human Rights Watch interview with officer-4 (who requested anonymity), former senior official from the state health department, Lucknow, March 16, 2009, telephone conversation, April 17, 2009.; Dr. G. Kumariya, chief medical officer, Rae Bareilly district, March 9, 2009. Dr. Kumariya said that only after he took office in May 2008 was the ANM training center in his district re-started.
[214] Ministry of Health and Family Welfare et al., Joint Review Mission-RCH-2, Uttar Pradesh, Report of the Visit, January 16-20, 2007, http://mohfw.nic.in/NRHM/RCH/JRM.htm (accessed May 12, 2009).
[215] Human Rights Watch interview with official-4 (who requested anonymity), former senior official from the health department, March 16, 2009, telephone conversation, April 17, 2009.
[216] Human Rights Watch does not have full information about the content of these training programs and whether these programs addressed the importance of monitoring, particularly data collection.
[217] Human Rights Watch interview with Niraja N. (pseudonym), ASHA, village RB-5 (name withheld), Rae Bareilly district , February 26, 2009.
[218] See above, section titled "Gaps in Continuity of Care."
[219] Human Rights Watch group interview with Suresh S. and Meena M. (pseudonyms), neighbor and mother-in-law of the pregnant woman who died, village U-2, Unnao district, March 2, 2009.
[220] Human Rights Watch group interview with the mother-in law (who chose to remain anonymous) and others related to Munira M. (pseudonym), family of deceased pregnant woman, Chitrakoot district, March 8, 2009.
[221] Human Rights Watch group interview with Additional Chief Medical Officers Dr. Adi Ram and Dr. Ram Bahadur Patel and others, Chitrakoot district, March 7, 2009. Human Rights Watch was not able to independently verify whether these deaths were reported in the registers of field-based health workers and failed to make their way into the records of the district health authorities or whether the death was unreported in the primary register itself.
[222] Human Rights Watch group interview with Revati R. (pseudonym) and others, relatives and neighbors of deceased mother, village RB-1 (name withheld), Rae Bareilly district,February 26, 2009; Suraj S. (pseudonym) and others; Niharika N. (pseudonym) and others, relatives of the deceased mother, village U-1 (name withheld), Unnao district, March 2, 2009; Vikram V. (pseudonym), brother of deceased pregnant woman, village C-1 (name withheld), Chitrakoot district, March 8, 2009.
[223] Human Rights Watch interviews with families of deceased pregnant women, Unnao, Chitrakoot, and Rae Bareilly districts, February and March 2009.This is based on information given to Human Rights Watch by the relevant district health officials. Human Rights Watch could not access the primary records maintained by health workers to determine whether the death went completely unrecorded or got lost in transmission from the village-level records to the district authorities.
[224] The district medical officer of Rae Bareilly district stated that there had been 107 deaths in the district since April 2008 to January 2009. Human Rights Watch did not have access to the details of the 107 deaths and hence is not in a position to say whether the maternal deaths documented by Human Rights Watch in Rae Bareilly were part of the 107 documented deaths or not.
[225] NFHS-3 2005-2006, p. 209.
[226] Human Rights Watch interviews with ASHAs and ANMs, Rae Bareilly, Unnao, and Chitrakoot districts, February and March 2009.
[227] Human Rights Watch group interview with Ratna R. and Kishori K. (pseudonyms), anganwadi workers, village RB-3 (name withheld), Rae Bareilly district, February 26, 2009; interview with Pooja P. (pseudonym), ASHA, March 3, 2009.
[228] Human Rights Watch interview with Pooja P. (pseudonym), ASHA, March 3, 2009.
[229] Human Rights Watch group interview with Dr. Ramesh Sahani and Dr. Nimmi Suri, chief medical officer and deputy chief medical officer, Unnao district, March 4, 2009.
[230] Human Rights Watch group interview with Ratna R. and Kishori K. (pseudonyms), February 26, 2009.
[231] Human Rights Watch interviews with Officer-1 (who requested anonymity), official involved with the World Bank funded Uttar Pradesh Health Systems Development Project (UPHSDP), Lucknow, February 25, 2009; Dr. Sinha and Dr. V. K. Shrivastava, chief medical officer and additional chief medical officer, Allahabad, March 5, 2009; Dr. G.S. Bajpai, district surveillance officer, Rae Bareilly, March 9, 2009; telephone interview with Dr. Narendra Malhotra, immediate past president of the Federation of Obstetric and Gynecological Societies of India, Lucknow, March 12, 2009.
[232] Human Rights Watch interviews with Officer-1 (who requested anonymity), official involved with the World Bank funded Uttar Pradesh Health Systems Development Project (UPHSDP), Lucknow, February 25, 2009; group interview with Dr. Sinha and Dr. V. K. Shrivastava, chief medical officer and additional chief medical officer, Allahabad, March 5, 2009.; Dr. G.S. Bajpai, district surveillance officer, Rae Bareilly, March 9, 2009; Jashodhara Dasgupta, coordinator, SAHAYOG, Lucknow, December 12, 2008.
[233] Human Rights Watch group interview with Dr. Sinha and Dr. V. K. Shrivastava, chief medical officer and additional chief medical officer, Allahabad, March 5, 2009.
[234] Human Rights Watch interview with Dr. G.S. Bajpai, district surveillance officer, Rae Bareilly, March 9, 2009
[235] Human Rights Watch telephone interview with Dr. Narendra Malhotra, immediate past president of the Federation of Obstetric and Gynecological Societies of India, Lucknow, March 12, 2009.
[236] Human Rights Watch interview with Sheela Rani Chunkath, former health secretary of Tamil Nadu, Chennai, April 3, 2009.
[237] Human Rights Watch interview with Dr. Padmanabhan, Advisor on NRHM, National Health Systems Resource Center, New Delhi, March 19, 2009.
[238] Human Rights Watch documented only one instance where an inquiry into a maternal death was held and health staff were suspended.
[239] Human Rights Watch group interview with Dr. Ramesh Sahani and Dr. Nimmi Suri, chief medical officer and deputy chief medical officer, Unnao district, March 4, 2009. According to the official version of the facts, the nurse-midwife who admitted the pregnant woman left her unattended and went on field duty. The doctor who was on duty also failed to notice her. She delivered unattended that resulted in a still birth. Subsequently, the mother also died of post partum hemorrhage.
[240] Human Rights Watch interview with Latha L. (pseudonym), staff nurse, community health center, location withheld, March 15, 2009.
[241] Human Rights Watch telephone interview with Dr. Narendra Malhotra, immediate past president of the Federation of Obstetric and Gynecological Societies of India, Lucknow, March 12, 2009; Dr. Chandravati, former professor of gynecology, KGMU and advisor to the Uttar Pradesh health department, Lucknow, March 16, 2009.
[242] Human Rights Watch interview with Dr. Rastogi, director of medical and director of community health centers and primary health centers, Lucknow, March 12, 2009. See D. K. Joshi v. State of Uttar Pradesh, (2000) 5 SCC 80. The Indian Supreme Court has directed all district magistrates and chief medical officers of Uttar Pradesh to identify within a specified time all unqualified and unregistered medical practitioners and initiate legal action against those persons immediately. Further, the court has directed the secretary of the Department of Health and Family Welfare to issue guidelines from time to time specifying the nature of information that should be provided to district health authorities. See also Charan Singh v. State of Uttar Pradesh, AIR 2004 All 373. Similar orders were issued by the Uttar Pradesh High Court.
[243] Human Rights Watch group interviews with district health officials from Allahabad, Unnao, Rae Bareilly, and Chitrakoot, February and March 2009.
[244] Human Rights Watch group interview with Dr. Ramesh Sahani and Dr. Nimmi Suri, chief medical officer and deputy chief medical officer, Unnao district, March 4, 2009.
[245] Human Rights Watch interview with NRHM District Program Manager (who requested anonymity), location withheld, March 4, 2009.
[246] Human Rights Watch group interview with doctors from private health facilities in Unnao and Rae Bareilly districts (names of doctors and hospitals withheld), February 28 and March 4, 2009.
[247] Human Rights Watch phone discussions with public health experts and women's rights activists, November 2008 to February 2009.
[248] Ibid.
[249] Registrar General of India, Maternal Mortality in India: 1997-2003, p. 23. According to this study, 10 percent of all maternal deaths are due to abortions in Empowered Action Group states such as Uttar Pradesh. The confidence interval for this estimate is 7-12 percent.
[250] Human Rights Watch phone discussions with public health experts and women's rights activists, November 2008 to February 2009. The implementation of the Medical Termination of Pregnancies Act,1971is beyond the scope of this report.
[251] NFHS-3 2005-2006. See data reproduced in Appendix III. See also, UNICEF, Maternal and Perinatal Death Inquiry and Response, p. 37. See also "Incidents of maternal death and ill-health in nine districts of UP, As presented at Lucknow (UP) on 28 May 2009 by Mahila Swasthya Adhikar Manch (Women's Health Rights Forum) and Healthwatch Forum UP, Case Summaries," http://www.sahayogindia.org/media/Case%20Summaries.pdf (accessed June 12, 2009). Further, four landmark legal cases pending before the Uttar Pradesh High Court pertain to cases of pregnant women from lower castes, particularly Dalits, who were denied timely medical attention. See People's Union of Civil Liberties, District Unit, Banda district v. State of Uttar Pradesh and others, Public Interest Litigation No. 6464 of 2006, para. 7 of the petition. According to the petition, Sushila Devi is a Dalit; Stree Adhikar Sangathan v. Union of India and others, Civil Miscellaneous Writ Petition (PIL) No. 5144 of 2009, Annexure No. 2, p. 28. According to the petition, Geeta Devi, the pregnant woman who was denied care in a government hospital, belonged to the Gaderiya community which is considered a Dalit community; Stree Adhikar Sangathan v.Union of India and others, Civil Miscellaneous Writ Petition (PIL) No. 6723 of 2009, Annexure 2, p. 30. According to the petition, Anita Devi belonged to "samaj ke subse pichchde varg." The lawyer appearing in these petitions, advocate K. K. Roy clarified that Anita Devi belonged to "one of the most backward classes from the OBC category." Human Rights Watch interviews and phone discussion with K. K. Roy, Allahabad, March 5 and June 24, 2009.
[252] Human Rights Watch group interview with six women from the kol community, village C-4 (name withheld),Chitrakoot district, March 6, 2009.
[253] Ibid.
[254] Ibid.
[255] Human Rights Watch interview with Rathrani, activist from Vanangana, March 6, 2009.
[256] Human Rights Watch interview with Mohini M. (pseudonym), ASHA, village C-3, Chitrakoot, March 6, 2009.
[257] Human Rights Watch interview with Rajdaiyya, President of the Dalit Mahila Samiti (Dalit Women's Society), March 7, 2009.
[258] Ibid.
[259] See the Constitution (Scheduled Castes) Order, 1950, http://lawmin.nic.in/ld/subord/rule3a.htm (accessed June 23, 2009), part XVIII, item 49. Kol is listed as a scheduled caste in Uttar Pradesh.
[260]Human Rights Watch group interview with Trishna T. (pseudonym) and others, women who had recently delivered, village C-1 (name withheld), Chitrakoot district, March 7, 2009.
[261] Ibid.
[262] See the Constitution (Scheduled Castes) Order, 1950, http://lawmin.nic.in/ld/subord/rule3a.htm (accessed June 23, 2009), part XVIII, item 24. Chamar is listed as a scheduled caste in Uttar Pradesh.
[263] Human Rights Watch discussions with Dr. Rakhal Gaitonde and Dr. Subha Sri, health and human rights activists, April 4, 2009; interviews with Dr. Kolanda Swamy, former deputy director of health services, Dr. Chari, director of state reproductive and child health program, Poonamalee, April 2, 2009; Dr. P. Padmanaban, former director of health services of Tamil Nadu and Indian government advisor on public health administration, National Health Systems Resource Center of NRHM, New Delhi and Poonamalee, March 19 and April 2, 2009.
[264] Human Rights Watch interview with Dr. P. Padmanaban, March 19 and April 2, 2009.
[265] A critical evaluation of the Tamil Nadu system is beyond the scope of this report. Dr. Gaitonde told Human Rights Watch on April 4, 2009, that several concerns had been expressed about the process, the biggest being that it was conducted entirely by the government and decisions were not made public, making it difficult to discern who was and was not punished. A lack of transparency around the process was said to be a considerable drawback of the Tamil Nadu system.
[266] Human Rights Watch interviews with Dr. P. Padmanaban, March 19 and April 2, 2009. He explained that initially Tamil Nadu introduced a system of facility-based death reviews which has now been changed.
[267] Human Rights Watch interview with a senior state government official overseeing maternal health issues (who requested anonymity), Chennai, April 3, 2009;
[268] Human Rights Watch interview with Sheela Rani Chunkath, formerly secretary of health for the Tamil Nadu government, Chennai, April 3, 2009.
[269] Human Rights Watch interviews with Sheela Rani Chunkath, April 3, 2009, and Dr. P. Padmanaban, March 19 and April 2, 2009.
[270] Human Rights Watch interviews with Dr. P. Padmanaban, March 19, 2009, and Sheela Rani, April 3, 2009.
[271] Human Rights Watch interview with Alphonse Mary, MCH officer, Dharmapuri district, April 7, 2009.
[272] Ibid.
[273] Human Rights Watch interviews with Sheela Rani Chunkath, Dr. P. Padmanaban, Dr. Chari, Kolanda Swamy, April 2009.
[274] Ibid.
[275] Human Rights Watch interview with Kolanda Swamy, deputy director of health services on sabbatical, Poonamalee, April 2, 2009.
[276] Human Rights Watch group interview with Dr. Iyyannar, deputy director of health services, Dharmapuri district, April 7, 2009.
[277] Human Rights Watch interview with Dr. Kolanda Swamy, April 2, 2009.
[278] Human Rights Watch interviews with Dr. Iyyannar and Alphonse Mary, April 7, 2009.
[279] Human Rights Watch group discussion with Dr. Rakhal Gaitonde, community health researcher and Dr. Subha Sri, obstetrician working in rural areas, Tirukalukundram, April 4, 2009.
[280] Human Rights Watch interview and phone discussion with Dr. Kolanda Swamy, April 2 and June 24, 2009.
[281] Ibid.
[282] Ibid. A critical evaluation of the control room feature of the Tamil Nadu government is beyond the scope of this report.
[283] Ibid.
[284] Ibid.
[285] Human Rights Watch interviews with Dr. Iyyannar and Alphonse Mary, April 7, 2009.
[286] "Ensuring Safe Motherhood for JSY," Government of India press release, RTS/VN, December 30, 2008, http://pib.nic.in/release/rel_print_page.asp?relid=46232 (accessed June 29, 2009); Human Rights Watch phone discussions and interviews with public health experts and women's health activists in India, November 2008 to February 2009.
[287] Human Rights Watch phone discussion and email communication with Dr. Abhijit Das, August 22, 2009.
[288] See SAHAYOG and Center for Legislative Research and Advocacy, "Maternal Death and Disability in India, Welcome Kit for Parliamentarians," 2009, http://www.sahayogindia.org/media/Welcome%20Kit%20Final.pdf (accessed August 6, 2009), p. 7. Some conditions for a safe delivery within the Indian health system have been outlined as follows: Subcenter with additional ANM, ANM living in subcenter, primary health centers function around the clock, primary health centers have around-the-clock facilities, new born care, and referral facilities and have conducted at least 10 deliveries per month. Similarly, the conditions for comprehensive emergency obstetric facilities have been identified as CHCs having obstetrician/gynecologist, having a functional operation theater, offering cesarean section, around-the-clock new born care, and blood storage facilities.
[289] Directorate of Family Welfare, Janani Suraksha Yojana, Uttar Pradesh, Sameeksha Report (Maah April 2008 Se February 2009 Thak) (Mother Protection Scheme, Uttar Pradesh, Review Report (From April 2008 to February 2009). Column 3 of this report presents the lakshya or target for 2008-2009 for each district of Uttar Pradesh. Column 4 presents "laabharthi ki sankhya" or number of beneficiaries.
[290] Human Rights Watch group interviews with Dr. Ramesh Sahani and Dr. Nimmi Suri, chief medical officer and deputy chief medical officer, Unnao district, March 4, 2009.
[291] Human Rights Watch group interview with Dr. Sinha and Dr. V. K. Shrivastava, chief medical officer and additional chief medical officer, Allahabad, March 5, 2009.
[292] See Directorate of Family Welfare, Janani Suraksha Yojana, Uttar Pradesh, Sameeksha Report (Maah April 2008 Se February 2009 Thak) (Mother Protection Scheme, Uttar Pradesh, Review Report (From April 2008 to February 2009). Column 3 of this report presents the lakshya or target for 2008-2009 for each district of Uttar Pradesh. Column 4 presents "laabharthi ki sankhya" or number of beneficiaries. Column 5 presents "laabharthi ka prathishat (kaalam 3 ke sapeksh)."
[293] Human Rights Watch phone discussions with Dr. Abhijit Das and Jashodhara Dasgupta, December 2008-August 2009.
[294] Human Rights Watch interviews with women in Rae Bareilly and Chitrakoot districts, February and March 2009 respectively. This was also mentioned by several women during Human Rights Watch preliminary field investigations in Hardoi district in December 2008.
[295] "Incidents of maternal death and ill-health in nine districts of UP, As presented at Lucknow (UP) on 28 May 2009 by Mahila Swasthya Adhikar Manch (Women's Health Rights Forum) and Healthwatch Forum UP, Case Summaries," http://www.sahayogindia.org/media/Case%20Summaries.pdf (accessed June 12, 2009).
[296] Human Rights Watch phone discussion with Jashodhara Dasgupta, coordinator, SAHAYOG, June 11, 2009.
[297] Ibid.
[298] Human Rights Watch interview with officer-2 (who requested anonymity), senior official from the Directorate of Family Welfare, Government of Uttar Pradesh, Lucknow, March 12, 2009.
[299] Human Rights Watch interviews with I.S. Shrivastava, Director General of Medical Services and Health, Government of Uttar Pradesh; Alka Shrivastav, Director (Administration), Dr. Rastogi, Director (Medical Care) and Director (Community Health Centers and Primary Health Centers); Savitri Arya, Joint Director (Nursing), Lucknow, Uttar Pradesh, March 12, 2009.
[300] Human Rights Watch interview with Dr. Rastogi, Director (Medical Care) and Director (Community Health Centers and Primary Health Centers), Lucknow, Uttar Pradesh, March 12, 2009.
[301] Human Rights Watch group interviews with Dr. Ramesh Sahani and Dr. Nimmi Suri, March 4, 2009; Dr. Sinha and Dr. V. K. Shrivastava, March 4, 2009; Dr. Adi Ram, Dr. Ram Bahadur Patel, and others, March 7, 2009.
[302] Ibid.
[303] Human Rights Watch interviews with health staff in community health centers in Lucknow, Rae Bareilly, and Unnao districts, February and March 2009.
[304] Human Rights Watch interview with L. B. Prasad, former Director General of Health and Family Welfare; officer-4 (who requested anonymity), former senior official from the state health department, Lucknow, March 16, 2009, telephone conversation, April 17, 2009; Dr. Chandravati, former professor of gynecology, KGMU and advisor to the health department, Lucknow, March 16, 2009; Dr. Gaurav Arya, UNICEF and Dr. Neelam Singh, gynecologist and activist, Vatsalya, Lucknow, March 14, 2009.
[305] Human Rights Watch interview with officer-4 (who requested anonymity), former senior official from the state health department, March 16, 2009.
[306] National Rural Health Mission Common Review Mission: Uttar Pradesh, November 2007, http://mohfw.nic.in/NRHM.htm# (accessed May 12, 2009), p. 7. For example, since 60 percent of maternal deaths are estimated to occur in the postnatal period, the 2007 government Common Review Mission's observations about "tripling of delivery cases" resulting in "women… being discharged post delivery earlier than usual… due to shortage of personnel and beds" raises concerns about the scheme's impact on maternal mortality.
[307] Human Rights Watch interview with Dr. Chandravati, March 16, 2009.
[308] Human Rights Council, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Preliminary note on the mission to India, Addendum, A/HRC/7/11/Add.4, February 29, 2008, http://daccessdds.un.org/doc/UNDOC/GEN/G08/112/70/PDF/G0811270.pdf?OpenElement (accessed June 23, 2009), para. 12. Even though the UN Special Rapporteur did not make field visits to Uttar Pradesh state, the concerns raised by him are relevant in the context of Uttar Pradesh as well.
[309]Ibid.
[310] Human Rights Watch phone discussion with Jashodhara Dasgupta, coordinator, SAHAYOG, December 12, 2008; phone discussions and interviews with public health experts and women's health activists in India, November 2008 to February 2009.
[311] For the definition of "skilled birth attendant," see Making Pregnancy Safer: The Critical Role of the Skilled Attendant," A joint statement by WHO, the International Confederation of Midwives (ICM), and the International Federation of Gynaecologists and Obstetricians (FIGO) (Geneva: WHO, 2004), http://whqlibdoc.who.int/publications/2004/9241591692.pdf (accessed June 23, 2009),p.1: "a skilled attendant is an accredited health professional-such as a midwife, doctor or nurse-who has been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth and the immediate post-partum period, and in the identification, management and referral of complications in women and newborns."
See Deborah Maine, "Detours and shortcuts on the road to maternal mortality reduction," vol. 370 The Lancet 1380 (2007), p. 1381. Maine is considered one of the pioneers of the global safe motherhood initiative. She draws a distinction between measuring institutional deliveries and measuring deliveries attended by a skilled birth attendant, and says that "in many settings" there is a "substantial overlap" between the two, there are many places where this is not the case. Further, Maine refers to a category of "semi-skilled attendants," those attendants who are working as "skilled birth attendants" but in reality do not have the requisite skills or cannot be classified as such according to WHO/ICM/FIGO definition.
[312]See Graham, Bell, and Bullough 2001, pp. 97-129 and WHO, UNICEF, UNFPA, and AMDD 2006, as cited in Countdown to 2015, Maternal, Newborn, and Child Survival, 2008 report, p. 34.
[313] Graham and Bell, Ibid. See also, definition of "skilled care."
[314] See WHO, "Making pregnancy safer: the critical role of the skilled attendant: A joint statement by WHO, ICM, and FIGO," 2004, p.1. "Skilled care refers to the care provided to a woman and her newborn during pregnancy, childbirth, and immediately after birth by an accredited and competent health care provider who has at her/his disposal the necessary equipment and the support of a functioning health system, including transport and referral facilities for emergency obstetric care."
[315] Ibid.
[316] Human Rights Watch phone discussions with public health experts and women's rights activists, November 2008 to February 2009.
[317] Human Rights Watch interview with officer-2 (who requested anonymity), senior official from the Directorate of Family Welfare, Government of Uttar Pradesh, Lucknow, March 12, 2009. See also Human Rights Watch group interview with with Dr. Sinha and Dr. V. K. Shrivastava, chief medical officer and additional chief medical officer,Allahabad, March 5, 2009; interview with officer-3 (name withheld), official from the Uttar Pradesh State Project Management Unit of the NRHM, Lucknow, March 13, 2009.Planning Commission, Eleventh Plan, p. 72. Similar reports from other states were given to Human Rights Watch by activists in Gujarat, Rajasthan, Assam, Orissa, Karnataka, and Jharkhand during phone discussions between November 2008 and June 2009.
[318] UNICEF et al., Guidelines for Monitoring the Availability and Use of Obstetric Services (2nd edn., New York: UNICEF, 1997), pp. 11-12, Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 78, Sundari Ravindran and Marge Berer, "Maternal Mortality Statistics: What's In a Number," Women's Global Network on Reproductive Health (1988).
[319] United Nations Process Indicators to Monitor the Availability, Utilization, and Quality of Emergency Obstetric Care, and the UN Guidelines, 1997. See Appendix III.
[320] Ibid., p. 22. See Appendix III.
[321] Human Rights Watch interviews with district level officials of Rae Bareilly, Unnao, and Chitrakoot districts, Human Rights Watch phone discussions with Dr. Abhijit Das, director, Center for Health and Social Justice, New Delhi, June 13, 2009. Barring some donor mid-term reviews of the government's NRHM program, the government's joint review and common review missions under NRHM do not throw light on key maternal mortality reducing processes.
[322] Human Rights Watch email communication with Dr. Geetha Rana, India technical advisor for Averting Maternal Death and Disability, August 27, 2009. Dr. Rana points out that since health is a state subject, states can take additional measures to improve reporting. Orissa, for example, is planning to introduce additional indicators for monitoring access to emergency obstetric care.
[323] Human Rights Watch interview with Dr. Geetha Rana, consultant, National Health Systems Resource Center, New Delhi, and technical advisor, Averting Maternal Deaths and Disability, March 18, 2009, email communication, August 27, 2009.
[324] Human Rights Watch interviews with Dr. T. Sundararaman, Executive Director, National Health Systems Resource Center, New Delhi, March 18, 2009.
[325] Human Rights Watch interviews with officers from the Registrar General's Office, New Delhi, March 18 and 19, 2009.
[326] Human Rights Watch filed an application under the Right to Information Act, 2005 to get additional information about the proposed Annual Health Survey. The Indian government would not provide additional information on the ground that the survey was still being finalized.
[327] See below, section titled "International Human Rights and the Indian Legal Framework."
[328] See for instance, Philip W. Setel et al., "A scandal of invisibility: making everyone count by counting everyone," vol. 370 issue 9598 The Lancet (2007), p. 1569. Experts believe that the lack of a strong civil registration system has been one of the most critical failures of development over the past 30 years, stating that the "continued cost of ignorance borne by countries without civil registration far outweighs the affordable necessity of action."
[329] Richard Horton, "Counting for health," 370 The Lancet (2007), p. 1526. See also, WHO, Maternal Mortality, Appendices 1 and 2, pp. 29-30. Appendix 1 provides a list of 59 countries with a good death registration with good attribution of cause of death and Appendix 2 provides a list of 6 countries with good death registration but uncertain cause of death attribution.
[330] Ibid.
[331] Maternal Mortality in India: 1997-2003, p. xi.
[332] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, addendum, A/HRC/7/11/Add.4, pp. 3-4.
[333] UN Task Force on Child Health and Maternal Health, p. 137
[334] Report of the UN Millennium Project Task Force on Child Health and Maternal Health, 2005, p. 70.See Miller and others, 2003 as cited in UN Millennium Project Task Force on Child Health and Maternal Health, p. 71: Adolescent child bearing also has an impact on infants and children since babies born to adolescent mothers are at increased risk of stillbirth and perinatal mortality.
[335] NFHS-3 2005-2006, p. xxxi.
[336] DLHS-3, 2007-2008, Fact Sheet for Uttar Pradesh, under the head "Indicators based on currently married women," unpaginated. 7 percent of all births were to women between ages 15 and 19; more than 50 percent of women between ages 20 and 24 reported having 2 or more children, and nearly 60 percent of them were married before age 18.
[337] Registration of Births and Deaths Act, 1969. For further details, see Appendix IV.
[338] Under the Constitution of India, Seventh Schedule, List III, entry 30, 'vital statistics' is a shared center-state subject.
[339] National Population Policy, 2000, Box 2.
[340] Central Bureau of Health Intelligence, Ministry of Health and Family Welfare, Mortality Statistics in India 2006, Status of Mortality Statistics Reporting in India, A Report, March 2007, http://www.cbhidghs.nic.in/writereaddata/mainlinkfile/File976.pdf (accessed on May 7, 2009), p. 15.
[341] Office of the Registrar General of India, "Extracts of the Proceedings of the National Conference of Chief Registrars of Births and Deaths," New Delhi, January 27-28, 2005, p. 2; May 23-24, 2006, p. 3; October 16-17, p. 14 where Uttar Pradesh is once again listed as a "low performing state."
[342] Registrar General of India, Vital Statistics of India Based on the Civil Registration System, Special Report: 1996-2001 (New Delhi: 2009), p. 5; Special Report: 2002-2005, p. 5. While the 1996-2001 special report says "complete report not available," the 2002-2005 report says "report not available."
[343] Central Bureau of Health Intelligence, Mortality Statistics in India 2006.
[344] Central Bureau of Health Intelligence, Mortality Statistics in India 2006, p. 16.
[345] National Conference of Chief Registrars, 2006, p. 3.
[346] Human Rights Watch interviews with Anjani Kumar and another, March 16, 2009.
[347] National Conference of Chief Registrars, 2005, p. 2; Human Rights Watch interviews with Anjani Kumar, March 16, 2009.
[348] Human Rights Watch interview with official at Registrar General's Office (who requested anonymity), New Delhi, March 18, 2009.
[349] See for instance Letter from Chief Registrar (Births and Deaths) to Deputy Registrar General, Government of India, 24F/V.S./08/554 dated February 27, 2008. The following districts showed zero reporting and registration of deaths: Bijnor, Jyotibaphulenagar, Gautambudhnagar, Mathura, Badaun, Lakhimpur-kheri, Sitapur, Hardoi, Unnao, Kannauj, Auraiya, Hamipur, Mahoba, Fatehpur, Kaushambi, Barabanki, Ambedkarnagar, Sultanpur, Bahraich, Shirawasti, Balrampur, Sant Kabir Nagar, and Sant Ravidas Nagar.
[350] Human Rights Watch interview with official at the Registrar General's Office (who requested anonymity), New Delhi, March 18, 2009.
[351] Ibid.
[352] Human Rights Watch interview with Anjani Kumar, activist, Vatsalya, Lucknow, March 16, 2009.
[353] Human Rights Watch interviews with ANMs and families of deceased pregnant women, Rae Bareilly, Unnao, and Chitrakoot districts, February and March 2009.
[354] Human Rights Watch interview with activists and families, Rae Bareilly and Barabanki districts, March and June 2009.
[355] Ibid.
[356] Human Rights Watch interview with superintendent (name withheld), community health center, Unnao district, March 3, 2009. For more details about the registration duties of ANMs and superintendents of CHCs, see below, Appendix IV.
[357] Human Rights Watch interview with Vimal V. (pseudonym) panchayat mitra, village RB-5 (name withheld), Rae Bareilly district, February 26, 2009.
[358] Human Rights Watch interview with panchayat mitra (who chose to remain anonymous), village C-3, Chitrakoot district, March 6, 2009.
[359] Human Rights Watch interviews with families and friends of deceased pregnant women, February, March, and June 2009.
[360] Government of Uttar Pradesh, Department of Health-7, Government Order no. 2775/5-7/2002-V.S.-6/2000 dated 2002. The Uttar Pradesh government has made the scheme applicable to the following hospitals: Hospitals connected with Sanjay Gandhi Post Graduate Institution, Lucknow; central government hospitals having more than 300 beds; state government hospitals having more than 300 beds; and hospitals connected with all medical colleges of the state.
[361] Human Rights Watch interview with an official from the Office of the Registrar General (who requested anonymity), New Delhi, March 19, 2009.
[362] Constitution of India, Seventh Schedule, List III, entry 30: Vital statistics including registration of births and deaths.
[363] Human Rights Watch interview with K.K.Roy, human rights activist and practicing lawyer, Allahabad, March 5, 2009.
[364] Human Rights Watch interview with Latha L. (pseudonym), staff nurse, community health center, location withheld, March 15, 2009.
[365] Human Rights Watch interviews with health staff in community health centers and district hospitals, Rae Bareilly, Unnao, and Lucknow districts, February and March 2009.
[366] Human Rights Watch interview with Ruth Daniel, President, Uttar Pradesh State Nurses Association, Lucknow, March 10, 2009.
[367] Human Rights Watch interviews with women, Rae Bareilly, Unnao, and Chitrakoot districts, February and March 2009.
[368] Human Rights Watch interviews with women beneficiaries of JSY, activists, and ASHAs, Unnao and Chitrakoot districts, March 2009.
[369] Human Rights Watch interviews with seven ASHAs and women, Rae Bareilly, Unnao, and Chitrakoot districts, February and March 2009.
[370] Human Rights Watch interviews with state health officials from directorates of health and family welfare and district health officials from Unnao, Lucknow, and Chitrakoot, February and March 2009.
[371] Human Rights Watch interview with health staff (who chose to remain anonymous), district hospital, Unnao, March 4, 2009.
[372] Human Rights Watch interview with officer-2 (who requested anonymity), Lucknow, March 12, 2009.
[373] Rogi Kalyan Samitis, National Rural Health Mission, https://mohfw.nic.in/NRHM/RKS.htm (accessed May 21, 2009). The governing body of the RKS consists of T members from local self-governance institutions (panchayats), nongovernmental organizations, local elected representatives, and officials.
[374] Ibid., para. 5.5.2.The governing body of the RKS has the power to establish a public grievance mechanism that should be implemented.
[375] Ibid.
[376] Human Rights Watch group interview with Trishna T. (pseudonym) and others, women who had recently delivered, village C-1 (name withheld), Chitrakoot district, March 7, 2009.
[377] Human Rights Watch interviews with Shakuntala Joshi, health and human rights activist, SAHAYOG, Lucknow, February 26, 2009; K.K.Roy, lawyer representing pregnant women or mothers through public interest litigations in the Allahabad High Court, Allahabad, March 5, 2009.
[378] SAHAYOG, "Evidence submitted to the United Kingdom All Party Parliamentary Group on Population, Development, and Reproductive Health," http://www.appg-popdevrh.org.uk/Publications/Maternal%20Morbidity%20Hearings/Written%20 Evidence/7.5.1%20SAHAYOG%20Evidence.doc, unpaginated, case A (accessed August 25, 2009).
[379] Human Rights Watch interviews with Shakuntala Joshi.
[380] Human Rights Watch interviews with activists, women, and families from Rae Bareilly, Unnao, Lucknow, Barabanki, and Chitrakoot districts, February, March, and June 2009.
[381] Human Rights Watch interviews with Jashodhara Dasgupta and Shakuntala Joshi, activists from SAHAYOG, Lucknow, December 12 and February 25, 2009 respectively.
[382] Human Rights Watch interview with Saroj S., Dalit woman who had recently delivered, Chitrakoot district, March 7, 2009.
[383] Human Rights Watch phone discussion with district official (who requested anonymity), Unnao district, August 24, 2009.
[384] Human Rights Watch interviews with senior official (name withheld) overlooking nursing operations in the state, Lucknow, March 12, 2009, Jashodhara Dasgupta, Dr. Neelam Singh, and Ruth Daniel, December 12, 2009.
[385] Human Rights Watch interview with senior official (name withheld) overlooking nursing operations in the state, Lucknow, March 12, 2009.
[386] Application from Aruna Kashyap to Director General (Family Welfare)/Public Information Officer, letter no. 27-3-2009-NHRM-1, dated March 31, 2009 seeking information about inquiries and outcomes involving permanent and contractual auxiliary nurse midwives; application from Aruna Kashyap to Director General (Medical and Health Services)/Public Information Officer, letter no. 27-3-2009-MHS-2, dated March 31, 2009, seeking information about inquiries and outcomes involving permanent and contractual doctors and staff nurses.
[387] Human Rights Watch interview with Latha L. (pseudonym), staff nurse, community health center, location withheld, March 15, 2009.
[388] Ibid.
[389] Human Rights Watch interview with senior official (name withheld) overlooking nursing operations in the state, Lucknow, March 12, 2009.
[390] Human Rights Watch interview with officer-4 (who requested anonymity), former senior official from the state health department, Lucknow, March 16, 2009, telephone conversation, April 17, 2009.
[391] International Covenant on Economic, Social and Cultural Rights (ICESCR), G.A. res. 2200A (XXI), 993 U.N.T.S. 3, entered into force January 3, 1976, acceded to by India on April 10, 1979,
[392] International Covenant on Civil and Political Rights (ICCPR), G.A. res. 2200A (XXI), 999 U.N.T.S. 171, entered into force March 23, 1976, acceded to by India on April 10, 1979.
[393]Convention on the Elimination of All Forms of Discrimination against Women (CEDAW), G.A. res. 34/180, entered into force September 3, 1981, ratified by India on July 9, 1993.
[394]Convention on the Rights of the Child, G.A. res. 44/25, U.N. Doc. A/44/49, entered into force September 2 1990, ratified by India on December 11, 1992.
[395] See for example, Committee on Economic Social and Cultural Rights (CESCR), "The nature of States parties obligations (Art. 2, para. 1)," General Comment 3, 1990, E/1991/23.
[396]Vishaka v. State of Rajasthan, AIR 1997 SC 3011.
[397] International Covenant on Civil and Political Rights General Comment 6, The right to life (Article 6), UN ESCOR Human Rights Commission, 16th Session, UN Doc HRI/GEN/1/Rev. 1 (1994) para.5.
[398]Ibid.
[399] General Comment No. 28: Equality of rights between men and women (article 3) CCPR/C/21/Rev.1/Add.10, para. 10.
[400] Concluding Observations of the Human Rights Committee: Nepal, Concluding Observations/Comments, at 8, 12-19, UN Doc 10/11/94, CCPR/C/79/Add42 (1994).
[401]See for example, Concluding Observations of the Human Rights Committee: Peru, UN Doc CCPR/C/79/Add72 (1996); Concluding Observations of the Human Rights Committee: Senegal, UN Doc CCPR/C/79/Add82. (1997). Concluding Observations of the Human Rights Committee: Sudan, UN Doc CCPR/C/79/Add 85 (1997); Concluding Observations of the Human Rights Committee: Bolivia, UN Doc CCPR/C/79/Add 74 (1997); Concluding Observations of the Human Rights Committee: Costa Rica, UN Doc CCPR/C/79/Add107 (1999); Concluding Observations of the Human Rights Committee: Mali, UN Doc CCPR/CO/77/MLI (2003).
[402] Concluding Observations of the Human Rights Committee: Sri Lanka, at para. 12, UN Doc CCPR/CO/79/LKA (2003).
[403] Concluding Observations of the Human Rights Committee: Mali, supra, n 115.
[404] Human Rights Committee, General Comment No. 31, "Nature of the legal obligation on States Parties to the Covenant" (2004), CCPR/C/21/Rev.1/Add.13, para. 8.
[405]UN Committee on Economic, Social and Cultural Rights (CESCR), "Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social and Cultural Rights," General Comment No. 14, The Right to the Highest Attainable Standard of Health, 2000, E/C.12/2000/4 (2000), http://www.unhchr.ch/tbs/doc.nsf/(symbol)/E.C.12.2000.4.En (accessed May 11, 2009), para. 14.
[406] Ibid., para. 21.
[407] Ibid., paras. 43 and 44.
[408] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, February 2003, E/CN.4/2003/58, para. 25; Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, February 2004, E/CN.4/2004/49, para. 29.
[409]Ibid., para. 11. Some of the underlying determinants health identified by the Committee are access to safe and potable water and adequate sanitation, an adequate supply of safe food, nutrition and housing, healthy occupational and environmental conditions, and access to health-related education and information, including on sexual and reproductive health. Further, in the context of availability of health care, the Committee has stated in para. 12 (a) of health care facilities, goods, and services "will include … the underlying determinants of health, such as safe and potable drinking water and adequate sanitation facilities, hospitals, clinics and other health-related buildings, trained medical and professional personnel receiving domestically competitive salaries, and essential drugs, as defined by the WHO Action Programme on Essential Drugs."
[410]Ibid.
[411] CEDAW, General Recommendation No. 24 (20th session, 1999) Article 12: Women and health, para. 31.
[412] CESCR, General Comment 14, para. 33.
[413] Ibid., para. 34.
[414] Ibid.
[415] Ibid.
[416] Ibid., para. 50.
[417] Committee on CESCR rights, General Comment 14, para. 33.
[418] Ibid., para. 35.
[419] Ibid.
[420] Ibid., para. 51. The private sector would arguably fall within the category of "individuals, groups, and corporations."
[421] Ibid., para. 33.
[422] Ibid. para. 36.
[423] Ibid.
[424] CEDAW, General Recommendation No. 24, para. 17.
[425]Ibid para. 26
[426]Ibid. para. 27.
[427] Ibid. para. 37.
[428] Ibid. para. 37.
[429] Ibid., para. 52.
[430] Ibid.
[431]Ibid., para. 37.
[432]UN Committee on the Rights of the Child, "Adolescent health and development in the context of the Convention on the Rights of the Child," General Comment No. 4, CRC/GC/2003/4, http://www.unhchr.ch/tbs/doc.nsf/898586b1dc7b4043c1256a450044f331/504f2a64b22940d4c1256e1c0042dd4a/$FILE/G0342724.pdf (accessed February 3, 2009), para. 31.
[433] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, August 2008, A/63/263, para. 8.
[434] Ibid. Several other reports of the UN Special Rapporteur discuss accountability in the context of health. See for example, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, October 2004, A/59/422, paras. 36-41, where he discusses the importance of accountability in the context of achieving the Millennium Development Goals, including goal 5 on maternal mortality reduction; Human Rights Council, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, A/HRC/7/11, January 31, 2008, http://daccessdds.un.org/doc/UNDOC/GEN/G08/105/03/PDF/G0810503.pdf?OpenElement (accessed June 23, 2009), paras. 65, 99-106.
[435] Ibid., para. 9.
[436] Ibid.
[437] Reports of the UN Special Rapporteur on the right to health, August 2008, para. 9; October 2004, paras. 36-41; January 2008, paras. 65, 99-106.
[438] Report of the UNSR on the right to health, August 2008, para. 12.
[439] ICESCR, art. 2.
[440] CESCR, General Comment 14, para. 31.
[441] ICCPR, article 2; CESCR, General Comment 14, para. 37.
[442] ICESCR, art. 2.
[443] CESCR General Comment 3, para. 4.
[444] Ibid., para. 30.
[445] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, January 2008, A/HRC/7/11, para. 50.
[446] CESCR, General Comment 3, para. 9.
[447] For JSY eligibility criteria, please refer to JSY: Features and Frequently Asked Questions and Answers, 2006.
[448] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, January 2008, A/HRC/7/11, para. 65.
[449] Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, A/61/338, September 13, 2006, http://www2.essex.ac.uk/human_rights_centre/rth/docs/GA%202006.pdf (accessed June 23, 2009), para. 28 (e).
[450] Committee on Economic, Social and Cultural Rights, "Reporting by States parties," General Comment 1, E/1989/22, 1989, para. 3.
[451] Ibid.
[452] Ibid., para. 6.
[453] General Comment No. 14, para. 43 (f).
[454] Ibid.
[455] Report of the UNSR on health, January 2008, para. 48.
[456] General Comment 20, para. 41.
[457]General Comment 14, para. 56.
[458] Ibid., para. 21.
[459] General Comment 1, para. 8.
[460] See section above, titled "Key Gaps in Accountability."
[461] General Comment 3, para. 9.
[462] Ibid., para. 2.
[463] General Comment 14, para. 31.
[464] Commission of Human Rights, Report of the Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, E/CN.4/2005/51, February 11, 2005, http://daccessdds.un.org/doc/UNDOC/GEN/G05/108/93/PDF/G0510893.pdf?OpenElement (accessed June 23, 2009), para.34; Report of the UNSR on health, January 2008, para. 51 (b).
[465] General Comment 3, para. 11.
[466] Report of the UNSR on health, January 2008, para. 51(d).
[467] Ibid., para. 52.
[468] Article 2.1 of the ICCPR states and Article 2.2 of the ICESCR states that states party to each Covenant undertake to guarantee that the rights enunciated therein "without discrimination of any kind as to race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status."
[469] Report of the Special Rapporteur on the right to health, September 2006, para. 28(b).
[470] General Comment 14, para.18; UN Committee on Economic, Social and Cultural Rights, "Non-Discrimination in Economic, Social and Cultural Rights (art. 2 para. 2)," General Comment 20, E/C.12/GC/20 (2009), http://74.125.153.132/search?q=cache:YZAXM-YomoAJ:www2.ohchr.org/english/bodies/cescr/docs/gc/E.C.12.GC.20.doc+Non-Discrimination+in+Economic,+Social+and+Cultural+Rights&cd=1&hl=en&ct=clnk (accessed July 28, 2009), para. 7.
[471] CESCR, General Comment 14, para. 18.
[472] General Comment 20, paras. 27-35.
[473] General Comment 20, para. 13.
[474] General Comment 14, para. 18; para. 7.
[475] Human Rights Watch phone discussions with public health experts and women's rights activists from India, November 2008 to February 2009.
[476] Ibid.
[477] Ibid.
[478] See section above, titled "Poor follow-up of pregnancies" for more information about jurisdictional division of health workers.
[479] UN Human Rights Committee, "Nature of the General Legal Obligation Imposed on State Parties to the Covenant," General Comment 31, CCPR/C/21/Rev.1/Add.13 (2004), http://www.unhchr.ch/tbs/doc.nsf/0/58f5d4646e861359c1256ff600533f5f?Opendocument (accessed July 28, 2009), Para. 16.
[480] CESCR, General Comment No. 14, Ibid., para. 59, UN Human Rights Committee, General Comment 31, para. 15.
[481] Ibid.
[482] The European Court of Human Rights has repeatedly held that where death or serious injury occurs at the hands of state agents during a law enforcement operation, an effective investigation should examine whether the operation was planned and controlled by the authorities so as to minimize, to the greatest extent possible, any risk to life.See McCann and others v. the United Kingdom, judgment of 27September 1995, Series A no. 324, pp. 45-46, §§ 146-50 and p. 57, §194; Andronicou and Constantinou v. Cyprus, judgment of 9 October 1997, Reports 1997-VI, pp. 2097-98, § 171, p.2102, § 181, p. 2104, § 186, p. 2107, § 192 and p. 2108, § 193 and Hugh Jordan v. the United Kingdom, no. 24746/95, §§ 102 – 104, ECHR 2001-III; Makaratzis v. Greece [GC], judgment of 20 December 2004, no. 50385/99, § 49-55.
[483] See for example, General Comment 14, para. 3; CEDAW, General Recommendation No. 24, para. 28.
[484]Committee on ESC Rights, ibid., para. 11.
[485] Ibid., para. 14.
[486]Ibid., para. 35.
[487]Ibid., para. 36.
[488] Ibid., para. 39.
[489] Ibid., para. 39;Report of the UNSR on health, February 2004, para. 46.
[490] Ibid.
[491] Ibid., para. 45.
[492] Report of the UNSR on health, February 2004, para. 46.
[493] Reports of the UNSR on health, August 2008, para. 9; October 2004, paras. 36-41; January 2008, paras. 65, 99-106.
[494] CESCR, General Comment 14, para. 57.
[495] Report of the UNSR on health, August 2008, para. 13. See also Report of the UNSR on health, September 2006, para. 28(d) where he says that "right to health demands accountability of various stakeholders, including… national Governments, international organizations…"
[496] Paris Declaration on Aid Effectiveness, http://www.oecd.org/dataoecd/11/41/34428351.pdf (accessed June 23, 2009).
[497] For a list of countries and organizations that have adhered to the Paris Declaration, see "Countries, Territories, and Organizations Adhering to the Paris Declaration," http://www.oecd.org/document/22/0,3343,en_2649_3236398_36074966_1_1_1_1,00.html (accessed June 23, 2009).
[498] Paris Declaration, para. 16.
[499] Ibid., para. 17.
[500] Ibid., para. 49.
[501] Accra Agenda for Action, Third High Level Forum on Aid Effectiveness, Ghana, September 2-4, 2008, http://www.oecd.org/dataoecd/58/16/41202012.pdf (accessed June 23, 2009), para. 10.
[502] Ibid., para. 22.
[503] Ibid., para. 23(b).
[504] Ibid., para. 23(c).
[505] Ibid., para. 24(a).
[506] NRHM Framework for Implementation, p. 8.
[507] Since the draft legislation is at its early stages and is open for comments, Human Rights Watch is still in the process of consulting with public health experts and lawyers to evaluate its effectiveness.
[508]Ratlam v.Vardhichand and Others, 1960 Cri. L.J. 1075; CESC Ltd. v. Subash Chandra Bose, AIR 1992 SC 573; Mahendra Pratap Singh v. State of Orissa, AIR 1997 Ori 37; Consumer Education and Research Center v. Union of India, (1995) 3 SCC 42.
[509]Consumer Education and Research Center v. Union of India, (1995) 3 SCC 42.
[510]Mahendra Pratap Singh v. State of Orissa, AIR 1997 Ori 37.
[511]S. K. Garg v. State of Uttar Pradesh, as cited in Fundamental Right to Health and Public Care, p. 22. While decisions of the Supreme Court are binding on the Indian central and all state governments, decisions of the Uttar Pradesh High Court are only binding on the Uttar Pradesh government.
[512] (1996) 4 SCC 37.
[513] Ibid.
[514] Ibid.
[515] Ibid.
[516] Human Rights Watch phone discussion with Dr. Usha Ramanathan, April 18, 2009.
[517] Registration of Births and Deaths Act, 1969, section 10.
[518] Ibid., section 10.
[519] Ibid., section 8.
[520] Uttar Pradesh Registration of Birth and Death Rules, 2002.
[521] Registration of Births and Deaths Act, 1969, section 7(1).
[522] Uttar Pradesh Registration of Birth and Death Rules, 2002, Rule 5 and Form No. 2. Rule 5 read with Form No. 2 lays out the death report form. Rule 8 read with Form No. 6 gives the form in which the death certificate should be issued.
[523] Government of Uttar Pradesh, Department of Health-7, Government order no. 252/5-7-2008-V.S.2/97 TC, dated February 12, 2008. Formerly, nurse-midwives were appointed deputy registrars by an order dated June 17, 2004.
[524] Human Rights Watch interviews with Anjani Kumar and another, activists from Vatsalya, Lucknow, March 16, 2009.